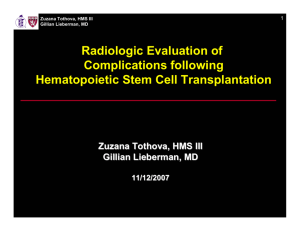
Round Pneumonia in Adults
advertisement

Joseph Garland, HMS IV Gillian Lieberman, MD Round Pneumonia Joseph Garland, HMS IV Gillian Lieberman, MD Joseph Garland, HMS IV Gillian Lieberman, MD Case 1: Mr. H Mr. H is a 45-year-old man who presents with a 4 day history of full-body myalgias, headaches and fever to 103˚F. He also complains of sharp leftsided chest pain worse on deep inspiration. Joseph Garland, HMS IV Gillian Lieberman, MD Other Relevant Information ROS: otherwise negative PMH: asthma, one episode of pneumonia 6m ago requiring hospitalization SH: Nonsmoker, no IVDU, occasional EtOH. PE: T=101.6˚F, HR=120. Crackles heard in mid-lung field on the left. Otherwise wnl. Labs: WBC 19.7, otherwise WNL. Joseph Garland, HMS IV Gillian Lieberman, MD A chest X-ray was obtained… Joseph Garland, HMS IV Gillian Lieberman, MD Mr. H, Chest Radiographs PACS, BIDMC PACS, BIDMC This was called a LLL pneumonia, cannot rule out infarct or malignancy. Do you agree? Joseph Garland, HMS IV Gillian Lieberman, MD Mr. H, Chest Radiographs – Magnification of Lesion PACS, BIDMC The lateral view suggests the mass is in the lingula. PACS, BIDMC Joseph Garland, HMS IV Gillian Lieberman, MD The patient went on to have a CT scan…Why? Joseph Garland, HMS IV Gillian Lieberman, MD The Solitary Pulmonary Nodule Has a lengthy differential… Neoplastic (malignant or benign) Bronchogenic carcinoma Metastasis Lymphoma Carcinoid Hamartoma Connective tissue and neural tumors - Fibroma, neurofibroma, blastoma, sarcoma Inflammatory (infectious) Granuloma - TB, histoplasmosis, coccidioidomycosis, blastomycosis, cryptococcosis, nocardiosis Lung abscess Round pneumonia Hydatid cyst Inflammatory (noninfectious) Congenital Rheumatoid arthritis Wegener granulomatosis Sarcoidosis Lipoid pneumonia Arteriovenous malformation Sequestration Lung cyst Miscellaneous Pulmonary infarct Round atelectasis Mucoid impaction Progressive massive fibrosis Reference: Sharma S, Navaratnam S. “Solitary Pulmonary Nodule.” E-Medicine. 2004. http://www.emedicine.com Joseph Garland, HMS IV Gillian Lieberman, MD In this case, we are most worried about differentiating Pneumonia (based on clinical presentation) and Bronchogenic carcinoma (the most concerning possibility) Joseph Garland, HMS IV Gillian Lieberman, MD Mr H, CT with IV contrast PACS, BIDMC Joseph Garland, HMS IV Gillian Lieberman, MD Mr H, CT with IV contrast Inferior lobar bronchus R intermediate bronchus Superior division Lingular bronchus Major fissure PACS, BIDMC Joseph Garland, HMS IV Gillian Lieberman, MD Mr H, Coronal CT with IV contrast 5.6 x 2.9 cm peripheral area of consolidation in the lingula PACS, BIDMC Joseph Garland, HMS IV Gillian Lieberman, MD Treatment started for CAP Mr H was started on Levofloxacin 500 mg PO QD for clinical pneumonia. His CXR and CT could not rule out malignancy. He clinically improved and returned for a follow-up Chest X-ray two months later… Joseph Garland, HMS IV Gillian Lieberman, MD Mr. H, Follow-up Chest Radiographs (2 months later) PACS, BIDMC PACS, BIDMC The lesion has resolved. The pleural thickening on the left is unchanged in 4 yrs. Joseph Garland, HMS IV Gillian Lieberman, MD Case 2: Mr. G. Mr G is a 75 yo man who presented to the emergency department with a fever to 104˚F and chills x 1 day, and mild shortness of breath. Joseph Garland, HMS IV Gillian Lieberman, MD Other Relevant Information ROS: otherwise unremarkable PMH: CAD s/p MI (1y ago), Hypertension, permanent pacemaker SH: 20 pack-year smoking history, quit 30y ago PE: VS are stable, rest of exam is normal Labs: WBC of 20.9, otherwise WNL Joseph Garland, HMS IV Gillian Lieberman, MD As part of a fever workup, a chest X-ray was obtained… Joseph Garland, HMS IV Gillian Lieberman, MD Mr. G, Chest Radiographs 2.5 m poorly-defined nodule Left Upper Lobe PACS, BIDMC PACS, BIDMC Joseph Garland, HMS IV Gillian Lieberman, MD What should the next step be? Clinical presentations suggestive respiratory tract infection. Chest radiograph findings are atypical for (but not inconsistent with) pneumonia. Again, the major concern is “benign vs malignant?” Joseph Garland, HMS IV Gillian Lieberman, MD The patient went on to have a CT scan… Joseph Garland, HMS IV Gillian Lieberman, MD Mr G, CT without contrast PACS, BIDMC Joseph Garland, HMS IV Gillian Lieberman, MD Mr G, CT without contrast PACS, BIDMC Joseph Garland, HMS IV Gillian Lieberman, MD Mr G, CT without contrast PACS, BIDMC Joseph Garland, HMS IV Gillian Lieberman, MD Mr G, CT without contrast Tethering of the major fissure PACS, BIDMC Joseph Garland, HMS IV Gillian Lieberman, MD Mr G, CT without contrast PACS, BIDMC Joseph Garland, HMS IV Gillian Lieberman, MD Mr G, CT without contrast – Soft Tissue Window Air bronchogram PACS, BIDMC Joseph Garland, HMS IV Gillian Lieberman, MD Findings Findings may be consistent with round pneumonia, but are suggestive of invasive adenocarcinoma with bronchioloalveolar component. Also consider post-obstructive pneumonia. Pt was started on Levofloxacin 500mg PO QD for 14 days. He was scheduled for CT-guided biopsy but, after clinical improvement, this was postponed. Joseph Garland, HMS IV Gillian Lieberman, MD Mr. G, Follow-up Chest Radiographs (2 weeks later) PACS, BIDMC PACS, BIDMC Joseph Garland, HMS IV Gillian Lieberman, MD Mr. G, Initial and Follow-up Chest Radiographs Initial Presentation 2 weeks later, s/p antibiotics PACS, BIDMC PACS, BIDMC Though still present, the nodule has partially resolved. A follow-up in 4w was recommended. Joseph Garland, HMS IV Gillian Lieberman, MD Round Pneumonia First reported in the radiology literature in 1954 (though it was mentioned in the surgical literature in 1940). Describes any pneumonia presenting as a nodule or “coin lesion” It is rare, it accounts for less than 1% of “coin lesions” of the lung Joseph Garland, HMS IV Gillian Lieberman, MD Varied Clinical Presentations Presentation may be with acute or subacute symptoms of communityacquired pneumonia Symptoms may also be mild, mimicking a viral syndrome or bronchitis Patients may even be completely asymptomatic. Joseph Garland, HMS IV Gillian Lieberman, MD Radiologic Features On Chest films: Rounded lesion. Air bronchograms may be present. They are only present in 17% of patients with round pneumonia and are not generally helpful because they can also be seen in adenocarcinoma and bronchioloalveolar carcinoma. Recent Chest films are often helpful. 2-3cm masses that appeared in the last 2-6 weeks are more likely infectious than neoplastic. On CT: heterogeneous mass of soft-tissue attenuation that can have spicules, air bronchograms, pleural thickening and satellite lesions. Joseph Garland, HMS IV Gillian Lieberman, MD Pediatric Round Pneumonia Round pneumonia is more commonly a disease of children. It is a diagnosis considered in younger patients with classic clinical picture of pneumonia and a coin lesion on chest film. Children rarely get a CT if the clinical picture fits. Joseph Garland, HMS IV Gillian Lieberman, MD Pediatric case of Round Pneumonia Courtesy Dr. Jason Handwerker, BIDMC Courtesy Dr. Jason Handwerker, BIDMC A typical presentation for this would be a very high fever in a child. Joseph Garland, HMS IV Gillian Lieberman, MD Theories on Formation Round pneumonia may result from an infectious focus that spreads centrifugally through the pores of Kohn and canals of Lambert, or by destroying the walls of alveoli. However, children have underdeveloped pores of Kohn and canals of Lambert, suggesting that in children, the “roundness” may actually occur because the lack of interalveolar pathways limits the spread of the organism. Round pneumonia may also represent incomplete resolution of a lobar pneumonia. Joseph Garland, HMS IV Gillian Lieberman, MD Relevant Anatomy Pores of Kohn: openings in the alveolar walls connecting adjacent alveolar lumens Canals of Lambert: connections between terminal bronchioles and adjacent alveoli They allow for collateral ventilation and also are a means of bacterial spread in the lungs. Adapted from http://www.mevis.de/~hhj/Lunge/ima/InfKohnP.htm Joseph Garland, HMS IV Gillian Lieberman, MD The Offending Agents Usually Streptococcus pneumoniae There are also reports of Klebsiella pneumoniae, Mycobacterium tuberculosis, and Coxiella burnetii (Q fever) presenting with a round pneumonia. Joseph Garland, HMS IV Gillian Lieberman, MD Treatment Standard treatment with antibiotics that cover Strep. pneumoniae pneumonia should suffice. Always order a follow-up chest film to document resolution of the lesion, and to rule out a malignant process. Joseph Garland, HMS IV Gillian Lieberman, MD When to Consider Round Pneumonia Suspect round pneumonia in an adult patient who present with a pulmonary mass, especially if s/he has respiratory infection symptoms, is a young nonsmoker, and has no other findings to suggest malignancy. A recent normal chest radiograph is also helpful. Remember! Any patient with a pulmonary nodule that does not decrease in size or resolution after antibiotic treatment should be further assessed with bronchoscopy or transthoracic needle biopsy. Joseph Garland, HMS IV Gillian Lieberman, MD 41-year-old female nonsmoker with fever and bibasilar rales. Courtesy Dr. Andetta Hunsaker, BWH Joseph Garland, HMS IV Gillian Lieberman, MD References Ackerman LV, et al. 1954. “Localized Organizing Pneumonia: Its Resemblance to Carcinoma.” AJR. 71(6): 988-996. Antón E. 2004. “A Frequent Error in Etiology of Round Pneumonia.” Chest. 125:1592-1593 Durning SJ, et al. 2003. “Pulmonary Mass in Tachypneic, Febrile Adult.” Chest. 124:372-375. Greenfield H, Gyepes MT. 1964. “Oval-Shaped Consolidation Simulating New Growth of the Lung” AJR. 91(1):125-129. Lossos IS, Breuer R. 1989. “Round Pneumonia.” Isr J Med Sci. 25:713-714. Fox LA, Hunsaker AR. 1997. “Localized Organizing (Round) Pneumonia.” BrighamRad. http://brighamrad.harvard.edu/Cases/bwh/hcache/210/full.html Price J. 1999. “Round Pneumonia and Focal Organizing Pneumonia are Different Entities.” AJR. 172:549. Sharma S, Navaratnam S. 2004. “Solitary Pulmonary Nodule.” E-medicine. http://www.emedicine.com Wagner AL, et al. 1998. “Radiologic Manifestations of Round Pneumonia in Adults.” AJR. 170:723-726. http://oac.med.jhmi.edu/Pathology/Idmicro/Bacteria/137B.html http://www.mevis.de/~hhj/Lunge/ima/InfKohnP.htm Beth Israel Deaconess Medical Center PACS system. Joseph Garland, HMS IV Gillian Lieberman, MD Special Thanks Dr. Maryellen Sun, BIDMC. Dr. Phillip Boiselle, BIDMC. Dr. Jason Handwerker, BIDMC. Dr. Andetta Hunsaker, BWH. Ms. Pamela Lepkowski, BIDMC.

![Title of the Presentation Line 1 [36pt Calibri bold blue] Title of the](http://s2.studylib.net/store/data/005409852_1-2c69abc1cad256ea71f53622460b4508-300x300.png)
![[Enter name and address of recipient]](http://s3.studylib.net/store/data/006894526_1-40cade4c2feeab730a294e789abd2107-300x300.png)