BIO 142 Unit 2 Learning Objectives
advertisement

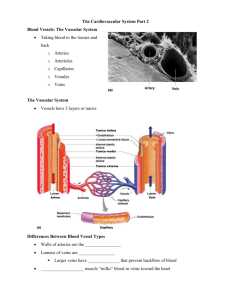
NOVA – ELI BIO 142 Unit 2 Learning Objectives Upon your successful completion of this unit, you will be able to do the following. Chapter 19 – Cardiovascular System: Heart 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Describe general function of the cardiovascular system. Differentiate the three types of blood vessels: arteries, veins, and capillaries. State a major function of the heart. Briefly describe the following significant anatomic features of the heart: a. Name the four chambers of the heart. b. State the type of blood (oxygenated or deoxygenated) within the right and left chambers of the heart. c. Name the great vessels (arteries and veins) opening into and emerging out of the heart. d. Name the two sets of valves located within the heart. Briefly describe the differences between the pulmonary and systemic circulations with respect to the following: a. location in the heart, b. the type of blood the circulation carries, c. the functions, and d. the pattern of blood flow within each circulation, including each chamber, valve, and great vessel. Begin at the right atrium (use figure 19.4). Describe the location and position of the heart in the thoracic cavity. Name the structural components of the pericardium. Describe the function of the pericardium and the serous fluid within the pericardial cavity. Name the vessels located within the coronary sulcus, the anterior and posterior interventricular sulci on the surface of the heart, and state one major function of those vessels. Name the three distinctive layers that compose the wall of the heart. Identify and briefly describe the function of the following structures within the heart: a. Right atrium: I. Fossa ovalis/foramen ovale. II. Coronary sinus. III. Right atrioventricular (AV) valve or tricuspid valve. b. Right ventricle: I. Trabeculae carneae. II. Papillary muscle. III. Chordae tendinae. IV. Pulmonary trunk. V. Pulmonary semilunar valve. c. Left atrium: I. Pulmonary veins. II. Left atrioventricular (AV) valve (aka bicuspid valve or mitral valve). d. Left ventricle: 1 NOVA – ELI 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. I. Aorta. II. Aortic semilunar valve. Explain heart sounds (Use clinical view page 745 as reference). Cardiac muscle. a. Briefly describe the characteristics of cardiac muscle. b. Name two structures that make up the intercalated discs. c. State the functions of intercalated discs. d. Name structures in the cardiac muscle that support aerobic cellular respiration. Coronary blood vessels. a. Name two coronary arteries that branch off from the ascending aorta. b. State the general function of coronary arteries. c. Name two major branches of the right and left coronary arteries. d. Name three major veins that drain deoxygenated blood from the heart muscle. e. Name the largest vein that drains deoxygenated blood into the right atrium. The heart’s conduction system. a. Identify the four structures that make up the heart’s conduction system in the right order (Use figure 19.14), and state a general function of the conduction system. b. Briefly explain why the sinoatrial (SA) node is referred to as the pacemaker of the heart. Innervation of the heart. a. State a general function of the sympathetic and parasympathetic innervation to the heart. b. Differentiate the sympathetic and parasympathetic innervation to the heart with respect to the following (Use figure 19.14): I. Receptors. II. Control center. III. Sensory & Motor nerves. IV. Response of the effector (cardiac muscle). Using figure 19.15, briefly explain the association between the heart’s conduction system and cardiac muscle contraction, a. in the cells of atria. b. in the cells of ventricle. Using figure 19.17, briefly explain the initiation and spread of an action potential through the heart’s conduction system. Using figure 19.19, briefly explain why an extended refractory period in the cardiac muscle prevents tetany. Using the electrocardiogram (ECG) recording in figure 19.20a, briefly describe what the following waves and segments of an ECG represent: a. P wave. b. QRS complex. c. T wave. d. PQ segment. e. ST segment. f. PR interval. g. QT interval. Define systole and diastole of the cardiac cycle. 2 NOVA – ELI 22. Briefly explain the pressure changes during the contraction and relaxation of the heart muscle. 23. Explain the role of pressure changes in a. movement of blood flow within the heart, and b. opening and closing of the heart valves. 24. Define cardiac output (CO). 25. Calculate the cardiac output (CO) at rest, with a heart rate of 75 beats per minute and a stroke volume of 70mL. 26. Calculate the cardiac output during exercise, with heart rate of 150 beats per minute and a stroke volume of 100mL. 27. Define cardiac reserve. 28. Variables that influence heart rate. a. Define chronotropic agents. b. Explain the role of sympathetic nerves as positive chronotropic agents. c. Explain the role of parasympathetic nerves as negative chronotropic agents. d. Describe the atrial reflex. 29. Variables that influence stroke volume (SV). a. Define stroke volume. b. Name three variables that influence stroke volume. c. Briefly explain how venous return influences stroke volume. d. Define inotropic agents. e. Name some positive inotropic agents. f. Name some negative inotropic agents. g. Explain how changes in afterload influence stroke volume. Chapter 20 – Cardiovascular System: Vessels and Circulation 1. Structure and function of blood vessels. a. Name three primary types of blood vessels. b. Name three basic tunics (layers) that make up the wall of blood vessels. c. Name the major components in each tunic. d. Differentiate between arteries and veins (Use table 20.1). 2. Arteries. a. Name three types of arteries and explain how you would differentiate the three types. (Use figure 20.3). b. Describe the functions of each type of artery. c. State the location of each type of artery. 3. Capillaries. a. Using figure 20.3, describe the anatomic structure and function of capillaries. b. Name three different types of capillaries. c. Using table 20.2, differentiate the three types of capillaries with regards to, I. their anatomic structure, II. their specific location, and 3 NOVA – ELI III. substances that can pass through the capillary wall. 4. Veins. a. Using figure 20.3, name and describe the anatomic structures of the three types of veins. b. State the general function of veins. c. Using figure 20.6, briefly explain why veins serve as blood reservoirs for the cardiovascular system. d. Explain what is a sinus, and give two locations where sinuses can be found in the body. 5. Two pathways of blood vessels. a. Name two major pathways of blood vessels. b. Define anastomosis. c. Name three different types of alternative anastomoses. d. Describe portal system. e. Name the sequence of blood vessels in a portal system: starting with an artery…… ……ending with a vein. f. Provide two locations where portal systems are found in the body. 6. Using figure 20.9, state the relationship between total cross sectional area and blood flow velocity. 7. Explain the significance of capillaries of having the greatest cross sectional area but the slowest blood flow. 8. Capillary exchange. a. Explain the exchange function of capillaries. b. Name three different exchange processes that occur across capillaries. c. Bulk flow. I. Explain the processes of bulk flow, reabsorption, and filtration. II. Define blood hydrostatic pressure. III. Define interstitial hydrostatic pressure. IV. Define blood colloid osmotic pressure. V. Define interstitial fluid colloid osmotic pressure. VI. Using the values provided in figure 20.10, learn to calculate the following pressures at the arterial end of the capillary and at the venous end of the capillary i. Net Hydrostatic Pressure (HP) = the difference between blood hydrostatic pressure and interstitial hydrostatic pressure. ii. Net Colloid Osmotic Pressure (COP) = the difference between blood colloid osmotic pressure and interstitial fluid colloid osmotic pressure. iii. Net Filtration Pressure (NFP) = HP -­‐ COP. VII. Using the value of NFP from figure 20.10, explain why filtration occurs at the arterial end and reabsorption occurs at the venous end of the capillary. 4 NOVA – ELI 9. 10. 11. 12. d. The role of lymphatic system. I. Explain why there is a slight excess of interstitial fluid under normal circumstances, even though filtration and reabsorption occur simultaneously at the capillary. II. Explain the role of lymphatic system. Local blood flow. a. Define local blood flow. b. Name four factors that influence local blood flow. c. Define angiogenesis. Blood pressure. a. Define blood pressure. b. Define blood pressure gradient. c. Define diastolic blood pressure. d. Define systolic blood pressure. e. Define pulse pressure. f. Define Mean Arterial Pressure (MAP). g. Calculate the MAP for a person with average blood pressure of 120/80 mm Hg. h. Using figure 20.11, determine the blood pressure in different types of blood vessels. i. Describe the advantage of low capillary blood pressure. j. Venous blood pressure I. Define venous return. II. Name two factors that help assist venous return to the heart. III. Briefly describe how the skeletal muscle pump and the respiratory pump help in returning blood back to the heart in the standing position. Resistance. a. Define resistance. b. Name three factors affecting resistance, and briefly explain how each of these factors affects blood flow in vessels. c. Give one clinical application example for each of these three factors. Relationship of blood flow to blood pressure gradients and resistance. a. Using the formula to calculate total blood flow, name two factors that affect blood flow. b. Using figure 20.13, describe how total blood flow can be increased by altering, I. blood pressure gradient, II. blood viscosity, III. blood vessel length, and IV. diameter of the blood vessels. c. Using figure 20.13, describe how total blood flow can be decreased by altering, I. blood pressure gradient, II. blood viscosity, 5 NOVA – ELI III. blood vessel length, and IV. diameter of the blood vessels. 13. Regulation of blood pressure and blood flow. a. Name three primary variables affecting blood pressure. b. Neural regulation of blood pressure. I. Short term regulation. i. Describe the short term mechanism of regulation of low blood pressure with regards to the following: a) Baroreceptors. b) Control center in medulla oblongata, 1) Cardiac center. 2) Vasomotor center. c) Sympathetic division pathway. d) Effector response: 1) heart. 2) blood vessels. c. Hormonal regulation of blood pressure. I. Describe how the following hormones involved in the Renin-­‐ Angiotensin System increase blood pressure: i. Angiotensin II. ii. Aldosterone. iii. Antidiuretic hormone (ADH). II. Describe how Atrial Natriuretic Peptide (ANP) is able to decrease blood pressure. 14. Blood flow distribution during exercise. a. Using figure 20.17, compare the total blood flow and distribution at rest and during exercise. b. Name the organs that receive an increased proportion of the cardiac output during exercise. c. Name the organs that receive a decreased proportion of the cardiac output during exercise. 15. Systemic Circulation: Vessels from and to the heart. a. Coronary circulation: Using figure 20.19, trace the arteries from the left ventricle that supply blood to the entire heart muscle. b. Using figure 20.19, trace the arteries from the left ventricle to the right subclavian artery and to the left subclavian artery. c. Hepatic Portal System: Using figure 20.25, name three veins that drain into the hepatic portal vein, and list the functions of hepatic portal system. d. Upper limb: Using figure 20.27, trace the arteries from the subclavian arteries to the fingers. e. Lower limb: Using figure 20.28, trace the arteries from the common iliac arteries to the toes. 6 NOVA – ELI f. Fetal circulation: Using figure 20.29, describe five changes from fetal cardiovascular structures to postnatal structures. 7