Morphofunctional considerations on the atrioventricular node arterial
advertisement

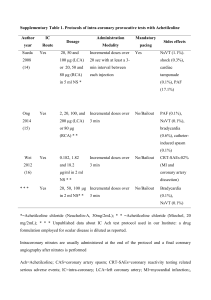
Rom J Leg Med 17 (2) 101 - 110 (2009) © 2009 Romanian Society of Legal Medicine Morphofunctional considerations on the atrioventricular node arterial vascularization Mugurel C. Rusu*1, Dumitru Ferechide2, George Cristian Curcă3, Dan Dermengiu3 Received: 2.02.2009/ Accepted: 3.05.2009 _____________________________________________________________________ Abstract: The atrioventricular node (AVN) is the relay station for electrical impulses passing from the atria to the ventricles. The arterial resources of the AVN are functionally relevant and may be interfered by various surgical procedures which deal with the cardiac valves. Our study aim to bring detailed evidences on the arterial supply of the AVN. We dissected and microdissected 50 human adult hearts without any known history or evident cardiac pathology, in order to evidence the arterial suppliers of the AVN; subepicardial dissections were continued in the interatrial septum (the triangle of Koch). We were able to define 5 morphological types (each with distinctive subtypes) of the atrioventricular node artery (AVNA) emerged at crux cordis: type I (22%, AVNA from the U-turn of the right coronary artery (RCA), the left retroventricular artery (RVA) absent), type II (18%, AVNA from PIVA, left RVA present), type III (34%, AVNA from the left RVA, PIVA from the RCA), type IV (AVNA from the bifurcation of the RCA into the PIVA and the left RVA – trifurcated RCA) and type V (AVNA from the circumflex artery). In 18% of specimens we found duplicated AVNA. In 22% of specimens, the AVN area was additionally supplied by the descending septal artery (right descending superior artery) originating from the sinoatrial artery, on the right side of the aorta. The origin of the AVNA, which is variable, and the accessory resources, such as the descending septal artery, can explain the possible individual occurrences of the cardiac rhythm alterations determined by coronary ischemia. Our AVNA types are all related to the atrioventricular and aortic valves and thus liable to damage during specific surgical procedures, interfering with the respective valves. Duplicated AVNAs must be kept in mind during the selective atrioventricular nodal artery catheterizations and AVNA must be evaluated angiographically prior to the interventions. Our study demonstrates that classical dissections combined with microdissections can still offer valuable informations for a pathologist assigning not only the mechanisms but also the morphological conditions of the cardiac arrest. A seek and search investigation is launched in every sudden cardiac death: the forensic pathologist make a good team with the anatomist retrieving very useful etiological data. Key words: coronary artery; conduction system; right atrium S udden cardiac death is an important issue not only clinically but also from the forensic perspective mainly because most jurisdictions demand for a full detailed autopsy. Revealing the cardiac etiology is even more complicate. Initiating factors may superimpose premorbid conditions such as cardiac anomalies, blood reduction flow conditions, etc., triggering cardiac arrest. In reaching conclusions a forensic pathologist must ________________________ *) Corresponding author; University of Medicine and Pharmacy “Carol Davila” 8, Bd. Eroilor Sanitari, RO-76241, Bucharest, Romania, Phone: +40722363705 E-mail: anatomon@gmail.com 1) Discipline of Anatomy and Embryology, Faculty of Dental Medicine, University of Medicine and Pharmacy Carol Davila, Bucharest, Romania; 2) Chair of Physiology, Faculty of Medicine, University of Medicine and Pharmacy Carol Davila, Bucharest, Romania; 3) National Institute of Legal Medicine “Mina Minovici”, Sos. Vitan Birzesti 9, Sector 4, 042122 – Bucharest, E-mail: cgcurca@yahoo.com 101 Rusu M C et al Morphofunctional considerations on the atrioventricular node arterial vascularization correlate and discriminate between terminal events and pathological findings [6]. A sudden cardiac arrest must have an acute etiopathogenetic mechanism and the forensic pathologist should seek acute morphological changes [7]. Therefore our study was conducted to demonstrate that classical dissections combined with microdissections can still offer valuable informations for a pathologist assigning not only the mechanisms but also the morphological conditions of the cardiac arrest. The atrioventricular node (AVN) acts as an electrical relay station for electrical impulses, passing from the atria to the ventricles [11]. The origin of blood supply to the conduction system is highly relevant to clinical and surgical procedures [2]. In severe conduction disturbances, patients tend to have specific coronary lesion distribution, involving either the anterior interventricular artery (AIVA) branches or a combination of this with significant right coronary artery (RCA) disease, compromising supply to sinoatrial or AV nodes [26]. The location of narrowings in the AIVA and RCA as the arteries supplying the conduction system was classified according to Mosseri et al. in 4 types: in type II pathological coronary anatomy involves the septal branches of the AIVA, in type III it compromises the blood supply to the sinoatrial or the atrioventricular node but not that one of the AIVA septal branches while type IV represents a combination of types II and III [13, 26]. As a major risk factor, the atherosclerotic or thrombotic obstruction of the sinoatrial node artery may induce severe heart rhythm disturbances or even sudden cardiac death [15]. Identification of the anatomical variants of the arterial blood supply to the SA and AV nodes may help in overcoming potential difficulties when treating arrhythmias and in mitral valve surgery [16], while the presence of coronary artery disease should be sought in every patient over 45 who presents with severe conduction disturbance [26]. Removal of the heart and careful examination of the major extramural arteries and veins is mandatory in every thorough autopsy conducted in sudden cardiac death. Intramural coronary arteries, such as sinus node and atrioventricular node atrial branches should be, as possible, search and examined: beneficial information may be gathered despite time consuming appearence. Examination of the conduction system may be further on necessary when the etiology still remains uncertain or a specific pathology is established (WPW sd., etc.). The best undertaken action is therefore to remove three tissue blocks containing the SA node, the AV node and the AV bundles, respectively [19]. The atrioventricular node artery The AVNA arises at crux cordis [16] and continues towards the triangle of Koch, close to the orifice of the coronary sinus, the endocardial surface of the right atrium, the middle cardiac vein, and the specialized conduction tissues in most hearts [17]. The AVNA and/or the AV conduction tissues arteries can be at risk of damage when ablative procedures are carried out at the base of the triangle of Koch. Suppliers of the AVN may be the RCA, the CxA or both [18]. Kügel’s artery and the DSA (RDSA) were discovered to supply 40% of AVN and 70% of the hearts [2]. Angelini pointed out that only two coronary atrial arteries are generally recognized with the specific expression of “atrial branch”: SNA and AVNA. Of the two, multiple branches, only one is frequently (but inconsistently) recognized in literature with a specific name, but no real definition: the Kügel’s artery. The same author emphasized that the generally understood attribute of any so-called Kugel’s artery is that it connects an anterior coronary artery located around the aortic root (the LCA, the CxA or the RCA) to a posterior arterial branch (the RCA or the CxA) in the coronary groove [4]. 102 Romanian Journal of Legal Medicine Vol. XVII, nr. 2, 2009 The descending septal artery (right descending superior artery) The blood supply to the upper ventricular septum in the region of the conduction system is more abundant than literature suggests. A significant arterial contribution to the upper ventricular septum from the proximal segment of the RCA, or one of its early branches, was found in 77% of the hearts studied by Taylor, who named these contributors as „descending septal arteries (DSA)”. In 68% of the hearts, the DSAs supplied the region of the proximal conduction system [22]. The DSA was later called „Right Descending Superior Artery (RDSA)” by Abuin [1, 2], who evaluated its distribution as being at the level of the bundle of His and the area within the triangle of Koch, including the AVN [2]. Kügel's artery, DSA (RDSA) and SNA, were discovered as being affected by the surgical procedures performed [1]. Our study aimed to bring detailed evidence regarding the arterial suppliers of the atrioventricular node in humans and to evaluate the atrioventricular node artery morphological patterns. We also took into account the considerations of Abuin and Nieponice, who claimed that classical dissection techniques proved useless in the efforts of following the atrial vessels to the nodal target, which deterred many anatomists from the attempt [2], and intended to demonstrate that classical disssections combined with microdissections can still offer valuable informations. Materials and methods We performed the present study by dissecting 50 human adult hearts, in compliance with the acting ethical rules of our institution. Complete subepicardial dissections of the coronary arteries were performed. In those specimens, with the sinoatrial artery emerged from the right coronary artery, the presence of the descending septal artery was observed and, if present, that artery was dissected/microdissected in the posterior wall of the right atrium. The arteries at the level of the crux cordis, on the diaphragmatic surface of the heart, were also identified, and the atrioventricular node arteries were dissected within the triangle of Koch, after removing/reflecting the anterior wall of the right atrium. The topography at the level of the triangle of Koch was evaluated in accordance to the description of Yanagawa and Nakajima (2009), who described its base as being formed by the opening of the coronary sinus, the apex resinding at the AV septum (right atrial region of the membranous septum), the two sides bordered by the septal leaflet of the tricuspid valve and the tendon of Todaro; according to these authors, AVN is connected to AVB under the fibrous ring [25]. We defined as dominant coronary arteries those arteries sending the posterior interventricular artery, PIVA. The coronary arteries also sending the opposite retroventricular artery and not only the PIVA, we defined as hyperdominant coronary arteries. Results The dissections of AVNA at the level of the crux cordis leaded us to define 5 different morphological patterns (AVNA types I - V), as follows: - type I, with AVNA emerged from the U-shaped turn of the RCA-to-PIVA arteries, in hearts with right coronary dominance (PIVA continuing the RCA); we found this pattern in 11 specimens (22%) with 2 subtypes: Ia – single AVNA (9 specimens, 18%) and Ib – duplicated AVNA (2 specimens, 4%): o in a specimen type Ia the ANAV left the U-turn of the RCA in a common trunk with the first two PSA (fig. 1); o in a specimen type Ib from the U-turn of the RCA was leaving, distally to the duplicated AVNA, a right postero-lateral branch (fig. 2), for the left ventricle; 103 Rusu M C et al - - - - Morphofunctional considerations on the atrioventricular node arterial vascularization type II, with AVNA emerged from the origin of PIVA, in hearts with right coronary hyperdominance (PIVA and left RVA given at crux cordis by the RCA), was encountered in 9 specimens (18%), also with two subtypes: IIa – unique AVNA (8 specimens, 16%)(fig. 3) and IIb – duplicated AVNA (1 specimen, 2%); type III, with AVNA emerged from the origin of the left RVA at crux cordis, in hearts with right coronary hyperdominance, in 17 specimens (34%); single AVNA (subtype IIIa) was present in 12 cases (24%), while duplicate AVNA (subtype IIIb) was present in 5 specimens (10%) (fig. 4); a single specimen type IIIb presented the distal AVNA continued at the level of the membranous septum to supply the AVB (fig. 4); type IV (trifurcation of the RCA) – AVNA leaving the V-shaped angle of the RCA terminal bifurcation into the PIVA and the left RVA (4 specimens, 8%) as a unique artery (1 heart) or in common trunk with the first (1 specimen, 2%), or with the first two PSA (2 specimens, 4%) (fig. 5); type V, with the AVNA emerging from the CxA, in 9 specimens (18%) with left coronary dominance and hyperdominance, having the following subtypes: o Va: single AVNA leaving the CxA in hearts with left coronary dominance (5 specimens, 10%); o Vb: duplicated AVNA leaving the CxA in a single specimen (2%) with left coronary dominance; the distal AVNA in that case left the U-turn of the CxA in a common trunk which also supplied two PSA (fig. 6); o Vc: single AVNA leaving the CxA in the presence of a right RVA (left coronary hyperdominance), in 3 specimens (6%). Fig. 1 Dissection of the arteries at the crux cordis. 1.RCA; 2.common posterior septal trunk; 3.PIVA; 4.ANAV; 5.first PSA; 6.second PSA; 7.right ventricle. 104 Fig. 2 Dissection of the posterior wall of the right atrium. 1. fossa ovalis; 2.medial cusp of the tricuspid valve; 3.opening of the coronary sinus; 4.duplicate atrioventricular node artery, emerged at crux cordis from the U turn of the RCA to PIVA (right coronary dominance); 5.sinoatrial artery, emerged from the initial segment of the RCA and sending off a descending septal artery (arrowheads) that distribute in the area of the triangle of Koch; 6.RCA. Romanian Journal of Legal Medicine Vol. XVII, nr. 2, 2009 Fig. 3 Dissection of the arteries at the level of the posterior right atrial wall, by an antero-lateral approach, for the anatomical evaluation of the AVNA. 1.aorta; 2.right SNA; 3.RCA; 4.anterior cusp of the TV, detached and partially reflected; 5.septal cusp of the TV; 6.PIVA; 7.limbus fossae ovalis; 8.oval fossa; 9.small artery for the limbus fossae ovalis; 10.right fibrous trigone, at the tip of the triangle of Koch; 11.AVNA, emerged in a short common trunk from the left RVA with a posterior septal branch and a small right posterolateral branch (for the left ventricular myocardium); 12.left RVA. The small arrows indicate an artery emerged from the right fibrous trigone and coursing on the right side of the membranous septum, in the area corresponding to the AVB. Fig. 4 Dissection of the arteries of the cardiac septa, at the level of the right atrium and superior part of the right ventricle. 1.aorta; 2.anterior parietal branch of the RA, emerged from the SNA; 3.anterior parietal branches of the RA, emerged from the DSA(RDSA); 4.branch of the oval fossa limbus; 5.branch of the interatrial septum, projected on the tendon of Todaro and coursing towards the valve of Eustachio; 6.left RVA; 7.primary common trunk of the AVNA and PSA (further sending the main AVNA– asterisk and the first right PSA – small arrows; the later sends from its loop accessory branches of the AVN – two asterisks); 8.left PSA; 9.RCA; 10.PIVA; 11.septal cusp of the TV; 12.anterior cusp of the TV; 13.SNA; 14.RCA; 15.right branch to conus arteriosus, with common ostial origin with the RCA; 16.DSA (RDSA); 17.parietal branches of the right ventricle; 18.AIVA; 19.RSSA, emerged from the origin of the RCA. 105 Rusu M C et al Morphofunctional considerations on the atrioventricular node arterial vascularization The AVNA’s emerged at crux cordis deepened to course endocardially, successively at the level of the cavo-tricuspid isthmus, medially to the sub-thebesian isthmus and next at the level of the septal isthmus, to reach the base of the triangle of Koch. The duplicated AVNA’s we encountered were either arising from a single common trunk or had different close origins from the coronary system, according to the types we defined above. We defined these duplicated AVNA’s as proximal, the one closer to the eustachian valve, and distal, the one closer to the TV. Invariably, the distal one sent off the first PSA at about the level of the septal isthmus. In 11 hearts (22%) we also found the presence of the descending septal artery (right descending superior artery) emerged from the initial segment of the sinoatrial artery; all these hearts were AVNA types I-IV (fig. 1, 3). Fig. 5 Dissection of the arteries at crux cordis, right coronary dominance. 1.RCA; 2.PIVA; 3.first two PSA; 4.AVNA; 5.left RVA; 6.right ventricle; 7.left ventricle. Fig. 6 Dissection of a duplicate atrioventricular node artery supplied by the CxA; left coronary dominance. 1.proximal AVNA, emerged from the CxA trunk; 2.CxA; 3.PIVA; 4.anterior cusp of the tricuspid valve; 5.inferior cusp of the tricuspid valve; 6.medial cusp of the tricuspid valve; 7.right ventricle; 8.common arterial trunk emerged from the CxA-to-PIVA angle, further sending off a distal AVNA (12), the first posterior septal branch (9) and a parietal branch (10); 11.RCA. 106 Romanian Journal of Legal Medicine Vol. XVII, nr. 2, 2009 These DSAs (RDSAs) initially coursed in the atrioventricular (coronary) groove on the right side of aorta to enter the interatrial septum near its junction with the membranous interventricular septum. - The distributed DSA (RDSA): parietal branches of the right ventricle, in the vicinity of the anterior cusp of the TV; branches of the interatrial septum, coursing laterally, at the level and above the limbus fossa ovalis; a descending branch that reached the apex of the triangle of Koch, distributing in the AVN area. Discussion On the origin of the AVNA from the coronary system, we are in accordance with Pejković et al (2008), who stated that the origin of the AV node artery is dependent on coronary arterial dominance [16]; there are authors who found the AVNA leaving the left coronary artery in 10% of their specimens [10, 16], while we found such origin of AVNA in 18% of those cases. In our specimens, we did not encounter a dual supply of AVNA, from codominant right and left coronary arteries, although such dual supply is described in literature [12]. Our study demonstrated that the usual description on the origin of AVNA, from the Uturn into the base of the posterior interatrial septum made by the artery (either right or left coronary) crossing the crux of the heart [21] is quite general; the AVNA may be considered as arising from that arterial U-turn only in situations of coronary dominance (types I, Va and Vb in our study), but not those of coronary hyperdominance (the other types we defined), when a retroventricular artery (RVA) continues the sender, either RCA or CxA and may serve as origin for AVNA. Arid et al (2000) also evidenced similar to us, the possible origin AVNA from the retroventricular artery and not only from the RCA or the CxA; however in their study were not evidenced duplicated AVNA’s. Arid et al identified in 60,86% the AVNA arising from the left RVA (it corresponds to our type IV that we encountered in 8%) and had singular cases (4,34% each) of AVNA emerged from the CxA (corresponds to our type V identified in 18%) and from the CxA division into the right RVA and the PIVA (we didn’t get at dissection such morphology). Arid et al also found, in 33,33% of the specimens with “right coronary dominance” (there was made no distinction with the hyperdominance), the AVNA leaving “from the terminal part of the right coronary a., as well as the left retroventricular a. and the posterior interventricular a. thus forming a sort of trifurcation” – in our study we defined as trifurcated only the arteries (RCA’s, type IV) with adjacent origins of the PIVA, left RVA and AVNA and if the AVNA emerged from the initial part of the RVA or the PIVA we considered that artery as origin (types II and III) and didn’t take the RCA branching pattern as trifurcation. Moreover, Arid et al didn’t found any specimen with the AVNA leaving the Uturn of the RCA, with left RVA absent [5]. Tanaka et al (1998) reported a case with a posterior SNA and an accessory AVNA arising by a common origin from the CxA, on the diaphragmatic surface of the heart [21]. These authors considered the AVNA emerged at the crux cordis as “principal atrioventricular node artery”, while defining the “accessory atrioventricular node artery” as corresponding to Taylor’s DSA (1980) and to Abuin’s RDSA (1998) [1, 2, 22]. In our study, we preferred to use the terms DSA (RDSA), which we considered more appropriated, due to the fact that the respective artery is not uniquely distributed to the AVN so as to be called accessory AVNA. 107 Rusu M C et al Morphofunctional considerations on the atrioventricular node arterial vascularization Tanaka et al evaluated their accessory AVNA (DSA or RDSA) as being quite similar to the initial portion of Kügel’s anastomotic artery, but this evaluation must be discussed. The “arteria anastomotica auricularis magna” was described by Kügel in 1928 and documented in 100 hearts by Nerantzis et al (2004). In 6% of cases, they evidenced several morphologic and topographic distinctive types of Kügel’s artery (KA), connecting the proximal RCA or CxA, either directly or through the SNA, with the distal arterial segment [14]. Nerantzis et al identified four different types of origin and connections of the KA; in the second type, the KA was a right intracoronary connection of the proximal and distal portions of the RCA, coursing in the interatrial septum on the right of the coronary sinus orifice. So, it appears to us that only the second type of KA, described by Nerantzis, can be considered in its initial part as similar to the DSA and the initial general evaluation of Tanaka must be revised. We consider that the only relevant difference between the KA leaving the RCA or the SNA and the DSA (RDSA) is represented by their distal connection at the crux cordis: the DSA (RDSA) is unconnected distally. No matter the anatomical diagnostic, any of these arteries are, if present, suppliers of the AVN. Moreover, the RCA, CxA, SNA, KA, DSA (RDSA) and AVNA may contribute, in various individual morphological pictures, to an anastomotic network in the lower part of the interatrial septum, mainly in its right side [14], which complicates the diagnostic of the dissections. We found in 2% (fig.3, specimen type IIb) an AVB branch, continuing the AVNA. With this evidence we improve the evidences of Van der Hauwaert et al (1972) who reported that in none of the 10 hearts they studied did the AVNA reach the common bundle [23] and correlate with Anderson and Murphy (1983) who reported that the AVNA supplied the AVB in 64% [3], a percent consistently higher than ours. The respective authors also described that in 7 from 10 hearts, AVNA invariably made a sharp caudal turn (50 to 90o), left the conducting tissue, and ramified further in the adjacent myocardium – such caudal turns of the AVNA we found only in 6 specimens (12%) of types Ia, IIIa and IIIb (the distal AVNA). We found duplicated AVNA in 9 specimens (18%), of different types. It was hard for us to document in the anatomical references such duplications. Saremi et al (2008) described an “accessory atrioventricular nodal artery” arising from the distal RCA was reported in a single case (0,98%). The “accessory” AVNA of Saremi is different to that one of Tanaka and refers to a duplication of AVNA at the crux [18]. The noticeable difference of frequencies (18% vs. 0,98%) is probably due to the hazard of specimens, on one hand, and to the different methods used (dissection vs. CT). Also Brugada et al (1990), in a report on the chemical ablation of the atrioventricular tissue, mention the presence, in 2 from 7 patients, of duplicated AVNA’s at the crux [8]. The hearts presenting not only the AVNA, but also the DSA (RDSA) and those hearts with duplicated AVNAs, appear to us as provided with additional anatomical resources of perfusion for the AVN, which will be better protected from ischemia. The difference is that an occlusion of the distal RCA will spare the DSA (RDSA) emerged from the SNA, but may not spare a duplicated AVNA (the occlusion of the proximal RCA may spare or not the DSA, depending on the reciprocal relation of the occlusion site and the origin of the SNA). As we did not find hearts, where the DSA (RDSA) associated with AVNA emerged from the CxA, we cannot evaluate the former as an alternative supplier of the AVN in such specimens. Our AVNA types are all related to the atrioventricular and aortic valves and are thus liable to damage during specific surgical procedures interfering with the respective valves. 108 Romanian Journal of Legal Medicine Vol. XVII, nr. 2, 2009 Duplicated AVNA’s must be held in mind during the selective atrioventricular nodal artery catheterizations [8, 20, 24], being able to determine failures of such procedures. The AVNA, duplicated or not, must be evaluated angiographically prior to the interventions. We must keep in mind that a complete investigation must be launched in every sudden cardiac death, especially in young. In this perspective the forensic pathologist make a good team with the anatomist, dissection and microdissection techniques still being very useful for both SA and AV nodes examination. Actually a seek and search is launched and a complex team will look for the cause of death and etiology: forensic pathologist, anatomist, radiologist, histopathologist, toxicologist, geneticians [9]. Acknowledgements Funding resource: Grant, code 2642, of the National University Research Council (UEFISCSU), Romania. Abbreviations: References 1. Abuin G, Nieponice A, Martinez S, Fernando C. The role of atrial vessels in aortic root and mitral valve operations. Ann Thorac Surg. 2000 Oct;70(4):1234-1237. 2. Abuin G, Nieponice A. New findings on the origin of the blood supply to the atrioventricular node. Clinical and surgical significance. Tex Heart Inst J. 1998;25(2):113-117. 3. Anderson KR, Murphy JG. The atrio-ventricular node artery in the human heart. Angiology. 1983 Nov;34(11):711-716. 4. Angelini P. Kugel's artery: What's in a name? Questions on atrial circulation. Tex Heart Inst J. 2004;31(3):271-2. Comment on: Tex Heart Inst J. 2004;31(3):267-70. 5. Arid JM, Armstrong O, Rogez JM, Robert R, Lardoux MC, Leborgne J. Arterial vascularisation of the atrioventricular node. Surg Radiol Anat. 2000;22(2):93-6. 6. Baroldi G., Fineschi, V. Introduction, in Pathology of the heart and sudden death in forensic medicine, Baroldi G., Fineschi, V. Silver, MD, Eds. Taylor and Francis 2006, p.1 7. Baroldi G., Interpretation of patholoigcal changes in sudden death, in Pathology of the heart and sudden death in forensic medicine, Baroldi G., Fineschi, V. Silver, MD, eds. Taylor and Francis 2006, p.271 8. Brugada P, de Swart H, Smeets J, Wellens HJ. Transcoronary chemical ablation of atrioventricular conduction. Circulation. 1990;81(3):757-61. 9. Curcă GC, Drugescu N, Ardeleanu C, Ceauşu M. Investigative protocole of sudden cardiac death in young adults, Rom J Leg Med 16 (1) 57-66 (2008) 10. Futami C, Tanuma K, Tanuma Y, Saito T.The arterial blood supply of the conducting system in normal human hearts. Surg Radiol Anat. 2003 Apr;25(1):42-49. Epub 2003 Jan 30. 11. Kirby ML. Cardiac Development, Oxford, UK: Oxford University Press; 2007 12. Krauss D, Carter JE Jr, Feldman T. Anomalous connection between the sinus node artery and the A-V node artery. Cathet Cardiovasc Diagn. 1993 Jul;29(3):236-9. 109 Rusu M C et al Morphofunctional considerations on the atrioventricular node arterial vascularization 13. Mosseri M, Meir G, Lotan C, Hasin Y, Applebaum A, Rosenheck S, Shimon D, Gotsman MS. Coronary pathology predicts conduction disturbances after coronary artery bypass grafting. Ann Thorac Surg. 1991 Feb;51(2):248-252. Comment in: Ann Thorac Surg. 1995 Feb;59(2):546-547. 14. Nerantzis CE, Marianou SK, Koulouris SN, Agapitos EB, Papaioannou JA, Vlahos LJ. Kugel's artery: an anatomical and angiographic study using a new technique. Tex Heart Inst J. 2004;31(3):267-70. 15. Onciu M, Tuţă LA, Baz R, Leonte T. Specifics of the blood supply of the sinoatrial node. Rev Med Chir Soc Med Nat Iasi. 2006 Jul-Sep;110(3):667-673. 16. Pejković B, Krajnc I, Anderhuber F, Kosutić D. Anatomical aspects of the arterial blood supply to the sinoatrial and atrioventricular nodes of the human heart. J Int Med Res. 2008 Jul-Aug;36(4):691-698. 17. Sánchez-Quintana D, Ho SY, Cabrera JA, Farré J, Anderson RH. Topographic anatomy of the inferior pyramidal space: relevance to radiofrequency catheter ablation. J Cardiovasc Electrophysiol. 2001 Feb;12(2):210-217. 18. Saremi F, Abolhoda A, Ashikyan O, Milliken JC, Narula J, Gurudevan SV, Kaushal K, Raney A. Arterial supply to sinuatrial and atrioventricular nodes: imaging with multidetector CT. Radiology. 2008 Jan;246(1):99-107; discussion 108-9. Epub 2007 Nov 16. 19. Sheaff MT, Hopster DJ, Hopster DJ Organ dissection - cardiovascular system. Heart; Block selection, in Post mortem technique handbook, Springer 2001, p.101 20. Sneddon JF, Ward DE, Simpson IA, Linker NJ, Wainwright RJ, Camm AJ. Alcohol ablation of atrioventricular conduction. Br Heart J. 1991 Mar;65(3):143-7. Comment in: Br Heart J. 1991 Mar;65(3):115. 21. Tanaka S, Lee HY, Mizukami S, Nakatani T, Chung IH. Posterior sinus node artery and accessory atrioventricular node artery arising by a common origin: a case report. Clin Anat. 1998;11(2):106-11. 22. Taylor JR. The descending septal artery. Its relation to the conduction system of the heart. Arch Pathol Lab Med. 1980 Nov;104(11):599-602. 23. Van der Hauwaert LG, Stroobandt R, Verhaeghe L. Arterial blood supply of the atrioventricular node and main bundle. Br Heart J. 1972 Oct;34(10):1045-51. 24. Wang PJ, Sosa-Suarez G, Friedman PL. Modification of human atrioventricular nodal function by selective atrioventricular nodal artery catheterization. Circulation. 1990 Sep;82(3):817-29. 25. Yanagawa N, Nakajima Y. A simple dissection method for the conduction system of the human heart. Anat Sci Educ. 2009 Mar;2(2):78-80. 26. Yesil M, Arikan E, Postaci N, Bayata S, Yilmaz R. Locations of coronary artery lesions in patients with severe conduction disturbance. Int Heart J. 2008 Sep;49(5):525-531. 110