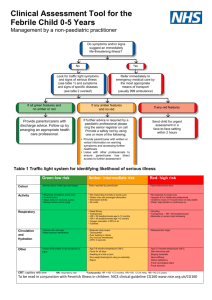
Clinical assessment tool for children 0
advertisement
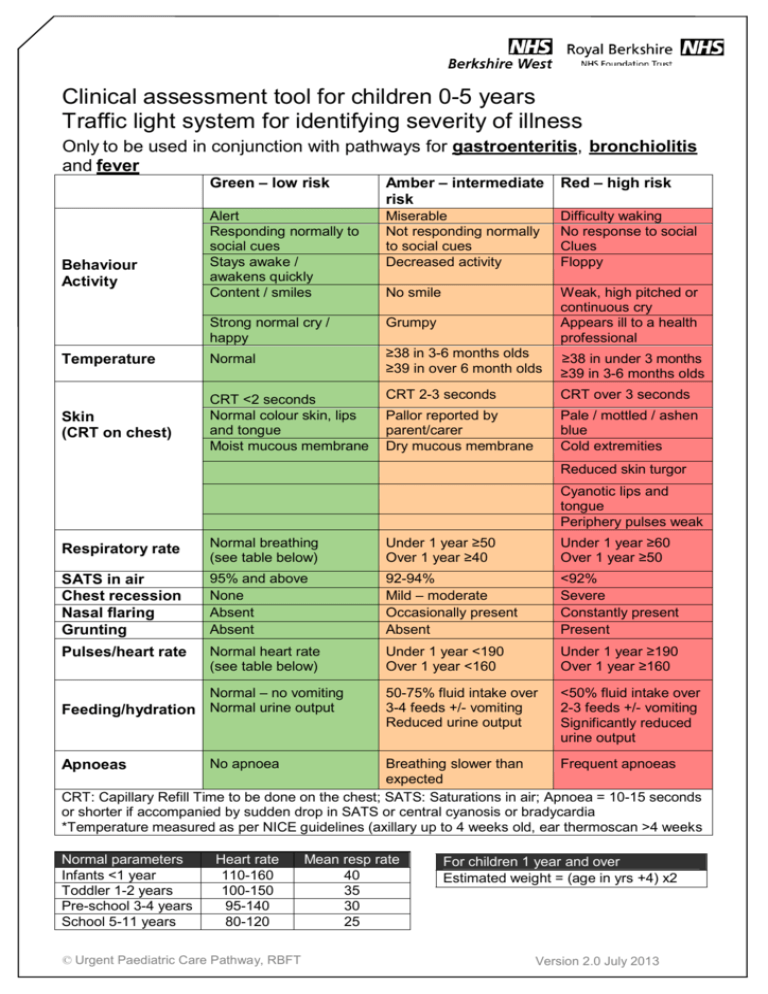
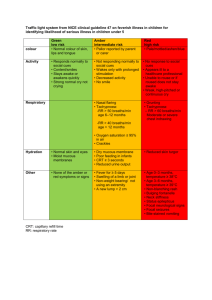
Clinical assessment tool for children 0-5 years Traffic light system for identifying severity of illness Only to be used in conjunction with pathways for gastroenteritis, bronchiolitis and fever Behaviour Activity Green – low risk Amber – intermediate risk Red – high risk Alert Responding normally to social cues Stays awake / awakens quickly Content / smiles Miserable Not responding normally to social cues Decreased activity Difficulty waking No response to social Clues Floppy No smile Strong normal cry / happy Grumpy Weak, high pitched or continuous cry Appears ill to a health professional Temperature Normal Skin (CRT on chest) CRT <2 seconds Normal colour skin, lips and tongue Moist mucous membrane ≥38 in 3-6 months olds ≥39 in over 6 month olds ≥38 in under 3 months ≥39 in 3-6 months olds CRT 2-3 seconds CRT over 3 seconds Pallor reported by parent/carer Dry mucous membrane Pale / mottled / ashen blue Cold extremities Reduced skin turgor Cyanotic lips and tongue Periphery pulses weak Respiratory rate Normal breathing (see table below) Under 1 year ≥50 Over 1 year ≥40 Under 1 year ≥60 Over 1 year ≥50 SATS in air Chest recession Nasal flaring Grunting 95% and above None Absent Absent 92-94% Mild – moderate Occasionally present Absent <92% Severe Constantly present Present Pulses/heart rate Normal heart rate (see table below) Under 1 year <190 Over 1 year <160 Under 1 year ≥190 Over 1 year ≥160 50-75% fluid intake over 3-4 feeds +/- vomiting Reduced urine output <50% fluid intake over 2-3 feeds +/- vomiting Significantly reduced urine output Normal – no vomiting Feeding/hydration Normal urine output Breathing slower than Frequent apnoeas expected CRT: Capillary Refill Time to be done on the chest; SATS: Saturations in air; Apnoea = 10-15 seconds or shorter if accompanied by sudden drop in SATS or central cyanosis or bradycardia *Temperature measured as per NICE guidelines (axillary up to 4 weeks old, ear thermoscan >4 weeks Apnoeas Normal parameters Infants <1 year Toddler 1-2 years Pre-school 3-4 years School 5-11 years No apnoea Heart rate 110-160 100-150 95-140 80-120 © Urgent Paediatric Care Pathway, RBFT Mean resp rate 40 35 30 25 For children 1 year and over Estimated weight = (age in yrs +4) x2 Version 2.0 July 2013 Table 1 Symptoms and signs of specific diseases Diagnosis to be considered Meningococcal disease Meningitis1 Herpes simplex encephalitis Pneumonia Urinary tract infection (in children >3 months)2 Septic arthritis/osteomyelitis Kawasaki disease3 Symptoms and signs in conjunction with fever Non blanching rash, particularly with one or more of the following: - An ill looking child - Lesions larger than 2mm in diameter (purpura) - CRT >3 seconds - Neck stiffness - Neck stiffness - Bulging fontanelle - Decreased level of consciousness - Convulsive status epilepticus - Focal neurological signs - Focal seizures - Decreased level of consciousness - Tachypnoea measured as: 0-5 months – RR >60 breaths/minute 6-12 months – RR >50 breaths/minute >12 months – RR >40 breaths/minute - Crackles in the chest - Nasal flaring - Chest drawing - Cyanosis - Oxygen saturation <95% - Vomiting - Poor feeding - Lethargy - Irritability - Abdominal pain or tenderness - Urinary frequency or dysuria - Offensive urine or haematuria - Swelling of a limb or a joint - Not using an extremity - Non-weight bearing Fever lasting longer than 5 days and at least 4 of following: - Bilateral red eyes - Change in upper respiratory tract mucous membrane (e.g. inflamed pharynx, dry cracked lips or strawberry tongue) - Change in peripheral extremities (e.g. oedema, erythema or desquamation) - Polymorphous rash - Cervical lymphadenopathy CRT: capillary refill time RR: respiratory rate 1 Classical signs (neck stiffness, bulging fontanelle, high-pitched cry) are often absent in infants with bacterial meningitis. 2 Urinary tract infection should be considered in any child <3 months with fever. See ‘Urinary tract infections in children’ (NICE clinical guideline, published August 2007) 3 Note: in rare cases, incomplete/atypical Kawasaki disease may be diagnosed with fewer features This guidance is written in the following context: This assessment tool is based on NICE guidance, which was arrived at after careful consideration of the evidence available. Healthcare professionals are expected to take it fully into account when exercising clinical judgement. The guidance does not, however, over-ride the individual responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or parents/carers.