- Hartmann
advertisement

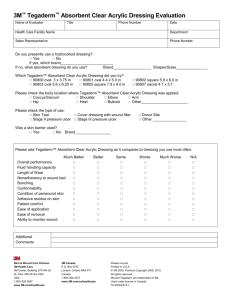
Pressure ulcer classification and degrees of severity Category/Stage I: Non-blanchable redness of intact skin Intact skin with non-blanchable erythema of a localized area usually over a bony prominence. Discoloration of the skin, warmth, edema, hardness or pain may also be present. Darkly pigmented skin may not have visible blanching. Further description: The area may be painful, firm, soft, warmer or cooler as compared to adjacent tissue. Category/Stage I may be difficult to detect in individuals with dark skin tones. May indicate “at risk” persons. Category/Stage II: Partial thickness skin loss or blister Partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough. May also present as an intact or open/ruptured serum-filled or sero-sanginous filled blister. Further description: Presents as a shiny or dry shallow ulcer without slough or bruising. This category/stage should not be used to describe skin tears, tape burns, incontinence associated dermatitis, maceration or excoriation. Category/Stage III: Full thickness skin loss (fat visible) Full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon or muscle are not exposed. Some slough may be present. May include undermining and tunneling. Further description: The depth of a Category/Stage III pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have (adipose) subcutaneous tissue and Category/Stage III ulcers can be shallow. In contrast, areas of significant adiposity can develop extremely deep Category/Stage III pressure ulcers. Bone/tendon is not visible or directly palpable. Category/Stage IV: Full thickness tissue loss (muscle/bone visible) Source: www.hartmanntraining.co.uk Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present. Often include undermining and tunneling. Further description: The depth of a Category/Stage IV pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have (adipose) subcutaneous tissue and these ulcers can be shallow. Category/Stage IV ulcers can extend into muscle and/or supporting structures (e.g., fascia, tendon or joint capsule) making osteomyelitis or osteitis likely to occur. Exposed bone/muscle is visible or directly palpable. Source: http://www.epuap.org/guidelines/Final_Quick_Treatment.pdf For more information about the HARTMANN eLearning programme, HeLP and medicaledition please go to www.hartmanntraining.co.uk Product Guide To protect: Professional consensus (in the treatment of pressure ulcers) recommends to create the optimum wound healing environment by using modern dressings –e.g. hydrocolloids, hydrogels, hydrofibres, foams, films, alginates, soft silicones, in preference to basic dressing types – e.g. gauze, paraffin gauze and simple dressing pads1. Hydrocoll® gelatin-free hydrocolloid wound dressing Hydrofilm® high MVTR transparent film dressing The smooth slippery backing minimises the friction coefficient of the patient-support surface. This means that the patient is able to move more easily over the support surface and the area covered by the dressing is likely to be exposed to lower levels of pressure, shear and friction2. By applying a film dressing to vulnerable areas, the risk of pressure ulcers may be reduced due to the low friction external surface of the film4. Also consider using film dressings as a secondary dressing for ulcers treated with alginates or other wound filler that will likely remain in the ulcer bed for an extended period of time (e.g. 3-5 days). To debride: To absorb: Hydrocoll® gelatin-free hydrocolloid wound dressing Hydrosorb® sheet hydrogel dressing Provides the ideal environment for the formation of granulation tissue, particularly the activity of fibroblasts, accelerating the wound healing process3. Hydrocoll® facilitates debridement of necrotic tissue and slough by promoting autolysis. Supplies the wound with moisture from the outset and facilitates autolytic debridement. Its transparency allows inspection of the wound at all times without dressing change (highly economical due to prolonged dressing change intervals), ideal for keeping granulation and epithelial tissue moist. Zetuvit® Plus super absorbent wound dressing pad PermaFoam® hydroactive foam dressing and Sorbalgon® calcium alginate dressing The blend of cellulose fluff and fluid retaining super absorbent particles (SAP) means that Zetuvit® Plus is particularly suitable for the treatment of heavily exuding pressure ulcers. The unique structure of the dressing provides cushioning3. PAUL HARTMANN LIMITED, Heywood Distribution Park, Pilsworth Road, Heywood, Lancashire 0L10 2TT Tel: 01706 363200 Fax: 01706 363201 Web: www.hartmann.co.uk E-mail: info@uk.hartmann.info Also suitable for the management of exuding pressure ulcers. 1 Bazin, S. et al (2005) The management of pressure ulcers in primary and secondary care. A Clinical Practice Guideline. Royal College of Nursing 2 Fletcher J. et al (2011) Pressure ulcers and hydrocolloids made easy. Wounds International, Volume 2, issue 4 3 Data on file 4 Nakagami G. et al. Comparison of two pressure ulcer preventative dressings for reducing shear force on the heel. Journal of Wound Ostomy. Continence Nurse. 2006 May-Jun;33(3):267-72