- WOUND CARE NURSING SPECIALTY
advertisement

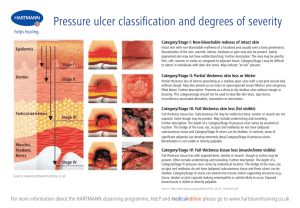
Pressure Ulcers Assessment and Management By Alex Khan RN BSN CWCN CFCN Jesse Lewis RN BSN CWCN DEVELOPED FOR Pressure Ulcer Assessment and Management OBJECTIVES By the end of the course participants will be able to: Classify pressure ulcers by stage and differentiate ulcers of non-pressure etiology. Discuss current treatment practices and interventions for pressure ulcer management. Overview: Layers of the skin The skin is comprised of three major components: Epidermis Dermis Subcutaneous tissue Though interrelated, each layer of skin has different structures, cell types and functions. What are Pressure Ulcers? Localized areas of tissue necrosis which develop when soft tissue is compressed between a bony prominence and an external surface for a prolonged period of time. Most pressure ulcers occur over bony prominences, where combined with friction and shearing forces result in skin breakdown. Several factors other than pressure contribute to ulcers including moisture, friction, shear, immobility, sensory loss and some underlying medical conditions. Common Pressure Ulcers sites Supine: 23% sacro-coccygeal 8% heels 1% occiput; spine Sitting: 24% ischium 3% elbows Lateral: 15% trochanter 7% malleolus 6% knee 3% heels Classification of Pressure Ulcers The staging of pressure ulcers, as defined by national guidelines (NPUAP, CMS), allow for common understandings for healthcare professionals. The staging of a pressure ulcer reflects the amount of tissue damage. STAGE I STAGE II STAGE III STAGE IV SUSPECTED DEEP TISSUE INJURY (DTI) UNSTAGEABLE Stage I Pressure Ulcer Intact skin with non-blanchable redness of a localized area usually over a bony prominence. Darkly pigmented skin may not have visible blanching; its color may differ from the surrounding area. Management of Stage- I Pressure Ulcers Stage I on Trunk of the Body – Manage incontinence, keeping area clean and dry. Use moisture barrier cream PRN. Off load area of pressure ulcer with pressure reducing / distribution surface and turning and repositioning schedule. Stage I on Heels – Ensure that heel(s) are floated at all times with frequent monitoring. Stage II Pressure Ulcer Partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough. May also present as an intact or open/ruptured serum-filled blister. Management of Stage- II Pressure Ulcers Dry Wound Bed Cleanse with normal saline, apply small amount of hydrogel and cover with non adherent dressing, change every day. Off load area of pressure ulcer with pressure reducing / distribution surfaces and turning and repositioning schedule. Minimal Drainage Cleanse with normal saline, apply hydrocolloid dressing every three days and PRN soiling or dislodging. Monitor placement every day. Stage III Pressure Ulcer Full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon or muscles are not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining and tunneling Management of Stage- III Pressure Ulcers Minimal Drainage and Clean Wound Bed Cleanse with normal saline, apply small amount of hydrogel and cover with non adherent dressing change every day. Off load area of pressure ulcer with pressure relieving / distribution surface and turning and repositioning schedule. Presence of Slough with drainage Sharp debridement / Enzymatic debridement Use Foam or Calcium Alginate dressing for moderate to copious drainage management. Slough 30% or less in the wound, negative pressure wound therapy is preferred treatment. Stage IV Pressure Ulcer Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present on some parts of the wound bed. Often include undermining and tunneling. Management of Stage- IV Pressure Ulcers Minimal Drainage and Clean Wound Bed Cleanse with normal saline, apply hydrogel and cover with non adherent dressing change every day. Off load area of pressure ulcer with pressure relieving surface and turning and repositioning schedule. Presence of Slough with drainage Sharp debridement / Enzymatic debridement Use Foam or Calcium Alginate dressing for moderate to copious drainage management. Slough 30% or less in the wound, negative pressure wound therapy is preferred treatment. Tunneling and undermining shall be filled appropriately. Suspected Deep Tissue Injury Purple or maroon localized area of discolored intact skin or blood-filled blister due to damage of underlying soft tissue from pressure and/or shear. The area may be preceded by tissue that is painful, firm, mushy, boggy, warmer or cooler as compared to adjacent tissue. Management of Suspected Deep Tissue Injury Cleanse with normal saline, apply foam dressing change every day. Off load area of pressure ulcer with pressure relieving / distribution surface and turning and repositioning schedule. Use Foam dressing for drainage management. Castor oil / Balsam / Peru / Trypsin spray is the preferred treatment. Un-stageable Pressure Ulcer Full thickness tissue loss in which the base of the ulcer is covered by slough (yellow, tan, gray, green or brown) and/or eschar (tan, brown or black) in the wound bed. Base of the wound cannot be visualized. Management of Un-stageable Pressure Ulcers Cleanse with normal saline, apply hydrogel and cover with non adherent dressing change every day. Off load area of pressure ulcer with pressure relieving / distribution surface and turning and repositioning schedule. Use Foam dressing for drainage management. Castor oil / Balsam / Peru / Trypsin spray is the preferred treatment for wounds with Intact eschar. Sharp or enzymatic debridement for the management of slough. Causative Factors for the Development of Pressure Ulcers Immobility or limited mobility Bowel & Bladder Incontinence Shearing and friction injuries Advanced age Malnutrition or debility Obesity History of pressure ulcers Dehydration Contractures Use of orthotic devises or restraints Lack of compliance Use of diapers / excess skin moisture Pressure Ulcer Prevention / Nursing Interventions Turn every 2 hours (q2h) Schedule: e.g. alternating positions Right/Back/Left q2h. May place pillow under one hip at a time if patient cannot tolerate full turning. Maximal Remobilization: Passive range of motion, physical therapist (PT) consult to plan appropriate measures for patient. Spinal Cord Injury and Disorder (SCI&D) patients (or any patient with custom chairs) are to sit in their own wheelchairs and cushions only. Protect Heels: Support entire leg with pillows to allow heels to suspend above the mattress or use heel protectors. Assess heels everyday for signs of pressure. Consider pressure relieving / distribution bed surface. Manage Moisture: Correct cause, (e.g., diarrhea), reduce or eliminate incontinent episodes (e.g., bladder training); Use mild soap, rinse, and dry skin well and apply moisture barrier cream. No diapers while patient in bed. Manage Nutrition: Increase protein intake more than 100% RDA, if not renal or liver impaired. Dietary consult to determine dietary needs and/or effectiveness of tube feedings. Reduce Friction and Shear: Use bed trapeze or pull sheet for lifting and moving patient up in bed. Apply transparent film or hydrocolloid dressing (Duoderm) over friction areas (e.g., elbows) Keep the head of the bed less than 30 degrees as often as possible. References Myers, B.A. (2004). Wound Management: Principles and Practice. Prentice Hall: Upper Saddle River, New Jersey, 37-45, 369-391. National Pressure Ulcer Advisory Panel (NPUAP). www.npuap.org.