Statins for Calcific Aortic Valve Stenosis: Into Oblivion After SALTIRE
advertisement

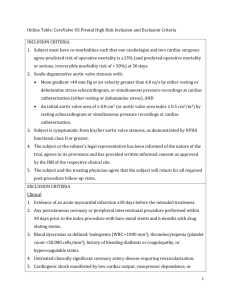
Statins for Calcific Aortic Valve Stenosis: Into Oblivion After SALTIRE and SEAS? An Extensive Review from Bench to Bedside Hadewich Hermans, MD, Paul Herijgers, MD, PhD, Paul Holvoet, PhD, Eric Verbeken, MD, PhD, Bart Meuris, MD, PhD, Willem Flameng, MD, PhD, and Marie-Christine Herregods, MD, PhD Abstract: Calcific aortic stenosis is the most frequent heart valve disease and the main indication for valve replacement in western countries. For centuries attributed to a passive wear and tear process, it is now recognized that aortic stenosis is an active inflammatory and potentially modifiable pathology, with similarities to atherosclerosis. Statins were first-line candidates for slowing down progression of the disease, as established drugs in primary and secondary cardiovascular prevention. Despite promising animal experiments and nonrandomized human trials, the prospective randomized trials SEAS and SALTIRE did not confirm the expected benefit. We review SEAS and SALTIRE starting with the preceding studies and discuss basic science experiments covering the major known contributors to the pathophysiology of calcific aortic valve disease, to conclude with a hypothesis on the absent effect of statins, and suggestions for further research paths. (Curr Probl Cardiol 2010; 35:284-306.) alcific aortic valve disease is a common and progressive pathology. The prevalence of sclerosis is reported to be ⬎25% in the population aged ⬎65 years; the prevalence of severe aortic valve stenosis is reported to be ⬎2.5% in the population aged ⬎75 years and C The authors have no conflicts of interests to disclose. Hadewich Hermans, MD, is supported by the Flanders Research Foundation (FWO) to prepare a PhD thesis. Curr Probl Cardiol 2010;35:284-306. 0146-2806/$ – see front matter doi:10.1016/j.cpcardiol.2010.02.002 284 Curr Probl Cardiol, June 2010 ⬎8% in the population aged ⬎85 years.1 Aortic valve stenosis (AS) is the primary indication for valve replacement in western countries, and the number will only increase as elderly people are a growing subpopulation. At present the only established therapy for AS is valve replacement.2 Medical prevention of progression is a subject of substantial research for a decade as it was recognized that aortic valve disease is not only a passive wear and tear process but an active inflammatory process with histopathologic changes and risk profile similar to atherosclerosis, occurring from the age of 35 years. This generated possible targets for therapy. Statins were first-line candidates as commercially available drugs with established benefit in primary and secondary cardiovascular prevention by atherosclerosis stabilization. Retrospective studies3-7 and prospective nonrandomized studies8,9 have shown that statins significantly slowed down progression. SEAS10 and SALTIRE,11 being the only prospective randomized trials published to date, did not confirm the effect of statins on rate of progression. How come? What Preceded SALTIRE and SEAS? Epidemiology and Histopathology: (Dis)Similarities Between Calcific Aortic Valve Disease and Atherosclerosis Since the Helsinki Aging Study12 and Cardiovascular Health Study,13 it is recognized that calcific aortic valve disease and atherosclerosis show an overlap in clinical risk factors, ie, age, male gender, hypertension, smoking, dyslipidemia, renal dysfunction, and diabetes. However, there is no absolute correlation as only 33% of the patients in the Euro Heart Survey underwent concomitant coronary artery bypass grafting (CABG) at aortic valve replacement (AVR).14 Histopathologic comparison revealed that both entities are characterized by accumulation of (oxidized) low-density lipoprotein (oxLDL), inflammation, calcification, and bone formation.15-17 We have to emphasize that there are also differences: calcification occurs much earlier in AS, the most prominent cell type is not the smooth muscle cell but the “fibroblast,” and plaque instability as the cause of symptoms is not a main issue in contrast to atherosclerosis. Animal Experiments: Based on a Dyslipidemic Model To date, the only animal experiment showing benefit of statins is AS, concerns a hypercholesterolemic rabbit model.18 As such, this might only be translated to patients with dyslipidemia as the facilitating factor. The quest for drug therapy is hampered by the lack of a low-cost spontaneous Curr Probl Cardiol, June 2010 285 animal model. Only aging swine develop valvular sclerosis without an inciting factor,19 while the other species require diets or genetic mutations. The rabbit models are based on high-cholesterol diets with or without vitamin D supplementation.18,20-25 The mouse models are either dyslipidemic like the rabbit models, by diets or by mutations in the lipid metabolism (apolipoprotein, LDL receptor, apolipoproteinB), or are based on mutations in players of calcification and bone formation (endothelial nitric oxide synthase (eNOS), matrix gla protein, and Notch1 or Madh6) and as such they might not mirror the development and progression of the disease in humans where AS develops at later age by a complex inflammatory process.26-33 Nalini M. Rajamannan: In 2009, the current use of hyperlipidemic animal models, whether genetic or diet-induced, provides a foundation for evolving studies in the field of calcific aortic valve disease. The authors are correct that the published animal models do not recapitulate fully human calcific aortic valve disease. Each published model, to date, has provided unique cellular features that recapitulate the published discoveries important in the phenotype of calcification in the aortic valve. The eNOS null mouse by Lee TC, et al,28 expresses bicuspid aortic valves in only 27% of the mouse colonies and not spontaneous calcification. The genetic mouse model that has demonstrated severe aortic stenosis in a third of the mice over a 2-year period is the Reversa mouse published by Weiss RM, et al.32 This mouse model is the first to develop severe stenosis in a third of the mouse cohorts studied. Retrospective Observational Studies: Patients on Statins for Established Indication Early 2000 retrospective observational studies were reported (Table 1).3-7 Note that consequently all patients received statins in primary or secondary prevention, and note that in the stage of aortic valve disease, none included sclerosis. Aronow focused on aortic valve calcification; the other groups focused on hemodynamic severity. All investigators found a significant benefit of statins on the parameters regardless of the degree of AS. As such, the authors concluded that statins might be beneficial in advanced stages of the evolutionary disease, considered the retrospective and nonrandomized nature of the studies. The impact of cholesterol level on hemodynamic progression was controversial: Aronow and Novaro described an association between cholesterol level and progression; in the trials of Bellamy and Rosenhek they were unrelated. Nalini M. Rajamannan: There is a recent publication by Antonini-Canterin F, et al,98 demonstrating that there is a stage-related effect of statin treatment 286 Curr Probl Cardiol, June 2010 TABLE 1. Retrospective and prospective nonrandomized trials Investigators (y) Retrospective Aronow (2001) Novaro (2001) Bellamy (2002) Shavelle (2002) Rosenhek (2004) Prospective RAAVE (2007) n (n on statins) Follow-up Grade, AS at baseline Endpoint Pro statins 180 (62) 2.75 ⫾ 1 y Mild ⌬Pmax Yes (P ⬍ 0.01) 174 (57) 1.75 ⫾ 0.6 y Mild to moderate Yes (P ⫽ 0.03) 156 (38) 3.7 ⫾ 2.3 y Mild to moderate ⌬Pmax, AVA AVA, Vmax 65 (28) 2.5 ⫾ 1.6 y 211 (82) 2.0 ⫾ 1.5 y No hemodynamic AVC evaluation Mild to severe AVA, Vmax 121 (61) 1.4 ⫾ 0.46 y Moderate to severe Vmax Yes (P ⫽ 0.04) Yes (P ⫽ 0.006) Yes (P ⬍ 0.0001) Yes (P ⫽ 0.007) Abbreviations: y, year; n, number of patients; ⌬Pmax, peak transaortic gradient; AVA, aortic valve area; Vmax, peak transaortic velocity; AVC, aortic valve calcium; RAAVE, Rosuvastatin affecting aortic valve endothelium to slow the progression of aortic valve stenosis. on the progression of aortic valve sclerosis and stenosis. This study also demonstrates the importance of treating the earlier stages of this disease with a notable difference in treatment effect. Prospective Nonrandomized Studies: Patients on Statins for Established Indication Moura et al performed the Rosuvastatin Affecting Aortic Valve endothelium to slow the progression of aortic stenosis study (RAAVE).8 Although this study was prospective, it was nonrandomized comprising only 121 patients with moderate to severe AS; 61 of them were on statins in accordance to current guidelines. Statins significantly slowed down hemodynamic progression, but here again the observed effect of statins cannot be broadened to AS patients without dyslipidemia as facilitating factor. Pohle et al performed electron beam tomography on 104 patients at baseline and after a mean interval of 15 months.9 Patients were divided in 2 groups according to LDL cholesterol level: 57 patients ⬍130 mg/dL, of which 39 were on statin treatment; and 47 patients ⬎130 mg/dL, of which 15 were on statin treatment. All patients had progression of aortic valve calcification score, but progression was significantly less in the group ⬍130 mg/dL. Multiple regression analysis showed that LDL level was an independent predictor of progression, while age, smoking, Curr Probl Cardiol, June 2010 287 hypertension, and diabetes were not. Statin use was not entered in the regression model, but the authors describe that the patients on statin treatment with LDL ⬍130 mg/dL had a significantly slower progression than patients on insufficient dose to control plasma LDL and concluded that adequate lipid-lowering decreases progression of AS. Nalini M. Rajamannan: The RAAVE study was designed to treat patients with elevated LDL and calcific aortic valve disease compared with patients with normal LDL and calcific aortic valve disease, because of the ethical issues related to randomizing patients with elevated LDL to no statin after the series of published papers demonstrating the clinical benefits of lipid lowering, for example, the 4-S trial. Lancet 344(8934):1383-9, 1994. Pleiotropic Effects of Statin: Pathways Partly Unknown The discrepancies regarding the association between cholesterol level and hemodynamic progression of AS give rise to the question of the mechanisms by which statins slow down progression in patients with dyslipidemia: only by lipid lowering or in combination with pleiotropic effects. In atherosclerosis the importance of the pleiotropic effects of statins on cardiovascular mortality and morbidity is well established; the pathways and their relative contribution however are partly unknown. Statins are reported to cause an improvement of endothelial dysfunction, to have anti-inflammatory and antioxidant effects, and to be capable of plaque stabilization, as is nicely reviewed by Davignon.34 The improvement of endothelial dysfunction is shown to be caused by increased NO production: at first by diminished inhibition of eNOS-activity by lowering of LDL, as LDL is able to increase caveolin-1, an inhibitor of eNOS; second, by enhancement of constitutive eNOS activity by (1) stabilization of eNOS messenger RNA, (2) activation of Akt (protein kinase B) in endothelial cells and as such phosphorylation of its substrate eNOS, and (3) prevention of translocation to the cell membrane of Rho GTPase with consequently less negative regulation of eNOS. The antioxidant effect of statins with less production of the cytotoxic oxLDL might be due to direct diminution of the oxidative ability of macrophages, and to free radical scavenging. On top statins might decrease the activity of macrophage CD36, a receptor of oxLDL and as such foam cell formation. With regards to the anti-inflammatory effect, statins are reported to cause a reduction of plasma C-reactive protein and reduction of adhesion molecules, the latter however with conflicting results. Plaque stabilization is described as the net effect of the mechanisms discussed above, caused by 288 Curr Probl Cardiol, June 2010 a smaller lipid core, less macrophages and T-lymphocytes, less apoptosis, and more collagen content with less matrix metalloproteinase-2 (MMP-2), and enhanced tissue inhibitor of matrix metalloproteinase-1 (TIMP-1) immunoreactivity. As conviction grew that AS has a genesis and evolution similar to atherosclerosis, the next step was the hypothesis that statins might be able to influence the progression. There was preliminary proof of concept by the mentioned retrospective and prospective nonrandomized trials that paved the way for the setup of prospective randomized trials. Nalini M. Rajamannan: The experimental studies in the field of vascular disease and statins have been clearly defined. The pleiotropic effects of statins in the signaling pathways include eNOS, hsCRP, MMP-2, and TIMP-1. There is a growing body of literature in the field of aortic valve disease in vitro and in vivo demonstrating that statins have specific pleiotropic effects in the valve also, including the following: eNOS, Rajamannan et al. Atorvastatin inhibits calcification and enhances nitric oxide synthase production in the hypercholesterolemic aortic valve. Heart 91(6):806-10, 2005; extracellular nucleotides, Osman et al. A novel role of extracellular nucleotides in valve calcification: a potential target for atorvastatin. Circulation 114(1)(Suppl): I566-72, 2006; and inhibition of bone matrix synthesis, Wu B, et al.56 SALTIRE and SEAS Study Aim The investigators hypothesized that statins ⫾ ezetimibe slow down progression of AS. SALTIRE had as primary endpoint progression in aortic jet velocity and computed tomography aortic valve calcium score, and as secondary endpoints, AVR, death from any cause, hospitalization for any cause, hospitalization for cardiovascular causes, and a composite of clinical endpoints (death from cardiovascular causes, AVR, hospitalization attributable to severe AS). The primary endpoint of SEAS was the composite of cardiovascular death, AVR, nonfatal myocardial infarction, congestive heart failure because of progression of AS, CABG, percutaneous coronary intervention, hospitalized unstable angina, and nonhemorrhagic stroke. The secondary endpoints were aortic valve events (AVR, congestive heart failure because of progression of AS, and cardiovascular death), echocardiographic progression, and ischemic events (CABG, percutaneous coronary intervention, stroke, unstable angina, nonfatal myocardial infarction, death from cardiovascular cause). The rationale for the composite primary endpoint was the assessment of aggressive lipid-lowering on the entire cardiovascular burden in AS patients (Table 2). Curr Probl Cardiol, June 2010 289 TABLE 2. Published prospective randomized trials n (n on statins ⫾ ezetimibe) Follow-up Grade, AS at baseline Primary endpoints Secondary endpoints Pro statins SALTIRE (2005) SEAS (2008) 155 (77) 2.08 y Mild to severe Vmax (P ⫽ 0.95) AVC (P ⫽ 0.80) Composite (P ⫽ 0.19) Death from cardiovascular causes (P ⫽ 1.0) Aortic valve replacement (P ⫽ 0.17) Hospitalization for severe AS (P ⫽ 0.73) Death from any cause (P ⫽ 0.73) Hospitalization for any cause (P ⫽ 0.84) No 1873 (944) 4.35 y Mild to moderate Composite (P ⫽ 0.59) AVA, Vmax (P ⫽ 0.83) Aortic valve events (P ⫽ 0.73) Ischemic events (P ⫽ 0.02) No Abbreviations: n, number of patients; Vmax, peak transaortic velocity; AVC, aortic valve calcium; AVA, aortic valve area; SALTIRE, Scottish Aortic Stenosis and Lipid Lowering Trial, Impact on Regression; SEAS, Simvastatin and Ezetimibe In Aortic Stenosis Study. Study Design and Baseline Characteristics The trials were double-blind, randomized, and placebo-controlled, and SEAS was multicenter. The inclusion criterion was asymptomatic calcific AS, in SALTIRE with a peak jet velocity of at least 2.5 m/s, in SEAS between 2.5 and 4 m/s. Both had similar exclusion criteria namely age ⬍18 y, contraindications for or current therapy with statins, guidelines indication for statins, left ventricular dysfunction, significant valvular disease other than AS, uncontrolled hypertension, or renal insufficiency. As such, the study population of the 2 trials does not fully resemble the general AS population as the study cohorts had limited clinical risk factors for AS progression. All patients underwent echocardiography ⫾ computed tomography at baseline, annually during follow-up, and at study termination, while adverse effects and lipid profile were monitored more frequently. Results SALTIRE did not show a significant reduction in AS progression rate, nor in clinical endpoints. SEAS showed similar results, with the exception of a significant effect on ischemic events, dominated by a reduction of the need for CABG in the simvastatin-ezetimibe group. SEAS did not have a treatment group on simvastatin or ezetimibe alone. Long-term outcome 290 Curr Probl Cardiol, June 2010 trials of ezetimibe, acting on the intestinal sterol transporter, are not published yet. As such, the relative contribution of both drugs on this endpoint cannot be determined. Nalini M. Rajamannan: The SEAS and SALTIRE investigators are pioneers in the field of valvular heart disease trials. These studies provide valuable information for the future design of valvular heart disease trials. The design of these trials came out before the series of publications for the hyperlipidemic animal models, which have contributed to the future design of clinical valve trials. Back to Basics: Pathophysiology of Aortic Valve Stenosis The normal aortic valve leaflets are covered with endothelium, are avascular, and consist of the 3 following layers: the ventricularis at the ventricular side; the spongiosa; and the fibrosa at the aortic side of the leaflet. The ventricularis is composed of closely aligned elastin fibers; the spongiosa consists of loose connective tissue, and the fibrosa contains collagen fibers. The layers are populated by mesenchymal cells namely valve interstitial cells (VICs), maintaining leaflet integrity. The early lesion is characterized by subendothelial plaque-like lesions at the aortic side, with progressive infiltration of the adjacent fibrosa, and consists of accumulation of lipoproteins, inflammatory cells, and microcalcifications.15-17 As the lesion progresses, neo-angiogenesis is noted,35 a process of enhanced calcification, and active bone formation.36 While the AS lesion is characterized at the microscopic level, the molecular pathways remain challenging to unravel. We discuss the most studied pathways in the (patho)physiology as presented in Fig 1. Mechanical Stress and Shear Stress Although calcific AS is now recognized as an active process with similarities to atherosclerosis, instead of an unmodifiable pathology, due to long-term mechanical stress and leading to passive accumulation of calcium, caution is warranted to forget the contribution of increased mechanical and decreased or turbulent shear stress to the initiation and progression of AS. Patients with bicuspid valves present 2 decades earlier than patients with tricuspid valves.37 Hypertension is a risk factor for AS,12,13 and lesions are noted to initiate at the flexion area of the leaflets where stress is highest.38 All emphasizing the role of mechanical stress currently believed to be leading to endothelial disruption. The noncoroCurr Probl Cardiol, June 2010 291 FIG 1. Pathophysiology of calcific aortic valve stenosis. Abbreviations: NO, nitric oxidep; ICAM, intercellular adhesion molecule; VCAM, vascular cell adhesion molecule; TGF, transforming growth factor ; ACE, angiotensin converting enzyme; oxLDL, oxidized LDL; TNF-␣, tumor necrosis factor ␣; A1R, angiotensin receptor 1; B2R, bradykinin receptor 2; Lrp 5, low-density lipoprotein receptor-related protein 5; RANK, receptor activator of nuclear factor kappa (B); RANKL, RANK ligand; NF-B, nuclear factor kappa (B); cbfa-1, core binding factor alpha-1; Msx-2, msh homeobox 2; qVIC, quiescent valvular interstitial cell; obVIC, osteoblastic valvular interstitial cell; aVIC, activated valvular interstitial cell; EGF, vascular endothelial growth factor; MMPs, matrix metalloproteinases; AS, aortic stenosis. (Color version of figure is available online.) nary cusp is often the first affected, probably by more pronounced endothelial dysfunction as this cusp might encounter less shear stress than the coronary cusps due to absence of diastolic coronary flow. The fibrosa is affected first as the aortic side of the valve is exposed to turbulent flow, while the ventricularis is exposed to laminar flow.39 The molecular pathways from stress to endothelial dysfunction are subjected to substantial research in the atherosclerosis field, with NO as a key player.40 As soon as subendothelial lesions are present, endothelial dysfunction is maintained by oxLDL and inflammatory cells.41 The endothelium covering the valve leaflets, however, is distinct from vascular endothelium. We comment on this below. Regarding the role of mechanical and shear stress, we now leave the ground paths. Quoting Robicsek et al and Singh et al, the importance of 292 Curr Probl Cardiol, June 2010 the functional assembly of the valve leaflets, corresponding sinuses, and sinotubular junction is often overlooked.42,43 Intact sinuses and sinotubular junction create optimal distribution of pressure load and proper valve opening and closure, while loss of aortic wall compliance leads to significant stress overload of the leaflets. Loss of vascular compliance occurs in every aging subject due to gradual loss of elastin fibers in the media and is more pronounced in patients with hypertension, diabetes, and renal failure, the latter due to superposition of media calcification. As such, the role of mechanical stress is not restricted to the initiating step, but instead is continuous and progressive. Once sclerosis is initiated in the leaflets, the thickened and stiffened leaflets themselves also promote unfavorable stress distribution. This self-perpetuating process might partly cause the failure of statins to slow down AS progression when administrated at later stages. Recent reports on the molecular bridge between mechanical stress and AS describe in vitro testing of intact porcine valves or aortic VICs. To interpret the results of in vitro experiments, remember that the aortic valve is exposed to a composite of hemodynamic forces: during systole pulsatile pressure and shear stress (laminar at the ventricularis, turbulent at the fibrosa), and during diastole cyclic stretch and turbulent shear stress, transmitted to the VICs by endothelial cells and matrix.44 Cell proliferation, apoptosis, collagen content, cathepsin S and K expression, MMP-1, -2, and -9 expression and activity increase with increased cyclic stretch, while cathepsin L expression, TIMP-1 expression, and activity are reduced.45 Transforming growth factor 1 (TGF1) acts synergistically with cyclic stress46 and is also a key player in upregulation of vascular cell adhesion molecule-1 and intercellular adhesion molecule 1 in the valvular endothelium at the aortic side in response to oscillatory shear stress.47 The endothelium is also capable of regulating the mechanical properties of the aortic valve cusps. Endothelin-1 leads to increase in cusp stiffness, while serotonin has the opposite effect; both are endothelium-dependent effects exerted on the VICs.48 The role of the valvular endothelium in vivo in stress distribution, and how mechanotransduction to the VICs takes place, requires further research. Valvular Endothelium The endothelium is not a uniform organ, similarly functioning in the entire cardiovascular bed. Butcher et al highlighted that the valvular endothelium is distinct from the vascular endothelium. They showed that in response to shear stress valvular endothelial cells respond by aligning perpendicular and vascular endothelial cells parallel to the direction of the Curr Probl Cardiol, June 2010 293 flow, with differences in focal adhesion arrangement and signal kinases.49 Subsequently they showed transcriptional differences between porcine aortic valve and aortic endothelial cells exposed to laminar shear stress: valvular endothelial cells are less intrinsically inflammatory, although similar antioxidant and anti-inflammatory genes are expressed and express more genes associated with chondrogenesis and less with osteogenesis. In both cell types shear stress protected against calcification by downregulation of bone morphogenic protein 4, in valvular cells also by inhibition of cadherin-11 and in aortic cells by inhibition of periostin.50 As such, the effect of statins on endothelial dysfunction as described for vascular endothelium might not be as pronounced for valvular endothelium. Nalini M. Rajamannan: The gene expression of valve endothelium has been described by Simmons CA, et al,19 demonstrates the unique genotype of the valve aortic endothelial surface versus the ventricular surface the geographic differences that may contribute to the difference in the predisposition of the valve to calcify on the aortic surface. Aortic Valve Interstitial Cells As discussed by Liu et al, the terms valvular fibroblasts and osteoblasts should be replaced by the at present known 5 phenotypes of valvular interstitial cells: either embryonic progenitor, quiescent (qVICs), activated (aVICs), progenitor (pVICs), or osteoblastic (ob)VICs.51 VICs are distinct mesenchymal cells that adapt to the valvular environment with a change in phenotype with specific detectable markers. Embryonic progenitor endothelial/mesenchymal cells, present in the embryonic cardiac cushions, give rise to qVICs by the developmental process of endothelialto-mesenchymal transformation (EMT). Their role seems however not finished after the developmental period, as plasticity of aortic and pulmonary valve endothelium was described, which might lead to the hypothesis that EMT takes place again in adult valves in response to injury, giving rise to pVICs.52,53 Quiescent VICs maintain physiologic valve structure and inhibit angiogenesis in the leaflets. They can give rise to activated and obVICs in response to a number of chemokines and growth factors, one of the most important being TGF from activated endothelium. Activated VICs contain ␣-smooth-muscle actin and respond to valve injury and mechanical forces by repair processes including proliferation, migration, and matrix remodeling. ObVICs participate in calcification, osteogenesis, and chondrogenesis and secrete alkaline phos294 Curr Probl Cardiol, June 2010 phatase, osteocalcin, osteopontin, and bone sialoprotein. The least defined phenotype is the pVIC that might originate from the heart valve, the bone marrow via the circulation, or the endothelium via EMT and is CD-34-, CD-133-, and/or S100-positive. In case of in vitro experiments, next to the VIC phenotype used, also the culture conditions should meticulously be described as the passage number; cell density and matrix all affect the phenotype via incompletely known pathways. Recent intriguing papers describe that VIC-differentiation and -calcification is regulated by extracellular matrix stiffness, as is the efficacy of statin treatment. Yip et al describe that on compliant calcifying matrices VICs transform to an osteoblast phenotype and form calcification noduli by active deposition. On a stiff matrix, however, they transform to an ␣-smooth-muscle actin-expressing phenotype with apoptosis-dependent dystrophic calcification. On the stiff matrix, calcification was strongly enhanced by TGF1, but not on compliant matrices, where the VICs expressed less TGF receptor I.54 This is important, as in current opinion, “myofibroblasts” are transforming to “osteoblasts” in the evolution of AS, while this study implicates that the main cell type might be the “osteoblast” or obVIC in the early stage and the “myofibroblast” or aVIC in the later stage. Monzack et al reported that the inhibiting and even dissipating effect of simvastatin on calcific nodule formation was dose-dependent, matrix-dependent, and time-dependent.55 In most VIC studies cells are cultured on unmodified tissue culture polystyrene (TCPS), but they cultured the cells also on TCPS coated with either laminin or fibrin and found that the effect of simvastatin was more pronounced in laminin TCPS. Their time experiments showed that the effect of simvastatin was only significant when applied within 1 hour after application of TGF. Adding to the importance of time dependency of statin admission, Wu et al described that simvastatin inhibited dystrophic calcification by valve “myofibroblasts,” but promoted calcific nodule formation by “osteoblasts,”56 analogous to the “statin paradox” described in osteoporosis research. Anger et al showed that statin therapy enhanced phosphorylated ERK in end-stage AS, which might enhance proliferative degeneration.57 These experiments underscore the absolute necessity of studying the complete in vivo evolution of the disease, with attention for macromechanics, cells and cell types, matrix composition, and matrix micromechanics to understand the pathophysiology, and investigate drug effects, including timing of administration. With the advent of molecular imaging as described by Aikawa et al, this could be in the near future for animal models, but not yet for patients.33 Curr Probl Cardiol, June 2010 295 Nalini M. Rajamannan: Aortic valve myofibroblast cell is a mesenchymalderived cell that has the ability to differentiate to different valve phenotypes including a robust osteogenic phenotype. Chen JH, et al. Identification and characterization of aortic valve mesenchymal progenitor cells with robust osteogenic calcification potential. Am J Pathol 174(3):1109-19, 2009. Extracellular Matrix To date, little is known about the evolution of extracellular matrix, although primordial to understand both cell-cell- and cell-matrix communication. Comparison of degenerative aortic valves obtained at replacement surgery and normal valves at heart transplantation learned that the diseased valves have an extensive matrix remodeling process, with as a result disrupted basal membranes, more collagen than elastin, and opportunity for invasion of inflammatory cells and neoangiogenesis. The MMPs and cathepsins are the most studied. An increase of MMP-1, -3, and -9 have consistently been reported, while the effect on their inhibitors TIMP-1 and -2 have shown conflicting results.58-60 Cathepsin S, K, V, and G are significantly increased in stenotic aortic valves, with cathepsin G being highly expressed in activated mast cells.61,62 The importance of inflammation is underscored by colocalization of TGF1 and cathepsin G in mast cells, and of tumor necrosis factor-␣ with MMP-1.62,63 Remember that both inflammation and mechanical stress are reported to be able to upregulate matrix remodeling and can act synergistically as described above. Nalini M. Rajamannan: Grande-Allen KJ, et al. Glycosaminoglycan synthesis and structure as targets for the prevention of calcific aortic valve disease. Cardiovasc Res 2007;76(1):19-28, have demonstrated that extracellular matrix synthesis is an important disease phenotype and target for therapeutic interventions. Lipoproteins In the 1990s the uptake of serum neutral lipids and apolipoproteins, and lipid oxidation around calcium deposits and leukocytes were described in AS, resembling the atherosclerotic process.16,17 Mohty et al recently conducted an important study on severely stenotic valves, explanted at AVR,64 supporting the hypothesis that oxLDL also in AS participates in recruitment and activation of macrophages, as oxLDL colocated with macrophages, and an increased oxLDL score correlated with higher tumor 296 Curr Probl Cardiol, June 2010 necrosis factor-␣ expression. An increase in oxLDL score also correlated with increased tissue remodeling score, as defined by Warren and Yong,65 supporting the contribution of oxLDL to calcification in AS, while plasma small LDL correlated with disease progression and oxLDL score. The authors emphasize, however, that 9% of the patients had no oxLDL in their valves, which might indicate that oxLDL is a contributor but not a requisite for the development of AS. Nalini M. Rajamannan: For patients who do not have a genetic abnormality, most authorities agree that the traditional cardiovascular risk factors are critical in the initiation event for this disease. The early histopathologic findings in these patients are critical for the development of animal models, and future medical therapies. Patients with familial hypercholesterolemia also develop aortic valve disease. Sprecher DL, Schaefer EJ, Kent KM, et al. Cardiovascular features of homozygous familial hypercholesterolemia: analysis of 16 patients. Am J Cardiol 54(1):20-30, 1984; Rajamannan NM, Edwards WD, Spelsberg TC. Hypercholesterolemic aortic-valve disease. N Engl J Med 349(7):717-8, 2003. Oxidative Stress Analogous to the role of oxidative stress in atherosclerosis, oxidant generation was confirmed in human AS.66-68 Superoxide and hydrogen peroxide levels were significantly elevated in calcified regions of stenotic valves, but the process might be different from oxidant generation in atherosclerosis, namely by reduced expression and activity of antioxidant enzymes and possibly NOS uncoupling instead of NADPH oxidase activity.66-68 Whether peroxide upregulates Msx2, Wnt/-catenin, and runx2/cbfa-1 as in vascular osteochondrogenic mineralization,69 needs further research. We hypothesize that oxidative stress might affect calcification/osteogenesis through different pathways and cell types during the evolution of AS, as the dominant cell types may vary at different stages of the disease. Nalini M. Rajamannan: The authors have clearly defined the different potential pathways for the development of this disease as described in this paragraph and also shown in Fig 1. Mineralization and Bone Formation Both calcific noduli and mature bone formation appear in AS, with calcific noduli being the first to be described in the era when calcification Curr Probl Cardiol, June 2010 297 was still considered passive, and later linked to plasma calcium and parathyroid hormone, with and without renal disease.70-72 To date calcific noduli are known to be initiated by macrophage- and obVIC-vesicles, and by apoptosis of aVICs, in response to (inflammatory) chemokines. Bone formation was described later, with presence of obVICs and upregulation of the osteoblast and bone markers osteopontin, bone sialoprotein, osteocalcin, alkaline phosphatase, and the osteoblast-specific transcription factor runx2/cbfa-1.73,74 The pathways modulating osteogenesis in AS known to date consist of Lrp-5/Wnt/-catenin,75 osteoprotegerin/ rankl/RANK,76,77 tenascin-C,78 Toll-like receptors 2 and 4,79,80 and angiotensin II, formed by chymase and cathepsin G from mast cells,81 and by ACE colocalizing with apolipoproteins.82 All pathways are considered potential new drug targets and subject to research. The exact timing of and contribution to calcification and bone formation in vivo needs to be further mapped. Nalini M. Rajamannan: The presence of osteoblastogenesis in the calcified aortic valve presents the foundation for the future experimental studies in this field. Further understanding the timing of the cellular pathways provides the future direction for the experimental studies in this field. Inflammatory Mechanisms of Degeneration Inflammation covers in AS the “cooperation” of endothelium, leukocytes, VICs, oxLDL,83 matrix and neo-angiogenesis as described above. Via a TGF1-dependent pathway (among others) the endothelium expresses adhesion molecules, facilitating uptake of LDL, lymphocytes, monocytes/macrophages, mast cells, and possibly pVICs. oxLDL might also in valvular endothelium upregulate caveolin-1 and consequently maintain the expression of endothelial adhesion molecules, and activate macrophages. qVICs might transform to aVICs and obVICS in response to inflammatory chemokines, with TGF again as main player, and an emerging role for Toll-like receptors. Neoangiogenesis further facilitates inflammation, serving as highway to the leaflet matrix.84 Genetics Last but not least, all the above-mentioned players in aortic valve pathobiology are subject to genetic variations, from which only the top of the iceberg is visible to date. Regarding bone metabolism, vitamin D receptor polymorphisms and a nonsense mutation with haploinsufficiency 298 Curr Probl Cardiol, June 2010 in Notch 1 have been described. The receptor B allele, leading to reduced calcium absorption, bone loss, and higher parathormone levels, is more frequent among patients with AS, from which we might deduct that calcium mobilization from bone enhances aortic valve calcification.85 Because Notch 1 acts, among other functions, as a repressor of Runx2, regulating osteoblast activity, a nonsense mutation might lead to diminished inhibition of calcium deposition.86 The Pvull polymorphism in the estrogen receptor ␣ gene might facilitate aortic stenosis through dyslipidemia.87 Regarding lipid metabolism, only conflicting data about allelic variants of apolipoproteins are published to date,88-90 while the results for genetic variations in inflammation and cell cycle regulatory genes are even more preliminary.91,92 The search for culprit genes should however be continued, both for early diagnosis in patients with genetic predisposition or in siblings in case of familial AS, as for treatment optimization guided by pharmacogenomics. The need is illustrated by a Finnish necropsy study with microcalcifications in anatomically normal aortic leaflets of young subjects,93 while the Finnish population is known for limited genetic variation, and a French epidemiologic study suggesting an autosomal-dominant inheritance, different from apoE or vitamin D receptor genes.94 Hypothesis on Calcific Aortic Valve Stenosis We hypothesize that all human individuals develop aortic sclerosis to a certain (subclinical) degree, due to aging and longstanding mechanical stress. However, only the patients with the appropriate genetic background and/or facilitating factors such as a bicuspid valve, smoking, diabetes, hypertension, dyslipidemia, or renal dysfunction will progress to severe AS within their lifespan, with an as reported variable rate of progression.95-97 AS is the common endpoint of diverse pathophysiological processes, able to develop independently from oxLDL. Why Did SEAS and SALTIRE Show No Effect on Aortic Valve Stenosis Progression? With the background provided, several possible reasons can be indicated. At first, the selected patients did not have dyslipidemia as facilitating factor for the progression of AS, so the effect would only depend on the pleiotropic effects of statins. Second, only patients with at least mild stenosis were included. As such the dysfunctional stress distribution and inflammation might already be self-perpetuating and surpassing the beneficial effect of statins. This hypothesis is supported by Curr Probl Cardiol, June 2010 299 the recent retrospective study of Antonini-Canterin et al, showing that statins only reduced progression in aortic sclerosis and mild AS, not in more advanced stages.98 Third, statins do not act on all pathways of AS pathophysiology, which on top do not fully resemble atherosclerosis. Last, but not least, plaque stabilization accounts for most of the beneficial effects of statins in atherosclerosis, but plaque rupture as a cause of symptoms is not an issue in AS. These trials are very valuable, however. As they emerged from the internationally growing conviction that statins alone could be capable of slowing the progression of AS, they can now be seen as the catalysts for further maturation of AS research. Nalini M. Rajamannan: LDL-Density-Radius Theory is a recently published theory describing trial design for future valvular heart disease. This theory incorporates the biology and the importance of the hemodynamic measurement for aortic valve disease using the continuity equation. Rajamannan NM. Mechanisms of aortic valve calcification: the LDL-density-radius theory: a translation from cell signaling to physiology. Am J Physiol Heart Circ Physiol 2009. What Should Be the Next Step? Further characterization of VICs and response to culture conditions is warranted, to optimize in vitro experiments to search for and test new drug targets, and test combinations and optimal timing of established drugs (statins, ACE-inhibitors, angiotensin-receptor blockers). In parallel the search for low cost animal models needs to be continued, at first to completely characterize the evolution of AS, both by immunohistochemics as by in vivo molecular imaging, followed by testing the drug regimens emerging from the in vitro experiments. Meanwhile, the genetic background influencing the evolution of AS and response to pharmacotherapy should be further mapped, to direct further human trials. At present statins are established players in cardiovascular prevention and should be administered to AS patients with a current guidelines indication. To date statins cannot be advocated to patients solely to prevent progression of AS. They might prove valuable as part of a drug regimen, as lipids are an important but not the only player in AS, taking into account timing and genetic background of the patient. Nalini M. Rajamannan: In summary, the authors have summarized the field of calcific aortic valve disease from experimental models to clinical trials extremely well. This paper demonstrates the potential for future experimental and clinical studies in this field. The authors have carefully reviewed the 300 Curr Probl Cardiol, June 2010 published data and have defined numerous mechanisms for this disease. In the future, medical therapy for calcific aortic valve disease will have many signaling pathways to target to try and slow progression of this disease. REFERENCES 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. Lindroos M, Kuppari M, Heikkilä J, et al. Prevalence of aortic valve abnormalities in the elderly: an echocardiographic study of a random population sample. J Am Coll Cardiol 1993;21(5):1220-5. Vahanian A, Baumgartner H, Bax J, et al. Guidelines on the management of valvular heart disease: the Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology. Eur Heart J 2007;28(2):230-68. Aronow WS, Ahn C, Kronzon I, et al. Association of coronary risk factors and use of statins with progression of mild valvular aortic stenosis in older persons. Am J Cardiol 2001;88(6):693-5. Novaro GM, Tiong I, Pearce GL, et al. Effect of hydroxymethylglutaryl coenzyme A reductase inhibitors on the progression of calcific aortic valve stenosis. Circulation 2001;104:2205-9. Bellamy MF, Pellikka PA, Klarich KW, et al. Association of cholesterol levels, hydroxymethylglutaryl coenzyme A reductase inhibitor treatment, and progression of aortic stenosis in the community. J Am Coll Cardiol 2002;40:1723-30. Shavelle DM, Takasu J, Budoff MJ, et al. HMG CoA reductase inhibitor (statin) and aortic valve calcium. Lancet 2002;359(9312):1125-6. Rosenhek R, Rader F, Loho N, et al. Statins but not angiotensin-converting enzyme inhibitors delay progression of aortic stenosis. Circulation 2004;110:1291-5. Moura LM, Ramos SF, Zamorano JL, et al. Rosuvastatin affecting aortic valve endothelium to slow the progression of aortic stenosis. J Am Coll Cardiol 2007; 49:554-61. Pohle K, Mäffert R, Ropers D, et al. Progression of aortic valve calcification. Association with coronary atherosclerosis and cardiovascular risk factors. Circulation 2001;104:1927-32. Rossebø AB, Pedersen T, Boman K, et al. Intensive lipid lowering with simvastatin and ezetimibe in aortic stenosis. N Engl J Med 2008;359:1343-56. Cowell SJ, Newby DE, Prescott RJ, et al. A randomized trial of intensive lipid-lowering therapy in calcific aortic stenosis. N Engl J Med 2005;352:2389-97. Lindroos M, Kupari M, Valvanne J, et al. Factors associated with calcific aortic valve degeneration in the elderly. Eur Heart J 1994;15(7):865-70. Stewart BF, Siscovick D, Lind BK, et al. Clinical factors associated with calcific aortic valve disease. Cardiovascular health study. J Am Coll Cardiol 1997;29: 630-4. Iung B, Baron G, Butchart EG, et al. A prospective survey of patients with valvular heart disease in Europe: the Euro heart survey on valvular heart disease. Eur Heart J 2003;24:1231-43. Olsson M, Dalsgaard CJ, Haegerstrand A, et al. Accumulation of T-lymphocytes and expression of interleukin-2 receptors in nonrheumatic stenotic aortic valves. J Am Coll Cardiol 1994;23(5):1162-70. Curr Probl Cardiol, June 2010 301 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 302 Otto CM, Kuusisto J, Reichenbach DD, et al. Characterization of the early lesion of degenerative valvular aortic stenosis. Histological and immunohistochemical studies. Circulation 1994;90:844-53. O’Brien KD, Reichenbach DD, Marcinova SM, et al. Apolipoproteins B, (a), and E accumulate in the morphologically early lesion of degenerative valvular aortic stenosis. Arterioscler Thromb Vasc Biol 1996;16:523-32. Rajamannan NM, Subramaniam M, Springett M, et al. Atorvastatin inhibits hypercholesterolemia-induced cellular proliferation and bone matrix production in the rabbit aortic valve. Circulation 2002;105:2660-5. Simmons CA, Grant GR, Manduchi E, et al. Spatial heterogeneity of endothelial phenotypes correlates with site-specific vulnerability to calcification in normal porcine aortic valves. Circ Res 2005;96:792-9. Vasile E, Antohe F. An ultrastructural study of beta very low density lipoprotein uptake and transport by valvular endothelium of hyperlipidemic rabbits. J Submicrosc Cytol Pathol 1991;23:279-87. Nievelstein-Post P, Mottino G, Fogelman A, et al. An ultrastructural study of lipoprotein accumulation in cardiac valves of the rabbit. Arterioscler Thromb 1994;14:1151-61. Rajamannan NM, Sangiorgi G, Springett M, et al. Experimental hypercholesterolemia induces apoptosis in the aortic valve. J Heart Valve Dis 2001;10:371-4. Drolet MC, Arsenault M, Couet J. Experimental aortic valve stenosis in rabbits. J Am Coll Cardiol 2003;41:1211-7. Cimini M, Boughner DR, Ronald JA, et al. Development of aortic valve stenosis in a rabbit model of atherosclerosis: an immunohistochemical and histological study. J Heart Valve Dis 2005;14:365-75. Zeng Z, Nievelstein-Post P, Yin Y, et al. Macromolecular transport in heart valves III: experiment and theory for the size distribution of extracellular liposomes in hyperlipidemic rabbits. Am J Physiol Heart Circ Physiol 2007;292:H2687-97. Luo G, Ducy P, McKee MD, et al. Spontaneous calcification of arteries and cartilage in mice lacking matrix gla protein. Nature 1997;386:78-81. Galvin KM, Donovan MJ, Lynch CA, et al. A role for SmadVI in development and homeostasis of the cardiovascular system. Nat Genet 2000;24:171-4. Lee TC, Zhao YD, Courtman DW, et al. Abnormal aortic development in mice lacking endothelial nitric oxide synthase. Circulation 2000;101:2345-8. Tanaka K, Sata M, Fukuda D, et al. Age-associated aortic stenosis in apolipoprotein E-deficient mice. J Am Coll Cardiol 2005;46:134-41. Garg V, Muth AN, Ransom JF, et al. Mutations in NOTCH 1 cause aortic valve disease. Nature 2005;437:270-4. Drolet MC, Roussel E, Deshaies Y, et al. A high fat/high carbohydrate diet induces aortic valve disease in C57BL/6J mice. J Am Coll Cardiol 2006;47:850-5. Weiss RM, Ohashi M, Miller JD, et al. Dl. Calcific aortic valve stenosis in old hypercholesterolemic mice. Circulation 2006;114:2065-9. Aikawa E, Nahrendorf M, Sosnovik D, et al. Multimodality molecular imaging identifies proteolytic and osteogenic activities in early aortic valve disease. Circulation 2007;115:377-86. Davignon J. Beneficial cardiovascular pleitropic effects of statins. Circulation 2004;109(suppl III):III-39-III-43. Curr Probl Cardiol, June 2010 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. 51. 52. Soini Y, Salo T, Satta J. Angiogenesis is involved in the pathogenesis of nonrheumatic aortic valve stenosis. Hum Pathol 2003;34(8):756-63. Rajamannan NM, Subramaniam M, Rickard D, et al. Human aortic valve calcification is associated with an osteoblast phenotype. Circulation 2003;107: 2181-4. Roberts WC, Ko JM. Frequency by decades of unicuspid, bicuspid and tricuspid aortic valves in adults having isolated aortic valve replacement for aortic stenosis, with or without associated regurgitation. Circulation 2005;111:920-5. Thubrikar MJ, Aouad J, Nolan SP. Patterns of calcific deposits in operatively excised stenotic or purely regurgitant aortic valves and their relation to mechanical stress. Am J Cardiol 1986;58(3):304-8. Nicosia MA, Cochran RP, Reichenbach DR, et al. A coupled fluid-structure finite-element model of the aortic valve and root. J Heart Valve Dis 2003;12:781-9. Davignon J, Ganz, P. Role of endothelial dysfunction in atherosclerosis. Circulation 2004;109(suppl lIII):III-27-III-32. Tiwari RL, Singh V, Barthwal MK. Macrophages: an elusive yet emerging therapeutic target of atherosclerosis. Med Res Rev 2008;28(4):483-544. Robicsek F, Thubrikar MJ, Fokin AA. Cause of degenerative disease of the trileaflet valve: review of the subject and presentation of a new theory. Ann Thorac Surg 2002;73:1346-54. Singh R, Strom JA, Ondrovic L, et al. Age-related changes in the aortic valve affect leaflet stress distributions: implications for aortic valve degeneration. J Heart Valve Dis 2008;17(3):290-8. Sacks MS, Yoganathan AP. Heart valve function: a biomechanical perspective. Philos Trans R Soc Lond 2007;362:1369-91. Balachandran K, Sucosky P, Jo H, et al. Elevated cyclic stretch alters matrix remodelling in aortic valve cusps: implications for degenerative aortic valve disease. Am J Physiol Heart Circ Physiol 2009;296:H756-764. Merryman WD, Lukoff HD, Long RA, et al. Synergistic effects of cyclic tension and transforming growth factor -1 on the aortic valve myofibroblast. Cardiovasc Pathol 2007;16:268-76. Sucosky P, Balachandran K, Elhammaly A, et al. Altered shear stress stimulates upregulation of endothelial VCAM-1 and ICAM-1 in a BMP-4- and TGF1dependent pathway. Arterioscler Thromb Vasc Biol 2009;29:254-60. El-Hamamsy I, Balachandran K, Yacoub MH, et al. Endothelium-dependent regulation of the mechanical properties of aortic valve cusps. J Am Coll Cardiol 2009;53:1448-55. Butcher JT, Penrod AM, Garcia AJ, et al. Unique morphology and focal adhesion development of valvular endothelial cells in static and fluid flow environments. Arterioscler Thromb Vasc Biol 2004;24:1429-34. Butcher JT, Tressel S, Johnson T, et al. Transcriptional profiles of valvular and vascular endothelial cells reveal phenotypic differences. Influence of shear stress. Arterioscler Thromb Vasc Biol 2006;26:69-77. Liu AC, Joag VR, Gotlieb AI. The emerging role of valve interstitial cell phenotypes in regulating heart valve pathobiology. Am J Pathol 2007;171:1407-18. Paranya G, Vineberg S, Dvorin E, et al. Aortic valve endothelial cells undergo transforming-growth-factor--mediated and non-transforming-growth-factor-mediated transdifferentiation in vitro. Am J Pathol 2001;159:1335-43. Curr Probl Cardiol, June 2010 303 53. 54. 55. 56. 57. 58. 59. 60. 61. 62. 63. 64. 65. 66. 67. 68. 69. 304 Paruchuri S, Yang JH, Aikawa E, et al. Human pulmonary valve progenitor cells exhibit endothelial/mesenchymal plasticity in response to vascular endothelial growth factor-A and transforming-growth-factor-2. Circ Res 2006;99:861-9. Yip CYY, Chen JH, Zhao R, et al. Calcification by valve interstitial cells is regulated by the stiffness of the extracellular matrix. Arterioscler Thromb Vasc Biol 2009;29:936. Monzack EL, Gu X, Masters KS. Efficacy of simvastatin treatment of valvular interstitial cells varies with the extracellular environment. Arterioscler Thromb Vasc Biol 2009;29:246-53. Wu B, Elmariah S, Kaplan FS, et al. Paradoxical effects of statins on aortic valve myofibroblasts and osteoblasts. Implications for end-stage valvular heart disease. Arterioscler Thromb Vasc Biol 2005;25:592-7. Anger T, El-Chafchak J, Habib A, et al. Statins stimulate RGS-regulated ERK ½ activation in human calcified and stenotic aortic valves. Exp Mol Pathol 2008; 85:101-11. Edep ME, Shirani J, Wolf P, et al. Matrix metalloproteinase expression in nonrheumatic aortic stenosis. Cardiovasc Pathol 2000;9:281-6. Fondard O, Detaint D, Iung B, et al. Extracellular matrix remodeling in human aortic valve disease: the role of matrix metalloproteinases and their tissue inhibitors. Eur Heart J 2005;26:1333-41. Satta J, Oiva J, Salo T, et al. Evidence for an altered balance between matrixmetalloproteinase-9 and its inhibitors in calcific aortic stenosis. Ann Thorac Surg 2003;76:681-8. Helske S, Syvaranta S, Lindstedt KA, et al. Increased expression of elasolytic cathepsins S, K, V and their inhibitor cystatin C in stenotic aortic valves. Arterioscler Thromb Vasc Biol 2006;26:1791-8. Helske S, Syvaranta S, Kupari M, et al. Possible role for mast cell-derived cathepsin G in the adverse remodeling of aortic valves. Eur Heart J 2006; 27:1495-504. Kaden JJ, Dempfle CE, Grobholz R, et al. Inflammatory regulation of extracellular matrix remodeling in calcific aortic valve stenosis. Cardiovasc Pathol 2005;14: 80-7. Mohty D, Pibarot P, Després JP, et al. Association between plasma LDL particle size, valvular accumulation of oxidized LDL, and inflammation in patients with aortic stenosis. Arterioscler Thromb Vasc Biol 2008;28:187-93. Warren BA, Yong JL. Calcification of the aortic valve: its progression and grading. Pathology 1997;29(4):360-8. Chen K, Thomas SR, Keaney JF Jr, et al. Oxidation: ROS in vascular signal transduction. Free Radic Biol Med 2003;35:117-32. Miller JD, Chu Y, Brooks RM, et al. Dysregulation of antioxidant mechanisms contributes to increased oxidative stress in calcific aortic valvular stenosis in humans. J Am Coll Cardiol 2008;52:843-50. Liberman M, Bassi E, Martinatti MK, et al. Oxidant generation predominates around calcifying foci and enhances progression of aortic valve calcification. Arterioscler Thromb Vasc Biol 2008;28:463-70. Towler DA. Oxidation, inflammation, and aortic valve calcification. J Am Coll Cardiol 2008;52:851-4. Curr Probl Cardiol, June 2010 70. 71. 72. 73. 74. 75. 76. 77. 78. 79. 80. 81. 82. 83. 84. 85. 86. Maher ER, Young G, Smyth-Walsh B, et al. Aortic and mitral valve calcification in patients with end-stage renal disease. Lancet 1987;2(8564):875-7. Ortlepp JR, Pillich M, Schmitz F, et al. Lower serum calcium levels are associated with greater calcium hydroxyapatite deposition in native aortic valves of male patients with severe calcific aortic stenosis. J Heart Valve Dis 2006;15(4):502-8. Linhartova K, Veselka J, Sterbakova G, et al. Parathyroid hormone and vitamin D levels are independently associated with calcific aortic stenosis. Circ J 2008;72: 245-50. O’Brien KD, Kuusisto J, Reichenbach DD, et al. Osteopontin is expressed in human aortic valvular lesions. Circulation 1995;92:2163-8. Mohler ER III, Gannon F, Reynolds C, et al. Bone formation and inflammation in cardiac valves. Circulation 2001;103:1522-8. Caira FC, Stock SR, Gleason TG, et al. Human degenerative valve disease is associated with up-regulation of low-density lipoprotein receptor-related protein-5 receptor-mediated bone formation. J Am Coll Cardiol 2006;47:1707-12. Kaden JJ, Bickelhaupt S, Grobholz R, et al. Receptor activator of nuclear factor kB ligand and osteoprotegerin regulate aortic valve calcification. J Mol Cell Cardiol 2004;36:57-66. Steinmetz M, Skowasch D, Wernert N, et al. Differential profile of the OPG/ RANKL/RANK system in degenerative aortic native and bioprosthetic valves. J Heart Valve Dis 2008;17(2):187-93. Satta J, Melkko J, Pöllänen R, et al. Progression of human aortic valve stenosis is associated with tenascin-C expression. J Am Coll Cardiol 2002;39:96-101. Meng X, Ao L, Song Y, et al. Expression of functional toll-like receptors 2 and 4 in human aortic valve interstitial cells: potential roles in aortic valve inflammation and stenosis. Am J Physiol Cell Physiol 2008;294:C29-35. Yang X, Fullerton DA, Su X, et al. Pro-osteogenic phenotype of human aortic valve interstitial cells is associated with higher levels of toll-like receptors 2 and 4 and enhanced expression of bone morphogenic protein 2. J Am Coll Cardiol 2009; 53(6):491-500. Helske S, Lindstedt KA, Laine M, et al. Induction of local angiotensin II producing systems in stenotic aortic valves. J Am Coll Cardiol 2004;44:1859-66. O’Brien KD, Shavelle DM, Caulfield MT, et al. Association of angiotensinconverting enzyme with low-density lipoprotein in aortic valvular lesions and in human plasma. Circulation 2002;106:2224-30. Holvoet P, De Keyzer D, Jacobs DR, et al. And the metabolic syndrome. Futures Lipidol 2008;3(6):637-49. Mazzone A, Epistolato MC, De Caterina R, et al. Neoangiogenesis, T-lymphocyte infiltration, and heat shock protein- 60 are biological hallmarks of an immunomediated inflammatory process in end-stage calcified aortic valve stenosis. J Am Coll Cardiol 2004;43:1670-6. Ortlepp JR, Hoffmann R, Ohme F, et al. The vitamin D receptor genotype predisposes to the development of calcific aortic valve stenosis. Heart 2001;85: 635-8. Garg V, Muth AN, Ransom JF, et al. Mutations in Notch 1 cause aortic valve disease. Nature 2005;437:270-4. Curr Probl Cardiol, June 2010 305 87. 88. 89. 90. 91. 92. 93. 94. 95. 96. 97. 98. 306 Nordström P, Glader CA, Dahlen G, et al. Oestrogen receptor alpha gene polymorphism is related to aortic valve sclerosis in postmenopausal women. J Intern Med 2003;254:140-6. Novaro GM, Sachar R, Pearce GL, et al. Association between apolipoprotein E alleles and calcific valvular heart disease. Circulation 2003;108:1804-8. Avakian SD, Annicchino-Bizzacchi JM, Grinberg M, et al. Apolipoproteins AI, B, and E polymorphisms in severe aortic valve stenosis. Clin Genet 2001;60:381-4. Ortlepp JR, Pillich M, Mevissen V, et al. ApoE alleles are not associated with calcific aortic stenosis. Heart 2006;92:1463-6. Ortlepp JR, Schmitz F, Mevissen V, et al. The amount of calcium-deficient hexagonal hydroxyapatite in aortic valves is influenced by gender and associated with genetic polymorphisms in patients with severe calcific aortic stenosis. Eur Heart J 2004;25:514-22. Golubnitschaja O, Yeghiazaryan K, Skowasch D, et al. P21WAF1/CIP1 and 14-3-3 sigma gene expression in degenerated aortic valves: a link between cell cycle checkpoints and calcification. Amino Acids 2006;31:309-16. Kuusisto J, Räsänen K, Särkioja T, et al. Atherosclerosis-like lesions of the aortic valve are common in adults of all ages: a necropsy study. Heart 2005;91:576-82. Probst V, Le Scouarnec S, Legendre A, et al. Familial aggregation of calcific aortic valve stenosis in the western part of France. Circulation 2006;113:856-60. Roger VL, Tajik AJ, Bailey, KR, et al. Progression of aortic stenosis in adults: new appraisal using Doppler echocardiography. Am Heart J 1990;119:331-8. Rosenhek R, Klaar U, Schemper M, et al. Mild and moderate aortic stenosis. Natural history and risk stratification by echocardiography. Eur Heart J 2004;25: 199-205. Briand M, Lemieux I, Dumesnil JG, et al. Metabolic syndrome negatively influences disease progression and prognosis in aortic stenosis. J Am Coll Cardiol 2006;47:2229-36. Antonini-Canterin F, Hirsu M, Popescu BA, et al. Stage-related effect of statin treatment on the progression of aortic valve sclerosis and stenosis. Am J Cardiol 2008;102:738-42. Curr Probl Cardiol, June 2010