Calcific Aortic Valve Disease and Aortic Atherosclerosis
advertisement

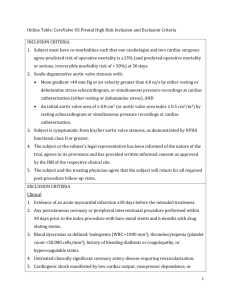
Calcific Aortic Valve Disease and Aortic Atherosclerosis – Two Faces of the Same Disease? CARMEN GINGHINĂ¹,², ANCA FLORIAN², C. BELADAN¹,², M. IANCU², ANDREEA CĂLIN¹,², B.A. POPESCU¹,², RUXANDRA JURCUŢ¹,² ¹Department of Cardiology, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania ²Department of Cardiology, “Prof. Dr. C.C. Iliescu” Institute of Emergency for Cardiovascular Diseases, Bucharest, Romania Calcific (degenerative) aortic valve disease is the most common etiology of acquired aortic valve stenosis. Historically, it was seen as a degenerative, “senile-like” process, resulting from aging – “wearing and tearing” – of the aortic valve. However, several lines of evidence suggest that calcific valve disease is not simply due to age-related degeneration but, rather, it is an active disease process with identifiable initiating factors, clinical and genetic risk factors, and cellular and molecular pathways that mediate disease progression. Histopathologically, the early lesions of aortic valve sclerosis resemble arterial atherosclerotic plaques. Furthermore, atherosclerotic risk factors and clinical atherosclerotic cardiovascular disease are independently associated with aortic sclerosis suggesting that it represents an atherosclerosis-like process involving the aortic valve. Until now, the only established treatment for symptomatic aortic valve stenosis has been valve replacement. Newer therapies that may modify or reduce the likelihood of developing aortic valve disease are highly desirable and are currently under investigation. In this article we tried to review the available data on calcific aortic valve disease, starting from histological and pathogenic aspects and finishing with therapeutic implications, in order to characterize its relationship with the atherosclerotic process. Key words: aortic stenosis, aortic sclerosis, atherosclerosis risk factors. Calcific aortic valve disease is identified by thickening and calcification of the aortic valve leaflets in the absence of rheumatic heart disease. It is divided, on a functional basis, into aortic sclerosis, in which the leaflets do not obstruct left ventricular outflow and aortic stenosis in which obstruction to left ventricular outflow is present. Aortic sclerosis is present in more than 25% of patients over age 65 and is associated with a 50% increase of risk of cardiovascular events [1]. Aortic stenosis is present in 2% to 5% of very elderly patients, is the second most common indication for cardiac surgery [2] and carries an 80% 5-year risk of progression to heart failure, valve replacement, or death [3]. Calcific (degenerative) aortic valve disease is the most common etiology of acquired aortic valve stenosis [4]. Historically, it was seen as a degenerative, “senile-like” process, resulting from aging – “wearing and tearing” – of the aortic valve [5]. However, several lines of evidence suggest that calcific valve disease is not simply due to agerelated degeneration but, rather, is an active disease process with identifiable initiating factors, clinical and genetic risk factors, and cellular and molecular ROM. J. INTERN. MED., 2009, 47, 4, 319–329 pathways that mediate disease progression [6]. Histopathologically, the early lesions of aortic valve sclerosis resemble arterial atherosclerotic plaques [7]. Furthermore, atherosclerotic risk factors [8] and clinical atherosclerotic cardiovascular disease [1] are independently associated with aortic sclerosis suggesting that it represents an atherosclerosis-like process involving the aortic valve [9]. CALCIFIC AORTIC VALVE DISEASE: HISTOLOGIC AND PATHOGENIC FEATURES – SIMILARITIES AND DISSIMILARITIES WITH ATHEROSCLEROTIC CARDIOVASCULAR DISEASE As we mentioned above, emerging data suggest that calcific aortic valve disease is an active disease process with initiating factors, “early lesions” and more advanced processes comprising cellular and molecular pathways that mediate disease progression. Among the proposed theories for the initiating factor that leads to aortic stenosis, there is most support for a mechanical stress hypothesis [7]. Hydrodynamic studies have shown that a high mechanical stress occurs at the flexion area of the aortic cusps near the attachment to the aorta root and 320 Carmen Ginghină et al. the line of coaptation [10]. Aortic endothelium at areas of high mechanical stress demonstrates subtle changes consistent with mild damage and becomes more susceptible to lipid deposition and infiltration by macrophages. This process is accelerated in the bicuspid aortic valve because the abnormal cusps and raphe are subject to greater mechanical stress [11]. Although all aortic valves are subject to longterm mechanical stress and this is the initiating factor, only a minority of elderly individuals develop aortic stenosis, so other factors must be important in subsequent disease progression [12]. The “early lesions “of degenerative aortic stenosis are characterized by subendothelial thickening with disruption of the basement membrane, intra- and extracellular lipid deposition, chronic inflammation, renin-angiotensin system local activation and accumulation of protein, lipid, and calcium [13]. Similarly to atherosclerosis, the “atherogenic” lipoproteins, LDL and Lp(a), are deposited in human aortic valve lesions [14] and aortic valve cholesterol content is increased in a hypercholesterolemic rabbit model of aortic valve disease [15]. Oxidized lipids have also been detected in human aortic valve lesions, particularly in areas of developing calcification. In vitro studies have shown that oxidized cholesterol stimulates calcified nodule formation by valve fibroblasts, and that calcified nodule formation by these cells is inhibited by simvastatin [16]. In 1994 a series of 3 studies reported that aortic valve lesions contained the cell types characteristic of chronic inflammation: macrophages and T lymphocytes [7][17]. More recently, mast cells and the proinflammatory cytokines, IL-1 β and tumor necrosis factor (TNF)-α, also have been identified in stenotic aortic valves [18][19]. In addition, aortic valves lesions contain a number of matrix-metalloproteinases (MMPs), which degrade various components of the extracellular matrix [18]. In the case of atherosclerosis, MMPs appear to play important roles in the regulation of vascular calcification, but they are also thought to play a key role in the extracellular matrix degradation and subsequent plaque instability [20]. Recent studies have also implicated the renin–angiotensin system, particularly angiotensin converting enzyme (ACE), angiotensin II (Ang II), and the angiotensin II Type 1 (AT1) receptor in aortic valve lesion pathogenesis [21][22]. Aortic valve lesions contain a number of potential sources of Ang II: LDL-associated ACE, macrophage associated ACE and mast cells. Ang II has a number of potential, AT-1 receptor–mediated, lesion-promoting effects: stimulating inflammation 2 and macrophage cholesterol accumulation, impairing fibrinolysis, increasing oxidant stress and stimulating fibroblast expression. The major pathogenic receptor for Ang II is present in valve lesion fibroblasts [21]. In addition to fibrosis, dystrophic calcification is the defining feature of aortic valve lesions and in advanced stages it becomes the dominant process [11]. Calcification first occurs in the areas of lipid deposition and, in time, may contribute to lesion rigidity, thereby worsening obstruction to left ventricular outflow. Moreover, the extent of lesion calcification correlates both with more rapid disease progression and worse clinical outcomes [23]. Aortic valve calcification now has been shown unequivocally to be an active, rather than a passive, process. Valvular calcium deposits contain both calcium and phosphate as hydroxyapatite, the form of calciumphosphate mineral present in both calcified arterial tissue and bone [24][25]. Proteins such as osteopontin [26], implicated in calcification and calcifying valve cells with osteoblast-like activities, have been detected in calcified aortic valves [27]. Also, lamellar bone was found in 13% of valves with dystrophic calcification. In summary, calcific aortic disease initiation and progression consists in an active inflammatory process with some similarities (lipid deposition, macrophage and T cell infiltration, and basement membrane disruption) and some dissimilarity (presence of prominent mineralization and small numbers of smooth muscle cells) to atherosclerosis [7]. CALCIFIC AORTIC VALVE DISEASE: HISTOLOGIC AND PATHOGENIC FEATURES – ASSOCIATION WITH ATHEROSCLEROSIS Early atherosclerosis involves the endothelium of many arteries. Vascular dysfunction has been implicated as an early event in atherogenesis [28] and, associated with vascular injury, has been postulated as the precursor of atherosclerosis [29]. Poggiati et al. [30] examined the association between aortic valve sclerosis (imaged by transthoracic echocardiography) and systemic endothelial manifestations of the atherosclerotic process in a study population with known or suspected coronary artery disease, referred for a stress echocardiography test. They used, among the investigational tools, an endothelial function study, with assessment of endothelium-dependent, post-ischemic, flow-mediated dilation. They demonstrated that aortic valve stenosis is associated with systemic endothelial dysfunction with flow- 3 Calcific aortic valve disease and aortic atherosclerosis mediated dilation being highly predictive of aortic valve sclerosis. No significant differences were found in patients with or without aortic valve sclerosis regarding the presence of significant coronary artery disease at coronarography. Agmon et al. [31] examined the association between atherosclerosis risk factors, anatomically defined atherosclerosis (atherosclerosis of the thoracic aorta imaged by transesophageal echocardiography) and aortic valve sclerosis in the general population from the SPARC study [32]. “Atherosclerosis” was defined as irregular intimal thickening (≥2mm) with increased echogenicity. Aortic valve abnormalities were examined both morphologically and functionally (peak transaortic flow velocities). They demonstrated that atherosclerotic risk factors and proximal aortic atherosclerosis are independently associated with aortic valve abnormalities in the general population (p< 0.001). Weisenberg et al. [33] evaluated, by intraoperative transesophageal echocardiography, 91 consecutive patients with severe aortic stenosis who underwent aortic valve replacement (with matching pairs without valve disease) in order to determine the presence and characteristics of aortic atheromas. They found a strong association between the presence of severe aortic stenosis and the presence and severity of aortic atheromas, the majority of patients having the lesions localized in the aortic arch (66% pts, 45.7% complex atheromas) and descending aorta (77% pts, 50% complex atheromas). They also suggested that transesophageal echocardiography might become part of the preoperative evaluation and the presence of aortic atheromas should be taken into account when analyzing the risk/benefit ratio for these patients considering the high incidence of perioperative stroke associated with complex atheromas. Goland et al. [34] retrospectively evaluated 105 consecutive patients with severe degenerative aortic stenosis who underwent aortic valve replacement. These patients were compared with 54 sex- and agematched patients without aortic stenosis or coronary artery disease. Aortic atheroma (localized intimal thickening of >3 mm) prevalence and morphology in three segments of aorta were assessed with echocardiography. They found that patients with severe aortic stenosis and coexisting coronary artery disease had more extensive atherosclerotic changes in the thoracic aorta as compared with those with aortic stenosis alone and control subjects. They also had more complex atheromas in the aortic arch and a higher percentage for the presence of plaques in two 321 or three segments (p < 0.0001) as compared with the other groups. CALCIFIC AORTIC VALVE DISEASE: RISK FACTORS – SIMILARITIES AND DISSIMILARITIES WITH ATHEROSCLEROTIC CARDIOVASCULAR DISEASE The effect of hypercholesterolemia on the development of sclerotic changes involving the heart valves has been demonstrated on animal models [35][36]. For example, a recent study showed that mice with hyperlipidemia due to over expression of apolipoprotein E4 all developed severe aortic stenosis in addition to coronary disease [37]. Also, valvular and supravalvular aortic stenosis are well known in human subjects with familial hypercholesterolemia, and aortic stenosis may regress with aggressive reduction of serum cholesterol [38]. Several studies have documented overlap in the clinical factors traditionally associated with calcific valve disease and atherosclerosis [39– 47][79][80][81]. Some of these studies had obvious limitations given the fact that they included patients expected to have a high prevalence of atherosclerotic risk factors: older age (Aronow et al., Lindroos et al.), patients referred for cardiac catheterization (Deutscher et al., Hoagland et al.). The largest prospective population-based study, the Cardiovascular Health Study [39], which included 5621 adults over the age of 65 years, reported a positive association of aortic valve disease with risk factors including age, male gender, smoking, history of hypertension and high Lp (a) and LDL cholesterol levels. Interestingly, the strength of these associations is comparable to that seen with atherosclerotic disease [39]. Mohler et al. [41] was one of the less who compared risk factors for aortic stenosis in bicuspid versus tricuspid aortic valves. Race, male gender and low triglyceride levels were correlated with age at surgery in bicuspid aortic valves, whereas male gender and smoking were the risk factors for patients with degenerative tricuspid aortic stenosis. Many of the studies looking at atherosclerotic risk factors in aortic stenosis were limited by the use of retrospective data, varying definition of aortic valve disease (only five of these studies assessed the morphology of the aortic valve: bicuspid vs. tricuspid) and referral bias (surgery, cardiac catheterization). Carmen Ginghină et al. 322 4 Jeevanantham et al. proposed Hs-CRP as a tool for identifying patients in the early stages of calcific aortic valve disease, in whom medical treatment may be beneficial to halt the progression to irreversible aortic valvular calcification and stenosis. The second risk factor studied was homocysteine; Novaro et al. [52] failed in finding any association between aortic valve disease and serum homocysteine. Taken together, we may state that atherosclerotic risk factors, particularly hypercholesterolemia, are associated with calcific aortic stenosis. However, there are differences between the processes underlying aortic stenosis and atherosclerosis (Table I). Only one-half of the patients with aortic stenosis have coronary artery disease and a minority of patients with coronary artery disease have concomitant aortic stenosis [53]. Katz et al. [48], compared the prevalence of aortic valve calcification, assessed by computed tomography in 6780 Multi-Ethnic Study of Atherosclerosis (MESA) participants with metabolic syndrome, diabetes mellitus, or neither condition. In this cohort, the metabolic syndrome and diabetes mellitus were associated with increased risk of aortic valve calcification and its prevalence was increased with increasing the number of metabolic syndrome components. A number of studies analyzed the association between “novel” risk factors of atherosclerosis and aortic valve disease. The first one of the risk factors was Hs-CRP (high sensitivity C-reactive protein) and the results were various, ranging from no correlation [49], weak association [50] to significant association with calcific aortic valve disease during its early stage [51]. In the last study, Table I Comparison of sclerotic process in aortic stenosis with that in atherosclerosis Aortic stenosis Atherosclerosis Inflammatory changes Systemic markers of inflammation ++++ ++++ + ++ Lipid accumulation Oxidized lipids ++++ ++++ Calcification ++++ +++++ ++++ ++ Role of infective agents ± ± Dominant cell Fibroblast Smooth muscle Role of genetic factors ++ +++ Modified from Chan KL (13) and Freeman RV (78) Causes accounting for the discordance between the two processes have not been well defined, but may be related to genetic factors acting through pathways such as those involving angiotensin-converting enzyme and vitamin D [13]. A recent study by Ortlepp et al. suggested that the B allele of the vitamin D receptor may be a predisposing factor for aortic stenosis [54]. Recent studies have emphasized not only the importance of bicuspid aortic valves as a risk factor for aortic stenosis [55], but also demonstrated one specific genetic defect that can contribute to bicuspid valve morphogenesis [56]. A recent, single center, consecutive series of 932 surgically excised nonrheumatic aortic stenosis valves found 49% of these valves to be congenitally bicuspid. This would represent a substantial enrichment of the proportion of congenitally abnormal valves in nonrheumatic aortic stenosis as compared with the overall population and suggests that the bicuspid valve has a much more powerful and widespread influence on progression to severe disease than recognized previously [55]. Also, in patients with bicuspid aortic valves, compared with those having normal trileaflet aortic valves, ascending aortic dilatation occurs more frequently and at a younger age and the presence of associated medial defects lead to a higher prevalence and faster rate of ascending aortic dilatation, with increased risk of dissection (Fig. 1). Other factors that may be associated with aortic valve sclerosis include: uremia [57], elevated calcium [58], elevated parathyroid hormone [59], osteoporosis [60], Paget disease [61], and significant renal failure [62]. Some of these factors act by accelerating atherosclerosis, but, in addition, they promote the valvular disease process by altering systemic calcium metabolism and by generating a high-output state with increased valvular mechanical stress. 5 Calcific aortic valve disease and aortic atherosclerosis A 323 B C Fig. 1. – 2D transthoracic and transesophageal echocardiographic images showing an intense calcified bicuspid aortic valve with severe aortic stenosis (A, B) and a dilated ascending aorta (C). It is known that in time, not all patients with aortic sclerosis develop some degree of aortic stenosis, with a substantial variability in the annual rate of progression between individuals [63]. A number of studies that have examined this question found a series of factors associated with the progression of aortic sclerosis: increasing age [64–66], male sex [67], dyslipidemia [65][67][68], tobacco use [65][67][68], hypertension [67], diabetes mellitus [67], obesity (69), elevated serum calcium [68], elevated serum creatinine [68], aortic valve calcification [70], coronary artery disease [71], baseline aortic valve area [72][73], baseline pressure gradient [74]. CALCIFIC AORTIC VALVE DISEASE: CLINICAL AND PROGNOSTIC FEATURES – ASSOCIATION WITH ATHEROSCLEROSIS The relationship between aortic calcific disease and atherosclerosis is bidirectional. On the one hand, aortic sclerosis was linked to adverse ischemic cardiovascular events. For example, in the population based cardiovascular health study, the presence of aortic sclerosis on echocardiography in adults over age 65 years, with no known coronary artery disease at study entry, was associated with a 50% increased risk of cardiovascular mortality and 324 Carmen Ginghină et al. myocardial infarction over a mean follow-up interval of 5.5 years [1]. In addition, patients admitted with chest pain and aortic sclerosis had a higher incidence of cardiovascular events and worse event-free survival than did those without aortic sclerosis [75]. It has been proposed that aortic sclerosis gives a “window to the coronary arteries” without the need for an angiogram [76]. These findings suggest that there is a pathogenic link between aortic sclerosis and acute coronary syndromes that is beyond that of shared coronary risk factors and that aortic sclerosis is an incremental risk above conventional risk factors. Nightingale et al. concluded in their review article [77] that “aortic sclerosis is not an innocent murmur but a marker of increased cardiovascular risk”. On the other hand, most patients with coronary artery disease do not have aortic stenosis and in adults with severe aortic stenosis, only about 50% have significant coronary artery disease. Last, but not least, in aortic stenosis a large contributor of disease progression is prominent calcification with a gradual increase in leaflet thickness and outflow obstruction. In contrast, events in patients with coronary atherosclerosis are acute, related to plaque rupture with associated thrombosis and vascular occlusion. Thus, as a bridge to the discussion about treatment options in aortic sclerosis, plaque stabilization and anti thrombotic treatment strategies are less likely to be beneficial calcific valve disease [78]. TREATMENT OF CALCIFIC AORTIC VALVE DISEASE PROGRESSION – TARGETING ATHEROSCLEROTIC DISEASE PROCESSES There is no effective therapy for severe symptomatic aortic stenosis other than surgical aortic valve replacement. As we have shown above, calcific aortic valve disease consists in an active pathobiological process, having common pathways with atherosclerosis. Endothelial dysfunction [30] and increased low-grade systemic inflammation were demonstrated in patients with calcific aortic valve disease [51] and one question is if the relationship between these findings and the valvular degenerative process is bidirectional. Chenevard et al. [82] hypothesized that altered hemodynamics in aortic stenosis may be partly responsible for endothelial dysfunction and thus potentially normalize after aortic valve replacement. Their results suggest that there is an ongoing disease process that may not be entirely halted by removal 6 of the diseased valve, similar to that described in atherosclerosis. This strengthens even more the need to pharmacologically control these processes. Targeted pharmacotherapeutic regimens to interfere with the disease pathways to either slow or halt the disease are under investigation [78]. Potential points of action of these medical regimens would be: leaflet endothelial layer disruption, activation of inflammatory cascade, release of inflammatory cytokines, lipoprotein accumulation and deposition, lipid oxidation, angiotensin-mediated effects, tissue calcification and osteogenesis [78]. The two pharmacological agents currently evaluated for potentially delaying disease progression are HMG-CoA reductase inhibitors (statins) and ACE inhibitors. HMG-CoA reductase inhibitors have mechanisms of action that expand their effects beyond cholesterol lowering [83]. Statins may influence both risk factors and inflammatory pathways by lowering lipid levels and exerting a range of anti-inflammatory properties, called “pleiotropic effects”. These pleiotropic effects include: anti-oxidation [84], improvement of endothelial function, anti-thrombotic actions, plaque stabilization, reduction of the vascular inflammatory process and modulation of the T-cell activation [85][86]. The hypothesis that lipid-lowering therapy might slow or prevent disease progression was tested in several types of studies, first experimental models and retrospective studies and in the last years, a number of prospective, randomized controlled trials. In an experimental hypercholesterolemic rabbit model of early calcific aortic valve disease, Rajamannan et al. demonstrated a decrease in cellular proliferation and bone matrix production within the aortic valve after administration of atorvastatin [87]. Table II illustrates some of the available clinical studies that support an association of statin use and slowed disease progression. In the retrospective cohorts, statins were generally prescribed by the primary care providers for conventional indications, and the association of statin use with progression of calcific valve disease was assessed. Interestingly, despite the relatively consistent slowing of disease progression in those patients receiving statin therapy, there was a relative lack of correlation with the effect on serum cholesterol levels, with some studies showing an association [67][88] [89][97] and others showing none [66][90–92]. This inconsistency likely represents some of the limitations inherent in retrospective analyses but also supports the theory that statins provide additional, pleiotropic benefits beyond cholesterol lowering. 7 Calcific aortic valve disease and aortic atherosclerosis 325 Table II Statin therapy in aortic stenosis: clinical studies Study (year) Retrospective Aronow et al. (2001) (81) Novaro et al. (2001) (66) Pohle et al. (2001) (88) Bellamy et al. (2002) (90) Shavelle et al. (2002) (91) Rosenhek et al. (2004) (92) Antonini-Canterin et al. (2008) (97) Prospective Moura et al. (2007) RAAVE (93) Cowell et al. (2005) SALTIRE (94) Rosseb et al. (2008) SEAS (95) Total number of patients (% taking statins) 180 (34%) Average follow-up Method of evaluation > 2 years Echocardiography 174 (33%) 104 (52%) 156 (24%) 65 (43%) 211 (39%) 1046 (29.5%) 21 months 15 months 3.7 ± 2.3 years 2.5 ± 1.6 years 2.0 ± 1.5 years 5.6 ± 3.2 years 121 (50.4%) Parameter followed p Echocardiography EBCT Echocardiography EBCT Echocardiography Echocardiography peak transaortic gradient AVA decrease median AVC change AVA decrease median AVC change jet velocity increase jet velocity increase 0.03 NS 0.04 0.006 <0.0001 0.01 73 ± 24 weeks Echocardiography jet velocity increase 0.007 155 (50.3%) 25 months 52.2 months jet velocity increase AVC change primary outcome NS 1873 (50.3) Echocardiography EBCT Primary outcome: composite of major cardiovascular events* Echocardiography (In progress) ASTRONOMER (96) 0.001 NS AVA indicates aortic valve area; EBCT, electron-beam computed tomography; and AVC, aortic valve calcium. * death from cardiovascular causes, aortic-valve replacement, nonfatal myocardial infarction, hospitalization for unstable angina pectoris, heart failure, coronary-artery bypass grafting, percutaneous coronary intervention, and nonhemorrhagic stroke. Modified from Freeman RV, Otto CM [78] There are 4 prospective, randomized, placebocontrolled, multicenter studies with conflicting results regarding the role of statin therapy in calcific aortic disease progression. In the Rosuvastatin Affecting Aortic Valve Endothelium (RAAVE) study [93] prospective treatment of moderate to severe aortic stenosis with 20 mg rosuvastatin per day by targeting serum LDL slowed the disease progression as measured by echocardiography. In opposition, at least two years of atorvastatin at 80 mg/day in the Scottish Aortic Stenosis and Lipid Lowering Trial, Impact on Regression (SALTIRE) study [94], reduced LDL cholesterol by more than 50% but had no significant effect on the extent of aortic-valve calcification or change in aortic-jet velocity. But, in SALTIRE the patient aortic disease was, on average, substantially more advanced than in RAAVE (mean valve area 1 cm2 vs. 1.23 cm2). The SEAS trial (Simvastatin and Ezetimibe in Aortic Stenosis) [95] randomized and followed for a median of 52 months, 1873 patients with mild-to-moderate, asymptomatic aortic stenosis, receiving either 40 mg of simvastatin plus 10 mg of ezetimibe or placebo daily. Simvastatin and ezetimibe did not reduce the composite outcome of combined aortic-valve events and ischemic events in patients with aortic stenosis. One ongoing trial: Aortic Stenosis Progression Observation: Measuring the Effect of Rosuvastatin (ASTRONOMER) assessing the effects of 40 mg rosuvastatin daily compared to usual care in patients diagnosed with mild to moderate aortic valvular stenosis and no clinical indication for the use of cholesterol lowering agents should eventually help determine whether statins and other lipid-lowering agents are indeed beneficial in patients with aortic stenosis [96]. Another problem to be solved is if and when there is an optimal time interval in which patients might benefit from statin therapy in the course of their disease progression. Although there are strong proponents of ACE inhibitor use in aortic stenosis, the basis of the recommendations to date has been on the potentially favorable effect of ACE inhibitors on the remodeling and hypertrophic changes of the myocardium in aortic stenosis, [98] rather than an effect on delaying disease progression at the tissue level. However, it is premature to conclude that ACE inhibition is not beneficial. Further investigations will be needed to Carmen Ginghină et al. 326 establish the potential benefit of ACE inhibitors on disease progression. CONCLUSION Calcific aortic disease represents a disease spectrum ranging from aortic sclerosis to severe aortic stenosis and consisting in an active process with risk factors, initiating lesions, clinical factors 8 and pathogenic pathways of progression. Calcific aortic disease and atherosclerosis share a large number of common features on different levels from histologic and pathogenic to, a lesser extent, clinical, prognostic and therapeutic ones. Nevertheless, from a clinical and therapeutic point of view, calcific aortic disease and atherosclerosis remain two different conditions, both associated with increasing prevalence and morbidity as the population ages. Afectarea valvulară degenerativă reprezintă cea mai frecventă cauză dobândită a stenozei aortice. În trecut, aceasta a fost considerată consecinţa unui proces degenerativ, asemănător îmbătrânirii, datorat „uzurii” valvei aortice. În ultimii ani s-au adunat tot mai multe date care sugerează că afectarea valvulară degenerativă nu se datorează modificărilor legate de îmbătrânire, ci constituie un proces activ caracterizat prin factori iniţiatori, factori de risc clinici şi genetici şi procese celulare şi moleculare care mediază progresia bolii. Din punct de vedere anatomopatologic, leziunile iniţiale din scleroza aortică sunt asemănătoare celor din placa aterosclerotică. Mai mult decât atât, factorii de risc pentru ateroscleroza şi boala vasculară aterosclerotică manifestă se asociază independent cu scleroza aortică sugerând că aceasta reprezintă rezultatul unui proces asemănător aterosclerozei la nivelul valvelor aortice. La acest moment, singurul tratament al stenozei aortice severe simptomatice este înlocuirea valvulară. Terapiile noi, cu potenţialul de a reduce sau modifica progresia bolii valvulare aortice degenerative, reprezintă o necesitate şi sunt în curs de evaluare. În acest articol, am încercat să sumarizăm datele existente până în acest moment cu privire la afectarea valvulară aortică degenerativă, începând cu aspectele histologice şi de patogenie şi încheind cu implicaţiile terapeutice, cu scopul de a caracteriza relaţia dintre aceasta şi procesul aterosclerotic. Corresponding address: Carmen Ginghina, MD Department of Cardiology, “Prof. Dr. C.C. Iliescu” Institute of Emergency for Cardiovascular Diseases Sos. Fundeni no. 258, 022328, Bucharest, Romania E-mail: carmenginghina2001@yahoo.com REFERENCES 1. 2. 3. 4. 5. 6. 7. 8. OTTO C.M., LIND B.K., KITZMAN D.W. et al., Association of aortic valve sclerosis with cardiovascular mortality and morbidity in the elderly. N. Eng. J. Med., 1999; 341:142–7. ROBERTS W.C., KO J.M., Frequency by decades of unicuspid, bicuspid, and tricuspid aortic valves in adults having isolated aortic valve replacement for aortic stenosis, with or without associated aortic regurgitation. Circulation, 2005; 111:920–25. OTTO C.M., BURWASH I.G., LEGGET M.E. et al., Prospective study of asymptomatic valvular aortic stenosis. Clinical, echocardiographic, and exercise predictors of outcome. Circulation, 1997; 95:2262–70. SELZER A., Changing aspects of the natural history of valvular aortic stenosis. N. Engl. J. Med., 1987; 317:91–8. POMERANCE A., Ageing changes in human heart valves. Br. Heart J. 1967; 29:222–231. OTTO C.M., Calcific aortic stenosis – time to look more closely at the valve. N. Engl. J. Med., 2008; 359(13):1395–8. OTTO C.M., KUUSISTO J., REICHENBACH D.D. et al., Characterization of the early lesion of “degenerative” valvular aortic stenosis; histologic and imunohistochemical studies. Circulation, 1994; 90:844–53. STEWART B.F., SISCOVICK D., LIND B.K. et al., Clinical factors associated with calcific aortic valve disease. J. Am. Coll. Cardiol., 1997; 29:630–4. 9 Calcific aortic valve disease and aortic atherosclerosis 327 9. WIERZBICKI A., SHETTY C., Aortic stenosis an atherosclerotic disease? J. Heart Valve disease, 1999; 8:416–423. 10. ZAND T., MAJNO G., NUNNARI J.J. et al., Lipid deposition and intimal stress and strain: a study in rats with aortic stenosis. Am. J. Pathol., 1991; 139:101–13. 11. DAVIES M.J., TREASURE T., PARKER D.J., Demographic characteristics of patients undergoing aortic valve replacement for stenosis: relation to valve morpholoy. Heart, 1996; 75:174–8. 12. LINDROOS M., KUPARI M., HEIKKILA J., Prevalence of aortic valve abnormalities in the elderly: an echocardiographic study of a random population sample. J. Am. Coll. Cardiol., 1993; 21:1220–5. 13. CHAN K.L., State of the art paper: Is aortic stenosis a preventable disease? J. Am. Coll. Cardiol., 2003; 42(4):593–9. 14. O’BRIEN K.D., REICHENBACH D.D., MARCOVINA S.M. et al., Apolipoproteins B, (a), and E accumulate in the morphologically early lesion of ‘degenerative’ valvular aortic stenosis. Arterioscler. Thromb. Vasc. Biol., 1996; 16:523–32. 15. RAJAMANNAN N.M., SUBRAMANIAM M., SPRINGETT M. et al., Atorvastatin inhibits hypercholesterolemia-induced cellular proliferation and bone matrix production in the rabbit aortic valve. Circulation, 2002; 105:2660–65. 16. WU B., ELMARIAH S., KAPLAN F.S. et al., Paradoxical effects of statins on aortic valve myofibroblasts and osteoblasts: implications for end-stage valvular heart disease. Arterioscler. Thromb. Vasc. Biol., 2005; 25:592–97. 17. OLSSON M., DALSGAARD C.J., HAEGERSTRAND A. et al., Accumulation of T lymphocytes and expression of interleukin2 receptors in nonrheumatic stenotic aortic valves. J. Am. Coll. Cardiol., 1994; 23:1162–1170. 18. KADEN J.J., DEMPFLE C.E., GROBHOLZ R. et al., Interleukin-1 beta promotes matrix metalloproteinase expression and cell proliferation in calcific aortic valve stenosis. Atherosclerosis, 2003; 170:205–211. 19. KADEN J.J., DEMPFLE C.E., GROBHOLZ R. et al., Inflammatory regulation of extracellular matrix remodeling in calcific aortic valve stenosis. Cardiovasc. Pathol., 2005; 14:80–87. 20. GALIS Z.S., SUKHOVA G.K., LARK M.W. et al., Increased expression of matrix metalloproteinases and matrix degrading activity in vulnerable regions of human atherosclerotic plaques. J. Clin. Invest., 1994; 94:2493–2503. 21. O’BRIEN K.D., SHAVELLE D.M., CAULFIELD M.T. et al., Association of Angiotensin-converting enzyme with low-density lipoprotein in aortic valvular lesions and in human plasma. Circulation, 2002; 106:2224–2230. 22. HELSKE S., LINDSTEDT K.A., LAINE M. et al., Induction of local angiotensin II-producing systems in stenotic aortic valves. J. Am. Coll. Cardiol., 2004; 44:1859–1866. 23. BAHLER R.C., DESSER D.R., FINKELHOR R.S. et al., Factors leading to progression of valvular aortic stenosis. Am. J. Cardiol., 1999; 84:1044–1048. 24. MOHLER E.R., III, CHAWLA M.K., CHANG A.W. et al., Identification and characterization of calcifying valve cells from human and canine aortic valves. J. Heart Valve Dis., 1999; 8:254–260. 25. ANDERSON H.C., Calcific diseases. A concept. Arch. Pathol. Lab. Med., 1983; 107:341–348. 26. O’BRIEN K.D., KUUSISTO J., REICHENBACH D.D. et al., Osteopontin is expressed in human aortic valvular lesions. Circulation, 1995; 92:2163–8. 27. PARHAMI F., MORROW A.D., BALUCAN J. et al., Lipid oxidation products have opposite effects on calcifying vascular cell and bone cell differentiation: a possible explanation for the paradox of arterial calcification in osteoporotic patients. Arterioscler. Thromb. Vasc. Biol., 1997; 17:680–7. 28. ANDERSON T, UEHATA A, GERHARTD M, et al., Close relation of endothelial function in the human coronary and peripheral circulations. J. Am. Coll. Cardiol., 1995; 26:1235–41. 29. ROSS A., Atherosclerosis: current understanding of mechanisms and future strategies in therapy. Transplant Proc., 1993; 25:2041–3. 30. POGGIANTI E., VENNERI L., CHUBUCHNY V. et al., Aortic valve sclerosis is associated with systemic endothelial dysfunction. J. Am. Coll. Cardiol., 2003; 41:136–41. 31. AGMON I., KHANDHERIA B.K., MEISSNER I. et al., Aortic valve sclerosis and aortic atherosclerosis: different manifestations of the same disease? J. Am. Coll. of Cardiol., 2001; 38(3):827–34. 32. MEISSNER I., WHISNANT J.P., KHANDHERIA B.K. et al., Prevalence of potential risk factors for stroke assessed by transesophageal echcardiography and carotid ultrasonography: the SPARC study. Mayo Clin. Proc., 1999; 74:862–9. 33. WEISENBERG D., SAHAR Y., SAHAR G. et al., Atherosclerosis of the aorta is common in patients with severe aortic stenosis: an intraoperative transesophageal echocardiographic study. J. Thorac. Cardiovasc. Surg., 2005; 130:29–32. 34. GOLAND S., TRENTO A., CZER L.S., Thoracic aortic arteriosclerosis in patients with degenerative aortic stenosis with and without coexisting coronary artery disease. Ann. Thorac. Surg., 2008; 85:113–119. 35. ZAHOR Z., CZABANOVA V., Experimental atherosclerosis of the heart valves in rats following a long-term atherogenic regimen. Atherosclerosis, 1977; 27:49–57. 36. SARPHIE T.G., Surface responses of aortic valve endothelia from diet-induced, hypercholesterolemic rabbits. Atherosclerosis, 1985; 54:283–99. 37. FAZIO S., SANAN D.A., LEE Y.L. et al., Susceptibility to diet-induced atherosclerosis in transgenic mice expressing a dysfunctional human apolipoprotein E. Arterioscler. Thromb. Vasc. Biol., 1994; 14:1873–9. 38. BARR D.P., ROTHBARD S., EDER H.A. et al., Atherosclerosis and aortic stenosis in hypercholesterolemic xanthomatosis. JAMA, 1954; 156:943–7. 39. STEWART B.F., SISCOVICK D., LIND B.K. et al., Clinical factors associated with calcific aortic valve disease: Cardiovascular Health Study. J. Am. Coll. Cardiol., 1997; 29:630–634. 40. ARONOW W.S., SCHWARTZ K.S., KOENIGSBERG M., Correlation of serum lipids, calcium, and phosphorus, diabetes mellitus and history of systemic hypertension with presence or absence of calcified or thickened aortic cusps or root in elderly patients. Am. J. Cardiol., 1987; 59:998–999. 328 Carmen Ginghină et al. 10 41. MOHLER E.R., SHERIDAN M.J., NICOLS R. et al., Development and progression of aortic valve stenosis: atherosclerosis risk factors—a causal relationship? A clinical morphologic study. Clin. Cardiol., 1991; 14:995–999. 42. LINDROOS M., KUPARI M., VALVANNE J. et al., Factors associated with calcific aortic valve degeneration in the elderly. Eur. Heart J., 1994; 15:865– 870. 43. BOON A., CHERIEX E., LODDER J., KESSELS F., Cardiac valve calcification: characteristics of patients with calcification of the mitral annulus or aortic valve. Heart, 1997; 78:472–472. 44. PELTIER M., TROJETTE F., SARANO M.E. et al., Relation between cardiovascular risk factors and nonrheumatic severe calcific aortic stenosis among patients with a three-cuspid aortic valve. Am. J. Cardiol., 2003; 91:97–99. 45. DEUTSCHER S., ROCKETTE H.E., KRISHNASWAMI V., Diabetes and hypercholesterolemia among patients with calcific aortic stenosis. J. Chronic Dis., 1984; 37:407–15. 46. HOAGLAND P.M., COOK F., FLATLEY M. et al., Case-control analysis of risk factors for presence f aortic stenosis in adults. Am. J. Cardiol., 1985; 55:744–7. 47. CHUI M.C., NEWBY D.E., PANARELLI M. et al., Association between calcific aortic disease and hypercholesterolemia: is there need for a randomised controlled trial of cholesterol-lowering therapy? Clin. Cardiol., 2002; 24:52–5. 48. KATZ R., WONG N.D., KRONMAL R. et al., Features of metabolic syndrome and diabetes mellitus as predictors of aortic valve calcification in the Multi-Ethnic Study of Atherosclerosis. Circulation, 2006; 113:2113–2119. 49. GUNDUZ H., AKDEMIR R., BINAK E. et al., Can serum lipids and CRP levels predict the “severity” of aortic valve stenosis? Acta Cardiol., 2003; 58:321–326. 50. AGMON I., KHANDHERIA B.K., TAJIK A.J. et al., Inflammation, infection, and aortic valve sclerosis: insights from the Olmsted County (Minnesota) population. Atherosclerosis, 2004; 174:337–342. 51. JEEVANANTHAM V., SINGH N., IZUORA K. et al., Correlation of high sensitivity C-reactive protein and calcific aortic valve disease. Mayo Clin. Proc., 2007; 82:171–174. 52. NOVARO G.M., ARONOW H.D., SABIK E.M. et al., Plasma homocysteine and calcific aortic valve disease. Heart, 2004; 90:802–803. 53. OTTO C., O’BRIEN K.D., Why is there discordance between calcific aortic stenosis and coronary artery disease? Heart, 2001; 85:601–2. 54. ORTLEPP J.R., HOFFMAN R., OHME F. et al., The vitamin D receptor genotype predisposes the development of calcific aortic valve stenosis. Heart, 2001; 85:635–8. 55. ROBERTS W.C., KO J.M., Frequency by decades of unicuspid, bicuspid, and tricuspid aortic valves in adults having isolated aortic valve replacement for aortic stenosis, with or without associated aortic regurgitation. Circulation, 2005; 111:920–925. 56. GARG V., MUTH A.N., RANSOM J.F. et al., Mutations in NOTCH1 cause aortic valve disease. Nature, 2005; 437:270–274. 57. MAHER E.R., PAZIANAS M., CURTIS J.R., Calcific aortic stenosis: a complication of chronic uraemia. Nephron, 1987; 47:119–122. 58. ROBERTS W.C., WALLER B.F., Effect of chronic hypercalcemia on the heart. Am. J. Med., 1981; 71:371–384. 59. STEFENELLI T., MAYR H., BERGLER-KLEIN J., GLOBITS S., WOLOSZCZUK W., NIEDERLE B., Primary hyperparathyroidism: incidence of cardiac abnormalities and partial reversibility after successful parathyroidectomy. Am. J. Med., 1993; 95: 197–202. 60. STEWART B.F., SISCOVICK D., LIND B.K., et al., Clinical factors associated with calcific aortic valve disease. Cardiovascular Health Study. J. Am. Coll. Cardiol., 1997; 29:630–634. 61. STRICKBERGER S.A., SCHULMAN S.P., HUTCHINS G.M., Association of Paget’s disease of bone with calcific aortic valve disease. Am. J. Med., 1987; 82:953–956. 62. MAHER E.R., YOUNG G., SMYTH-WALSH B., PUGH S., CURTIS J.R., Aortic and mitral valve calcification in patients with endstage renal disease. Lancet, 1987; 2:875–877. 63. FAGGIANO P., ANTONINI-CANTERIN P., ERLICHER A. et al., Progression of aortic valve sclerosis to aortic stenosis. Am. J. Cardiol., 2003; 91:99–101. 64. PETER M., HOFFMANN A., PARKER C. et al., Progression of aortic stenosis. Role of age and concomitant coronary artery disease. Chest, 1993; 103:1715–1719. 65. NASSIMIHA D., ARONOW W.S., AHN C. et al., Rate of progression of valvular aortic stenosis in patients > or = 60 years of age. Am. J. Cardiol., 2001; 87:807–809, A9. 66. NOVARO G.M., TIONG I.Y., PEARCE G.L. et al., Effect of HMG-CoA reductase inhibitors on the progression of calcific aortic stenosis. Circulation, 2001; 104:2205–2209. 67. ARONOW W.S., AHN C., KRONZON I. et al., Association of coronary risk factors and use of statins with progression of mild valvular aortic stenosis in older persons. Am. J. Cardiol., 2001; 88:693–695. 68. PALTA S., PAI A.M., GILL K.S. et al., New insights into the progression of aortic stenosis: implications for secondary prevention. Circulation, 2000; 101:2497–2502. 69. NGO M.V., GOTTDIENER J.S., FLETCHER R.D. et al., Smoking and obesity are associated with the progression of aortic stenosis. Am. J. Geriatr. Cardiol., 2001; 10:86–90. 70. ROSENHECK R., BINDER T., PORENTA G. et al., Predictors of outcome in severe, asymptomatic aortic stenosis. N. Engl. J. Med., 2000; 343:611–617. 71. PETER M., HOFFMAN A., PARKER C. et al., Progression of aortic stenosis: role of age and concomitant coronary artery disease. Chest, 1993; 6:1715–9. 11 Calcific aortic valve disease and aortic atherosclerosis 329 72. BAHLER R.C., DESSER D.R., FINKELHOR R.S. et al., Factors leading to progression of valvular aortic stenosis. Am. J. Cardiol., 1999; 84:1044–8. 73. PALA S., PAI A.M., GILL K.S. et al., New insights into the progression of aortic stenosis: implications for secondary prevention. Circulation, 2000; 101:2497–502. 74. FAGGIANO P., GHIZZONI G., SORGATO A. et al., Rate of progression of valvular aortic stenosis in adults. Am. J. Cardiol., 1992; 70:229–33. 75. CHANDRA H.R., GOLDSTEIN J.A., CHOUDHARY N. et al., Adverse outcome in aortic sclerosis is associated with coronary artery disease and inflammation. J. Am. Coll. Cardiol., 2004; 43:169–75. 76. CARABELLO B.A., Aortic sclerosis: a window to the coronary arteries? N. Engl. J. Med., 1999; 341:193–5. 77. NIGHTINGALE A.K., HOROWITZ J.D., Aortic sclerosis: not an innocent murmur but a marker of increased cardiovascular risk. Heart, 2005; 91:1389–93. 78. FREEMAN R.V., OTTO C.M., Spectrum of calcific aortic disease. Pathogenesis, disease progression, and treatment strategies. Circulation, 2005; 111:3316–3326. 79. WILMSHURST P.T., STEVENSON R.N., GRIFFITHS H. et al., A case-control investigation of the relation between hyperlipidaemia and calcific aortic valve stenosis. Heart, 1997; 78:475–9. 80. CHAN K.L., GHANI M., WOODEND K. et al., Case-controlled study to assess risk factors for aortic stenosis in congenitally bicuspid aortic valve. Am. J. Cardiol., 2001; 88:690–3. 81. ARONOW W.S., AHN C., KRONZON I. et al., Association between coronary risk factors and use of statins with progression of mild valvular aortic stenosis in older persons. Am. J. Cardiol., 2001; 88:693–5. 82. CHENEVARD R., BECHIR M., HURLIMANN D. et al., Persistent endothelial dysfunction in calcified aortic stenosis beyond valve replacement surgery. Heart, 2006; 92:1862–63. 83. HALCOX J.P.J., DEANFIELD J.E., Beyond the laboratory: clinical implications for statin pleiotropy. Circulation, 2004; 109(Suppl. II):II-42–II-48. 84. ROSENSON R.S., Statins in atherosclerosis: lipid-lowering agents with antioxidant capabilities. Atherosclerosis, 2004; 173:1–12. 85. TAKEMOTO M., LIAO J., Pleiotropic effects of 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitors. Arterioscler. Thromb. Vasc. Biol., 2001; 21:1712–1719. 86. KWAK B., MULHAUPT F., MYIT S., MACH F., Statins as a newly recognized type of immunomodulator. Nat. Med. 2000; 6:1399–1402. 87. RAJAMANNAN N.M., SUBRAMANIAM M., SPRINGETT M., SEBO T.C., NIEKRASZ M. et al., Atorvastatin inhibits hypercholesterolemia-induced cellular proliferation and bone matrix production in the rabbit aortic valve. Circulation, 2002; 105:2660–2665. 88. POHLE K., MAFFERT R., ROPERS D. et al., Progression of aortic valve calcification: association with coronary atherosclerosis and cardiovascular risk factors. Circulation, 2001; 104:1927–1932. 89. YILMAZ M.B., GURAY U., GURAY Y. et al., Lipid profile of patients with aortic stenosis might be predictive of rate of progression. Am. Heart J., 2004; 147:915–918. 90. BELLAMY M.F., PELLIKKA P.A., KLARICH K.W. et al., Association of cholesterol levels, hydroxymethylglutaryl coenzyme A reductase inhibitor treatment, and progression of aortic stenosis in community. J. Am. Coll. Cardiol., 2002; 40:1731–1734. 91. SHAVELLE D.M., TAKASU J., BUDOFF M.J. et al., HMG CoA reductase inhibitor (statin) and aortic valve calcium. Lancet, 2002; 359:1125–1126. 92. ROSENHEK R., RADER F., LOHO N. et al., Statins but not angiotensinconverting enzyme inhibitors delay progression of aortic stenosis. Circulation, 2004; 110:1291–1295. 93. MOURA L.M., RAMOS S.F., ZAMORANO J.L. et al., Rosuvastatin Affecting Aortic Valve Endothelium to Slow the Progression of Aortic Stenosis. J. Am. Coll. Cardiol., 2007; 49:554–561. 94. COWELL S.J., NEWBY D.E., PRESCOTT R.J. et al., Scottish Aortic Stenosis and Lipid Lowering Trial, Impact on Regression (SALTIRE) Investigators A randomized trial of intensive lipid-lowering therapy in calcific aortic stenosis. N. Engl. J. Med., 2005; 352:2389–2397. 95. ROSSEB A.B., PEDERSEN T.R., BOMAN K. et al., Intensive Lipid Lowering with Simvastatin and Ezetimibe in Aortic Stenosis. NEJM, 2008; 359:1343–56. 96. RAJAMANNAN N.M., OTTO C.M., Targeted therapy to prevent progression of calcific aortic stenosis. Circulation, 2004; 110:1180 –1182. 97. ANTONINI-CANTERIN F., HÎRŞU M., POPESCU B.A., LEIBALLI E., PIAZZA R. et al., Stage-related effect of statin treatment on the progression of aortic valve sclerosis and stenosis. Am. J. Cardiol., 2008 Sep. 15; 102(6):738–42. 98. ROUTLEDGE H.C., TOWNEND J.N., ACE inhibition in aortic stenosis: dangerous medicine or golden opportunity? J. Hum. Hypertens., 2001; 15:659–667. Received August 20, 2009 330 Carmen Ginghină et al. 12