Examination of the Cranial Nerves (I – XII) Dr. A. Cassim
advertisement

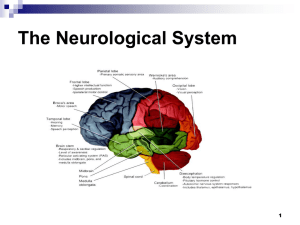
Examination of the Cranial Nerves (I – XII) Dr. A. Cassim Stations 1 & 2 At these stations there will be an S.P. and a Clinical teacher. Delivery Objectives: 1. Demonstrate with a clear commentary the examination of the Cranial Nerves. 2. Familiarise yourself with the clinical signs and symptoms of disorders of the cranial nerves that can be detected on your examination of a patient. Cranial Nerve examination forms part of the routine neurological examination. I. Olfactory Nerve Not routinely examined, but any disturbance of smell should be enquired about in the history. Before applying the test to the patient exclude possible obstruction of the nasal passages by occluding each nostril in turn and assessing if the patient is able to breathe in through the nose. • • • • • Patient should be asked to close his eyes Examiner applies a familiar odour eg. perfume or coffee to patient’s one nostril whilst closing off the other with his index finger. The patient is then asked to identify the odor. The procedure is then repeated with the other nostril. Each nostril is tested separately. Disorders of Smell can be due to disorders of the olfactory pathways at the level of: - olfactory receptors in nasal mucosa - neurons of the olfactory bulb - olfactory tract - uncus lesions (cause olfactory hallucinations, not anosmia) II. Optic Nerve This skill will be covered in detail in the Ophthalmology skill with Prof. Welsh Visual Acuity This is tested using Snellen’s Chart and ordinary newsprint. Snellen's chart is imprinted with block letters that line-by-line decrease in size, corresponding to the distance at which that line of letters is normally visible. Snellen’s Chart A N.B. If the patient wears corrective lenses he should be tested both with and without them Using Snellen’s Chart: • • • • • • The patient should be standing / seated 3 m from the chart. The patient’ is instructe to cover one eye with his hand whilst he is reads letters pointed to him on the chart up to the lowest line. If difficulty is experienced reading a selected line the patient is asked to attempt the one immediately above. The procedure is repeated for the opposite eye. Each eye is tested separately. The visual acuity is reported separately for each eye. Recording the visual acuity: Visual acuity is recorded as a fraction. The numerator indicates the distance (in metres) from the chart which the subject can read the line. The denominator indicates the distance at which a normal eye can read the line. Normal vision is 3/3. A pocket screener used at the bedside can be substituted for the Snellen’s chart. Pocket screener should be held at a distance of 30 cm. At this distance the letters are equivalent to those on Snellen's chart. Visual Fields This is tested by Confrontation Tests. • • • The patient is instructed to cover e.g. the right eye and look into the examiner’s left eye with the examiner’s right eye also covered. The examiner is seated / standing roughly at the same level as the patient and at an arm’s length away. Starting at the periphery of each quadrant of vision the examiner moves his finger or hat pin towards the centre of the patient’s vision. • The patient is asked to indicate as soon as he sees the finger or hatpin. • The test is repeated for the left eye. A red topped hat pin is used for testing the central area of vision and a white topped one for the peripheries). B The test reveals gross field defects only and needs to be confirmed by formal perimetry if a disturbance is found. Field defects may be due to disturbances in the visual pathways at any of the following levels: Lesion Optic nerve Optic chiasm Optic tract / lateral geniculate body Occipital lobe Field Defect Partial / complete blindness in affected eye Blindness in both temporal visual fields (bitemporal hemianopia) Blindness in contralateral half of both visual fields (hemianopia) Blindness in contralateral half of both visual fields (hemianopia) Ophthalmoscopy (fundoscopy) The patient’s fundus is examined and observations should include the state of: • • • • The The The The Optic Discs, vessels, macula and periphery of the retina Note: A short acting mydriatic such as mydriacil can be used to dilate the patient’s pupil. The patient should be warned that he will experience blurred vision for a period of time. Establish if the patient will need to drive back home if he has arrived alone before putting in the mydriatic drops. III, IV and VI Oculomotor, Trochlear and Abducens Nerves The action of these nerves is innervation of the eye muscles and they are therefore tested collectively as a unit. Nerve III also supplies fibres to constrict the pupil and to levator palpebrae superioris which elevates the eyelids. D Ocular Movements: • • • • • • The patient is asked to look straight ahead. The eyes are inspected for alignment (squint, skew deviation), pupillary size and symmetry, and ptosis. The examiner instructs the patient to follow his finger as he moves it The patient follows the movement of the examiner’s fingers without moving his head. The range of ocular movement is assessed in all directions of gaze. Observe for the presence of nystagmus and diplopia (double vision). Note: Brief horizontal nystagmus in the extremes of lateral gaze is normal. Pupillary Response To light: • • • The examination should be conducted in a darkened room. A light is shone into the patient’s eye and constriction of the pupil is observed in each eye. Assessment is made of the pupillary size and shape. Direct and consensual light reflexes are observed. To accommodation: • The patient begins by fixating on a distant object and then changes his focus to a close object. • Pupillary constriction is assessed and compared to the other eye. • Each eye is tested separately. Disturbances of nerve III result in: • • Ptosis of the lid An inability to look up, down or medially with the affected eye. The eye is deviated down and out. • Dilatation of the pupil (non reactive to light) Disturbances of nerve IV result in: • An inability to look downward, especially with the eye turned inwards. • The affected eye is deviated upward and outward causing vertical diplopia. • Compensary head tilt to the side contralateral to the VIth nerve palsy • Difficulty in reading and going downstairs Disturbances of nerve VI result in: • V An inability to look laterally with the affected eye, resulting in horizontal diplopia on lateral gaze to the affected side. Trigeminal Nerve This nerve innervates the skin of the face, muscles of mastication viz. the medial and lateral pterygoids, masseters and temporalis and supplies sensory fibres to the cornea. E Facial sensation • • • The patient’s eyes should be closed. Different modalities of sensation (light touch, pinprick and warm and cold objects) are assessed on the face in all 3 divisions of the trigeminal nerve. The patient reports each sensation as instructed. • The sides of the face are compared for sensation perception. Responses are reported as intact, increased or reduced Corneal Reflex • The patient’s cornea is gently touched with a wisp of cotton wool approaching from the side. • A blink reflex is observed for. Note: Avoid stroking only the sclera Muscles of mastication • • • • The masseters and temporalis muscles are observed for wasting and palpated with the jaw tightly clamped. The patient is instructed to bite down hard The patient then opens the mouth and symmetry of jaw opening is assessed. Any deviation is noted. In unilateral paralysis of the muscles of mastication the jaw deviates to the affected side on jaw opening. Jaw Jerk (Masseter reflex) • • VII Next, ask the patient to open the mouth and tap the examiner’s finger placed above the patient’s chin with a gentle downward strike of the reflex hammer. Observe for jaw contraction. Facial Nerve The facial nerve supplies motor fibres to the muscles of facial expression and taste sensation to the anterior part of the tongue. F • • • • The patient is instructed to imitate the examiner as he frowns, smiles and raises his eyebrows. Symmetry of facial expression is compared. Strength is tested (eye closure, lip closure) The patient is asked to shut his eyes tightly while you attempt to open them. • • • The patient is asked to puff up his cheeks as the examiner attempts to deflate the cheeks. Taste sensation is tested by having the patient identify sugar and salt placed on the anterior part of the tongue keeping the tongue protruded until the sensation of taste has been perceived. The patient should have sips of water between each test. Weakness of the muscles of the lower part of the face indicates an upper motor neurone lesion Weakness affecting the whole face implies a lower motor neurone lesion. VIII Vestibulocochlear / Acoustic Nerve G This examination with be covered in detail in the E.N.T. skills session. This nerve comprises 2 parts: the cochlear (hearing) and the vestibular nerves (balance) Vestibular nerve Not routinely tested and requires special equipment (caloric tests) If the patient gives a history of tinnitus or vertigo vestibular tests are indicated. Cochlear nerve The external auditory meatus should be inspected with an otoscope prior to performing the test to exclude any abnormalities. The ticking clock test • • • • • Establish the patient’s ability to perceive the sensation. Compare with your own to establish normality. The patient’s eyes should be closed. A ticking clock is placed a few inches away from the ear and moved further away until the patient can no longer hear it ticking. The test can also be conducted by starting well away from the ear and then slowly approaching the ear until the patient first perceives the sensation. Weber Test This lateralizes the hearing. • • • The base of the tuning fork is placed on top of the patient’s skull and held firmly in position The patient is asked where the sound is heard. The sound is normally heard in the centre/ middle If the Weber lateralizes to one ear it indicates either a sensorineural hearing loss in the contralteral ear or a conductive hearing loss in the same ear. Rinne Test Compares air conduction with bone conduction using a tuning fork. Normally air conduction is better than bone conduction. • The base of a vibrating tuning fork is placed on the mastoid process • The patient reports when he can no longer feel the vibration. • The vibrating tuning fork is then brought in front on the ear to assess if the patient can hear the sound H IX X Glossopharyngeal and Vagus Nerves These are normally tested together. I The patient’s voice is assessed for hoarseness and swallowing is observed. The Gag Reflex • The sides of the pharynx are stroked with a spatula and the patient’s ability to gag is assessed. The palatal reflex • • The patient can be instructed to say Ahh whilst the examiner observes the movement of the uvula and compares symmetry. The sensation of the uvula and pharynx is assessed with a spatula. J Symmetrical movement of the uvula, the absence of hoarseness and the ability to swallow indicates an intact Vagus nerve. Unilateral palsy causes deviation of soft palate and uvula to the sound side on saying ahh. The autonomic functions of the Vagus will not be covered here. XI Accessory Nerve The accessory nerve supplies motor fibres to the sternocleidomastoid and the trapezius muscles K • • • • The trapezius muscle is palpated for strength The patient is then asked to shrug the shoulders against resistance. The patient is asked to flex the neck against resistance Then the patient is asked to laterally rotate the head against resistance. Hypoglossal Nerve XII This nerve supplies motor fibres to the tongue. • • • • The patient is instructed to protrude the tongue Inspect for wasting and fasciculation. Any lateral deviation of the tongue is noted. The strength of the tongue is tested by instructing the patient to move it from side to side against resistance provided by a spatula or against the inner side of the cheek. • Unilateral paralysis causes tongue deviation to the affected side on tongue protrusion. L REFERENCES: 1. Essentials of the Neurological Examination, American Medical Association 2. The Precise Neurological Examination, University of New York Medical School, 3. Clinical Examination, Tally and O’Çonnor, Third edition. 4. Hutchinson’s Clinical Methods 5. Macleod’s Clinical Examination. Acknowledgements to the following sources for images used in this presentation: • B- Precise Neurological Exam, American Med. School • C- Mc Cleod’s Clinical Examination • D,E,F,G,I,K – American Medical Association, Essentials of the Neurological Examination • H,L &J– Univ. of California, ST. Diego EXAMINATION OF CEREBELLAR FUNCTION DR. R.M. Alexandrescu Station 3 At this station there is an S.P. and a Clinical teacher Station Objective: 1. Demonstrate with a clear commentary the examination of the Cerebellum 2. Revise the anatomy of the cerebellum The cerebellum is the large brain mass lying dorsal to the pons and medulla within the posterior fossa. The cerebellum controls balance and coordination of movement. It consists of two hemispheres (neocerebellum) united by a narrow middle part, the vermis (paleocerebellum). Between the vermis and each hemisphere lies the paravermis (intermediate zone). Phylogenetically, there are three components: the archicerebellum, palaeocerebellum and neocerebellum. 1. The Archicerebellum (flocculo – nodular lobe) receives its principal input from the vestibular nuclei (vestibulocerebellum) 2. Paleocerebellum (the cerebellar midline structures-vermis) receives projections from the spinal cord (spinocerebellum): - adjusts the tone and coordination of motor activity in order to maintain the equilibrium of rest and movement. E.g. to maintain a posture by standing without any support, change posture in walking, running, turning or bending 3. Neocerebellum (the cerebellar hemispheres) lies on a circuit incorporating the cerebral cortex and the pons. - reinforces the tonus and coordination of muscular activity when voluntary movements are performed. The fibers projecting in and out of the cerebellum pass through the superior, middle and inferior cerebellar peduncles. THE CEREBELLUM AND ITS CONNECTIONS The diagram shows the afferent spinal-cerebellar and ponto-cerebellar pathways and the efferent cerebellar pathways. Acknowledgements: (Essentials of the neurological examination. A.M.A) Acknowledgements: Clinical Examination. N J Tally & S O’Connor The features of cerebellar disease: - dysarthria nystagmus - dysdiadochokinesia ataxia (trunk and limbs) dysmetria intention tremor hypotonia vertigo titubation Dysathria: Difficulty with articulation In cerebellar dysathria, the pronunciation is difficult; the rhythm of speech is lost, with pauses then accelerates, becomes jerky, explosive and loud. Cerebellar dysarthria is described as scanning or staccato speech. Nystagmus: Usually jerky horizontal nystagmus with the fast phase towards the side of the lesion. and increased amplitude on gaze towards the side of the lesion. Dysdiadochokinesia: Inability to perform rapid alternating movements. Ataxia: Disorderly or uncoordinated movement. Patients do not present any instability of the trunk in the sitting position (only if there is a substantial disturbance of midline cerebellar structures) When walking, the patient will use a wide-base gait and shows caution when turning. and on walking. This is because most cerebellar fibers cross twice in the brain-stem, both on entry to, and exit from the cerebellum. Intention tremor: Side - to- side tremor on approaching a target. Vertigo: A subject sensation of movement Titubation: Head tremor A. Upper limbs: Coordination is evaluated by testing the patient’s ability to perform rapidly alternating (RAM) and point-to-point movements correctly (finger-nose-finger test): 1. Rapid alternating movements 2. Finger-nose-finger test 1. Rapid alternating movements (RAM): There are few tests for RAM: A. The patient should make rapidly alternating movements, such as patting his thighs with his palms and the backs of his hands, by pronating and supinating the hands. Once the patient understands this movement, tell him to repeat it rapidly for 10 seconds. Normally this is possible without difficulty. B. The patient should make RAM, by patting his thighs with the palmar surface of the hand in rapid succession. C. The patient must oppose each finger to the thumb in rapid succession. D. Ask the patient to place one palm facing upwards and then alternately hit the palm with the palmar and then dorsal aspects of the fingertips of the other hand as quickly as possible. Acknowledgements: Clinical Examination. Macleod’s. Tenth Edition. Note: Rapidly alternating movements are not only impaired in cerebellar disease but also in pyramidal and extrapyramidal disease. 2. Finger-nose test (testing for intention tremor) With the eyes open, the patient touches his nose with his index finger and then touches the examiner’s outstretched finger. This action is repeated with increasing rapidity. The examiner can change the position of his finger. This test is performed for each hand. Ask the patient to touch the tip of the nose (A) and the examiner’s finger (B). Move the finger from one position to another (C, D). Acknowledgements: Clinical Examination. Macleod’s. Tenth Edition. Past pointing / overshoot 1. Patient must track the rapid movements of the examiner’s index finger with his own. 2. While seated the patient is asked to rapidly elevate his extended arms to shoulder height. B. Lower limbs: Coordination: 1. Heel-shin test With the patient in supine position instruct the patient to place the right heel on the left knee Then ask the patient to slide the heel down the shin to the foot. Repeat the same movement going back to the starting position at the knee and down To the shin several times. The test is carried out with the other foot. A. Beginning of the test B. Normal result. The hell runs smoothly and straight down the skin. C. Abnormal result. The heel is ataxic and jerky with oscillations from side to side whilst sliding down the shin. 2. Toe-finger test: With the patient in supine position, ask the patient to lift the foot and touch the examiner’s finger with the big toe. Look for intention tremor. 3. Foot-tapping test: rapid alternating movements are tested by getting the patient to tap the sole of the foot on the ground. Each limb is tested individually. . Slowness in movements or inability to perform this task may indicate a cerebellar lesion, proprioception disturbation, or hemiparesis. Balance To achieve balance, 2 out of the 3 following inputs to the cortex must be intact: 1. Visual confirmation of position 2. Non-visual confirmation of position (proprioceptive and vestibular input). 3. A normally functioning cerebellum. The Romberg test: Acknowledgements: www.aafp.com This test evaluates mainly propioception. Functions (vermis). The patient should remove his footwear. Ask the patient to stand erect with heels together. Then compare the balance with the eyes open and then closed. The physician should remain near the patient to prevent injury in case the patient falls A normal person may sway slightly with the eyes closed. In cerebellar ataxia balance is poor with eyes opened or closed. In sensory ataxia the patient is steady with eyes opened and falls with eyes closed. A positive Romberg’s test (losing balance with closed eyes) indicates sensory ataxia. Gait is also controlled by the cerebellum and should always be included in the cerebellar testing. Gait is evaluated by having the patient walk across the room under observation. Observe the patient for the base of his stance and gait Cerebellar disease causes gait ataxia manifesting with a broad based and unsteady gait... When the vermis is involved, the patient widens his base and walks with difficulty. When the lesion is in the hemisphere you can see a tendency to fall to the same Side of the lesion Heel-toe walking test: The patient should remove his footwear. Ask the patient to walk heel-to-toe (tandem gait) This test evaluates the function of the vermal / midline cerebellar structures. Acknowledgements: www.aafp.com Observe the patient rising from the sitting position.for truncal ataxia. Note gross abnormalities. Acknowledgements: www.aafp.com Cerebellar Syndromes 1. Axial /vermal /midline cerebellar syndrome: truncal,gait, stance ataxia 2. Appendicular /hemispheric cerebellar syndrome: limb ataxia (ipsilateral to side of lesion) References: 1. Clinical Examination. A systematic Guide to Physical Diagnosis. N.J.Talley& Simon O’Connor.Fourth Edition. 2. Clinical Examination. Third Edition. Owen Epstein & all. 2003. 3. Clinically oriented anatomy. Keith L. Moore & Arthur F. Dailey. Fourth Edition. Deep Tendon & Superficial Reflexes Dr. A. Cassim Station 4 At this station there is an S.P. and a Clinical teacher Station Objectives: 1. Demonstrate with a clear commentary the examination of Superficial and Deep tendon Reflexes. 2. Recognise abnormal responses and be able to correlate it with the affected dermatomes. A somatic reflex arc is the simplest functional unit of the nervous system. A simple arrangement of elements permits a response to stimuli, where the final element in the chain is skeletal muscle. Acknowledgements: Dr. Thomas Caceci Reflexes have both sensory and motor components (afferent & efferent). In evaluating reflexes, the part of the body being tested should be relaxed and the stimuli applied with the same intensity on corresponding sites. Deep Tendon Reflexes (Monosynaptic reflex arc): Essential tips when using the patella hammer: • • • • • The patella hammer should be held nearer the end. The movement as the tendon is being struck with the hammer should be delivered from the wrist. The head of the hammer should be allowed to fall with gravity on the intended forefinger or muscle tendon An observation of the rapidity and strength of muscle contraction / jerk is observed. A comparison is made with the opposite side, Results are reported as: Normal / present Increased / brisk Decreased / absent, and graded out of 4. GRADING OF DEEP TENDON REFLEXES Grade Biceps • • • Interpretation 0 (0/4) Absent 1+ (1/4) Slight jerk or a palpable or visible muscle contraction 2+ (2/4) A moderate or average jerk 3+ (3/4) A very brisk jerk 4+ (4/4) Clonus Jerk (C5, C6) Forefinger of one hand is placed on the biceps tendon The biceps tendon is struck by the patella hammer. For the corresponding biceps tendon (furthest away from the examiner’s side) the thumb of the hand may be substituted for the forefinger. Brachioradialis (Supinator) Jerk (C5, C6) • The patient’s elbow is flexed and pronated. • The examiner places two fingers over the lower end of the patient’s radius just above the wrist. • The tendon of the brachioradialis is struck on examiner’s two fingers placed over this area. Triceps Jerk (C7, C8) • Examiner supports the wrist with one hand as the forearm is pronated and resting across the patient’s body • The triceps tendon is struck with the tendon hammer. Finger (flexor) Jerks (C8) Patients holds hand palm upwards, fingers slightly flexed and relaxed. Examiner places his hand over the patient’s and the hammer is struck over the former’s hand. Knee Jerk (L3, L4) Examiner slides his arms under the patient’s slightly flexed knees and supports them. The tendon hammer is struck over the infra patellar tendon. Ankle Jerk (S1, S2) Patient’s foot is held in mid position at the ankle, whilst the examiner bends the knee, externally rotates the hip and holds the foot dorsiflexed. The Archilles tendon is struck with the tendon hammer. Superficial Reflexes (Polysynaptic reflex arc): • • The patient’s skin is stroked with an object that is moderately sharp but should not injure the skin (e.g. with the end of the reflex hammer). The skin response is observed and compared to the opposite side. GRADING OF SUPERFICIAL REFLEXES Reflex tested Result Upper abdominal reflex Normal / Absent Lower abdominal reflex Normal / Absent Cremasteric reflex Normal / Absent Anal Reflex Normal /Absent Plantar Reflex Down going /up going Upper Abdominal • The examiner strokes the skin just above the patient’s umbilicus on either side using the object chosen for the examination. Lower Abdominal • The skin below the umbilicus is similarly stroked with an instrument. Cremasteric • Anal • The skin of the inner aspect of the thigh is stroked on both sides in a male patient with the instrument. Skin close to the anal canal is stroked on either side Plantar Reflex (Babinski) (L5, S1, S2) • • The patient’s foot should be dorsiflexed at 90 degrees to the ankle. The examiner strokes the lateral aspect of the patient’s sole with a blunt instrument such as a car key. • • He then curves the stroke inwards towards the M.T. P. joint before reaching the toes An observation is made of the response of the toes at the M.T.P. joint REFLEXES Reflex Normal Response Biceps Jerk Contraction of biceps with flexion of the forearm at the elbow followed by prompt relaxation Pertinent Central Nervous System Segment / Roots C5, C6 H Triceps Jerk Triceps contracts with elbow extension C7 I Brachioradial is Jerk Contraction of the brachioradialis with flexion of the elbow C5, C6 Finger Jerks Slight flexion of all fingers occurs C8 Knee Jerk Quadriceps contracts causing extension of the knee Ankle Jerk Plantar flexion of the foot L2, L3, L4 S1 Upper abdominal Umbilicus moves up and toward area being stroked T7 – T9 Lower Abdominal Umbilicus moves down T11, T12 Cremasteric Ipsilateral scrotal elevation T12, L1 Anal Skin tenses at the gluteal area Plantar Reflex (Babinski) Plantarflexion of the foes L4 – S3 Ss K REFERENCES: 1. Clinical Examination. Tally & O’Connor 2. Essentials of the Neurological Examination. The American Medical Association. 3. Veterinary Medicine. Dr. T. Caceci. Acknowledgements to the following sources for the images used in this presentation: H–K TEXAS A & M University