Diabetes Update 2015 - Virginia Pharmacists Association
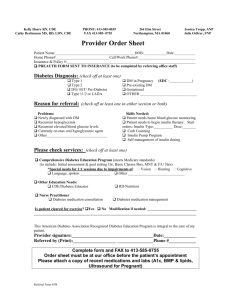
advertisement

7/23/2015 Financial Disclosures David Matthews has no relevant financial relationship(s) with any commercial interest(s) to disclose. Diabetes Update 2015 David E. Matthews, PharmD Assistant Professor Department of Pharmacy Practice Shenandoah University Bernard J. Dunn School of Pharmacy 1 Objectives 2 Objectives, Continued • Review the most recent recommendations for diabetes management according to the 2015 American Diabetes Association (ADA), including management of common comorbidities • Discuss the efficacy, safety, and place in therapy for newly‐approved non‐insulin anti‐ diabetic medications • Discuss recent developments in insulin therapy, including concentrated insulin products, biosimilar products, and novel routes of administration • Given a patient case, apply information related to recent developments in diabetes management to provide optimal care 3 Presentation Outline • • • • • 4 Patient Case Diabetes pathophysiology review Approach to therapy: 2015 ADA Guidelines Recent advances in non‐insulin therapies Recent advances in insulin therapies Patient case RS is a 54 year old white female who presents to your community pharmacy for a medication therapy management (MTM) visit. She is feeling well, but says she is disappointed that she has been unable to control her diabetes adequately. She was told by her physician at a recent visit that her A1c is 8.4%. 5 6 1 7/23/2015 Patient Case, Continued Patient Case, Continued PMH: T2DM, HTN SH: non‐smoker, EtOH 1‐2 times per week FH: Father died of MI at age 55, had DM Mother died of lung CA at age 78 Blood glucose log over past week: Date Pre‐breakfast (fasting) Bedtime (~2hr post‐dinner) BP today: 138/88, right arm, seated 7/19 7/20 156 168 251 Medication list: • Metformin 500 mg BID • Lisinopril 40 mg once daily • HCTZ 25 mg once daily • Januvia 100 mg once daily • Glipizide 10 mg BID 7/21 128 279 7/22 133 240 7/23 170 7/24 7/25 192 155 301 7 Patient Case, Continued 8 Patient Case: Questions RS has a prescription for a new medication today: • How would you assess RS’s current control of her diabetes? What are her goals? • What changes could you suggest making to RS’s physician after your MTM session? • Is the new prescription for RS appropriate? • Would any other new agents be appropriate? • What counseling points would be appropriate for RS? Bydureon pen 2mg, inject subQ once weekly 9 10 DM Pathophysiology DIABETES PATHOPHYSIOLOGY: REVIEW 11 12 2 7/23/2015 Diagnosis Glycemic Targets Any of the following: • A1c >6.5%* • Fasting blood glucose (FBG) >126 mg/dL* • 2hr post‐prandial BG >200 mg/dL following oral glucose tolerance test (OGTT)* • Random plasma glucose >200 in the presence of classic hyperglycemic symptoms • A1c <7% for most patients* • Fasting BG 80‐130 mg/dL* • Previously 70‐130 mg/dL • Peak post‐prandial BG <180 mg/dL* *All goals should be individualized *In the absence of unequivocal hyperglycemia, must be repeated for confirmation of diagnosis • Disease duration, life expectancy, comorbidities, risk of hypoglycemia, support system, etc. 13 14 Approach to Therapy: ADA2015 • Lifestyle modification for all • Metformin preferred initial therapy • If no contraindications or intolerance • Add second agent if needed after 3 months • Tailor to patient‐specific factors • Add third agent if needed after 3 months • Tailor to patient‐specific factors 15 16 Approach to Therapy: ADA2015 • Consider starting with dual therapy if A1c >9% • Consider starting with insulin if: • BG >300 • A1c >10% • Catabolic features present 17 18 Diabetes Care. 2015 Jan;38 Supp 1: S1‐S93 3 7/23/2015 Hypertension in DM Cardioprotection in DM • BP Goal for most diabetic patients 140/90 • Specific LDL target no longer recommended • Statins recommended for most diabetics • Change from 140/80 in 2014 Guidelines • Lower goals may be acceptable in some patients • ACE or ARB first line due to nephroprotection BP Goal JNC 8 ADA 2015 ADA 2014 ADA 2013 140/90 140/90 140/80 • Decrease risk of CV events • Choice of statin based on patient‐specific factors • Overt cardiovascular disease / CV risk factors • Age • Tolerability 130/80 19 20 Classification of Statins • Based on percentage of LDL lowering High Intensity (LDL lowering >50%) Moderate Intensity (LDL lowering 30‐50%) Low‐Intensity (LDL lowering <30%) Atorvastatin 40*‐80 mg Atorvastatin 10‐20 mg Pravastatin 10‐20 mg Rosuvastatin 20‐40 mg Rosuvastatin 10 mg Lovastatin 20 mg Simvastatin 20‐40 mg Pravastatin 40 mg Lovastatin 40 mg Diabetes Care. 2015 Jan;38 Supp 1: S1‐S93 22 21 Immunizations Pneumococcal Update • Pneumococcal polysaccharide vaccine (PPSV23) • Influenza annually for patients >6 mo. • Pneumococcal vaccination (PCV13 / PPSV23) • First dose >2yo • Second dose >65yo • Minimum 5 years between doses • See next slide • Hepatitis B series • Pneumococcal conjugate vaccine (PCV13) • Recommended for ages 19‐59 • Consider for age >60 • Now recommended for all adults >65yo • Adults >65yo should receive PCV13 first, then PPSV23 6‐12 months later • If already received PPSV23, give PCV13 12 months later 23 24 4 7/23/2015 Summary of Major Changes • Fasting blood glucose goal now 80‐130 mg/dL • (previously 70‐130 mg/dL) RECENT ADVANCES: NON‐INSULIN THERAPIES • BP goal now <140/90 • (previously <140/80) • Lipid goal now risk‐based similar to 2013 ACC/AHA guidelines • (previously targeted LDL levels) 25 26 Non‐Insulin Anti‐Diabetic Agents SGLT‐2s: Available Agents • Most recently approved therapies • • • • • SGLT‐2 inhibitors • GLP‐1 agonists • Daily or twice daily • Once weekly Canagliflozin (Invokana®) Dapagliflozin (Farxiga®) Empagliflozin (Jardiance®) Others under investigation www.invokana.com/ • DPP‐4 inhibitors https://www.farxiga.com/ 27 SGLT‐2 Inhibitors: MOA https://www.jardiance.com/ 28 SGLT‐2 Inhibitors: MOA • SGLT = sodium‐glucose transport protein • Expressed in kidney and promotes glucose reabsorption • SGLT‐2 is responsible for ~90% of glucose reabsorption in the kidney • Inhibition leads to increased glucose excretion in the urine 29 SGLT2 inhibitor SGLT2 inhibitor 30 5 7/23/2015 SGLT‐2 Inhibitors SGLT‐2s: “The Good” • Do not use in: • • • • • • Renal impairment • Patients predisposed to side effects (use caution) May decrease BP Weight loss Once daily PO Rarely cause hypoglycemia More potent than DPP‐4 Inhibitors • A1c lowering ~1% 31 SGLT‐2s: “The Bad” SGLT‐2s: Place in Therapy • Lack long‐term safety data • Increase LDL • Side effects • • • • 32 • Consider as add‐on therapy AFTER usual second‐line options • Patients who decline insulin who need additional oral therapy • Patients at low risk of side effects Urinary tract and genital yeast infections Hyperkalemia Hypotension Ketoacidosis? • Cost 33 GLP‐1 Agonists: Available Agents 34 The Incretin Effect • Agents given once or twice daily • Exenatide (Byetta®)—twice daily before meals • Liraglutide (Victoza®)—once daily • Agents given once weekly • Exenatide extended release (Bydureon®) • Albiglutide (Tanzeum®) • Dulaglutide (Trulicity®) https://www.trulicity.com/ https://www.byetta.com/ www.victoza.com/ https://bydureon.com/ 35 http://www.tanzeum.com/ http://www.medscape.org/viewarticle/702364 36 6 7/23/2015 GLP‐1 Agonists: MOA GLP‐1 Agonists • Mimics endogenous glucagon‐like peptide‐1 • Do not use in: • History of pancreatitis • History of thyroid carcinoma • Gastroparesis • Effect on BG: • Shortest acting agent (Byetta®) mostly post‐prandial • Weekly agents affect fasting AND post‐prandial readings 37 38 GLP‐1 Administration GLP‐1s: “The Good” • Byetta® and Victoza®: pen injector • • • • • Prime prior to first use only • Byetta® before meals; Victoza without regard to meals • Bydureon®: vial for reconstitution OR pen • Tanzeum® and Trulicity®: pen injector • Trulicity® pen requires no mixing Weight loss Relatively potent “Glucose‐dependent” action Synergistic with insulin 39 GLP‐1s: “The Bad” • • • • 40 GLP‐1s: Place in Therapy GI Upset Injection only Pancreatitis / thyroid tumors? Cost • Add‐on therapy to metformin • Patients within 1‐1.5% of A1c goal • In combination with insulin (unlabeled but common) • Patients who desire weight loss or have concerns regarding weight gain with insulin 41 42 7 7/23/2015 DPP‐4 Inhibitors: Available Agents • • • • • DPP‐4 Inhibitors: MOA Sitagliptin (Januvia®) Saxagliptin (Onglyza®) Linagliptin (Tradjenta®) Alogliptin (Nesina®) Combination products (with metformin, sulfonylureas etc.) www.januvia.com/ https://www.onglyza.com/ https://www.tradjenta.com/ • Dipeptidyl peptidase 4 (DPP‐4) is an enzyme that breaks down GLP‐1 • Inhibition of DPP‐4 increases levels of endogenous GLP‐1 by preventing breakdown • End result = enhanced incretin effect in response to a meal • Affects only post‐prandial BG www.nesina.com/ 43 44 DPP‐4 Inhibitors: MOA DPP‐4s: “The Good” • • • • Usually well tolerated Weight neutral Does not cause hypoglycemia Once daily PO 45 DPP‐4s: “The Bad” 46 DPP‐4s: Place in Therapy • Not very potent and only affects post‐prandial blood glucose • Heart failure? • Pancreatitis (rare) • Little to no effect on fasting BG • Cost 47 • Add‐on to be considered after metformin / possibly other oral agents • Patient with elevated post‐prandial readings who is otherwise near goal 48 8 7/23/2015 Developments in Insulin Therapy • Concentrated insulin • Insulin glargine U‐300 (Toujeo®) • Insulin lispro U‐200 (Humalog U‐200®) RECENT ADVANCES: INSULIN THERAPIES • Biosimilar products (on the horizon) • Inhaled insulin (Afrezza®) • Disposable insulin delivery systems (V‐Go®) 49 50 Insulin Glargine U‐300 (Toujeo®) Toujeo® vs. Lantus® • What it is: • Non‐inferior in terms of A1c reduction • No difference in overall hypoglycemic events • Significantly fewer episodes of nocturnal hypoglycemia • Patients on Toujeo® required 10‐17% more insulin to maintain glycemic control • Concentrated version of Lantus® that allows for small injection volume • Slower onset and longer duration than Lantus® • May cause less nocturnal hypoglycemia • What it IS NOT: • Substitute for Humulin U‐500 in patients requiring high dose insulin 51 52 Toujeo® Solostar® Pen Insulin Lispro U‐200 (Humalog®) • Administration similar to Lantus® Solostar® • 1 pen = 450 units • 1 box = 3 pens = 1350 units • • • • • Compared to 1500 units for Lantus® Solostar® 53 Approved late May 2015 Comes in Kwikpen® device (same as U‐100) 1 pen = 600 units Marketed by Eli Lilly as a method to reduce the need for frequently switching pens http://www.humalog.com/ 54 9 7/23/2015 Biosimilar Agents Biosimilar Pathway for Approval • January 2014: Eli Lilly’s application for glargine biosimilar blocked by Sanofi lawsuit • August 2014: FDA tentatively approves glargine biosimilar pending outcome of lawsuit • September 2014: EC approves glargine biosimilar in Europe • March 2015: FDA approves first biosimilar in US market (Zarxio®, biosimilar to filgrastim) • August‐September 2015: Anticipated launch of glargine biosimilar in Europe • Future: ?????? • Products derived from living organisms have interbatch variability no “generics” • FDA created pathway for approval of “biosimilar” agents • Biosimilar vs. interchangable 55 Inhaled Insulin (Afrezza®) 56 Afrezza® Inhaler • Inhaled insulin was previously available as Exubera® (Pfizer) but discontinued in 2007 • Concept reintroduced in 2015 by Sanofi under the name Afrezza® • Smaller inhaler with easier administration www.afrezza.com/ 57 Afrezza® Inhalation 58 Afrezza® Components Open inhaler and insert cartridge; keep level Lower mouthpiece to close inhaler Exhale completely Place mouthpiece in mouth, tilt inhaler down slightly toward chin • Inhale deeply, hold breath as long as comfortable before exhaling • • • • 59 • Each Rx comes with 2 inhalers • Each inhaler lasts 15 days • Each package = 3 foil packs • Each foil pack = 2 blister cards with 15 cartridges • Cartridges in groups of 3 per blister 60 10 7/23/2015 Afrezza® Storage • Unopened: refrigerate (cartridge should be at room temp for 10 min before use) • Opened foil pack • Good for 10 days at room temperature • Opened blister (group of 3 cartridges) • Good for 3 days at room temperature • Inhaler device • Good for 15 days http://www.healthline.com/diabetesmine/test‐driving‐new‐inhaled‐insulin‐afrezza 62 61 Afrezza®: “The Good” Afrezza®: “The Bad” • Option for patients who dislike multiple daily injections • Relatively easy administration compared to predecessor product • • • • Confusing storage requirements Must be dosed in 4 unit increments Cough common Possible decrease in lung function • Spirometry required at baseline, 6 months, then annually during therapy • Cost 63 Novel Delivery Devices 64 V‐Go® system • V‐Go® disposable insulin delivery system • “Patch pump” system replaced each day • Releases rapid acting insulin (lispro or aspart) at slow controlled “basal” rate • 20, 30, or 40 units/day • Ability to “bolus” increments of 2 units at mealtime • Maximum 36 bolus units per 24 hours • 1 click = 2 units http://www.go‐vgo.com/ 65 66 11 7/23/2015 V‐Go® System V‐Go® System • A new patch must be prepared each day • A new patch must be prepared each day http://www.go‐vgo.com/sites/default/files/upload/patient‐start‐guide.pdf http://www.go‐vgo.com/sites/default/files/upload/patient‐start‐guide.pdf 68 67 V‐Go® System: “The Good” V‐Go® System: “The Bad” • Option for patients who need prandial coverage but do not want or refuse to give multiple daily injections • Small and discreet • Patient’s insulin requirements must match system’s capabilities: • Basal rate limited to 20, 30, or 40 units/day • Bolus max of 36 units/day • Must prepare new patch each day, somewhat complicated • Cost 69 Patient Case 70 Patient Case, Continued RS is a 54 year old white female who presents to your community pharmacy for an MTM visit. She is feeling well, but says she is disappointed that she has been unable to control her diabetes adequately. She was told by her physician at a recent visit that her A1c is 8.4%. 71 PMH: T2DM, HTN SH: non‐smoker, EtOH 1‐2 times per week FH: Father died of MI at age 55, had DM Mother died of lung CA at age 78 BP today: 138/88, right arm, seated Medication list: • Metformin 500 mg BID • Lisinopril 40 mg once daily • HCTZ 25 mg once daily • Januvia 100 mg once daily • Glipizide 10 mg BID 72 12 7/23/2015 Patient Case, Continued Patient Case, Continued Blood glucose log over past week: Date Pre‐breakfast (fasting) Bedtime (~2hr post‐dinner) 7/19 7/20 156 168 251 7/21 128 279 7/22 133 240 7/23 170 7/24 7/25 192 155 RS has a prescription for a new medication today: Bydureon pen 2mg, inject subQ once weekly 301 73 74 Patient Case: Questions Thank You for Coming! • How would you assess RS’s current control of her diabetes? What are her goals? • What changes could you suggest making to RS’s physician after your MTM session? • Is the new prescription for RS appropriate? • Would any other new agents be appropriate? • What counseling points would be appropriate for RS? 75 • • • • • • • • • • • • • • • • • • • • • • Afrezza® [package insert]. Bridgewater, NJ: Sanofi; 2015. American Diabetes Association. Standards of medical care in diabetes—2015. Diabetes Care. 2015;38(suppl1):S1‐S93. Baruah MP, Kalra S.. The novel use of GLP‐1 analogue and insulin combination in type 2 diabetes mellitus. Recent Pat Endocr Metab Immune Drug Discov. 2012 May;6(2):129‐35. Bydureon® [package insert]. Wilmington, DE: AstraZeneca; 2015. Byetta® [package insert]. Wilmington, DE: AstraZeneca; 2015. Centers for Disease Control and Prevention PCV13 (Pneumococcal Conjugate Vaccine). Accessed July 22, 2015. Farxiga® [package insert]. Wilmington, DE: AstraZeneca; 2015. Humalog® [package insert]. Indianapolis, IN: Eli Lilly and Company; 2015. Invokana® [package insert]. Titusville, NJ: Janssen Pharmaceuticals; 2015. Januvia® [package insert]. Kenilworth, NJ: Merck and Company; 2015. Jardiance® [package insert]. Indianapolis, IN: Eli Lilly and Company; 2015. PL Detail‐Document, Comparison of Insulins and Injectable Diabetes Meds. Pharmacist’s Letter/Prescriber’s Letter. March 2015. Riddle MC, Yki‐Järvinen H, Bolli GB, Ziemen M, Muehlen‐Bartmer I, Cissokho S, Home PD. One‐year sustained glycaemic control and less hypoglycaemia with new insulin glargine 300 U/ml compared with 100 U/ml in people with type 2 diabetes using basal plus meal‐ time insulin: the EDITION 1 12‐month randomized trial, including 6‐month extension. Diabetes Obes Metab. 2015 Apr 2. Role of the Inhaled Insulin, Afrezza, for Diabetes. Pharmacist's Letter 2015; 31: SGLT2 Inhibitors (Flozins) and Risk of Ketoacidosis. Pharmacist's Letter 2015; 31(7):310704. Accessed July 22, 2015. Stone NJ, Robinson J, Lichtenstein AH, et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. Published online November 12, 2013. Tanzeum® [package insert]. Philadelphia, PA; GlaxoSmithKline; 2015. Toujeo® [package insert]. Indianapolis, IN: Eli Lilly and Company; 2015. Tradjenta® [package insert]. Indianapolis, IN: Eli Lilly and Company; 2015. Trulicity® [package insert]. Indianapolis, IN: Eli Lilly and Company; 2015. Victoza® [package insert]. Plainsboro, NJ: Novo Nordisk, Inc,; 2015. Winter A, Lintner M, Knezevich E. V‐Go Insulin Delivery System Versus Multiple Daily Insulin Injections for Patients With Uncontrolled Type 2 Diabetes Mellitus. J Diabetes Sci Technol. 2015 Apr 21. 76 Diabetes Update 2015 David E. Matthews, PharmD Assistant Professor Department of Pharmacy Practice Shenandoah University Bernard J. Dunn School of Pharmacy 77 13