Bone 33 (2003) 753–759
www.elsevier.com/locate/bone
Histomorphometric analysis of the effects of osteocyte density on
osteonal morphology and remodeling
Lionel N. Metz,a R. Bruce Martin,a,* and A. Simon Turnerb
a
Orthopaedic Research Laboratory, University of California, Davis Medical Center, Sacramento, CA, USA
b
Colorado State University, Fort Collins, CO, USA
Received 20 November 2002; revised 26 June 2003; accepted 30 June 2003
Abstract
Osteocytes, the most abundant cells in the cortical bone matrix, are thought to have mechanosensory and chemosensory regulatory roles.
Marotti theorized that osteocytes signal to osteoblasts to recruit them into the osteocyte lineage. Martin extended this theory, assuming that
osteocytes display a general inhibitory effect on osteoblast function. The current study provides a quantitative analysis of the relationships
between osteonal osteocyte density (Ot.N/BV), wall width (W.Wi), individual osteon porosity (IOP), and formation period (FP) in ulnar
cortices from sheep labeled with tetracycline and calcein double labels. We postulated that osteocytes inhibit refilling so that the osteon wall
width is thin enough, and the haversian canal is large enough, to allow adequate delivery of nutrients to the osteocytes throughout the
forming and completed osteon. Therefore we tested the hypotheses that Ot.N/BV correlates negatively to FP and W.Wi, and positively to
IOP, and that FP correlates positively with W.Wi. We found that Ot.N/BV correlated positively with IOP (P ⬍ 0.0001) and W.Wi correlated
positively with FP (P ⬍ 0.0001). Significant negative correlations were observed between Ot.N/BV and both W.Wi (P ⬍ 0.0001) and FP
(P ⫽ 0.006). These data support the general hypothesis that osteocytes contribute to the regulation of osteon morphology via the control
of refilling rate and formation period, and the specific hypotheses that, for a given cement line diameter, high osteocyte density (1) reduces
the rate of refilling and decreases the formation period and (2) decreases wall width and increases individual osteon porosity.
© 2003 Elsevier Inc. All rights reserved.
Keywords: Osteocyte; Osteon; Remodeling; Apposition rate; Inhibition
Introduction
Osteocytes are the most abundant cells in the cortical
bone matrix, and although there is limited knowledge of
their function in bone, theories exist about possible mechanosensory, chemosensory, and regulatory roles in bone
maintenance and remodeling [1– 6]. Osteocytes differentiate
from osteoblasts that become buried in osteoid during bone
formation. Marotti [7] theorized that an inhibitory signal
traveling through canalicular processes from osteocytes to
osteoblasts initiates recruitment of selected osteoblasts into
the osteocyte lineage. Martin [8] extended this theory to
* Corresponding author. Orthopaedic Research Laboratory, Research
Building I, UC Davis Medical Center, 4635 Second Avenue, Sacramento,
CA 95817. Fax: ⫹1-916-734-5750.
E-mail address: rbmartin@ucdavis.edu (R.B. Martin).
8756-3282/$ – see front matter © 2003 Elsevier Inc. All rights reserved.
doi:10.1016/S8756-3282(03)00245-X
explain the nonlinear refilling rate in secondary osteons as
the result of a more general inhibitory signal acting on the
entire population of osteoblasts at the refilling surface. He
hypothesized that the strength of the inhibitory signal perceived by each osteoblast is proportional to the number of
osteocytes in communication with it and inversely proportional to the distances involved. This hypothesis was found
to be consistent with the observed exponentially declining
apposition rate during the course of bone formation in a
newly forming osteon [9].
If osteocytes send signals that govern both the rate of
osteonal refilling and the recruitment of osteocytes to populate the new bone, this has important implications for the
control of both the remodeling process and the resulting
bone tissue structure. For example, greater initial osteocyte
density should reduce subsequent bone formation and increase the recruitment of osteoblasts into the osteocyte pop-
754
L.N. Metz et al. / Bone 33 (2003) 753–759
ulation, resulting in a higher osteocyte density in the completed osteon. The existence of this kind of positive
feedback loop could help insure that the bone matrix is
sufficiently filled with osteocytes to enable them to fulfill
their putative roles in strain and microdamage monitoring.
[1,10 –12].
If there is some critical level of the inhibitory signal at
which osteoblasts cease their function and either apoptose
or differentiate into osteocytes and bone lining cells, the
osteocyte population and its density should also determine
the duration of refilling and the thickness of the completed
osteonal wall. The latter is important because it affects the
distance that nutrients must travel from the haversian canal
to reach the outermost osteocytes after the osteon is complete. According to this hypothesis, formation period would
decrease in high osteocyte density osteons not because they
refill at a greater rate, but because high osteocyte density
halts refilling earlier. In these cases osteons having high
osteocyte density should have a larger haversian canal,
providing (a) room for a larger blood vessel to supply
nutrients to the increased number of osteocytes and (b) more
canal wall surface to support greater nutrient transport into
the adjacent bone tissue.
Thus, we propose that osteocyte density regulates the
osteon wall thickness and relative haversian canal space.
The force governing the change in wall thickness and relative haversian canal space is diminishing nutrient availability sensed by osteocytes, which causes them to send an
inhibitory signal to osteoblasts. With this theory in mind, we
studied osteocyte density in relationship to radial location in
the osteon and various remodeling parameters. We sought to
test the following hypotheses: (1) An osteon’s osteocyte
density is correlated negatively to its rate of refilling and
formation period, (2) an osteon’s osteocyte density is correlated negatively to its wall width and positively to its
relative haversian canal space, and (3) diminishments of
apposition rate and formation period are the means by
which osteocytes control access to nutrition through the
osteonal wall.
Materials and methods
Specimens
To study the effects of osteocyte density on osteonal
remodeling, we used middiaphyseal cross sections from
sheep ulnae. These were archival specimens from a study by
Turner et al. [13] on the skeletal effects of ovariectomy and
estrogen replacement therapy. There were four experimental groups: OVX, OVXE, OVX2E, and SHAM. The OVX,
OVXE, and OVX2E animals were surgically ovariectomized. The OVXE and OVX2E animals were then administered one and two estradiol implants, respectively. The
SHAM animals were sham ovariectomized. All the animals’
physical activity was controlled and they were similarly
housed so that these factors would not influence the results
[13].
Histomorphometry
We studied the right ulnae of 12 sheep (4 SHAM, 4
OVX, 2 OVXE, and 2 OVX2E) randomly selected from the
45 in Turner’s study. The sheep ulna is relatively small and
an entire midshaft cross section could be mounted on a
single (25 ⫻ 75 mm) microscope slide. Midshaft segments
of the bones were bulk stained in basic fuchsin using the
method of Burr and Stafford [14], dried, and embedded in
methyl methacrylate. Four sections, nominally 100 m
thick, were cut from each specimen and mounted on glass
slides.
During Turner’s study each sheep had been administered
double tetracycline labels 11 days apart and double calcein
green labels, again 11 days apart. The tetracycline and
calcein double labels were administered far enough apart so
that no osteon had both types of labels.
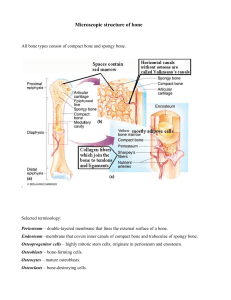
One section from each sheep was evaluated to determine
the osteocyte density and refilling data in 10 arbitrarily
selected double labeled osteons (Fig. 1). Each of the selected osteons had completed refilling as evidenced by the
absence of an osteoid seam. The diameters of the cement
line (Cm.Dm), the outer label (L1.Dm), the inner label
(L2.Dm), and the haversian canal (H.Dm) were measured
along two orthogonal directions and averaged in each selected osteon. L1.Dm, L2.Dm, and H.Dm measurements
were made at ⫻400 magnification, and Cm.Dm measurements were made at ⫻200 magnification, using an Olympus
eyepiece micrometer measuring graticule. Osteocyte lacunae were counted in three regions within each osteon: the
outer region, between the cement line and outer label; the
middle region, between the outer and inner labels; and the
inner region, between the inner label and the haversian
canal. When counting osteocytes the fine focus adjustment
was used to change the field of focus so that all lacunae
could be visualized in each osteon through the entire depth
of the section. Osteocytes were counted indirectly by counting lacunar footprints irrespective of their contents. Because
our intent was to understand the role of osteocytes in controlling osteoblasts during osteonal refilling, we were interested in the osteocyte density as it originally was in the
refilling and newly formed osteon. Therefore, assuming that
each osteocyte lacuna had originally contained a living cell
during osteon formation, we counted all lacunae regardless
of whether they contained evidence of a cell body. All
measurements were made by the same person (LNM).
Calculations
The radial measurements were converted to micrometers
using an Olympus 2 mm (0.01 mm increment) micrometer
slide as a length reference. Based on the work of Manson
L.N. Metz et al. / Bone 33 (2003) 753–759
755
Fig. 1. A magnified image (⫻400) of a double-labeled osteon under white light (left) and ultraviolet light (right).
and Waters [9] the refilling rate was assumed to decay
exponentially as refilling progressed to completion. Thus,
R 2 ⫽ R 1 ⫻ exp(⫺␣T L).
(1)
Here, R1 ⫽ L1.Dm/2 is the radius at the first label, R2 ⫽
L2.Dm/2 is the radius at the second label, TL is the time
between the labels (11 days), and the decay constant ␣
characterizes the change in the refilling rate over time.
Rearranging Eq. (1), ␣ (in days⫺1) was calculated for each
osteon as follows:
ln共R 2/R 1兲
␣⫽ ⫺
.
TL
共R 1 ⫺ R 2兲
.
TL
(2)
(3)
In principle MAR is linearly proportional to the unfilled
percentage of the osteon wall width, defined as follows:
%W.Wi.UF ⫽
R 1 ⫺ H.Rd
⫻ 100%,
Cm.Rd ⫺ H.Rd
ln
FP ⫽ ⫺
H.Rd
Cm.Rd
.
␣
(4)
where R1 is the radius of the outer label. Since MAR is zero
at R ⫽ H.Rd as opposed to R ⫽ 0, only % W.Wi.UF can be
used to normalize MAR accurately. Normalized mineral
apposition rate (MARN) was therefore calculated as MAR/
%W.Wi.UF.
(5)
Wall width was calculated as the difference between haversian canal and cement line radii as follows:
W.Wi ⫽ Cm.Rd ⫺ H.Rd.
The average mineral apposition rate between labels was
also calculated as
MAR ⫽
Based on an exponential refilling process the filling period (FP), in days, was calculated as
(6)
Individual osteon porosity was calculated as the percentage
of an osteon’s area occupied by the haversian canal as
follows:
IOP ⫽
冉
冊
H.Rd
Cm.Rd
2
⫻ 100%.
(7)
Finally, osteocyte density was calculated for each osteon,
taking into account both the osteon wall area, ⫻ (Cm.Rd2
⫺ H.Rd2), and section thickness, Sec.Th, to obtain osteocyte volumetric density,
Ot.N/BV ⫽
#osteocytes
⫻ 共Cm.Rd2 ⫺ H.Rd2兲 ⫻ Sec.Th
(8)
Osteocyte densities in the outer, middle, and inner regions
were also determined using similar equations.
756
L.N. Metz et al. / Bone 33 (2003) 753–759
Fig. 2. Mineral apposition rate is linearly proportional to the percentage of
unfilled wall width. Because MAR is zero when refilling is complete, the
regression line was forced through the origin.
Fig. 3. The radius of the second label is linearly proportional to the radius
of the first label. The slope of the line is significantly different from 1,
consistent with an exponentially decaying refilling rate.
Statistical analysis
However, wall width was also very significantly correlated
with osteocyte density, and negatively so (Fig. 5). The value
of R2 indicates that osteocyte density accounts for only
about 15% of the variability in wall width, but this is due to
the strong effect of cement line radius. Nevertheless, with P
⬍ 0.0001 for the influence of osteocyte density, we can
have high confidence in this additional effect.
Multiple-regression analysis showed that W.Wi was simultaneously related to cement line radius and osteocyte
density by the following equation:
ANOVA was used to determine whether the experimental groups OVX, OVXE, OVX2E, and SHAM showed significant differences for any of the measured or calculated
parameters. Then, regression analysis was performed to
study the relationships between the various osteocyte density and osteonal parameters. To test the hypotheses concerning osteocytes controlling osteoblast refilling, we correlated osteocyte density with individual osteon porosity,
wall width, normalized mineral apposition rate, and formation period. The criterion for statistical significance was P ⬍
0.05 and variability was expressed as the standard deviation.
Results
Three sections contained only 9 osteons suitable for
evaluation. Consequently, 117 osteons were evaluated in the
12 sections. Osteocyte density varied widely in these osteons, ranging from 6,158 to 59,940 mm⫺3 (mean 24,940 ⫾
10,420 mm⫺3). Linear regression showed that osteocyte
density was not affected by section thickness (P ⫽ 0.2936;
R2 ⫽ 0.010). Neither ovariectomy nor estrogen implantation
had a significant effect on osteocyte density or any other
histomorphometric parameters, so all 12 sections were
grouped for the remaining analysis.
The assumption that MAR is linearly proportional to
%W.Wi.UF was confirmed (Fig. 2). The plot of the label
radii, R2 vs. R1, showed a linear relationship with a slope
significantly different from 1 (P ⬍ 0.0001) (Fig. 3). This
finding fits Manson and Waters [9] description of an exponentially decaying refilling process, confirming the basis for
subsequent remodeling calculations in this paper.
Cement line radii varied greatly (range ⫽ 44 –132 m),
and this was the dominant factor governing wall width
because the range of Haversian canal radii was only 17 m
(i.e., 4 –21 m). Indeed, cement line radius accounted for
96.6% of the variability in osteonal wall width (Fig. 4).
W.Wi ⫽ ⫺1.30 ⫹ 0.885 Cm.Rd ⫺ 8.98
⫻ 10 4 Ot.N/BV,
with P ⬍ 0.0001 and R2 ⫽ 0.969. The fact that Cm.Rd
and Ot.N/BV together account for little more of the
variability in W.Wi than Cm.Rd alone indicated that
Ot.N/BV was also correlated with Cm.Rd. This was the
case, and although the correlation was again relatively
weak, its statistical significance was high: R2 ⫽ 0.119,
P ⫽ 0.0001, y ⫽ 4.15 ⫻ 10 ⫺5 ⫺ 2.08 ⫻ 10 ⫺7x.
Individual osteon porosity (IOP) was positively correlated with osteocyte density (R2 ⫽ 0.142; P ⬍ 0.0001;
y ⫽ 1.41 ⫹ 5.64 ⫻ 10 ⫺5x). IOP varied from 0.4 to
Fig. 4. Wall width is positively correlated with cement line radius.
L.N. Metz et al. / Bone 33 (2003) 753–759
757
Fig. 5. Wall width is negatively correlated with osteocyte density (On.N/
BV).
Fig. 7. Normalized apposition rate (MARN) is negatively correlated with
osteocyte density (On.N/BV).
9.8% of osteon area (mean 2.8% ⫾ 1.6%), and IOP also
correlated negatively with wall width (P ⬍ 0.0001;
R 2 ⫽ 0.276; y ⫽ 6.26 ⫺ 5.15 ⫻ 10 ⫺2x), as one
would expect.
Formation period (FP) ranged from 34 to 109 days, with
an average of 65 days. FP was positively correlated with
wall width (Fig. 6) and cement line radius (P ⬍ 0.0001; R2
⫽ 0.159; y ⫽ 34.2 ⫹ 0.379x). This was to be expected
because W.Wi and Cm.Rd entered into the calculation of FP
[Eq. (5)]. However, FP also exhibited a weak (R2 ⫽ 0.0637)
but quite significant (P ⫽ 0.0060) negative correlation with
osteocyte density (y ⫽ 74.3 ⫺ 3.98 ⫻ 10⫺4x). In addition,
IOP correlated negatively with FP (P ⬍ 0.0001; R2 ⫽
0.353; y ⫽ 6.44 ⫺ 5.63 ⫻ 10⫺2 x).
Because apposition rate declines as refilling proceeds,
MAR correlated positively with the percentage of the osteon
wall that was unfilled (%W.Wi.UF; Fig. 2). We therefore
divided MAR by %W.Wi.UF to obtain a normalized apposition rate, MARN, that was corrected for variations in the
completeness of refilling when the osteon was labeled.
MARN was negatively correlated with osteocyte density
(Fig. 7) and positively correlated with W.Wi (P ⬍ 0.0001;
R2 ⫽ 0.367; y ⫽ 29.7 ⫹ 1.62 ⫻ 103x).
Discussion
Fig. 6. Wall width is positively correlated with formation period.
Osteocytes were postulated to control osteoblast function
by means of an inhibitory signal that is proportional to
osteocyte density within the osteon. Pursuing this concept,
we tested the hypothesis that osteocytes regulate the rate
and duration of bone formation in the osteon wall, thus
decreasing W.Wi and increasing IOP, to help control their
subsequent access to nutrients from the haversian canal. We
found relationships between osteocyte density and formation period, mineral apposition rate, wall width, and individual osteon porosity that support the proposed hypotheses
and provide additional evidence for the effects of the inhibitory signal postulated in previous studies [7,8,11].
Several limitations and assumptions influenced the current study. Only those osteocytes within refilling secondary
osteons were assumed to affect their refilling because dendritic processes to osteocytes outside of the cement line are
presumably severed during resorption cavity and cement
line formation, thus diminishing signal travel into the osteon
from interstitial bone [15]. We calculated a volumetric density because the sections were relatively thick (83 to 133
m) and osteocytes (diameter ⬃8 m) lay at different
depths in the section. Changing the field of focus ensured
that all osteocyte lacunae were counted in each osteon’s
section regardless of their depth; calculating volumetric
osteocyte density eliminated errors due to variations in
section thickness or opacity. Although osteocyte lacunae
that were partially in the section were also counted, we
believe that this limitation did not seriously influence our
results because section thickness correlated nonsignificantly
with osteocyte density.
Our mean osteocyte volumetric density for sheep is
somewhat higher than, but not significantly different from,
values reported for human cortical bone (13,900 –19,400
mm⫺3) [16] and cancellous bone (13,000 mm⫺3) [17].
Other reports give osteocyte lacunar density per square
millimeter of section. Converting these values to volumetric
density by dividing by section thickness (realizing that this
may not be accurate), we obtained estimates of 18,000 –
758
L.N. Metz et al. / Bone 33 (2003) 753–759
Fig. 8. If high osteocyte density reduces the average value of MAR during
refilling and decreases the filling period (FP), the result is a larger haversian
canal and thinner wall width.
23,000 mm⫺3 for mouse ulnae, 46,400 mm⫺3 for women of
various ages, and 70,000 mm⫺3 for elderly women [4,18].
Osteocyte density apparently varies considerably among
bones and individuals as well as among osteons.
Clearly, there are many factors that effect osteon morphology. Certainly one of the dominant variables is cement
line radius, which is dictated by osteoclast activity. In this
study we accounted for the effect of variations in cement
line radius to demonstrate that osteonal wall width is inversely related to osteocyte density. The effects of osteocyte
density on the osteon refilling rate were demonstrated despite the influence of cement line radius and refilling completeness at the time of labeling. In concert with this, we
found that the formation period was shorter and individual
osteon porosity was greater in osteons with high osteocyte
density. These results support the hypothesis that osteocytes
inhibit refilling.
We postulated that osteoblasts cease matrix production
by differentiating into osteocytes or bone lining cells, or by
apoptosing, when a threshold inhibitory signal is received.
Our data suggest that, other things being equal, a threshold
signal is perceived sooner in osteons of high osteocyte
density, thus shortening FP. FP correlates positively with
wall width and negatively with individual osteon porosity,
suggesting that FP modulation by osteocytes further affects
the morphology of the osteons. A low correlation coefficient
between FP and osteocyte density alone is expected because
the FP is strongly affected by the size of the osteon. However, the statistical significance of the correlation (P ⬍
0.0001) strongly supports the hypothesized influence of
osteocyte density.
The mineral apposition rate was shown to decrease as
refilling progressed toward completion, as observed by others [9]. Thus, MAR was proportional to the percentage of
the wall width that was unfilled (%W.Wi.UF). When MAR
was normalized by the %W.Wi.UF, the resulting parameter
MARN was negatively correlated with osteocyte density. In
this case, as well, the explanatory effect of osteocyte density
was relatively small (⬃12%), but the level of statistical
confidence was high (P ⫽ 0.0001). Thus, other factors are
implicated in the control of MARN, but the probability
seems high that osteocyte density plays a role. Taken to-
gether, the results suggest that the apposition rate diminishes more rapidly in high-osteocyte-density osteons, and
the more rapidly diminishing MAR leads to a shorter formation period and subsequent narrower wall width (Fig. 8).
Concerning osteocytes’ self-regulating nutrient availability, the word nutrient could refer to one or more molecules
that are needed or sensed by the osteocytes in the bone
matrix. These could include hormones, ions, peptides, carbohydrates, or other signaling biomolecules. The inhibitory
signal referred to in this article may also involve such
molecules, or it may be electrical in nature [19].
Wall width and individual osteon porosity are obviously
inversely related parameters as indicated by their strong
negative correlation. However, whereas individual osteon
porosity affects the nutrient flow to the osteon, the wall
width affects nutrient level decays as nutrient molecules
travel farther from the haversian canal wall [20]. We propose two mechanisms to explain the observed effects of
osteocyte density on osteonal refilling. Both models assume
a condition of unidirectional nutrient transfer from the haversian canal into the osteon wall. That is, they assume that
the cement line, formed after resorption, becomes a barrier
to nutrients, so that all osteocytes within an osteon must
receive nutrients from the haversian canal [15].
The first mechanism involves transport within the osteon
wall. Those osteocytes in the outermost region of the refilling osteon receive the least nutrients due to depletion by
inner osteocytes and the effect of distance (Fig. 9). This type
of nutrient gradient was demonstrated by Qin et al. [15] for
large protein molecules (⬃400 kDa) and by Knothe Tate et
al. [21] for Procion Red, a smaller molecule (⬃400 Da),
approximately the size of nutrients such as vitamins D and
E. An exceptionally thick osteon wall would create a condition in which the outermost osteocytes become “starved.”
To avoid starvation by being buried too deeply in the osteon
wall during refilling, the outer osteocytes signal to the osteoblasts on the remodeling surface to slow or cease pro-
Fig. 9. The left side demonstrates a segment of an osteon with low
osteocyte density where the nutrient level from the haversian canal is
sufficient throughout the osteonal wall; consequently, the inhibitory signal
is weak. The right side demonstrates an osteon with high osteocyte density,
where the nutrient level is inadequate at the outer osteocytes, producing a
strong inhibitory response.
L.N. Metz et al. / Bone 33 (2003) 753–759
duction of the osteoid matrix. In a high-osteocyte-density
osteon the nutrients would be depleted by inner osteocytes
to a greater degree, causing the outermost osteocytes to send
a threshold-level inhibitory signal to the osteoblasts to stop
earlier in the refilling process. Furthermore, in such osteons,
the inhibitory signal would be stronger if signal strength is
proportional to osteocyte density [8].
The second mechanism involves haversian canal transport. Both nutrient flow through the blood vessel and transport out of the vessel and across the haversian canal surface
(i.e., the nutrient transport surface) must be adequate to
support nutrient transfer to all osteocytes. We have found no
data on haversian capillary dimensions relative to canal size.
However, inhibitory osteocyte signals could provide a
larger haversian canal, allowing a larger blood vessel, resulting in both a greater blood flow and greater surface area
for nutrient transport into the osteon. If the radius of the
haversian canal doubles, the nutrient transfer surface also
doubles, and the flow rate through the blood vessel increases
substantially more (by a factor of 16, to the extent that
Poiseuille’s Law applies).
The data presented here support the theory that osteocytes have an important role in the regulation of osteonal
refilling and haversian canal diameter. Clearly, other factors
(such as cement line radius) play very important roles in
governing osteonal morphology. However, the strong statistical significance of the correlations between osteocyte
density and osteon dimensions supports the existence of the
hypothesized inhibitory signal and its effect on osteoblast
function. If this mechanism has evolved such that osteocytes
will sacrifice bone mass by increasing haversian canal area
to protect their survival in new bone, the implication is that
osteocyte vitality and function are essential for other reasons as well, such as their putative mechanosensory and
chemosensory functions.
Acknowledgments
This work was supported by the Biological Undergraduate Scholars Program (L.N.M.) and the Doris Linn Chair of
Bone Biology (R.B.M.), at the University of California,
Davis.
References
[1] Burger EH, Klein-Nulend J. Mechanotransduction in bone-role of the
lacuno-canalicular network. Faseb J 1999;13(Suppl):S101–12.
759
[2] Mullender MG, Huiskes R, Versleyen H, Buma P. Osteocyte density
and histomorphometric parameters in cancellous bone of the proximal
femur in five mammalian species. J Orthop Res 1996;14:972–9.
[3] Mullender MG, van der Meer DD, Huiskes R, Lips P. Osteocyte
density changes in aging and osteoporosis. Bone 1996;18:109 –13.
[4] Power J, Loveridge N, Rushton N, Parker M, Reeve J. Osteocyte
density in aging subjects is enhanced in bone adjacent to remodeling
haversian systems. Bone 2002;30:859 – 65.
[5] Weinstein RS, Nicholas RW, Manolagas SC. Apoptosis of osteocytes
in glucocorticoid-induced osteonecrosis of the hip. J Clin Endocrinol
Metab 2000;85:2907–12.
[6] Yeni YN, Vashishth D, Fyhrie DP. Estimation of bone matrix apparent stiffness variation caused by osteocyte lacunar size and density.
J Biomech Eng 2001;123:10 –7.
[7] Marotti GI, Ferritti M, Remaggi F, Palumbo C. Quantitative evaluation on osteocyte canalicular density in human secondary osteons.
Bone 1995;16:125– 8.
[8] Martin RB. Does osteocyte formation cause the nonlinear refilling of
osteons? Bone 2000;26:71– 8.
[9] Manson JD, Waters NE. Observations on the rate of maturation of the
cat osteon. J Anat London 1965;99:539 – 49.
[10] Cowin SC, Weinbaum S, Zeng Y. A case for bone canaliculi as the
anatomical site of strain generated potentials. J Biomech 1995;28:
1281–97.
[11] Martin RB. Toward a unifying theory of bone remodeling. Bone
2000;26:1– 6.
[12] Weinbaum S, Cowin SC, Zeng Y. A model for the excitation of
osteocytes by mechanical loading-induced bone fluid shear stresses.
J Biomech 1994;27:339 – 60.
[13] Turner AS, Mallinckdrodt CH, Alvis MR, Bryant HU. Dose–response
effects of estradiol implants on bone mineral density in ovariectomized ewes. Bone 1995;17:421S– 427S.
[14] Burr DB, Stafford T. Validity of the bulk-staining technique to
separate artifactual from in vivo bone microdamage. Clin Orthopaed
Relat Res 1990;260:305– 8.
[15] Qin L, Mak AT, Cheng CW, Hung LK, Chan KM. Histomorphological study on pattern of fluid movement in cortical bone in goats. Anat
Rec 1999;255:380 –7.
[16] Sissons HA, O’Connor P. Quantitative histology of osteocyte lacunae
in normal human cortical bone. Calcif Tissue Res 1977;22(Suppl):
530 –3.
[17] Hobdell MH, Howe CE. Variation in bone matrix volume associated
with osteocyte lucunae in mammalian and reptilian bone. Isr J Med
Sci 1971;7:492–3.
[18] Power J, Noble BS, Loveridge N, Bell KL, Rushton N, Reeve J.
Osteocyte lacunar occupancy in the femoral neck cortex: an association with cortical remodeling in hip fracture cases and controls.
Calcif Tissue Int 2001;69:13–9.
[19] Zhang D, Cowin SC, Weinbaum S. Electrical signal transmission and
gap junction regulation in a bone cell network: a cable model for an
osteon. Ann Biomed Eng 1997;25:357–74.
[20] Wang L, Cowin SC, Weinbaum S, Fritton SP. Modeling tracer transport in an osteon under cyclic loading. Ann Biomed Eng 2000;28:
1200 –9.
[21] Tate ML, Niederer P, Knothe U. In vivo tracer transport through the
lacunocanalicular system of rat bone in an environment devoid of
mechanical loading. Bone 1998;22:107–17.