Peripheral Auditory System
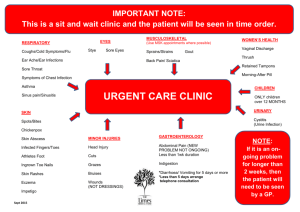
advertisement

Auditory Science Peripheral Auditory System Karolina Kluk karolina.kluk@manchester.ac.uk Coronal section http://www.cartage.org.lb/ Horizontal section Sagittal section http://www.cartage.org.lb/ 1 Auditory System Central Auditory System Peripheral Auditory System • outer ear • middle ear Peripheral Auditory System • cochlea • auditory nerve Outer ear How the Ear Works Inner ear Middle ear How the Ear Works Sound waves enter the ear canal and cause the eardrum to vibrate. These vibrations are carried by three tiny bones, the malleus, incus, and stapes, to the cochlea. The cochlea is a thin tube filled with fluid that is curled up into a spiral. In the cochlea, acoustic vibrations are transduced into electrical neural impulses. 2 How the Ear Works Running the length of the cochlea is the basilar membrane. Each place on the membrane is tuned to a particular frequency: How the Ear Works The sensory cells in the ear, the hair cells, are arranged in rows along the length of the basilar membrane: Outer Hair Cells Inner Hair Cell 3 Central auditory system: • Cochlear Nucleus • Superior Olivary Complex • Lateral Lemniscus • Inferior Colliculus • Medial Geniculate Body • Auditory Cortex FROM AIR TO EAR – OUTER EAR Composed of elastic fibro-cartilage Peripheral Auditory System • outer ear • middle ear • cochlea • auditory nerve Outer ear Inner ear Middle ear PINNA (Auricle) Composed of elastic fibro-cartilage 4 S shaped Functions of the Pinna The pinna collects sound energy and funnels the energy into the ear canal. The pinna modifies sound entering ear depending on direction, resolving ambiguities and providing cues to source elevation: 15° Elevation Ear Canal (External Auditory Meatus) Bony external auditory meatus Cartilaginous external auditory meatus -15° Elevation 15° 10 dB! Surrounded by bone, extremely thin skin, hairless, very sensitive -15° 3 4 5 6 7 8 9 10 Frequency (kHz) Functions of the Ear Canal The ear canal protects the tympanic membrane (eardrum). The sticky nature of earwax helps to prevent dust and foreign objects penetrating the ear canal. The ear canal acts as a resonator (like an organ pipe), amplifying frequencies in the region of 3000-4000 Hz. Surrounded by cartilage, thick skin, hair and earwax glands Ear Canal Resonance RESONANCE is the tendency of a system to oscillate at larger amplitude at some frequencies than at others 5 Ear Canal Resonance V f 0 = sound 4 Ltube Total Canal Pinna Vsound = 344 m/s EAM length = 2.5 – 3 cm Wavelengths at resonance = 10 – 12 cm 2.5 kHz 5.5 kHz 3 kHz Resonance frequency = 3500 – 4000 Hz Natural resonances of ear canal not heard – subject has grown up with them! Sandlin (2000) Hearing Aid Amplification, Chapter 12 Hearing aid resonances and changed ear-canal acoustics combine Sandlin (2000) Hearing Aid Amplification, Chapter 12 6 Babies! • As well as a higher resonant frequency due to the shorter canal, babies also have a smaller canal volume. • This means that for a given sound source, the intensity is higher in the baby s ear than in an adult s. • Thus, fitting a baby s hearing aid needs to take this into account – see hearing aids lectures & their discussions on RECDs Baby s ear-canal is smaller (shorter) than adult s – resonant frequency is higher Modified from: Sandlin (2000) Hearing Aid Amplification, Chapter 12 Directional Effects – head and torso Cues for localization diffraction 1. Interaural Time Difference (ITD) direc t reflection 2. Interaural Level Difference (ILD) Owing to the physical nature of sounds, ITDs and ILDs are not equally effective at all frequencies. 7 Outer ear – summary: Outer ear & localisation • See later lecture: – Differences between time of arrival at the two ears – interaural time difference (ITD – effective cue at low frequencies) – Differences in interaural level (ILD) – effective cue at high frequencies – Monaural cues (different reflections from pinna depending on direction of source) – high frequency cue for location in vertical plane Peripheral Auditory System 1. The outer ear consists of pinna and the ear canal. 2. The skin of the ear canal is innervated by four cranial nerves 3. Functions of the outer ear are: • protection of tympanic membrane • acoustic transmission path to the tympanic membrane • sound collection • acoustic amplification by resonance • sound localization 4. Interaural Time Difference (ITD) is useful for sound localization at low frequencies, Interaural Level Difference (ILD) is useful at high frequencies. The Middle Ear malleus incus stapes Composed of: • Air spaces • outer ear • Tympanic membrane • middle ear • cochlea • auditory nerve Outer ear Inner ear Middle ear c ni e pa ran m b ty em m e ow ub t d in an w hi d c a un st ro u E • Auditory ossicles • Middle ear muscles 8 Tympanic Membrane Tympanic Membrane The tympanic membrane (TM) has three layers: 1. An outer layer of very thin skin, continuous with that of the external ear canal; 2. A middle layer of radially and concentrically arranged connective tissue fibres; 3. An inner layer, a single layer of cells, continuous with the lining of the middle ear cavity. Posterosuperior Pars flaccida quadrant Posteroinferior quadrant AnteriorParssuperior tensa quadrant Anteriorinferior quadrant The TM is shaped like a blunt cone, with the apex (umbo) extending toward the middle ear space. The connective tissue layer makes the TM a stiff structure (pars tensa), the posteriosuperior quadrant with very little connective tissue is less stiff (pars flaccida). Otoscopic appearance of normal right tympanic membrane Ossicles Incus Malleus Stapes 9 The Middle Ear – Auditory Ossicles The axis of rotation of the ossicular chain Anterior ligament of the malleus Posterior ligament of the incus Functions of the Middle Ear (1): Impedance Matching The middle ear ensures that sound is transmitted efficiently between the air and the fluids in the cochlea. The middle ear acts as an impedance-matching transformer. Middle Ear Impedance Matching z Acoustical impedance ( ) of any substance (be it gas, fluid, or solid) is, by definition, equal to the sound pressure p vibrating the substance ( ) divided by the velocity (speed) v of vibration ( ). The closer the impedances of two media (such as air and fluid) are to each other, the more acoustical energy will be transmitted from one to the other. Z = p/v Impedance Matching If the sounds were to arrive directly onto the oval window, most of the energy would be reflected back. The middle ear acts as impedance-matching device that improves sound transmission and reduces the amount of reflected sound. Transmission of sound through the middle ear is most efficient at middle frequencies (500-4000 Hz). 10 1. Areal ratio mechanism: AIR WATER incident sound reflected sound transmitted sound Water is denser than air and has a higher speed of sound, giving it a much higher impedance. Only 0.1% of sound energy is transmitted across the air/water boundary. 99.9% is reflected (like throwing a ping-pong ball against a basketball). 3. TM buckle: 2. Lever mechanism: (depends on the conical shape of the TM) d1 d2 11 Impedance Matching Middle Ear Impedance Matching 1. The difference between the areas of TM and the footplate of the stapes increases pressure Z2 = 17 ⋅ Z1 2. The difference between the lengths of the two lever arms both increases pressure and decreases velocity at the oval window Z 2 = 1.7 ⋅ Z1 3. The tympanic membrane buckle increases pressure and decreases velocity Impedance is greater at the stapes footplate (oval window) than at the tympanic membrane Z 2 = (17 ⋅1.7 ⋅ 2)Z1 = 58⋅ Z1 20 x log (58/1) = 35 dB total advantage Z 2 = 2 ⋅ Z1 Impedance Matching Taken together, the three mechanisms result in at most 74% of energy being transmitted to the cochlea. Functions of the Middle Ear (2): Reducing Bone Conducted Sound The middle ear reduces the transmission of boneconducted sound to the cochlea. Best transmission Chewing, blood flow, air flow, creaking joints, and contraction of muscles attached to the head, cause the skull to vibrate. The arrangement of the ossicles reduces the transmission of skull vibration because there is little relative movement of skull and ossicles when the skull vibrates. 12 Middle Ear Muscles Stapedius 1. Stapedius 2. Tensor Tympani Tensor Tympani Stapedius Muscle When stapedius muscle contracts it stiffens ossicular chain and reduces transmission of low frequencies (< 1000 Hz). Involved in two reflexes: stapedius reflex, which is triggered by high sound levels and prevents damage and masking by low-frequency sounds (because of delay, useless for impulsive sounds). Vocalisation reflex: stapedius contracts just before and relaxes just after vocalisations, reducing masking by self-generated speech. http://www.iurc.montp.inserm.fr Tensor Tympani When tensor tympani contracts it pulls on malleus, stiffens TM and pulls it into middle ear cavity, reducing the volume of the cavity. The muscle contracts (with tensor veli palatini) when we swallow or yawn, pushing fluid in the middle ear out of the Eustachian tube. Also helps equilibrate pressure in the middle ear with atmospheric pressure. Middle ear – summary: 1. Two muscles are attached to the ossicles, the tensor tympani to the manubrium of malleus and the stapedius to the stapes. 2. Function of the middle ear is: • to ensure the efficient transfer of sound from the air to the fluids in the cochlea (impedance matching) • to reduce the transmission of bone-conducted sound to the cochlea. 3. There are 3 mechanisms involved in middle ear impedance matching: • areal ratio mechanism • lever mechanism • tympanic membrane buckle 13 Peripheral Auditory System • outer ear • middle ear • cochlea • auditory nerve Outer ear Inner ear Middle ear Basilar Membrane Running the length of the cochlea is the basilar membrane. Each place on the membrane is tuned to a particular frequency: Travelling Wave High frequency sound Low frequency sound http://www.iurc.montp.inserm.fr 14 Travelling Wave Travelling Wave When pressure waves enter the cochlea, the basilar membrane starts to vibrate. The vibration takes the form of a “travelling wave”, that appears to travel from the base of the cochlea to the apex. The wave peaks at the place tuned to the frequency of the sound, then dies away rapidly. Travelling Wave Von Békésy (1947) observed travelling waves in the apex of the cochlea from human cadavar ears, using a microscope and stroboscopic illumination. Travelling Wave Basilar membrane “Envelope” of travelling wave “Envelope” of travelling wave 15 Low frequency tone – 250 Hz Mid frequency tone – 1000 Hz BM displacement BM displacement Base Distance Apex Base Distance Apex High frequency tone – 12500 Hz BM displacement Base Distance Apex 16 Passive Mechanism Passive Mechanism Von Békésy observed travelling waves in cadavar ears, in poor physiological condition and using very high levels (140 dB SPL). He observed quite broad tuning: Each tone excited a large region of the basilar membrane. Passive Mechanism - Linear Growth High" FREQUENCY" Low" Bekesy" Stimulus" B!a!s!e! Courtesy of Richard Baker Passive Mechanism 1. Broad tuning and therefore poor frequency selectivity. 2. Insensitivity to low-level sounds. INTENSITY" BASILAR MEMBRANE DISPLACEMENT" 17000 PLACE" 3. Linear response growth. So how do we explain the excellent frequency selectivity and high sensitivity exhibited by healthy human listeners? A!p!e!x! 17 Recent Measurements Recent Measurements (Data from Sellick et al., 1982) Recent physiological measurements of tuning in healthy ears show much sharper tuning. Also, the tuning depends critically on the physiological condition of the animal: the better the condition, the sharper the tuning. Sellick et al. (1982) measured tuning curves at a single place on the basilar membrane. Figure shows the input sound level, in dB SPL, required to produce a constant velocity of motion at a particular place on the BM, as a function of frequency. CF Response Functions Active Mechanism The shallow response growth, and sensitivity, goes away if the cochlea is in a poor physiological condition: 50 40 Gain ≈ 50 dB 30 Active! Gain! BM Velocity (dB)! 60 BM Velocity (dB) Alive Post-mortem Linear 70 BM Velocity (dB) The frequency selectivity of the basilar membrane is enhanced by the active amplification of frequencies close to the CF of each place: Gain! Passive! 20 0 10 20 30 40 50 60 70 80 90 100 110 Frequency Input Level (dB) Level (dB SPL) Ruggero et al. (1997) 18 OHC Transduction As the basilar membrane vibrates up and down, the hairs (stereocilia) on the hair cells are bent from side to side: Outer Hair Cells Stereocilia Cuticular plate Tight junction Deiters cell phalangeal process Mitochondrion Motile apparatus Nucleus Efferent nerve Fettiplace & Hackney (2006) Nature Reviews – Neuroscience, 7, 19-29 Good animations available at http://www.cochlea.org Outer Hair Cells Afferent nerve http://www.iurc.montp.inserm.fr Outer Hair Cells 1. 12 000 OHCs 2. The upper surface of each OHC contains: - Cuticular plate - Three rows of stereocilia - A noncuticular area that contains the basal body of a rudimentary kinocilium (at the bottom of the W or V , towards the stria vascularis) 3. On each OHC are about 150 stereocilia, arranged in two or more rows that form a shape of a V 4. The tips of the tallest raw of stereocilia are in contact with a tectorial membrane 19 OHC When the stereocilia are bent in one direction, tip links stretch and open ion channels. Positively-charged potassium ions enter the cell causing it to become “depolarised.” http://www.iurc.montp.inserm.fr/cric/audition/english/start2.htm OHC Electromotility OHC Electromotility OHC membrane depolarisation changes the conformation of the motor protein PRESTIN Fettiplace & Hackney (2006) Nature Reviews – Neuroscience, 7, 19-29 http://www.iurc.montp.inserm.fr 20 Reverse, or electro-mechanical transduction OHC damage Cochlear trauma causes OHC dysfunction and loss or reduction of active amplification. Causes include: Exposure to loud sounds Ototoxic drugs Hypoxia Dancing OHC, courtesy of Jonathan Ashmore, UCL Santos-Sacchi, J. (2003) New tunes from Corti s organ: the outer hair cell boogie rules. Current Opinions in Neurobiology, 13, 1-10 http://130.132.220.165/publications/santos-sacchi%202003.pdf Inner Hair Cells Stereocilia Cuticular plate Rudimentary kinocilium Mitochondrion Nucleus Rough endoplasmic reticulum Afferent nerve ending Efferent nerve ending Death Inner Hair Cells 1. 3500 IHCs 2. The upper surface of each IHC contains: - Cuticular plate - Three rows of stereocilia - A noncuticular area that contains the basal body of a rudimentary kinocilium 3. On each IHC are about 40 stereocilia, arranged in two or more parallel rows that form a very shallow U http://www.iurc.montp.inserm.fr 21 Inner Hair Cell Activation Mechanoelectric Transduction -40mV Excitation ! stereocilia bend towards the basal body +40mV Inhibition ! stereocilia bend away from the basal body -60mV http://www.physiology.wisc.edu/ftp/pub/aud-tour/ http://www.iurc.montp.inserm.fr/cric/audition/english/start2.htm Mechanoelectric Transduction Mechanoelectric Transduction When the stereocilia are bent in one direction, tip links stretch and open ion channels. Positively-charged potassium ions enter the cell causing it to become “depolarised”: increase in voltage from -40 mV to +40 + 80 mV - 40 mV mV. 1. Stereocillia bend 2. K+ flows into the IHC 3. IHC gets depolarised 4. Voltage-gated Ca2+ channels open; Ca2+ flows into the IHC 5. Neurotransmitter – glutamate – is released into the synaptic clefts at the base of the IHC http://www.iurc.montp.inserm.fr 22 Mechanoelectric Transduction + 80 mV 6. The neurotransmitter causes depolarisation of the dendrite of the auditory nerve. 7. Action potentials are generated in the auditory nerve fibre. 8. Transduction complete. - 40 mV Transduction The inner hair cells depolarise, and release neurotransmitter, only when the stereocilia are bent in one direction: Displacement of Basilar Membrane! 0 5 10 15 20 Inner Hair Cell! Auditory Nerve Fiber! http://www.iurc.montp.inserm.fr Cochlear Electrical Potentials Vibration of Basilar Membrane! Auditory Nerve Spikes! Electric Potential Auditory nerve fibres produce spikes that are phase-locked (synchronised) to the vibration of the basilar membrane: Displacement Phase Locking The electro-chemical properties of the cochlea determine how the transduction process occurs. Single Fiber! Information about the cochlear transduction process can be obtained from the cochlear potentials. Many Fibers! Time! 23 Resting Potentials Scala Vestibuli Perilymph (+) 2-5 mV Scala Media Endolymph + 80 mV - 70 mV Scala Tympani Perilymph 0 mV The voltage gradients in different fluid-filled compartments can be assessed by passing an electrode from the scala tympani through the organ of Corti and into the scala media. http://www.iurc.montp.inserm.fr Von Békésy (1952) Endocochlear Potential A large +80 mV endocochlear potential is recorded when the electrode is in the scala media. The endocochlear potential is the main driving force that is responsible for moving positively charged ions through the transduction channels of the hair cell stereocillia. The endocochlear potential is generated by active metabolic processes in cells within the stria vascularis. Resting Potentials The endolymph has a resting potential of approximately + 80 mV at all times. The OHCs have intracellular resting potentials of about -70 mV. There is approximately a 150 mV difference between the endolymph and the inside of OHCs. The IHCs have intracellular resting potentials of about -40 mV. 24 OHC IHC Radial afferent Lateral efferent Afferent Innervation (To the Brainstem) All cochlear hair cells are innervated by peripheral processes of spiral ganglion cells. Medial efferent Spiral afferent The central processes comprise the cochlear division of the VIIIth cranial nerve, which terminates in the cochlear nucleus. http://www.iurc.montp.inserm.fr Afferent Innervation (To the Brainstem) Although there are 3 times as many OHCs as IHCs, 95% of the spiral ganglion neurons of the cochlea innervate only IHCs. In humans, about 18 spiral ganglion neurons synapse on each IHC. Type I Spiral Ganglion Cells Both their cell bodies and their peripheral and central processes are well myelinated. These are the Type I spiral ganglion cells. Schematic representation of the hair cell afferent innervation (from Liberman) 25 Type II Spiral Ganglion Cells Are only 5% of sensory neurons to the cochlea. They are small, unmyelinated cells whose physiological properties are unknown. Go to OHCs, with each fibre making small afferent sensory synapses with many OHCs. Efferent Innervation (From the Brainstem) Organ of Corti receives efferent innervation from the olivocochlear bundle (OCB). Neurons with cell bodies in the superior olivary complex of the brainstem. Carry information from the brain to the ear instead of the reverse, i.e. brainstem is controlling some activities of the cochlea. There are two types of olivocochlear bundle (OCB) neurons: Those that terminate just under IHCs (lateral OCB) Those that go to OHCs (medial OCB) Schematic representation of the hair cell afferent innervation (from Liberman) Lateral Olivocochlear Bundle Neurons Cell bodies lie in the lateral part of the superior olivary complex. Small with unmyelinated (slow) axons that stay mostly on the same side (don t cross over). Lateral Olivocochlear Bundle Neurons They synapse just under the IHCs, on the peripheral processes of Type I spiral ganglion neurones of the cochlea. Lateral OCB Neurons Lateral OCB neurons 26 Neurotransmitters at IHC Synapses Medial Olivocochlear Bundle Neurons From medial olivocochlear bundle to the OHCs. Cell bodies in the medial portion of the superior olivary complex. Large neurons, well-myelinated axons (fast!). afferent efferent Medial OCB neurons http://www.iurc.montp.inserm.fr Medial Olivocochlear Bundle Neurons Neurotransmitters at OHC Synapses Most of the axons cross the midline to the opposite side of the brain and leave the brain with the vestibular division of the VIIIth cranial nerve. Synapse directly onto base of OHC. Medial OCB neurons efferent afferent http://www.iurc.montp.inserm.fr 27 Innervation of the IHCs and OHCs - Summary IHCs 1. Afferent Innervation - Type I fibres (95% of all afferent fibres), well-myelinated - many-to-one connection to IHCs (in humans, about 18 synapse on each IHC) 2. Efferent Innervation Lateral olivocochlear bundle fibres - synapse on the afferent nerves leaving the IHCs - unmyelinated OHCs 1. Afferent Innervation - Type II fibres (5% of all afferent fibres), unmyelinated - one-to-many connection to OHCs (in humans, each innervates about 10 OHCs) 2. Efferent Innervation Medial olivocochlear bundle fibres - synapse directly on the OHCs - well-myelinated Reading List Core reading: Musiek, F.E., Baran, J.A. The Auditory System; Anatomy, Physilogy, and Clinical Correlates (1st Edition) Allyn & Bacon, 2006. ISBN-10: 0205335535 Plack CJ. The Sense of Hearing. Routledge, 2005. ISBN: 0805848843 Yost WA. Fundamentals of Hearing: An Introduction (5th Edition), Academic Press, 2006. ISBN-10: 0123704731 Additional reading: Moore B.C.J. Introduction to the Psychology of Hearing (4th ed). Academic Press, 1997 Webster, B.D. Neuroscience of Communication (2nd Ed.) Singular, San Diego, 1999 Pickles, J.O. An Introduction to the Physiology of Hearing , 3nd Ed. Academic Press, 2008 Thank you for your attention ! Durrant JD and Lovrinic JH. Bases of Hearing Science (4rd Ed). Williams and Wilkins, 2008 Geisler DC. From Sound to Synapse: physiology of the mammalian ear. Oxford University Press, 1998 28