Effects of levosimendan on mortality and hospitalization. A meta
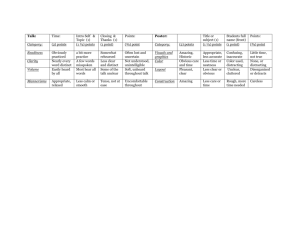
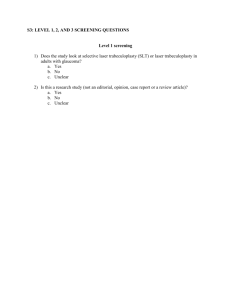
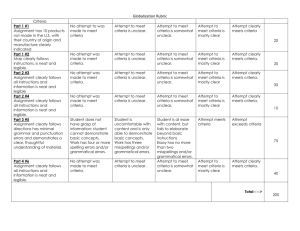
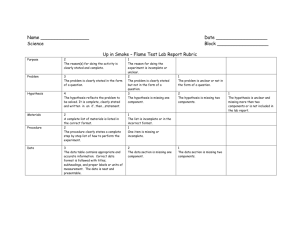
advertisement
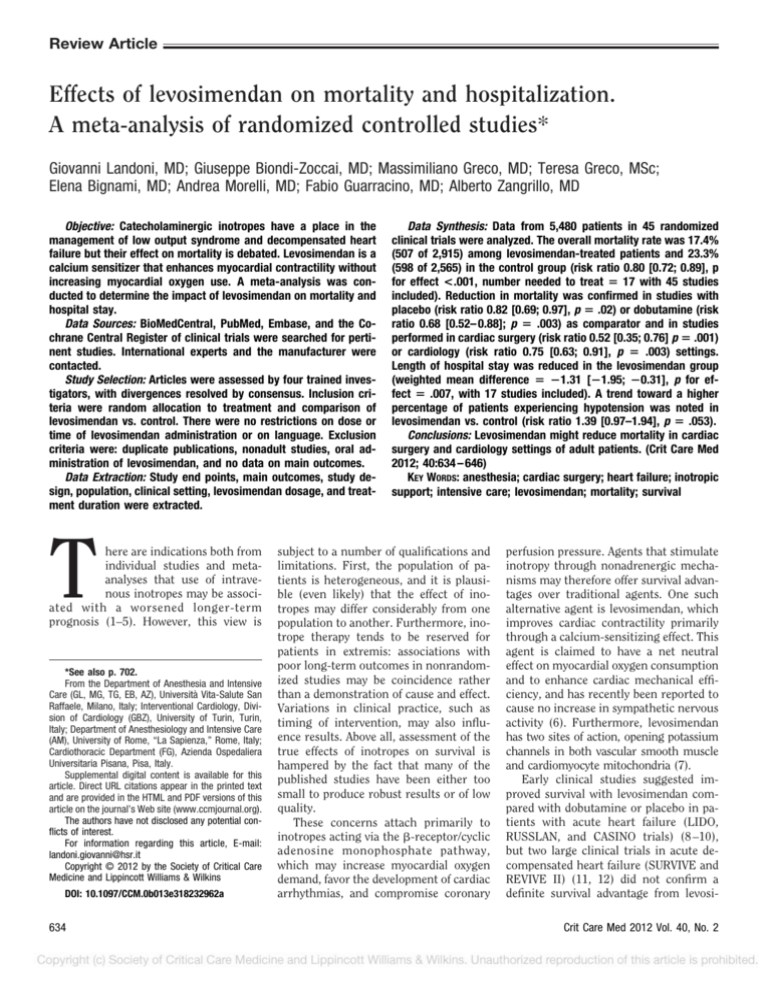
Review Article Effects of levosimendan on mortality and hospitalization. A meta-analysis of randomized controlled studies* Giovanni Landoni, MD; Giuseppe Biondi-Zoccai, MD; Massimiliano Greco, MD; Teresa Greco, MSc; Elena Bignami, MD; Andrea Morelli, MD; Fabio Guarracino, MD; Alberto Zangrillo, MD Objective: Catecholaminergic inotropes have a place in the management of low output syndrome and decompensated heart failure but their effect on mortality is debated. Levosimendan is a calcium sensitizer that enhances myocardial contractility without increasing myocardial oxygen use. A meta-analysis was conducted to determine the impact of levosimendan on mortality and hospital stay. Data Sources: BioMedCentral, PubMed, Embase, and the Cochrane Central Register of clinical trials were searched for pertinent studies. International experts and the manufacturer were contacted. Study Selection: Articles were assessed by four trained investigators, with divergences resolved by consensus. Inclusion criteria were random allocation to treatment and comparison of levosimendan vs. control. There were no restrictions on dose or time of levosimendan administration or on language. Exclusion criteria were: duplicate publications, nonadult studies, oral administration of levosimendan, and no data on main outcomes. Data Extraction: Study end points, main outcomes, study design, population, clinical setting, levosimendan dosage, and treatment duration were extracted. T here are indications both from individual studies and metaanalyses that use of intravenous inotropes may be associated with a worsened longer-term prognosis (1–5). However, this view is *See also p. 702. From the Department of Anesthesia and Intensive Care (GL, MG, TG, EB, AZ), Università Vita-Salute San Raffaele, Milano, Italy; Interventional Cardiology, Division of Cardiology (GBZ), University of Turin, Turin, Italy; Department of Anesthesiology and Intensive Care (AM), University of Rome, “La Sapienza,” Rome, Italy; Cardiothoracic Department (FG), Azienda Ospedaliera Universitaria Pisana, Pisa, Italy. Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.ccmjournal.org). The authors have not disclosed any potential conflicts of interest. For information regarding this article, E-mail: landoni.giovanni@hsr.it Copyright © 2012 by the Society of Critical Care Medicine and Lippincott Williams & Wilkins DOI: 10.1097/CCM.0b013e318232962a 634 Data Synthesis: Data from 5,480 patients in 45 randomized clinical trials were analyzed. The overall mortality rate was 17.4% (507 of 2,915) among levosimendan-treated patients and 23.3% (598 of 2,565) in the control group (risk ratio 0.80 [0.72; 0.89], p for effect <.001, number needed to treat ⴝ 17 with 45 studies included). Reduction in mortality was confirmed in studies with placebo (risk ratio 0.82 [0.69; 0.97], p ⴝ .02) or dobutamine (risk ratio 0.68 [0.52– 0.88]; p ⴝ .003) as comparator and in studies performed in cardiac surgery (risk ratio 0.52 [0.35; 0.76] p ⴝ .001) or cardiology (risk ratio 0.75 [0.63; 0.91], p ⴝ .003) settings. Length of hospital stay was reduced in the levosimendan group (weighted mean difference ⴝ ⴚ1.31 [ⴚ1.95; ⴚ0.31], p for effect ⴝ .007, with 17 studies included). A trend toward a higher percentage of patients experiencing hypotension was noted in levosimendan vs. control (risk ratio 1.39 [0.97–1.94], p ⴝ .053). Conclusions: Levosimendan might reduce mortality in cardiac surgery and cardiology settings of adult patients. (Crit Care Med 2012; 40:634 – 646) KEY WORDS: anesthesia; cardiac surgery; heart failure; inotropic support; intensive care; levosimendan; mortality; survival subject to a number of qualifications and limitations. First, the population of patients is heterogeneous, and it is plausible (even likely) that the effect of inotropes may differ considerably from one population to another. Furthermore, inotrope therapy tends to be reserved for patients in extremis: associations with poor long-term outcomes in nonrandomized studies may be coincidence rather than a demonstration of cause and effect. Variations in clinical practice, such as timing of intervention, may also influence results. Above all, assessment of the true effects of inotropes on survival is hampered by the fact that many of the published studies have been either too small to produce robust results or of low quality. These concerns attach primarily to inotropes acting via the -receptor/cyclic adenosine monophosphate pathway, which may increase myocardial oxygen demand, favor the development of cardiac arrhythmias, and compromise coronary perfusion pressure. Agents that stimulate inotropy through nonadrenergic mechanisms may therefore offer survival advantages over traditional agents. One such alternative agent is levosimendan, which improves cardiac contractility primarily through a calcium-sensitizing effect. This agent is claimed to have a net neutral effect on myocardial oxygen consumption and to enhance cardiac mechanical efficiency, and has recently been reported to cause no increase in sympathetic nervous activity (6). Furthermore, levosimendan has two sites of action, opening potassium channels in both vascular smooth muscle and cardiomyocyte mitochondria (7). Early clinical studies suggested improved survival with levosimendan compared with dobutamine or placebo in patients with acute heart failure (LIDO, RUSSLAN, and CASINO trials) (8 –10), but two large clinical trials in acute decompensated heart failure (SURVIVE and REVIVE II) (11, 12) did not confirm a definite survival advantage from levosiCrit Care Med 2012 Vol. 40, No. 2 mendan. Recent published meta-analyses (13, 14) suggest a modest survival benefit from levosimendan, but have been limited by the lack of a complete dataset from clinical trials. We therefore devised an updated meta-analysis of all the randomized clinical trials of levosimendan to reach a definitive conclusion about the role of this agent in the management of patients requiring inotropic drugs. The analysis was strengthened by the inclusion, for the first time, of the results of all the large clinical studies: SURVIVE (11, 15–18), LIDO (8, 19, 20), RUSSLAN (9), CASINO study (10, 21, 22), and REVIVE I and II (12, 17, 23–25). In addition, we analyzed mortality and hospital length of stay (LOS) in different settings (i.e., cardiology and cardiac surgery) and in subsets of studies in which levosimendan was compared to dobutamine or to placebo. MATERIALS AND METHODS Search Strategy Pertinent studies were independently searched in BioMedCentral, PubMed, Embase, and the Cochrane Central Register of clinical trials (updated November first 2010) by four trained investigators. The full PubMed search strategy was developed according to BiondiZoccai et al (26), available in the Appendix, and aimed to include any randomized study ever performed with levosimendan in any clinical setting in humans. In addition, we employed backward snowballing (i.e., scanning of references of retrieved articles and pertinent reviews) and contacted international experts and the manufacturer for further studies. No language restriction was enforced. Study Selection References obtained from database and literature searches were first independently examined at a title/abstract level by four investigators, with divergences resolved by consensus, and then, if potentially pertinent, retrieved as complete articles. The following inclusion criteria were used for potentially relevant studies: random allocation to treatment and comparison of levosimendan vs. control. There were no restrictions on dose or time of administration. The exclusion criteria were: duplicate publications either acknowledged or not (in this case we referred to the first article published while retrieved data from the article with the longest follow-up available), nonadult studies, oral administration of levosimendan, and lack of data on mortality. Two investigators inde- Crit Care Med 2012 Vol. 40, No. 2 pendently assessed compliance to selection criteria and selected studies for the final analysis, with divergences finally resolved by consensus. Data Abstraction and Study Characteristics Baseline, procedural, and outcome data were independently abstracted by four trained investigators, with divergences resolved by consensus. Specifically, we extracted potential sources of significant clinical heterogeneity, such as study design, sample size, clinical setting/ indication, levosimendan bolus dose, infusion dose and duration, control treatment, and follow-up duration, as well as primary study end points and other key outcomes. If a trial reported multiple comparisons, the control group was considered as a whole in the overall analysis and single groups were considered separately in subset analysis. At least two separate attempts at contacting original authors were made in cases of missing data. The primary end point of the present review was mortality at the longest follow-up available. The secondary end point was LOS. Internal Validity and Risk of Bias Assessment The internal validity and risk of bias of included trials was appraised by two independent reviewers according to Cochrane Collaboration methods (27), with divergences resolved by consensus. Publication bias was assessed by visually inspecting funnel plots, by analytical appraisal based on the Peters regression asymmetry test and on the Begg adjusted-rank correlation test for publication bias, and finally, with trim and fill method (28 –30). According to the Peters (28) or Begg (29) methods for publication bias evaluation, a two-sided p value of .10 or less was regarded as significant. Sensitivity analyses were performed by sequentially removing each study and reanalyzing the remaining dataset (producing a new analysis for each study removed), by selecting each individual subset (defined by setting and control drug), and by analyzing only data from studies with low risk of bias. Data Analysis and Synthesis Computations were performed with Stata (Stata Statistical Software: Release 11, College Station, TX) and RevMan 5 (a freeware available from The Cochrane Collaboration) (31). Hypothesis of statistical heterogeneity was tested by means of Cochran Q test, with statistical significance set at the two-tailed .10 level, whereas extent of statistical consistency was measured with I2, defined as 100% ⫻ (Q-df)/Q, where Q is Cochran’s heterogeneity statistic and df the degrees of freedom. Binary outcomes from individual studies were analyzed to compute individual and pooled risk ratios (RRs) with pertinent 95% confidence intervals (with equivalence set at 1, RR ⬍1 favoring the first treatment, and RR ⬎1 favoring the second treatment), by means of inverse variance method and with a fixed-effect model in case of low statistical inconsistency (I2 ⱕ25%) or with random-effect model (which better accommodates clinical and statistical variations) in case of moderate or high statistical inconsistency (I2 ⬎25%). In addition, we computed the number needed to treat (NNT) with corresponding 95% confidence intervals for the primary end point. Weighted mean differences (WMD) and 95% confidence intervals were computed for continuous variables using the same methods as just described (27). To explore the relation between log-risk mortality and the length of study follow-up, we performed univariate metaregression analyses. Statistical significance was set at the twotailed 0.05 level for hypothesis testing. Unadjusted p values are reported throughout. This study was performed in compliance with The Cochrane Collaboration and Preferred Reporting Items for Systematic Reviews and MetaAnalyses guidelines (27, 32). RESULTS Database searches, snowballing, and contacts with experts yielded a total of 541 articles. Excluding 453 nonpertinent titles or abstracts, we retrieved in complete form and assessed 88 studies according to the selection criteria (Fig. 1). Twenty-four studies were excluded because there were no outcome data and further details could not be obtained by the authors (33–56), two, including the PERSIST study (57, 58), because levosimendan was administrated orally, six because they were not randomized (5, 59 – 63), ten because of duplicate publication (15, 16, 20, 25, 64 – 69), and one because it involved a pediatric population (70). Ultimately, therefore, we identified 45 eligible randomized clinical trials for inclusion in the analysis (8 –12, 23, 71–109). Study Characteristics The 45 included trials randomized 5,480 patients (2,915 to levosimendan and 2,565 receiving control) (Table 1). Seventeen studies reported data on LOS. Clinical heterogeneity was mostly due to setting, dose, control treatment, and fol635 Figure 1. Flow diagram for selection of articles. low-up duration. Indeed, 23 studies (8 – 12, 23, 71, 77, 78, 81, 82, 84, 88, 90, 96, 98, 99, 101, 103–105, 108, 109) used levosimendan in a cardiological setting (decompensated heart failure); four of these studies used intermittent 24-hr infusions of levosimendan (77, 90, 96, 99). Seventeen studies used levosimendan in cardiac surgery (73, 76, 79, 80, 83, 87, 89, 91, 93–95, 97, 102, 106, 107), two trials were performed in septic patients (72, 100), two in an interventional cardiology setting (85, 86), and one in vascular surgery (92). Thirty-six authors administered a bolus (8 –12, 23, 71, 73–78, 81– 83, 85– 87, 90 –95, 97, 99, 101, 102, 104 – 109, 112), and 41 authors used a continuous infusion (8 –12, 23, 71–75, 77– 86, 88 –105, 108, 109), 32 of them following bolus (8 –12, 23, 71, 73–75, 77, 78, 81– 83, 85, 86, 90 –95, 97–99, 101, 102, 104, 105, 108, 109). Dose varied between 3 and 36 g/kg as intravenous bolus and between 0.05 and 0.6 g/kg/min as a continuous infusion. Seventeen studies were multicentered (8 –12, 23, 78, 83, 90, 93–97, 100, 101, 104). Study quality appraisal indicated that studies were of variable quality (Table 2) and that 13 of them had a low risk of bias. Quantitative Data Synthesis Overall analysis showed that the use of levosimendan was associated with a significant reduction in mortality at the longest follow-up available (507 of 2,915 [17.4%] in the levosimendan group vs. 636 598 of 2,565 [23.3%] in the control arm, RR ⫽ 0.80 [0.72; 0.89], p for effect ⬍ .001, Q ⫽ 51.98, p for heterogeneity ⫽ .191, I2 ⫽ 15.4%, NNT ⫽ 17 with 5,480 patients and 45 studies included) (Fig. 2). The reduction in mortality was confirmed when studies with at least 30, 90, and 180 days of follow-up were analyzed (Table 3, and supplemental data [Supplemental Digital Material 1–3, http://links.lww.com/ CCM/A342]). Furthermore, a univariate metaregression of average follow-up against log-risk mortality showed no significant effects for time on mortality (n ⫽ 45, slope coefficient ⫽ 0.01 [-0.01, 0.03]; p ⫽ .36) (see supplemental data [Supplemental Digital Material 4, http://links.lww. com/CCM/A342]). A reduction in mortality was also found when studies with short-term follow-up (ⱕ30 days) were analyzed, and when studies with follow-up longer than 30 days were analyzed (see supplemental data [Supplemental Digital Material 5 and 6, http://links.lww.com/ CCM/A342]). The reduction in mortality was confirmed when only the studies comparing levosimendan to placebo were included (233 of 1581 [14.7%] vs. 205 of 1097 [18.7%], RR ⫽ 0.82 [0.69; 0.97], p for effect ⫽ .02, Q ⫽ 21.95, p for heterogeneity ⫽ .582, I2 ⫽ 0% with 25 studies included, NNT ⫽ 25; see supplemental data [Supplemental Digital Material 7, http://links.lww.com/CCM/A342]), and when only the studies comparing levosimendan with dobutamine were included (280 of 1383 [15.0%] vs. 361 of 1305 [27.7%], RR ⫽ 0.68 [0.52– 0.88]; p for effect ⫽ .003, Q ⫽ 27.74, p for heterogeneity ⫽ .023, I2 ⫽ 45.9% with 16 studies included, NNT ⫽ 13; see supplemental data [Supplemental Digital Material 8, http://links. lww.com/CCM/A342]). Furthermore, the reduction in mortality was confirmed in the cardiac surgery setting (37 of 635 [5.8%] in the levosimendan group vs. 77 of 598 [12.9%] in the control arm, RR ⫽ 0.52 [0.35; 0.76], p ⫽ .001, Q ⫽ 13.69, p for heterogeneity ⫽ .622, I2 ⫽ 0% with 17 studies included, NNT ⫽ 14; see supplemental data [Supplemental Digital Material 9, http:// links.lww.com/CCM/A342]), in the cardiology setting (441 of 2207 ([20.0%] in the levosimendan group vs. 484 of 1893 [25.6%] in the control group, RR ⫽ 0.67 [0.51; 0.86], p ⫽ .002, RR ⫽ 0.75 [0.63; 0.91], p ⫽ .003, Q ⫽ 29.51, p for heterogeneity ⫽ .131, I2 ⫽ 25.5% with 23 studies included, NNT ⫽ 18; see supplemental data [Supplemental Digital Material 10, http://links.lww.com/CCM/A342]), and in those patients undergoing revascularization, either surgical or percutaneous (Table 3 and Supplemental Digital Material 11, http://links.lww.com/CCM/ A342). Numerous other subanalyses on risk of mortality were conducted and are summarized in Table 3 and as supplemental data (Supplemental Digital Material 1217, http://links.lww.com/CCM/A342). A significant reduction in mortality for levosimendan-treated patients was found when only studies on patients on mechanical ventilation, only studies with mortality as a primary end point, and only studies with ⬎100 patients were included in the analysis. A subanalysis including only blind studies found a significant reduction in mortality favoring levosimendan. When study drug infusion rate was considered, a significant reduction in mortality was found, either for studies with low infusion rates (ⱕ0.1 g/kg/min) or in studies with infusion rate ⬎0.1 g/ kg/min. A significant reduction in mortality was found in those administering or not levosimendan bolus. A subanalysis on sepsis with only two studies included found no difference in mortality between levosimendan and control groups (see supplemental data [Supplemental Digital Material 18, http:// links.lww.com/CCM/A342]). LOS was reduced in the levosimendan group (WMD ⫽ ⫺1.31 [⫺1.95; ⫺0.31], p Crit Care Med 2012 Vol. 40, No. 2 Table 1. Description of the 45 studies included in the meta-analysis First Author Setting Levosimendan Control Patients Patients Control Bolus Continuous Dose Infusion Dose g/kg g/kg/min Adamopoulos (71) Al-Shawaf (73) Alhashemi (72) Cardiology 23 46 Cardiac surgery Septic shock 14 21 16 21 Dobutamine, placebo Milrinone Dobutamine Alvarez (75) Alvarez (74) Barisin (76) Berger (77) Cardiac surgery Cardiac surgery Cardiac surgery Cardiology 15 25 21 39 15 25 10 36 Dobutamine 12 Dobutamine 12 Placebo 12–24 Prostaglandin E1 12 Cardiology Cardiac surgery Cardiac surgery Cardiology Cardiology Cardiac surgery Cardiology Cardiology Cardiology (primary coronary angioplasty) García-González Cardiology (primary (86) coronary angioplasty) Husedzinovií Cardiac surgery (87) Ikonomidis (88) Cardiology Järvelä (89) Cardiac surgery Kleber (90) Cardiology 29 15 40 30 20 30 30 103 16 31 15 20 32 20 30 15 100 16 Dobutamine Milrinone Milrinone Dobutamine Dobutamine Placebo Placebo Dobutamine Enoximone 6–12 6–12 12 24 12 0.1–0.2 0.1 0.1 0.1 0.1 0.2 0.1 0.1–0.2 0.1–0.2 11 11 Dobutamine 24 0.1 12 13 Placebo 12 21 12 18 21 12 10 Placebo Placebo Placebo 12 0.1–0.2 0.2 0.1–0.2 Lahtinen (91) Leppikangas (92) Levin (95) Levin (93) Levin (94) Levin (97) Levin (96) Cardiac surgery Vascular surgery 103 10 104 11 Placebo Placebo 24 24 0.2 0.2 Cardiac surgery Cardiac surgery Cardiac surgery Cardiac surgery Cardiology 69 36 39 127 40 68 35 38 126 40 Dobutamine Dobutamine Placebo Dobutamine Placebo 10 10 10 10 0.1 0.1 0.1 0.1 0.1 Lilleberg (98) Mavrogeni (99) Cardiology Cardiology 11 25 11 25 Placebo Nothing 12 6 0.1–0.2 0.1–0.2 Mebazaa (11) Moiseyev (9) Cardiology Cardiology 664 402 663 102 Dobutamine Placebo 12 6/12/ 24/24 0.2 0.1–0.4 Morelli (100) Nieminen (101) Sepsis Cardiology 15 95 15 56 Nijhawan (102) Packer (23) Packer (12) Parissis (103) Slawsky (104) Trikas (105) Tritapepe (107) Tritapepe (106) Tziakas (108) Zairis (10) Cardiac surgery Cardiology Cardiology Cardiology Cardiology Cardiology Cardiac surgery Cardiac surgery Cardiology Cardiology 12 51 299 42 98 24 12 53 30 100 6 49 301 21 48 24 12 53 30 99 Zemljic (109) Cardiology 20 20 Dobutamine Dobutamine, placebo, ethanol vehicle Placebo Placebo Placebo Placebo Placebo Placebo Placebo Placebo Placebo Dobutamine, placebo Nothing Bergh (78) De Hert (79) De Hert (80) Duygu (81) Duygu (82) Eriksson (83) Flevari (84) Follath (8) Fuhrmann (85) Crit Care Med 2012 Vol. 40, No. 2 Length of Infusion Follow-Up 6 0.1 24 hrs 4 mos 12 0.1–0.2 0.05–0.2 24 hrs 24 hrs 0.2 0.2 24 hrs 24 hrs End of hospitalization End of intensive care unit stay 1 day 15 days End of hospitalization 12 mos 12 3/6/ 12/24/ 36 18/26 12 12 6 6 24 24 6 16 12 0.1 Monthly 24 hrs intermittent infusion 24 hrs 19 ⫾ 4 hrs 22–23 hrs 24 hrs 24 hrs 24 hrs 24 hrs 24 hrs 24 hrs 24 hrs 30 days End of hospitalization 30 days 6 mos 30 days 30 days 3 mos 6 mos 30 days 12 mos End of hospitalization 24 hrs 24 hrs 24 hrs, then intermittent infusion 6 hrs every 2 wks 24 hrs 24 hrs 18 mos 1 yr 84 days 24 hrs 24 hrs 24 hrs 24 hrs 24 hrs every 2 months intermittent infusion 24 hrs Monthly 24 hrs intermittent infusion 24 hrs 6 hrs End of hospitalization 30 days 30 days End of hospitalization 1 yr End of hospitalization 5 yrs 14 days 6 mos 6 mos 6 mos 0.2 0.05–0.6 24 hrs 24 hrs 30 days 2–9 days 0.2–0.3 0.1–0.2 0.2 0.1 0.1–0.4 0.1–0.4 6 hrs 24 hrs 24 hrs 24 hrs 4–6 hrs 24 hrs 0.1 0.2 24 hrs 24 hrs End of hospitalization 5 days 3 mos End of hospitalization 30 days 30 days End of hospitalization 30 days End of hospitalization 6 mos 0.1 24 hrs 3 mos 637 Table 2. Methodologic quality summary: Review authors’ judgments about each methodologic quality item for each included study Domain/Question Adequate Sequence Generation? Allocation Concealment Used? Adamopoulos (71) Al-Shawaf (73) Alhashemi (72)a Alvarez (75) Alvarez (74) Barisin (76) Berger (77) Bergh (78) De Hert (79) De Hert (80) Duygu (81) Duygu (82) Eriksson (83) Flevari (84) Follath (8) Fuhrmann (85) García-González (86) Husedzinovií (87) Ikonomidis (88) Järvelä (89) Kleber (90) Lahtinen (91)a Leppikangas (92) Levin (95) Levin (93)a Levin (94)a Levin (97)a Levin (96)a Lilleberg (98) Mavrogeni (99) Mebazaa (11) Moiseyev (9) Morelli (100) Nieminen (101) Nijhawan (102) Packer (23)a Packer (12)a Parissis (103) Slawsky (104) Trikas (105) Tritapepe (106) Tritapepe (107) Tziakas (108) Zairis (10)a Zemljic (109) Unclear Unclear Unclear Unclear Unclear Yes Unclear Unclear Yes Yes Unclear Unclear Unclear Unclear Yes Yes Unclear No Unclear Yes Yes Unclear Unclear Yes Unclear Unclear Unclear Unclear Unclear Yes Unclear Yes Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear Yes Yes Unclear Unclear Unclear Unclear Yes Unclear Unclear Unclear Yes Yes Unclear Yes Yes Unclear Unclear Unclear Unclear Yes Unclear Unclear Yes Unclear Yes Yes Unclear Yes Unclear Unclear Unclear Unclear Unclear Unclear Unclear Yes Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear a Incomplete Outcome Data Addressed? Uniform and Explicit Outcome Definitions? Free From Selective Outcome Reporting? Free From Other Bias? Overall Risk of Bias? No No No No No Yes No Yes Yes Yes Yes Yes Yes No Yes No No Yes Yes Yes Yes Yes Yes No Unclear Unclear Unclear Unclear Yes No Yes Yes Yes Yes Yes Yes Yes No Yes Yes Yes Yes No Yes No Yes Yes Unclear Yes Yes Yes Yes Unclear Yes Yes Yes Yes Yes Yes Yes Unclear Unclear Yes Yes Yes Yes Yes Yes Yes Unclear Unclear Unclear Unclear No Yes Yes Yes Yes Yes Yes Unclear Unclear Yes Yes Yes Yes Yes Yes Unclear Yes Unclear Unclear Unclear Unclear Unclear Unclear Unclear Yes Unclear Unclear Unclear Unclear Unclear Unclear Yes Yes Unclear Unclear Unclear Unclear Yes Unclear Unclear Unclear Unclear Yes Unclear Unclear Yes Unclear Yes Yes Unclear Unclear Unclear Unclear Unclear Unclear Unclear No Unclear Unclear Unclear Unclear Unclear Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Unclear Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Unclear Yes Yes Unclear Unclear Unclear Unclear Yes Yes Yes Yes Yes Yes Yes Unclear Unclear Yes Yes Yes Yes Yes Yes Unclear Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes Yes No Yes Yes Yes Unclear Yes Yes Unclear Unclear Unclear Unclear Yes Yes Yes Yes Yes Yes No Unclear Unclear Yes Yes Yes Yes Yes Yes Unclear Yes Moderate Moderate High Moderate Moderate Low Moderate Low Low Low Moderate Low Moderate Moderate Low Moderate High Moderate Moderate Low Low Moderate Low Moderate High High High High Moderate Moderate Low Low Moderate Moderate Moderate Moderate Moderate Moderate Moderate Moderate Moderate Low Moderate High Moderate Study published as abstract only. for effect ⫽ .007, Q ⫽ 56.15, p for heterogeneity ⬍.0001, I2 ⫽ 71% with 17 studies included) (Fig. 3). The reduction in LOS was not found in the cardiac surgery setting (see supplemental data [Supplemental Digital Material 19, http://links. lww.com/CCM/A342]) but was confirmed in the cardiology setting (WMD ⫽ ⫺1.59 [⫺2.33; ⫺0 – 85], p for effect ⬍.0001, Q ⫽ 15.52, p for heterogeneity ⫽ .03, I2 ⫽ 54.9% with eight studies included; see supplemental data [Supplemental Digital Material 20, http://links.lww.com/ CCM/A342]), even when only studies with placebo as comparator were considered 638 Blinding? Concurrent Therapies Similar? (WMD ⫽ ⫺2.05 [⫺2.70; ⫺1.40], p for effect ⬍ .001, Q ⫽ 1.94, p for heterogeneity ⫽ .379, I2 ⫽ 0% with three studies included; see supplemental data [Supplemental Digital Material 21, http://links. lww.com/CCM/A342]). Numerous other subanalyses of adverse events and complications rate were conducted and are summarized in Table 4 and in Supplemental Digital Material 22–26 (http://links.lww.com/CCM/A342). Visual inspection of funnel plots did not identify a skewed or asymmetrical shape for mortality (Fig. 4) or LOS (Fig. 5). Quantitative evaluation did not sug- gest a presence of publication bias, as measured by the Begg test (p ⫽ .512 for mortality, p ⫽ .967 for LOS) and Peters test (p ⫽ .135 for mortality, p ⫽ .849 for LOS). Absence of bias was also confirmed by trim and fill approach. Sensitivity analyses confirmed the overall results of our work for the overall mortality results (see supplemental data [Supplemental Digital Material 27, http:// links.lww.com/CCM/A342]). Indeed, sensitivity analyses performed by sequentially removing each study and reanalyzing the remaining dataset (producing a new analysis for each study reCrit Care Med 2012 Vol. 40, No. 2 Study ID RR (95% CI) % Weight Adamopoulos S 2006 Al−Shawaf E 2006 Alhashemi JA 2009 Alvarez J 2005 Alvarez J 2006 Barisin S 2004 Berger R 2007 Bergh CH 2010 De Hert SG 2007 De Hert SG 2008 Duygu H 2008 Duygu H 2008 Eriksson HI 2009 Flevari P 2006 Follath F 2002 Fuhrmann JT 2008 Garcia−Gonzalez MJ 2006 Husedzinovic I 2005 Ikonomidis I 2007 Jarvela K 2008 Kleber FX 2009 Lahtinen P 2009 Leppikangas H 2008 Levin R 2008 Levin R 2008 Levin R 2008 Levin R 2009 Levin R 2009 Lilleberg J 2007 Mavrogeni S 2007 Mebazaa A 2007 Moiseyev VS 2002 Morelli A 2005 Nieminem M 2000 Nijhawan N 1999 Packer M 2003 Packer M 2005 Parissis JT 2007 Slawsky MT 2000 Trikas A 2006 Tritapepe L 2006 Tritapepe L 2009 Tziakas DN 2005 Zairis MN 2004 Zemljic G 2007 Overall (I−squared = 15.4%, p = 0.191) 0.44 (0.10, 1.89) 1.14 (0.08, 16.63) 0.77 (0.44, 1.35) 2.00 (0.07, 55.24) 1.00 (0.07, 15.12) 0.48 (0.01, 22.31) 0.79 (0.29, 2.13) 2.14 (0.20, 22.34) 0.25 (0.01, 5.10) 0.13 (0.01, 1.05) 1.54 (0.77, 3.07) 0.50 (0.21, 1.20) 0.25 (0.01, 5.32) 1.50 (0.17, 13.23) 0.69 (0.46, 1.04) 0.50 (0.22, 1.14) 3.00 (0.37, 24.58) 1.08 (0.02, 50.43) 0.17 (0.01, 3.13) 3.00 (0.36, 24.92) 0.28 (0.01, 7.57) 1.01 (0.48, 2.14) 1.10 (0.37, 3.27) 0.35 (0.15, 0.83) 0.22 (0.05, 0.93) 0.12 (0.02, 0.93) 0.45 (0.21, 0.94) 0.32 (0.14, 0.71) 1.00 (0.02, 46.05) 0.25 (0.06, 1.06) 0.93 (0.78, 1.11) 0.72 (0.51, 1.01) 0.78 (0.39, 1.54) 0.59 (0.04, 9.24) 0.50 (0.01, 22.25) 0.77 (0.22, 2.70) 1.10 (0.84, 1.44) 0.50 (0.01, 24.33) 0.49 (0.10, 2.34) 0.33 (0.08, 1.42) 1.00 (0.02, 46.40) 1.00 (0.02, 49.47) 1.00 (0.02, 48.77) 0.51 (0.32, 0.81) 1.00 (0.02, 47.97) 0.80 (0.72, 0.89) 0.53 0.16 3.56 0.10 0.15 0.08 1.13 0.20 0.12 0.25 2.35 1.45 0.12 0.24 6.66 1.66 0.25 0.08 0.13 0.25 0.10 1.97 0.94 1.48 0.52 0.27 2.00 1.72 0.08 0.53 35.55 9.70 2.41 0.15 0.08 0.71 15.67 0.07 0.46 0.53 0.08 0.07 0.07 5.30 0.07 100.00 .00888 1 113 Figure 2. Forest plot for the risk of mortality. The use of levosimendan was associated with a significant reduction in mortality at the longest follow-up available (507 of 2915 [17.4%] in the levosimendan group vs. 598 of 2565 [23.3%] in the control arm, risk ratio [RR]: 0.80 [0.72; 0.89], p for effect⬍ .001, Q ⫽ 51.98, p for heterogeneity ⫽ .191, I2 ⫽ 15.4%, NNT ⫽ 17 with 5,480 patients and 45 studies included). CI, confidence interval. moved), and by analyzing only data from studies with low risk of bias did not determine major changes in direction or magnitude of statistical findings, confirming for each analysis the pooled effect (RR ⬍1 or WMD ⬍0) and the statistical significance (p ⬍ .05). Crit Care Med 2012 Vol. 40, No. 2 DISCUSSION This is the most comprehensive metaanalysis yet performed on levosimendan, and statistically the most robust. Survival benefits of levosimendan were confirmed in numerous subanalyses and sensitivity analyses. The findings of the present meta-analysis are more important if we consider that we noted a reduction in LOS in patients receiving levosimendan. The central finding of our analysis is that levosimendan reduced mortality in both the overall population, and in the subpopulations of cardiac surgery and 639 Table 3. Subanalyses on mortality Subgroups of Interest Studies with the longest follow-up of at least 30 days Studies with the longest follow-up of at least 90 days Studies with the longest follow-up of at least 180 days Studies with surgical or percutaneous revascularization Studies with patients on mechanical ventilation Studies with mortality as primary end point Studies with more than 100 patients Blinded studies Studies with levosimendan infusion ⱕ0.1 g/kg/min Levosimendan infusion ⬎0.1 g/kg/min Studies with Levosimendan bolus Studies without levosimendan bolus Studies with sepsis patients Number Event Levosimendan of Studies Group Event Control Group Risk Ratio (95% Confidence Interval) p I2 Number Needed to Treat 28 464 of 2255 (21%) 522 of 1981 (26%) 0.725 (0.597–0.879) .001 34% 17 (16–18) 17 438 of 1880 (23%) 468 of 1683 (28%) 0.794 (0.641–0.983) .034 42% 22 (21–23) 12 346 of 1457 (24%) 377 of 1252 (30%) 0.745 (0.570–0.974) .032 52% 16 (15–17) 16 30 of 484 (6.7%) .001 14 (13–15) 22 232 of 1380 (17%) 304 of 1343 (23%) 0.612 (0.457–0.820) .001 26% 17 (16–18) 9 397 of 1726 (23%) 397 of 1421 (28%) 0.669 (0.507–0.882) .004 66% 20 (19–22) 12 27 18 427 of 2164 (20%) 449 of 2273 (20%) 68 of 727 (9%) 459 of 1864 (25%) 474 of 1961 (24%) 120 of 650 (18%) 0.758 (0.620–0.927) 0.86 (0.77–0.97) 0.556 (0.396–0.782) .007 40% .011 1.0% .001 26% 20 (19–22) 23 (21–24) 11 (10–12) 22 35 10 2 421 of 1990 (21%) 459 of 2579 (18%) 48 of 336 (14%) 17 of 36 (47%) 398 of 1628 (24%) 476 of 2186 (22%) 122 of 379 (32%) 22 of 36 (61%) 0.878 (0.779–0.990) .033 0.0% 0.843 (0.752–0.945) .003 5.3% 0.579 (0.437–0.768) ⬍.001 12% 0.77 (0.50–1.19) .2 0.0% 59 of 448 (13.7%) 0.511 (0.342–0.764) 0.0% 30 (28–33) 25 (24–27) 5.6 (5.3–5.8) Forest plots are presented as supplemental material (Supplemental Digital Material, http://links.lww.com/CCM/A342). cardiology. Survival benefit from levosimendan was apparent in comparison with conventional inotrope therapy (i.e., dobutamine), as reported in our own and other, earlier meta-analyses. In addition, and in important contrast to earlier estimates (14, 110), our new analysis of an enlarged dataset revealed a survival benefit of levosimendan in trials vs. placebo. In some of the included studies, cardiogenic shock was an exclusion criteria, and this may be reflected by the low mortality rate reported in patients hospitalized for heart failure in our metaanalysis. On the other side, the cardiac surgery population of our meta-analysis was at high risk and presented a perioperative risk of mortality (5%–10%) that is highly increased when compared to modern cardiac surgery (about 1%–3% as reported in literature [111]). Since the effect of levosimendan on mortality was stronger in the cardiac surgery setting, we suggest that the increased effects in populations at higher risk of mortality may reflect a specific action of levosimendan, which may be translated to other critically ill populations. Many of the studies included in our analysis were individually statistically underpowered. However, as illustrated in Figure 2, many of them (28 studies, 62%) conformed to the trend for benefit identified in the aggregate estimate, while six studies (13%) had neutral findings. We regard this indication of broad consistency between numerous individual stud640 ies and the overall result as a noteworthy feature of this exercise: it provides assurance that the net survival benefit attributable to levosimendan is not the product of a single dominating trial (or a few dominating trials) in a narrowly defined patient population. All the secondary analyses, including bias, influence, and robustness analysis, confirmed the validity of our findings. This demonstration of a survival benefit from levosimendan is in contrast to investigations into the effects of conventional inotropes, in which demonstrations of improvement in hemodynamic indices has not been accompanied by survival benefits (1–5). Bayram et al (1) concluded that short-term use of these agents was associated with increased postdischarge mortality, particularly in patients with ischemic heart disease, while Thackray et al (2) reported that, compared to placebo, intravenous administration of adrenergic inotrope agents tended to increase mortality (odds ratio 1.50, 95% confidence interval 1.51–3.92), albeit this did not reach significance. Levosimendan is in fact the first inotropic agent to establish a positive impact on patient survival time for any inotropic agent in comparison with placebo. Previous positive findings in comparisons vs. active controls have all favored levosimendan over agents such as dobutamine: our new inspection of the data affirm that finding. It is also interesting to note that large, head-to-head comparisons of other inotropic agents were recently performed and no difference was noted. Annane et al (112) suggested that there is no evidence for a difference in efficacy and safety between epinephrine alone and norepinephrine plus dobutamine for the management of septic shock, while De Backer et al (113) found that there was no significant difference in the rate of death between patients with shock who were treated with dopamine as the first-line vasopressor agent and those who were treated with norepinephrine. However, dopamine treatment was associated with a significantly higher rate of cardiac adverse events together with a borderline p value (.07) for increased intensive care unit mortality in dopamine-treated patients when compared to norepinephrine, suggesting a detrimental effect of highdose dopamine. Data from 17 of the studies we identified revealed that levosimendan was associated with a reduced LOS. This finding was replicated in a subset of nine studies in the cardiology setting. This finding is compatible with the work of Ribeiro et al (110). The absence of evidence for any similar reduction in LOS in the cardiac surgery setting may be a paradoxical effect of the survival benefit seen with levosimendan: the greater proportion of levosimendan-treated survivors leads to an increase in average LOS vis-à-vis controltreated patients who do not survive. Crit Care Med 2012 Vol. 40, No. 2 % Study ID WMD (95% CI) Weight Barisin S 2004 −0.80 (−4.67, 3.07) 3.26 Bergh CH 2010 −1.40 (−9.00, 6.20) 1.07 De Hert SG 2007 −3.00 (−7.32, 1.32) 2.77 De Hert SG 2008 −6.00 (−11.06, −0.94) 2.16 Duygu H 2008 0.00 (−1.10, 1.10) 9.72 Duygu H 2008 −2.00 (−2.62, −1.38) 11.02 Eriksson HI 2009 0.10 (−3.53, 3.73) 3.58 Follath F 2002 0.80 (−2.59, 4.19) 3.93 Husedzinovic I 2005 −1.20 (−5.64, 3.24) 2.66 Jarvela K 2008 1.60 (−0.32, 3.52) 7.15 Leppikangas H 2008 −3.00 (−8.49, 2.49) 1.89 Mebazaa A 2007 −2.50 (−5.51, 0.51) 4.56 Packer M 2005 −1.60 (−2.56, −0.64) 10.14 Parissis JT 2007 −2.60 (−3.63, −1.57) 9.91 Trikas A 2006 −2.00 (−3.71, −0.29) 7.78 Tritapepe L 2006 −1.50 (−3.10, 0.10) 8.14 Tritapepe L 2009 0.90 (−0.01, 1.81) 10.27 Overall (I−squared = 71.0%, p = 0.000) −1.13 (−1.95, −0.31) 100.00 NOTE: Weights are from random effects analysis −11.1 0 11.1 Figure 3. Forest plot for the length of hospital stay. Length of hospital stay was reduced in the levosimendan group (weighted mean difference [WMD] ⫺1.31 [⫺1.95; ⫺0.31], p for effect ⫽ .007, Q ⫽ 56.15, p for heterogeneity ⬍ .0001, I2 ⫽ 71% with 17 studies included). CI, confidence interval. Table 4. Adverse events Outcome of Interest Myocardial infarction Ventricular arrhythmias Supraventricular arrhythmias Hypotension Composite end point of hypotension and/or norepinephrine use Number of Studies Event Levosimendan Event Control Risk Ratio (95% Confidence Interval) p I2 23 9 19 22 25 28 of 1161 (2.4%) 157 of 1344 (12%) 239 of 1958 (12%) 330 of 1532 (22%) 388 of 1599 (24%) 32 of 726 (4.4%) 152 of 1292 (12%) 203 of 1619 (13%) 211 of 1090 (19%) 268 of 1157 (23%) 0.804 (0.512–1.261) 0.885 (0.611–1.281) 0.997 (0.776–1.280) 1.389 (0.996–1.936) 1.219 (0.954–0.558) .3 .5 .9 .053 .11 0.0% 43% 37% 48% 61% Forest plots are presented in Supplemental Digital Material, http://links.lww.com/CCM/A342). Levosimendan is currently used in ⬎50 countries and is listed in the European Society of Cardiology guidelines for treatment of acute heart failure (114). However, to the best of our knowledge, the Federal Drug Administration has not yet approved it for use in the United States. Detailed explanation of the beneficial effects of levosimendan is beyond the Crit Care Med 2012 Vol. 40, No. 2 scope of a meta-analysis, but various aspects of the pharmacology of the drug may be relevant. Levosimendan is primarily a calcium sensitizer. It displays calcium-dependent binding to troponin C, with higher affinity at high calcium concentrations and lower affinity at low calcium concentrations. By stabilizing the calcium-troponin C complex, levosi- mendan prolongs the actin-myosin crossbridge association rate. This mechanism differentiates levosimendan from classic inotropes and is regarded as the basis of the drug’s ability to improve myocardial efficiency without increasing myocardial oxygen demand (115). The beneficial effects of levosimendan may also be related to a vasodilatory effect mediated 641 tal discharge (WMD ⫽ ⫺1.38 days [⫺2.78, 0.03], p ⫽ .05) in patients (n ⫽ 74) receiving levosimendan (117). Another meta-analysis of randomized controlled trials (118) already suggested a beneficial effect of levosimendan on survival, but the analysis was limited to the specific setting of cardiac surgery. s.e. ln(RR) 1 .5 0 Funnel plot with pseudo 95% confidence limits 2 1.5 Limitations of the Study −4 −2 0 ln(RR) 2 4 Figure 4. Funnel plot for the risk of mortality. RR, risk ratio; s.e., standard error. 4 3 s.e.WMD 2 1 0 Funnel plot with pseudo 95% confidence limits −10 −5 0 WMD 5 10 Figure 5. Funnel plot for the length of hospital stay. WMD, weighted mean difference; s.e., standard error. by an adenosine triphosphate-sensitive potassium-channel opening effect, which may reduce ventricular afterloading (115, 116). The beneficial effect of levosimendan on mortality seems to be more pronounced when the drug is administered at an infusion rate ⱕ.01 g/kg/min, even if only a trend was noted toward an increased survival in this group. This hypothesis is strengthened by the signifi642 cant increase in the rate of hypotension that was evidenced only in the subgroups of patients receiving an infusion rate ⬎.01 g/kg/min or a bolus dose. A recent meta-analysis of five randomized trials (139 patients) undergoing cardiac surgery was powered sufficiently to demonstrate a significant reduction in postoperative peak release of cardiac troponin (WMD ⫽ 2.5 ng/dL [⫺3.86, ⫺1.14], p ⫽ .0003) and in time to hospi- Although this is the most comprehensive dataset so far assembled from clinical trials of levosimendan, the range of critical illness situations is largely restricted to cardiological settings. The dataset for sepsis is too small to draw conclusions about the relative or absolute merits of levosimendan vs. conventional inotropes in this setting. Our analysis included only two trials in interventional cardiology and does not explicitly address the situation of preemptive hemodynamic intervention to improve postoperative outcomes in moderate or high-risk surgical cases (119). Our conclusions about the relative superiority of levosimendan over conventional inotropes cannot be assumed to extend to that situation. We have reported previously (13) that the significant reduction in mortality and rate of myocardial infarction associated with levosimendan is achieved at the expense of a significant increase in the rate of hypotension (p ⫽ .02 vs. controls). This is a recognized feature of levosimendan and should be part of any risk-benefit calculation. Nonetheless, the present meta-analysis did not confirm a significant effect of the drug on hypotension. LOS was not corrected for mortality in most of the included studies, so in our results, LOS is not corrected for mortality. This may underestimate the real effect of levosimendan on LOS and its real impact on costs. Whereas a network meta-analysis including all available cardiac inotropes could have been envisioned, it was beyond the scope of our work. Finally, no formal test of agreement between reviewers was performed, since all divergences were solved with consensus as soon as evident. CONCLUSIONS This meta-analysis suggests that the use of levosimendan in lieu of usual therapies is associated with a significant reduction in mortality. Additional large, multicenter, randomized trials (120) powered to clinically relevant end points, Crit Care Med 2012 Vol. 40, No. 2 including mortality, will be needed to confirm these deductions about the clinical advantages of levosimendan over conventional inotropes. 9. ACKNOWLEDGMENTS We thank A. Mizzi, P. Prati, V. Ajello, G. Bruno, C. Gerli, V. De Santis, L. Corno, L. Tritapepe, G. Marino, and M. Zambon for their contribution on data extraction, sharing their expertise, and their valuable comments on the report. Their substantial assistance and support greatly favored the preparation of this paper. We also thank the primary and contact authors of the included studies who kindly provided additional details for this review. 10. 11. REFERENCES 12. 1. Bayram M, De Luca L, Massie MB, et al: Reassessment of dobutamine, dopamine, and milrinone in the management of acute heart failure syndromes. Am J Cardiol 2005; 96:47G–58G 2. Thackray S, Easthaugh J, Freemantle N, et al: The effectiveness and relative effectiveness of intravenous inotropic drugs acting through the adrenergic pathway in patients with heart failure-a meta-regression analysis. Eur J Heart Fail 2002; 4:515–529 3. Metra M, Eichhorn E, Abraham WT, et al: Effects of low-dose oral enoximone administration on mortality, morbidity, and exercise capacity in patients with advanced heart failure: The randomized, doubleblind, placebo-controlled, parallel group ESSENTIAL trials. Eur Heart J 2009; 30: 3015–3026 4. Abraham WT, Adams KF, Fonarow GC, et al: In-hospital mortality in patients with acute decompensated heart failure requiring intravenous vasoactive medications: An analysis from the Acute Decompensated Heart Failure National Registry (ADHERE). J Am Coll Cardiol 2005; 46:57– 64 5. Mebazaa A, Parissis J, Porcher R, et al: Short-term survival by treatment among patients hospitalized with acute heart failure: The global ALARM-HF registry using propensity scoring methods. Intensive Care Med 2011; 37:290 –301 6. Despas F, Trouillet C, Franchitto N, et al: Levosimedan improves hemodynamics functions without sympathetic activation in severe heart failure patients: Direct evidence from sympathetic neural recording. Acute Card Care 2010; 12:25–30 7. Papp Z, Csapó K, Pollesello P, et al: Pharmacological mechanisms contributing to the clinical efficacy of levosimendan. Cardiovasc Drug Rev 2005; 23:71–98 8. Follath F, Cleland JG, Just H, et al: Efficacy and safety of intravenous levosimendan compared with dobutamine in severe low- Crit Care Med 2012 Vol. 40, No. 2 13. 14. 15. 16. 17. 18. 19. 20. output heart failure (the LIDO study): A randomised double-blind trial. Lancet 2002; 360:196 –202 Moiseyev VS, Põder P, Andrejevs N, et al: Safety and efficacy of a novel calcium sensitizer, levosimendan, in patients with left ventricular failure due to an acute myocardial infarction. A randomized, placebocontrolled, double-blind study (RUSSLAN). Eur Heart J 2002; 23:1422–1432 Zairis MN, Apostolatos C, Anastasiadis P, et al: The effect of a calcium sensitizer or an inotrope or none in chronic low output decompensated heart failure: Results from the calcium sensitizer or inotrope or none in low output heart failure study (CASINO). J Am Coll Cardiol 2004; 43:A206 –A207 Mebazaa A, Nieminen MS, Packer M, et al: Levosimendan vs dobutamine for patients with acute decompensated heart failure: The SURVIVE Randomized Trial. JAMA 2007; 297:1883–1891 Packer M, Revive II Trial Investigators: REVIVE II: Multicenter placebo-controlled trial of levosimendan on clinical status in acutely decompensated heart failure. Circulation 2005; 112:3363 Landoni G, Mizzi A, Biondi-Zoccai G, et al: Levosimendan reduces mortality in critically ill patients. A meta-analysis of randomized controlled studies. Minerva Anestesiol 2010; 76:276 –286 Delaney A, Bradford C, McCaffrey J, et al: Levosimendan for the treatment of acute severe heart failure: A meta-analysis of randomised controlled trials. Int J Cardiol 2010; 138:281–289 Mebazaa A, Nieminen MS, Filippatos GS, et al: Levosimendan vs. dobutamine: Outcomes for acute heart failure patients on beta-blockers in SURVIVE. Eur J Heart Fail 2009; 11:304 –311 Cohen-Solal A, Logeart D, Huang B, et al: Lowered B-type natriuretic peptide in response to levosimendan or dobutamine treatment is associated with improved survival in patients with severe acutely decompensated heart failure. J Am Coll Cardiol 2009; 53:2343–2348 Cleland JG, Freemantle N, Coletta AP, et al: Clinical trials update from the American Heart Association: REPAIR-AMI, ASTAMI, JELIS, MEGA, REVIVE-II, SURVIVE, and PROACTIVE. Eur J Heart Fail 2006; 8:105–110 Gheorghiade M, Pang PS: Are BNP changes during hospitalization for heart failure a reliable surrogate for predicting the effects of therapies on post-discharge mortality? J Am Coll Cardiol 2009; 53:2349 –2352 Nieminen MS: Levosimendan compared with dobutamine in low output patients. Minerva Anestesiol 2003; 69:258 –263 Cleland JG, Takala A, Apajasalo M, et al: Intravenous levosimendan treatment is cost-effective compared with dobutamine in severe low-output heart failure: An analysis 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. based on the international LIDO trial. Eur J Heart Fail 2003; 5:101–108 Cleland JG, Ghosh J, Freemantle N, et al: Clinical trials update and cumulative metaanalyses from the American College of Cardiology: WATCH, SCD-HeFT, DINAMIT, CASINO, INSPIRE, STRATUS-US, RIO-Lipids and cardiac resynchronisation therapy in heart failure. Eur J Heart Fail 2004; 6:501–508 Coletta AP, Cleland JG, Freemantle N, et al: Clinical trials update from the European Society of Cardiology Heart Failure meeting: SHAPE, BRING-UP 2 VAS, COLA II, FOSIDIAL, BETACAR, CASINO and metaanalysis of cardiac resynchronisation therapy. Eur J Heart Fail 2004; 6:673– 676 Packer M, Colucci WS, Fisher L, et al: Development of a comprehensive new end point for the evaluation of new treatments for acute decompensated heart failure (results with levosimendan in the REVIVE-1 study). Abstr. J Card Fail 2003; 9:S61 Kota B, Prasad AS, Economides C, et al: Levosimendan and calcium sensitization of the contractile proteins in cardiac muscle: Impact on heart failure. J Cardiovasc Pharmacol Ther 2008; 13:269 –278 de Lissovoy G, Fraeman K, Teerlink JR, et al: Hospital costs for treatment of acute heart failure: Economic analysis of the REVIVE II study. Eur J Health Econ 2010; 11:185–193 Biondi-Zoccai GG, Agostoni P, Abbate A, et al: A simple hint to improve Robinson and Dickersin’s highly sensitive PubMed search strategy for controlled clinical trials. Int J Epidemiol 2005; 34:224 –225; author reply 225 Higgins JPT, Green S: Cochrane handbook for systematic reviews of interventions (v 5.0.2). Available at: http://www.cochranehandbook.org. Accessed January 4, 2011 Peters JL, Sutton AJ, Jones DR, et al: Comparison of two methods to detect publication bias in meta-analysis. JAMA 2006; 295: 676 – 680 Dear KBG, Begg CB: An approach for assessing publication bias prior to performing a meta-analysis. Statistical Science 1992; 7:237–245 Duval S, Tweedie R: Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in metaanalysis. Biometrics 2000; 56:455– 463 Review manager (RevMan) [computer program] version 5.0. Copenhagen: The Nordic Cochrane Centre, the Cochrane Collaboration, 2008. Available at: http://ims.cochrane. org/revman. Accessed January 4, 2011 Liberati A, Altman DG, Tetzlaff J, et al: The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009; 339:b2700 Akselrod B, Trekova N, Tolstova I, et al: Preoperative levosimendan administration: What is the vascular payment during anaes- 643 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 644 thesia? J Cardiothorac Vasc Anesth 2010; 24:S18 Avgeropoulou C, Andreadou I, MarkantonisKyroudis S, et al: The Ca2⫹-sensitizer levosimendan improves oxidative damage, BNP and pro-inflammatory cytokine levels in patients with advanced decompensated heart failure in comparison to dobutamine. Eur J Heart Fail 2005; 7:882– 887 Chamos C, Daidou T, Delis E, et al: The effects of levosimendan compared with milrinone in cardiac surgery patients. J Cardiothorac Vasc Anesth 2009; 23:S19 De Luca L, Proietti P, Celotto A, et al: Levosimendan improves hemodynamics and coronary flow reserve after percutaneous coronary intervention in patients with acute myocardial infarction and left ventricular dysfunction. Am Heart J 2005; 150: 563–568 De Luca L, Sardella G, Proietti P, et al: Effects of levosimendan on left ventricular diastolic function after primary angioplasty for acute anterior myocardial infarction: A Doppler echocardiographic study. J Am Soc Echocardiogr 2006; 19:172–177 Duman D, Palit F, Simsek E, et al: Effects of levosimendan versus dobutamine on left atrial function in decompensated heart failure. Can J Cardiol 2009; 25:e353– e356 Duygu H, Nalbantgil S, Zoghi M, et al: Comparison of ischemic side effects of levosimendan and dobutamine with integrated backscatter analysis. Clin Cardiol 2009; 32: 187–192 Harjola VP, Oikarinen L, Toivonen L, et al: The hemodynamic and pharmacokinetic interactions between chronic use of oral levosimendan and digoxin in patients with NYHA Classes II-III heart failure. Int J Clin Pharmacol Ther 2008; 46:389 –399 Jörgensen K, Bech-Hanssen O, Houltz E, et al: Effects of levosimendan on left ventricular relaxation and early filling at maintained preload and afterload conditions after aortic valve replacement for aortic stenosis. Circulation 2008; 117:1075–1081 Kasikcioglu HA, Uyarel H, Tartan Z, et al: Do calcium sensitizers affect right ventricular functions in patients with chronic heart failure? Int J Cardiol 2007; 118: 246 –248 Knez I, Schweiger S, Ovcina I, et al: Effects of Ca2⫹ sensitiser levosimendan on flow in internal thoracic and radial arteries in patients undergoing CABG–preliminary results. Abstr. Eur Heart J 2005; 26:527 Kurt IH, Yavuzer K, Batur MK: Short-term effect of levosimendan on free light chain kappa and lambda levels in patients with decompensated chronic heart failure. Heart Vessels 2010; 25:392–399 Lilleberg J, Nieminen MS, Akkila J, et al: Effects of a new calcium sensitizer, levosimendan, on haemodynamics, coronary blood flow and myocardial substrate utilization early after coronary artery bypass grafting. Eur Heart J 1998; 19:660 – 668 46. Moertl D, Berger R, Huelsmann M, et al: Short-term effects of levosimendan and prostaglandin E1 on hemodynamic parameters and B-type natriuretic peptide levels in patients with decompensated chronic heart failure. Eur J Heart Fail 2005; 7:1156 –1163 47. Parissis JT, Adamopoulos S, Antoniades C, et al: Effects of levosimendan on circulating pro-inflammatory cytokines and soluble apoptosis mediators in patients with decompensated advanced heart failure. Am J Cardiol 2004; 93:1309 –1312 48. Parissis JT, Adamopoulos S, Farmakis D, et al: Effects of serial levosimendan infusions on left ventricular performance and plasma biomarkers of myocardial injury and neurohormonal and immune activation in patients with advanced heart failure. Heart 2006; 92:1768 –1772 49. Parissis JT, Andreadou I, Markantonis SL, et al: Effects of Levosimendan on circulating markers of oxidative and nitrosative stress in patients with advanced heart failure. Atherosclerosis 2007; 195:e210 – e215 50. Parissis JT, Karavidas A, Bistola V, et al: Effects of levosimendan on flow-mediated vasodilation and soluble adhesion molecules in patients with advanced chronic heart failure. Atherosclerosis 2008; 197: 278 –282 51. Parissis JT, Panou F, Farmakis D, et al: Effects of levosimendan on markers of left ventricular diastolic function and neurohormonal activation in patients with advanced heart failure. Am J Cardiol 2005; 96:423– 426 52. Sonntag S, Sundberg S, Lehtonen LA, et al: The calcium sensitizer levosimendan improves the function of stunned myocardium after percutaneous transluminal coronary angioplasty in acute myocardial ischemia. J Am Coll Cardiol 2004; 43:2177–2182 53. Yilmaz MB, Karadas F, Erdem A, et al: Improvement in Doppler alternans in patients with severe heart failure: Levosimendan versus dobutamin. Int J Cardiol 2008; 125: 104 –106 54. Yilmaz MB, Yalta K, Yontar C, et al: Levosimendan improves renal function in patients with acute decompensated heart failure: comparison with dobutamine. Cardiovasc Drugs Ther 2007; 21:431– 435 55. Wang L, Cui L, Wei JP, et al: [Efficacy and safety of intravenous levosimendan compared with dobutamine in decompensated heart failure]. Zhonghua Xin Xue Guan Bing Za Zhi 2010; 38:527–530 56. Yilmaz MB, Yontar C, Erdem A, et al: Comparative effects of levosimendan and dobutamine on right ventricular function in patients with biventricular heart failure. Heart Vessels 2009; 24:16 –21 57. Nieminen MS, Cleland JG, Eha J, et al: Oral levosimendan in patients with severe chronic heart failure –the PERSIST study. Eur J Heart Fail 2008; 10:1246 –1254 58. Põder P, Eha J, Sundberg S, et al: Pharma- 59. 60. 61. 62. 63. 64. 65. 66. 67. 68. 69. 70. codynamics and pharmacokinetics of oral levosimendan and its metabolites in patients with severe congestive heart failure: A dosing interval study. J Clin Pharmacol 2004; 44:1143–1150 Branzi G, Malfatto G, Villani A, et al: Acute effects of levosimendan on mitral regurgitation and diastolic function in patients with advanced chronic heart failure. J Cardiovasc Med (Hagerstown) 2010; 11: 662– 668 Lehmann A, Kiessling AH, Isgro F, et al: Levosimendan in patients with acute myocardial ischaemia undergoing emergency surgical revascularization. Eur J Anaesthesiol 2008; 25:224 –229 Nanas JN, Papazoglou P, Tsagalou EP, et al: Efficacy and safety of intermittent, longterm, concomitant dobutamine and levosimendan infusions in severe heart failure refractory to dobutamine alone. Am J Cardiol 2005; 95:768 –771 Liu T, Li G, Xu G: Levosimendan may prevent postoperative atrial fibrillation through anti-inflammatory and antioxidant modulation. J Cardiothorac Vasc Anesth 2009; 23:757–758 Tasouli A, Papadopoulos K, Antoniou T, et al: Efficacy and safety of perioperative infusion of levosimendan in patients with compromised cardiac function undergoing open-heart surgery: Importance of early use. Eur J Cardiothorac Surg 2007; 32: 629 – 633 Dominguez-Rodriguez A, Samimi-Fard S, Garcia-Gonzalez MJ, et al: Effects of levosimendan versus dobutamine on left ventricular diastolic function in patients with cardiogenic shock after primary angioplasty. Int J Cardiol 2008; 128:214 –217 Duygu H, Nalbantgil S, Ozerkan F, et al: Effects of levosimendan on left atrial functions in patients with ischemic heart failure. Clin Cardiol 2008; 31:607– 613 Duygu H, Ozerkan F, Zoghi M, et al: Effect of levosimendan on right ventricular systolic and diastolic functions in patients with ischaemic heart failure. Int J Clin Pract 2008; 62:228 –233 Kivikko M, Lehtonen L, Colucci WS: Sustained hemodynamic effects of intravenous levosimendan. Circulation 2003; 107:81– 86 Samimi-Fard S, Garcia-Gonzalez MJ, Dominguez-Rodriguez A, et al: Effects of levosimendan versus dobutamine on long-term survival of patients with cardiogenic shock after primary coronary angioplasty. Int J Cardiol 2008; 127:284 –287 Levin RL, Degrange M, Porcile R, et al: The preoperative utilization of levosimendan (preoperative optimization) reduced mortality and low output syndrome after cardiac surgery in patients with low ejection fraction (EF⬍25%). Circulation 2007; 116:82 Momeni M, Rubay J, Matta A, et al: Levosimendan in congenital cardiac surgery: A randomized, double-blind clinical trial. Crit Care Med 2012 Vol. 40, No. 2 71. 72. 73. 74. 75. 76. 77. 78. 79. 80. 81. 82. 83. 84. J Cardiothorac Vasc Anesth 2011; 25: 419 – 424 Adamopoulos S, Parissis JT, Iliodromitis EK, et al: Effects of levosimendan versus dobutamine on inflammatory and apoptotic pathways in acutely decompensated chronic heart failure. Am J Cardiol 2006; 98: 102–106 Alhashemi JA, Alotaibi QA, Abdullah GM, et al: Levosimendan vs dobutamine in septic shock. J Crit Care 2009; 24:e14 – e15 Al-Shawaf E, Ayed A, Vislocky I, et al: Levosimendan or milrinone in the type 2 diabetic patient with low ejection fraction undergoing elective coronary artery surgery. J Cardiothorac Vasc Anesth 2006; 20: 353–357 Alvarez J, Bouzada M, Fernández AL, et al: [Hemodynamic effects of levosimendan compared with dobutamine in patients with low cardiac output after cardiac surgery]. Rev Esp Cardiol 2006; 59:338 –345 Alvarez J, Taboada M, Rodríguez J, et al: [Hemodynamic effects of levosimendan following cardiac surgery]. Rev Esp Anestesiol Reanim 2005; 52:389 –394 Barisin S, Husedzinovic I, Sonicki Z, et al: Levosimendan in off-pump coronary artery bypass: A four-times masked controlled study. J Cardiovasc Pharmacol 2004; 44: 703–708 Berger R, Moertl D, Huelsmann M, et al: Levosimendan and prostaglandin E1 for uptitration of beta-blockade in patients with refractory, advanced chronic heart failure. Eur J Heart Fail 2007; 9:202–208 Bergh CH, Andersson B, Dahlström U, et al: Intravenous levosimendan vs. dobutamine in acute decompensated heart failure patients on beta-blockers. Eur J Heart Fail 2010; 12:404 – 410 De Hert SG, Lorsomradee S, Cromheecke S, et al: The effects of levosimendan in cardiac surgery patients with poor left ventricular function. Anesth Analg 2007; 104:766 –773 De Hert SG, Lorsomradee S, vanden Eede H, et al: A randomized trial evaluating different modalities of levosimendan administration in cardiac surgery patients with myocardial dysfunction. J Cardiothorac Vasc Anesth 2008; 22:699 –705 Duygu H, Ozerkan F, Nalbantgil S, et al: Effect of levosimendan on E/E’ ratio in patients with ischemic heart failure. Int J Cardiol 2008; 123:201–203 Duygu H, Turk U, Ozdogan O, et al: Levosimendan versus dobutamine in heart failure patients treated chronically with carvedilol. Cardiovasc Ther 2008; 26:182–188 Eriksson HI, Jalonen JR, Heikkinen LO, et al: Levosimendan facilitates weaning from cardiopulmonary bypass in patients undergoing coronary artery bypass grafting with impaired left ventricular function. Ann Thorac Surg 2009; 87:448 – 454 Flevari P, Parissis JT, Leftheriotis D, et al: Effect of levosimendan on ventricular arrhythmias and prognostic autonomic in- Crit Care Med 2012 Vol. 40, No. 2 85. 86. 87. 88. 89. 90. 91. 92. 93. 94. 95. 96. 97. dexes in patients with decompensated advanced heart failure secondary to ischemic or dilated cardiomyopathy. Am J Cardiol 2006; 98:1641–1645 Fuhrmann JT, Schmeisser A, Schulze MR, et al: Levosimendan is superior to enoximone in refractory cardiogenic shock complicating acute myocardial infarction. Crit Care Med 2008; 36:2257–2266 García-González MJ, Domínguez-Rodríguez A, Ferrer-Hita JJ, et al: Cardiogenic shock after primary percutaneous coronary intervention: Effects of levosimendan compared with dobutamine on haemodynamics. Eur J Heart Fail 2006; 8:723–728 Husedzinoviæ I, Barisin S, Bradiæ N, et al: Levosimendan as a new strategy during offpump coronary artery bypass grafting: Double-blind randomized placebo-controlled trial. Croat Med J 2005; 46:950 –956 Ikonomidis I, Parissis JT, Paraskevaidis I, et al: Effects of levosimendan on coronary artery flow and cardiac performance in patients with advanced heart failure. Eur J Heart Fail 2007; 9:1172–1177 Järvelä K, Maaranen P, Sisto T, et al: Levosimendan in aortic valve surgery: Cardiac performance and recovery. J Cardiothorac Vasc Anesth 2008; 22:693– 698 Kleber FX, Bollmann T, Borst MM, et al: Repetitive dosing of intravenous levosimendan improves pulmonary hemodynamics in patients with pulmonary hypertension: Results of a pilot study. J Clin Pharmacol 2009; 49:109 –115 Lahtinen P, Pitkänen O, Pölönen P, et al: Levosimendan reduces heart failure after high risk cardiac surgery–a prospective, randomized, placebo-controlled trial. Eur Heart J 2009; 30:596 Leppikangas H, Tenhunen JJ, Lindgren L, et al: Effects of levosimendan on indocyanine green plasma disappearance rate and the gastric mucosal-arterial pCO2 gradient in abdominal aortic aneurysm surgery. Acta Anaesthesiol Scand 2008; 52:785–792 Levin RL, Degrange MA, Del-Mazo C, et al: Superiority of levosimendan over dobutamine in low cardiac output syndrome after aortic valve replacement. Circulation 2008; 118: E231 Levin RL, Degrange MA, Porcile R, et al: Preoperative use of calcium sensitizer levosimendan reduces mortality and low cardiac output syndrome in patients with aortic stenosis and left ventricular dysfunction. Circulation 2008; 118:E217 Levin RL, Degrange MA, Porcile R, et al: [The calcium sensitizer levosimendan gives superior results to dobutamine in postoperative low cardiac output syndrome]. Rev Esp Cardiol 2008; 61:471– 479 Levin R, Porcile RT, Degrange M: The intermittent infusion of levosimendan reduces mortality and readmissions in patients with advanced heart failure. Circulation 2009; 120:s865 Levin R, Porcile R, Salvagio F, et al: Levosi- 98. 99. 100. 101. 102. 103. 104. 105. 106. 107. 108. 109. 110. 111. mendan reduces mortality in postoperative low cardiac output syndrome after coronary surgery. Circulation 2009; 120:S987–S988 Lilleberg J, Laine M, Palkama T, et al: Duration of the haemodynamic action of a 24-h infusion of levosimendan in patients with congestive heart failure. Eur J Heart Fail 2007; 9:75– 82 Mavrogeni S, Giamouzis G, Papadopoulou E, et al: A 6-month follow-up of intermittent levosimendan administration effect on systolic function, specific activity questionnaire, and arrhythmia in advanced heart failure. J Card Fail 2007; 13:556 –559 Morelli A, De Castro S, Teboul JL, et al: Effects of levosimendan on systemic and regional hemodynamics in septic myocardial depression. Intensive Care Med 2005; 31:638 – 644 Nieminen MS, Akkila J, Hasenfuss G, et al: Hemodynamic and neurohumoral effects of continuous infusion of levosimendan in patients with congestive heart failure. J Am Coll Cardiol 2000; 36:1903–1912 Nijhawan N, Nicolosi AC, Montgomery MW, et al: Levosimendan enhances cardiac performance after cardiopulmonary bypass: A prospective, randomized placebo-controlled trial. J Cardiovasc Pharmacol 1999; 34:219 –228 Parissis JT, Papadopoulos C, Nikolaou M, et al: Effects of levosimendan on quality of life and emotional stress in advanced heart failure patients. Cardiovasc Drugs Ther 2007; 21: 263–268 Slawsky MT, Colucci WS, Gottlieb SS, et al: Acute hemodynamic and clinical effects of levosimendan in patients with severe heart failure. Study Investigators. Circulation 2000; 102:2222–2227 Trikas A, Antoniades C, Latsios G, et al: Long-term effects of levosimendan infusion on inflammatory processes and sFas in patients with severe heart failure. Eur J Heart Fail 2006; 8:804 – 809 Tritapepe L, De Santis V, Vitale D, et al: Levosimendan pre-treatment improves outcomes in patients undergoing coronary artery bypass graft surgery. Br J Anaesth 2009; 102:198 –204 Tritapepe L, De Santis V, Vitale D, et al: Preconditioning effects of levosimendan in coronary artery bypass grafting–a pilot study. Br J Anaesth 2006; 96:694 –700 Tziakas DN, Chalikias GK, Hatzinikolaou HI, et al: Levosimendan use reduces matrix metalloproteinase-2 in patients with decompensated heart failure. Cardiovasc Drugs Ther 2005; 19:399 – 402 Zemljic G, Bunc M, Yazdanbakhsh AP, et al: Levosimendan improves renal function in patients with advanced chronic heart failure awaiting cardiac transplantation. J Card Fail 2007; 13:417– 421 Ribeiro RA, Rohde LE, Polanczyk CA: Levosimendan in acute decompensated heart failure: Systematic review and metaanalysis. Arq Bras Cardiol 2010; 95: 230 –237 Bonaros N, Vill D, Wiedemann D, et al: 645 112. 113. 114. 115. 646 Major risk stratification models do not predict perioperative outcome after coronary artery bypass grafting in patients with previous percutaneous intervention. Eur J Cardiothorac Surg 2011; 39:e164 – e169 Annane D, Vignon P, Renault A, et al: Norepinephrine plus dobutamine versus epinephrine alone for management of septic shock: A randomised trial. Lancet 2007; 370:676 – 684 De Backer D, Biston P, Devriendt J, et al: Comparison of dopamine and norepinephrine in the treatment of shock. N Engl J Med 2010; 362:779 –789 Dickstein K, Cohen-Solal A, Filippatos G, et al: ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: The Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur J Heart Fail 2008; 10:933–989 Follath F: Newer treatments for decompen- 116. 117. 118. 119. 120. sated heart failure: Focus on levosimendan. Drug Des Devel Ther 2009; 3:73–78 Tavares M, Rezlan E, Vostroknoutova I, et al: New pharmacologic therapies for acute heart failure. Crit Care Med 2008; 36: S112–S120 Zangrillo A, Biondi-Zoccai G, Mizzi A, et al: Levosimendan reduces cardiac troponin release after cardiac surgery: A meta-analysis of randomized controlled studies. J Cardiothorac Vasc Anesth 2009; 23:474 – 478 Landoni G, Mizzi A, Biondi-Zoccai G, et al: Reducing mortality in cardiac surgery with levosimendan: A meta-analysis of randomized controlled trials. J Cardiothorac Vasc Anesth 2010; 24:51–57 Hamilton MA, Cecconi M, Rhodes A: A systematic review and meta-analysis on the use of preemptive hemodynamic intervention to improve postoperative outcomes in moderate and high-risk surgical patients. Anesth Analg 2011; 112:1392–1402 Levosimendan in High Risk Patients Undergoing Cardiac Surgery (HSR-LEVO). ClinicalTrials.gov Identifier NCT00994825. Available at: http://www.clinicaltrials.gov. Accessed January 5, 2011 APPENDIX Search strategy for PubMed, developed according to Biondi-Zoccai et al (26): (levosimendan OR simdax) AND (randomized controlled trial[pt] OR controlled clinical trial[pt] OR randomized controlled trials[mh] OR random allocation[mh] OR double-blind method[mh] OR single-blind method[mh] OR clinical trial[pt] OR clinical trials[mh] OR (clinical trial[tw] OR ((singl*[tw] OR doubl*[tw] OR trebl*[tw] OR tripl*[tw]) AND (mask*[tw] OR blind[tw])) OR (latin square[tw]) OR placebos[mh] OR placebo*[tw] OR random*[tw] OR research design[mh:noexp] OR comparative study[tw] OR follow-up studies[mh] OR prospective studies[mh] OR crossover studies[mh] OR control[tw] OR controls[tw] OR controlled[tw] OR prospectiv*[tw] OR volunteer*[tw]) NOT (animal[mh] NOT human[mh]) NOT (comment[pt] OR editorial[pt] OR meta-analysis[pt] OR practice-guideline[pt] OR review[pt])). Crit Care Med 2012 Vol. 40, No. 2