Patient Guide - Duke Raleigh Hospital
advertisement

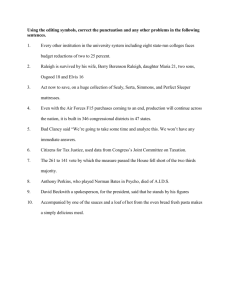
Patient Guide Duke Raleigh Hospital Welcome to Duke Raleigh Hospital At Duke Raleigh, our mission is to provide you extraordinary care. Since 1998, Duke Raleigh has been an important part of the Duke University Health System. Our affiliation with one of the country’s best health systems provides our patients with access to the most advanced technology and leading edge medicine available. In addition to surgical services, Duke Raleigh Hospital offers our patients state of-the-art services including the Duke Raleigh Cancer Center, Orthopaedic & Spine Center, Neurosciences, Cardiovascular Center, Wound Healing Center and Diabetes Center. Our services also include hospitalist and intensivist services, cardiac and pulmonary rehabilitation, a 24-hour emergency department, a pain clinic, an outpatient imaging center and patient education. Our award-winning nursing staff has been recognized with the North Carolina Nurses Association Hallmarks of Healthy Workplaces distinction and with MagnetTM designation by the American Nurses Credentialing Center. Duke Raleigh is fully accredited by The Joint Commission. From our beginnings in 1914 as Mary Elizabeth Hospital to today, our commitment to health care excellence continues to be our guiding principle. We strive to ensure that the care and services we provide exceed your expectations as a patient, a visitor or even a member of our staff. We value your input. When you get home, you may receive a patient satisfaction survey in the mail. This is your opportunity to tell us what we did well, and where we could use some improvement. However, if we are not meeting your expectations, please don’t hesitate to share your thoughts with the unit manager while you are here. We want to make sure you have a positive, nurturing experience and will do our best to correct any shortcomings on the spot. Duke Raleigh Hospital Mission, Vision and Values Mission: Duke Raleigh Hospital’s mission is to provide extraordinary care. Thank You for Choosing Duke Raleigh Hospital As our guest, please remember three things: U Your well-being is our primary concern. U Our staff will give you the compassionate, individualized care you need. U We will make sure your stay with us is as comfortable and pleasant as possible. At Duke Raleigh Hospital, we respect our patients. We recognize that you are an individual with unique values, beliefs and needs, and we understand that you want to make informed choices about your health care. Douglas B. Vinsel Please discuss your specific health care needs with our staff so that we may provide you the best possible care and attention and help you take advantage of the many resources and options available to you. Let us know how we can answer your questions and address your concerns. Sincerely, Douglas B. Vinsel President Duke Raleigh Hospital Vision: Duke Raleigh Hospital is recognized as the community leader for compassionate care with distinct centers of clinical excellence in oncology, orthopaedics, neurosciences and cardiovascular services. Values: UÊÊSafety: We believe that extraordinary begins with providing a safe environment. ÊUÊÊTeamwork: We value collaboration with our health care colleagues and work as a team to meet the needs of those who seek care. UÊRespect: We celebrate our accomplishments and take pride in our professional appearance and in the presentation of our hospital facility and campus. ÊUÊDiversity: We work in a culture that fosters respect for differences. ÊUÊService: We put our patients first as we seek to exceed the expectations of our customers with superior service, outstanding clinical care and unsurpassed responsiveness. UÊCommunity: We reach beyond our walls to engage in partnerships that improve the education and health care needs of our community. ÊUÊAchievement: We empower our employees and volunteers to achieve their full potential. Tobacco-Free Duke Raleigh Hospital is proud to be a tobacco-free campus. Smoking is prohibited on all Duke Raleigh Hospital property and inside all facilities. Thank you for helping us keep our hospital 100 percent tobacco-free. Welcome to Your Room Welcome to Duke Raleigh where your room is a place we expect you to receive extraordinary care. If, during your stay, you have any questions or concerns about anything in your room, please do not hesitate to ask anyone on your healthcare team for assistance. Thermostat. Every room has its own thermostat located on one of the room’s walls. To adjust the temperature, turn the dial at bottom to adjust while watching the numbers. Higher numbers mean hotter. Lower numbers Hospital Bed Side rails. Two side rails should be up at all times. Side rails that are raised are to help keep you from falling out of bed. Please leave them in place or ask your nurse if you may put one down. Fall alarms. If the light is lit, the alarm is on to alert the nurse of your interest in getting out of bed. Family members should never turn alarms off. Please ask your nurse the reason for the alarm if you have a concern. Bed wheel lock. Bed wheels should always remain locked. Bed controls. Please speak with your nurse before you raise or lower the head of your bed. Sometimes the doctor would like your head or back at a certain level. If okay with your nurse, you may use the controls as indicated. Your mattress. The mattress in your bed will inflate and deflate to keep you from getting a bed sore. mean cooler. Please adjust the room to your comfort level and feel free to ask for assistance when needed. Television. There are two ways to turn on your television: your remote control and your call bell box. To use your remote control, push the red power button on the bottom. To change the channels and the volume control, press the arrows. Please ask for assistance if you cannot locate your television remote. You may also operate your television via your call bell box. Push the on/off button to power your television and the up and down arrows for the channels. Please note, the volume should only be adjusted by using the remote control and not by using the controls directly on your television. If you require any further assistance, please let us know. Room phone. To operate your telephone, push the red button and wait for the dial tone. Dial “9” and then the seven digit local phone number. Long distance calls are generally not available. If you need to make a long distance call, please contact your nurse and she/he will assist you. Nurse call. Your call bell should be within your reach at all times. Remind your caregiver and visitors to always place the call bell box where you can reach it. Call bell boxes keep you in touch with us and enable your team to assist you by your simple push on the button. Always feel free to ask your caregiver for assistance while they are in your room. If you require assistance when a caregiver is not in your room, you may use either your call bell box by pushing the red “nurse hat” button or you may use the nurse call button located on the side of your bed. Feel free to ask your nurse to show you where these call buttons are located, should you need them. If you request has not been met within 15 minutes, do not hesitate to press the call button again. We want to be sure your needs are met. Lighting. There are many types of light in your room. This is to help your health care providers to clearly see you and for you to see them. It is for this reason that we keep a small light on in your room. Your nurse or assistant will try to find the best lighting so you can be safe while you rest. You may push the picture of the light bulb on your call bell box to turn on the light at the head of your bed. Reclining chairs. The chair in your room should not move and should remain locked in place. Please call for assistance if you notice that your chair is not locked in place. Do not attempt to get in or out of the chair that is not locked. Window. Please ask your health care team member to adjust the window shades to your comfort. Comfort (S H H H = Silent Hospitals Help Healing). Our goal is for you to rest. If you are being disturbed due to noise, dial 5683 (LOUD) on your room phone and tell operator that your rest is being disturbed due to noise. The operator will ensure your peace is restored. You may also request a white noise machine, music or ear plugs to help drown out noise. Hearing devices. If you have a hard time hearing, please ask your caregiver for a hearing amplifier. Computers. Each patient room is equipped with a computer. This computer is for staff use only. Your nurse will use this computer to document your care. For Your Safety Identification. During registration, you will have an ID band placed on your wrist. This ID band has information that is specific to only you and is a critical tool to help keep you safe. Make sure all information on your ID band is correct and, if it is removed for a procedure, that it is promptly replaced. If your healthcare provider does not check your ID band at every encounter, or if you think you’re being mistaken for another patient, please speak up. Hand washing. We care about your health and safety at Duke Raleigh. One of the ways we provide outstanding care for you is through practicing good hand washing. Proper hand hygiene is the very best way to prevent the spread of infections. Health care providers should wash their hands with soap and water or use alcohol hand cleaner prior to caring for you and before they leave your room. It is okay to ask us if we have washed our hands. Also, please have your visitors use the alcohol hand cleaner before and after visiting with you. Falls. A fall while in the hospital could delay your recovery or cause additional harm/injury. Please do not get out of bed without help, even if you feel okay. The main cause of falls in the hospital is toileting, so please do not attempt to go to the bathroom without assistance. Other important points to remember; Keep call button close to you — never climb over bed rails, never grab beds, chairs or tables to support your weight as they have wheels and may move. Medication safety. Medication errors are one of the most common health care mistakes. Patient identification is key to preventing some medication errors. Speak up if your health care provider does not check your ID band at every encounter, or if you think you’ve been mistaken for another patient. Please communicate if you experience any side effects from any of the medications you’ve been given. For your safety, it is important that your physician and nurse coordinate all of the medicine you take while you are in the hospital. It is also important that you educate yourself about the medications you take and why you take them—especially when you are going to receive a new medication. Make sure to tell your treatment team about allergies you have and all medications you are taking, including vitamins and supplements. It is a good practice to keep a list of all the medications you currently take, and keep it with you. Include the name, dosage and number of times a day you take the medication(s). If you brought any medications into the hospital with you please send them home with a loved one. Translation Services for Non-English Speaking Patients. Duke Raleigh provides multi-lingual interpretation for its non-English speaking patients and their families through CyraCom International. CyraCom provides multi-lingual interpretation twenty-four hours per day, seven days per week over the telephone. Any hospital telephone can access the CyraCom interpretation service at 1-800-481-3293 or please contact your nurse for assistance. Enlist a healthcare partner. Consider bringing a trusted family member or friend to the hospital to partner with you. With your permission, this person, your advocate, can ask questions that you may not think of while you are under stress and can help you remember the answers. Ask this person to stay with you, overnight if you like. Having someone else to listen with you and ask clarifying questions can be a big help when it comes to understanding information and remembering instructions once back at home. Condition HELP. Duke Raleigh Hospital knows that families are a vital part of the medical care team. We realize that they know the patient better than anyone, and we want them to partner with us to keep their family member safe while hospitalized. If a family member or any visitor becomes concerned about a significant change in a patient’s medical condition while at Duke Raleigh, they can call for our medical emergency team called Condition HELP. The Condition HELP team is a group of trained hospital staff who take care of medical emergencies and provides a safety net for our patients. Examples of reasons to call Condition HELP include—if the patient isn’t breathing well (too fast or too slow), you can’t wake them up, the patient complains of chest pain or a fast heart beat, the patient is confused, or just doesn’t look right to you. Call 3111 from any phone for Condition HELP. Leaving your room. For your safety, it is important that we know where you are at all times. We request that you not leave the patient care unit without telling your nurse. However, there are times when patients choose to leave the patient care unit to visit other areas of the hospital like the cafeteria, gift shop, or garden. If you leave your unit, please be sure to tell your nurse. If the nurse determines you are safe to leave the unit without an escort, you will be given a badge to wear that tells DRAH staff that you have permission to be off the nursing unit. The badges are color coded so staff will know which unit you came from. If you are seen in any area of the hospital or grounds without a DRAH escort or a badge, you will be stopped and returned to your room. Important Phone Numbers To call a Duke Raleigh Hospital extension from within the hospital, dial the last four digits beginning with “3,” “4” or “5.” To place a local call, dial “9” plus the number. For long distance, dial “0” and the hospital operator will assist you. Hospital Operator Patient Information Desk Public Safety Administration Business Services Cancer Center Care Ambassadors Case Management/Discharge Planning Diabetes Center Engineering Environmental Services The Guilded Lily Gift Shop 954-3000 954-3126 954-3911 954-3100 620-1299 862-5400 954-4444 954-3955 954-3616 954-3390 954-3731 954-3115 Imaging Inpatient Medical Services (Hospitalist) Nursing Administration Nutrition Pain Clinic Plaza Pharmacist (Outpatient Pharmacy) Rehabilitation Services Spiritual Care/Chaplain Volunteer Services Wellness Center Wound Healing Center Medical Records 954-3370 954-3965 954-3292 954-3161 954-3776 954-3921 954-3139 954-3268 954-3887 954-3174 862-5573 954-3150 (L to R) Rehabilitation Services, Patient Care Equipment Tech, Public Safety, Special Diagnostics, Case Management, Nursing Assistant, Nurse, Unit Secretary, Environmental Services, Pharmacy, Radiology, Maintenance, Volunteers Your Health Care Team Duke Raleigh has a team of professionals dedicated to providing you with extraordinary care. Your team includes: Medical Staff. The doctor who admits you is responsible for your care. Sometimes a hospitalist or intensivist, a doctor who cares for only hospitalized patients, will coordinate your care. Your doctor will discuss the plan for your care and answer questions about your condition. Nursing Staff. The nursing staff will care for you 24 hours a day. Your nursing staff includes registered nurses, licensed practical nurses, nursing assistants and the unit secretary. This team will collaborate with all members of your healthcare team to coordinate and carry out the plan for your care. The nurses will also provide you with education and be there as your advocate. Case Management. Our case management staff of nurse case managers and social workers will help to coordinate your care during your hospital stay and ensure you have a safe discharge plan. Recognizing Health Care Team Members Duke Raleigh Hospital recognizes that the hospital environment can be confusing and it is important that you identify members of the health care team easily. So in addition to our expectation that all team members introduce themselves to you, we have standard uniform colors to help you recognize your health care team members (pictured above and at left). Pictured Left: Dietary Hostess Environment Services (Housekeeping). It is our intention to provide a clean and comfortable environment for our patients. If you identify any housekeeping issues during your stay, please call 954-3730 or inform your nurse so the issue can be corrected as quickly as possible. Rehabilitation Services. This team will provide treatment to help you attain maximum physical function, a sense of well being and a personally satisfying level of independence. Volunteer Services. Many people from our community volunteer at Duke Raleigh every day. They provide a variety of services including newspaper, flower and mail delivery, escorting patients, visiting patients and information services at the front desk. Spiritual Care. Spiritual Care is available to patients, families, caregivers, physicians and staff members who seek ministries of growth, hope and healing. Our chaplains can be contacted by calling 954-3268 or asking your health care provider to make this contact on your behalf. Customer Service. Our Customer Service Center can help you with any questions you may have regarding our financial policies or billing. They are available Monday through Friday from 8 a.m. to 5 p.m. and can be contacted by dialing 919-620-1299 or 1-800-782-6945 (toll free). Special Diagnostics. Special Diagnostics provides all respiratory care services within the hospital. These services include breathing treatments and oxygen administration. In addition, the department provides cardiology services such as EKG’s, cardiac doppler studies and cardiac stress testing. Public Safety Officers. Public Safety Officers, one of the most visible staff in the facility, provide protection and assure a safe environment for patients, visitors and staff. Some of the many responsibilities and services Public Safety provides are to safeguard patient valuables, and hospital property and to provide directions and escorts on or around the campus. Dietary Host/Hostess. The dietary host or hostess provides the highest level of service to you during your stay and ensures your nutritional needs are being met based on the diet the physician has ordered to help you get well. Services provided include delivering your meals, assisting with filling out menus and working with hospital staff to customize your nutritional needs. Hospitalists and Intensivists Duke Raleigh Hospital What is a Hospitalist? Hospitalists are physicians who specialize in caring for patients in the hospital and generally practice only in the acute care setting. Most hospitalists are board certified in internal medicine, family practice or pediatrics; but some also have additional certification in specialties such as pulmonology, cardiology or critical care medicine. Because our hospitalist program operates on a 24 hours a day, 7 days a week schedule, our team of highly qualified, dedicated physicians works together to provide care. This means you will likely be seen by more than one physician during hospitalization, but the care will be well coordinated, and seamless. How does the Hospitalist communicate with my physician? At the time of admission to Duke Raleigh Hospital, your primary care physician contacts the hospitalists to inform them of your condition and treatment needs. The primary care physician is asked to provide as much information as possible about your illness and health background. This process is similar to what your physician does when referring you to a specialist. Upon discharge, written information will be forwarded to your physician’s office so he/she will have a record of your care and treatment during your hospitalization in order to resume your medical care. DRAH Hospitalists and Intensivists Dr. Charles Hodges (H) Medical Director Dr. Scott Gersh (H) Dr. Melinda Battaile (H) Dr. Brian Britt (H) Dr. Martin Estok (H) Dr. Lauren Holmes Griffin (H) Dr. Greg Ingram (H) Dr. Dean Morgan (H) Dr. Sanjay Narayanaswamy (H) Dr. Adeel Siddiqui (H) Dr. James Soldin (H) Dr. David Thurber (H) Dr. Asghar Yamadi (H) Dr. Amal Youssef (H) Dr. Michael Russell (I) Dr. Okoronkwo “OK” Ogan (I) The Critical Care Service at Duke Raleigh Hospital Modern critical care medicine is a process of managing complex medical and surgical conditions in patients that often have significant and multiple chronic illnesses. At Duke Raleigh Hospital, a multidisciplinary team of physicians, nurse practitioners (NPs), bedside nurses, pharmacists, respiratory therapists, physical therapists and dieticians are available around the clock to help you, your family member, and your admitting physician when you are a patient in the Intensive Care Unit (ICU). The Critical Care Service (CCS) will see each patient in the ICU at the request of the admitting physician or, rarely, will be the primary admitting service (for certain patients admitted through the emergency department, for example). The CCS also sees and makes recommendations for any patient who has been in the ICU for more than 24 hours. The core Critical Care Service is made up of board certified intensivists, physicians with special training and qualifications in the care of the critically ill, and advanced level nurse practitioners. At any given time, at least one member of the MD/NP team is in the hospital to care for patients on the Critical Care Service. Rounds are conducted on each CCS patient in the morning and involve the entire care team. Family members are encouraged to be available for rounds for interactive exchanges of information. If you have questions about your or your loved one’s condition or care plan, please ask to speak to a member of the CCS team, and we will do our best to get you a timely and accurate response. Likewise, any information you can provide regarding medical history and especially contact information for your or your loved ones’ primary care provider is extremely helpful. Please contact the Critical Care Service administrative office at 919-8625065 for any questions or comments. The MD/NP members of the Critical Care Service are: Michael W. Russell, MD; Sangeetta Joshi, MD; Okoronkwo “OK” Ogan, MD; Hili Metjian, MD; Jerry Hung, MD; Tara Sanders, RN, ACNP; Eric Reyer, RN, ACNP; Maria Sealey, RN, FNP; and Jill Tetterton, RN, ANP. Registration and Billing At Duke Raleigh Hospital, we understand that billing and payment for health care services can be confusing and complicated. The following information provides you with an overview of our registration and billing processes and what you can expect before and after your care. For your visit to the hospital. Duke Raleigh Hospital participates with most insurance companies, Medicare and Medicaid. Prior to your hospital visit, check with your employer or insurance company to see if you have access to health care services at Duke. Otherwise, you may be responsible for all or a large portion of your bill. Bring your complete health insurance information, including identification, insurance cards and authorization forms when you register. During the registration process, we will verify and update your information and ask you to sign forms. If you are a Medicare patient, you will be asked a series of questions regarding your status, including other insurances you may have and your retirement date. These questions are required by law and must be asked each time you visit us. Co-payments for physician and hospital care and other balances you may owe are due on the day you receive services. If your insurance company requires it, you may also be required to pay for estimated coinsurance or deductibles related to your care. In many cases, you will be notified prior to your visit if your estimated payment due is greater than $250. For your convenience, you may pay this balance by credit card prior to your date of service. If paying at the point of registration, we accept cash, checks, and all major credit cards. Please call your insurance company if you have questions regarding your co-payments, deductibles or coinsurance requirements. After your visit. Due to the many different physician groups and hospitals within Duke Medicine, you may receive more than one bill for your hospital visit. Bills from Duke Raleigh Hospital include but are not limited to services related to lab, radiology, and other testing services; operating room; emergency; pharmacy; medical supplies; inpatient room and board and other services provided by the hospital. Bills for physician services may be from Duke providers such as the Private Diagnostic Clinic or Duke Primary Care or you may receive separate bills from community-based physicians. If you receive a bill from a communitybased physician, you should contact these physicians directly with any questions. For questions regarding Duke Medicine related bill(s), please contact our Customer Service Center at 919-620-4555 or 1-800-782-6945 and request to speak with a Patient Account Representative. The center is open Monday through Friday from 8:00 a.m. to 5:00 p.m. You can also visit healthview.dukehealth.org to pay a bill online with a credit card, see your payment history and more. If you cannot pay your bill in full, please tell us and let us help. Our Patient Account Representatives and Financial Care Counselors will assist you with filling out applications for government sponsored programs, monthly payment plans and other financial assistance programs available for those patients who meet certain financial criteria. Additional information can be found in our “Paying for Your Health Care” brochure available in our registration areas. Patient Rights Access to care. Patients have the right to receive treatment at DRAH facilities without regard to race, color, religion, gender, sexual orientation, gender identity, national origin, disability or source of payment for care. You have the right to access advocacy or protective services with help from your health care team. You have the right to request that a family member, friend or physician be notified that you are under the care of this facility. Respect and dignity. Patients have the right to individualized care that respects your personal dignity, values and beliefs. You have the right to be cared for in an environment free from all forms of abuse and harassment and free from restraints that are not medically required. You have the right to privacy and confidentiality regarding your treatment, care and medical record. Communication and participation in decision making. Patients are encouraged to be involved in all aspects of their care. You will be educated by your health care team about your role in helping to facilitate delivery of safe, high quality medical care. You have the right to know the name and role of your health care providers and to request a second opinion. You have the right to expect your illness, treatment, pain, alternatives and outcomes explained to you in a language or method of communication you understand. You have the right to refuse any prescribed drugs, procedures or treatment, including life-sustaining treatments after you are informed of the consequences of refusing the recommended treatment. You have the right to know the policies that affect your care and treatment. You have the right to access your medical record and be informed of your financial obligations. You have the right to be informed about transfers to another facility or organization and be provided a complete explanation including alternatives to a transfer. You have the right to receive information about care needs at the end of your visit. Pain management. Patients have the right to have their pain recognized and addressed. You will receive education about your pain and pain relief measures. Your health care team is committed to providing an effective pain prevention and management plan. Advance directives. Patients have the right to receive information about advance directives (living will, health care power of attorney or mental health directives). Patients of legal age have the right to express their wishes regarding treatment at any time during their treatment course. Informed consent. You have the right to receive information, such as risks, benefits, and alternatives, about your treatment. In some cases, such as surgery or a research study, you may be asked to confirm in writing that you understand what is planned and agree to it. You have the right to decide if you want to participate in a research study. You may decline to participate in research without compromising your access to care, treatment, and services. You have the right to be informed of charges and receive counseling on the availability of known financial resources for health care. Visitation. You have the right to receive the visitors whom you designate, including, but not limited to, your spouse, a domestic partner (including a same sex domestic partner), another family member, or a friend. You also have the right to withdraw or deny your consent to visitation at any time. In the event you are unable to designate who can visit, the person you have designated as your “support person” can make that designation. Hospital visitation will not be limited or denied based on race, color, national origin, disability, religion, gender, sexual orientation, gender identity or expression. However, it may become clinically or otherwise reasonably necessary for a patient’s care, safety or well-being to impose restrictions on visitation. Reasons to limit visitation, if deemed necessary, may include but are limited to: interference with care interventions; infection control issues; interference with care of other patients; court order restricting visitation or contact; need for privacy or rest; need to limit the number of visitors during specific time period; disruptive, threatening or violent behavior by visitor; and visitation protocols for substance abuse or mental health treatment. Conflict resolution. While we strive to meet and exceed the expectations of our patients, staff and visitors, at times we may fall short. An important aspect of effective Duke Raleigh management is receiving, responding to and resolving all concerns in a courteous and timely manner. Your feedback helps us to continuously improve our care and delivery systems. If you have a concern or complaint, you may speak with any Duke Raleigh employee or volunteer and they will address your concern. If the individual can resolve the issue, he or she has the authority to do so. If the issue cannot be resolved on the spot, your concern will be communicated to the appropriate person for resolution. If you feel your concern is not adequately resolved, you may contact a Senior Administrator at 954-3100, the North Carolina Department of Health Service Regulation, or The Joint Commission. Sharing your concerns will not compromise your access to care, treatment or services. Patient’s Responsibilities Respect and dignity. Patients are responsible for acting in a manner that is respectful of other patients, staff and facility property. You are responsible to follow all rules and regulations established by Duke Raleigh. you are responsible for telling your health care team. Your health care team will explain the consequences of not following the prescribed plan of care. You are responsible for the outcomes of not following your plan of care. Communication and participation in decision making. Patients are responsible for communicating accurate and complete information about their medical history and insurance benefits. You are responsible for following your plan of care and for asking your health care team for clarification when you do not understand your plan of care. If you are unable or unwilling to follow the plan of care, Protecting others from spread of communicable illness. Family and friends who are sick or who have recently been exposed to communicable diseases such as influenza, TB or the chicken pox should not visit patients during their hospital stay. Visitors should be reminded to wash their hands before visiting patients. Patients are also encouraged to wash their hands frequently. Pain Management While you are a patient at the hospital, you may experience discomfort or pain. It may be due to disease, surgery or a procedure. Your health care team will work with you to keep you as comfortable as possible. The following information may help you prepare and understand how we work together to manage your pain or discomfort. Communicating pain. Everyone involved in your care works together to get your pain under control. Physicians plan and order treatment for pain, nurses carry out and monitor the treatment and you, the patient, must tell nurses and physicians when you are experiencing pain and about how your pain management plan is working. To more easily tell your caregivers about your pain, patients are asked to use the pain scale (at right). The scale helps physicians and nurses measure how well the treatment is working and to adjust the treatment plan if needed. By using the pain scale, caregivers will better understand your pain. 0 No Hurt 2 Hurts little bit 4 Hurts little more Financial obligations. Patients are responsible for meeting their financial obligation to the facility. 6 Hurts even more 8 Hurts whole lot 10 Hurts worse During Your Hospital Stay and At Home Patients can help control pain by: UÊ/>}ÊÜÌ ÊÞÕÀÊ« ÞÃV>ÊÀÊÕÀÃiÊ>LÕÌÊ ÜÊÕV Ê«>ÊÌÊiÝ«iVÌÊ UÊÊ/i}ÊÞÕÀÊ« ÞÃV>Ê>`ÊÕÀÃiÊ ÜÊÞÕÊ >ÛiÊLiÃÌÊ`i>ÌÊÜÌ Ê«>ÊÊÌ iÊ«>ÃÌÊ UÊÃ}Ê>LÕÌÊ`vviÀiÌÊ`ÃÊvÊi`ViÊÀÊÌÀi>ÌiÌÃÊÌÊÀiiÛiÊÞÕÀÊ«>Ê UÊÃ}ÊvÀÊ«>Êi`ViÊÜ iÊÞÕÀÊ«>ÊwÀÃÌÊLi}ÃÊ UÊÊ/i}ÊÞÕÀÊ« ÞÃV>Ê>`ÊÕÀÃiÊ ÜÊÕV Ê«>ÊÞÕÊ>ÀiÊ >Û}ÊÕÃ}ÊÌ iÊ«>ÊÃV>iÊ UÊÊ/i}ÊÞÕÀÊ« ÞÃV>Ê>`ÊÕÀÃiÊvÊÌ iÊÌÀi>ÌiÌÊ >ÃÊ i«i`ÊLÞÊÕÃ}ÊÌ iÊ«>ÊÃV>iÊ UÊÊ/i}ÊÞÕÀÊ« ÞÃV>Ê>`ÊÕÀÃiÊ>LÕÌÊ>ÞÊVViÀÃÊÞÕÊ >ÛiÊ>LÕÌÊÌ>}Ê«>Êi`V>ÌÊ UÊÊ/i}ÊÞÕÀÊ« ÞÃV>ÊÀÊÕÀÃiÊ>LÕÌÊ>ÞÊÃ`iÊivviVÌÃÊÌ >ÌÊÞÕÊ>ÞÊiÝ«iÀiViÊiÊ>ÕÃi>]Ê vomiting, weakness, hard stools (constipation), drowsiness, unsteadiness or dizziness Other Ways to Help Reduce Your Pain UÊÊii«ÊLÀi>Ì }p/>iÊwÛiÊ`ii«]ÊÃÜÊLÀi>Ì ÃÊÌ >ÌÊwÊÞÕÀÊV iÃÌÊ>ÊÌ iÊÜ>ÞÊÌÊÞÕÀÊÃÌ>V Ê UÊÊ,i>Ý>ÌpÃÌiÊÌÊ>ÊLÊÊÌ>«iÊÀÊÕÃV]Êi`Ì>ÌÊÀÊ«À>ÞiÀÊ UÊÊÃÌÀ>VÌpVÕÃÊÞÕÀÊ>ÌÌiÌÊÊÃiÌ }ÊiÃiÆÊÌiiÛÃ] radio, games and talking with others UÊÊÝiÀVÃipvÊÞÕÊ >ÛiÊ >`ÊÃÕÀ}iÀÞ]ÊvVÕÃÊÊÃÌ>Þ}Ê>VÌÛiÊ>`Ê}iÌÌ}ÊÞÕÀÊL`ÞÊÛ}Ê 10 Ways to Improve Communication While in the Hospital Good health care begins with good communication. However, research indicates that as many as half of adults in this country have problems understanding health information. There are many reasons for this. Often, health care professionals use terms that patients may not know. For example, you may use the word —“stomach ache” to describe how you feel and your doctor may use the word “gastroenteritis.” Often times patients report they cannot remember what their doctor has said after they leave. Taking steps to make sure you understand information your doctor has given you is important, as miscommunications and misunderstandings can lead to serious situations where people do not receive the medical treatment they need. The following steps can help improve communication between you and your doctor: Make a list. Write down any questions or concerns you have about your health and use it when discussing your healthcare with the doctors and nurses. Ask for definitions. If your doctor uses a word you do not understand, ask him or her to explain using plain language. Many words sound alike or have different meanings when talked about in health care. For example, whereas the word “negative” has bad implications outside a doctor’s office, when a test comes back negative, it is good news. It is okay to say you don’t understand. Know your goals. Ask your doctor to define your health care goals. For example, if your doctor tells you to check your blood pressure to make sure it is within normal range, you will need to know what “normal” means. Do the talking. After your doctor, nurse or other healthcare worker has finished explaining something to you, explain it back to them. This will help you remember it and help to make sure everyone understands the information in the same way. Picture it. A picture can be worth a thousand words. Ask your doctor to draw a picture or give you an illustration of the concept he or she is talking about. For example, a doctor might suggest certain exercises for someone with low back pain. A drawing may be far easier to understand than a spoken description. Slow down. If your health care provider speaks quickly, ask him or her to speak slowly so that you do not miss information. Follow-up. If you get home and cannot remember instructions, contact your doctor. If your physician offers communication via secure e-mail, you will have the added bonus of a written copy of the answer. (Regular e-mail does not provide complete privacy of your health information. If you have questions about whether your doctor uses secure e-mail, be sure to ask). Don’t be shy. If you have concerns regarding treatment, tell your health care provider. He or she may have information that will relieve your concerns, or there may be alternative treatments. Health care is a team effort. Make your doctor and nurses partners in your health with open communication. This is your health and it is important that you understand how to take care of it. Don’t come alone. Consider bringing a trusted family member or friend. Having someone else with you can be a big help when it comes to understanding information and remembering instructions once back at home. Ask for a recap. Ask your doctor to repeat the main points. Discharge planning. Duke Raleigh Hospital is committed to accommodating the needs of all our patients through well-coordinated and thoughtful care, including the transition Adapted from Journal of Patient Safety ©2006, Lippincott, Williams & Wilkins Questions for my Caregiver What should I know about my condition? What new medicines am I taking and what are they for? What side affects should I be aware of? When am I going home? What do I need to know now about going home? Other to home or your next place for care. Please remember that once your doctor has discharged you, there are still many things that have to be completed before you leave the hospital, including prescriptions, instructions about your home care and follow up appointments. Sometimes this process can take up to 3– 4 hours. Your nurse can give you the best estimate of the time you will actually be leaving. We know you are eager to go home and we thank you for letting us take care of you. Patient Comfort Cart Providing alternative options for relief The patient Comfort Cart was developed to help patients deal with various discomforts that can occur during a hospital stay. An assortment of items are available to assist with providing distractions from pain or discomfort, helping to reduce anxiety about pain, or providing tools to increase a patient’s comfort. Tips for Better Sleep How to get an Item from the Comfort Cart? Relieve stress. Stress may lead to insomnia. Light exercise, or meditation may help you relax. Try stretching (with a stretch band), yoga, massage or a stress ball to help you unwind. U A volunteer will visit most patient rooms Monday through Friday. Ask the volunteer for one of the complimentary items when he/she stops by with the cart. U Call a Care Ambassador at 954-4445 to request an item Monday through Friday, 8:00 a.m. to 4:00 p.m. After hours, or any time, ask your nurse to obtain an item for you. What is Available from the Comfort Cart? A patient or caregiver can select from a wide range of items to help increase patient comfort. U Distractions—Books, magazines, games, puzzles, ear plugs, spiral notebook U Relaxation—Relaxation CD’s, progressive muscle relaxation U Anxiety—Aromatherapy, breathing exercises U Pain—Visualization, cold and heat therapy U Stress relief—Sleep mask, lavender sachets, crossword, sudoku, word find, books, playing cards U Electronics—Sudoku game, solitaire game U Pain management—Stress balls, ear plugs, tea lights/votives, back scratchers U Inspirational—Pocket rosary, prayer shawl/blanket, Bibles Sponsored by the Duke Raleigh Hospital Guild. Additional toiletries and other comfort items are available for purchase in the Guilded Lily Gift Shop in the hospital lobby. SHHH… Silent Hospitals Help Healing Positive outlook. Keeping a gratitude journal might get you in a positive frame of mind for sleep, and over time give you a whole new outlook on life which is more positive and less stressed. Tick-tock don't watch the clock. Watching the clock may make you more anxious and less sleepy. Turn away from or cover the clock where you can’t see it. Clear your mind. Journaling by writing down your thoughts can help clear your mind and process emotions so you can sleep and rest more soundly. Request a Patient journal. Relaxation DVD. Try the relaxation DVD, Pacific Light. Program available on the education channel 154. DVD features scenery of the Pacific Ocean, CA and Oregon coasts. Soft music. Listening to soft music at bedtime may help you sleep better. Try classical music or a relaxation music DVD. Milk. Dairy products contain a sleep producing substance called tryptophan. Drink it warm or cold. But try not to drink after 8 p.m. to keep you from getting up to go to the bathroom. Turn off the lights. Monitors and other lights may give off too much light. Wear a sleep mask and close the privacy curtains and blinds to darken the room. Limit caffeine. Avoid caffeine (coffee, tea, soda) at least 4-6 hours before going to sleep. Studies show caffeine keeps people awake. Relax. Try taking a hot bath or doing some light reading. This will help you unwind, relax and drift off to sleep. Hot bath: sprinkle Epsom salt, baking soda and lavender oil. Soak for 20 minutes before bed. White noise. Too much noise may make it hard to fall asleep. Try wearing ear plugs or turn on some “white noise” such as the sound of a fan running (available on CD or white noise machine for your room) to drone out unwanted noise. Check the thermostat. The ideal temperature for most people to fall and stay asleep is between 68 –72 degrees Fahrenheit. Each patient room is equipped with its own thermostat. Stop eating. Limit eating 3–4 hours before going to sleep. This may prevent digestion problems which can interfere with your sleep. Fragrances. Lavender and chamomile scents can be calming and tranquilizing. Try body wash, room spray, sachets, or pillows. Sunshine. Try to get plenty of sunshine in the morning by sitting close to a window. Keep the blinds open and lower the lights at bedtime. If you find you cannot rest because of hospital noise, please call LOUD (Extension 5683). Your confidential call will be handled quickly by one of our friendly operators. Items in bold are available on the Comfort Cart. Additional rest and relaxation items for purchase can be found in the Guilded Lily Gift Shop. For Our Visitors Visiting hours. Regular visiting hours at Duke Raleigh Hospital are 8:00 a.m. until 9:00 p.m. We appreciate your assistance in maintaining a peaceful, healing environment during “quiet time”, when visitation is not permitted in ICU and PCU: 2:00 p.m. to 4:00 p.m. and 2:00 a.m. to 4:00 a.m. daily. If you are wishing to stay with a patient overnight, you must obtain a visitor’s badge from the nurse’s station where the patient is located. Overnight visitors must be at least 18 years of age and must renew privileges each night. Visitors play an important role in a patient’s recovery, but the health and well being of our patients come first. Please do not visit a patient if you have a fever, severe cold or flu or any other illness. We ask that you limit visitors to two at a time and stays should be brief so others may visit, but most importantly, so your relative or friend can rest. Children. Children are welcome at Duke Raleigh. We ask that parents/guardians supervise their children at all times. Please do not bring sick children to visit. Children may not spend the night with a patient in the hospital. If you are scheduled for all-day tests in radiology or any other department, please do not bring your children with you. Mail & flowers. Mail and flowers should be addressed to patients in care of Duke Raleigh Hospital, 3400 Wake Forest Road, Raleigh, NC 27609. Please include the patient’s full name and return address. Patients in ICU cannot receive flowers, balloons or gift baskets. Cards, however, are welcomed and encouraged. Flowers and mail received after discharge will be redirected to the patient’s home address. Security & safety. Duke Raleigh Hospital is committed to providing a safe and secure environment for all patients, visitors, physicians and staff. However, you should be alert to your surroundings and notify the Public Safety Department at 3911 of any unusual situations. Public Safety shuttle service. The Duke Raleigh Hospital Public Safety Department offers a shuttle service for employees, patients and visitors to enhance safety. The shuttle service provides transportation to and from all campus buildings and parking lots. To request the campus shuttle service, call public safety at 954-3164. Valuables. Patients and visitors should leave valuables such as jewelry, cash and credit cards at home as Duke Raleigh will not be responsible for personal items. Public Safety, however, can assist you in placing any valuables in the hospital safe during your stay. You must call Public Safety directly or ask your nurse to contact them on your behalf. Cellular phones & electronic devices. Please do not use cellular phones or other electronic devices near ICU, Telemetry or the Emergency Department. The Guilded Lily gift shop. Visit The Guilded Lily for that little “something special” to brighten someone’s day. The shop is ready to meet any gift giving need, from flowers, candy and magazines to jewelry, gift cards and home and garden decor. The shop is conveniently located in the front lobby of the hospital. Café hours and offerings. Located on the first floor of Duke Raleigh Hospital, the hospital café provides a variety of dining options for employees and visitors. Visit the hospital café during the following hours of operation: Weekday Hours Breakfast 6:30 a.m.–10:00 a.m. Lunch/Dinner 11:00 a.m.–7:30 p.m. Weekend Hours Breakfast 7:30 a.m.–10:00 a.m. Lunch 11:30 a.m.–2:00 p.m. Dinner 5:00 p.m.–6:30 p.m. Vending machines. Vending machines are located inside the hospital dining room on the first floor and outside of the Same Day Surgery side entrance also on the first floor. Duke Raleigh Gardens. The Duke Raleigh Gardens are located adjacent to Medical Office building 7 and offer a unique quiet haven for patients, visitors and employees. This peaceful retreat includes plants native to North Carolina, walking paths and tranquil nooks for sitting and resting. Banking. There is one automated teller machine located in the Duke Raleigh Café. Internet access. Duke Raleigh Hospital is pleased to provide free wireless internet access for our patients and visitors. CarePages. Duke Raleigh Hospital is pleased to provide CarePages websites as a benefit to families and their loved ones. Through free, personalized CarePages websites, member can create their own community of hope. In just a few easy steps, you can begin to share your journey with others. To create a CarePages website, please visit CarePages.com/dukehealth and click on “create a CarePages website” at the top of the page. Nutrition Services Welcome. All of us in Food and Nutrition Services extend a warm welcome to you. Our staff is available to visit with you to discuss any questions that you may have regarding food and nutrition services. We do want your stay with us to be as positive and comfortable as possible. Please call us at 954-3161 with any questions or concerns you have regarding our services. Information about your diet. During the course of your hospital stay, your diet order may change several times. This can be due to tests, surgery, or your clinical course of treatment. Diets are ordered by your physician and provided by the Food and Nutrition Services Department. This brochure provides you some basic information about your current diet and any other diet you may be on during your hospital stay. Please be aware that some medications may alter the taste of your food. If you have any dietary or nutritional needs, please contact your dietitian. We will be glad to assist you. Diet General Indications Foods Allowed Foods to Avoid Rest the GI tract None All Clear Liquid diet Pre- or post-operative, GI disturbances Broths, gelatin, clear juices (apple, grape, cranberry), clear soda, Popsicles, tea All other foods Full Liquid diet Pre- and post-operatively, GI disturbances All foods on clear liquid diet, strained cereals, milk, pudding, ice cream, health shakes All other foods Regular General diet All None Heart Healthy, Low Fat / Low Cholesterol, Sodium controlled diet Prevent fluid retention, prevent elevations in fat and cholesterol blood levels Foods prepared without salt or excess fat, breads and cereals, fresh fruits & veggies, lean meats and reduced fat dairy products Highly processed foods such as canned soups, processed meats (bacon, ham, sausage), fatty meats, table salt, whole milk, butter, ice cream and rich desserts Carb-controlled, Diabetic diet Control blood sugar levels related to diabetes, help achieve or maintain a desirable weight Foods prepared without added sugar, fat, or sodium, unsweetened cereals, unsweetened canned fruits, diet gelatin, diet soda, sugar substitutes Cakes, candies, regular sodas, fruit drinks, gelatin, sherbet, high fat foods, processed meats Renal diet Restricts protein, sodium, and potassium; mainly pre- and post-dialysis patients Limited portions of protein, no more than one serving of milk daily canned fruits, rice, noodles, and sugar candies Fruits and veggies high in potassium (tomatoes, banana, oranges, potatoes), excess servings of protein foods such as meat, dairy products, processed meats and salt Soft Diet Prevent or reduce GI stress Soft and bland foods, canned fruits, cooked vegetables, white breads, cream/broth soups Fresh/raw fruits and vegetables (except bananas), nuts, fried and highly seasoned foods Pureed diet For patients who have chewing and/ or swallowing problems Pureed meats, vegetables, fruits, cereals, strained cream, soup, ice cream, pudding, custard Solid foods, highly seasoned foods Fluid restricted diet Fluids are restricted to prevent excess fluid retention Any fluid so long as it does not exceed total amount of fluid allowance per day Any fluid that exceeds the total amount of fluids allowed per day Sodium-controlled diet Sodium is restricted to prevent excess fluid retention and help control high blood pressure Unsalted crackers, low sodium soups, fresh fruits, vegetables, and meats, foods prepared without added salt Highly processed foods such as canned soups, processed meats (bacon, ham, sausage), biscuits, and table salt or" NPO You May Prefer Menu Your physician has ordered a diet for you that best fits your nutritional needs and aid in your recovery. Because of this, certain items may not be available. Your selection will be provided if allowed by your current diet order. To Start" Chicken, Beef, or Vegetable Broth (0) Cream of Chicken Soup (10 gm) Cream of Mushroom Soup (10 gm) Vegetable Beef Soup (14 gm) Side Garden Salad (0) Italian · 1000 Island · French · Ranch Main Courses" Chef Salad (22 gm) Fresh Fruit & Cottage Cheese Plate (32 gm) Pizza Cheese or Pepperoni (46 gm) Hamburger or Cheeseburger (25 gm) Veggie Burger (34 gm) Grilled Chicken Sandwich (31 gm) Hot Dog (19 gm) Cream of Wheat (20 gm) Peanut Butter & Crackers (24 gm) Cottage Cheese (5 gm) Assorted Yogurt (15 gm) Celery & Carrot Sticks (0 gm) Potato Chips (17gm) Apple (25 gm) · Banana (27 gm) · Orange (22 gm) Sandwiches)" (Sandwiches (25 gm unless stated otherwise) Turkey · Ham · Cheese · Tuna Salad Grilled Cheese · Chicken Salad Peanut Butter & Jelly (35 gm) White · Wheat Mayonnaise · Mustard Lettuce · Tomato Lighter Choices" Biscuit (25 gm) Bagel w / Cream Cheese (32 gm) Cheerios (12 gm) · Rice Krispies (16 gm) Corn Flakes (18 gm) · Granola (52 gm) Raisin Bran (27 gm) Grits (22 gm) or Oatmeal (19 gm) Sweets" Gelatin(19 gm) · Diet Gelatin (2 gm) Pudding Vanilla or Chocolate (25 gm) Ice Cream Vanilla or Chocolate (14 gm) Cookies Chocolate Chip, Sugar (48 gm) Applesauce (21 gm) Hot Chocolate (23 gm) Lact-Aid Milk (13 gm) Soy Milk (10 gm) Chocolate Milk (28 gm) Buttermilk (12 gm) To Order" Please call x 3161 from your room phone. *For those patients who are diabetic, the carbohydrate content of the items a part of your diet are located in the parentheses. This will assist you in making meals selections that are our diet. TIGR Patient Education Videos Program Guide Welcome to your Patient Video Education Service How to view your video. Dial 4966, you will be told: Press 1 for English Instructions or Press 2 for Spanish Instructions. You will be asked: Which video do you want to view? Using the telephone keypad, enter the 3 numbers of the video you have chosen. TIGR will tell you which channel to watch. For the following areas, please use the staff ID and passwords to access the TIGR video system. (These areas do not have bedside patient phones.) Staff ID Password ICU 111111# 1111# ED 333333# 3333# SDS 444444# 4444# Radiology 555555# 5555# The Diabetic Education Channel Line Up Taking Insulin Making Lifestyle Changes Basic Skills for Controlling Diabetes Preventing Diabetic Foot Ulcers Video Title Video Time 300 Introduction to Heart Disease Risk Factors (15:00) 301 Secondary Prevention of Heart Disease (CC) (19:00) 302 Atrial Fibrillation (12:00) 303 Coronary Angiography & Angioplasty 2nd Ed (CC) (15:00) 305 (CHF) Taking Care of Your Heart (14:00) 306 Spanish: (CHF) Taking Care of Your Heart (14:00) 307 Living with Your Pacemaker (14:00) 308 Understanding Pacemakers: Pre-implantation (18:00) 309 The Heart of the Matter: Living with your ICD (11:00) Medications # Video Title Video Time 310 Coumadin Therapy & You (2008) (18:00) 311 Lovenox: Learning the Convenient Steps (2007) (12:00) 8:00, 10:00 312 Staying Active and Healthy with Blood Thinners (2009) (CDC) (15:00) PM 12:00 noon, 2:00, 4:00, 6:00, 10:00 313 (15:00) AM 8:30, 10:30 Spanish: Staying Active and Healthy with Blood Thinners (2009) (CDC) PM 12:30, 2:30, 4:30, 6:30, 8:30 AM 9:00, 11:00 PM 1:00, 3:00, 5:00, 7:00, 9:00 AM 9:30, 11:30 200 Taking Insulin (20:00) PM 11:30, 3:30, 5:30, 7:30, 9:30 201 Spanish: Taking Insulin (20:00) 202 Making Lifestyle Changes (2008) (19:00) 203 Spanish: Making Lifestyle Changes (2008) (19:00) Video Time 204 Basic Skills for Controlling Diabetes (2008) (12:00) 205 Spanish: Basic Skills for Controlling Diabetes (2008) (12:00) 206 Preventing Diabetic foot Ulcers (2008) (18:00) 207 Spanish: Preventing Diabetic foot Ulcers (2008) (18:00) Diabetes # Video Title 100 Duke Medicine: Partners In Safety: Keeping You Safe (2008) (12:00) 101 Duke Medicine: (Spanish) Partners In Safety: Keeping You Safe (2008) (12:00) 102 Hand Hygiene Saves Lives (2006) (5:29) 103 Spanish: Hand Hygiene Saves Lives La higiene de las manos salva vidas: (2006) (5:31) 104 Partners in Care: Preventing Falls (11:00) 105 Spanish: Partners in Care: Preventing Falls (11:00) Oncology # # AM Patient Admission # Cardiology Video Title Video Time 110 Controlling Cancer Pain (12:00) 111 Cancer Clinical Trials (19:00) 112 Zometa and Bone Metastasis 10:00 (10:00) 113 Welcome to Duke Oncology Video (12:00) Video Title Video Time Respiratory/Pulmonary # Video Title Video Time 400 COPD: Chronic Obstructive Pulmonary Disease (17:00) 401 Breathing Training & Pulmonary Illness (10:00) 402 Smoking: Getting Ready to Quit (15:00) 403 Guide to Stop Smoking (15:00) 404 Spanish: Guide to Stop Smoking (15:00) 405 Pleurx Chest Drainage (10:00) 406 Spanish: Pleurx Chest Drainage (10:00) 407 Xolair: Introduction (18:00) General Surgery Neurology/Orthopedics # Video Title Video Title Video Time Video Time 500 Stroke (2008) (10:00) 700 Coloplast: Life After Your Ostomy (2007) (11:00) 501 Scoliosis: Dr. H. Hey (2007) lecture (45:00) 701 Spanish: Coloplast: Life After Your Ostomy (2007) (11:00) 702 Convatec: Sur fit Natura: Ostomy Self Care Guide (15:00) 703 Spanish: Convatec: Sur fit Natura: Ostomy Self Care Guide (15:00) 704 Convatec: Active Life Self Care Ostomy Guide (2006) (12:00) 705 Ostomy Supplies & Discharge Planning (2008) (14:00) 706 Living With An Ostomy (2009) United Ostomy Associations of America (15:00) 707 KCI-NPWT, The Active VAC Home Unit (20:00) 708 Spanish: KCI-NPWT, The Active VAC Home Unit (20:00) 709 Sensura Coloplast Ostomy / Urostomy Instructions (11:00) 710 Hollister Ostomy Education Modules 8-19 (How to use a pouching systems) (34:00) 711 Hollister Ostomy Education modules 1-7 (Which pouching system is right for you?) (18:00) General Medicine # Video Title Video Time 600 Adult Male: Intermittent Self Catheterization (2008) (14:00) 601 Adult Female: Intermittent Self Catheterization (2008) (14:00) 602 Venous Leg Ulcers: A guide for Patients and Caregivers (2008) (21:00) 603 Spanish: Venous Leg Ulcers: A guide for Patients and Caregivers (2008) (21:00) 604 Pressure Ulcers: What Caring People Need to Know (2008) (14:00) 605 Tube Feeding at Home: The Road Ahead (Abbott-2009) (32:00) 606 Tube Feeding at Home: Tube Feeding Techniques (Abbott-2009) (32:00) ARTS Channel Selections Video Title Relaxation and Pain Reduction Video Title 904 Pacific Light Video: for relaxation and stress reduction Video Time (36:00) Video Time 900 Carolina Ballet Presents “Monet Impressions” n/a 901 Carolina Ballet Presents “Innovations” n/a 902 Carolina Ballet Presents n/a 903 Carolina Ballet Presents “Swan Lake” n/a TIGR Patient Education Videos Highlights Patient Safety Video. Plays continuously on Channel 46. This video shows how you and our staff together, make your stay a safe one. The Diabetic Education Channel. Plays continuously on Channel 48. A must see for any patient or family member dealing with diabetes. The ARTS Channel 45. Featuring “The Carolina Ballet.” Video selections 147 thru 150. Pacific Light: This award winning stress reduction-relaxation video successfully alleviates acute fears and anxiety. Video Selection #154. Experience the power of healing peace. Tim Janis’ In Room Symphony. Plays continuously on channels 51 & 52. A relaxing blend of music and picturesque videos of the American landscape, original music by the award winning composer Tim Janis. Viewing And Listening TV And Music Channel Guide TV Channel Guide XM Music Channels Channel Program Channel Program 2 WLFL – 22 41 CNN Headline 3 WRAL – 5 42 The Weather Channel 4 WUNC – 4 43 CNBC 5 n/u 44 MSNBC 6 WNCN – 17 45 TIGR Channel—1 Pt Ed 7 WKFT – 40 46 TIGR Channel—5 Pt Ed 8 n/u 47 TIGR Channel—2 Pt Ed 9 WTVD – 11 48 TIGR Channel—6 Pt Ed 10 CNN 49 TIGR Channel—3 Pt Ed 11 n/u 50 TIGR Channel—7 Pt Ed 12 UPN – 28 51 TIGR Channel—4 Pt Ed 13 WRAZ – 50 52 TIGR Channel—8 Pt Ed 14 Oxygen 53 F/X 15 Nickelodeon 54 Game Show Network 16 CCSPAN 55 Logo TV 17 CSPAN 2 56 Military Channel 18 Univision 27 NFL Network 19 Galavision 58 ESPNU—College Sports 20 E! Entertainment 59 CSTV—College Sports 21 Fuel TV 60 ESPN 22 G4 61 ESPN 2 23 Animal Planet 62 ESPNews 24 Sci-Fi 63 ESPN Classic 25 USA 64 Speed Channel 26 TNT 65 TV One 27 A&E 66 SOAP Network 28 ABC Family 67 TV Land WE—Womens 29 History Channel 68 30 Discovery 69 Comedy Central 31 Discovery Health 70 Current TV 32 National Geographic 71 Fox News Channel 33 The Science Channel 72 Lifetime 34 Bloomberg 73 MTV 35 Cartoon Network 74 MTV 2 36 TBS 75 VH 1 Classic 37 BET 76 VH 1 Classic 38 AMC 77 Court TV 39 TLC 40 Spike Channel Description 78 BigTracks From mullets to air guitars, Big Tracks picks up where Top Tracks leaves off. . . these are the biggest classic rock hits from the mid 70s through the early 90s. 79 Bluesville Bluesville is like a beginning course in art history. We play music of the forefathers and mothers from the 20s and 30s and we play the most contemporary blues acts of today, without forgetting all the great artists in between. 80 Highway 16 Highway 16 is your home for Today’s Top Country Hits featuring the latest from country music’s biggest stars and hot new artists. You’ll also hear in-depth, exclusive interviews with all of today’s hit makers, including XM World Premieres of new album releases and intimate introductions to hot country newcomers! 81 Spirit Glory is what gospel is all about . . . the glory of its inspirational message and the sheer glorious sound of the music. Let your heart soar with your favorite gospel recordings of all time on Spirit. 82 The Blend A great blend of music from the 70s through today... nothing too sleepy and never any rap or hard rock, The Blend plays the biggest superstars of pop music from the past 30 years...it’s the musical soundtrack of your life. 83 The Groove R&B is the international language of partying and The Groove goes back in the day every day with all the great R&B headliners from the mid 70s through the 80s. You’ll hear a great mix of R&B, funk, dance, and party music along with some songs you forgot you knew. 84 The Heart The Heart plays the biggest love songs and lite rock favorites from the 60s through today. This is the perfect place to relax, unwind, and lose the stress. 85 Watercolors Cool, Contemporary Jazz instrumentals, and hip vocals create a muted musical backdrop of sophistication on Watercolors. These groovy sounds expand the boundaries of smooth to not only seduce and relax but to engage and inspire. 86 XM Classics All genres and all eras of classical music are offered in a style that mixes unassuming authority with genuine friendliness and enthusiasm. XM Classics strives to inform, entertain and inspire, believing without apology that music is one of the greatest gifts that humankind has bestowed upon itself. 87 XM Pops XM Pops is classical music for ever one . . . the classical music you know, even if you don’t think you know classical music. These are the biggest names in classical music history, and their best pieces of music. Entertainment My Medication List For your safety keep this form current. Always bring the list with you to all doctor and hospital visits or anytime you go for tests. Name _________________________________________________________________________________________________ Doctor ___________________________________________________________ Phone _______________________________ Pharmacy __________________________________________________________ Phone _______________________________ IMMUNIZATION RECORD (Date last received for the following) Date Last Received Pneumonia Vaccine Date Last Received Hepatitis Vaccine Date Last Received Tetanus Date Last Received Other Date Last Received Flu Vaccine Date Last Received Other ALLERGIES AND REACTIONS (Please describe) Allergic to: Describe Reaction List all medicines you are currently taking: prescription and over-the-counter medications. Examples: aspirin, vitamins, herbs, oxygen, inhalers. Include medications taken as needed. Name of Medication Date Started Dose (mg, drops, etc) When Taken Reason for Taking S L E E P T A T S O M R E H T M N D S Y Y T I S R E V I D A T C E P S E R I E T V O L U N T E E R Y R A T E I D E S C I C O U R T E S Y S E R V I C E I N C N N K R O W M A E T C O M F O R T C I H A U F C N O I T A C I N U M M O C A H A R M A Y R D T H M E O I F S S A P S S I I H T O O A N U L P S I A E S T K T I E C E E J N P L T I O S N U R G E G A R M O C puzzle Time Medication Volunteer Admission Comfort Discharge Housekeeping Safety Communication Teamwork Sleep Respect Discharge Diversity Sunshine Service Relax Community Fragrances Achievement Nurse Thermostat Patient Hospitalist Courtesy Dietary T N E M E V E I H C A E S R U N S M F J e Duk icine e M da Plaz e Duk igh e Ral ens d Gar Registra tion/ Same D ay Surg ery Public Safety Shuttle Service The Duke Raleigh Hospital Public Safety Department offers a free shuttle service for patients and visitors to enhance safety. The shuttle service provides transportation to and from all campus buildings and parking lots. To request the campus shuttle service, call public safety at 954-3164. 3400 Wake Forest Road Raleigh, NC 27609-7373 dukeraleighhospital.org 1305 Building Outpatient Services at Duke Raleigh Hospital Duke Raleigh Hospital offers a variety of outpatient services conveniently located on our campus: Duke Raleigh Hospital is the first hospital in North Carolina to receive the Hallmarks of Healthy Workplaces designation by the North Carolina Nurses Association Professional Practice Advocacy Coalition (NCNA). The nursing recognition is given to facilities that have developed healthy workplaces for nursing staff and advocate nursing involvement in all facets of the organization to provide the highest level of patient care. Duke Raleigh Hospital has achieved MagnetTM designation for excellence in nursing by the American Nurses Credentialing Center (ANCC). Only 5 percent of the nation’s hospitals have earned this designation, the highest level of national recognition to health care organizations that demonstrate sustained excellence in nursing care. Duke Raleigh Cancer Center: 919-862-5400 Duke Raleigh Cancer Center provides state-of-the-art care that’s also friendly, convenient, and easily accessible. Services include medical oncology, radiation oncology, gynecologic oncology, surgical oncology as well as support services. Diabetes Center: 919-954-3616 The Diabetes Center is a comprehensive service providing diabetes self-management education to individuals with diabetes. Our team of certified diabetes educators works closely with the patient’s physician on plans to improve and maintain blood glucose control. Outpatient Imaging Center: 919-862-5200 The center is located on the first floor of the Duke Medicine Plaza and offers radiography services including the latest technology in computed tomography (CT scans), bone density, mammography and ultrasound. Outpatient Rehabilitation: 919-954-3492 Our diversified, dedicated and experienced staff provides one-on-one therapy in the areas of physical, occupational and speech language therapy. Plaza Pharmacy: 919-954-3921 We offer medication counseling by a Pharmacist, ostomy supplies, Insulin pump supplies, over-the-counter products and prescription compounding. The Plaza Pharmacy also accepts most third party insurance plans. Sleep Lab: 919-862-5863 The Duke Raleigh Hospital Sleep Lab is available to patients suffering from a variety of sleep disorders including snoring, sleep apnea and restless leg syndrome. Wellness Center: 919-954-3174 Whether serving someone with special needs including cardiac or pulmonary rehab or someone simply looking to develop a healthier lifestyle, the Wellness Center is fully equipped to meet individual needs through a variety of specialized programs. Wound Healing Center: 919-862-5573 Our center includes a comprehensive, multidisciplinary service for chronic wound treatment including hyperbaric medicine with the resources of the only hyperbaric fellowshiptrained physician in Wake County.