December 2013
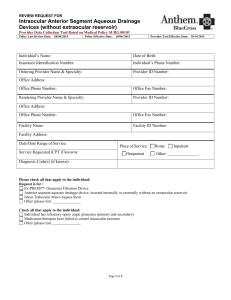
advertisement

December 2013 In this issue Page Health care reform update Health care reform updates on anthem.com Inovalon to conduct health assessments for Exchange plans 2 3 Administrative and policy update ICD-10 check-up: how am I doing? Update to claims processing edits and reimbursement policies Don’t miss out on secure messaging Expanded list of predetermination recommendations for outpatient procedures Misrouted protected health information (PHI) 2013 National Uniform Billing Committee UB-04 code changes Refer members to participating ambulance providers Improving members’ health care experience 4 4 5 6 6 6 9 9 Medicare Advantage (MA) update 2014 MA plan changes Refer MA members to MA network physicians Physicians to receive home test kits results for MA members Adult BMI and medical records – record exact number, not range Avoidable MA readmissions may lead to claim denials Sleep Management Program expanded to include MA eff. 1/1/2014 Medicare reports on osteoporosis management after bone fracture MA Part D Formulary changing for 2014 Speaking the language of ICD-10 - Part 2 ADA offers medication guidelines for members with diabetes and hypertension Please complete recommended screenings for MA members Timely response to chart review requests appreciated 10 10 10 11 11 11 12 13 13 14 15 16 Programs and benefits update 2014 FEP benefit information available online 16 anthem.com 17 17 Important phone numbers Behavioral health update Behavioral health pass-through visits for 2014 Applied Behavioral Analysis (ABA) Clinical Guideline ME13020 MENL1213 1 of 32 In this issue (continued) Page Quality programs update Clinical practice and preventive health guidelines on anthem.com Case management - better health for members who need care most NurseLine offers 24/7 access to nurses Future Moms promotes healthy pregnancies and healthy babies MyHealth Advantage works with you to help our members Member satisfaction survey results regarding physician care HEDIS® 2013 results are in 17 18 18 19 20 21 22 Pharmacy update Pharmacy information available on anthem.com Coverage for compound drugs 28 28 Medical policy update Medical policy updates are available on anthem.com 28 Clinical guidelines update Clinical guidelines updates are available on anthem.com 31 Health care reform update Health care reform updates on anthem.com Please be sure to check the Health Care Reform Updates and Notifications and Information about Health Insurance Exchanges sections of our website regularly for the latest updates we’ve posted on health care reform and Health Insurance Exchanges. The most recent updates include: Many Members will Have New Health Plans in 2014 Important Information about Provider Referrals for Plans Purchased On and Off the Exchange New Provider Networks will Support Health Plans Sold On and Off the Health Insurance Marketplace Important Drug List Information for Plans Purchased On and Off the Exchange Health Insurance Exchange Product/Provider Network Reference Tool In addition, in December we will be posting on our website a Fact Sheet (FAQ) document that will contain a variety of information about Health Insurance Exchanges, including sample images of Health Insurance Exchange member ID cards as well as a Provider Checklist document to help you prepare for the new plans. Note that in addition to this newsletter and our website, we will also be using our email service, Network eUPDATE to communicate information about Health Insurance Exchanges. If you are not yet signed up to receive Network eUPDATEs, we encourage you to enroll now so you’ll be sure to receive all of the information we’ll be sending about Exchanges. To sign up, visit anthem.com > Providers > Maine > Network eUPDATE. December 2013 Maine 2 of 32 Anthem engages Inovalon to conduct health assessments for members enrolled in health plans purchased on and off the Exchange The implementation of the Health Insurance Marketplace (often called the Exchange) brings new and unique challenges for health plans, providers, consumers, and state and federal regulating agencies. We are working to adhere quickly and responsively to government guidance as it is issued. To that end, we want to share information about risk management programs associated with the Exchanges, our business relationship with Inovalon (a health care technology company), and upcoming outreach efforts to both members and providers. Three protective programs – the “three Rs” As mandated by the Affordable Care Act (ACA), health insurers for both individual and small group markets will no longer perform medical underwriting on individuals who apply for health insurance. This allows individuals who had previously been unable to obtain health care coverage to enter the health insurance market. As part of the ACA, the U.S. Department of Health and Human Services (HHS) introduced three protective programs – often called the “three Rs” – with emphasis on risk management and premium stabilization. The provisions of these programs are designed to help level the competitive playing field with health insurers and protect against adverse selection (attracting a higher than average risk pool) on and off the Exchange beginning 2014. The three programs are: Reinsurance (temporary program that provides funding to health plans that enroll high-cost individuals) Risk Adjustment (permanent program that transfers funds from lower risk plans to higher risk plans, helping to protect against adverse selection) Risk Corridors (temporary program that limits issuers’ losses and gains to help protects against inaccurate rate settings) Anthem works with Inovalon in outreach efforts to members and providers To comply with the programs’ provisions, our company is updating member health documentation for members in the individual and small group markets who purchased our health insurance plans on and off the Exchange. We have engaged Inovalon – an independent company that provides secure, clinical documentation services – to contact our members and conduct health assessments beginning mid-January 2014. The purpose of conducting these assessments is to collect clinical information regarding chronic disease diagnoses, medications, recent physician visits and hospital stays, and clinical history. As a result of the outreach efforts, our members may have questions about their health care options and may contact their physicians for appointments. As part of this initiative, Inovalon will be contacting certain network-participating providers to collect additional clinical information about our members. This process is intended to help the treating provider identify care gaps and encourage members to meet with their physicians for overdue appointments and/or to overcome barriers to accessing care. Members can be better supported with recommendations for member-specific interventions such as care management programs. Providers can submit assessments electronically using ePASS® – an online or mobile application, encounter support platform available through Inovalon. The easy-to-use, electronic tool compiles claims (including diagnoses), prescription drug and lab information to identify care gaps and potential health care recommendations/interventions. Inovalon’s outreach efforts begin in the new year On our behalf, Inovalon will begin reaching out via written correspondence in mid- January to certain providers in our networks that will support our 2014 product offerings. To help minimize any potential disruptions in providers’ offices, December 2013 Maine 3 of 32 Inovalon will request only a small list of members for whom a patient assessment is needed. We encourage providers to comply with Inovalon’s requests for assessments. Watch for further updates about this process in upcoming editions of our Network Update provider newsletter and on our website at anthem.com. Administrative and policy update ICD-10 check-up: how am I doing? The end of the year is a great time to look back and review the status of important projects and activities. The implementation plan for your practice’s transition to ICD-10 is one of those long term efforts where periodic check-ups can help to make sure you are still on target to be ready by October 1, 2014. Below is a list of some of the planning activities that your practice should have completed during the last year. Processes/workflows changes – You should have identified which internal processes and workflows will be affected by using the new code set, how each workflow is affected and have a plan to address the changes that need to occur to incorporate ICD-10. Systems changes – Complete an assessment of all systems used by your practice. You should have a comprehensive list of all necessary system changes, upgrades and/or other adjustments, the cost of these changes, the amount of time it will take to complete these changes and the timeline for implementation. External partners – You should have a clear picture of how each of your vendors, clearinghouses and/or billing services plan to handle the transition to ICD-10 and how their plan will affect your practice. Documentation requirements –You should have assessed a sample of your practice’s member records to determine if the clinical documentation is complete and detailed enough to properly code claims using ICD-10 diagnosis codes. With the new level of specificity of each code, having the right documentation available for your medical coders will reduce the potential for decreased productivity associated with using the new code set. Training – You should have a comprehensive list of the education and training needs for your staff members. The list should detail the type of training needed (coding, systems, etc.), who will receive the training and timeline for the training to occur. Training costs should also be determined and budgeted as appropriate in future fiscal planning. As you move into the active phases of your implementation plan for ICD-10, having this knowledge as your foundation will be the key to a smooth transition to ICD-10. Update to claims processing edits and reimbursement policies On December 1, 2013, we will update our Anthem Online Provider Services (AOPS) website with the following new and/or revised reimbursement policies. The updates below indicate whether the article pertains to professional or facility provider billing. December 2013 Maine 4 of 32 Review of reimbursement policies – professional The following professional reimbursement policies received an annual review and may have word changes or clarifications, but do not have significant changes to the policy position or criteria: Claim Editing Overview Co-Surgeon/Team Surgeon Services Documentation and Reporting Guidelines for Consultations Documentation and Reporting Guidelines for Evaluation and Management Services Durable Medical Equipment Health and Behavior Assessment/Intervention Injectable Substances with Injection Services Multiple Diagnostic Imaging Physical and Manipulative Maintenance Services Qualitative Drug Screen Testing Routine Obstetric Services “Rule of Eight” Reporting Guidelines for Physical Medicine and Rehabilitation Services Screening Services with E/M services Urgent Care (Coding and Bundled Supplies) Customized Edits – professional We have updated our Customized Edit posting to indicate the 2013 reimbursement policies that include customized edits. Frequency Editing – professional Effective for claims with dates of service on or after March 1, 2014, our Frequency Editing policy will be updated to include CPT ® code 96116 (Neurobehavioral status exam (clinical assessment of thinking, reasoning and judgment, e.g., acquired knowledge, attention, language, memory, planning and problem solving, and visual spatial abilities), per hour of the psychologist's or physician's time, both face-to-face time with the individual and time interpreting test results and preparing the report) will have limit of five (5) per 365 days. Significant Edits – professional We have updated our Significant Edits posting to reflect the 2013 analysis of claims data for significant edits. In addition, we have identified significant edits contained within our reimbursement policies. System updates for 2014 – professional As a reminder, our ClaimsXten editing software package will be updated quarterly in February, May, August and November of 2014. These upgrades will: reflect the addition of new and revised CPT/HCPCS codes and their associated edits include updates to National Correct Coding Initiative (NCCI) edits include updates to incidental, mutually exclusive, and unbundled (rebundle) edits include assistant surgeon eligibility in accordance with the policy include edits associated with reimbursement policies including, but not limited to preoperative and post operative periods assigned by The Centers for Medicare & Medicaid Services (CMS) Notice of reimbursement policy modifications due to these updates will continue to be published in Network Update and on AOPS. December 2013 Maine 5 of 32 Coding tip: “Irrigation of implanted venous access device for drug delivery systems” – professional CPT code 96523 is used to report the irrigation of an implanted venous access device for drug delivery systems and, according to CPT, should not be reported in conjunction with other services. Based on this CPT instruction, 96523 is eligible for reimbursement when it is the only code reported on the day of service by the same provider. According to the Resource-Based Relative Value Scale (RBRVS) Data Manager, supplies such as saline A4216 and A4217, and heparin J1642 are included in the relative value units (RVUs) for 96523 and are not reported separately. CPT® is a registered trademark of the American Medical Association. Don’t miss out on secure messaging What is secure messaging? Secure messaging is a feature accessed at availity.com that allows a user to send a question online about a claim. This functionality is available only on Availity’s web portal. Secure messages can be sent for local Connecticut, Maine and New Hampshire, National, Medicare Advantage, Taft Hartley, BlueCard® and FEP (Federal Employee Program) member claims. How are secure messages processed? At the bottom of the claims detail page, click on the link “Do you have a question about this claim?” Once this link is selected, a new window will open and you will choose one of the seven questions from a dropdown box and use the free-form text box to add any additional information related to your question and click “submit.” Your secure message is routed to the Anthem Customer Service departments for a response through the secure messaging system, eliminating the need for you to make a phone call for the same information. Secure messages are housed within a self-contained secure email system, separate from your office email account. The messages are sent and received using your login credentials on Availity. Messages are stored within the secure messaging tool using an Inbox and an Outbox. You can review messages you previously sent via the Inbox; view new responses received via the Outbox; and, save messages to your computer or print for your records. To access the responses to your messages sent, go to claims management/secure messaging from the left navigation menu on the Availity Web Portal. If you have additional questions on a claim based on the response you receive in your Inbox, you can reply to Provider Service’s response with further questions. How do I get access to secure messaging? Starting November 16, 2013, any user with access on Availity to claim status inquiry, is able to see the link “Do you have a message about this claim?” at the bottom of the claim detail page. In addition, the secure messaging link under claims management is available to you to view the responses to your inquiries. The primary access administrator (PAA) as of November 16, 2013 needs to make sure users have access to claim status inquiry in order for a user to access secure messaging. Once the PAA has added the role of claim status inquiry on the Availity Web Portal, the user can follow these steps to help ensure the functionality has been added successfully: – Log into availity.com and submit a claims inquiry transaction on an Anthem or BlueCard member claim. – Click on the date span link on the claims summary page to navigate to the claims detail page. – From the claims detail page, look in the lower left hand corner of the screen for the “Do you have a question about this claim?” link. If this link appears, this confirms that you have access to the secure messaging functionality and you can start to use this great feature! December 2013 Maine 6 of 32 Ongoing access to AOPS functionality At this time, we are postponing the full transition of access to AOPS only through the Availity Web Portal until 2014. Users who need access to AOPS functionality like fee schedules or remits should continue to use the existing process for AOPS access until further notice. To register for access Availity’s web portal or to view a demo, go to availity.com or call Availity Client Services at 800AVAILITY (800-282-4548). Expanded list of predetermination recommendations for outpatient procedures Our standardized review process for certain outpatient procedures allows providers to determine the member’s benefits before rendering the service/procedure. Below are some upcoming additions to the list of services for which we recommend predetermination of benefits effective March 1, 2014. These recommendations apply only to our local plans and do not apply to National accounts, Medicare supplemental, Medicare Advantage, the Federal Employee Program (FEP), BlueCard®, TaftHartley, or when Anthem is secondary. Predetermination recommendations for the following services Changes effective March 1, 2014 DME.00037. Cooling Devices and Combined Cooling/Heating Devices. Codes added for clinical review are E0218, E0236 and E0217. GENE.00001. Genetic Testing for Cancer Susceptibility. Along with the current codes on the policy, these codes will also be added for predetermination: 81321, 81323. Note: It is important to identify whether the request is for outpatient or inpatient on your faxed request for review. In addition, if the provider does not initiate the predetermination process, records may be requested for post service review based on the same criteria listed in the applicable medical policy or clinical guideline. To obtain a copy of any clinical guideline or medical policy, visit anthem.com > Providers > select state > enter > Medical Policies and Clinical UM Guidelines. Misrouted protected health information (PHI) Providers and facilities are required to review all member information received from Anthem to help ensure no misrouted PHI is included. Misrouted PHI includes information about members that a provider or facility is not currently treating. PHI might be misrouted to providers and facilities by mail, fax or e-mail. Providers and facilities are required to immediately destroy any misrouted PHI or safeguard the PHI for as long as it is retained. In no event are providers or facilities permitted to misuse or re-disclose misrouted PHI. If providers or facilities cannot destroy or safeguard misrouted PHI, providers and facilities must contact Anthem’s Provider Call Center to report receipt of misrouted PHI. 2013 National Uniform Billing Committee (NUBC) UB-04 code changes This article was published in the October 2013 Network Update, and is being reprinted in this December issue as a reminder. December 2013 Maine 7 of 32 The following changes have been made by the National Uniform Billing Committee (NUBC) and are outlined below: New patient (discharge) status codes Type of bill (TOB) 32X and 34X: description change Type of bill 33X: code eliminated Type of bill 084X and 089X: revised New revenue code: 0953 Source of admission: required on all types of bill except 014X New patient discharge status codes (FL-17) approved by NUBC effective October 1, 2013 are as follows: NOTE: Patient discharge status codes are required by NUBC on both the inpatient and outpatient claims. Value 69 81 82 83 84 85 86 87 88 89 90 91 92 93 94 95 Description Discharge Transferred to a Designated Disaster Alternate Care Discharged to Home or Self Care with a Planned Acute Care Hospital Inpatient Readmission Discharged/Transferred to a Short Term General Hospital for Inpatient Care with a Planned Acute Care Hospital Inpatient Readmission Discharged/Transferred to a SNF with Medicare Certification with a Planned Acute Care Hospital Inpatient Readmission Discharged/Transferred to Facility that Provides Custodial or Supportive Care with a Planned Acute Care Hospital Inpatient Readmission Discharged/Transferred to a Designated Cancer Center or Children’s Hospital with a Planned Acute Care Hospital Inpatient Readmission Discharged/Transferred to Home Under Care of Organized Home Health Organization with Planned Acute Care Hospital Inpatient Readmission Discharged/Transferred to Court/Law Enforcement with a Planned Acute Care Hospital Inpatient Readmission Discharged/Transferred to a Federal Health Care Facility with a Planned Acute Care Hospital Inpatient Readmission Discharged/Transferred to a Hospital-based Medicare Approved Swing Bed with a Planned Acute Care Hospital Inpatient Readmission Discharged/Transferred to an IRF including Rehabilitation Distinct Part of a Hospital with a Planned Acute Care Hospital Inpatient Readmission Discharged/Transferred to a Medicare Certified Long Term Care Hospital (LTCH) with a Planned Acute Care Hospital Inpatient Readmission Discharged/Transferred to Nursing Facility Certified by Medicaid but not Certified by Medicare with Planned Acute Care Hosp IP Readmission Discharged/Transferred to Psychiatric Hospital or Psychiatric Distinct Part of a Hospital with a Planned Acute Care Hosp IP Readmission Discharged/Transferred To a Critical Access Hospital (CAH) with a Planned Acute Care Hospital Inpatient Readmission Discharged/Transferred to Another Type of Health Care Institution not Defined in this Code List with a Planned Acute Care Hosp IP Readmission December 2013 Maine 8 of 32 Type of bill (FL-4) description changes 032X Description change - Home Health Services under a Plan of Treatment (eff 10/01/13) 034X Description change - Home Health Services not under a Plan of Treatment (eff 10/01/13) Type of bill (FL-4) eliminated 033X Code Eliminated - No longer a valid code as of 10/01/13 Type of bill changes (FL-4) from inpatient / outpatient to outpatient ONLY Change from Inpatient / Outpatient to Outpatient only service designation - Specialty Facility 084X Free Standing Birthing Center (eff 07/01/12) Change from Inpatient / Outpatient to Outpatient only service designation - Specialty Facility 089X Other (eff 07/01/13) New revenue code (FL-42) 0953 Chemical Dependency effective for claims received on or after 10/01/2013 Source of admission (point of origin) (FL-15) required on all claims (except TOB 014x) Effective October 1, 2013, the Blue Cross Blue Shield Association (BCBSA) is requiring Source of Admission/Point of Origin codes for all TOBs (except 014X lab services). This BCBSA ALL modification is needed by Home Plans for pricing non-par claim encounters and is in alignment TOBs with the NUBC changes. Please make sure all billing staffs are aware of these changes. Changes affect commercial and Medicare Advantage products. Additional information regarding the discharge status codes may be communicated by the Centers for Medicare & Medicaid Services (CMS) in the future. Refer members to participating ambulance providers We recently implemented an enterprise air ambulance member and provider education strategy. This approach encourages the use of the Anthem participating provider network for non-emergent, air-ambulance transport. Currently, member certificate language states that prior authorization is required for non-emergent air ambulance services. Please remember that as a participating provider, you have agreed to refer members to other participating providers. When it is necessary to refer a member to a non-participating provider, remember to inform the member that services provided by a non-participating provider may result in reduced benefits. The non-participating provider may bill them for amounts other than deductibles and copayments and for medical services not covered under the member’s benefit agreement. Our collaboration and work on this effort is another strong example of how we can help control medical costs and improve the quality, affordability and safety of our members. Improving members’ health care experience We are committed to working with our network physicians to help make our members’ health care experience a positive one. Towards this end we wanted to share with you a document that was developed by the California Quality Cooperative. This December 2013 Maine 9 of 32 resource outlines some helpful tips you can use to improve your relationship with our members and provide better care at the same time. Simply log onto our website at anthem.com and follow this path: Providers > select state > Communications > General Information > Guide to Improving the Patient Experience. "This information is provided by the California Quality Collaborative. A healthcare improvement organization dedicated to advancing the quality and efficiency of outpatient care in California." Medicare Advantage update 2014 Medicare Advantage plan changes Annual benefits changes for Medicare Advantage plan members will be effective January 1, 2014. Each year, we renew our contract with the Centers for Medicare & Medicaid Services (CMS) and CMS re-evaluates and approves the benefits we’ll offer to our Medicare Advantage members for the upcoming year. There are changes in the individual Medicare Advantage offerings from Anthem. You can help members manage their health care costs by being aware of these changes. In addition, remember to check the member ID card at the beginning of each calendar year, as the member may have changed plans. Anthem MediBlue Select (HMO) plan changes In 2014, we will be offering a new HMO plan. Anthem MediBlue Select (HMO) will be available in the following counties: Cumberland, Kennebec, Penobscot, and York. Anthem MediBlue Select (HMO) plan highlights (prefix XVJ) Low plan premiums at $9 with Anthem MediBlue Select (HMO) Combined maximum-out-of-pocket of $3,800 $5 primary care physician (PCP) copay - $40 specialist copay $0 copay for Medicare-covered preventive care To view additional Medicare Advantage plan changes in 2014, click here. Making a referral for a Medicare Advantage member? Please ensure physician is in the Medicare Advantage network When referring an Anthem Medicare Advantage member to a specialist, please ensure that the physician participates in the member’s health plan. Depending on the member’s benefit plan, services may not be covered or a significant member cost share may exist when seeking services from a non-participating provider. You can use Find a Doctor at anthem.com to make sure the referral is to an in-network provider. Physicians to receive home test kits results for Medicare Advantage members Medicare Advantage members who appeared to be missing key tests or screenings for colorectal cancer, blood sugar, and cholesterol screenings began receiving a home test kit from us in August, and will receive these home test kits as needed December 2013 Maine 10 of 32 through the end of the year. Providers will receive a letter from us detailing the member’s test results. Please review the test results and discuss with the member as needed. Adult BMI and medical records – please record exact number, not range Healthcare Effectiveness Data and Information Set (HEDIS) is updating the medical records specifications for adult body mass index. In the past, it was acceptable to record a range for BMI, such as >30. In 2014, HEDIS specifies that the exact BMI number should be recorded in the medical record, such as 32. Greater precision in charting the member’s BMI will help the provider help the member achieve or remain at a healthy weight. Update: avoidable Medicare Advantage readmissions may lead to administrative claim denials To help encourage the best possible quality of care outcomes for our Medicare Advantage members and support the clinical quality issue that is being driven by CMS’ Readmission Quality Improvement Program (QIP), we have an obligation to review readmissions for clinical relatedness. In accordance with the diagnosis related groups (DRG) payment methodology, Anthem will be following a uniform 30-Day Readmission Review Program for our Medicare Advantage program that is consistent with Centers for Medicare & Medicaid Services (CMS) quality improvement guidance. 1 Payment for a Medicare Advantage member’s DRG readmission to the same acute facility within 30 days of the first admission may be administratively denied if, the readmission is determined to be related to the previous admission. This Program will apply to facilities’ claims only. We will not administratively deny professional or ancillary claims based upon the 30-Day Readmission Review Program. The administrative denial of these claims will apply to participating and nonparticipating facilities. 2 As a reminder, all claims denied administratively under this Readmission Review Program are denied as provider liability. Our member is not liable for these denied claims. Providers are not permitted to balance bill the member for the denied claim. Additional information can be found in the Anthem Medicare Advantage Guidebook. Please share this information with clinical staff and others involved with admissions. 1 Chapter 4, Section 4240 (Readmission Review) of the Medicare Quality Improvement Organization Manual: Readmission review involves admissions to an acute, general, short-term hospital occurring less than 31 calendar days from the date of discharge from the same or another acute, general, short-term hospital (See §1154(a)(13) and 42 CFR 476.71(a)(8)(ii)). Medicare QIO Manual, Chapter 4, Section 4240: Perform case review on both stays. Analyze the cases specifically to determine whether the patient was prematurely discharged from the first confinement, thus causing readmission. Perform an analysis of the stay at the first hospital to determine the cause(s) and extent of any problem(s) (e.g., incomplete or substandard treatment). Consider the information available to the attending physician who discharged the patient from the first confinement. Do not base a determination of a premature discharge on information that the physician or provider could not have known or events that could not have been anticipated at the time of discharge. 2 Subject to explicit language that sets forth a different payment methodology Sleep Management Program expanded to include Medicare Advantage members effective January 1, 2014 As we advised in the October 2013 issue of Network Update, we will be implementing a new specialty benefit management program effective January 1, 2014 for home-based (unattended) diagnostic study and facility-based (not inpatient) sleep December 2013 Maine 11 of 32 testing and therapy services provided to Medicare Advantage members. Please note that effective January 1, 2014, prior authorization for sleep testing and therapy services will be required through AIM for Medicare Advantage members. Prior authorization will be required to determine the medical necessity of the sleep study, including the need for use of a facility test versus doing the test in the home. Prior authorization will also be required for any subsequent treatment (therapy), both initial and ongoing. For therapy services, members must meet usage criteria for the continued rental of equipment and replacement of supplies. This program is administered by AIM Specialty Health SM (AIM) and includes the following: Home sleep test (HST) In-lab sleep study (PSG) Multiple sleep latency test (MSLT) and maintenance of wakefulness test (MWT) Titration study Initial treatment order (APAP, CPAP, BPAP, oral devices, appliances and related supplies) Ongoing treatment order (APAP, CPAP, BPAP, oral devices, appliances and related supplies) Services performed in conjunction with emergency room services, inpatient hospitalization, or urgent care facilities are excluded. Anthem established this program to promote clinically appropriate services for our members. Sleep testing and therapy services provided on or after January 1, 2014, that are not prior authorized may be denied. Beginning December 16, 2013, providers should contact AIM to obtain an order number for the following elective services or supplies for Medicare Advantage members scheduled January 1, 2014 or later: home-based (unattended) diagnostic sleep study or a facility-based (not inpatient) diagnostic or titration study (free-standing or hospital). In addition, ordering physicians should contact AIM to obtain an order number for sleep treatment (therapy) equipment and related supplies for Medicare Advantage members. To submit your request, you may access AIM’s ProviderPortal SM at aimspecialtyhealth.com/gowebsleep. From the dropdown menu, select “Anthem CT’, ‘Anthem ME’ ‘Anthem NH’. Sleep Management Clinical Checklists to help you prepare the precertification request, and a Frequently Asked Questions document are available at www.aimspecialtyhealth.com/gowebsleep. Or, you may call AIM toll-free at 866-714-1107, Monday – Friday, 8:00 a.m. – 5:00 p.m. Please note: Both ordering physicians (those referring the member for sleep testing or therapy) and servicing providers may submit requests for sleep testing and therapy. Medicare reports on osteoporosis management after bone fracture Once a woman has had a fracture, she has a four times greater risk of another fracture, reports the National Institute of Arthritis and Musculoskeletal and Skin Diseases. To monitor osteoporosis management, the National Committee for Quality Assurance reports to Medicare which of our female members 67 years old or older has had a fracture and has had either bone mineral density testing or medication to treat or prevent osteoporosis within six months of the fracture. December 2013 Maine 12 of 32 Screening and treatment can significantly improve health outcomes by preventing fractures. Osteoporosis therapy may reduce the risk of fracture by nearly 50 percent, according to the Journal of Rheumatology. Medicare-covered bone density scans are covered with no cost share to the member. With some plans, there may be a cost share if the member receives these services out of network. All qualified people with Medicare who are at risk for osteoporosis and meet one of the following five criteria are eligible: A woman whose doctor determines she's estrogen deficient and at risk for osteoporosis, based on her medical history and other findings A person whose X-rays show possible osteoporosis, osteopenia, or vertebral fractures A person taking prednisone or steroid-type drugs or is planning to begin this treatment A person who has been diagnosed with primary hyperparathyroidism A person who is being monitored to see if their osteoporosis drug therapy is working Medicare Advantage Part D Formulary changing for 2014 – please help members with new choices Each year we evaluate our benefits and formulary and may make changes to update them. Formulary changes in the upcoming year include: tier changes, drug removals, and new prior authorization and quantity limit requirements. Members will have formulary changes and will need your assistance to help ensure they get their needed treatments at the most affordable cost. For insulin dependent diabetic members, it is important to note that for many of our products, we will be removing the Novolin line of products from our formulary. We are communicating this change directly to impacted members by letter and phone encouraging them to contact their providers regarding this change in coverage. Please encourage members to review the 2014 formulary information within their Annual Notice of Change (ANOC) mailing, or to view the information online. Ask them if the coverage for any of their prescriptions has been changed, and consider alternative medications in a lower cost-sharing tier that may meet their needs. American Diabetes Association offers medication guidelines for members with diabetes and hypertension The Centers for Medicare & Medicaid Services (CMS) tracks several performance and quality measures in place for Medicare Part D members. To help ensure that we are in alignment with CMS, one of the measures we’ll be focusing on for the remainder of this year is medication treatment for members with diabetes and hypertension. The American Diabetes Association guidelines recommend that ACE inhibitors or ARB medications be given to individuals with diabetes and hypertension to help reduce the risk of cardiovascular events and the progression of nephropathy indicated by levels of microalbuminuria/albuminuria. If our members have hypertension, we ask that you please consider whether an ACE inhibitor or ARB medicine may be an appropriate treatment at this time. Based on the American Diabetes Association guidelines, we offer you this information with the hope that you may find it useful in your efforts to help ensure high-quality care for our members. December 2013 Maine 13 of 32 Speaking the language of ICD-10 - part 2 In the last publication, as part of our implementation ICD-10 efforts we discussed the critical role complete and accurate medical record documentation and diagnosis coding plays in managing our Medicare Advantage membership. Remember, your coding and record documentation efforts have a direct impact on accurate risk adjusted payment, as well as the services and benefits we are able to provide to our membership. ICD-10 preparation You and your coding staff do not have to learn the entire code set. One way to help your practice prepare for the upcoming ICD-10 changes is to review your documentation for the most commonly used ICD-9 codes in your practice. You can then begin working with your coding staff to select the appropriate corresponding ICD-10 codes. Identifying the challenges now will help reinforce the documentation requirements in order for your coders to assign the most appropriate diagnoses code for ICD-10. This may also provide you with a tool for assessing your staff and training needs. As a guideline, coding professionals recommend that any required coding training take place approximately six months prior to the ICD-10 compliance deadline. ICD-10 impact on clinical documentation While ICD-10 will not change the way you provide care to individuals, the amount of details documented in the medical record for your coding staff will need to be expanded. Specificity will be a key component to ICD-10 documentation. It will be even more important to help ensure you are documenting to the highest degree of specificity. For example, in ICD-10, the selection of laterality is expanded. Clinical documentation for the diagnosis should include information as to which side of the body is affected (i.e., right, left, or bilateral). We realize that concepts that are new to ICD-10 may not be new to you. However, to assist you with your preparation, you will find an example of what to include in your documentation for a fracture diagnosis to help ensure your coders can accurately assign ICD-10 codes: To code for the diagnosis of a fracture in ICD-10, the following details will need to be provided: Site Laterality Type Location For traumatic fracture, the ICD-10 code set has the following 7 th character selection: A. B. C. D. E. F. G. Initial encounter for closed fracture Initial encounter for open fracture Subsequent encounter for fracture with Subsequent encounter for fracture with Subsequent encounter for fracture with Subsequent encounter for fracture with Sequela routine healing delayed healing nonunion malunion In addition to providing details for the diagnosis of the fracture, it is important to also document how the injury occurred and where. For accurate code assignment, provide the following information for injuries: External cause – Provide the cause of the injury; ask and document “how” the injury happened. December 2013 Maine 14 of 32 Place of occurrence – Document where the individual was when the injury occurred; for example, include if the individual was at home, at work, in the car, etc. Activity code – Describe what the individual was doing at the time of the injury; for example, was he or she playing a sport or using a tool? External cause status – Indicate if the injury was related to military, work, or other. This example was provided as acute injury codes are included in the 2013 HCC Model for risk adjustment. As you can see from this example, fracture is one of the diagnoses that have expanded the level of specificity required to code the fracture which includes the activity codes involved. In our next article in this 3-part series our focus will be on specific diseases, providing you with suggestions and recommendations to help you prepare for the transition to ICD-10. We have been busy transforming our business as well in preparation for this upcoming transition, not only for working toward the ICD-10 deadline requirement, but to also add value and innovation. You will also find some valuable information at any of the following websites: https://www.cms.gov/Medicare/Coding/ICD10/ProviderResources.html http://www.ama-assn.org/go/ICD-10 End-of-year reminder – please complete recommended screenings for Medicare Advantage members We are conducting a number of outreach efforts to help ensure our Medicare Advantage members see you for all annual preventive care and screenings recommended by the Centers for Medicare & Medicaid Services. Through the end of the year, we’ll be contacting members, their primary care physicians or both to complete these important services. Flu shots – Since September, we’ve been reminding members of the importance of getting an annual flu vaccination. LDL/A1C – We call to encourage members with elevated LDL and A1C lab results to see their primary care physicians to be retested and determine an appropriate care plan if levels continue to be elevated. Diabetes self-management program –Online classes are offered to members with Type 2 diabetes. Osteoporosis – We call members and providers when a recent bone fracture is identified on claims. The call provides timely education on the importance of bone mineral density testing and osteoporosis medication treatment if appropriate for the member. Healthy Checklist –The Healthy Checklist is personalized for each Medicare Advantage member and reminds them to ask you about preventive care and screenings they may need throughout the year. We encourage members to bring this checklist to you during office visits to help ensure they are up-to-date on preventive care. Mammograms – Female Medicare Advantage members age 40-69 who do not appear to have a claim for a mammogram in the past two years will be encouraged to complete this important screening by the end of the year. The mailing will be delivered through the end of the year. Home lab kit – We have been calling to offer home test kits to Medicare Advantage members in select markets who appear to be missing key tests or screenings for colorectal cancer, cholesterol management for members with a cardiovascular event, comprehensive diabetes care for LDL cholesterol screening and HBA1c control. For members who opt in to the December 2013 Maine 15 of 32 program, a home collection kit will be mailed to their home address. If a member has been identified as your patient based on our claims records (physician most often seen and/or most recently visited), we will send a letter notifying you that the member agrees to accept a home collection kit. These members are asked to collect their specimens and mail them back to the lab for analysis. Members who complete the kit and return it to the lab will have the results mailed to their homes. A copy of the results will be mailed to the members’ primary care physicians (identified from our claims records). Please review the test results and discuss with the member as needed. We also are placing reminder calls to members to complete and return the kit if they requested a home lab kit but have not returned it. The reminder calls will continue through the end of the year. Fall prevention, urinary incontinence – When our Medicare Advantage Clinical Quality Care team calls members to remind them to complete important preventive care and screenings, they’ll also take the opportunity to speak with our Medicare Advantage members about any concerns they may have about urinary incontinence and the risk of falling. During those conversations, we’ll encourage those members to speak with their physicians about these issues. We will send educational brochures to members who request this additional information and also offer them to members during home health visits. We encourage you to also check in with our senior members about these issues to help ensure they are receiving needed care. High blood pressure – if you treat a member who has uncontrolled high blood pressure, please consider asking the member to come in for an office visit for an up-to-date blood pressure assessment and to discuss treatment options if needed. For more information, please contact the Clinical Quality Department at CQMI@wellpoint.com. Timely response to chart review requests appreciated As a participating physician who provides care to our Medicare Advantage members, you play a key role in our compliance with Centers for Medicare & Medicaid Services. By maintaining quality coding and documentation practices and by cooperating with our medical chart requests in a timely manner, you will be instrumental in helping us meet our CMS obligations. Y0071_13_18594_I 10 /22/2013 Programs and benefits update 2014 FEP benefit information available online To view the 2014 benefits and changes for the Blue Cross Blue Shield Service Benefit Plan, also known as the Federal Employee Program (FEP), go to anthem.com/fep > select state > Coverage Options > Standard or Basic Option. You’ll find the 2014 Service Benefit Plan Brochure and Plan Benefit Summary information for year 2014. For questions please contact FEP Customer Service at 800-722-0203. Behavioral health update Behavioral health providers – please review the entire newsletter While the articles in this section are of specific interest to participating behavioral health providers, there are other articles in this publication that apply to or could be of interest to behavioral health providers as well. Please review the entire issue. In addition, please note that the information and articles in this newsletter related to behavioral health services are for plans and products managed by Anthem Behavioral Health. December 2013 Maine 16 of 32 Behavioral health pass-through visits for 2014 We recognize that regular maintenance visits are often indicated for members with chronic psychiatric illness. To simplify the administrative management of these members enrolled in our fully-insured plans, we eliminated outpatient management for standard outpatient behavioral health services. However, members enrolled in self-funded groups administered by us, also known as administrative services only (ASO), may still require outpatient management after 12 pass-through visits have been utilized. A participating provider is not required to submit an Outpatient Treatment Report (OTR) until the specified number of pass-through visits have occurred. In calendar year 2014, 12 behavioral health sessions per provider are eligible for coverage for these members without prior authorization or an OTR submission. This applies to members who begin treatment in 2014, as well as to members who were in treatment in 2013, and who have exhausted any initial pass-through visits that were assigned by Anthem Behavioral Health prior to 2014. If the member has a managed outpatient benefit and requires more than 12 visits in a calendar year, the provider will need to complete an OTR and fax it to us at 866-613-4246 before the 13th visit. This requirement pertains to services managed by Anthem Behavioral Health only and includes the following plans: HMO Maine, HMO Choice, HMO Blue New England, Blue Choice New England and Individual HMO (standard and basic). OTRs that are submitted late may result in administrative denials for service dates. In addition, please note: Evaluation and management services rendered by psychiatrists do not require authorization. Applied behavioral analysis (ABA), transcranial magnetic stimulation (TMS), IOP and PHP continue to require prior authorization for all members. Federal Employee Program (FEP) and Medicare Advantage members do not require prior authorization for outpatient services. If you have questions please contact Provider Service at 800-755-0851. Applied Behavioral Analysis (ABA) Clinical Guideline Effective March 1, 2014, we will be implementing clinical guideline CG-BEH-02, Applied Behavioral Analysis for Autism Spectrum Disorder. This guideline addresses the use of applied behavioral analysis (ABA) or similar services that use intensive behavioral intervention (collectively, ABA), when included in relevant state mandates, as treatment for autism spectrum disorder (ASD) when a state mandate requires or benefit plan language explicitly provides coverage for ABA. Please note that ABA therapy does require prior authorization for most plans and products. Services for ABA should be billed only with one of the following HCPCS codes, H2019 or H2020, and the appropriate ASD diagnosis. The guideline can be located at anthem.com > Providers > select State > Anthem Behavioral Health Policies and Guidelines. Quality programs update Clinical practice and preventive health guidelines available on anthem.com As part of our commitment to provide you with up to date clinical information and educational materials, we have adopted nationally recognized medical, behavioral health, and preventive health guidelines, which are available to providers on our December 2013 Maine 17 of 32 website. The guidelines, which are used for our Quality programs, are based on reasonable medical evidence, and are reviewed for content accuracy, current primary sources, the newest technological advances and recent medical research. All guidelines are reviewed annually, and updated as needed. The current guidelines are available on our website at anthem.com > Providers > select state > Health & Wellness > Practice Guidelines. Case management - better health for members who need care most Our Case Management program helps members who are at risk for greater illness and cost and who would benefit from outreach and support. Our goal is to offer information and guidance to optimize members’ health, from the very sick to those returning to full health. We offer case management to members who are currently going through major medical care. We also reach out to members who are likely to need significant health care services in the near future. Our goals are: To help you by supporting your plan of care for our members To help members have better health which could lower their cost of care Who qualifies for the program? Case management uses more than 500 health markers to find members who may be at highest risk for serious conditions. We also reach out to members who currently have serious health problems. These are members who are going through major procedures and treatments and may need extra help and follow-up care. Some typical conditions for which members often need significant levels of care: Multiple sclerosis Severe heart problems Major stomach diseases Severe neurological issues Any major hospitalization from a diagnosis or injury • • Case Management gets a thumbs-up* More than 86% of members were “satisfied” or “very satisfied” with case management. 93% of members thought our program was “extremely valuable” or “very valuable.” *2012 Member Satisfaction Survey How the program works We call members who qualify for the program and tell them how we can help. When they join the program, our nurse coaches work closely with them to support your treatment plan. The nurses answer questions about diagnoses and drugs, and help set goals for better health. Members who have recently left the hospital receive support on discharge planning, home health care, follow-up appointments and community resources. We focus mainly on spotting and resolving gaps in care. Our outreach for enrollment includes live and automated telephone calls and letters to members. NurseLine offers 24/7 access to nurses Our 24/7 NurseLine program gives our members access to trained registered nurses any time of the day or night. Members can get help deciding what kind of care they need. NurseLine is a great resource for members, especially after office hours – and even on weekends. 24/7 NurseLine doesn’t replace medical care or handle emergencies. During the call, if the nurse believes that the member needs emergency care, the nurse starts a three-way 911 call. The nurse stays on the call until emergency help comes. December 2013 Maine 18 of 32 How 24/7 NurseLine serves members 24/7 NurseLine records and tracks each call along with data from our programs. For instance, if a member is enrolled in our diabetes program, the nurse can access the member’s records. Members can get help based on their health history and receive resources to drive their care. The NurseLine staff is skilled and dedicated. Our nurses average 19 years of nursing experience. They also have quick access to doctor support on all shifts. Each call center has a medical director who provides clinical oversight and advice to our nurses. We use a huge database with about 5,000 topics. They cover signs, medical tests, drugs, wellness and general health problems. Our audio library has more than 400 topics in both English and Spanish. We have nurses who speak Spanish and a language line for interpreters for most languages. Members whose benefit plans include 24/7 NurseLine may have the toll-free number on the back of their member ID cards. 24/7 NurseLine by the numbers In 2011, callers to 24/7 NurseLine were mostly women (62% overall). Studies show that women are more likely to be seekers of health information in a family. The highest users were 23 to 55 years old (52%), followed by 0 to 17 years old (23%). The top health topic was pediatrics (24%). Users also asked about digestion (12%), bone/muscle/joint (12%), dermatology (6%), neurology (6%) and cardiovascular (5%) issues. The other 34% fell under one of 15 other topics. When you see Anthem members, please tell them about the 24/7 NurseLine program. It’s a helpful resource any time they have a health issue. Future Moms promotes healthy pregnancies and healthy babies Our Future Moms program helps women have a healthy pregnancy, a safe delivery and a healthy baby. The program serves you and our members through education, risk assessments and early interventions. Future Moms supports your plan of care for our members and works with you to: Help them understand the importance of prenatal care and regular clinical visits. Encourage them to make better decisions about their health Spot risks and problems to help ensure they get the help they need. Lower the risk of birth defects and low birth weight. How Future Moms supports you Maternity care providers benefit when we offer these services to our members: Self-help resources so members can be well-informed about their health and care. This takes some of the burden off you. December 2013 Maine 19 of 32 24/7 phone access to a nurse. We do encourage members to talk to you about any concerns. But we take care of basic questions on health, benefits and care management so you don’t have to. Multilingual resources that help members who don’t speak English talk more easily with nurses. Resources include a Network Services Language Line, educational materials in Spanish and TTY capabilities for the speech- and hearing-impaired. Again, this takes some of the burden off you when language is a barrier. Help in authorizing and arranging for home health or other outpatient services. This frees up your time and helps to ensure members get the extra care they need. Updates for you on the health status of high-risk members and proposed interventions. How Future Moms helps members Future Moms guides women toward a healthy lifestyle from the start of the pregnancy until after the baby is born. Participants get: Help tracking the progress of the pregnancy from the first trimester through delivery. Each participant is placed in a high- or low-risk group based on health status and care needs. Customized support from nurses experienced in obstetrics. Participants work with a nurse care manager with at least three years of OB experience. 24/7 toll-free access to nurses. Participants can call with questions or concerns any time. If you’d like to refer Education on proper self-care, diet, signs of pre-term labor and other problems linked to Anthem members pregnancy. into the program, Help on health issues that may affect their pregnancy. We offer support for conditions please call 800-828such as diabetes and high blood pressure. We also help participants with high-risk issues 5891. You can also such as smoking, drug use, high stress levels and domestic matters. find a referral form Help finding health care services and getting referrals. by going to the Follow-up support after the baby is born. The nurse: provider pages at – Checks for postpartum depression anthem.com. Click – Sends educational materials on the Health and – Refers members to behavioral health and EAP programs, social workers and lactation Wellness tab and experts as needed then Future Moms. MyHealth Advantage works with you to help your members MyHealth Advantage uses advanced technology to help our members follow your plan of care. The program helps improve member health and coordination of care. We work with doctors to find and address medical gaps and health risks. How it works MyHealth Advantage scans medical, pharmacy and lab claims. We compare the information with current medical guidelines and best clinical practices. If we find health risks, members get a confidential message called MyHealth Note by mail. We suggest specific actions that when endorsed by their doctors can help the members improve their health. All MyHealth Notes tell members to speak with their doctors before making any changes in their medical care. MyHealth Note also includes a list of recent medical, lab and pharmacy claims that a member can share with you. These may be helpful for you in providing care, especially if members have other doctors. We keep you in the loop If we find a clinical issue, we let you know by mail, too. For example, if the member is overdue for an annual test or if there’s a drug therapy issue, we tell you. If you get a notice, you may add medical information about the member or about the recommendation. You may fax a form back or call a MyHealth Advantage representative. December 2013 Maine 20 of 32 Messages are also posted on two websites, Availity, and MMH+. You can get real-time information when treating individuals in the ER or in the office. MMH+ is a secure and free Internet site where you can check member’s history. Availity is a payment website that shows benefit eligibility, which you can check before an office visit or procedure. Our goal is to offer you updated information to help you take care of our members. Program benefits MyHealth Advantage alerts members if they can save money by switching to a generic drug. The results of the program can include better health through improved compliance with medical standards. A recent study showed 46% of participants who received a MyHealth Note were brought back into clinical compliance. 1 The personal health guidance in MyHealth Note can help members understand their current health status. With MyHealth Note, members can make better decisions for their health and wellness. 1 Based on an internal review of current participants; members acted within 12 months of getting the first MyHealth Note. Member satisfaction survey results regarding physician care Every year we send the Consumer Assessment of Healthcare Providers and Systems (CAHPS®) survey to our HMO/POS members. The survey gives our members an opportunity to share their perceptions of the quality of care and services provided by our HMO/POS network physicians. This same survey is used by all HMO/POS plans that undergo accreditation review by the National Committee for Quality Assurance (NCQA). The following charts compare results from 2012 with those in 2013. You’ll also see two other columns. One reflects the score trend from 2012 to 2013 the other shows the 2013 NCQA Quality Compass Percentile Achieved comparing Anthem network scores to scores from other HMO plans across the country. Our goal is to achieve the 75th Percentile. This is the level we encourage our network physicians to strive to achieve. When you’re reviewing these results, we encourage you to focus on and address those areas of your own practice that may have room for improvement. Addressing those areas will help ensure our members have a positive experience that meets their medical needs and their satisfaction with the level of services provided. 2013 HMO/POS CAHPS® Adult Member Satisfaction Survey Results 2012 2013 Trend 2013 HMO/POS Percentile Achieved 5 84% 84% 87% 89% 75th 90th 79% 81% 75th Got appointment for urgent care as soon as needed 92% 97% 90th Got appointment for check-up or routine care as soon as needed 89% 89% = 75th Survey Question Rating of physician 1 Rating of personal doctor Rating of specialist seen most often Rating of all health care provided in past 12 months Getting Care Quickly 2 December 2013 Maine 21 of 32 Got help or advice needed when calling doctor after regular office hours 77% DNA -- DNA How often personal doctor explained things understandably to you 96% 97% 75th How often personal doctor listened carefully to you 95% 97% 75th How often personal doctor showed respect for what you had to say 98% 98% = 90th How often personal doctor spent enough time with you 95% 96% 90th -- 90% -- DNA -- 64% -- DNA -- 86% -- DNA 84% 87% 90th Doctor’s Communication with Patients 2 Shared Decision Making Doctor discussed reasons to take a medicine 3 Doctor discussed reasons not to take a medicine 3 Did you and your doctor discuss ways to prevent illness? 4 Continuity of Care 2 How often did your personal doctor seem informed about care you received from other health providers? 1 = Percent responding 8, 9 or 10 (0-10, where 0 is the worst and 10 is the best). 2 = Percent responding “Usually” or “Always.” 3 = responding “A lot” or “Some” 4 = % responding "Yes" 5 = Percentile Definition - A score equal to or greater than 75 percent of all those attained on a survey question is said to be in the 75th percentile. DNA = Data not available NA = Number of survey respondents too low to be valid. Consumer Assessment of Healthcare Providers and Systems (CAHPS®) is a registered trademark of the Agency for Healthcare Research and Quality (AHRQ). *The source of data contained in this report is Quality Compass ® 2013 and is used with the permission of the National Committee for Quality Assurance (NCQA). Any analysis, interpretation or conclusion based on these data is solely that of the authors, and NCQA specifically disclaims responsibility for any such analysis, interpretation or conclusion. Quality Compass is a registered trademark of NCQA. HEDIS® 2013 results are in Thank you for participating in the annual Healthcare Effectiveness Data and Information Set (HEDIS) data collection for 2013. You play a central role in promoting the health of our members. One way to improve care is to document services in a consistent way. This makes it easy for you to track care provided and see what additional care is needed to meet the recommended timeframes. Consistent documentation will also help improve HEDIS scores, both by improving care itself and by improving our ability to report validated data. Further information regarding documentation guidelines can be found on the HEDIS page of our website at anthem.com > Providers > select state > Health and Wellness > Quality Improvement and Standards > HEDIS. You will find reference documents titled “HEDIS 101 for Providers” and “HEDIS Documentation Guidelines”. December 2013 Maine 22 of 32 The tables below show some of our key measure rates for our HMO/POS and PPO plans as compared to the Quality Compass® National Averages. HEDIS 2013 Rate (Percent) Effectiveness of Care – Prevention and Screening Adult BMI Assessment 77.14 Breast Cancer Screening 82.50 Cervical Cancer Screening 80.35 Childhood Immunization Status – DTAP 93.06 Childhood Immunization Status – IPV 94.44 Childhood Immunization Status – MMR 93.75 Childhood Immunization Status – HIB 96.53 Childhood Immunization Status – HEP B 90.51 Childhood Immunization Status – VZV 90.28 Childhood Immunization Status – PCV 91.90 Childhood Immunization Status – HEP A 31.48 Childhood Immunization Status – Rotavirus 66.90 Childhood Immunization Status – Influenza 72.45 Colorectal Cancer Screening 76.56 Immunizations for Adolescents – Meningitis 63.08 Immunizations for Adolescents – TDAP/TD 74.08 Weight Assessment and Counseling – BMI Total 43.31 Weight Assessment and Counseling – Nutritional Counseling - Total 70.80 Weight Assessment and Counseling – Physical Activity- Total 67.15 Access/Availability of Care Adults’ Access to Preventive/Ambulatory Health – Total 97.86 Children & Adolescents’ Access to PCP (25 mos-6yrs) 95.44 Children & Adolescents’ Access to PCP (7-11 yrs) 97.03 Children & Adolescents’ Access to PCP (12-19 yrs) 95.97 Effectiveness of Care – Respiratory Conditions Antibiotic Treatment Adults w/ Acute Bronchitis 23.54 Appropriate Testing for Children w/ Pharyngitis 84.52 Appropriate Treatment Children w/ URI 91.92 Spirometry Testing for COPD 42.69 Utilization & Relative Resource Use - Utilization Well-Child Visits in the first 15 Months of Life (0 visits) 0.00 Well-Child Visits in the first 15 Months of Life (1 visit) 0.12 Well-Child Visits in the first 15 Months of Life (3 visits) 0.60 Well-Child Visits in the first 15 Months of Life (6+visits) 91.90 Adolescents Well-Care Visits 51.15 Effectiveness of Care - Cardiovascular Cholesterol Management – LDL-C Control <100 67.95 Persistence of Beta-Blocker Treatment after AMI 95.79 Commercial HMO/POS Measures December 2013 Maine Comparison to National Average 23 of 32 Effectiveness of Care - Diabetes HbA1c Testing Poor HbA1c Control (>9)* Eye Exams LDL-C Controlled (LDL-C<100 mg/dL) Nephropathy Blood Pressure Control <140/80 Blood Pressure Control <140/90 Effectiveness of Care - Musculoskeletal Use of Imaging Studies for Low Back Pain Effectiveness of Care – Behavioral Health Antidepressant Medication Mgmt – Acute Antidepressant Medication Mgmt – Continuation FU Care Children’s ADHD Medication – Initiation FU Care Children’s ADHD Medication – Continuation *lower rate is better Comprehensive Comprehensive Comprehensive Comprehensive Comprehensive Comprehensive Comprehensive Diabetes Diabetes Diabetes Diabetes Diabetes Diabetes Diabetes Care Care Care Care Care Care Care – – – – – – – 93.74 20.00 78.09 51.30 89.22 57.39 76.35 83.23 80.95 63.24 49.01 54.05 HEDIS Commercial PPO Measures 2013 Rate (Percent) Effectiveness of Care – Prevention and Screening Adult BMI Assessment 2.15 Breast Cancer Screening 78.52 Cervical Cancer Screening 76.64 Childhood Immunization Status – DTAP 53.47 Childhood Immunization Status – IPV 67.76 Childhood Immunization Status – MMR 76.64 Childhood Immunization Status – HIB 73.75 Childhood Immunization Status – HEP B 12.16 Childhood Immunization Status – VZV 76.06 Childhood Immunization Status – PCV 57.34 Childhood Immunization Status – HEP A 62.16 Childhood Immunization Status – ROTAVIRUS 45.95 Childhood Immunization Status – INFLUENZA 55.41 Colorectal Cancer Screening 60.91 Immunizations for Adolescents – MENINGITIS 53.57 Immunizations for Adolescents – TDAP/TD 64.09 Weight Assessment and Counseling – BMI TOTAL 1.23 Weight Assessment and Counseling – Nutrition Counseling TOTAL 1.59 Weight Assessment and Counseling – Physical Activity TOTAL 0.66 Access/Availability of Care Adults’ Access to Preventive/Ambulatory Health – TOTAL 95.90 Children’s & Adolescents’ Access to PCP (7-11 yrs) 92.71 Children’s & Adolescents’ Access to PCP (12-19 yrs) 91.86 December 2013 Maine Above or below National Average 24 of 32 Effectiveness of Care – Respiratory Conditions Appropriate Testing for Children w/ Pharyngitis Appropriate Treatment Children w/ URI Spirometry Testing for COPD Utilization & Relative Resource Use - Utilization Well-Child Visits in the first 15 Months of Life (0 visits) Well-Child Visits in the first 15 Months of Life (3 visits) Well-Child Visits in the first 15 Months of Life (6+visits) Adolescent Well-Care Visits Effectiveness of Care - Cardiovascular Cholesterol Management – LDL-C Control <100 Persistence of Beta-Blocker Treatment after AMI Effectiveness of Care - Diabetes Comprehensive Diabetes Care – HbA1c Testing Comprehensive Diabetes Care – Poor HbA1c Control (>9)* Comprehensive Diabetes Care – Eye Exams Comprehensive Diabetes Care – LDL-C Controlled (LDL-C<100 mg/dL) Comprehensive Diabetes Care – Nephropathy Effectiveness of Care - Musculoskeletal Use of Imaging Studies for Low Back Pain Effectiveness of Care – Behavioral Health Antidepressant Medication Mgmt – Acute Antidepressant Medication Mgmt – Continuation FU Care Children’s ADHD Medication – Initiation FU Care Children’s ADHD Medication – Continuation *lower rate is better December 2013 Maine 86.14 90.38 40.39 4.56 0.91 66.06 48.46 1.24 83.02 88.21 98.45 54.80 1.50 80.93 83.69 75.70 60.39 44.31 50.00 25 of 32 This year our commercial HMO product had rate increases in multiple important measures with most remaining above the national average. The exception was IMA where both measures showed an increase from last year but did not meet the national average, Tdap with a 4.40% increase and meningococcal with a 3.82% increase. Persistence of beta-blocker treatment after AMI had the most significant increase with 13.35% improved. The behavioral health measures showed improvement in rates of 0.99% to 9.21%, WCC nutrition counseling and counseling for physical activity both increased, 3.90% and 2.57% respectively with all above the national average. R A T E 100 50 0 IMA-… IMA-… COLO… BETA… WELL… ANTI… ANTI… P E R C E N T A G E MAINE COMMERCIAL PPO 2013 HEDIS RATE INCREASES vs. NATIONAL AVERAGE HEDIS MEASURE 2012 2013 NAT'L AVERAGE Our commercial PPO product experienced double digit increases in many of the childhood immunization measures ranging from 8.41% improvement for influenza to 67.76% for IPV, while only rotavirus, Hep A and VZV are below the national average. Both IMA measures increased meningitis by 9.67% and Tdap 11.59% and increases were seen in colorectal cancer screening of 3.11%, persistence of beta-blocker treatment after AMI of 12.12% and well child visits 6+ visits of 18.46% with all above the national average. The behavioral health measures showed increases in antidepressant medication mgmt-acute 7.10% and continuation of 8.79% with both above the national average. P E R C E N T A G E December 2013 MAINE COMMERCIAL HMO 2013 HEDIS RATE DECREASES vs. NATIONAL AVERAGE R A T E 100 50 2012 0 2013 HEDIS MEASURES Maine NAT'L AVERAGE 26 of 32 In the commercial HMO product, multiple important measures showed decreased rates. All childhood immunizations rates declined while three fell below the national average including VZV, Hep A and rotavirus. All comprehensive diabetes care rates fell but remain above the national average while WCC BMI total fell 5.53% and is below the national average. Appropriate testing children with pharyngitis fell 1.08% and spirometry testing for COPD fell 1.99%, CBP fell 6.02% and timeliness of prenatal care fell 4.43% For our commercial PPO product, there was a decline in rates for several of the important measures - most less than 5%. All components of the comprehensive diabetes care measure fell less than 5% (0.07 – 2.55%) but all remained above the national average. Follow up care children’s ADHD medication-initiation fell 4.89% and continuation fell 1.20%, while LDL screening fell the most at 5.10% with all remaining above the national average. Childhood immunization status (CIS) - Hep B fell 1.92% and is below the national average. Each year our goal is to improve our process for requesting and obtaining medical records for our HEDIS project, and to demonstrate the exceptional care that you have provided to our members. In an effort to improve our scores, you and your office staff can help facilitate the HEDIS process improvement by: responding to our requests for medical records within five days providing the appropriate care within the designated timeframes coding all claims accurately documenting all care in the member’s medical record Again, we thank you and your staff for demonstrating teamwork and collaboration as we work together to help improve the health of our members. We look forward to working with you next HEDIS season. The source for data contained in this publication is Quality Compass® 2013 and is used with the permission of the National Committee for Quality Assurance (NCQA).Quality Compass 2013 includes certain CAHPS data. Any data display, analysis, interpretation, or conclusion based on these data is solely that of the authors, and NCQA December 2013 Maine 27 of 32 specifically disclaims responsibility for any such display, analysis, interpretation, or conclusion. Quality Compass is a registered trademark of NCQA. CAHPS® is a registered trademark of the Agency for Healthcare Research and Quality (AHRQ). HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA) Quality Compass® is a registered trademark of the National Committee for Quality Assurance (NCQA). Pharmacy update Pharmacy information available on anthem.com Visit http://www.anthem.com/pharmacyinformation for more information on copayment/coinsurance requirements and their applicable drug classes, Drug Lists and prior authorization criteria, procedures for generic substitution, therapeutic interchange, step therapy or other management methods subject to prescribing decisions, and any other requirements, restrictions or limitations that apply to certain drugs. Coverage for compound drugs Due to the recent enhancement of the HIPAA standard for electronic submission of prescription drug claims, we now have the ability to better administer our drug benefits as they pertain to compounded drugs. During a recent review, we identified that claims for certain compounded drugs have been submitted and paid as a prescription drug benefit. For a compound drug to be covered, it must contain at least one ingredient/drug that requires a prescription to obtain. Additionally, that ingredient/drug must also be approved by the Food and Drug Administration (FDA). Claims for certain compound drugs paid prior to November 1, 2013, will no longer be paid. These include: Compounded bulk powders (not FDA approved) Pharmaceutical adjuvants (compounding vehicles, not FDA approved) Letters were mailed to impacted members in advance of this change. Please note: We will still cover compound drugs whose primary ingredient is FDA-approved and not otherwise excluded, as defined under the Plan. Medical policy update Medical policy updates are available on anthem.com The following new and revised policies were endorsed at the August 8, 2013 Medical Policy & Technology Assessment Committee (MPTAC) meeting. These, and all Anthem medical policies, are available at anthem.com > Providers > Select state > Enter > Medical Policies and Clinical UM Guidelines. If you do not have access to the Internet, you may request a hard copy of any updated policy by calling Provider Service at 800-832-6011. Revised medical policies effective August 12, 2013 (The following policies were revised to expand medical necessity indications or criteria.) DRUG.00002 Tumor Necrosis Factor Antagonists December 2013 Maine 28 of 32 DRUG.00038 DRUG.00043 MED.00080 SURG.00017 SURG.00055 SURG.00122 Bevacizumab (Avastin®) for Non-Ophthalmologic Indications Tocilizumab (Actemra®) Cryopreservation of Oocytes or Ovarian Tissue Stereotactic Radiosurgery (SRS) and Stereotactic Body Radiotherapy (SBRT) Cervical Artificial Intervertebral Discs Venous Angioplasty with or without Stent Placement Revised medical policies effective October 8, 2013 (The following policies were revised to expand medical necessity indications or criteria.) RAD.00035 Coronary Artery Imaging: Contrast – Enhanced Coronary Computed Tomography Angiography (CCTA), Coronary Magnetic Resonance Angiography (MRA), and Cardiac Magnetic Resonance Imaging (MRI) SURG.00064 Cardiac Resynchronization Therapy (CRT) with or without an Implantable Cardioverter Defibrillator (CRT/ICD) for the Treatment of Heart Failure Revised medical policies effective October 8, 2013 (The following policies were reviewed and may have word changes or clarifications, but had no significant changes to the policy position or criteria.) ADMIN.00001 ADMIN.00002 ADMIN.00004 ADMIN.00005 ADMIN.00006 ANC.00006 ANC.00007 ANC.00008 ANC.00009 BEH.00004 DME.00004 DME.00024 DME.00027 DME.00030 DRUG.00017 DRUG.00031 DRUG.00044 GENE.00002 GENE.00015 GENE.00021 LAB.00011 LAB.00016 LAB.00027 MED.00064 MED.00081 MED.00090 December 2013 Medical Policy Formation Preventive Health Guidelines Medical Necessity Criteria Investigational Criteria Review of Services for Benefit Determination in the Absence of a Company Applicable Medical Policy or Clinical Utilization Management (UM) Guideline Biomagnetic Therapy Cosmetic and Reconstructive Services: Skin Related Cosmetic and Reconstructive Services of the Head and Neck Cosmetic and Reconstructive Services of the Trunk and Groin Behavioral Health Treatments for Autism Spectrum Disorders and Rett Syndrome Electric Bone Growth Stimulation Transtympanic Micropressure for Treatment of Meniere’s Disease Ultrasound Bone Growth Stimulation Altered Auditory Feedback (AAF) Devices for the Treatment of Stuttering Hyaluronan Injections in Joints Other than the Knee Subcutaneous Hormone Replacement Implants Belimumab (Benlysta®) Preimplantation Genetic Diagnosis Testing Predictive Genetic Testing for Non-Malignant Diseases Cytogenomic Microarray Analysis (CMA) for Developmental Delay, Autism Spectrum Disorder and Mental Retardation Analysis of Proteomic Patterns Fecal Analysis in the Diagnosis of Intestinal Dysbiosis Antigen Leukocyte Cellular Antibody Test (ALCAT) for Chemical and Food Allergies Transcatheter Ablation of Arrhythmogenic Foci in the Pulmonary Veins as a Treatment of Atrial Fibrillation (Radiofrequency and Cryoablation) Cognitive Rehabilitation Wireless Capsule for the Evaluation of Suspected Gastric and Intestinal Motility Disorders Maine 29 of 32 MED.00098 MED.00107 MED.00112 RAD.00019 RAD.00023 RAD.00034 RAD.00042 RAD.00045 RAD.00046 RAD.00060 RAD.00063 SURG.00005 SURG.00007 SURG.00010 SURG.00011 SURG.00020 SURG.00023 SURG.00047 SURG.00048 SURG.00049 SURG.00051 SURG.00054 SURG.00059 SURG.00066 SURG.00071 SURG.00074 SURG.00076 SURG.00077 SURG.00084 SURG.00085 SURG.00089 SURG.00090 SURG.00105 SURG.00116 SURG.00117 SURG.00118 SURG.00125 SURG.00126 SURG.00131 SURG.00132 SURG.00133 SURG.00134 December 2013 Hyperoxemic Reperfusion Therapy Medical and Other Non-Behavioral Health Related Treatments for Autism Spectrum Disorders and Rett Syndrome Autonomic Testing Magnetic Source Imaging and Magnetoencephalography Single Photon Emission Computed Tomography ( SPECT) Scans for Noncardiovascular Indications Dynamic Spinal Visualization (Including Digital Motion X-ray and Cineradiography / Videofluroscopy) SPECT/CT Fusion Imaging Cerebral Perfusion Imaging using Computed Tomography Cerebral Perfusion Studies using Diffusion and Perfusion Magnetic Resonance Imaging Digital Breast Tomosynthesis Magnetization-Prepared Rapid Acquisition Gradient Echo Magnetic Resonance Imaging (MPRAGE MRI) Partial Left Ventriculectomy Vagus Nerve Stimulation Treatments for Urinary Incontinence Allogeneic, Xenographic, Synthetic and Composite Products for Wound Healing and Soft Tissue Grafting Bone-Anchored Healing Aids Breast Procedures: including Reconstructive Surgery, Implants and Other Breast Procedures Transendoscopic Therapy for Gastroesophageal Reflux Disease and Dysphagia Panniculectomy and Abdominoplasty Mandibular/Maxillary (Orthognathic) Surgery Hip Resurfacing Endovascular / Endoluminal Repair of Aortic Aneurysms, Aortoiliac Disease, Aortic Dissection and Aortic Transection Recombinant Human Bone Morphogenetic Protein Percutaneous Neurolysis for Chronic Neck and Back Pain Percutaneous and Endoscopic Spinal Surgery Nasal Surgery for the Treatment of Obstructive Sleep Apnea (OSA) and Snoring Nerve Graft after Prostatectomy Uterine Fibroid Ablation: Laparoscopic or Percutaneous Image Guided Techniques Implantable Middle Ear Hearing Aids Mastectomy for Gynecomastia Balloon Sinus Ostial Dilation Radiofrequency and Pulsed Radiofrequency Neurolysis for Trigeminal Neuralgia (TGN) Bicompartmental Knee Arthroplasty High Resolution Anoscopy Screening for Anal Intraepithelial Neoplasia (AIN) and Squamous Cell Cancer of the Anus Sacral Nerve Stimulation (SNS) and Percutaneous Tibial Nerve Stimulation (PTNS) for Urinary and Fecal Incontinence; Urinary Retention Bronchial Thermoplasty Radiofrequency and Pulsed Radiofrequency Ablation of Trigger Point Pain Irreversible Electroporation (IRE) Lower Esophageal Sphincter Augmentation Devices for the Treatment of Gastroesophageal Reflux Disease (GERD) Devices for Maintaining Sinus Ostial Patency Following Sinus Surgery Alcohol Septal Ablation for Treatment of Hypertrophic Cardiomyopathy Interspinous Fixation Devices Maine 30 of 32 TRANS.00014 TRANS.00035 Mechanical Circulatory Assist Devices (Ventricular Assist Devices, Percutaneous Ventricular Assist Devices and Artificial Hearts) Mesenchymal Stem Cell Therapy for Orthopedic Indications Revised medical policies effective March 1, 2014 (The policies listed below might result in services that were previously covered now being considered either not medically necessary and/or investigational.) DRUG.00015 Prevention of Respiratory Syncytial Virus Infections DRUG.00038 Bevacizumab (Avastin®) for Non-Ophthalmologic Indications GENE.00001 Genetic Testing for Cancer Susceptibility SURG.00037 Treatment of Varicose Veins (Lower Extremity) New medical policies effective March 1, 2014 (The policies listed below were created and might result in services that were previously covered now being considered either not medically necessary and/or investigational.) DME.00037 Cooling Devices and Combined Cooling/Heating Devices DRUG.00055 Denosumab (Prolia®, Xgeva™) DRUG.00057 Canakinumab (Ilaris®) DRUG.00058 Pharmacotherapy for Hereditary Angioedema LAB.00030 Measurement of Serum Concentrations of Infliximab (IFX) or Antibodies-to-Infliximab (ATI) Clinical guidelines update Clinical guideline updates are available on anthem.com The following new and revised clinical guidelines were endorsed at the August 8, 2013 Medical Policy & Technology Assessment Committee (MPTAC) meeting. These, and all Anthem medical policies, are available at anthem.com > Providers > Select state > Enter > Medical Policies and Clinical UM Guidelines. If you do not have access to the Internet, you may request a hard copy of any updated policy by calling Provider Service at 800-832-6011. New clinical guidelines adopted effective October 8, 2013 (The following guidelines were adopted and have no significant changes to reimbursement.) CG-BEH-03 Psychiatric Disorder Treatment CG-BEH-04 Substance Abuse Treatment CG-BEH-05 Eating Disorder Treatment CG-BEH-06 Psychiatric Outpatient Treatment CG-BEH-07 Psychological and Neuropsychological Testing Revised clinical guidelines effective October 8, 2013 (The following adopted guidelines were revised to expand medical necessity indications or criteria.) CG-DRUG-11 Infertility Drugs CG-DRUG-28 Alglucosidase alfa (Lumizyme®, Myozyme®) December 2013 Maine 31 of 32 Revised clinical guidelines effective October 8, 2013 (The following adopted guidelines were revised and had no significant changes to the position or criteria.) CG-DME-07 Augmentative and Alternative Communication (AAC) Devices/Speech Generating Devices (SGD) CG-DRUG-27 Clostridial Collagenase Histolyticum Injection CG-MED-31 Skilled Nursing Facility Services CG-REHAB-09 Acute Inpatient Rehabilitation CG-SURG-05 Maze Procedure CG-SURG-08 Sacral Nerve Stimulation as a Treatment of Neurogenic Bladder Secondary to Spinal Cord Injury CG-SURG-18 Septoplasty CG-SURG-24 Functional Endoscopic Sinus Surgery (FESS) CG-SURG-27 Gender Reassignment Surgery New clinical guideline adopted effective March 1, 2014 (The guideline listed below is being adopted and might result in services that were previously covered but may now be found to be either not medically necessary and/or investigational.) CG-BEH-02 Applied Behavioral Analysis for Autism Spectrum Disorder December 2013 Maine 32 of 32