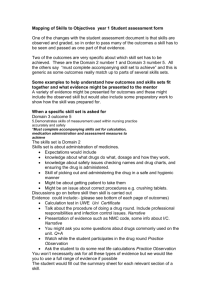
-1- Stages of infections: The body's defense against infection:
advertisement

University of Kerbala / College of Nursing Fundamentals of Nursing Department Subject: Fundamentals of Nursing I Asepsis and infection control Assistant Instructor: Hassan Abdullah athbi Stages of infections: 1 2 3 4 5 6 7 8 9 10 11 An infection progresses through the following phases: 1) Incubation period: the time between the entry of infectious agents in the host and the onset of nonspecific symptoms. During this time the infectious agent invades the tissue and multiplies to produce infection. 2) Prodromal stage: the time from the onset of nonspecific symptoms until specific symptoms begin manifested. 3) Full stage of illness: the time when the client has specific signs and symptoms of an infectious disease. 4) Convalescent period: the time from the beginning of the disappearance of acute symptoms until the client returns to the previous state of health. 12 The body's defense against infection: 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 1. Nonspecific defenses: protect the person against all microorganisms, regardless of prior exposure. Nonspecific defenses include: a. Anatomic and physiological barriers: Intact skin and mucous membrane are the body's first line of defense against microorganisms. Cilia in the respiratory passage has protective mechanisms against infection, Tears in the eye has protective mechanisms against infection, Acidity of the stomach has protective mechanisms against infection, Resident flora of the large intestine help to prevent the establishment of microorganisms, peristalsis also tend to move microbes out of the body, The vagina also has natural defenses against infection (low pH 3.5-4.5 of vaginal secretions inhibits the growth of many disease producing microorganisms), It is believed that the urine flow has a flushing and bacteriostatic action that keep the bacteria from ascending the urethra. b. Inflammatory response: Inflammation: Is a local and nonspecific defensive response of the tissue to injurious or infectious agent. It is characterized by: 1. Redness (erythema): result from increase blood flow to the area. 2. Heat: results from increase blood flow and metabolism in the area. 3. Pain: result from increased pressure by the accumulating fluid on nerve endings and the irritating chemical mediators in the area. 4. Swelling(edema): result from fluid and electrolytes entering the tissues from the circulatory system. 5. Loss of function: result from both pain and swelling. 6. Pus (purulent exudates): resulting from infection, is a secretion made up of white blood cells, dead cells, bacteria, and other debris. 31 32 33 34 35 36 37 38 39 Fundamentals of Nursing I -1- University of Kerbala / College of Nursing Fundamentals of Nursing Department Subject: Fundamentals of Nursing I Asepsis and infection control Assistant Instructor: Hassan Abdullah athbi 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 Stages of inflammatory response: a. Vascular and cellular responses: At the start of the first stage of inflammation, blood vessels at the site of injury constrict. This is rapidly followed by dilatation of small blood vessel , thus more blood flows to the injured area as a result of vasodilatation at the site of injury that’s responsible for signs of redness and heat .Vascular permeability increases at the site with dilation of the vessels in response to cell death, the release of chemical mediators (serotonin and prostaglandin), and the release of histamine. Fluid , protein, and leukocytes (WBCs) leak into the interstitial spaces, and the signs of inflammation (swelling, and pain) appear. b. Exudates production: consisting from fluid that escaped from the blood vessels, dead phagocytic cells, and dead tissue cells and products that’s release. c. Reparative phase: involves the repair of injured tissues by regeneration or replacement with fibrous tissue (scar) formation. 2. Specific defenses: involve the immune system, are directed against identifiable infectious agent. Factors increasing susceptibility to infection: 1. Age (newborns and older adults have reduced defenses against infections). 2. Heredity (some may be deficient in serum immunoglobulin). 3. Level of stress (stressors elevated blood cortisone, prolonged elevation of blood cortisone decrease anti-inflammatory responses, depletes energy stores, lead to state of exhaustion, and decreases resistance to infection). 4. Nutritional status ( the ability of synthesize antibodies may be impaired by inadequate nutrition). 5. Current medical therapy (for example anticancer may depress bone marrow function resulting in inadequate production of WBCs). 6. Preexisting disease processes. 28 Fundamentals of Nursing I -2-