Signaling pathways perturbing muscle mass
advertisement

Signaling pathways perturbing muscle mass
David J. Glass
Novartis Institutes for Biomedical Research,
Cambridge, Massachusetts, USA
Correspondence to David J. Glass, Novartis Institutes
for Biomedical Research, 100 Technology Square,
Cambridge, MA 02139, USA
Tel: +1 617 871 7820;
e-mail: david.glass@novartis.com
Current Opinion in Clinical Nutrition and
Metabolic Care 2010, 13:225–229
Purpose of review
To discuss the mechanisms of muscle loss during cachexia.
Recent findings
Cachexia can be defined as a wasting of lean body mass that cannot be reversed
nutrionally, indicating a dysregulation in the pathways maintaining body composition. In
skeletal muscle, during cachexia, there is an upregulation of protein degradation. A
search for transcriptional markers of muscle atrophy led to the discovery of the E3
ubiquitin ligases MuRF1 and MAFbx (also called Atrogin-1). These genes are
upregulated in multiple models of atrophy and cachexia. They target particular protein
substrates for degradation via the ubiquitin/proteasome pathway. The insulin-like
growth factor-1 can block the transcriptional upregulation of MuRF1 and MAFbx via the
phosphatidylinositol-3 kinase/Akt/Foxo pathway. MuRF1’s substrates include several
components of the sarcomeric thick filament, including myosin heavy chain. Thus, by
blocking MuRF1, insulin-like growth factor-1 prevents the breakdown of the thick
filament, particularly myosin heavy chain, which is asymmetrically lost in settings of
cortisol-linked skeletal muscle atrophy.
Insulin-like growth factor-1/phosphatidylinositol-3 kinase/Akt signaling also dominantly
inhibits the effects of myostatin, which is a member of the transforming growth factor-b
family of proteins. Deletion or inhibition of myostatin causes a significant increase in
skeletal muscle size. Recently, myostatin has been shown to act both by inhibiting gene
activation associated with differentiation, even when applied to postdifferentiated
myotubes, and by blocking the phosphatidylinositol-3 kinase/Akt pathway.
Summary
These findings will help to define strategies to treat cachexia.
Keywords
Akt, MuRF1, myosin, myosin heavy chain, myostatin, skeletal muscle atrophy
Curr Opin Clin Nutr Metab Care 13:225–229
ß 2010 Wolters Kluwer Health | Lippincott Williams & Wilkins
1363-1950
Introduction
Skeletal muscle atrophy occurs in a variety of settings,
including disuse, denervation, cachexia, renal failure, and
burns [1,2]. Endogenous cortisol is upregulated in many
of these settings of cachexia [3,4]. It is probable that this
cortisol effect is sufficient to mediate skeletal muscle
atrophy, as high levels of synthetic glucocorticoids such as
dexamethasone (DEX) are sufficient to cause loss of
muscle mass [5–9].
Skeletal muscle hypertrophy can be mediated by the
induction of insulin-like growth factor-1 (IGF-1), which
is a protein growth factor that is sufficient to induce
skeletal muscle mass [10,11]. IGF-1 acts in part by
stimulating the phosphatidylinositol-3 kinase (PI3K)/
Akt pathway, resulting in the downstream activation of
targets that induce protein synthesis [12,13]. Activation of
Akt is sufficient to induce hypertrophy in vivo, as was
shown by the production of transgenic mice in which a
1363-1950 ß 2010 Wolters Kluwer Health | Lippincott Williams & Wilkins
mutant, constitutively active, form of Akt is conditionally
expressed in adult skeletal muscle [14,15,16]. Acute
activation of Akt in an adult animal, for 2 weeks, was
sufficient to induce a doubling in the size of skeletal
muscle; this increase occurs via an increase in the average
cross-sectional area of individual muscle fibers, caused by
an increase in TORC1/p70S6K protein synthesis pathways [14]. Conversely, in settings of skeletal muscle
atrophy, Akt activation is downregulated [17].
In addition to stimulating protein synthesis, IGF-1 acts
by inhibiting the induction of skeletal muscle atrophy
pathways. A distinct set of genes are inversely regulated
under IGF-1-induced hypertrophy conditions vs. DEXinduced atrophy [7]; these include the gene MAFbx [18]
(for Muscle Atrophy F-box; also called Atrogin-1 [19]). A
second gene, MuRF1 [18] (for Muscle Ring Finger1), is
significantly upregulated under atrophy conditions [18].
Both MuRF1 and MAFbx/Atrogin encode E3 ubiquitin
ligases [18]. Expression of MuRF1 and MAFbx is
DOI:10.1097/MCO.0b013e32833862df
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
226 Anabolic and catabolic signals
stimulated in multiple distinct models of skeletal
muscle atrophy [18–22]. Mice that are null for MuRF1
(MuRF1 / ) and mice that are null for MAFbx
(MAFbx / ) appear phenotypically normal. However,
under atrophy conditions, significantly less muscle mass
is lost in either MuRF1 / or MAFbx / animals in
comparison to control littermates [18].
Skeletal muscle atrophy occurs via induction
of the E3 ubiquitin ligases MuRF1 and
MAFbx/atrogin-1
MuRF1 encodes a protein that contains a RING-finger
domain [23]. RING-finger domains are responsible for
the ubiquitin ligase activity [24] of the E3 ligases that
contain them, as it is this domain that interacts with the
ubiquitin-conjugating E2 enzyme [24]. In a recent study,
a mouse was produced in which only the RING domain of
MuRF1 was deleted [25]. These MuRF1 RING /
animals produce the remainder of the MuRF1 protein,
which would presumably allow for otherwise normal
MuRF1-mediated protein–protein interactions. The
MuRF1 RING / animals demonstrated an identical
phenotype to that of the previously published MuRF1
nulls, in which the entire MuRF1 gene was deleted: a
phenotypically ‘normal’ appearance in the unperturbed
state; less muscle loss under atrophy conditions [25].
This demonstrated that MuRF1 mediates the loss of
skeletal muscle by virtue of its E3 ubiquitin ligase
activity. This in-vivo finding confirmed previously published in-vitro data that also showed the requirement for
the RING domain [18]. MuRF1 has been shown to bind
to the myofibrillar protein titin, at the M line [26–28], but
it is not clear that MuRF1 actually causes the ubiquitination of titin.
The discovery of substrates for MuRF1 came from binding studies. MuRF1 and myosin heavy chain (MyHC)
physically interact – as demonstrated by immune precipitation of epitope-tagged MuRF1 protein, which coimmunoprecipitated MyHC protein [29]; this finding led
to the discovery that MyHC was a substrate of MuRF1
[29], which was demonstrated by several lines of evidence: first, MyHC was shown to be degraded by a
ubiquitin/proteasome-mediated pathway [30]; second,
loss of MyHC was blocked using proteasome inhibitors
[29] and by IGF-1 [30]; third, loss of MyHC was blocked
by siRNA-mediated inhibition of MuRF1[29]; fourth,
MyHC was found to be spared in MuRF1 / in comparison to wild-type mice under DEX-induced atrophy
conditions [29]; and finally, MuRF1 was able to directly
ubiquitinate MyHC in vitro [29]. Subsequently, it was
demonstrated that several other proteins in the thick
filament of muscle were also degraded by MuRF1,
including myosin light chain and myosin-binding protein
C [25]. Interestingly, the loss of myosin-binding protein
C occurs by distinct mechanisms, including transcriptional downregulation under atrophy conditions [31].
MAFbx/Atrogin-1 contains an F-box domain, a characteristic motif seen in a family of E3 ubiquitin ligases
called SCFs (for Skp1, Cullin, F-box) [32]. F-box-containing E3 ligases usually bind a substrate only after that
substrate has first been post-translationally modified, for
example, by phosphorylation [32]. This suggests the
possibility of a signaling pathway in which a potential
substrate is first phosphorylated as a response to an
atrophy-induced stimulus and then degraded via MAFbx.
Substrates have been reported for MAFbx in skeletal
muscle, including MyoD [33] and eIF3f [34,35]. eIF3f is a
translation initiation factor; it is ubiquitinated and
degraded in a MAFbx-dependent manner in myotubes
[34]; and upregulation of MAFbx causes breakdown of
eIF3f [34], giving a mechanism for MAFbx to control
protein synthesis in addition to protein breakdown [34].
In cardiac muscle, it was shown that though MAFbx has
no effect on Akt activation in response to IGF-1 or insulin
challenge in cardiomyocytes, nevertheless MAFbx can
repress Akt-dependent hypertrophy by activating the
Forkhead transcription factors via a distinct type of
ubiquitination – ubiquitination using lysine 63, which
perturbs transcriptional activity (in this case that of the
FOXO transcription factors) rather than inducing proteasomal degradation [36]; FOXO activation was shown to
be required to activate the atrophy transcriptional program [37,38], as will be discussed further. Because FOXO
proteins regulate MAFbx expression in skeletal and
cardiac muscle, these findings indicated the presence
of a feed-forward mechanism in which MAFbx is activated by, and in turn coactivates, FOXO3a and FOXO1
[36], making it clear why IGF-1’s ability to inhibit FOXO
via activation of Akt is necessary to inhibit uncontrolled
atrophy in skeletal muscle.
Insulin-like growth factor-1/
phosphatidylinositol-3 kinase/Akt inhibition
of FOXO transcription factors blocks
upregulation of MuRF1 and MAFbx
Studies of differentiated myotube cultures demonstrated
that treatment of myotubes with the cachectic glucocorticoid DEX promotes enhanced protein breakdown and
increased expression of genes broadly involved in the
ubiquitin-proteasome proteolytic pathway [39–41]. Invitro treatment of myotubes with DEX induces atrophy,
accompanied by the specific increased expression of
MAFbx and MuRF1 [37,38]. The upregulation of MAFbx
and MuRF1 was antagonized by simultaneous treatment
with IGF-1 [8,37,38], acting through the PI3K/Akt pathway [37,38]; this finding demonstrated a novel role for
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Signaling pathways perturbing muscle mass Glass 227
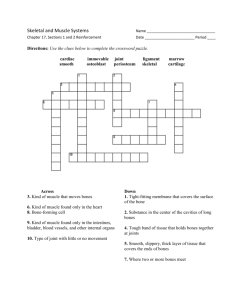
Figure 1 Signaling diagram illustrating myostatin, transforming growth factor-b, and insulin-like growth factor-1 pathway
interactions
Myostatin’s effects require both Smad2 and Smad3, which block muscle differentiation, including the E3 ligases MuRF1 and MAFbx, which are
normally upregulated during muscle atrophy. MuRF1 ubiquitinates myosin heavy chain (MyHC; not in figure). This distinguishes the effects of myostatin
with ‘typical atrophy’. Smad2 and 3 activation are both required for myostatin’s inhibitory effects on Akt. Inhibition of RAPTOR, and thus TORC1, is
additive with myostatin signaling. Smad2,3 phosphorylation increases when RAPTOR is downregulated. RICTOR is itself sufficient to block
differentiation. Transforming growth factor-b (TGF-b) family members that signal through the TGF-b type II receptor can also activate Smad2
and 3. Treatment with insulin-like growth factor-1 (IGF-1) can counteract myostatin’s antidifferentiation effects, indicating the IGF-1/Akt pathway is
dominant over the myostatin pathway.
Akt – in addition to stimulating skeletal muscle hypertrophy, Akt stimulation could dominantly inhibit the
induction of atrophy signaling (Fig. 1). Similarly, MuRF1
and MAFbx were activated in a separate model of atrophy,
diabetes, and here too IGF-1 blocked the transcriptional
upregulation [42]. Genetic activation of Akt was shown to
be sufficient to block the atrophy-associated increases in
MAFbx and MuRF1 transcription [38]. The mechanism
by which Akt inhibited MAFbx and MuRF1 upregulation
was demonstrated to involve the FOXO family of transcription factors [37,38,42]. In myotubes, FOXO transcription factors are excluded from the nucleus when
phosphorylated by Akt and translocate to the nucleus
upon dephosphorylation. The translocation and activity
of FOXO transcription factors is required for upregulation of MuRF1 and MAFbx – in the case of FOXO3,
activation was demonstrated to be sufficient to induce
atrophy [37], a finding that was subsequently supported
by the transgenic expression of FOXO1, which resulted
in atrophic phenotype [43].
Akt regulation of myostatin
In addition to IGF-1, other secreted proteins have been
demonstrated to perturb skeletal muscle size. Myostatin,
also called growth and differentiation factor 8 (GDF-8), is a
transforming growth factor-b (TGF-b) family member,
which is a negative regulator of muscle mass [42]. Myostatin’s effect was demonstrated in studies with mice which
were made null for the myostatin gene [44] and also by
correlating increases in muscle mass that were observed in
strains of cattle with a loss of myostatin [45–47]; the loss of
myostatin resulted in more than doubling in muscle mass.
It has been suggested that other TGF-b superfamily
molecules, distinct from myostatin, play a role in modulating skeletal muscle size, because myostatin / mice that
are mated with mice that are transgenic for follistatin
(TGfollistatin), which is capable of inhibiting not only myostatin, but also its close relative GDF-11, and other TGF-b
molecules such as the activins, resulted in an even greater
increase in muscle size [48].
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
228 Anabolic and catabolic signals
In-vitro studies with myostatin have been performed on
rodent cells. In these studies, it has been shown that
myostatin can block the differentiation of myoblasts into
myotubes [49–52]. Experiments both in vitro and in vivo
have demonstrated that myostatin signals by first binding
the type II activin receptor, IIb, which then allows for
interaction with type I receptors ALK4 or ALK5 [53].
The binding of myostatin to these receptor complexes
results in the phosphorylation and activation of the transcription factors Smad2 and Smad3, which translocate to
the nucleus upon phosphorylation [54]. In a study of
myostatin and other TGF-b molecules on human
skeletal myoblasts (HuSkMC) and myotubes, HuSkMCs
respond to myostatin at physiologic concentrations,
0.1–300 ng/ml, resulting in a decrease in fusion index,
myotube diameter, creatine kinase activity, and expression of MyoD and myogenin [55]. It was previously
demonstrated that follistatin, a more general inhibitor of
TGF-b molecules, could induce an additive increase in
muscle mass when combined with myostatin [48]. A
range of other TGF-b molecules are shown to be able
to block muscle differentiation, including the more distantly related activins, and BMP-2 [55]. Myostatin
inhibits activation of Akt, in both myoblasts and myotubes [55,56]. It was recently reported that musclespecific ablation of TORC1 (by ablating RAPTOR)
results in a dystrophic phenotype [57]. Inhibition of
RAPTOR, and thus TORC1, does not by itself block
muscle differentiation, but does contribute to myostatin’s
inhibitory effects, by resulting in an increase in myostatin-induced Smad phosphorylation, establishing a feedforward mechanism: myostatin activates Smad2, which
inhibits Akt, inhibiting TORC1, which in turn potentiates myostatin’s activation of Smad2 [55,56]. These
findings are outlined in Fig. 1.
Addition of IGF-1 dominantly blocks the effects of
myostatin, when applied to either myoblasts or myotubes
[55]. The precise intersection between the two pathways may be multifold, but it is clear that Akt is a
particular nexus and that IGF-1 can rescue the activation
of the PI3K/Akt pathway that is blunted by myostatin.
The demonstration that IGF-1 can dominantly overcome
myostatin inhibition via this pathway adds to the rationale for treatment regimens that activate the PI3K/Akt
pathway in clinical settings wherein myostatin is active.
Conclusion
A considerable amount of recent progress has been made
in the understanding of the signaling pathways that
mediate skeletal muscle hypertrophy and atrophy.
Whereas it was appreciated many years ago that hypertrophy comes about via an increase in the rate of protein
synthesis and atrophy through an increase in protein
degradation, only now can specific signaling pathways
be drawn, as the particular molecular mediators of hypertrophy and atrophy in skeletal muscle have only recently
been determined. Furthermore, it is only through recent
studies that it is understood that hypertrophy pathways
are dominant over the induction of atrophy mediators.
These findings help to give hope that novel drug targets
may be found to block skeletal muscle atrophy, seen in a
variety of clinical conditions, from the cachexia of AIDS,
sepsis, and cancer, to the gradual loss of muscle mass
observed during normal aging.
Acknowledgements
The authors would like to thank Drs. M. Fishman, B. Richardson, A.
Mackenzie, E. Trifilieff and the rest of the Novartis Muscle group as well
as the rest of the Novartis community for their enthusiastic support and
input.
References and recommended reading
Papers of particular interest, published within the annual period of review, have
been highlighted as:
of special interest
of outstanding interest
Additional references related to this topic can also be found in the Current
World Literature section in this issue (p. 346).
1
Glass DJ. Molecular mechanisms modulating muscle mass. Trends Mol Med
2003; 9:344–350.
2
Glass DJ. Skeletal muscle hypertrophy and atrophy signaling pathways. Int J
Biochem Cell Biol 2005; 37:1974–1984.
3
Bajusz E. Disuse atrophy of skeletal muscle in the rat, aggravated by cortisol
and various stress conditions. Can J Biochem Physiol 1958; 36:824–831.
4
Jaspers SR, Tischler ME. Role of glucocorticoids in the response of rat leg
muscles to reduced activity. Muscle Nerve 1986; 9:554–561.
5
Chromiak JA, Vandenburgh HH. Glucocorticoid-induced skeletal muscle
atrophy in vitro is attenuated by mechanical stimulation. Am J Physiol Cell
Physiol 1992; 262:C1471–1477.
6
Grounds MD. Reasons for the degeneration of ageing skeletal muscle: a
central role for IGF-1 signalling. Biogerontology 2002; 3:19–24.
7
Latres E, Amini AR, Amini AA, et al. Insulin-like growth factor-1 (IGF-1)
inversely regulates atrophy-induced genes via the phosphatidylinositol
3-kinase/akt/mammalian target of rapamycin (PI3K/Akt/mTOR) pathway.
J Biol Chem 2005; 280:2737–2744.
8
Sacheck JM, Ohtsuka A, McLary SC, Goldberg AL. IGF-1 stimulates muscle
growth by suppressing protein breakdown and expression of atrophy-related
ubiquitin-ligases, atrogin-1 and MuRF1. Am J Physiol Endocrinol Metab 2004;
287:E591–E601.
9
Stitt TN, Drujan D, Clarke BA, et al. The IGF-1/PI3K/Akt pathway prevents
expression of muscle atrophy-induced ubiquitin ligases by inhibiting FOXO
transcription factors. Mol Cell 2004; 14:395–403.
10 Coleman ME, DeMayo F, Yin KC, et al. Myogenic vector expression of insulinlike growth factor I stimulates muscle cell differentiation and myofiber hypertrophy in transgenic mice. J Biol Chem 1995; 270:12109–12116.
11 Musaro A, McCullagh K, Paul A, et al. Localized Igf-1 transgene expression
sustains hypertrophy and regeneration in senescent skeletal muscle. Nat
Genet 2001; 27:195–200.
12 Rommel C, Bodine SC, Clarke BA, et al. Mediation of IGF-1-induced skeletal
myotube hypertrophy by PI(3)K/Akt/mTOR and PI(3)K/Akt/GSK3 pathways.
Nat Cell Biol 2001; 3:1009–1013.
13 Bodine SC, Stitt TN, Gonzalez M, et al. Akt/mTOR pathway is a crucial
regulator of skeletal muscle hypertrophy and can prevent muscle atrophy in
vivo. Nat Cell Biol 2001; 3:1014–1019.
14 Lai K-MV, Gonzalez M, Poueymirou WT, et al. Conditional activation of Akt in
adult skeletal muscle induces rapid hypertrophy. Mol Cell Biol 2004;
24:9295–9304.
15 Mammucari C, Milan G, Romanello V, et al. FoxO3 controls autophagy in
skeletal muscle in vivo. Cell Metab 2007; 6:458–471.
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Signaling pathways perturbing muscle mass Glass 229
16 Izumiya Y, Hopkins T, Morris C, et al. Fast/glycolytic muscle fiber growth
reduces fat mass and improves metabolic parameters in obese mice. Cell
Metab 2008; 7:159–172.
This study demonstrates that induced expression of Akt in fast fibers decreases fat;
it might indicate the existence of ‘myokines’ that inhibit white fat.
17 Sugita H, Kaneki M, Sugita M, et al. Burn injury impairs insulin-stimulated Akt/
PKB activation in skeletal muscle. Am J Physiol Endocrinol Metab 2005;
288:367–376.
18 Bodine SC, Latres E, Baumhueter S, et al. Identification of ubiquitin ligases
required for skeletal muscle atrophy. Science 2001; 294:1704–1708.
19 Gomes MD, Lecker SH, Jagoe RT, et al. Atrogin-1, a muscle-specific F-box
protein highly expressed during muscle atrophy. Proc Natl Acad Sci U S A
2001; 98:14440–14445.
20 Li Y-P, Chen Y, Li AS, Reid MB. Hydrogen peroxide stimulates ubiquitin
conjugating activity and expression of genes for specific E2 and E3 proteins in
skeletal muscle myotubes. Am J Physiol Cell Physiol 2003; 285:C806–
C812.
21 Dehoux MJM, van Beneden RP, Fernandez-Celemin L, et al. Induction of
MafBx and Murf ubiquitin ligase mRNAs in rat skeletal muscle after LPS
injection. FEBS Lett 2003; 544:214–217.
22 Deruisseau KC, Kavazis AN, Deering MA, et al. Mechanical ventilation induces
alterations of the ubiquitin-proteasome pathway in the diaphragm. J Appl
Physiol 2004; 98:1314–1321.
23 Borden KL, Freemont PS. The RING finger domain: a recent example of a
sequence-structure family. Curr Opin Struct Biol 1996; 6:396–401.
24 Kamura T, Koepp DM, Conrad MN, et al. Rbx1, a component of the VHL tumor
suppressor complex and SCF ubiquitin ligase [see comments]. Science
1999; 284:657–661.
25 Cohen S, Brault JJ, Gygi SP, et al. During muscle atrophy, thick, but not thin,
filament components are degraded by MuRF1-dependent ubiquitylation.
J Cell Biol 2009; 185:1083–1095.
This study demonstrates that MuRF1 ubiquitinates additional members of the thick
filament besides only MyHC.
26 McElhinny AS, Kakinuma K, Sorimachi H, et al. Muscle-specific RING finger1 interacts with titin to regulate sarcomeric M-line and thick filament
structure and may have nuclear functions via its interaction with glucocorticoid modulatory element binding protein-1. J Cell Biol 2002; 157:125 –
136.
27 Centner T, Yano J, Kimura E, et al. Identification of muscle specific ring finger
proteins as potential regulators of the titin kinase domain. J Mol Biol 2001;
306:717–726.
28 Pizon V, Iakovenko A, van der Ven PFM, et al. Transient association of titin
and myosin with microtubules in nascent myofibrils directed by the MURF2
RING-finger protein. J Cell Sci 2002; 115:4469–4482.
37 Sandri M, Sandri C, Gilbert A, et al. Foxo transcription factors induce the
atrophy-related ubiquitin ligase atrogin-1 and cause skeletal muscle atrophy.
Cell 2004; 117:399–412.
38 Stitt TN, Drujan D, Clarke BA, et al. The IGF-1/PI3K/Akt pathway prevents
expression of muscle atrophy-induced ubiquitin ligases by inhibiting FOXO
transcription factors. Mol Cell 2004; 14:395–403.
39 Du J, Mitch WE, Wang X, Price SR. Glucocorticoids induce proteasome C3
subunit expression in L6 muscle cells by opposing the suppression of its
transcription by NF-kappa B. J Biol Chem 2000; 275:19661–19666.
40 Hong DH, Forsberg NE. Effects of dexamethasone on protein degradation
and protease gene expression in rat L8 myotube cultures. Mol Cell Endocrinol
1995; 108:199–209.
41 Wang L, Luo GJ, Wang JJ, Hasselgren PO. Dexamethasone stimulates
proteasome- and calcium-dependent proteolysis in cultured L6 myotubes.
Shock 1998; 10:298–306.
42 Lee SW, Dai G, Hu Z, et al. Regulation of muscle protein degradation:
coordinated control of apoptotic and ubiquitin-proteasome systems by phosphatidylinositol 3 kinase. J Am Soc Nephrol 2004; 15:1537–1545.
43 Kamei Y, Miura S, Suzuk M, et al. Skeletal muscle FOXO1 (FKHR) transgenic
mice have less skeletal muscle mass, down-regulated type I (slow twitch/red
muscle) fiber genes, and impaired glycemic control. J Biol Chem 2004;
279:41114–411123.
44 McPherron AC, Lawler AM, Lee SJ. Regulation of skeletal muscle mass in
mice by a new TGF-beta superfamily member. Nature 1997; 387:83–90.
45 Grobet L, Martin LJ, Poncelet D, et al. A deletion in the bovine myostatin gene
causes the double-muscled phenotype in cattle. Nat Genet 1997; 17:71–74.
46 McPherron AC, Lee SJ. Double muscling in cattle due to mutations in the
myostatin gene. Proc Natl Acad Sci U S A 1997; 94:12457–12461.
47 Kambadur R, Sharma M, Smith TP, Bass JJ. Mutations in myostatin (GDF8) in
double-muscled Belgian Blue and Piedmontese cattle. Genome Res 1997;
7:910–916.
48 Lee S-J. Quadrupling muscle mass in mice by targeting TGFbeta signaling
pathways. PLoS One 2007; 2:e789.
49 Langley B, Thomas M, Bishop A, et al. Myostatin inhibits myoblast differentiation by down-regulating MyoD expression. J Biol Chem 2002; 277:49831–
49840.
50 Rios R, Fernandez-Nocelos S, Carneiro I, et al. Differential response to
exogenous and endogenous myostatin in myoblasts suggests that myostatin
acts as an autocrine factor in vivo. Endocrinology 2004; 145:2795–2803.
51 McFarlane C, Plummer E, Thomas M, et al. Myostatin induces cachexia by
activating the ubiquitin proteolytic system through an NF-kappaB-independent, FoxO1-dependent mechanism. J Cell Physiol 2006; 209:501–514.
29 Clarke BA, Drujan D, Willis MS, et al. The E3 ligase MuRF1 degrades myosin
heavy chain protein in dexamethasone-treated skeletal muscle. Cell Metab
2007; 6:376–385.
52 Yang W, Zhang Y, Li Y, et al. Myostatin induces cyclin D1 degradation to
cause cell cycle arrest through a phosphatidylinositol 3-kinase/AKT/GSK3beta pathway and is antagonized by insulin-like growth factor 1. J Biol Chem
2007; 282:3799–3808.
30 Schulze PC, Fang J, Kassik KA, et al. Transgenic overexpression of locally
acting insulin-like growth factor-1 inhibits ubiquitin-mediated muscle atrophy
in chronic left-ventricular dysfunction. Circ Res 2005; 97:418–426.
53 Tsuchida K, Nakatani M, Uezumi A, et al. Signal transduction pathway through
activin receptors as a therapeutic target of musculoskeletal diseases and
cancer. Endocr J 2008; 55:11–21.
31 Mearini G, Gedicke C, Schlossarek S, et al. Atrogin-1 and MuRF1 regulate
cardiac MyBP-C levels via different mechanisms. Cardiovasc Res 2010;
85:357–366.
54 Rebbapragada A, Benchabane H, Wrana JL, et al. Myostatin signals through a
transforming growth factor {beta}-like signaling pathway to block adipogenesis. Mol Cell Biol 2003; 23:7230–7242.
32 Jackson PK, Eldridge AG. The SCF ubiquitin ligase: an extended look. Mol
Cell 2002; 9:923–925.
55 Trendelenburg AU, Meyer A, Rohner D, et al. Myostatin reduces AKT/TORC1/
p70S6K signaling, inhibiting myoblast differentiation and myotube size. Am J
Physiol Cell Physiol 2009; 296:1258–1270.
This study demonstrates inhibition of Akt/TORC1 pathway by myostatin and
inhibition of muscle expression even in postdifferentiated myotubes.
33 Tintignac LA, Lagirand J, Batonnet S, et al. Degradation of MyoD mediated by
the SCF (MAFbx) ubiquitin ligase. J Biol Chem 2005; 280:2847–2856.
34 Lagirand-Cantaloube J, Offner N, Csibi A, et al. The initiation factor eIF3-f is a
major target for Atrogin1/MAFbx function in skeletal muscle atrophy. EMBO J
2008; 27:1266–1276.
35 Csibi A, Leibovitch M-P, Cornille K, et al. MAFbx/Atrogin-1 controls the activity
of the initiation factor eIF3-f in skeletal muscle atrophy by targeting multiple
C-terminal lysines. J Biol Chem 2008; 284:4413–4421.
36 Li H-H. Atrogin-1 inhibits Akt-dependent cardiac hypertrophy in mice via
ubiquitin-dependent coactivation of Forkhead proteins. J Clin Invest 2007;
117:3211–3223.
56 Sartori R, Milan G, Patron M, et al. SMAD2 and 3 transcription factors control
muscle mass in adulthood. Am J Physiol Cell Physiol 2009; 296:1248–1257.
This study demonstrates inhibition of Akt by myostatin and potentiation of FOXO
signaling.
57 Bentzinger C, Romanino K, Cloëtta D, et al. Skeletal muscle-specific ablation
of raptor, but not of rictor, causes metabolic changes and results in muscle
dystrophy. Cell Metab 2008; 8:411–424.
This study illustrates the importance of TORC1 signaling and demonstrates
unexpected dystrophy-like disease upon raptor ablation.
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.