Medical Terminology and Abbreviations Amy Sayle, PhD, MPH This
advertisement

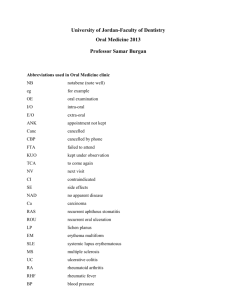
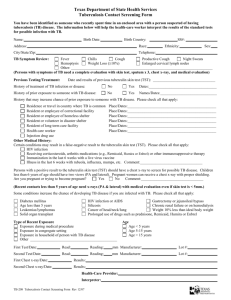
Medical Terminology and Abbreviations Amy Sayle, PhD, MPH This presentation by Brad Torok, MD, gives you an overview of medical terminology and abbreviations one might encounter when reviewing medical records. SLIDE 1 Medical Terminology and Abbreviations or How to Decipher the Secret Code in a Medical Record. This presentation explains some of the commonly seen types of medical chart notes and the terminology in them. SLIDE 2 The objectives of this presentation are to first, understand the organization of a medical chart; second, to recognize the three most common types of patient notes found in medical charts; third, to recognize common clinical terms used to describe symptoms in the major body systems and finally, recognize common clinical terms used to describe examination findings in the major body systems. SLIDE 3 Topics to be presented include medical chart organization, types of patient encounter notes, medical history terms and abbreviations, physical examination terms and abbreviations, and laboratory and chest x-ray terms and abbreviations. SLIDE 4 Medical charts are a highly-specialized, technical document. They are predominantly paper-based, although some are computerized, and many are hand-written. Like any technical document, medical charts are difficult to interpret; however, there is a great deal of standard formatting and terminology. Chart interpretation can sometimes be made more difficulty by physicians' notoriously illegible handwriting, but for the purposes of this exercise, we will assume any notes we encounter are typed. SLIDE 5 Chart organization. Most patient records are still composed of paper in a manila folder, usually divided into several sections. They are often close to this order if not identical, the first section consisting of patient demographic and insurance information. Flow sheets are used to concisely keep track of preventive care, medications, allergies, medical problems, surgeries, and other useful information. These are often followed by the patient's actual visit notes and then laboratory results, radiology results, consultant notes and letters, and other reports and communications. The exact format of charts and their organization can very quite a bit, depending on whether the patient is in a hospital, another institution, or in an outpatient setting. SLIDE 6 The three most commonly encountered types of patient notes are the history and physical, the SOAP note, and the discharge summary. SLIDE 7 First, we will review the history and physical. The history and physical note is usually a very in-depth note performed on the first visit or consultation with a patient or for routine, physical examinations. These begin with a section on the patient's history, which includes the following components. The CC or Chief Complaint, otherwise known as the reason for the visit, the HPI, or History of Present Illness, which is the history around the reason for the visit, the ROS or Review of Systems, which consists of asking the patient about the presence or absence of symptoms by body area. This is followed by the patient's prior history, including their past medical history, abbreviated PMHx, and past surgical history, abbreviated PSHx. SLIDE 8 The social history can include information regarding smoking, drinking, drug use, education, employment, the living situation, the sexual preference, and the marital status of the patient. The family history will usually pertain to illnesses present in the immediate family, such as parents and siblings. The final component is often medications, including medications the patient is currently taking and any medication allergies. A very commonly encountered abbreviation is NKDA, which is short for No Known Drug Allergies. You may also see just NKA for No Known Allergies. SLIDE 9 All of the objective or examination findings are after the subjective findings. This includes a section on physical examination findings, followed by a section on laboratory studies, and finally, other studies, such as radiologic studies like x-rays, CT scans, MRI scans, and ultrasounds. SLIDE 10 The history and physical concludes with an assessment consisting of either a Dx, the abbreviation for diagnosis, or DDx, the abbreviation for differential diagnosis. A differential diagnosis is a list of possible diagnoses when the diagnosis is unclear. For each diagnosis, a plan is laid out for treatment. If the diagnosis is unclear, a plan is laid out for determining the diagnosis. The full history and physical will often be dictated in narrative form and when typed, can cover two or more pages. SLIDE 11 Another commonly encountered note format is called the SOAP note. SLIDE 12 The SOAP note format is very brief and is usually used when a patient already has a more complete history and physical in their chart to refer back to. The SOAP note includes four basic sections. S stands for Subjective, meaning anything collected by verbal means rather than examination and testing. The subjective component includes the complaints the patient is being seen for and the surrounding information the provider collects verbally. Subjective includes the chief complaint or CC, the history of present illness, or HPI, and the review of systems, or ROS, from the more comprehensive history and physical note discussed above. The O is for Objective and includes any objectively obtain information, including the vital signs, physical examination findings, and laboratory and radiological results. The A is for Assessment and is usually a brief section where the provider notes the diagnosis or diagnoses or several potential diagnoses if the provider is unsure. P is for Plan where the further diagnostic testing to be done is noted, as well as any treatment plans and instructions for the patient are noted. SLIDE 13 The final type of note we'll discuss is the Hospital Discharge Summary. SLIDE 14 The Discharge Summary is a long history and physical format narrative summarizing a patient's hospital stay. It condenses the large amount of information from a hospital stay into one note, starting with the events surrounding the hospital admission and includes the course of events in the hospital, such as important test results, major diagnoses, and major treatments. It concludes with a summary of the patient's diagnoses, the condition of the patient at the time of discharge, and any treatment recommendations and follow up required once discharged. The format can be easily followed when you understand the format of the history and physical. SLIDE 15 The following section will present subjective terminology, which is encountered in the history section of a history and physical or the S section of a SOAP note. SLIDE 16 We will review these terms by body system. We will begin with HEENT, which stands for head, eyes, ears, nose, and throat. Some commonly encountered terms referring to these areas include occipital, meaning back of the head, photophobia, meaning literally fear of light but more commonly meaning light worsening a patient's head or eye pain, phonophobia, meaning again literally fear of sound but more commonly used to mean sound making a headache worse, and also diplopia, which is double vision or seeing double. SLIDE 17 Epistaxis is a term meaning nose bleed. Rhinorrhea is nasal drainage or runny nose. Otorrhea is discharge or drainage from the ear. Tinnitus means a constant ringing in one or both ears. SLIDE 18 Moving on from the HEENT system, the cor or coronary refers to the heart. Other than pain in the chest, the most common description patients may have regarding their heart is the sensation of palpitations, which is a fluttering sensation or the feeling of a skipped or extra beat. Next is pulm, which is short for pulmonary and refers to the lungs. Patients with SOB feel short of breath. A more concise term for short of breath is dyspnea. Those who cough up phlegm have a productive cough, whereas a dry cough is nonproductive. SLIDE 19 Wheezing is a high-pitched whistling sound when breathing, most often heard in patients with asthma. Hemoptysis is coughing up blood. Pleuritic is a symptom, usually pain that gets worse with deep breathing, such as a pleuritic chest pain. SLIDE 20 The abdomen is abbreviated Abd or GI, which is short for gastrointestinal. Patients with abdominal complaints often have pain in one area of the abdomen. The abdomen is divided into four sections or quadrants, as you see in the diagram, using the naval as the center of the dividing lines. The abbreviations used are right upper quadrant, right lower quadrant, left upper quadrant, and left lower quadrant. SLIDE 21 Sometimes pain is in the upper center, which is epigastric or near the stomach around the bellybutton, termed periumbilical, or in the low central abdomen, which can be called suprapubic, meaning above the pubic bone. SLIDE 22 Patients who have no appetite have anorexia. Post-prandial means after eating. An example would be post-prandial stomach pain. Emesis is the medical term for vomiting. If emesis is not green or bloody, it is NBNB emesis, which is short for non-bloody, nonbilious. Bilious means bile-like or green tinted. If one vomits blood, it's called hematemesis, he meaning blood. SLIDE 23 If one has a bloody stool, it is termed hematochezia. Black, tar-like stool is called melena and usually indicates old blood in the stool coming from somewhere higher in the gastrointestinal tract. A common abbreviation is BRBPR, which is short for bright red blood per rectum. This is usually concerning for a potentially dangerously fast rate of bleeding. Moving on, GU stands for genitourinary. The most common complaint that isn't readily understood by most people is dysuria, which means pain on urination. Another common term is hematuria, which is seeing blood in the urine. SLIDE 24 MS refers to musculoskeletal, and ext to extremities. These are often used interchangeably. Some common terms used are myalgias or muscle aches seen with flu-like illnesses and arthralgias, which are joint aches. SLIDE 25 Edema means swelling. Most body parts can swell, but edema often refers to peripheral edema, which is swelling of the peripheral body, most often the legs. Dependent edema is swelling usually of the legs that occurs only when they are below the heart, and this will get better with lying or elevating the legs. Another common place to see edema referred to is in the lungs called pulmonary edema, which we will review in the x-ray section coming up. SLIDE 26 Derm is short for dermatologic, pertaining to the skin. Puritic or non-puritic is referring to whether the skin itches, which is puritic, or does not itch, which is non-puritic. Neuro stands for neurologic, and patients will often complain of paresthesias, which are an abnormal sensation, such as tingling, in the absence of stimuli. This slide concludes Part I of terms and abbreviations. SLIDE 27 Terms and Abbreviations, Part II, Physical Examination. This is Part II of the Medical Terminologies and Abbreviations presentation. The next section will cover terms and abbreviations encountered with a physical examination of the patient. Many terms used for the PE, or physical exam, are unfamiliar to those without medical training. SLIDE 28 Common shorthand is on this slide. PE is an abbreviation for physical examination. If something is positive or present, it can be listed as a plus sign (+). If it is absent or negative, it is often a minus sign (-), or a zero with a slash through it 0. Normal is commonly abbreviated nl or wnl for within normal limits. SLIDE 29 Gen stands for general and refers to the general appearance of the patient, including mood, nutritional status, and if the patient appears to be in any distress. For example, an alert WDWN WF in NAD is an alert, well-developed, well-nourished, white female in no apparent distress. Other commonly used abbreviations for ethnicity include AA or usually African American and LA for Latin American. AOx3 means alert and oriented times three, referring to orientation to person, place, and time. The patient knows who they are and where and when they are. SLIDE 30 Terms and abbreviations used to describe the head, eyes, ears, nose, and throat area of the body commonly include NCAT, which means normocephalic, atraumatic, which means normal head with no trauma visible. PERRL is short for pupils are equal, round, and reactive to light, and the equal refers to equal in size. Erythema, which means redness. Erythema can be used to describe just about any visible part of the body which is red. Exudate is often used in describing the tonsils and the phrase tonsillar exudates, and exudates strictly defines is a material, such as fluid, cells, or cellular debris, which has escaped from blood vessels and has been deposited on or in a tissue. This is usually the result of inflammation. A person with tonsillar exudates would have white spots visible on their tonsils. SLIDE 31 Purulent means consisting of or containing pus and might be used to describe nasal discharge or the fluid draining from a ruptured, infected eardrum, though it may be used to describe the character of any fluid draining from or contained in a body part. Injected does not refer to needles in this case. It really refers to visible blood vessel congestion often seen in a bloodshot eye or an infected eardrum. The neck has a few common terms, including supple, which means moving easily and implies there is no neck stiffness and, therefore, probably no meningitis and infection. LAD is an abbreviation for lymphadenopathy, which means swollen lymph glands or lymph nodes. Lymphadenopathy can be present elsewhere, such as the armpit or groin but is most commonly examined routinely in the neck. Bruits, spelled B-R-U-I-T-S, or the absence of bruits is commonly examined in the neck and refers to the abnormal whoosh sound that one can hear when listening with a stethoscope to the arteries of someone with arterial narrowing, usually due to cholesterol deposits. SLIDE 32 The cor or cardiac examination findings most common encountered will be documented concisely in the normal individual as rrr no mgr, which are abbreviations short for regular rate and rhythm, no murmurs, gallops, or rubs. This refers to the fact that the heart is beating normally, meaning regularly, and there are no extra or unusual heart sounds. Sometimes a murmur will be described, but for the purposes of this talk, we will not go into the details of describing a cardiac murmur. Tachycardia and bradycardia or tachycardic and bradycardic refer to the rate or how fast the heart beats. Tachy, which is short for tachycardic, is too fast, and brady, short for bradycardic, is too slow. Irregular would refer to someone whose heartbeat does not follow the usual regular clock-tick rhythm of the heart beating but instead has a different amount of time between some of the beats. SLIDE 33 Pulm, which is pulmonary or lung findings, usually are described in the normal individual as CTAB no rrw. This is an abbreviation, which stands for clear to auscultation bilaterally, no rales, rhonchi, or wheezes. Auscultation is listening with a stethoscope, and this can refer to any part of the body. Bilaterally means both sides or both lungs in this case. Rales are also known as crackles as that is what they sound like. They sound like Rice Crispy cereal noises or Velcro being pulled. Rhonchi and wheezes are two words for the same sound, and they both refer to high-pitched whistling sounds, most commonly heard in someone who has asthma. Retractions refer to the visible drawing back of the skin when breathing in. It occurs between the ribs above the collarbone or in the abdomen. Retractions only occur when someone is having difficulty breathing and is usually accompanied by tachypnea, which means breathing more rapidly or taking more breaths per minute than is normal for the patient's age. SLIDE 34 Abd is the abbreviation for abdomen. BS means something quite different to medical personnel. It is an abbreviation for bowel sounds, which should be present and normal active, meaning normal amount of activity. One may also have ascent, hypoactive, or hyperactive bowel sounds if something is wrong. TTP can refer to any area of the body. It stands for tender to palpation. To palpate is to examine by touch or feeling. Often, if the patient has no tenderness, it will be documented as NTTP for nontender to palpation. Tenderness will often be greater in one of the four quadrants described earlier. Guarding refers to the tendency to tense the stomach muscles when someone is palpating a tender area. Rebound tenderness refers to a pain that is worse as the examining hands are quickly removed rather than as they press in. SLIDE 35 A few terms are commonly used when examining the extremities. 2+ DTR refers to deep tendon reflexes, otherwise known simply as reflexes. An example is the knee jerk response when the knee is struck with a reflex hammer. 2+ refers to how much of a response is elicited by the reflex hammer. The scale is from 0 to 4, with 2+ being normal, and less or more being abnormal. No CCE is an abbreviation for no cyanosis, clubbing, or edema. Cyanosis means blue tissues, which is an indication of low oxygen. Clubbing is a bulbous shape to the fingertips of someone who has lived for many years with a low oxygen concentration in their blood, such as someone with severe emphysema. Edema has been discussed above. In the context of the extremities, it usually pertains to swelling of the lower part of the legs. SLIDE 36 There is a lot of terminology specific to dermatology and describing the skin. A full overview is beyond this discussion, but some basics may be helpful. A macule is a flat spot of discoloration. A papule is a raised bump up to 5mm in diameter. A circumscribed, elevated, solid lesion bigger than 5mm is a nodule. This will look and feel like a pellet or something lodged under the skin. Groups of papules that have grown together to form a large raised area are called a plaque. SLIDE 37 Sacs in the skin have different names depending on their size and appearance. A vesicle is a fluid-filled sac less than 5mm in size. A bulla is a fluid-filled sac larger than 5mm, and a pustule is a sac filled with pus. An erosion is a superficial loss of skin, whereas an ulcer is a loss of skin deep enough to cause scarring. Scale refers to the dry, flaky areas of skin that you might see in someone with dander for allergies. The term is used because sometimes these dry flakes resemble the scales of a reptile. We've discussed erythema before. Erythema refers to visible redness. SLIDE 38 Neuro is short for neurologic, which pertains to the nervous system. A full neurologic examination is beyond the scope of this presentation, but a normal individual will often be described by notation, such as CNII-XII intact, meaning the cranial nerves which control the functions of the head and face are normal. These functions can include eye movement, vision, hearing, and sensation. Grossly intact implies that while no specific neurologic testing was done, the individual has no obvious problems. SLIDE 39 Next, we will briefly discuss laboratory terms and abbreviations. Laboratory studies should be relatively self-explanatory. The results will be either normal or abnormal and if abnormal, should be clearly marked so on the lab report form. We will cover only a few of the more commonly used abbreviations for some very common tests. SLIDE 40 The CBC stands for complete blood count, which is a count of the red or oxygencarrying cells, the white cells, which fight infection, and the platelets, which help blood clot. A Chem 7, 8, 14, or 20 refers to a large panel of chemistry tests looking at blood concentrations of chemicals, including salts, sugars, and certain enzymes. LFTs are specific to liver function tests and can be part of a larger chemistry panel. ABG stands for arterial blood gas, which is a test to determine the concentrations of various gases in the blood and, therefore, how well the patient's cardiopulmonary system is working. A urinalysis is abbreviated UA, and this is a chemical and often microscopic analysis of the patient's urine. SLIDE 41 Radiologic studies, such as x-rays, are another area full of specialized terminology. SLIDE 42 If you are relying on a non radiologist's interpretation of an x-ray or other imaging test in the overall chart note, you may only get the visual impression of the provider with no conclusion as to what the x-ray means, though it will often be implied in the overall assessment or diagnosis. On a dictated report from a radiologist, however, they will describe in radiologic terms what they see and then offer one diagnosis, or more often, several possible diagnoses that can appear similar to the pictures. If the study they are interpreting is not conclusive as to the diagnosis, they will often suggest another imaging test to determine the final diagnosis. SLIDE 43 For our purposes, learning some chest x-ray anatomy and terminology will probably be most helpful as the chest x-ray is one of the most commonly ordered studies. SLIDE 44 Two x-rays are usually taken, the PA, or posteroanterior view, and the lateral view. The PA is shot with the x-rays penetrating the patient's back, and the x-ray film in front of the patient's chest. The lateral is shot from the side. Included will be all of the lung anatomy, the surrounding boney tissue, including the ribs, the clavicle or collarbone, the spine, and the sternum, as well as other organs in the chest. When looking at the PA xray, you look at it as if the patient is standing in front of you, which means the patient's right side is on the left side of the x-ray and vice versa. SLIDE 45 The lungs themselves have five lobes or sections, three in the right lung and two on the left. They are called the right upper, right middle, and right lower lobes and on the left, the left upper and left lower lobes. On this lateral view, you can see all three of the right lobes roughly outlined. Knowing where the lobes are can tell you where an infection or mass is located. SLIDE 46 This diagram of a lateral chest x-ray shows the left upper and lower lobes. SLIDE 47 This is the right upper lobe viewed on a PA chest x-ray. SLIDE 48 The right middle lobe is visible on this PA chest x-ray. SLIDE 49 This is a picture of a pneumonia visible in the right middle lobe. SLIDE 50 The right lower lobe is highlighted on this PA chest x-ray. SLIDE 51 On this PA view, the left upper lobe is highlighted. SLIDE 52 And the left lower lobe again on a PA view. SLIDE 53 In the chest cavity, all organs besides the lungs will be in the center of the chest, which is called the mediastinum. SLIDE 54 This is an x-ray of someone with a widened mediastinum due to inhalational anthrax. An x-ray with this appearance could be due to infection, cancer, or dangerously enlarged blood vessels. SLIDE 55 The largest structure in the mediastinum is the heart. SLIDE 56 The silhouette sign refers to a loss of the silhouette outlining a structure in the chest. This sign occurs when fluid or a mass fills part of the lung next to a structure. This sign tells you that an abnormality is present, as well as its relative location. In this x-ray, the patient's right heart border is missing because of a pneumonia in the right lung. SLIDE 57 Atelectasis is one of the most common findings on a chest x-ray and refers to an incomplete expansion or collapse of all or part of the lung. This can be due to something blocking an airway or by something compressing the lung from the outside, but most often, it is due to some mucous plugging the airways. This x-rays shows several right-sided partial collapse. Notice the silhouette sign at the patient's right heart border. SLIDE 58 This x-ray shows complete collapse of the right lung, which is much easier to see than a partial collapse. SLIDE 59 Consolidation and air space disease refer to a non-collapsed lung filled with something. Most commonly, this is pus associated with pneumonia but could also be blood, other fluids, or cancer cells. This right middle lobe pneumonia is a good example of consolidation on a chest x-ray. SLIDE 60 Pleural effusions are collections of fluid in the pleural space compressing the lungs from the outside. The pleural space is between the lungs and the surrounding tissues and normally isn't a space at all. It should be invisible, unless it is filled with air or fluid. On this example x-ray, you can see the pleural effusions where the lower outer corners of the lungs are around it instead of coming to a sharp, downward point. SLIDE 61 Pulmonary edema is fluid accumulation in the lungs and swelling of the lung tissues. Without knowing anything about the patient's illness, differentiating pulmonary edema from a widespread infection can be difficult, as you can see from the example x-ray. SLIDE 62 This concludes Part II of Medical Terminology and Abbreviations.