ORIGINAL INVESTIGATION
Attitudes of Terminally Ill Patients Toward
Euthanasia and Physician-Assisted Suicide
Keith G. Wilson, PhD; John F. Scott, MD, MDiv; Ian D. Graham, PhD; Jean F. Kozak, PhD; Susan Chater, MB;
Raymond A. Viola, MD, MSc; Barbara J. de Faye, MA; Lynda A. Weaver, MHA; Dorothyann Curran, BA
Background: In jurisdictions that permit euthanasia or
physician-assisted suicide, patients with cancer comprise the largest group to die by these methods. We investigated the personal attitudes toward these practices
of patients receiving palliative care for advanced cancer.
Methods: Seventy patients (32 men and 38 women;
median survival, 44.5 days) took part in a survey using
in-depth semistructured interviews. The interviews
were audiotaped for transcription and content analysis
of themes.
Results: Most participants (73%) believed that eutha-
nasia or physician-assisted suicide should be legalized,
citing pain and the individual’s right to choose as their
major reasons. Participants who were opposed to legalization cited religious and moral objections as their central concerns. Forty (58%) of the 69 participants who completed the entire interview also believed that, if legal, they
From the Institute for
Rehabilitation Research and
Development, The Rehabilitation
Centre, Ottawa, Ontario
(Dr Wilson and Ms Curran);
University of Ottawa Institute of
Palliative Care (Drs Wilson,
Scott, Kozak, Chater, and Viola
and Ms Weaver); Department of
Medicine (Drs Wilson, Scott,
Graham, Chater, and Viola),
School of Psychology (Dr Wilson
and Ms de Faye), and
Department of Epidemiology and
Community Medicine
(Dr Graham), University of
Ottawa; SCO Hospital, Ottawa
(Drs Scott, Kozak, and
Ms Weaver); Clinical
Epidemiology Unit, Loeb Health
Research Institute, The Ottawa
Hospital (Dr Graham);
Palliative Care Service, The
Ottawa Hospital, Civic Campus
(Dr Chater); and Palliative Care
Service, The Ottawa Hospital,
General Campus (Dr Viola).
W
might personally make a future request for a hastened
death, particularly if pain or physical symptoms became
intolerable. Eight of these individuals (12%) would have
made such a request at the time of the interview. These
8 participants differed from all others on ratings of loss
of interest or pleasure in activities, hopelessness, and the
desire to die (Ps,.02). They also had a higher prevalence of depressive disorders (P,.05). However, they did
not differ on ratings of pain severity.
Conclusions: Many patients with advanced cancer favor policies that would allow them access to both euthanasia and physician-assisted suicide if pain and physical
symptoms became intolerable. For patients who would
actually make requests for a physician-hastened death,
however, psychological considerations may be at least as
salient as physical symptoms.
Arch Intern Med. 2000;160:2454-2460
ITH THE ongoing so-
cietal debate around
the issue of legalizing voluntary euthanasia or physician-assisted suicide for terminally ill
patients, there has been a growing interest in identifying the concerns of those who
would be most likely to make requests for
a hastened death. Studies have been conducted with various groups of patients who
have life-threatening illnesses.1-8 There are
also reports from the Netherlands, the Australian Northern Territory, and the US state
of Oregon that have described the characteristics of patients who have died by
these methods in jurisdictions where they
have been permitted.9-13 Finally, there are
surveys of physicians in other areas who
have provided euthanasia or assisted suicide, albeit illegally, to patients in their
care.14-16 These studies indicate that both
physical and psychosocial considerations are relevant in the assisted-suicide
debate, but they are limited because they
have been conducted (1) with physicians
rather than with the patients themselves
or (2) with patients who were not neces-
(REPRINTED) ARCH INTERN MED/ VOL 160, SEP 11, 2000
2454
sarily close to death, when these decisions would be most salient. In this study,
we examined attitudes toward euthanasia and physician-assisted suicide in the
group that would be most affected by legalization—patients who are nearing death
from advanced cancer, the diagnosis of
65% to 80% of those who receive hastened deaths in the Netherlands.9-11 The
goals were to examine patients’ attitudes
toward these practices and to investigate
the factors that are related to the personal interest in receiving a physicianhastened death.
RESULTS
RECRUITMENT
During the recruitment period, 789 patients with cancer were admitted or referred to the participating palliative care
services. However, only 229 patients met
the inclusion criteria for participation. The
main reasons for ineligibility were that the
patient was too ill to participate or died
before the case was reviewed (n=475, 85%
of those excluded). The remainder were
WWW.ARCHINTERNMED.COM
Downloaded from www.archinternmed.com on April 15, 2009
©2000 American Medical Association. All rights reserved.
PARTICIPANTS AND METHODS
RECRUITMENT
The survey was conducted from 1996 to 1998. The participants were patients admitted to a regional palliative care
inpatient unit or patients who received palliative care consultation services on the oncology wards of 2 Canadian tertiary care hospitals. The study protocol was approved by
the ethics review committees of all the participating institutions.
At each site, the clinical palliative care teams reviewed consecutive referrals or admissions for the following inclusion criteria: (1) in the team’s opinion, the patient was medically and cognitively able to participate; (2)
the patient had been informed that the malignant illness
was incurable; and (3) the palliative care team was confident that broaching a discussion of euthanasia and physician-assisted suicide would not undermine their clinical role
with the patient. If the patient agreed, a meeting was arranged with a research interviewer, who obtained written
informed consent.
PROCEDURE
The semistructured interviews were conducted by a clinical psychologist, doctoral students in psychology, or a research associate in palliative care. All interviews were attended by both a primary interviewer and an observer, to
permit the evaluation of interrater reliability. They were also
audiotaped for later transcription.
The interview first addressed the subject’s general attitudes toward the acceptability and legal status of both euthanasia and physician-assisted suicide. Euthanasia was defined as an action in which “a medical doctor gives an
overdose of medication to purposely end a patient’s life.
This is only done with patients who have asked their doctor to help them die in this way. Usually, the patients involved are very ill with a life-threatening disease.” Physicianassisted suicide was defined as an action in which “a medical
doctor provides drugs and advice, so that a patient could
commit suicide. The doctor does not actually inject the
drugs, but rather gives the patient the means to end his or
her own life.” The subject was then asked whether each of
these practices is acceptable, whether they should be legalized, and whether there are any important differences
between them.
The interview then moved on to review the subject’s personal circumstances, beginning with an inquiry into physical symptoms of pain, drowsiness, weakness, nausea, and
breathlessness, which are among the most prevalent problems in the final weeks of life.17-19 The protocol also addressed specific end-of-life concerns that have been relevant
in previous studies of euthanasia or assisted suicide in
medical populations, including the loss of control, loss of dignity, sense of being a burden to others, and hopelessness.7,9,20 Next, the interview addressed the mental health issues of anxiety, depression, and loss of interest or pleasure
in activities. This section then concluded with an inquiry into
the subject’s desire for death.21
Each of these 13 symptoms and concerns was
assessed using interview items that began with a structured lead question, followed by a series of follow-up
prompts to clarify the severity of the problem. Severity was
then rated by the interviewer on a 7-point scale (none,
minimal, mild, moderate, strong, severe, and extreme).
The screening items for anxiety, depression, and loss of
interest or pleasure were used in conjunction with the Primary Care Evaluation for Mental Disorders (PRIME-MD)22
to permit the full diagnostic assessment of discrete anxiety
and depressive syndromes, as defined by the Diagnostic
and Statistical Manual of Mental Disorders, Fourth Edition
(DSM-IV).23-25
The last section of the interview returned to the topics of euthanasia and physician-assisted suicide, with a focus on the subject’s personal situation. Specifically, the subject was asked (1) whether he or she would have asked for
euthanasia or assisted suicide, if they were legal and available, at any point in the current illness; (2) if there were
any foreseeable circumstances in which he or she would
make such a request in the future, and; (3) whether he or
she would actually initiate a request now, in the current
circumstances.
DATA ANALYSIS
The audiotaped responses were transcribed verbatim to facilitate content analysis.26,27 This is an inductive strategy
that involves the process of breaking down, constantly comparing and categorizing narrative information, resulting in
the identification of underlying themes. All transcripts were
reviewed independently by 3 investigators (K.G.W., I.D.G.,
and J.F.K.), who then met as a team to reach consensus on
themes. Categories of response that were provided by more
than 5% of the total study group (at least 4 participants)
are reported.
For the 13 clinical rating scales, the intraclass correlations between the 2 raters exceeded r= 0.92 in each case.
In the diagnosis of mental disorders, there was only 1 disagreement (k= 0.96), confirming that the assessments had
high interrater reliability.
For the quantitative analyses, we identified subgroups of subjects who differed with respect to their personal interest in receiving a physician-hastened death. The
demographic and clinical characteristics of these subgroups were compared statistically using x2 and Fisher exact tests for categorical data, and analyses of variance for
continuous measures and rating scales. Significant F tests
were followed up with Tukey pairwise comparisons.
excluded because of language barriers (n=35, 6%), a clinical decision that it would be inappropriate to approach
the patient about this topic (n=21, 4%), discharge within
24 hours (n=18, 3%), or objection by the patient’s family or attending physician (n = 11, 2%). Of the 229 patients who were initially considered to be eligible, 79
(34%) were not approached because they either deterio(REPRINTED) ARCH INTERN MED/ VOL 160, SEP 11, 2000
2455
rated medically or were discharged before the required
consents were obtained.
In total, the possibility of participation was raised
initially with 150 patients, 80 of whom declined. Thus,
the 70 participants who took part in the study represent
47% of the patients who were finally approached, and
9% of all patients with cancer who received palliative care
WWW.ARCHINTERNMED.COM
Downloaded from www.archinternmed.com on April 15, 2009
©2000 American Medical Association. All rights reserved.
Table 1. Demographic and Clinical Characteristics
Age, mean (SD), y
Sex, M/F
Married, No. (%)
Education, No. (%)
Less than high school
High school
More than high school
Religion, No. (%)
Roman Catholic
Protestant
None
Other
Primary tumor site, No. (%)
Lung
Genitourinary
Female breast
Gastrointestinal
Head and neck
Other
Unknown
Survival duration, median (range), d
Medications, No. (%)
Opioids
Antidepressants
Anxiolytics
Mental disorders, No. (%)
Depression
Anxiety
Any disorder
.1 Disorder
64.5 (12.1)
32/38
34 (49)
21 (30)
17 (24)
32 (46)
29 (41)
29 (41)
7 (10)
5 (7)
15 (21)
13 (19)
9 (13)
9 (13)
7 (10)
11 (16)
6 (9)
44.5 (1-183)
55 (79)
17 (24)
19 (27)
14 (20)
7 (10)
16 (23)
6 (9)
services on the participating units during the study period. Limited data about age and sex were available for
patients who declined participation. There were no differences in these characteristics between the patients who
did and did not participate (Ps..10).
One participant completed a partial interview before requesting a break, but was not able to complete the
full protocol because of progressive illness. The partial
data from this person have been included where they are
available.
PARTICIPANTS
The demographic characteristics of the 70 participants
(32 men and 38 women) are shown in Table 1. Their
average age was 64.5 years (range, 43-88 years). In general, the study group was highly educated, with 49 participants (70%) having at least a high school education.
From the date of the interview, the median survival duration of the study group was 44.5 days, with only 11
participants (16%) living as long as 6 months.
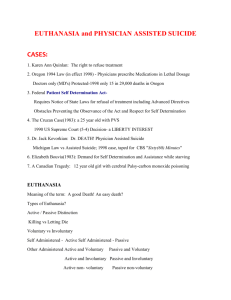
ATTITUDES TOWARD THE ACCEPTABILITY
AND LEGAL STATUS OF EUTHANASIA
AND ASSISTED SUICIDE
Forty-five participants (64%) considered that both euthanasia and physician-assisted suicide are acceptable
practices that should be legalized, whereas 15 (21%) reported that both are unacceptable and should not be legalized. Of the remaining 10 participants (14%), 3 were
(REPRINTED) ARCH INTERN MED/ VOL 160, SEP 11, 2000
2456
Table 2. Reasons for or Against Legalization of
Euthanasia and Physician-Assisted Suicide*
For Legalization (n = 51)
Individual’s right to choose
Pain
Diminished quality of life
Suffering
Hopeless situation
Mental symptoms
Burden for others
Physical symptoms (other than pain)
Knowledge of others’ experience
Against Legalization (n = 16)
Religious/spiritual beliefs
Secular moral values
Potential for abuse
Inappropriate role for physicians
Concerns about stability and rationality
22 (43)
22 (43)
18 (35)
12 (24)
12 (24)
9 (18)
7 (14)
5 (10)
4 (8)
8 (50)
6 (38)
5 (31)
5 (31)
4 (25)
*Data are given as number (percentage) of participants citing each reason.
Only reasons mentioned by at least 4 participants are presented.
uncertain, 4 reported that only euthanasia should be legalized, 1 reported that both practices are acceptable in
an informal way but should not be legalized, and 2 indicated that both are unacceptable in principle but should
be legalized anyway if they are going to be practiced surreptitiously.
The 51 participants who were in favor of at least limited legal access to either euthanasia or assisted suicide
provided a total of 122 individual reasons to support their
opinion. These reasons are summarized in Table 2. In
general, they believed that people have the right to decide how they will die. Other frequent reasons referred
to uncontrollable pain, diminished quality of life, and
other types of suffering, both physical and mental. Some
participants also expressed a concern about relieving the
burden on family members, and some noted that their
attitudes were influenced by their knowledge of the endof-life experiences of others.
The 16 participants who were against legalization
provided 36 individual reasons for their view, consisting mostly of opposition because of religious or spiritual beliefs, or because of secular moral values. They also
raised concerns about the potential for abuse, that causing death is not an appropriate role for physicians, and
that the desire to die is not always stable or rational.
PERCEIVED DIFFERENCES BETWEEN
EUTHANASIA AND ASSISTED SUICIDE
Participants were also asked whether there are any
important differences between euthanasia and assisted
suicide. Twenty-one participants (30%) reported that they
did see important distinctions between the practices; 14
(67%) found euthanasia to be more acceptable and 7
(33%) believed that physician-assisted suicide is more
acceptable.
The participants who found euthanasia to be more
acceptable than assisted suicide provided a total of 23 reasons for their view, including the argument that terminating life requires technical medical knowledge (n=10,
WWW.ARCHINTERNMED.COM
Downloaded from www.archinternmed.com on April 15, 2009
©2000 American Medical Association. All rights reserved.
71%), and that physicians are best able to assess the appropriate timing, stability, and rationality of the request
(n=6, 43%).
Those who considered physician-assisted suicide to
be more acceptable provided a total of 11 reasons, including the concern that the direct termination of life is
not an appropriate role for physicians (n = 5, 71%), and
that assisted suicide maximizes choice and control for
the patient (n= 5, 71%).
PERSONAL INTEREST IN RECEIVING
EUTHANASIA OR ASSISTED SUICIDE
When asked whether they could envision future circumstances in which they would personally request euthanasia or assisted suicide, 32 participants (46%) reported
that they could, 19 (28%) reported that they could not,
and 10 (14%) were uncertain. Of those with a possible
interest for the future, 3 participants believed that they
would already have made requests at earlier points in
their illness, but they no longer thought that way by the
time of the interview. In addition, however, there were
also 8 other patients, or 12% of the entire study group,
who reported that they would request euthanasia or
assisted suicide immediately, in their current circumstances.
REASONS FOR WANTING EUTHANASIA
OR ASSISTED SUICIDE IN THE FUTURE
The 32 participants who indicated a possible future interest in receiving euthanasia or assisted suicide reported a total of 63 reasons for why they would make
such requests. The most frequent reasons focused on the
physical distress associated with uncontrollable pain
(n=15, 47%) and other severe physical symptoms (n=11,
34%). Some participants also mentioned nonphysical circumstances that would motivate them to make a request, including if their global quality of life deteriorated (n=8, 25%), if they became a burden to others (n=7,
22%), if they were generally suffering (n=6, 19%), if they
developed mental symptoms (n = 6, 19%), if they believed that they were simply lingering while waiting to
die (n=5, 16%), or if they perceived their overall situation as hopeless (n = 4, 13%).
Twenty-two (69%) of these participants reported a
preference for a particular method of hastened death, with
the majority (n= 16) preferring euthanasia over assisted
suicide (n=6) (P = .03).
PATIENTS WHO WOULD REQUEST A HASTENED
DEATH IN THEIR CURRENT CIRCUMSTANCES
The 8 participants who currently desired a physicianhastened death comprised 5 men and 3 women, aged 47
to 82 years. Three were married, 3 were divorced, and 2
were widowed. Three were university graduates, 3 had
completed high school, and 2 had less than high school
educations. Three were from the Roman Catholic faith,
3 were from Protestant backgrounds, and 2 reported no
religious affiliation. The DSM-IV diagnoses within this
group included 4 patients with major depression, 2 of
(REPRINTED) ARCH INTERN MED/ VOL 160, SEP 11, 2000
2457
whom had comorbid anxiety disorders, and 1 with major depression in partial remission.
When asked about the method that they would
choose to end their lives, 4 participants indicated a preference for euthanasia, 2 for physician-assisted suicide,
and 2 had no preference. As a group, they provided a total of 48 individual statements that clarified why they were
ready to end their lives. In general, they recognized that
their illness was terminal (n=4, 50%; eg, “For two months
I have known that it was over for me.” “I have a terminal disease. I’m not going to get better.”), and they believed that they had achieved some degree of acceptance that they were going to die (n=4, 50%; eg, “I’m in
a position now in my life where I want to go.” “I’d like
to make my peace and go.”). They spoke of suffering (n=4,
50%; eg, “The family won’t suffer and I won’t suffer.” “If
suffering is inevitable, they [the patient] should have a
say.”) and of a diminished quality of life (n=4, 50%; eg,
“If a patient feels he can no longer function and is no more
a human being.” “God put us here to enjoy life. He didn’t
cause my illness but, I mean, I’m deteriorating and that’s
that.”). They believed that they had the right to exercise
choice and control over the manner of their deaths (n=6,
75%; eg, “I think I should have control over dying in dignity. “Nobody should be forced to stay alive by other
people.”) and that euthanasia or assisted suicide would
provide an easier means of dying than they were actually experiencing (n=5, 63%; eg, “You only have to press
a button to finish it and sleep peacefully.” “Just to expire in my sleep would be the perfect way for me.”). Pain
was cited as a contributing reason by 1 person, although
a fear of pain was discussed by another, and adverse reactions to narcotic analgesics were reported by a third.
Four of the 8 participants died within 2 weeks of
the interview, and 3 others died over the next 1 to 4
months. The last patient rallied medically during the admission, and lived for another 20 months.
CLINICAL CORRELATES
Statistical comparisons were conducted between 3 groups:
(1) those who would never consider euthanasia or assisted suicide (n=19); (2) those who would consider it
in the future, but who had no current interest (n=32);
and (3) those who would make requests in their current
circumstances (n=8) (Table 3).
The 3 groups did not differ on any demographic characteristic (Ps..10). Similarly, they did not differ with respect to the level of pain that they experienced, or in the
subjective sense of depressed mood (Ps..10). However, there were a number of differences between groups
in the severity of other symptoms and concerns, including drowsiness (P =.02), weakness (P =.04), loss of control (P = .04), loss of interest or pleasure in activities
(P=.007), hopelessness (P,.001), and desire for death
(P,.001).
In post hoc comparisons, participants with no interest in receiving a hastened death and those with only
a hypothetical future interest did not differ on any measure (Ps..05). Rather, the 8 participants with a current
interest accounted for all of the significant findings. They
reported greater loss of interest or pleasure in activities,
WWW.ARCHINTERNMED.COM
Downloaded from www.archinternmed.com on April 15, 2009
©2000 American Medical Association. All rights reserved.
Table 3. Interviewer Severity Ratings
of Symptoms and Concerns*
Symptom
or Concern
No Interest†
(n = 19)
Future Interest
(n = 32)
Current Interest
(n = 8)
Pain
Drowsiness‡
Nausea
Weakness‡
Breathlessness
Loss of control‡
Loss of dignity
Sense of burden
Hopelessness§
Anxiety
Depression
Loss of interest§
Desire for death§
2.32 (1.57)
1.79 (1.44)
1.16 (1.74)
2.68 (1.57)
1.42 (1.92)
0.79 (1.08)
0.74 (0.93)
2.26 (1.37)
0.74 (0.99)
0.95 (1.42)
0.84 (0.90)
0.95 (1.03)
1.68 (0.70)
1.56 (1.48)
2.44 (1.54)
0.82 (1.38)
3.09 (1.57)
1.66 (1.75)
1.31 (1.87)
0.91 (1.55)
2.00 (1.59)
0.69 (1.09)
1.03 (1.20)
1.00 (1.08)
1.00 (1.72)
2.03 (1.27)
2.25 (0.89)
3.63 (1.85)
1.38 (1.41)
4.38 (1.06)
2.50 (1.60)
2.63 (2.26)
1.50 (2.33)
2.13 (2.23)
2.88 (2.36)
1.75 (1.67)
1.75 (1.67)
3.00 (2.20)
5.00 (1.66)
*Data are given as mean (SD) values derived from 7-point rating scales
where 0 = none, 1 = minimal, 2 = mild, 3 = moderate, 4 = strong, 5 = severe,
and 6 = extreme.
†No interest refers to participants who report no interest in ever
requesting a death hastened by euthanasia or physician-assisted suicide;
future interest comprises participants who could foresee making a request in
the future, but who would not do so in their current circumstances; current
interest refers to participants who would make a request for a hastened
death in their current circumstances.
‡Participants with a current interest differ from those with no interest at
P,.05.
§Participants with a current interest differ from both other groups at
P,.05.
hopelessness, and desire for death than did participants
in both other groups (Ps,.02). They also reported greater
drowsiness, weakness, and loss of control than did participants with no interest (Ps,.04).
In addition, 5 (63%) of the 8 individuals with a current interest in euthanasia or assisted suicide met diagnostic criteria for a mental disorder, compared with 3
(16%) of 19 with no interest (P = .03) and 7 (22%) of 32
with only a possible interest for the future (P =.04).
COMMENT
Despite widespread interest in the issues of euthanasia
and physician-assisted suicide for people who are terminally ill, this study is the first to have directly examined
the attitudes of patients who are nearing death from advanced cancer. Although it would have been preferable
to have achieved a higher response rate than 47% of patients approached, the difficulties of recruitment in the
palliative care setting are well known.28,29 It is also important to note that most of the participants in the present study were gravely ill, the protocol was quite rigorous, and the topic is controversial. We suspect that these
are the major reasons for the observed rate of refusal. Nevertheless, it must be acknowledged that the patients who
chose not to take part in the study may have differed in
important ways from those who did.
With this proviso, our findings agree with those of
others who have reported that the majority of patients
with life-threatening illnesses support the general principle of legalizing euthanasia or physician-assisted suicide.3-6 The qualitative aspects of the protocol also shed
light on the reasons that underlie patient preferences. It
(REPRINTED) ARCH INTERN MED/ VOL 160, SEP 11, 2000
2458
is apparent from these reasons that people with different opinions about legalization are not simply arguing
for different sides of the same issue; rather, their positions are grounded in different issues altogether. People
who are against legalization are motivated primarily by
religious or secular moral concerns, which place the sanctity of human life above other considerations. Those who
are in favor of legalization are more concerned about the
relief of uncontrollable pain and suffering, as well as with
the rights of the individual to exercise choice and control. These are fundamental differences in the premises
on which the 2 positions are based, which suggests that
there is little common ground between them on which
to reach a compromise solution.
In the United States, the movement toward legalization has focused mostly on the specific issue of assisted suicide, as reflected in the Oregon Death With Dignity legislation. Nevertheless, many right-to-die activists
have acknowledged that their long-term goal includes access to euthanasia as well.30 The pro-legalization participants in the present study clearly saw euthanasia as being at least as acceptable as assisted suicide. Among those
who would personally consider requesting a hastened
death, euthanasia would actually have been the more common choice. This finding parallels the experience of the
Netherlands, where euthanasia takes place much more
frequently than assisted suicide.9-11 The arguments in favor of assisted suicide include concerns about patient autonomy and control, the moral limits of medical intervention, the potential for error or abuse, and the possibility
of greater legal safeguards for physicians.31,32 Patient preferences have seldom been cited as a relevant factor in this
debate. Indeed it can be argued that patient preferences
are not relevant if they point to a position that is immoral and unethical.33 At the empirical level, however,
it is apparent that many terminally ill patients see a role
for euthanasia. This is largely because they view the termination of life as requiring an advanced technical knowledge of medicine.
Almost half of the participants could imagine future circumstances in which they would personally ask
for assistance in hastening their own deaths. The most
common circumstances involved scenarios of uncontrolled pain and physical symptoms. For these individuals, there might be some comfort in knowing that euthanasia or assisted suicide were available, in the event that
their worst fears about pain and symptoms indeed came
true.34,35 These desperate situations remain hypothetical
future events for this group, however, and in the meanwhile they are doing their best to carry on. Apart from
their accepting attitude toward euthanasia and assisted
suicide, their clinical profiles appear to be quite similar
to those of patients who would never request a hastened
death.
On the other hand, the 8 participants who would
have made requests for euthanasia or assisted suicide in
their current circumstances appear to be quite different
from the others who took part in this study, and they illustrate some of the key issues that have emerged in the
legalization debate.
First, it is not always a straightforward task to specify
when a life-threatening illness has entered a terminal
WWW.ARCHINTERNMED.COM
Downloaded from www.archinternmed.com on April 15, 2009
©2000 American Medical Association. All rights reserved.
phase.13 One person who would have requested a physician-hastened death was admitted to the palliative care
unit, but improved, was discharged, and survived for another 20 months. Second, the desire to die is not necessarily stable over time.21,36 Three other participants reported that they would have requested a hastened death
at earlier points in their illness, but they would no longer
have done so by the time of the interview.
Third, the current desire for a physician-hastened
death was associated with a high prevalence of depressive disorders. This is significant in the present context
because depression is a potentially treatable problem,
which in severe cases may bias health decisions in a negative way.37 The clinical diagnoses of depression did not
always arise from reports of a greater subjective sense of
depressed mood, however, and none of the participants
explicitly mentioned depression as the reason for wanting to die. Rather, the diagnoses were sometimes based
in the report of a pervasive loss of interest or pleasure in
activities, which is also a core criterion symptom of depressive disorders.23 When coupled with a sense of hopelessness and loss of control, which were also elevated
among these individuals, then euthanasia and physicianassisted suicide may be seen as offering the relief of an
easier death.
Fourth, of the physical symptoms that we examined, weakness and drowsiness showed the strongest association with the desire for a hastened death. It is not
clear whether these symptoms directly cause the desire
to die, or whether they arise because of other factors, such
as a higher use of sedating medications in the treatment
of this distressed group, more advanced physical disease and nearness to death, or whether they emerge as
part of the symptom complex of depression in the medically ill. It is noteworthy, however, that pain, although
common at low levels in the majority of participants, did
not differ significantly between the groups. Among the
general public, support for legalization is highest in scenarios that involve terminally ill patients who have
uncontrollable pain.3 Public support is lower in scenarios that involve patients who have adequate pain
control, but who want to die because of physical debility
or a perceived loss of purpose and meaning.3 In reality,
patients in the latter circumstances may be more characteristic of those who would actually make requests for
hastened death. Therefore, if legalization is to be
reviewed on a more widespread basis, the public debate
should be broadened to include a discussion of the
acceptability of these factors as reasons to provide euthanasia or assisted suicide.
Finally, it must also be noted that all of the participants in this Canadian study had access to state-funded
palliative care services, at no personal financial cost. Unfortunately, this is not the case for every person who is
facing death. The lack of accessible palliative care is a compelling argument for prudence in the review of prohibitions against euthanasia and physician-assisted suicide.38,39 We also have much to learn about patients’
perceptions of quality end-of-life care, and how to provide it.40 Nevertheless, even with good care, it is evident
that there will still be patients who would prefer to end
their lives through direct physician intervention.41 Our
(REPRINTED) ARCH INTERN MED/ VOL 160, SEP 11, 2000
2459
results indicate that it is not necessarily extreme physical distress that motivates this desire. Rather, the psychological and existential dimensions of suffering—
which are, perhaps, no less central in determining quality
of life—also emerge as important reasons behind patient requests for physician-hastened death.
Accepted for publication March 8, 2000.
The research was supported by grant 6606-6475002 from the National Health Research and Development
Program (NHRDP) of Health Canada, and by a Career
Scientist award from the Ontario Ministry of Health (Dr
Graham).
The views expressed herein are those of the authors,
and do not necessarily reflect those of the NHRDP, Health
Canada, or the Ontario Ministry of Health.
We acknowledge the contributions of Cathe Boucher,
RN, Maryse Bouvette, MEd, RN, Michael Claessens, MD,
Pippa Hall, MD, MEd, Virginia Jarvis, BScN, RN, Liliane
Locke, BScN, RN, and Judi Paterson, MA, RN, who
assisted with the recruitment of participants; Julie Allston,
MSc, Anne-Marie Baronet, BA, Mariette Blouin, BA, Lori
deLaplante, BA, and Amanda Pontefract, MSc, who served
as interviewers; Maureen Ferrante, BSc, RN, who helped
with data collection; Suzanne Pelletier, who transcribed
the interviews and helped with report preparation; Paul
Hébert, MD, MHSc, who reviewed an earlier draft of the
manuscript, and Jay Lynch, BAdm, RN, who assisted with
the dissemination of results. We also thank the people who
participated in the study. Despite their failing health, they
gave their time generously to this project.
Reprints: Keith G. Wilson, PhD, Institute for Rehabilitation Research and Development, The Rehabilitation
Centre, 505 Smyth Rd, Ottawa, Ontario, Canada K1H
8M2.
REFERENCES
1. Owen C, Tennant C, Levi J, Jones M. Suicide and euthanasia: patient attitudes in
the context of cancer. Psychooncology. 1992;1:79-88.
2. Owen C, Tennant C, Levi J, Jones M. Cancer patients’ attitudes to final events in
life: wish for death, attitudes to cessation of treatment, suicide and euthanasia.
Psychooncology. 1994;3:1-9.
3. Emanuel EJ, Fairclough DL, Daniels ER, Clarridge BR. Euthanasia and physicianassisted suicide: attitudes and experiences of oncology patients, oncologists, and
the public. Lancet. 1996;347:1805-1810.
4. Suarez-Almazor ME, Belzile M, Bruera E. Euthanasia and physician-assisted suicide: a comparative survey of physicians, terminally ill cancer patients and the
general population. J Clin Oncol. 1997;15:418-427.
5. Sullivan M, Rapp S, Fitzgibbon D, Chapman CR. Pain and the choice to hasten
death in patients with painful metastatic cancer. J Palliat Care. 1997;13:18-28.
6. Breitbart W, Rosenfeld BD, Passik SD. Interest in physician-assisted suicide among
ambulatory HIV-infected patients. Am J Psychiatry. 1996;153:238-242.
7. Ganzini L, Johnston WS, McFarland BH, Tolle SW, Lee MA. Attitudes of patients
with amyotrophic lateral sclerosis and their care givers toward assisted suicide.
N Engl J Med. 1998;339:967-973.
8. Berkman CS, Cavallo PF, Chesnut WC, Holland NJ. Attitudes toward physicianassisted suicide among persons with multiple sclerosis. J Palliat Med. 1999;2:
51-63.
9. van der Maas PJ, van Delden JJM, Pijnenborg L, Looman CWN. Euthanasia
and other medical decisions concerning the end of life. Lancet. 1991;338:669674.
10. van der Maas PJ, van der Wal G, Haverkate I, et al. Euthanasia, physicianassisted suicide, and other medical practices involving the end of life in the Netherlands, 1990-1995. N Engl J Med. 1996;335:1699-1705.
11. Onwuteaka-Philipsen BD, Muller MT, van der Wal G, Van Eijk JTM, Ribbe MW.
WWW.ARCHINTERNMED.COM
Downloaded from www.archinternmed.com on April 15, 2009
©2000 American Medical Association. All rights reserved.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
Active voluntary euthanasia or physician-assisted suicide? J Am Geriatr Soc. 1997;
45:1208-1213.
Chin AE, Hedberg K, Higginson GK, Fleming DW. Legalized physician-assisted
suicide in Oregon—the first year’s experience. N Engl J Med. 1999;340:577583.
Kissane DW, Street A, Nitschke P. Seven deaths in Darwin: case studies under
the Rights of the Terminally Ill Act, Northern Territory, Australia. Lancet. 1998;
352:1097-1102.
Back AL, Alcser KH, Doukas DJ, Lichtenstein RL, Corning AD, Brody H. Attitudes of Michigan physicians and the public toward legalizing physicianassisted suicide and voluntary euthanasia. N Engl J Med. 1996;334:303-309.
Meier DE, Emmons C-A, Wallenstein S, Quitt T, Morrison RS, Cassel CK. A national survey of physician-assisted suicide and euthanasia in the United States.
N Engl J Med. 1998;338:1193-201.
Emanuel EJ, Daniels ER, Fairclough DL, Clarridge BR. The practice of euthanasia and physician-assisted suicide in the United States: adherence to proposed
safeguards and effects on physicians. JAMA. 1998;280:507-513.
Coyle N, Adelhardt J, Foley KM, Portenoy RK. Character of terminal illness in the
advanced cancer patient: pain and other symptoms during the last four weeks of
life. J Pain Symptom Manage. 1990;5:83-93.
Curtis EB, Krech R, Walsh TD. Common symptoms in patients with advanced
cancer. J Palliat Care. 1991;7:25-29.
Vertafridda Y, Ripamonti C, DeConno F, Tamburini M, Cassileth BR. Symptom
prevalence and control during cancer patients’ last day of life. J Palliat Care. 1990;
6:7-11.
Chochinov HM, Wilson KG, Enns M, Lander S. Depression, hopelessness, and
suicidal ideation in the terminally ill. Psychosomatics. 1998;39:366-370.
Chochinov HM, Wilson KG, Enns M, et al. Desire for death in the terminally ill.
Am J Psychiatry. 1995;152:1185-1191.
Spitzer RL, Williams JBW, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 Study. JAMA. 1994;
272:1749-1756.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental
Disorders, Fourth Edition. Washington, DC: American Psychiatric Association;
1994.
Chochinov HM, Wilson KG, Enns M, Lander S. Prevalence of depression in the
terminally ill: effects of diagnostic criteria and symptom threshold judgements.
Am J Psychiatry. 1994;151:537-540.
(REPRINTED) ARCH INTERN MED/ VOL 160, SEP 11, 2000
2460
25. Wilson KG, Chochinov HM, deFaye BJ. Diagnosis and management of depression
in palliative care. In: Chochinov HM, Breitbart W, eds. Handbook of Psychiatry in
Palliative Medicine. New York, NY: Oxford University Press; 2000:25-49.
26. Crabtree B, Miller M. Doing Qualitative Research: Research Methods for Primary Care. Newbury Park, Calif: Sage; 1992.
27. Altheide D. Ethnographic content analysis. Qualitative Sociol. 1987;10:65-77.
28. McWhinney IR, Bass MJ, Donner A. Evaluation of a palliative care service: problems and pitfalls. BMJ. 1994;309:1340-1342.
29. Calman K, Hanks G. Clinical and health services research. In: Doyle D, Hanks
GWC, MacDonald N, eds. Oxford Textbook of Palliative Medicine. 2nd ed. New
York, NY: Oxford University Press; 1998:159-165.
30. Annas GJ. Death by prescription: the Oregon initiative. N Engl J Med. 1994;331:
1240-1243.
31. Battin MP. Euthanasia: the way we do it, the way they do it. J Pain Symptom
Manage. 1991;6:298-305.
32. Quill TE, Cassel CK, Meir DE. Care of the hopelessly ill: proposed clinical criteria
for physician-assisted suicide. N Engl J Med. 1992;327:1380-1384.
33. Pellegrino ED. The limitation of empirical research in ethics. J Clin Ethics. 1995;
6:161-162.
34. Wilson KG, Viola RA, Scott JF, Chater S. Talking to the terminally ill about euthanasia and physician-assisted suicide. Can J Clin Med. 1998;5:68-74.
35. Breitbart W, Chochinov HM, Passik S. Psychiatric aspects of palliative care. In:
Doyle D, Hanks GWC, MacDonald N, eds. Oxford Textbook of Palliative Medicine. 2nd ed. New York, NY: Oxford University Press; 1998:933-954.
36. Chochinov HM, Tataryn D, Clinch JJ, Dudgeon D. Will to live in the terminally ill.
Lancet. 1999;354:816-819.
37. Ganzini L, Lee MA, Heintz RT, Bloom JD, Fenn DS. The effect of depression treatment on elderly patients’ preferences for life-sustaining medical therapy. Am J
Psychiatry. 1994;151:1631-1636.
38. Latimer EJ, McGregor J. Euthanasia, physician-assisted suicide and the ethical
care of dying patients. CMAJ. 1994;151:1133-1136.
39. Foley KM. The relationship of pain and symptom management to patient requests for physician-assisted suicide. J Pain Symptom Manage. 1991;6:289297.
40. Singer PA, Martin DK, Kelner M. Quality end-of-life care: patients’ perspectives.
JAMA. 1999;281:163-168.
41. Seale C, Addington-Hall J. Euthanasia: the role of good care. Soc Sci Med. 1994;
39:647-654.
WWW.ARCHINTERNMED.COM
Downloaded from www.archinternmed.com on April 15, 2009
©2000 American Medical Association. All rights reserved.