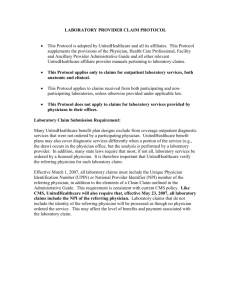
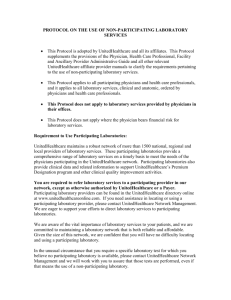
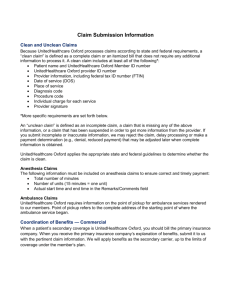
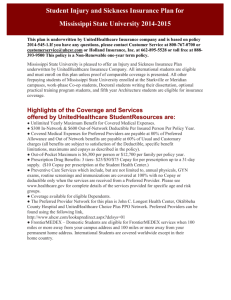
Network Bulletin - UnitedHealthcareOnline.com
advertisement

Network Bulletin: January 2014 - Volume 59 network bulletin An important message from UnitedHealthcare to health care professionals and facilities enter UnitedHealthcare respects the expertise of the physicians, health care professionals and their staff who participate in our network. Our goal is to support you and your patients in making the most informed decisions regarding the choice of quality and cost-effective care, and to support practice staff with a simple and predictable administrative experience. The Network Bulletin was developed to share important updates regarding UnitedHealthcare procedure and policy changes, as well as other useful administrative and clinical information.* *Where information in this bulletin conflicts with applicable state and/or federal law, UnitedHealthcare follows such applicable federal and/or state law Table of Contents 2 2 Front & Center UnitedHealthcare Commercial UnitedHealthcare Reimbursement Policy UnitedHealthcare Medicare Solutions UnitedHealthcare Community Plan Doing Business Better UnitedHealthcare Pharmacy UnitedHealthcare Claims, Billing & Coding UnitedHealthcare Affiliates Network Bulletin: November 2013 - Volume 58 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME Front & Center • UnitedHealthcare Medicaid Policy Alignment • 2014 UnitedHealthcare Administrative Guide Available – Effective April 1, 2014 • Important Changes in Advance Notification and Prior Authorization Requirements for Home Health Services for Medicare Advantage Plans • UnitedHealthcare Community Plan to Start Using National Comprehensive Cancer Network Compendium • Injectable Chemotherapy Prior Authorization Program for Florida Providers • UnitedHealthcare Shared Services Expansion for GEHA • myHCE: Providing Cost Transparency for a More Informed Health Care Consumer • Prepare for UnitedHealthcareOnline.com Login Migration to Optum Cloud Dashboard • The CMS “Two Midnight Rule” – Effective Oct. 1, 2013 • 2014: The Year of the ICD-10 Code • Enhanced HIPAA Edits to be Applied to Claim Submissions • HIPPS Codes Requirement for Home Health Care and Skilled Nursing Facility Encounters • Medicare Advantage to Require Prior Authorization for IMRT, SRS and SBRT as of April 1 • Medicare Advantage Radiology and Cardiology Prior Authorization Program to Deploy for UnitedHealthcare West Medicare Non-Capitated Participating Providers on April 1, 2014 • Women’s Preventive Care Services Updates NEXT SECTION> UnitedHealthcare Commercial 3 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME UnitedHealthcare Commercial • UnitedHealthcare Medical Policy, Drug Policy, Coverage Determination Guideline and Utilization Review Guideline Updates • New Disease-specific IMRT Forms for UnitedHealthcare Prior Authorization Process • The Preferred Payment Method for Your UnitedHealthcare Patients: Member Payments NEXT SECTION> UnitedHealthcare Reimbursement Policy 4 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME UnitedHealthcare Reimbursement Policy • UnitedHealthcare Reimbursement Policy • Revision to CCI Editing Policy • Revision to the Professional/Technical Component Policy - Denial of Drug Administration Codes and PC/TC Indicator 8 • Multiple Procedure Policy Revisions to Apply to Same Group NEXT SECTION> UnitedHealthcare Medicare Solutions 5 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME UnitedHealthcare Medicare Solutions • 2013 Member Rewards Program – Better Health has its Rewards • UnitedHealthcare Wins Bid for State of Illinois • UnitedHealthcare Medicare Advantage Coverage Summary Updates • Reminder for Advance Notification and Prior Authorization NEXT SECTION> UnitedHealthcare Community Plan 6 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME UnitedHealthcare Community Plan • Important Reimbursement Policy Reminder • Provider Disclosure of Ownership Form Now Online • Changes to the UnitedHealthcare Community Plan of Pennsylvania Claims Payer ID and Electronic Remittance Advice Payer ID • Readmission Policy Frequently Asked Questions NEXT SECTION> Doing Business Better 7 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME Doing Business Better NEXT SECTION> UnitedHealthcare Pharmacy 8 Network Bulletin: January 2014 - Volume 59 • Important Change: Arriva Medical has Acquired Diabetes Care Club • Medline Industries Joins Network • UnitedHealthcare Preventive Plan Design • Introducing COB Smart™: Receive Payments Accurately, Predictably and Reliably • UnitedHealthcare’s Position on “Never Events” • Navigate Products and Related Administrative Processes • Physician and Provider Demographic Changes • Training Sessions for Electronic Solutions • Wellness Programs: Recommending Alternative Actions • Electronic Inpatient Admission Notifications • Checking Status of Claim Reconsideration Requests With Attachments • Coverage Determination and Utilization Management Decisions • All Savers Alternative Funding Product - New Portal • UnitedHealth Premium® Results Available to Public Soon • BMI Documentation in the Medical Record For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME UnitedHealthcare Pharmacy • Medicare Change to Physician-initiated Prescriptions at Mail Pharmacies • Effective Feb. 1, 2014: New Prior Authorization Requirements for Enzyme Replacement Medications (For UnitedHealthcare Integrated Commercial Fully Insured and Self-funded Plans Only) • New OptumRx Specialty Pharmacy Resource Guide • Reminder: 25 Specialty Medications Added to Coupon Policy for Jan. 1, 2014 • UnitedHealthcare Consolidated Pharmacy Benefit Program NEXT SECTION> UnitedHealthcare Claims, Billing & Coding 9 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME UnitedHealthcare Claims, Billing & Coding • Accurate Billing Improves Office Efficiency and Dual SNP Member Satisfaction • Accessing Explanations of Benefits Online • Coding Update to Facility OPG Mapping – Effective Jan. 1, 2014 NEXT SECTION> UnitedHealthcare Affiliates 10 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME UnitedHealthcare Affiliates • Oxford Medical and Administrative Policy Updates • UnitedHealthcare of the River Valley Preauthorization List and Policy Updates • SignatureValue™ Benefit Interpretation Policy Updates • SignatureValue™ Medical Management Guideline Updates • UnitedHealthcare of the River Valley and Neighborhood Health Partnership: Disease Management Programs << FIRST SECTION Front & Center 11 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center UnitedHealthcare Medicaid Policy Alignment Effective March 1, 2014, UnitedHealthcare Community Plan will align our medical policies with the rest of UnitedHealthcare’s medical policies, to provide a streamlined, simplified experience for providers caring for members of our various health plans. The policies are available at UnitedHealthcareOnline.com >Tools & Resources > Policies, Protocols and Guides > Medical & Drug Policies and Coverage Determination Guidelines. Our medical policies, including established and new technologies, explain how we determine whether a service (e.g., test, device or procedure) is proven to be effective and/or to have a benefit on health outcomes based on the published clinical evidence. They are also used to decide whether a given health service is medically necessary. Services determined to be experimental, investigational, unproven, or not medically necessary by the clinical evidence are typically not covered. We understand that the first level of review for medical policies is the determination of coverage which is based on what the State defines as covered benefits. If the service is not a covered benefit, then the managed care organization does not have any responsibility to pay for the service. However, if the service is determined to be a covered benefit, we have the responsibility to determine if the service falls into the category of “medically necessary” based on clinical evidence and guidance. Continued > 12 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center UnitedHealthcare Medicaid Policy Alignment < Continued Medical policies are developed as needed and represent one of the important resources used to support UnitedHealthcare’s coverage decision making. Policies are developed as needed and subject to change through regular review. New and updated medical policy changes will be communicated in the Medical Policy Update Bulletin at UnitedHealthcareOnline.com > Tools & Resources > Policies, Protocols and Guides > Medical & Drug Policies and Coverage Determination Guidelines > Medical Policy Update Bulletin. 13 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center 2014 UnitedHealthcare Administrative Guide Available – Effective April 1, 2014 < Continued This essential resource for physicians, hospitals, facilities and other health care providers is now posted on UnitedHealthcareOnline.com. Download it today! Important Updates in the 2014 Guide Include: • • • Advance Notification List - The Advance Notification list of procedure codes has moved online for your convenience at UnitedHealthcareOnline.com > Clinician Resources > Advance & Admission Notification Requirements. Please reference the complete article for more details in the January Network Bulletin. • Exchanges - New product details on Individual Marketplace and/or Small Business Health Options Program (SHOP) Marketplace language added in the Commercial Product section. • Retroactive Eligibility Changes - Eligibility changes may occur retroactively if the member fails to pay their premium within a three month grace period for subsidized Individual Exchange members. Optum Cloud Dashboard - Is a cloud-based website that has new features and functionality which allows providers to submit claim reconsideration requests electronically with attachments. Supplement Updates and Changes for 2014: • Oxford Commercial Provider Reference Manual has been consolidated into a Supplement of the UnitedHealthcare Guide. High Performing Networks - Expansion of new Commercial product offerings for UnitedHealthcare Compass. • OneNet Provider Manual has been consolidated into a Supplement of the UnitedHealthcare Guide. Continued > 14 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center 2014 UnitedHealthcare Administrative Guide Available – Effective April 1, 2014 15 • Medicare Advantage Capitated Provider Supplement - A new supplement for all nonUnitedHealthcare West capitated providers. • Oxford Medicare Advantage Supplement has been removed and content has been integrated with the UnitedHealthcare standard Medicare Advantage section. • UnitedHealthOne and All Savers Supplements are now two separate supplements to the Guide and have been revised in accordance with the current product offerings. Most notably, the Choice Plus product offered by Golden Rule is now subject to the standard Admission Notification requirements described in the Guide. New products offered by UnitedHealthcare Life Insurance Company (UHCLIC) are now subject to the standard Advance AND Admission Notification requirements described in the Guide. Network Bulletin: January 2014 - Volume 59 Other Sections That Include Updates: When is Advance Notification Required, Cardiology Notification/Prior Authorization Protocol for Commercial Customers, Radiology Notification/Prior Authorization Protocol for Commercial Customers, Specialty Drug Prior Authorization for Medical Benefit (for Commercial Customers only), Self-Referral and Anti-Kickback, Claim reconsideration and appeals process and resolving disputes and UnitedHealth Premium Designation Program (for Commercial Customers only). Please contact your Network Management representative, Physician Advocate, or Hospital & Facility Advocate for a hard copy of the UnitedHealthcare Administrative Guide or Advance Notification List. * Except as otherwise noted, the new Guide is effective on April 1, 2014 for currently contracted providers, and effective immediately for providers newly contracted on or after Jan. 1, 2014. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center Important Changes in Advance Notification and Prior Authorization Requirements for Home Health Services for Medicare Advantage Plans Effective for dates of service on or after Feb. 1, 2014, Advanced Notification for the initial 60 days of home health services is no longer required for the following list of home health services. Notification for the second and subsequent 60 days of continuous home health services will be required. Clinical documentation may be requested in order to determine coverage for these services. Home infusion services are not included. • Nursing services in the home, including RN, LPN, and Home Health Aide • Therapies in the home, including occupational, physical, speech and respiratory • Social worker in the home The following documentation should be maintained for home health services in accordance with the Centers for Medicare & Medicaid Services (CMS) guidelines and may be requested for clinical review: • Current plan of care • Face-to-face encounter (documentation the physician has seen the patient and written the order) • Signed plan of care from previous 60 days (requires physician signature) • Current nursing and therapy notes with brief clinical summary and assessment of the patient including homebound status Authorization requests should include: • Start of care date • The date span for service being requested • Home health service codes and diagnosis codes • The number of units for each service requested, if applicable Continued > 16 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center Important Changes in Advance Notification and Prior Authorization Requirements for Home Health Services for Medicare Advantage Plans < Continued Please remember that private duty nursing and hospice services are generally not a covered benefit for Medicare Advantage Plans. There are some exceptions. For questions regarding benefit coverage please contact Customer Service at the # on the back of the member’s ID card. There is no change to the Authorization requirements related to Enteral Feed Services. Medicare coverage rules are still in effect for Medicare Advantage members and specific services will continue to not be covered by Medicare, including but not limited to home health services furnished when the member is not in need of any other skilled service and part time or intermittent skilled nursing or home health aide services (when combined) greater than eight hours a day or more than 28 hours per week except when authorized on a case-by-case basis to be more than eight hours a day and 35 hours or fewer hours per week. 17 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center UnitedHealthcare Community Plan to Start Using National Comprehensive Cancer Network Compendium Effective Feb. 15, 2014, UnitedHealthcare Community Plan will start using the National Comprehensive Cancer Network (NCCN) Compendium in reviewing requests for coverage for chemotherapy injectable drugs (J9000 – J9999) administered in an outpatient setting for members ages 19 and older. The NCCN Compendium provides an independent resource for use in making chemotherapy coverage decisions. There are some important details to note with this policy: 1. If the NCCN Compendium lists the drug with a recommendation level 1, 2A or 2B for the condition, the service is eligible for reimbursement based on the member’s certificate of coverage. In general, we do not cover recommendations with Level 3 evidence. 2. NCCN updates its compendium as new drugs or changes are made. 4. This policy applies to chemotherapy drugs (J9000 – J9999). It does NOT apply to supportive care drugs (i.e., erythropoiesis- stimulating agents, antiemtics, colony stimulating factors). 5. The policy applies to members ages 19 and older. The majority of pediatric patients receive treatments on national pediatric protocols that are similar in concept to the NCCN patient care guidelines. 3. This new drug policy requires that you always include the primary cancer diagnosis on the claim. Claims submitted with only a V58.1 diagnosis code may require additional information prior to a coverage decision. 18 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center Injectable Chemotherapy Prior Authorization Program for Florida Providers UnitedHealthcare’s Injectable Chemotherapy Prior Authorization Program will be managed by CareCore National’s Oncology Division and providers will be able to obtain injectable chemotherapy authorizations on CareCore’s website. 19 Network Bulletin: January 2014 - Volume 59 Authorizations that follow NCCN regimens will be approved at the time of the request online. Requests for pediatric chemotherapy regimens, rare cancers, or chemotherapy regimens that are not NCCN recommended, can also receive a timely response if necessary supporting documentation is provided at the time of prior authorization request. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center UnitedHealthcare Shared Services Expansion for GEHA Through a shared services arrangement, UnitedHealthcare provides access to the UnitedHealthcare Options Preferred Provider Organizations (PPO) Network to Government Employees Health Association (GEHA) members in AL, AK, CO, DC, DE, ID, IA, LA, MD, MS, MT, MN, NE, NM, ND, OK, SD, TN, UT, VA, WV, WI and WY. For eligibility, summary of benefits, outpatient precertification requirements and claim status, call the dedicated self-service line at 877-343-1887 or email uhss@umr.com. As of Jan. 1, 2014, GEHA will be accessing UnitedHealthcare Options PPO provider contracts in the state of Ohio. GEHA is the second-largest national health plan for civilian federal employees nationwide. Please check the back of the member’s ID card for contact information. 20 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center myHCE: Providing Cost Transparency for a More Informed Health Care Consumer UnitedHealthcare launched the myHealthcare Cost Estimator (myHCE) last year to assist members in making informed decisions regarding treatment options, providers and cost estimates. myHCE is an integrated online tool providing quality rating information and cost estimates for common treatments and procedures for in-network hospitals and physicians. Estimates are personalized to reflect a member’s specific health plan benefits, including their real-time copays and deductibles. We continue to enhance myHealthcare Cost Estimator to empower members with relevant information about estimated health care costs and quality rating information. Changes in 2014 to myHCE include: 21 • Continued expansion of Care Paths to include inpatient and outpatient high volume services such as behavioral health • Cost estimates for Optum business Network Bulletin: January 2014 - Volume 59 • Effective Jan. 1, 2014, a limited offering to one Medicare National Preferred Provider Organization (NPPO) Retiree Plan (State Health Plan of North Carolina retirees). Currently the tool is not available to other Medicare members. • Support for Executive Medical Plan Resources for Network Hospitals and Physicians can be found on UnitedHealthcareOnline > Tools & Resources > Health Resources for Patients > Transparency (myHCE). For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center Prepare for UnitedHealthcareOnline.com Login Migration to Optum Cloud Dashboard If you haven’t already transitioned to the new UnitedHealthcareOnline.com login process, you will be transitioned early this year. Please watch for an email notifying you of your migration date. When you login to UnitedHealthcareOnline.com on that date and after, you will automatically be redirected to the Optum Cloud Dashboard website. If you aren’t registered, please follow the steps for Password Owners or Standard Users so that you can continue to use secure transactions on UnitedHealthcareOnline.com. If you are registered on Optum Cloud Dashboard, you will be able to return to UnitedHealthcareOnline.com or stay on Optum Cloud Dashboard to use the available applications. No further action is required for login migration. 22 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center The CMS “Two Midnight Rule” – Effective Oct. 1, 2013 The Centers for Medicare & Medicaid Services (CMS) 2014 Fiscal Year Inpatient Prospective Payment System Final Rule became effective Oct. 1, 2013 and includes clarification about when a patient should be admitted to the hospital. This provision, known as the “Two Midnight Provision,” is intended to help you and auditors determine whether a Medicare claim should be billed under Part A (inpatient) or Part B (outpatient). two or more midnights, inpatient admission is appropriate. If you expect the member’s medically necessary treatment will span less than two midnights, assign it outpatient status.1 UnitedHealthcare started implementing the CMS TwoMidnight Provision for our Medicare Advantage plans in October 2013 by incorporating the clarification into our concurrent review programs. We plan to fully integrate the provision over the coming year. The Final Rule emphasizes the need for a formal order of inpatient admission to begin inpatient status, but permits the physician to consider all time a patient has already spent in the hospital as an outpatient receiving observation services, or in the emergency department, operating room, or other treatment area in guiding their two-midnight expectation. Please review the links at the end of this article for details about the provision, which states that if a member requires medically necessary hospital care that is expected to span Continued > 23 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center The CMS “Two Midnight Rule” – Effective Oct. 1, 2013 < Continued The Final Rule supports the continued use of evidencebased guidelines to help with deciding whether to admit a patient. Therefore, UnitedHealthcare will continue to use evidence-based guidelines to support consistent, clinically validated decision-making for hospital admissions which are medically necessary. We will review “the reasonableness of the physician’s expectation of the need for and duration of care based on complex medical factors such as history and comorbidities, the severity of signs and symptoms, current medical needs and the risk of an adverse event, which must be clearly documented.” 2 While CMS has delayed enforcing the Two Midnight Provision, they have not changed the effective date of Oct. 1, 2013. Rather, they are issuing guidance to Medicare Administrative Contractors (MACs) about how to select hospital claims for review during a “Probe and Educate” program for admissions that occur between Oct. 1, 2013 and March 31, 2014. While this guidance is not directed towards Medicare Advantage plans, we will continue to monitor CMS publications while developing 24 Network Bulletin: January 2014 - Volume 59 our internal clinical review programs, and will continue to work collaboratively with you as we adapt to these clarifications. CMS resources: Federal Register/Vol. 78, No. 160/Monday, August 19, 2013:http://www.gpo.gov/ fdsys/pkg/FR-2013-08-19/pdf/2013-18956.pdf CMS FAQ: http://cms.gov/Research-Statistics-Data-and-Systems/Monitoring-Programs/ Medical-Review/Downloads/QAsforWebsitePosting_110413-v2-CLEAN.pdf Selecting claims for patient status reviews: http://cms.gov/Research-Statistics-Data-and-Systems/MonitoringProgramsMedical-Review/Downloads/SelectingHospitalClaimsfor ReviewForWebPostingCLEAN.pdf Reviewing hospital claims for patient status: http://cms.gov/Research-Statistics-Data-and-Systems/Monitoring-Programs/ Medical-Review/Downloads/ReviewingHospitalClaimsforAdmissionFINAL.pdf CMS Frequently Asked Questions: 2 Midnight Inpatient Admission Guidance and Patent Status Reviews for Admissions after October 1, 2013 (“CMS FAQ”) (Question and Answer No. 8): http://cms.gov/Research-StatisticsData-and-Systems/Monitoring-Programs/Medical-Review/Downloads/ QAsforWebsitePosting_110413-v2-CLEAN.pdf 1 CMS FAQ (Question and Answer No. 9) 2 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center 2014: The Year of the ICD-10 Code This year the health care industry will adopt and use International Classification of Disease, Tenth Revision (ICD-10) codes. The Department of Health and Human Services mandates the use of ICD-10 codes for dates of service on or after Oct. 1, 2014. 25 To support our providers during this transition, UnitedHealthcare offers the following tools at UnitedHealthcareOnline.com to assist you in becoming ICD-10 compliant: • • ICD-10 Education - on-demand educational resources designed to provide general information regarding ICD-10 and the implementation process. ICD-10 Tools - in collaboration with the American Academy of Professional Coders (AAPC), the largest coding organization in the country, we have created a suite of tools including ICD-10 code selection decision trees and detailed clinical documentation improvement webinars. Network Bulletin: January 2014 - Volume 59 • ICD-10 Resources - a listing of industry-wide ICD-10 resources. • ICD-10 Partnerships - in addition to AAPC, we are working with Optum to offer value-added solutions for cost-effective adoption of ICD-10. For answers to your questions regarding ICD-10, please send your inquiry to ICD10questions@uhc.com. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center Enhanced HIPAA Edits to be Applied to Claim Submissions Effective April 23, 2014, UnitedHealthcare will apply an enhanced level of HIPAA edits to professional (837p) and institutional (837i) claims submitted electronically to most UnitedHealthcare and affiliate payer IDs.* Because the new edits will be applied on a pre-adjudication basis, an increase in the number of claim rejections may occur. This will enable you to identify and correct rejected information prior to the claim’s acceptance into our adjudication system for processing. The benefit will be fewer denied claims and less interruption to revenue streams. The primary impact to you will come from edits that will validate code sets (such as diagnosis, procedure, modifier and national drug codes) at a pre-adjudication level. The complete list of enhanced edits has been distributed to clearinghouses and software vendors. It is important to check all of your claim submission reports regularly. Claims may be rejected by your clearinghouse or UnitedHealthcare; therefore, you may receive multiple reports per submission. Visit UnitedHealthcareOnline.com for more information about tracking your electronic claims. Rejections that may occur from the enhanced edits will appear at a clearinghouse level. Your Electronic Data Interchange (EDI) vendor or clearinghouse should be your first point of contact for assistance regarding these edits or to resolve rejections. For more information, please contact EDI Support: UnitedHealthcare Commercial, UnitedHealthcare Medicare Solutions and UnitedHealthcare West EDI issue reporting form or 800-842-1109 UnitedHealthcare Community Plan ac_edi_ops@uhc.com or 800-210-8315 UnitedHealthcare Oxford ediproviderassistance@oxhp.com or 800-599-4334 * Exceptions: Harvard Pilgrim (04271), Medica HealthCare Plans (78857), Preferred Care Partners (65088), The Alliance (88461) and TRICARE West (99726) 26 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center HIPPS Codes Requirement for Home Health Care and Skilled Nursing Facility Encounters In the November 2013 Network Bulletin, we informed you of CMS’s new requirement for all Medicare Advantage Organizations to begin submitting HIPPS codes on all skilled nursing facility and home health care encounter data. Since our last communication, CMS has delayed implementation of the requirement to July 1, 2014. You should continue to prepare your systems and processes to be able to provide HIPPS codes on claims for UnitedHealthcare Medicare Advantage members, however until further notice, please continue to submit claims to us as you have in the past. We will notify you in advance regarding when to begin submitting HIPPS codes on claims. In the absence of specific CMS guidance, at this time please follow the standard Medicare process for identifying the appropriate HIPPS codes for your patients. 27 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center Medicare Advantage to Require Prior Authorization for IMRT, SRS and SBRT as of April 1 Effective Apr. 1, 2014, Medicare Advantage health plans will require prior authorization for Intensity Modulated Radiation Therapy (IMRT), Stereotaxic Radiosurgery (SRS) and Stereotactic Body Radiation Therapy (SBRT) when administered in an outpatient setting. Additional details about the program will be posted on our physician portal in two locations: UnitedHealthcareOnline.com > Clinical Resources > Cancer – Oncology > IMRT – Medicare Advantage. You can also go to: UnitedHealthcareOnline.com > Clinical Resources > Cancer – Oncology > SRS and SBRT – Medicare Advantage. 28 Network Bulletin: January 2014 - Volume 59 Medicare Advantage IMRT, SRS and SBRT Prior Authorization training and live question and answer sessions will be hosted by WebEx in March 2014. Additionally, registration details will be posted on the websites in March 2014. See the above websites for specific schedule dates. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center Medicare Advantage Radiology and Cardiology Prior Authorization Program to Deploy for UnitedHealthcare West Medicare Non-Capitated Participating Providers on April 1, 2014 For a complete list of CPT Codes that require prior authorization, please visit UnitedHealthcareOnline.com > Clinician Resources > Radiology > Medicare Advantage Radiology Prior Authorization Program > 2014 Radiology Prior Notification/Authorization CPT Code List. UnitedHealthcare West Medicare Advantage Non-Capitated Beginning April 1, 2014, participating physicians, facilities and other health care professionals who are subject to the Administrative Guide and the UnitedHealthcare West Non-Capitated Supplement and practice in Arizona, Oklahoma, Oregon, Texas and Washington, must obtain prior authorization for certain outpatient radiology procedures before they are rendered to UnitedHealthcare West Medicare Advantage members. Those states, as well as Colorado, must also do the same for cardiology procedures, beginning April 1, 2014. Radiology Prior Authorization Beginning April 1, 2014: • Ordering providers who are subject to the Administrative Guide and the UnitedHealthcare West Non-Capitated Supplement and practice in Arizona, Oklahoma, Oregon, Texas and Washington will have a new phone number and website link that is to be used to obtain prior authorization prior to scheduling certain CT, MRI, MRA, PET scan, Nuclear Medicine, and Nuclear Cardiology procedures for UnitedHealthcare West Medicare Advantage members. The advanced imaging procedures requiring prior authorization are referred to as advanced outpatient imaging procedures. Ordering providers will need to obtain the required prior authorization number by using the new contact methods: • Online: UnitedHealthcareOnline.com > Notifications/Prior Authorizations > Radiology Notification & Authorization - Submission & Status. • Phone: 866-889-8054 - select the option for Medicare Advantage customers and then select the option for outpatient diagnostic imaging. Once a prior authorization request for a planned advanced outpatient imaging procedure is received, UnitedHealthcare will conduct a clinical coverage review to determine whether the service is medically necessary. The provider will be informed of the decision. Continued > 29 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center Medicare Advantage Radiology and Cardiology Prior Authorization Program to Deploy for UnitedHealthcare West Medicare Non-Capitated Participating Providers on April 1, 2014 < Continued • Rendering providers who are subject to the Administrative Guide and the UnitedHealthcare West Non-Capitated Supplement and practice in Arizona, Oklahoma, Oregon, Texas and Washington must confirm that the prior authorization process has been completed and a coverage decision has been issued before rendering any advanced outpatient imaging procedure. If the ordering provider does not participate in UnitedHealthcare West’s network and is unwilling to complete the prior authorization process, the rendering provider must complete the prior authorization process and verify that a coverage decision has been issued prior to rendering the advanced outpatient imaging procedure. Providers are not required to obtain prior authorization for any advanced imaging procedures rendered in an emergency room, urgent care center, observation unit or during an inpatient stay. Cardiology Prior Authorization Beginning April 1, 2014: • Ordering providers who are subject to the Administrative Guide and the UnitedHealthcare West Non-Capitated Supplement and practice in Arizona, Colorado, Oklahoma, Oregon, Texas and Washington must obtain prior authorization prior to scheduling certain diagnostic catheterizations, electrophysiology implants, echocardiograms and stress echocardiograms procedures for UnitedHealthcare West Medicare Advantage members. For a complete list of CPT Codes that require prior authorization, please visit UnitedHealthcareOnline.com > Clinician Resources > Cardiology > Medicare Advantage Cardiology Prior Authorization Program > 2014 Cardiology Prior Authorization Table and CPT Code Crosswalk. Once a prior authorization request for a planned cardiology procedure is received, UnitedHealthcare will conduct a clinical coverage review to determine whether the service is medically necessary. The provider will be informed of the decision. • Rendering providers who are subject to the Administrative Guide and the UnitedHealthcare West NonCapitated Supplement and practice in Arizona, Colorado, Oklahoma, Oregon, Texas and Washington must confirm that the prior authorization process has been completed and verify that a coverage decision has been issued before rendering any cardiology procedure. Continued > 30 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center Medicare Advantage Radiology and Cardiology Prior Authorization Program to Deploy for UnitedHealthcare West Medicare Non-Capitated Participating Providers on April 1, 2014 Prior authorization for diagnostic catheterizations, echocardiograms and stress echocardiograms is required for outpatient and office-based services only. Prior authorization for electrophysiology implants is required for outpatient, officebased and inpatient services. Cardiology procedures rendered in and appropriately billed with any of the following places of service do not require prior authorization: emergency room, urgent care center or inpatient setting (except for electrophysiology implants, which require prior authorization during an inpatient stay). Medicare Advantage Plans Subject to This Prior Authorization Process As of the effective date of this communication, the prior authorization requirements set forth above will apply to UnitedHealthcare West’s Medicare Advantage plans that are subject to the Administrative Guide and UnitedHealthcare West Non-Capitated Supplement including but not limited to UnitedHealthcare® Medicare Complete®, UnitedHealthcare Dual Complete™, UnitedHealthcare® Chronic Complete and AARP® MedicareComplete® plans. Please note that excluded plans may have separate radiology or cardiology prior authorization requirements. Please refer to the respective supplements in the Administrative Guide for details. For additional information, see the following Additional Resource Information section: Additional Resource Information Prior Authorization Process Providers must (a) provide notification and complete the prior authorization process, and (b) confirm that a coverage decision has been made as follows: • Online at UnitedHealthcareOnline.com > Notifications/ Prior Authorizations > Radiology Notification & Authorization – Submission & Status. • Online at UnitedHealthcareOnline.com > Notifications/ Prior Authorizations > Cardiology Notification & Authorization – Submission & Status. • Call 866-889-8054 (7 a.m. to 7 p.m. local time, Monday – Friday). Please note that payment for covered services is contingent upon coverage under the member’s benefit plan, the provider’s eligibility for payment, any claim processing requirements and the provider’s participation agreement with UnitedHealthcare West. Continued > 31 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center Medicare Advantage Radiology and Cardiology Prior Authorization Program to Deploy for UnitedHealthcare West Medicare Non-Capitated Participating Providers on April 1, 2014 < Continued Failure to Complete the Prior Authorization Process and Meet Medical Necessity Criteria Failure to provide notification and complete the prior authorization process, or verify that a coverage determination has been issued, prior to rendering an advanced outpatient imaging procedure or cardiology procedure will result in an administrative claim reimbursement reduction, in part or in full. Members cannot be billed for claims that are administratively denied. For UnitedHealthcare West Medicare Advantage benefit plans, an authorization number is issued for both approved and clinically denied prior authorizations. A clinical denial will be issued if it is determined during the clinical coverage review process that the service does not meet medical necessity criteria. The clinical denial will be communicated via a letter faxed to the provider and a letter will be mailed to the Medicare Advantage member. Additional Information About Process Additional information regarding the requirements you must follow, including requirements with respect to urgent requests and the retrospective notification process, is set forth in the (a) Outpatient Radiology Prior Authorization Protocol for Medicare Advantage members, and (b) Cardiology Prior Authorization Protocol for Medicare Advantage members. These protocols are set forth in the Administrative Guide. We strongly encourage you to review the protocols. Members can be billed for requested services that are clinically denied, provided adequate written consent is obtained from the member prior to rendering the service. 32 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center RUN_DATE DATA_SEQ_NO CLIENT_NUMBER UHG_TYPE DOC_SEQ_ID DOC_ID NAME MAILSET_NUMBER CUSTCES_KEY1 00000100001_KEY0 CUSTCES_KEY2 CUSTCES_KEY3 CUSTCES_KEY4 CUSTCES_KEY5 CUSTCES_KEY6 CUSTCES_KEY7 CUSTCES_KEY8 CUSTCES_KEY9 SMITH 20130917 DIG2CARD 0000001 0000001 00000100001 0755733 EMPLOYEE HCAC/Medical 00 01 02 03 04 20130917 00000100001~00CARD1 00000100001~01CARD1 00000100001~02CARD1 00000100001~03CARD1 00000100001~04CARD1 00000100001~00CARD2 00000100001~01CARD2 00000100001~02CARD2 00000100001~03CARD2 00000100001~04CARD2 123456789 123456789~00CARD1 123456789~01CARD1 123456789~02CARD1 123456789~03CARD1 123456789~04CARD1 123456789~00CARD2 123456789~01CARD2 123456789~02CARD2 123456789~03CARD2 123456789~04CARD2 003082 0000001 CARD1 CARD2 09:08:54 Contraceptive Services Only Benefit and Eligible Organizations About the Contraceptive Services Only Benefit Under the Patient Protection and Affordable Care Act (PPACA), most health insurance plans must cover certain birth control methods (contraceptives and sterilization) for women at no cost - when received from an in-network doctor, health care professional or pharmacy. Women who request the Contraceptive Services Only (CSO) benefit will receive a CSO ID card. This card is like a regular UnitedHealthcare member ID card and must be used at the doctor’s office or pharmacy to ensure they don’t pay for the birth control drugs, products or services covered by the Contraceptive Services Only benefit. Contraceptive Services Only UHC 123 Any Street Hartford CT 12345 Download a free QR code reader and scan this code to learn about convenient Smartphone access to benefit and provider information with myuhc.com7 mobile. Member ID: Member: EMPLOYEE SMITH 755733 Contraceptive Services Only Dependents SPOUSE SMITH CHILD1 SMITH CHILD2 SMITH CHILD3 SMITH 03082 9275950 0000 0 Network Bulletin: January 2014 - Volume 59 Important: Please register at myuhc.com to view your coverage and manage claims. 911-87726-04 123456789 Group Number: Health Plan (80840) DOI-0501 33 >000001 9275950 001 003082 EMPLOYEE SMITH 111 MAIN ST. ANYTOWN ST 12345-6789 Some nonprofits, referred to as Eligible Organizations, don’t have to cover birth control as part of their group health plan for religious reasons. Eligible Organizations will not contract, arrange, pay, or refer for contraceptive coverage, as part of their group health plan. Instead, UnitedHealthcare will pay for certain types of female birth control for members without cost-sharing through our “Contraceptive Services Only” benefit, which we are required by law to make available to members. Welcome to UnitedHealthcare Women’s Preventive Care Services Updates This a pr For Payer ID 87726 Rx Bin: 610279 Rx PCN: 9999 Rx Grp: UHEALTH For Med UnitedHealthcare Choice Pha Underwritten by [Appropriate Legal Entity] Continued > 911-87726-04 Member ID: 123456789 Group Number: 755733 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com Member: Health Plan (80840) EMPLOYEE SMITH Dependents Contraceptive Services Only This a pr For HOME TABLE OF CONTENTS Next Article > Front & Center Women’s Preventive Care Services Updates < Continued Important Information About the CSO Benefit • Members may purchase breast pumps without cost-share by contacting a network doctor or durable medical equipment (DME) supplier within 30 days of the estimated delivery date. (Previously, mothers had to be lactating before receiving a breast pump.) Only female birth control on the CSO list is available at no cost. And includes many types of birth control that are covered, including: birth control pills, female condoms, and long-lasting birth control. • Birth control services must be received at an in-network pharmacy or doctor’s office. For a list of breast pump suppliers, members may call the number on the back of their ID card. • If contacting the breast pump supplier directly, members may be asked for their doctor’s contact information, the baby’s due date or the date the baby was delivered. The breast pump supplier may verify this and other information with the member’s doctor before the breast pump is shipped. • Members Can Now Receive Breast Pumps Within 30 Days of Delivery National breast pump suppliers ship the breast pump directly to the lactating mother. • Under PPACA, breast-feeding services and equipment are covered without cost-sharing when received by a network provider, during pregnancy and/or in the postpartum period. The doctor or DME supplier will bill UnitedHealthcare directly for reimbursement. • Members do not need a prescription when contacting a DME breast pump supplier. • Members will not be reimbursed for breast pumps purchased at retail stores. • • Members must have a prescription for this birth control to be covered at no cost - even for items that can be purchased without a prescription. For more information, please call your Provider Advocate or Provider Services. Continued > 34 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Front & Center Women’s Preventive Care Services Updates < Continued Our Preventive Care Services Coverage Determination Guideline was updated Jan. 1, 2014 to reflect this change. How Members Obtain a Breast Pump For more information, contact your Physician Advocate or Provider Services; or visit the United for Reform Resource Center at uhc.com/reform and click the preventive services provision for the latest health reform news or review our Preventive Care Services Coverage Determination Guideline information about what preventive services must be covered under the health reform law is found at HealthCare.gov. 35 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Commercial UnitedHealthcare Medical Policy, Drug Policy, Coverage Determination Guideline and Utilization Review Guideline Updates For complete details on the new and/or revised policies and guidelines listed in the table on the following page, refer to the monthly Medical Policy Update Bulletin at UnitedHealthcareOnline.com > Tools & Resources > Policies, Protocols and Guides > Medical & Drug Policies and Coverage Determination Guidelines > Medical Policy Update Bulletin. 36 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Medical Policy, Drug Policy, Coverage Determination Guideline and Utilization Review Guideline Updates Policy Title Policy Type Effective Date Medical Policy Update Bulletin All Jan. 1, 2014 Jan. 2014 Enzyme Replacement Therapy for Gaucher Disease Drug Policy Feb. 1, 2014 Nov. 2013 Dec. 2013 Jan. 2014 Mechanical Circulatory Support Device (MCSD) Clinical Guideline Jan. 1, 2014 Nov. 2013 Dec. 2013 Medical Policy Jan. 1, 2014 Dec. 2013 TAKE NOTE Annual CPT® and HCPCS Code Updates NEW UPDATED/REVISED Abnormal Uterine Bleeding and Uterine Fibroids Continued > 37 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > < Continued UnitedHealthcare Commercial UnitedHealthcare Medical Policy, Drug Policy, Coverage Determination Guideline and Utilization Review Guideline Updates Policy Title Policy Type Effective Date Medical Policy Update Bulletin Apheresis Medical Policy Jan. 1, 2014 Dec. 2013 Bariatric Surgery Medical Policy Jan. 1, 2014 Dec. 2013 Blepharoplasty, Blepharoptosis, and Brow Ptosis Repair Coverage Determination Guideline Jan. 1, 2014 Dec. 2013 Campath (Alemtuzumab) Drug Policy Jan. 1, 2014 Dec. 2013 Cardiovascular Disease Risk Tests Medical Policy Jan. 1, 2014 Dec. 2013 Epidural Steroid and Facet Injections for Spinal Pain Medical Policy Nov. 1, 2013 Nov. 2013 Hearing Aids and Devices Including Wearable, Bone-Anchored and Semi-Implantable Medical Policy Dec. 1, 2013 Nov. 2013 Hip Resurfacing Arthroplasty Medical Policy Jan. 1, 2014 Dec. 2013 Immune Globulin (IVIG) Drug Policy Dec. 1, 2013 Nov. 2013 Omnibus Codes Medical Policy Jan. 1, 2014 Dec. 2013 Oncology Medication Clinical Coverage Policy Drug Policy Jan. 1, 2014 Dec. 2013 Polysomnography and Portable Monitoring for Evaluation of Sleep Related Breathing Disorders Medical Policy Dec. 1, 2013 Nov. 2013 Preventive Care Services Coverage Determination Guideline Jan. 1, 2014 Dec. 2013 Continued > 38 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > < Continued UnitedHealthcare Commercial UnitedHealthcare Medical Policy, Drug Policy, Coverage Determination Guideline and Utilization Review Guideline Updates Policy Title Policy Type Effective Date Medical Policy Update Bulletin Proton Beam Radiation Therapy Medical Policy Jan. 1, 2014 Dec. 2013 Repository Corticotropin Injection (H.P. Acthar Gel) Drug Policy Dec. 1, 2013 Nov. 2013 Transcatheter Heart Valve Procedures Medical Policy Jan. 1, 2014 Dec. 2013 Breast Pump Utilization Review Guideline Jan. 1, 2014 Dec. 2013 Cardiac Outpatient Rehabilitation (Exercise Training) Coverage Determination Guideline Nov. 1, 2013 Nov. 2013 Complementary and Alternative Medicine Coverage Determination Guideline Nov. 1, 2013 Nov. 2013 Definition of Medically Necessary Coverage Determination Guideline Nov. 1, 2013 Nov. 2013 Dental Exclusion and Accidental Dental Coverage Determination Guideline Jan. 1, 2014 Jan. 2014 Hearing Aids Coverage Determination Guideline Dec. 1, 2013 Nov. 2013 Hyperbaric Oxygen Therapy and Topical Oxygen Therapy Medical Policy Jan. 1, 2014 Jan. 2014 Maternity Services and Complications Coverage Determination Guideline Dec. 1, 2013 Dec. 2013 RETIRED Continued > 39 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > < Continued UnitedHealthcare Commercial UnitedHealthcare Medical Policy, Drug Policy, Coverage Determination Guideline and Utilization Review Guideline Updates Policy Title Policy Type Effective Date Medical Policy Update Bulletin Nutrition (Including: Counseling, Therapy, Enteral Nutrition, Infant Formula, Breast Milk, Supplements and Food) Coverage Determination Guideline Dec. 1, 2013 Dec. 2013 Physical Medicine and Rehabilitation ServicesInpatient and Outpatient Coverage Determination Guideline Nov. 1, 2013 Nov. 2013 Pulmonary Rehabilitation - Outpatient Coverage Determination Guideline Nov. 1, 2013 Nov. 2013 Snoring Treatment Coverage Determination Guideline Dec. 1, 2013 Nov. 2013 Total Ankle Replacement (Arthroplasty) Medical Policy Jan. 1, 2014 Jan. 2014 Treatment of Complications Coverage Determination Guideline Nov. 1, 2013 Nov. 2013 Wireless Capsule Endoscopy Medical Policy Jan. 1, 2014 Jan. 2014 Note: The appearance of a service or procedure on this list does not imply that UnitedHealthcare provides coverage for the service or procedure. In the event of an inconsistency or conflict between the information provided in this bulletin and the posted policy, the provisions of the posted policy will prevail. 40 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > The new forms for the UnitedHealthcare Intensity Modulated Radiation Therapy (IMRT) prior authorization program will be posted on our website in January 2014. You can find the forms at: UnitedHealthcareOnline > Clinician Resources > Cancer – Oncology > IMRT > Related Links. We are changing the data collection form to enable the requesting physician to provide disease-specific clinical details for the radiation oncologist reviewing the prior authorization request. On our website, under Related Links, you will find the disease-specific forms. If a form is not available for the patient’s medical condition, a generic form will be available. Please note that incomplete forms may delay the review for IMRT services. 41 Network Bulletin: January 2014 - Volume 59 Questions can be forwarded to unitedoncology@uhc.com. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > The Preferred Payment Method for Your UnitedHealthcare Patients: Member Payments Last summer, UnitedHealthcare implemented a new online payment capability for UnitedHealthcare members to make online payments directly to you and all their health care providers through myuhc.com. We are the first national insurance carrier to offer our members online bill payment capabilities that are fully integrated with online claim information. Online Member Payments, designed in collaboration with InstaMed, a leading health care payments network, helps you get paid faster and easier than ever. Since the implementation, there has been a steady growth in patients using the service, averaging an additional 1,000 unique patients each day who are paying online at myuhc.com. • UnitedHealthcare members appreciate the capability because they can manage their claims and health care expenses all from one site. How Online Member Payments Work: Providers register to receive patient payments electronically, which are then deposited directly into your designated bank accounts. • The fee is a flat rate of 2.99 percent per transaction when patients pay using credit/debit cards, and 1.5 percent when patients pay using their bank account. • There are no sign-up fees, no monthly fees, and no minimum usage fees. • InstaMed (the payments processor) sends email notifications to providers when patient payments have been made. • Automatic posting of these payments can be made directly to your patient accounting system. Registered Providers: • Registered providers pay a low merchant transaction fee, similar to what you pay today when patients pay with credit/debit or bank withdrawals. Continued > 42 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > The Preferred Payment Method for Your UnitedHealthcare Patients: Member Payments < Continued Non-Registered Providers: 43 • If you haven’t registered, UnitedHealthcare members can still pay you online from their member portal. • You will receive these patient payments by mail in the form of a one-time use MasterCard debit card. • You incur normal costs to process these payments through your existing merchant account - no additional fee is charged. • Payments are manually processed similar to a remittance and posted to your patients’ accounts. Network Bulletin: January 2014 - Volume 59 Register to receive these payments directly deposited to your bank account by visiting www.uhcmemberpayments.com. If you have questions or want to learn more, sign up to attend a webinar training session. You can also contact info@instamed.com, call 215-789-3682 or contact your UnitedHealthcare Physician or Hospital Advocate. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Reimbursement Policy Unless otherwise noted, these reimbursement policies apply to services reported using the 1500 Health Insurance Claim Form (CMS-1500) or its electronic equivalent or its successor form. UnitedHealthcare reimbursement policies do not address all factors that affect reimbursement for services rendered to UnitedHealthcare members, including member benefit plan documents, UnitedHealthcare medical policies and the UnitedHealthcare Physician, Health Care Professional, Facility and Ancillary Provider Administrative Guide. Meeting the terms of a particular reimbursement policy is not a guarantee of payment. Once implemented the policies may be viewed in their entirety at UnitedHealthcareOnline.com > Tools & Resources > Policies and Protocols > Reimbursement Policies-Commercial. In the event of an inconsistency or conflict between the information provided in the Network Bulletin and the posted policy, the provisions of the posted policy prevail. 44 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Reimbursement Policy Revision to CCI Editing Policy Previously announced as a revision to the Rebundling Policy and effective in the first quarter of 2014, UnitedHealthcare will deny Preventive Medicine Evaluation and Management (E/M) services (CPT codes 99381-99397) when reported on the same date of service as an immunization administration service (CPT codes 90460-90461 and 90471-90474) through the CCI Editing Policy. This change aligns with the CMS National Correct Coding Initiative (NCCI) and the American Medical Association Current Procedural Terminology (CPT®) If modifier 25 is reported with the Preventive Medicine E/M service and the documentation supports that a significant and separately identifiable E/M service was provided on the same date as the administration service, both would be reimbursed. It would not be appropriate to additionally report the Preventive Medicine E/M code for the counseling provided when a vaccine is administered. 45 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Reimbursement Policy Revision to the Professional/Technical Component PolicyDenial of Drug Administration Codes and PC/TC Indicator 8 According to the CMS NCCI Policy Manual, drug administration codes (CPT 96360-96379, 96401-96425, and 96521-96523) are considered included in the facility payment when reported in place of service (POS) 24 (ambulatory surgical center (ASC)). Additionally, the CMS National Physician Fee Schedule guidelines advise that payment should not be recognized for professional/technical (PC/TC) Indicator 8 codes, which are defined as physician interpretation codes, furnished to patients in the outpatient or non-hospital setting. 46 Network Bulletin: January 2014 - Volume 59 To better align with CMS, UnitedHealthcare will deny drug administration codes (CPT 9636096379, 96401-96425, and 96521-96523) reported by a physician or other health care professional in a POS 24. We will also deny PCTC Indicator 8, CPT code 85060, when reported by a physician or other health care professional with a place of service code other than inpatient hospital (POS 21). This change will occur in the second quarter of 2014. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Reimbursement Policy Multiple Procedure Policy Revisions to Apply to Same Group The revision to the Multiple Procedure Policy, announced in the July 2013 Network Bulletin, was partially implemented for three weeks, from November 17, 2013 through December 7, 2013. The revision administered multiple procedure reductions to eligible surgical and medical procedures provided on the same day and reported by the same group practice, which included all physicians and other health care professionals with the same federal tax identification number. To allow for system enhancements, effective with dates of process beginning December 8, 2013, the Multiple Procedure Policy temporarily reverted to the previous method of applying multiple procedure reductions for secondary and subsequent eligible services only when provided on the same day to the same patient by the same individual physician or health care professional. 47 Network Bulletin: January 2014 - Volume 59 In February 2014, the Multiple Procedure Policy revision will be fully implemented to again apply multiple procedure reductions based on the same group practice. This revision will align the policy with CMS guidelines with application of multiple procedure reductions to all physicians and nonphysicians in the same group practice, acting in the same capacity. Co-surgeon and team surgeon services will continue to be ranked separately from procedures reported by another physician. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Medicare Solutions 2013 Member Rewards Program – Better Health has its Rewards At UnitedHealthcare, preventive screenings are an important part of our health promotion efforts and the basis of our Member Rewards program. The 2013 Member Rewards program has ended. As a result of us working together, we sent out the following numbers of prepaid debit cards as of mid-December: • 103,864 Annual Wellness Visit/BMI rewards • 10,718 Colorectal Screening rewards • 14,442 Glaucoma Screening rewards Please continue talking to your patients about the importance of scheduling and completing a health assessment and other preventive health screenings and exams. Also, be on the look-out for communication about the 2014 Member Rewards program in the coming months. For more information, please call Provider Services at 877-842-3210 or visit Member Rewards. • 3,502 Breast Cancer Screening rewards 48 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Medicare Solutions UnitedHealthcare Wins Bid for State of Illinois The State of Illinois Department of Central Management Services announced that UnitedHealthcare was one of three bidders awarded a competitive contract to offer a Medicare Advantage plan. 49 We will offer our UnitedHealthcare Group Medicare Advantage National PPO plan to the state’s 123,000 Medicare-eligible retirees. The plan is the only plan to be available across the entire service area including retirees who live outside of Illinois. State retiree coverage is effective Feb. 1, 2014. The UnitedHealthcare Group Medicare Advantage National PPO Plan is open access with no referrals or gatekeeper. In addition, under this plan the member’s cost share is the same whether using an in-network or out-of-network provider. Network Bulletin: January 2014 - Volume 59 • Providers who are in-network for UnitedHealthcare’s Medicare Advantage products will be paid according to their current agreement for these members. • Out-of-network providers for UnitedHealthcare’s Medicare Advantage products will be paid according to Medicare’s allowable fee schedule. The UnitedHealthcare Group Medicare Advantage National PPO plan does not require prior authorizations or prior notifications for out-of-network physicians who see our members. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Medicare Solutions UnitedHealthcare Medicare Advantage Coverage Summary Updates For complete details on the revised policies listed in the table below, please refer to the Medicare Advantage Coverage Summary Update Bulletin at UnitedHealthcareOnline.com > Tools & Resources > Policies, Protocols and Guides > UnitedHealthcare Medicare Advantage Coverage Summaries > Update Bulletin. Policy Title Approval Date Update Bulletin Bariatric Surgery Oct. 24, 2013 Nov. 2013 Blood, Blood Products and Related Procedures and Drugs Oct. 24, 2013 Nov. 2013 Cardiac Pacemakers and Defibrillators Oct. 24, 2013 Nov. 2013 Cosmetic and Reconstructive Procedures Oct. 24, 2013 Nov. 2013 Experimental Procedures and Items, Investigational Devices and Clinical Trials Oct. 24, 2013 Nov. 2013 Gastroesophageal and Gastrointestinal (GI) Services and Procedures Oct. 24, 2013 Nov. 2013 Hospital Observation Care (Outpatient Hospital) Oct. 24, 2013 Nov. 2013 Hospital Services (Inpatient and Outpatient) Oct. 24, 2013 Nov. 2013 REVISED Continued > 50 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Medicare Solutions UnitedHealthcare Medicare Advantage Coverage Summary Updates < Continued Policy Title Approval Date Update Bulletin Laboratory Tests and Services Oct. 24, 2013 Nov. 2013 Positron Emission Tomography (PET)/Combined PET-CT (Computed Tomography) Oct. 24, 2013 Nov. 2013 Rehabilitation - Medical Rehabilitation (PT, OT, and ST, including Cognitive Rehabilitation) Oct. 24, 2013 Nov. 2013 Skilled Nursing Facility (SNF) Care and Exhaustion of SNF Benefits Oct. 24, 2013 Nov. 2013 Ventricular Assist Device (VAD) and Artificial Heart Oct. 24, 2013 Nov. 2013 Veteran Administration (VA) and Indian Health Services (IHS) Oct. 24, 2013 Nov. 2013 Note: The appearance of a service or procedure on this list does not imply that UnitedHealthcare provides coverage for the service or procedure. 51 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Medicare Solutions Reminder for Advance Notification and Prior Authorization This is a reminder that UnitedHealthcare requires advance notification and prior authorization for the standardized list of inpatient and outpatient procedures across Medicare plans for UB04 and HCFA billers. If you do not obtain prior authorization or verify the authorization has been obtained before rendering the procedure, it may result in an administrative claim denial. A clinical denial will be issued if it is determined during the prior authorization process that the requested service does not meet Medicare’s medical necessity criteria. 52 Network Bulletin: January 2014 - Volume 59 Follow this link for more information about the Medicare Advantage prior authorization program including medical, radiology, and cardiology: https://www.unitedhealthcareonline.com /b2c/CmaAction.do?channelId=12f8c79 58f5fa010VgnVCM100000c520720a____ For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Community Plan Important Reimbursement Policy Reminder UnitedHealthcare Community Plan’s quality of care program factors readmission review to its reimbursements to participating and non-participating facilities based upon individual state and CMS published guidelines.* Acute care admissions which occur within 30 days - or another time period depending on state guidelines or your provider agreement - of another acute care admission with the same or similar diagnosis will require a medical record review on a post service/ prepayment basis. If a readmission undergoes clinical review because of a potential quality issue, the claim may be denied. Please note that if the claim is denied in full or part, providers cannot balance bill the member for a denied claim. Please note individual state regulations and contract requirements supersede specific policy language. For more information, please refer to the UnitedHealthcare Community Plan Readmission Policy (F7001). Information That may be Requested for Medical Record Reviews Patient medical records containing the admit through discharge information for the hospital stays beginning on admit dates of service (initial admission date and subsequent admission date) need to include: • History and Physical • Admission and Discharge Summary • Physicians’ orders • Emergency room records • Progress notes • Nurses’ notes • Diagnostic and laboratory testing Continued > 53 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Community Plan Important Reimbursement Policy Reminder < Continued General Information Regarding Our Reimbursement Policies Unless otherwise noted, our reimbursement policies apply to services reported using the CMS 1450 claim form (formerly known as UB-04), or its electronic equivalent, or its successor form. UnitedHealthcare Community Plan reimbursement policies do not address all issues related to reimbursement for services rendered to our members. Other resources that address reimbursement include the member’s benefit plan documents, UnitedHealthcare Community Plan medical policies, and the UnitedHealthcare Community Plan Physician, Health Care Professional, Facility and Ancillary Provider Administrative Guide. Meeting the terms of a particular reimbursement policy is not a guarantee of payment. Likewise, retirement of a reimbursement policy affects only those system edits on claims associated with the specific policy being retired. 54 Network Bulletin: January 2014 - Volume 59 Retirement of a reimbursement policy is not a guarantee of payment. Other applicable reimbursement policies, medical policies and claims edits will continue to apply. Once implemented, the policies may be viewed in their entirety at UHCCommunityPlan.com > Find Plans By State (click on the appropriate state) > If you are a Health Professional > Reimbursement Policies. In the event of an inconsistency or conflict between the information provided in this notification and the posted policy on UHCCommunityPlan.com, the provisions of the posted reimbursement policy will prevail. If you have any questions please contact your Provider Advocate or call the number on your Provider Remittance Advice/Explanation of Benefits. * Note: This only applies to the states of TN, PA, DC, DE, OH, KS, MS, WA, IA, NJ, NY, WI, NM, and HI. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Community Plan Provider Disclosure of Ownership Form Now Online UnitedHealthcare Community Plan is excited to roll out a new online form for providers (physician, facility and health care professionals) participating in UnitedHealthcare Community Medicaid plans. Providers can now complete the Disclosure of Ownership form securely online through a partnership with EchoSign. The Disclosure of Ownership form is a federal regulation requirement applicable to all providers that contract with a State Medicaid agency. The launch of the new online form allows providers easy access to an electronic version of the requirement disclosure elements, needed to meet federal regulation. The process is secure and complies with all federally requirement mandates to house personal information. EchoSign uses a Knowledge Based Authentication (KBA) protection that allows a more advanced security around who is completing and signing the Disclosure of Ownership form. The KBA is a method that is used by financial institutions all over the world to ensure your personal information is transmitted securely. 55 Network Bulletin: January 2014 - Volume 59 Once the Disclosure of Ownership form has been successfully submitted you will receive an automated message of confirmation. This form can be used in all UnitedHealthcare Community Plan markets. To complete the Disclosure of Ownership Form securely online, please visit UHCCommunityPlan.com and go to Health Care Professionals to select your state. The Disclosure of Ownership link is posted under Provider Forms at each state health plan site. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Community Plan Changes to the UnitedHealthcare Community Plan of Pennsylvania Claims Payer ID and Electronic Remittance Advice Payer ID Enhancements to the enrollment and claims system for UnitedHealthcare Community Plan of Pennsylvania will become operational on or after March 1, 2014. Your claims payer ID will change to 87726 and your electronic remittance advice payer ID will change to 04567. Readmission Policy Frequently Asked Questions To learn more about UnitedHealthcare Community Plan’s Readmission Review policies, please go to UnitedHealthcare Community Plan Readmission Review Frequently Asked Questions * * This only applies to the states of: TN, PA, DC, DE, NE, OH, WA, KS, MS, IA, NJ, NY, WI, HI, and NM. 56 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Doing Business Better Important Change: Arriva Medical Has Acquired Diabetes Care Club Diabetes Care Club, a national diabetic supply provider, has been acquired by Arriva Medical. Arriva Medical is now a nationally contracted provider for all lines of business. Arriva Medical provides diabetic test strips, lancets, testing monitors and supplies via mail order. Nationally Contracted Diabetic Testing Supplies Providers Are: 57 Network Bulletin: January 2014 - Volume 59 Arriva Medicalwww.arrivamedical.com 800-580-1871 Byram www.byramhealthcare.com 877-902-9726 Edgepark www.edgepark.com 800-321-0591 Liberty www.libertymedical.com 800-695-2500 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Doing Business Better Medline Industries Joins Network Medline Industries has joined our network of medical supply providers effective Nov. 1, 2013 for all lines of business. Medline provides incontinence products such as diapers and urologicals, and wound care supplies such as gauze, tapes, and bandages to our members. Nationally Contracted Medical Supply Providers Are: 58 Byram www.byramhealthcare.com 877-902-9726 Edgepark www.edgepark.com 800-321-0591 Gordian www.amtwoundcare.com800-568-5514 (Nursing home only) Medline www.medline.com800-MEDLINE (800-633-5463) Omnicare www.omnicare.com800-990-6664 (Nursing home only) Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Doing Business Better UnitedHealthcare Preventive Plan Design UnitedHealthcare has developed a limited plan design product called UnitedHealthcare Preventive. UnitedHealthcare Preventive will be indicated on the front of these members’ health care identification cards below where the patient’s employer/payer is located. This limited plan design provides coverage for preventive care which includes all Patient Protection and Accountable Care Act (PPACA)-mandated coverage, including women’s preventive health care. Other services covered include: • One physical checkup every year • One OB/GYN checkup every year (Pap smear) • One screening test for breast cancer every year • Birth control pills or other forms of birth control • Shots for measles or other childhood diseases • One colonoscopy every five years (colorectal cancer screening test) • Other preventive tests required by the Affordable Care Act • Over-the-counter medications prescribed by physicians mandated by ACA including: Aspirin, Fluoride and Vitamin D supplements UnitedHealthcare Preventive uses the UnitedHealthcare Options PPO network and services received outside of the network are not covered. 59 Network Bulletin: January 2014 - Volume 59 Costs for additional services, such as X-rays, blood tests, emergency department visits or other services to treat medical conditions, are not covered. Some employers may choose to buy-up an additional option and provide two sick office visits and one routine vision exam. • The sick office visits can either be at a specialist or general practitioners office but the vision exam must occur at a UnitedHealthcare vision provider location (Spectera). • The coverage for sick office visits includes the charge for the office visit. Related services such as diagnostic labs, x-rays, etc. are not covered. To determine if your patient has preventive care with sick office visit benefits, contact Customer Care at 877-842-3210 or go to UnitedHealthcareOnline.com and have the member’s information available to verify eligibility. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Doing Business Better Introducing COB Smart™: Receive Payments Accurately, Predictably and Reliably Last fall, UnitedHealthcare, in collaboration with other payers and the Council for Affordable Healthcare (CAQH), a nonprofit alliance of health plans and trade associations, introduced COB Smart. COB Smart helps improve the accuracy of Coordination of Benefits (COB) processes for providers and members. How Does COB Smart Work? COB Smart can assist providers in getting needed insurance information without the administrative hassle. UnitedHealthcare directly contributes to a registry of coverage information that can help providers and health plans correctly identify which members have benefits that should be coordinated in order for corresponding claims to be processed correctly the first time. Each week, UnitedHealthcare supplies coverage information to the registry, where it is compared with information 60 Network Bulletin: January 2014 - Volume 59 from other participating payers to identify individuals with more than one form of coverage. Standard primacy rules are then applied to determine the correct order of benefits. COB Smart can be integrated with most existing health information tools and processes, such as Electronic Health Records, to confirm a patient’s eligibility, allowing providers to access complete coordination of benefits information, helping increase payment accuracy and timeliness while reducing paperwork and improving cash flow. To learn more about COB Smart from CAQH, click here. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Doing Business Better UnitedHealthcare’s Position on “Never Events” In an ongoing effort to enhance the quality of care for its members, UnitedHealthcare continues to adopt the Never Event position of the Leapfrog Group. We ask physicians and other health care professionals to join us in the effort to eliminate preventable medical errors. The Leapfrog Group’s Never Events position is based on the National Quality Forum’s list of serious reportable events. This list looks at medical errors that should never happen to a patient. The Leapfrog Group’s position in the case of a Never Event occurrence is for hospitals to: 61 • Apologize to the patient and family • Report the event to at least one reporting program such as the Joint Commission on Accreditation of Healthcare Organizations, a state reporting program or a patient safety organization • Perform root cause analysis • Waive all costs directly related to the event and refrain from seeking reimbursement from the patient or a third-party payer Network Bulletin: January 2014 - Volume 59 In the instance a Never Event has not been reported, we will attempt to determine if any claims filed with us meet the criteria, as outlined by the NQF and adopted by CMS and The Leapfrog Group, as a Serious Reportable Adverse Event. To the extent that a provider does not comply with these requirements, that provider’s claim will be denied and will be a provider’s liability. The provider may not bill the member for these charges. For more information, tools, articles and resources on patient safety and the Leapfrog Group, visit UnitedHealthcareOnline.com > Clinician Resources > Patient Safety Resources. For coding guidance, also visit UnitedHealthcareOnline.com > Tools & Resources > Policies, Protocols and Guides > Reimbursement Policies - Commercial > Wrong Surgical or Other Invasive Procedures Policy. If you have questions about UnitedHealthcare’s Patient Safety Program, contact Rebecca Lankford at Rebecca_Lankford@uhc.com. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Doing Business Better Navigate Products and Related Administrative Processes UnitedHealthcare Navigate is a gated product that meets member needs around access and cost with an emphasis on primary care and referrals to network specialists. Navigate enrollment continues to grow as more UnitedHealthcare members are seeking lower cost options. ® As the Navigate product continues to expand, we will continuetosharestate/market-specificinformation and requirements. For more information about Navigate, please go to UnitedHealthcareOnline.com > Tools & Resources > Products & Services > UnitedHealthcare Navigate. 62 Network Bulletin: January 2014 - Volume 59 Here is a Checklist of Reminders When Seeing UnitedHealthcare Navigate Members: • Check the member’s ID card to identify their specific benefit product. • Verify the member’s benefits and eligibility on UnitedHealthcareOnline.com. • Check for prior notification/authorization requirements on UnitedHealthcareOnline.com (e.g. radiology, cardiology). • When making referrals, please ensure you’re referring to participating network specialists. Refer to the Referral Requirements Quick Reference Guide for more information on what requires a referral. • Submit referrals using our secure physician website by logging in at UnitedHealthcareOnline.com > Notifications/Prior Authorizations > Referral Submission prior to the specialist service being received. Referrals cannot be accepted by phone, fax or paper. • Submit claims to the address on the back of the member ID card. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Doing Business Better Training Sessions for Electronic Solutions Physician and Provider Demographic Changes To ensure that we have the most current information for our participating physicians and health care providers, please update your practice information at UnitedHealthcareOnline.com > Contact us. Or call 877-842-3210. For any tax ID updates, please use the Provider Demographic Change Form and include a W-9. If you have questions, please call your local UnitedHealthcare Physician Advocate. We offer instructor-led webcast training sessions that can help automate and streamline administrative processes. Session topics include: • UnitedHealthcareOnline.com • UnitedHealthcareOnline.com Password Owner • UnitedHealthcareOnline.com Notification/Prior Authorization Function Overview • Electronic Payments and Statements • Electronic Data Interchange 101 • OxfordHealth.com Overview • Post-n-Track® Demonstration • PNC Remittance Advantage for Electronic Oxford Payments and EOBs Click to learn more about UnitedHealthcare and Oxford sessions and how to register. 63 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Doing Business Better Wellness Programs: Recommending Alternative Actions One of the requirements of PPACA relates to wellness programs. PPACA regulations build on existing wellness program policies to help promote good health through wellness rewards. The new regulations, which affect group health plans for plan years beginning on or after Jan. 1, 2014, increase the maximum reward allowed under certain wellness programs and provide other clarifications regarding reasonable design of health-contingent wellness programs and the reasonable alternatives that must be offered to avoid prohibited discrimination. 64 Network Bulletin: January 2014 - Volume 59 Wellness programs should be reasonably designed to promote health or prevent disease. In the rare case when a health-contingent wellness program’s reasonable alternative is not medically appropriate for one of your patients, the regulations allow you to recommend an alternative action. To learn more, please click here. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Doing Business Better Checking Status of Claim Reconsideration Requests With Attachments 65 Electronic Inpatient Admission Notifications Now you can check the status of your requests submitted via Optum Cloud Dashboard without making a phone call. Please use the Electronic Data Interchange 278N to submit notifications from your practice management system for UnitedHealthcare, UnitedHealthcare Medicare Solutions and UnitedHealthcare Community Plan. For more information, go to Admission Notification (278N), contact your clearinghouse/vendor or UnitedHealthcare at 888-804-0663 or 278n@uhc.com. Simply log into Optum Cloud Dashboard to view information about your existing claim reconsideration requests with attachments. Statuses include In-Progress, Closed (completed) and Rejected. You can read reviewer comments and update your request if needed. Reconsideration requests are reviewed within 30 days. Network Bulletin: January 2014 - Volume 59 Please refer to the Claim Reconsideration with Attachment Quick Reference Guide for instructions. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Doing Business Better Coverage Determination and Utilization Management Decisions Our health care coverage decisions are based on applicable federal and state regulations, the patient’s specific benefit plan design and applicable clinical policies and/or guidelines. Other resources used during the coverage decision process include: • Federal and state requirements as applicable to commercial, Medicare and Medicaid members. • For commercial plan members we use the applicable definitions in the member-specific document to determine coverage. • For Medicare members, we use the CMS definition of “reasonable and necessary” within Medicare coverage rules and regulations. Please note that UnitedHealthcare does not offer incentives to physicians to encourage under-utilization of care or services, or to encourage barriers to care and service. The coverage determination process is focused on ensuring that UnitedHealthcare members receive the most appropriate care based on applicable law, evidence-based medicine and their benefit plan design. 66 Network Bulletin: January 2014 - Volume 59 All Savers Alternative Funding Product New Portal The All Savers Alternate Funding plan is an innovative product designed specifically for small businesses. All Savers plans give members access to the UnitedHealthcare Choice Plus network, which today includes nearly 705,000 health care professionals and 56,000 hospitals across the nation. Health care professions and hospitals can obtain eligibility, claim payment, EOB and additional information at www.myallsaversprovider.com For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Doing Business Better UnitedHealth Premium® Results Available to Public Soon Notifications of new UnitedHealth Premium designations for quality and cost efficiency were sent by mail to physicians in November 2013. The physicians’ letters included instructions on how to access their full suite of UnitedHealth Premium assessment reports online at UnitedHealthcareOnline.com. Physicians may also submit reconsideration requests online through this site. Most physician designations will be published to our online websites such as myuhc.com on Jan. 8, 2014. The publication date for physicians in Connecticut, Delaware, New Jersey, New York, Pennsylvania and Rhode Island will be on April 2, 2014. Further Information: Go to UnitedHealthcareOnline.com and select “UnitedHealth Premium” on the top navigation bar to find resources and tools that explain the program. Send us an email though the Contact Premium Program link or call 866-270-5588. The public designation display date allowed time for physicians to submit reconsiderations before the results were available to the public. Of course, as is our practice, physicians may submit a reconsideration request at any time during the review cycle. All requests will be reviewed expeditiously. 67 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Doing Business Better BMI Documentation in the Medical Record Supporting members in their efforts to maintain a healthy body weight is crucial to our commitment to “helping people live healthier lives.” The National Institutes of Health and the World Health Organization have adopted the measurement of a body mass index (BMI) of 30 or above as a method for identifying obesity in adults. BMI measurement is also a HEDIS measure that the National Committee for Quality Assurance is using in 2014 to evaluate health plan quality. Patients with a high BMI have a higher risk for chronic health problems, which includes high blood pressure, type 2 diabetes, coronary heart disease, stroke, gallbladder disease, osteoarthritis, respiratory problems and endometrial, breast, prostate and colon cancer. Conditions caused or exacerbated by obesity are the second leading cause of preventable death in our country. 68 Network Bulletin: January 2014 - Volume 59 It is important to note that BMI measurement is calculated differently for children than it is for adults. BMI calculations for adults are based strictly on the patient’s height and weight information. BMI calculations for children also include gender, age and use of growth charts. The Centers for Disease Control and Prevention have BMI graphs and charts available for both adults and children at www.cdc.gov. Your EMR programs may already have BMI calculations available, making documentation easy in the medical record. Make sure your electronic medical record (EMR) BMI calculation program is turned on. Further detail and information on how to incorporate BMI documentation into your medical records can be found at www.cdc.gov. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Pharmacy Medicare Change to Physician-initiated Prescriptions at Mail Pharmacies Starting in 2014, mail order pharmacies are required to get your patient’s confirmation and approval for any prescription orders that you send directly to the mail pharmacy. Any new prescription or renewal that you send to a mail order pharmacy will require your patient to confirm their order with the pharmacy. This includes both new and refill medications that you fax, phone or e-prescribe for your patients and send to a mail order pharmacy. Beginning Jan. 1, 2014, OptumRx and all other mail order pharmacies will contact your patients for any prescription you send to the mail order pharmacy. 69 Network Bulletin: January 2014 - Volume 59 UnitedHealthcare has informed your patients who are currently using mail order by providing a note in all existing prescriptions since October 1, 2013. Any help you can provide your patients by mentioning this change when you are discussing prescriptions you will send to a mail order pharmacy will help to ensure that there are no delays in any therapies you are prescribing. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Pharmacy Effective Feb. 1, 2014: New Prior Authorization Requirements for Enzyme Replacement Medications (for UnitedHealthcare Integrated Commercial Fully Insured and Self-funded Plans Only) Effective Feb. 1, 2014, 70 UnitedHealthcare will require all participating network providers billing under the medical benefit to obtain prior authorization before administering enzyme replacement medications, Cerezyme® and Elelyso®, to treat Gaucher disease for UnitedHealthcare commercial plan members. This requirement will affect both new and existing members. Please review the FAQ for information on the medical necessity review and how to request prior authorization for your patient. Request for coverage of Cerezyme and Elelyso may be subject to medical necessity review. As a result, you may be required to switch patients to VPRIV®, a lower-cost clinically similar medication, in order to continue benefit coverage. Prior authorization will not be required for VPRIV. ThisprotocolappliesonlytoUnitedHealthcaremembersincommercialbenefit plans insured or administered by UnitedHealthcare, Mid-Atlantic Medical Services, Neighborhood Health Partnership, Oxford and River Valley. This protocol does not apply to the State of New York Empire Plan, UnitedHealthcare West or UnitedHealthcare Community Plan. Network Bulletin: January 2014 - Volume 59 If you have questions, please contact your local network manager or call the provider services phone number on the back of the member’s health care ID card. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Pharmacy New OptumRx Specialty Pharmacy Resource Guide To give your patients the best experience and help make their transition to our specialty pharmacy as easy as possible, we encourage you to use our new OptumRx Specialty Pharmacy Resource Guide for access to: 71 • Direct phone numbers • How to submit prior authorizations – including online (the easiest and fastest way) • How to get your patient(s) set-up with the Specialty Pharmacy Program • Information on what we offer to your patients Network Bulletin: January 2014 - Volume 59 To download and print the Resource Guide, go to UnitedHealthcareOnline.com > Tools and Resources > Pharmacy Resources > Specialty Pharmacy Program. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Pharmacy Reminder: 25 Specialty Medications Added to Coupon Policy for Jan. 1, 2014 Effective Jan. 1, 2014, UnitedHealthcare will add 25 new specialty medications to our coupon policy. Our coupon policy limits pharmacies participating in UnitedHealthcare’ s Designated Specialty Pharmacy Program from facilitating redemption of manufacturersponsored coupons or cards as payment of the member’s cost share in the following instances: • For Tiers 3 or 4 (highest member cost) medications listed in this comprehensive drug list. • For any new specialty medications released to the market in a therapeutic class currently on the list. Coupons can encourage use of higher-cost medications, despite availability of lower-cost, clinically similar options, resulting in significant cost to members and employer groups. This policy change is meant to reinforce our Prescription Drug List (PDL) design, which encourages use of lower tier, lower-cost options. Our effort follows the U.S. government’s long-time practice of not allowing coupons to be redeemed for patients covered by Medicare, Medicaid and other federal health care programs. Physicians can help minimize the impact to patients by: 1. Prescribing Tiers 1 or 2 options first: For a comprehensive drug list with alternatives included, visit UnitedHealthcareOnline.com >Tools & Resources > Pharmacy Resources. 2. Working with pharmacies: Pharmacists from our Designated Specialty Pharmacies may contact your office on behalf of a member interested in switching to a lower cost option. They will review with you the lower cost options available to your patient. If you agree to change the patient’s prescription to a Tier 2 medication, please authorize this change by speaking to a pharmacist directly or by faxing a new prescription or e-prescribing to the specialty pharmacy. If you have questions about the policy for these specialty medications, please call the provider services phone number on your patient’s health plan ID card. This protocol applies only to UnitedHealthcare members in commercial benefit plans insured or administered by UnitedHealthcare. It also applies to Neighborhood Health Partnership, Oxford, River Valley, and Sierra. This protocol does not apply to the State of New York Empire Plan, Mid-Atlantic Medical Services, UnitedHealthcare West or UnitedHealthcare Community Plan. 72 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Pharmacy UnitedHealthcare Consolidated Pharmacy Benefit Program UnitedHealthcare is consolidating and managing its pharmacy benefit programs internally through OptumRx and in 2013 all services for our commercial members currently handled by Medco were transferred to OptumRx. The final transition, including members from UnitedHealthcare Employer & Individual, UnitedHealth One, Golden Rule, and All Savers, will occur on Jan. 1, 2014. You and Your Patients Bringing all our pharmacy services in-house will enhance our ability to partner with you and your patients to improve health outcomes and better manage total health care costs. Most existing mail service prescriptions will transfer to OptumRx. Prescriptions for certain medications, like painkillers, and expired prescriptions will not transfer, and your patient will receive a letter from UnitedHealthcare instructing them to contact your office for a new prescription. It is important to note that prescription drug lists, benefit plan designs, specialty pharmacy and clinical programs will continue to be managed within UnitedHealthcare. Members will continue to have access to more than 64,000 retail network pharmacies. These essential elements will not require any action on your part or that of your patients. We will simply transition information to OptumRx. Once your patients transition to OptumRx, you’ll find that the online prior authorization tool (available through UnitedHealthCareOnline.com) is easy to use. The majority of online prior authorizations are approved in real time, and an auto-population feature provides 95 percent of a member’s information. (The OptumRx Prior Authorization team is also available by phone at 800-711-4555.) Continued > 73 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Pharmacy UnitedHealthcare Consolidated Pharmacy Benefit Program < Continued In addition to members of UnitedHealthcare Employer & Individual, this change applies to prior authorizations for Oxford, Medica, Harvard Pilgrim, River Valley and Neighborhood Health Plan (Online Prior Authorization tool available through OptumRx.com). For members of the Health Plan of Nevada and Sierra Health & Life, please continue to use the current prior authorization process. If you E-prescribe through Sure Scripts, the NCPDP ID for OptumRx is #0556540. Timing Considerations To ensure that members experience seamless service and access to the covered full range of pharmacy benefits, the transition occurred on a staged basis throughout 2013 (see chart). The final groups of members will transition on January 1, 2014. We’ve provided the adjacent schedule (see chart, subject to change), but you may also want to ask patients to present their new ID card, which will contain the updated information. 74 Network Bulletin: January 2014 - Volume 59 Date Region Plans Jan. 1, 2013 UnitedHealthcare Employees and select clients UnitedHealthcare commercial, Harvard Pilgrim. Apr. 1, 2013 West region and Northeast region UnitedHealthcare commercial, Medica, Harvard Pilgrim. June 1, 2013 Central region UnitedHealthcare commercial, Medica, Harvard Pilgrim. July 1, 2013 National Account clients across all regions UnitedHealthcare commercial, Medica, Harvard Pilgrim. Sept. 1, 2013 Southeast region UnitedHealthcare commercial, Medica, Harvard Pilgrim. Oct. 1, 2013 All regions Oxford, Sierra, River Valley, Neighborhood Health Plan. Jan 1, 2014 All regions UnitedHealthcare commercial, UnitedHealth One, Golden Rule, All Savers. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Claims, Billing & Coding Accurate Billing Improves Office Efficiency and Dual SNP Member Satisfaction Inaccurate billing can lead to member dissatisfaction, confusion and frustration. Billing errors also generate workflow inefficiencies that lead to unnecessary administrative costs for providers. To help prevent billing errors, please ask members in the Dual Special Needs Plan (D-SNP) residing in AZ, MI, NJ, NY, PA, TN and WI to show their state Medicaid card and UnitedHealthcare Community Plan ID card at every visit. Verification of dual coverage when services are rendered expedites claim payments and reduces patient calls to your office. D-SNP members will also receive education about the benefits of presenting both cards at each office visit. 75 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Claims, Billing & Coding Accessing Explanations of Benefits Online You can reduce the time you spend requesting copies of Explanations of Benefits (EOBs) by using our websites rather than calling. Please see the following table for information about obtaining UnitedHealthcare and Oxford EOBs online: Plan Option 1 Option 2 UnitedHealthcare Commercial, Medicare Solutions and UnitedHealthcare Community Plan in some states. Single EOB Search With additional enrollment in Electronic Payments & Statements (EPS) you can: • Register or log on to UnitedHealthcareOnline.com • Select Claims & Payments > Electronic Payments and Statements (EPS) > Single EOB Search • You may locate EOBs by payment number or status and date. • Search for EOBs using additional options • View, save or print EOBs and consolidated payment summaries • Receive payments by direct deposit Learn more on our website or call 866-842-3278, option 5, for more information. A Quick Reference guide is available. Oxford Commercial Claim Status • Register or log on to OxfordHealth.com • Select Claims in the Check column on the Transaction tab • You may locate claims and EOBs using several search options. Provider and Facility Quick Reference guides are available. 76 Network Bulletin: January 2014 - Volume 59 With additional enrollment in PNC Remittance Advantage you can: • Search for EOBs using additional options • View, save or print EOBs • Receive payments by direct deposit Learn more on our website or call 877-597-5489, option 1, for more information or to request a demonstration. For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Claims, Billing & Coding Coding Update to Facility OPG Mapping – Effective Jan. 1, 2014 Effective Jan. 1, 2014, A list of the new and deleted codes is below: the following code updates were made to the current UnitedHealthcare 2013 Outpatient Procedure Grouper (OPG) mapping: NEW CODES ADDED TO OPG Description 1/1/2014 OPG Group • 77 codes that are new for Jan. 1, 2014 were added to the applicable 0-10 grouper levels. 0335T Extraosseous joint stblztion 3 0336T Lap ablat uterine fibroids 7 • 40 codes that expired effective Dec. 31, 2013 were removed from the mapping. 0338T Trnscth renal symp denrv unl 4 0339T Trnscth renal symp denrv bil 4 0340T Ablate pulm tumors + extnsn 6 0342T Thxp apheresis w/hdl delip 5 10030 Guide cathet fluid drainage 0 19081 Bx breast 1st lesion strtctc 2 19082 Bx breast add lesion strtctc 0 19083 Bx breast 1st lesion us imag 2 19084 Bx breast add lesion us imag 0 19085 Bx breast 1st lesion mr imag 2 There are no other grouper level assignment changes to existing codes. Please remember that for reimbursement under OPG, UnitedHealthcare requires the appropriate line level CPT/Healthcare Common Procedure Coding System (HCPCS) code in addition to the revenue code when billing for outpatient procedures. Continued > 77 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Claims, Billing & Coding Coding Update to Facility OPG Mapping – Effective Jan. 1, 2014 < Continued Description 1/1/2014 OPG Group Description 1/1/2014 OPG Group 19086 Bx breast add lesion mr imag 0 37238 Open/perq place stent same 7 19281 Perq device breast 1st imag 0 37239 Open/perq place stent ea add 6 19282 Perq device breast ea imag 0 37241 Vasc embolize/occlude venous 7 19283 Perq dev breast 1st strtctc 0 37242 Vasc embolize/occlude artery 7 19284 Perq dev breast add strtctc 0 37243 Vasc embolize/occlude organ 7 19285 Perq dev breast 1st us imag 0 37244 Vasc embolize/occlude bleed 7 19286 Perq dev breast add us imag 0 43191 Esophagoscopy rigid trnso dx 1 19287 Perq dev breast 1st mr guide 0 43192 Esophagoscp rig trnso inject 2 19288 Perq dev breast add mr guide 0 43193 Esophagoscp rig trnso biopsy 2 23333 Remove shoulder fb deep 1 43194 Esophagoscp rig trnso rem fb 2 23334 Shoulder prosthesis removal 3 43195 Esophagoscopy rigid balloon 2 37236 Open/perq place stent 1st 7 43196 Esophagoscp guide wire dilat 2 37237 Open/perq place stent ea add 6 43197 Esophagoscopy flex dx brush 1 Continued > 78 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Claims, Billing & Coding Coding Update to Facility OPG Mapping – Effective Jan. 1, 2014 < Continued Description 1/1/2014 OPG Group Description 1/1/2014 OPG Group 43198 Esophagosc flex trnsn biopy 1 43276 Ercp stent exchange w/dilate 3 43211 Esophagoscop mucosal resect 1 43277 Ercp ea duct/ampulla dilate 3 43212 Esophagoscop stent placement 4 43278 Ercp lesion ablate w/dilate 3 43213 Esophagoscopy retro balloon 2 49405 Image cath fluid colxn visc 2 43214 Esophagosc dilate balloon 30 2 49406 Image cath fluid peri/retro 2 43229 Esophagoscopy lesion ablate 3 49407 Image cath fluid trns/vgnl 2 43233 Egd balloon dil esoph30 mm/> 2 52356 Cysto/uretero w/lithotripsy 5 43253 Egd us transmural injxn/mark 2 64616 Chemodenerv musc neck dyston 0 43254 Egd endo mucosal resection 1 64617 Chemodener muscle larynx emg 1 43266 Egd endoscopic stent place 4 64642 Chemodenerv 1 extremity 1-4 1 43270 Egd lesion ablation 2 64643 Chemodenerv 1 extrem 1-4 ea 0 43274 Ercp duct stent placement 3 64644 Chemodenerv 1 extrem 5/> mus 1 43275 Ercp remove forgn body duct 3 64645 Chemodenerv 1 extrem 5/> ea 0 Continued > 79 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Claims, Billing & Coding Coding Update to Facility OPG Mapping – Effective Jan. 1, 2014 < Continued CODES DELETED FROM THE OPG Description 1/1/2014 OPG Group Code Description 64646 Chemodenerv trunk musc 1-5 1 0124T CONJUNCTIVAL DRUG PLACEMENT 64647 Chemodenerv trunk musc 6/> 1 0186T SUPRACHOROIDAL DRUG DELIVERY 66183 Insert ant drainage device 5 0192T INSERT ANT SEGMENT DRAIN EXT 93582 Perq transcath closure pda 8 13150 REPAIR OF WOUND OR LESION C5271 Low cost skin substitute app 1 19102 BX BREAST PERCUT W/IMAGE C5272 Low cost skin substitute app 0 19103 BX BREAST PERCUT W/DEVICE C5273 Low cost skin substitute app 3 19290 PLACE NEEDLE WIRE BREAST C5274 Low cost skin substitute app 0 19291 PLACE NEEDLE WIRE BREAST C5275 Low cost skin substitute app 1 19295 PLACE BREAST CLIP PERCUT C5276 Low cost skin substitute app 0 23331 REMOVE SHOULDER FOREIGN BODY C5277 Low cost skin substitute app 1 32201 DRAIN PERCUT LUNG LESION C5278 Low cost skin substitute app 0 37204 TRANSCATHETER OCCLUSION C9737 Lap esoph augmentation 7 37205 TRANSCATH IV STENT PERCUT Continued > 80 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Claims, Billing & Coding Coding Update to Facility OPG Mapping – Effective Jan. 1, 2014 < Continued 81 Code Description Code Description 37206 TRANSCATH IV STENT/PERC ADDL 43272 ENDO CHOLANGIOPANCREATOGRAPH 37207 TRANSCATH IV STENT OPEN 43456 DILATE ESOPHAGUS 37208 TRANSCATH IV STENT/OPEN ADDL 43458 DILATE ESOPHAGUS 37210 EMBOLIZATION UTERINE FIBROID 44901 DRAIN APP ABSCESS PERCUT 42802 BIOPSY OF THROAT 47011 PERCUT DRAIN LIVER LESION 43219 ESOPHAGUS ENDOSCOPY 48511 DRAIN PANCREATIC PSEUDOCYST 43228 ESOPH ENDOSCOPY ABLATION 49021 DRAIN ABDOMINAL ABSCESS 43256 UPPR GI ENDOSCOPY W/STENT 49041 DRAIN PERCUT ABDOM ABSCESS 43258 OPERATIVE UPPER GI ENDOSCOPY 49061 DRAIN PERCUT RETROPER ABSC 43267 ENDO CHOLANGIOPANCREATOGRAPH 50021 RENAL ABSCESS PERCUT DRAIN 43268 ENDO CHOLANGIOPANCREATOGRAPH 58823 DRAIN PELVIC ABSCESS PERCUT 43269 ENDO CHOLANGIOPANCREATOGRAPH 64613 DESTROY NERVE NECK MUSCLE 43271 ENDO CHOLANGIOPANCREATOGRAPH 64614 DESTROY NERVE EXTREM MUSC C9736 LAP SURG RF ABLAT UT FIBROIDS IO GD MON WHEN PER Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare Affiliates Oxford® Medical and Administrative Policy Updates For complete details on the new and/or revised policies listed in the table on the following page, refer to the monthly Policy Update Bulletin at OxfordHealth.com > Providers > Tools & Resources > Practical Resources > Medical and Administrative Policies > Policy Update Bulletin. Continued > 82 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > Oxford® Medical and Administrative Policy Updates < Continued Policy Title Policy Type Effective Date Policy Update Bulletin All Jan. 1, 2014 Jan. 2014 Brilinta (Ticagrelor) Clinical Policy Jan. 1, 2014 Dec. 2013 CystaranTM (Cysteamine) Ophthalmic Solution Clinical Policy Jan. 1, 2014 Dec. 2013 Enzyme Replacement Therapy for Gaucher Disease Clinical Policy Feb. 1, 2014 Nov. 2013 Dec. 2013 Jan. 2014 GilotrifTM (Afatinib) Clinical Policy Jan. 1, 2014 Dec. 2013 Lotronex (Alosteron) Clinical Policy Jan. 1, 2014 Dec. 2013 Mechanical Circulatory Support Device (MCSD) Administrative Policy Jan. 1, 2014 Nov. 2013 Dec. 2013 Mekinist (Trametinib) Clinical Policy Jan. 1, 2014 Dec. 2013 TAKE NOTE UPDATED/REVISED Annual CPT® and HCPCS Code Updates NEW Continued > 83 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > < Continued Policy Title Policy Type Effective Date Policy Update Bulletin Pulmozyme® (Dornase Alfa Clinical Policy Jan. 1, 2014 Dec. 2013 StribildTM (Elvitegravir/ Cobicistat/Emtricitabine/Tenofovir Disoproxil Fumarate) Clinical Policy Dec. 1, 2013 Nov. 2013 Tafinlar (Dabrafenib) Clinical Policy Jan. 1, 2014 Dec. 2013 TobiTM Nebulizer Solution (Tobramycin Inhalation Solution) and Tobi® Podhaler™ (Tobramycin Inhalation Powder) Clinical Policy Jan. 1, 2014 Dec. 2013 Agents for Migraine-Triptans Clinical Policy Jan. 1, 2014 Dec. 2013 Anticonvulsants - Depakote ER®, Keppra®, Keppra XR®, Lamictal®, Lamictal XR®, Generic Levetiracetam XR, Lamictal ODT®, Lamotrigine Extended-Release, Oxtellar XR™, Topamax®, Stavzor®, Banzel®, Potiga™, Vimpat® , Trokendi XR and Lamotrigine Oral Disintegrating Tablets Clinical Policy Jan. 1, 2014 Dec. 2013 Apheresis Clinical Policy Jan. 1, 2014 Dec. 2013 Autism Clinical Policy Dec. 1, 2013 Nov. 2013 Autologous Chondrocyte Transplantation in the Knee Clinical Policy Dec. 1, 2013 Nov. 2013 Bariatric Surgery Clinical Policy Jan. 1, 2014 Dec. 2013 Bosulif® (Bosutinib) Clinical Policy Jan. 1, 2014 Dec. 2013 NEW UPDATED/REVISED UnitedHealthcare Affiliates Oxford Medical and Administrative Policy Updates UPDATED/REVISED Continued > 84 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > < Continued Policy Title Policy Type Effective Date Policy Update Bulletin Breast Reconstruction Post Mastectomy Clinical Policy Dec. 1, 2013 Nov. 2013 Breast Repair/Reconstruction (Not Following a Mastectomy) Clinical Policy Dec. 1, 2013 Nov. 2013 Cardiovascular Disease Risk Tests Clinical Policy Jan. 1, 2014 Dec. 2013 Clinical Trials Clinical Policy Jan. 1, 2014 Dec. 2013 Compounds and Bulk Powders Clinical Policy Jan. 1, 2014 Dec. 2013 Connecticut Clinical Trials Clinical Policy Jan. 1, 2014 Dec. 2013 Core Decompression for Avascular Necrosis Clinical Policy Jan. 1, 2014 Dec. 2013 Daliresp® (Roflumilast) Clinical Policy Jan. 1, 2014 Dec. 2013 Discogenic Pain, Treatment Clinical Policy Jan. 1, 2014 Dec. 2013 DPP4 Inhibitors (Janumet, Januvia, Janumet XR) Check Title Clinical Policy Jan. 1, 2014 Dec. 2013 Drug Coverage Criteria - New and Therapeutic Equivalent Medications Clinical Policy Dec. 1, 2013 Jan. 1, 2014 Nov. 2013 Dec. 2013 Drug Coverage Guidelines Clinical Policy Jan. 1, 2014 Dec. 2013 Durable Medical Equipment, Orthotics and Prosthetics Multiple Frequency Reimbursement Policy Dec. 1, 2013 Nov. 2013 Erivedge (Vismodegib) Clinical Policy Jan. 1, 2014 Dec. 2013 Genetic Testing for Hereditary Breast and/or Ovarian Cancer Syndrome (HBOC) Clinical Policy Dec. 1, 2013 Nov. 2013 UPDATED/REVISED UnitedHealthcare Affiliates Oxford Medical and Administrative Policy Updates Continued > 85 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > < Continued Policy Title Policy Type Effective Date Policy Update Bulletin Home Health Care Clinical Policy Feb. 1, 2014 Jan. 2014 Iclusig (Ponatinib) Clinical Policy Dec. 1, 2013 Jan. 1, 2014 Dec. 2013 Immune Globulin (IVIG and SCIG) Clinical Policy Dec. 1, 2013 Nov. 2013 Dec. 2013 In-Office Laboratory Testing and Procedures List Reimbursement Policy Dec. 1, 2013 Jan. 1, 2014 Nov. 2013 Dec. 2013 Lyme Disease Clinical Policy Dec. 1, 2013 Nov. 2013 Isotretinoin Oral Products Clinical Policy Jan. 1, 2014 Dec. 2013 Kuvan (Sapropterin Dihydrochloride) Clinical Policy Jan. 1, 2014 Dec. 2013 Maximum Frequency Per Day Reimbursement Policy Dec. 1, 2013 Nov. 2013 Modafinil (Provigil) and Armodafinil (Nuvigil) Clinical Policy Jan. 1, 2014 Dec. 2013 Modifier SU Policy Reimbursement Policy Dec. 1, 2013 Nov. 2013 Multiple Sclerosis: Interferon B-1A (Avonex, Rebif), Interferon B-1B Betaseron, Extavia, Glatiramer (Copaxone), Fingolimod (Gilenya), and Teriflunomide (Aubagio) Clinical Policy Dec. 1, 2013 Nov. 2013 Multiple Sclerosis: Interferon B-1A (Avonex, Rebif), Interferon B-1B Betaseron, Extavia, Glatiramer (Copaxone), Fingolimod (Gilenya), Teriflunomide (Aubagio), and Dimethyl Fumarate (Tecfidera) Clinical Policy Jan. 1, 2014 Dec. 2013 Omnibus Codes Clinical Policy Jan. 1, 2014 Dec. 2013 UPDATED/REVISED UnitedHealthcare Affiliates Oxford Medical and Administrative Policy Updates Continued > 86 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > < Continued Policy Title Policy Type Effective Date Policy Update Bulletin Opioid Dependence Agents: Buprenorphine HCL and Naloxone (Suboxone) and Buprenorphine HCL Clinical Policy Jan. 1, 2014 Dec. 2013 Oral and Nasal Fentanyl Medications Clinical Policy Jan. 1, 2014 Dec. 2013 Oral Chemotherapy Drugs: Application of NCCN Clinical Practice Guidelines Clinical Policy Jan. 1, 2014 Dec. 2013 Osteochondral Grafting of Knee Clinical Policy Jan. 1, 2014 Dec. 2013 Oxford’s Outpatient Imaging Self-Referral Policy Clinical Policy Dec. 1, 2013 Nov. 2013 Plagiocephaly and Craniosynostosis Treatment Clinical Policy Dec. 1, 2013 Nov. 2013 Polysomnography and Portable Monitoring for Evaluation of Sleep Related Breathing Disorders Clinical Policy Jan. 1, 2014 Dec. 2013 Presacral Neurectomy and Uterine Nerve Ablation for Pelvic Pain Clinical Policy Dec. 1, 2013 Nov. 2013 Preventive Care Clinical Policy Jan. 1, 2014 Dec. 2013 Progesterone Products: Crinone (Progesterone Gel), Endometrin (Progesterone Vaginal Insert) and First Progesterone VGS (Progesterone Vaginal Suppository USP Compounding Kit) for Non-Fertility Use Clinical Policy Jan. 1, 2014 Dec. 2013 Pulmonary Arterial Hypertension (PAH) Drug Therapy Clinical Policy Jan. 1, 2014 Dec. 2013 Radiopharmaceuticals and Contrast Media Clinical Policy Dec. 1, 2013 Nov. 2013 Rectiv (Nitroglycerin Ointment) Clinical Policy Jan. 1, 2014 Dec. 2013 Routine Foot Care Clinical Policy Jan. 1, 2014 Dec. 2013 UPDATED/REVISED UnitedHealthcare Affiliates Oxford Medical and Administrative Policy Updates Continued > 87 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > < Continued Policy Title Policy Type Effective Date Policy Update Bulletin Sedative Hypnotic Agents Clinical Policy Jan. 1, 2014 Dec. 2013 Speech Therapy and Early Intervention Programs/Birth to Three Clinical Policy Dec. 1, 2013 Nov. 2013 Sprycel® (Dasatinib) Clinical Policy Jan. 1, 2014 Dec. 2013 Subcutaneous Leuprolide Acetate Clinical Policy Jan. 1, 2014 Dec. 2013 Topical Retinoids (Pharmaceutical Treatment of Acne) Clinical Policy Jan. 1, 2014 Dec. 2013 Transcatheter Heart Valve Procedures Clinical Policy Jan. 1, 2014 Dec. 2013 Unicondylar Spacer Devices for Treatment of Pain or Disability Clinical Policy Dec. 1, 2013 Nov. 2013 Vaccines Clinical Policy Jan. 1, 2014 Dec. 2013 Vagus Nerve Stimulation Clinical Policy Jan. 1, 2014 Dec. 2013 Virtual Upper Gastrointestinal Endoscopy Clinical Policy Dec. 1, 2013 Nov. 2013 Visual Information Processing Evaluation and Orthoptic and Vision Therapy Clinical Policy Dec. 1, 2013 Nov. 2013 Warming Therapy and Ultrasound Therapy for Wounds Clinical Policy Jan. 1, 2014 Dec. 2013 Xtandi® (Enzalutamide) Clinical Policy Jan. 1, 2014 Dec. 2013 UPDATED/REVISED UnitedHealthcare Affiliates Oxford Medical and Administrative Policy Updates Note: The appearance of a service or procedure on this list does not imply that Oxford provides coverage for the service or procedure. In the event of an inconsistency or conflict between the information provided in this bulletin and the posted policy, the provisions of the posted policy will prevail. Oxford HMO products are underwritten by Oxford Health Plans (NY), Inc., Oxford Health Plans (NJ), Inc. and Oxford Health Plans (CT), Inc. Oxford insurance products are underwritten by Oxford Health Insurance, Inc. 88 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > UnitedHealthcare of the River Valley Preauthorization List and Policy Updates For complete details on the new and/or revised policies and guidelines listed in the table below, refer to the monthly Policy Update Bulletin at UHCRiverValley.com > Providers > Coverage Policy Library > Policy Update Bulletin. These updates apply to UnitedHealthcare of the River Valley commercial and hawk-i plan membership only; they do not apply to members enrolled in a River Valley Ohio product or South Carolina product. Policy Title Effective Date Coverage Policy Update Bulletin Jan. 1, 2014 Jan. 2014 Enzyme Replacement Therapy for Gaucher Disease Feb. 1, 2014 Nov. 2013 Dec. 2013 Jan. 2014 Mechanical Circulatory Support Device (MCSD) Jan. 1, 2014 Nov. 2013 Dec. 2013 Abnormal Uterine Bleeding and Uterine Fibroids Jan. 1, 2014 Dec. 2013 Apheresis Jan. 1, 2014 Dec. 2013 Bariatric Surgery Jan. 1, 2014 Dec. 2013 Blepharoplasty, Blepharoptosis and Brow Ptosis Repair Jan. 1, 2014 Dec. 2013 Breast Reconstruction Post Mastectomy Dec. 1, 2013 Nov. 2013 TAKE NOTE Annual CPT® and HCPCS Code Updates NEW UPDATED/REVISED Continued > 89 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > < Continued UnitedHealthcare Affiliates UnitedHealthcare of the River Valley Prior Authorization List and Policy Updates Policy Title Effective Date Coverage Policy Update Bulletin Breast Repair/Reconstruction (Not Following Mastectomy) Dec. 1, 2013 Nov. 2013 Cardiovascular Disease Stress Tests Jan. 1, 2014 Dec. 2013 Cochlear Implants Dec. 1, 2013 Nov. 2013 Computed Tomographic Colonography Jan. 1, 2014 Nov. 2013 Dec. 2013 Core Decompression for Avascular Necrosis Dec. 1, 2013 Nov. 2013 Deep Brain Stimulation Jan. 1, 2014 Dec. 2013 Hip Resurfacing Arthroplasty Jan. 1, 2014 Dec. 2013 Hyperbaric Oxygen Therapy and Topical Oxygen Therapy Jan. 1, 2014 Dec. 2013 Immune Globulin (IVIG and SCIG) Jan. 1, 2014 Dec. 2013 Implantable Beta-Emitting Microspheres for Treatment of Malignant Tumors Jan. 1, 2014 Dec. 2013 Intensity-Modulated Radiation Therapy Jan. 1, 2014 Dec. 2013 Nerve Graft to Restore Erectile Function During Radical Prostatectomy Jan. 1, 2014 Dec. 2013 Noninvasive Prenatal Diagnosis of Fetal Aneuploidy Using Cell-Free Fetal Nucleic Acids in Maternal Blood Feb. 1, 2014 Dec. 2013 Jan. 2014 Omnibus Codes Jan. 1, 2014 Nov. 2013 Dec. 2013 Orencia® (Abatacept) Dec. 1, 2013 Nov. 2013 Polysomnography and Portable Monitoring For Evaluation of Sleep Related Breathing Disorders Dec. 1, 2013 Nov. 2013 Preventive Care Services Jan. 1, 2014 Dec. 2013 Continued > 90 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > < Continued UnitedHealthcare Affiliates UnitedHealthcare of the River Valley Prior Authorization List and Policy Updates Policy Title Effective Date Coverage Policy Update Bulletin Proton Beam Radiation Therapy Jan. 1, 2014 Dec. 2013 Repository Corticotropin Injection (HP Acthar Gel) Jan. 1, 2014 Dec. 2013 Transcatheter Heart Valve Procedures Jan. 1, 2014 Dec. 2013 Vaccines Jan. 1, 2014 Dec. 2013 Vagus Nerve Stimulation Dec. 1, 2013 Nov. 2013 Total Ankle Replacement Surgery (Arthroplasty) Jan. 1, 2014 Dec. 2013 Wireless Capsule Endoscopy Jan. 1, 2014 Dec. 2013 Xyntha - Factor VIII (Antihemophilic Factor, Recombinant) Jan. 1, 2014 Dec. 2013 RETIRED Note: The appearance of a service or procedure on this list does not imply that UnitedHealthcare provides coverage for the service or procedure. In the event of an inconsistency or conflict between the information provided in this bulletin and the posted policy, the provisions of the posted policy will prevail. 91 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > SignatureValue™ Benefit Interpretation Policy Updates For complete details on the revised policy listed below, refer to the monthly SignatureValue™ Benefit Interpretation Policy Update Bulletin at UHCWest.com > Provider Log In > Library > Resource Center > Guidelines & Interpretation Manuals. Policy Title Applicable State(s) Effective Date Policy Update Bulletin Biofeedback All Jan. 1, 2014 Dec. 2013 Clinical Trials: Routine Costs in Clinical Trials All Dec. 1, 2013 Nov. 2013 Jan. 1, 2014 Dec. 2013 UPDATED/REVISED Complementary and Alternative Medicine All Jan. 1, 2014 Dec. 2013 Detoxification: Chemical Dependency/Substance Abuse Detoxification Oregon Dec. 1, 2013 Nov. 2013 All Jan. 1, 2014 Dec. 2013 All Jan. 1, 2014 Dec. 2013 Durable Medical Equipment (DME), Prosthetics, Corrective Appliances/Orthotics (Non-Foot Orthotics) and Medical Supplies Grid Continued > 92 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > < Continued UnitedHealthcare Affiliates SignatureValue™ Benefit Interpretation Policy Updates Policy Title Applicable State(s) Effective Date Policy Update Bulletin Hearing: Hearing Screening, Hearing Examinations and Hearing Aids and Hearing Devices All Jan. 1, 2014 Dec. 2013 Hospice Care and Services California Jan. 1, 2014 Dec. 2013 Maternity and Newborn Care Oregon Jan. 1, 2014 Dec. 2013 Nutritional Therapy: Enteral and Oral Nutritional Therapy All Jan. 1, 2014 Dec. 2013 Ostomy: Ostomy Supplies All Jan. 1, 2014 Dec. 2013 Ostomy: Ostomy Supplies Grid All Jan. 1, 2014 Dec. 2013 Physician Services: Primary Care and Specialist Visits California, Oregon & Washington Jan. 1, 2014 Dec. 2013 Radiology: Diagnostic and Therapeutic Radiology Services All Jan. 1, 2014 Dec. 2013 Note: The appearance of a service or procedure on this list does not imply that coverage is provided for the service or procedure. In the event of an inconsistency or conflict between the information provided in this bulletin and the posted policy, the provisions of the posted policy will prevail. 93 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > SignatureValue™ Medical Management Guideline Updates For complete details on the new and/or revised policies listed in the table below, refer to the monthly SignatureValue™ Medical Management Guidelines Update Bulletin at UHCWest.com > Provider Log In > Library > Resource Center > Guidelines & Interpretation Manuals. Title Effective Date Update Bulletin Jan. 1, 2014 Jan. 2014 Clinical Trials Jan. 1, 2014 Nov. 2013 Dec. 2013 Hospital Readmissions: Quality of Care Guideline Dec. 1, 2014 Nov. 2013 Mechanical Circulatory Support Device (MCSD) Jan. 1, 2014 Nov. 2013 Dec. 2013 Abnormal Uterine Bleeding and Uterine Fibroids Jan. 1, 2014 Dec. 2013 Apheresis Jan. 1, 2014 Dec. 2013 Autism Spectrum Disorder Nov. 1, 2013 Nov. 2013 Bariatric Surgery Jan. 1, 2014 Dec. 2013 Cardiovascular Disease Risk Tests Jan. 1, 2014 Dec. 2013 TAKE NOTE Annual CPT® and HCPCS Code Updates NEW UPDATED/REVISED Continued > 94 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS Next Article > < Continued UnitedHealthcare Affiliates SignatureValue™ Medical Management Guideline Updates Title Effective Date Update Bulletin Hearing Aids and Devices Including Wearable, Bone-Anchored and Semi-Implantable Jan. 1, 2014 Dec. 2013 Hip Resurfacing Arthroplasty Jan. 1, 2014 Dec. 2013 Omnibus Codes Jan. 1, 2014 Dec. 2013 Polysomnography and Portable Monitoring for Evaluation of Sleep Related Breathing Disorders Dec. 1, 2013 Nov. 2013 Preventive Care Services Jan. 1, 2014 Dec. 2013 Proton Beam Radiation Therapy Jan. 1, 2014 Dec. 2013 Transcatheter Heart Valve Procedures Jan. 1, 2014 Dec. 2013 Hyperbaric Oxygen Therapy and Topical Oxygen Therapy Jan. 1, 2014 Jan. 2014 Total Ankle Replacement (Arthroplasty) Jan. 1, 2014 Jan. 2014 Wireless Capsule Endoscopy Jan. 1, 2014 Jan. 2014 RETIRED Note: The appearance of a service or procedure on this list does not imply that coverage is provided for the service or procedure. In the event of an inconsistency or conflict between the information provided in this bulletin and the posted policy, the provisions of the posted policy will prevail. 95 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com HOME TABLE OF CONTENTS UnitedHealthcareAffiliates UnitedHealthcare of the River Valley and Neighborhood Health Partnership:Disease Management Programs UnitedHealthcare of the River Valley (UnitedHealthcare River Valley) disease management programs serve members in the UnitedHealthcare River Valley and Neighborhood Health Partnership (NHP) plans. Services available for members include: • Educational materials • Periodic disease-specific newsletters • Notification of care opportunities such as missed tests, medication compliance, and emergent orinpatient admissions for an exacerbation • Case management interventions for members identified at highest risk Providers receive quarterly reports and notifications regarding care opportunities for patients. The UnitedHealthcare River Valley website at UHCrv.com provides information about the programs and disease management member and provider rights and responsibilities. Providers may contact the disease management staff to request information about the programs, refer patients for services or communicate a complaint or offer feedback. Normal business hours are from 8 a.m. to 4:30 p.m., Monday through Friday, with voicemail options after hours. To contact us, call 800-369-2704, Option 4; Fax: 866-950-7759; or send an email to MailWebCDM@UHC.com. Insurance coverage provided by UnitedHealthcare Insurance Company or its affiliates. Health plan coverage provided by UnitedHealthcare of California, UnitedHealthcare of Colorado, Inc., UnitedHealthcare of Oregon, Inc., and UnitedHealthcare of Washington, Inc. or other affiliates. Administrative services provided by United HealthCare Services, Inc. or its affiliates. 96 Network Bulletin: January 2014 - Volume 59 For more information call 877.842.3210, or visit UnitedHealthcareOnline.com