Capillary Collection You will begin practicing skin punctures
advertisement

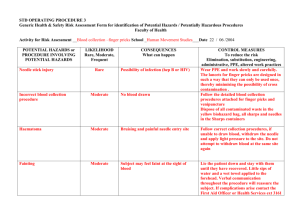
Capillary Collection Continuation of the BASIC PRINCIPLES of PHLEBOTOMY handout You will begin practicing skin punctures (capillary draws) during the Hematology Student Lab Rotation. The Capillary Competency Assessment is given at the end of Hematology Student Lab Rotation. XIV. Capillary Draws (Skin or Dermal Puncture, Microspecimen, Fingerstick, Heelstick) A. Why perform a capillary draw? (text, page 366) 1. Skin puncture is the method of choice for collecting blood from infants (neonates) and children <2 years old. 2. B. XV. In adults, skin puncture may be required because of the inability to locate a suitable vein in the antecubital area: a. burned or scarred patients b. patients receiving chemotherapy c. patients with hard, sclerosed veins d. patients with clot-forming (thrombotic) tendencies e. patients with fragile veins f. patients performing home glucose monitoring (POCT) g. patients with IV Composition of Capillary Blood 1. Mixture of arterial (from arterioles), venous (from venules), capillary blood, and fluid (interstitial, intracellular) from surrounding tissues 2. More closely resembles arterial blood than venous blood, especially if the site has been warmed (increases arterial flow into the area) 3. Reference ranges will differ between capillary and venous blood a. Glucose higher in capillary blood b. Protein, calcium, potassium are lower in capillary blood (unless specimen is hemolyzed, then potassium is falsely elevated) c. Always note on requisition if sample is capillary draw Specimen Collection: Capillary Draws A. Equipment used for capillary draws 1. PPE (gloves and gown/lab coat) 2. Cleaning agent: DO NOT use povidone iodine (bilirubin, uric acid, PO4, K+) a. 70% isopropyl alcohol prep pads b. Soap and water: used if patient allergic to routine cleaning agents 3. Cotton balls or sterile gauze pads 4. Bandage/Tape: should NOT be used on children <2 years old CLS 424 Phlebotomy: Student Lab Rotation Phlebotomy Lecture Handout 1 5. Sharps container 6. Warming device, if necessary a. Warm puncture site for neonatal heelstick and/or if site is cyanotic b. Warm wash cloth or towel, commercial heel warmer 3-5 minutes 7. Skin puncture device: generally referred to as a lancet (text, page 362) a. Always use standardized equipment that control puncture depth and are not capable of puncturing to a depth that penetrates bone. b. NEVER use a surgical blade for skin puncture c. Different devices designed to be used for adults, toddlers, neonates, preemies 8. Microspecimen Containers a. Capillary Tubes: fill by capillary action (text, page 364) 1) Used most often for hematocrit testing (microhematocrit tubes) and POCT 2) Tips of capillary tubes color-coded: red = heparin coated, blue = plain (no additive) 3) Volume: ~50-75 uL 4) After sample collection, one end of tube must be sealed with sealant/clay to prevent loss of sample when centrifuged b. B. Microcollection Tubes (text, page 363) 1) Plastic tubes called ‘microtainers’ 2) Caps are color-coded matching the color-coding system used for vacutainer equipment 3) Micro-tubes with anticoagulant MUST BE INVERTED and well mixed to prevent micro-clot formation after sample collection (a common cause for sample rejection) 4) Some tubes are supplied with a mini-capillary tube to facilitate collection of sample, which is replaced by a colorcoded top after collection is complete 5) Order of draw is critical: EDTA always drawn first, serum specimens drawn last 6) Volume: 250-500 uL Skin Puncture Procedure: CLS 424 Phlebotomy: Student Lab Rotation Phlebotomy Lecture Handout 2 1. 2. 3. Approaching the patient/bedside manner Patient identification Inquire for latex allergies and patient preparation requirements 4. Site Selection: select puncture sites that provide sufficient distance between the skin and bone to avoid accidental contact with the bone that may cause infection (osteomyelitis) (text, page 369) a. Finger puncture sites using approved finger puncturing device 1) Performed on adults and children >1 year old 2) Distal segments of third or fourth finger, fleshy area just to the side of the ball of the fingertip, away from the nail, away from the knuckle, palmar side 3) Avoid areas that appear edematous (swollen), scaly, bruised, calloused, scarred, infected 4) Do not puncture through old sites b. Heel puncture sites: (text, page 371) 5. Cleanse the puncture site. DO NOT use povidone-iodine. Failure to allow alcohol to dry will: a. Cause stinging sensation to patient b. Contaminate the specimen c. Hemolyze red cells d. Prevent formation of a rounded drop 6. Prior to puncture, the finger may be massaged several times to increase blood flow to area (this must be done before this finger is cleansed) 7. Perform the puncture (text, page 376-378) a. Hold the finger between your thumb and index finger with palmar surface facing up. b. Place the puncture device at an angle to the side of the finger tip. c. Puncture the finger using a quick, smooth motion which should be deep enough to allow free flowing blood. d. Discard the puncture device in the sharps biohazard container immediately. 8. Wipe away the first drop of blood. The first drop of blood is contaminated with tissue fluid released during the puncture which will falsely affect test results 9. Collect the sample a. Fingers are positioned slightly downward during collection to CLS 424 Phlebotomy: Student Lab Rotation Phlebotomy Lecture Handout 3 b. increase blood flow Slight pressure should be applied at a short distance from the wound and ‘gentle’ milking is suggested while collecting blood sample. Strenuous massaging, prolonged squeezing or milking may cause contamination of sample with tissue fluid, invalidating test results c. Touch the capillary tube or microtainer to the drop of blood. Sample will be drawn into the container/tube by capillary action. 1) Microtainers are held at an angle, slanting downward during collection to allow blood to run down the inside of the collection tube. 2) Capillary tubes are held horizontal to avoid collecting air bubbles d. Do NOT touch collecting device to surface of skin Do NOT scrape collecting device across surface of skin Do NOT scoop blood into collecting reservoir e. Periodically wipe the blood away from the wound to stimulate better blood flow and avoid clotted specimens f. When collection is completed immediately replace the cap and mix the microtainer by inversion a minimum of 10 times. 10. Order of draw is critical due to tendency of platelets to accumulate at the puncture (wound) site leading to ‘micro-clot’ formation (clotted specimen) Always follow SOP of your laboratory (text, page 367) a. Prepare blood smear, if needed b. EDTA c. Heparin d. Serum (red top) 11. Apply pressure to puncture site using sterile gauze; may also need to elevate finger or heel until bleeding has stopped 12. Label specimens using indelible marker pen in view of the patient XVI. Routine Fingerstick Procedure A. Remain cool, calm and collected ☺ B. Follow isolation protocol, if applicable C. Organize yourself 1. Always make sure you know what and how much you are going to draw 2. Always make sure your equipment is close at hand 3. Always have back up collection tubes if needed D. ALWAYS follow established protocol 1. Organize your equipment a. Gloves (PPE) Stick to Eleven minus 2 CLS 424 Phlebotomy: Student Lab Rotation Do Phlebotomy Not Need:Lecture Handout 1. tourniquet 2. syringe/vacutainer f. Sharps container 4 b. c. d. e. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. E. Labcoat (PPE) Alcohol wipe Cotton ball, gauze Bandage/tape g. h. i. Puncturing device (lancet) Collection tubes Indelible marker Wash hands and put on gloves Identify the patient Inquire about latex allergy and any required patient preparation (fasting?) Reassure the patient with your bedside manner ☺ Select the puncture site Cleanse the site allowing to air dry (can use sterile gauze to wipe dry) Puncture the site Dispose of sharps into sharps container Wipe away the first drop of blood Collect blood sample Apply pressure to puncture site Mix anticoagulated tubes well Label the tubes in patient’s sight Observe any special handling instructions Check patient’s wound to ensure bleeding has stopped and apply bandage Dispose of contaminated materials and non-contaminated materials Thank the patient Remove gloves and wash hands Wipe the perspiration from your forehead ☺ Accidental Needle Stick 1. Remain calm, complete the task at hand 2. Cleanse the wound immediately 3. Follow site protocol a. UNMC site students: page OUCH hotline: 1-402-888-6824 b. UNMC affiliate site students: page OUCH hotline for documentation c. Affiliated University: document your laboratory protocol here: Who do you call? _________________________________ Phone number: ___________________________________ Special instructions: _______________________________ 4. Notify your instructor/supervisor 5. Complete an incident report form CLS 424 Phlebotomy: Student Lab Rotation Phlebotomy Lecture Handout 5