differences hysterical somatoform disorders conversion disorder
advertisement

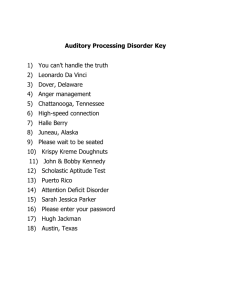
10/25/11 differences (a psychological conflict converted into a physical problem) SOMATOFORM DISORDERS Hysterical Preoccupation conversion disorder somatization disorder pain disorder hypochondriasis BDD suffer changes in physical functioning misinterpret/overreact to body symptom or features hysterical somatoform disorders conversion disorder somatization disorder pain disorder The physical ailments suggest a medical condition but there is no evidence of physical pathology. Not intentionally faking illness. In fact, distressed and goes to physician about it. Like dissociative disorders, viewed as ways to escape stress. conversion disorder DIAGNOSTIC CRITERIA • 1+ sensory or voluntary motor deficit • an associated stressor examples of deficits Visual (e.g. blindness or tunnel vision) Auditory (e.g. deafness) Tactile (e.g. selective numbness) Motor (e.g. partial paralysis, probs speaking/mutism) Other (e.g. dizziness, seizures) 1 10/25/11 conversion disorder • DEMOGRAPHICS • .005% prevalence (in past, very common in military & civilian life) • age of onset: adolescence to young adulthood • sex ratio: 2-10: 1 EXCEPTION: military combat (e.g. In WWI, it was the most frequently diagnosed disorder among soldiers) • rural residents • less educated • medically unsophisticated • low socioeconomic status (SES) conversion disorder CAUSE -rapid onset w/ trauma or stressor; -symptoms obviously function as “excuse” to escape when literal escape isn’t feasible or acceptable -symptoms resolve ~ 2 weeks after stressor removed TREATMENT • therapy for original trauma/stressor • exposure to stimuli that “produce” symptoms • do not reinforce deficits with attention/sympathy • physical exercises + pos reinforcement • SSRIs somatization disorder DIAGNOSTIC CRITERIA before 30 yrs old, years of many long-lasting physical complaints resulting in treatment sought or sig impairment • 4 pain • 2 gastro-intestinal (e.g. vomiting, diarrhea, nausea, bloating) • 1 sexual (e.g. menstrual irregularity, sex indifference or dysfunction) (e.g. see conversion disorder) • 1 neurological (just symptoms, not worried about a specific disease) 2 10/25/11 somatization disorder DEMOGRAPHICS • prevalence 4% • sex ratio: 2-10:1 • onset: adolescence • course: chronic • prognosis : poor, chronic • low SES, low edu, unmarried somatization disorder CAUSE (genes for disinhibition runs in families; males ASPD & females somatization disorder) impulsiveness – short term gain (attn) – long term probs (social isolation) pleasure-seeking – provocative sexual behavior TREATMENT (hard to treat) - 1 gateway physician - CBT to promote appropriate behavior of social skills/relating to others - discourage relying symptoms to relate to others - discourage help-seeking behaviors pain disorder DIAGNOSTIC CRITERIA • persistent/severe pain in 1+ sites • associated w/ a stressor STATS • 5-12% prevalence • onset: any • can start from condition w/ real pain but persists TREATMENT • relaxation training • schedule daily activities & reinforcement for “no pain” • SSRIs 3 10/25/11 preoccupation somatoform disorders hypochondriasis body dysmorphic disorder hypochondriasis DIAGNOSTIC CRITERIA • 6+ months • based on misinterpretation of symptoms, preoccupied that has serious disease despite medical reassurance otherwise NOTE - Preoccupied w/body functions (e.g. veins, HR) or minor irregularities (e.g. cough, sore) - not delusional; also, more anxiety than illness symptoms STATS • prevalence 1-7% • sex ratio: 1:1 • onset: early adulthood; trimodal (14,45,60+) • course: chronic but waxes & wanes hypochondriasis CAUSE • cognitive-behavioral view = disorder of cognition & perception; misinterpret bodily sensations • attentional bias for illness-related information • knowledge & experience w/ illness (even from media) • modeling illness in family, reinforcement by escaping circumstances TREATMENT • 6 research studies show CBT every effective • educate client about this disorder • show client that selective attn to body area = selective perception of symptoms • response & exposure prevention (no checking/reassurance) • SSRIs 4 10/25/11 body dysmorphic disorder DIAGNOSTIC CRITERIA • complete preoccupation w/ imagined defect or excessive concern over a minor defect NOTE • compulsive checking behavior (e.g. checking in mirror, hiding/repairing) • avoidance of everyday activities to avoid others • significant emotional pain STATS • 1-5% prevalence • sex ratio: 1:1 • onset: adolescence to 20’s • 50% have no job • comorbid w/ depression body dysmorphic disorder CAUSE • genes for being high on trait of neuroticism • as child, reinforced for appearance rather than behavior • teased/criticized for appearance • OCD is sometimes comorbid TREATMENT • SSRIs • exposure & response prevention helps 80% of patients • cognitive therapy (ID & change perception of body) ADDITIONAL DIAGNOSIS If firmly held, get “Delusional Disorder, Somatic Type” purposely faking these are NOT somatoform disorders Why do it? malingering to gain an incentive or avoid jail or work factitious disorder to play the sick role; for attn & sympathy 5 10/25/11 purposely faking MALINGERING (external incentive) • avoid military duty • avoid incarceration • avoid work • gain insurance money • gain personal injury lawsuit award purposely faking FACTITIOUS DISORDER Wants attention & sympathy associated features: • childhood exposure to extensive med treatment • childhood abuse or disruption • grudge against medical profession • worked in medical profession • dependent personality • no social supports MUNCHAUSEN SYNDROME Historically, considered extreme & long-term factitious disorder 6