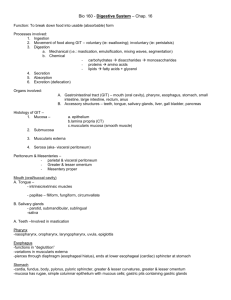
The Digestive System Student Objectives: Terms for review: Recall the definitions of the following terms pH Acidic pH Basic pH Neutral pH Enzyme Catalyze Starch Carbohydrate Protein Lipid Triglyceride Fatty acid Protein denaturation Peptide bond Buffer Exocrine gland Endocrine gland Vasoconstriction Vasodilation Terms: Define the following terms Peristalsis Bolus Segmentation Protease (proteinase) Peptidase Chyme Feces Excretion Emulsification Defecation Proenzyme Ingestion Digestion (chemical digestion) Mechanical processing (mechanical digestion) Absorption Secretion Mastication Mucins GI tract or alimentary canal Accessory digestive organs Overview: Explain the primary functions of the digestive system Define and discuss the digestive processes Identify the structures on a diagram Identify the structures on the available models Trace the path of bile salts from hepatocytes to digestive tract lumen Trace flow of blood from hepatic portal vein through liver to inferior vena cava Describe the histology of the structures Identify the organs and tissue structures on a diagram or prepared slide Discuss the functions for the specific layers of the GI tract Describe the processes involved in the movement of digestive materials through the GI tract. Explain the physiology of digestion through the GI tract. List and describe the mechanisms that regulate the activities of the digestive system. Discuss the regulation and coordination of gastric and intestinal movements and emptying. Explain where nutrients are absorbed in the GI tract. Melissa Gonzales McNeal --- Page 1 of 11 Layers of the GI Tract I. Mucosa A. Epithelium 1. Stratified squamous or simple columnar 2. Goblet cells 3. Enteroendocrine cells B. Lamina propria - areolar tissue C. Muscularis mucosae - smooth muscle 1. circular 2. longitudinal II. Submucosa A. Dense irregular connective tissue B. Submucosal plexus - plexus of Meissner III. Muscularis externa A. Skeletal and smooth muscle 1. Oblique smooth muscle fibers 2. Circular smooth muscle fibers 3. Longitudinal smooth muscle fibers B. Myenteric plexus IV. Serosa or adventitia A. Serosa (visceral peritoneum) - connective tissue covered with simple squamous epithelium B. Adventitia – dense network of collagen fibers Anatomy of The Gastrointestinal Tract (GI tract) – alimentary canal Peritoneum Parietal peritoneum Visceral peritoneum (serosa) Peritoneal fluid (serous fluid) Peritoneal cavity Retroperitoneal organs Mesenteries Mesocolon Falciform ligament Greater omentum Lesser omentum Mesentery proper Oral or buccal cavity (mouth) Lips or labia cheeks Vestibule Labial frenulum Hard palate Soft palate Uvula Pharyngeal arches Palatine tonsils Lingual tonsil Fauces Melissa Gonzales McNeal --- Page 2 of 11 Tongue Lingual lipase Body Root Lingual frenulum Intrinsic and extrinsic tongue muscles papillae Salivary Glands Parotid glands and ducts Submandibular glands and ducts Sublingual glands and lesser sublingual ducts Saliva Salivary amylase Teeth Crown Neck Root Pulp cavity Root canal Apical foramen Gingiva Enamel Dentin Cementum Periodontal ligament Incisors Cuspids or canines Bicuspids or premolars Molars Deciduous teeth (children’s teeth, primary teeth) Secondary dentition (permanent teeth) Pharynx Nasopharynx Oropharynx laryngopharynx Esophagus Upper and lower esophageal sphincters Hiatus Histology Mucosa Stratified squamous epithelium Lamina propria Muscularis mucosa Submucosa Muscularis Circular muscle fibers Longitudinal muscle fibers Adventitia Stomach Cardia Fundus Melissa Gonzales McNeal --- Page 3 of 11 Body Pylorus Pyloric antrum Pyloric canal Pyloric sphincter Rugae Histology Mucosa Simple columnar epithelium o Goblet cells Gastric pits Gastric glands o Chief cells o Parietal cells Lamina propria Muscularis mucosa Submucosa Muscularis Oblique, circular, and longitudinal smooth muscle Serosa Small Intestine Duodenum Jejunum Ileum Ileocecal valve (sphincter) Plica circularis (circular folds) Villi Lacteals Microvilli – brush border Peyers patch Histology - duodenum Villi Mucosa o Simple columnar epithelium Microvilli – brush border Goblet cells o Lamina propria Arteriole Venule Blood capillary Lacteal o Intestinal glands (crypt’s of Leiberkuhn) Base of villi – entrances Extend deep into underlying lamina propria o Muscularis mucosae Submucosa Duodenal glands (Brunner’s glands) Muscularis Circular and longitudinal smooth muscle Pancreas Melissa Gonzales McNeal --- Page 4 of 11 Pancreatic duct (duct of Wirsung) Accessory pancreatic duct (accessory duct, duct of Santorini) Histology Acini Pancreatic islet (islet of Langerhans) Liver and gallbladder Falciform ligament Right and left lobe Caudate lobe Quadrate lobe Hilus Right and left hepatic ducts Common hepatic duct Cystic duct Common bile duct Histology – liver Lobules Central vein hepatocytes Sinusoids Hepatic macrophages (kupffer cells) Portal triad Hepatic portal vein – edge of lobule Hepatic artery – edge of lobule Bile canaliculus – edge of lobule or in lobule Large Intestine Cecum Appendix (vermiform appendix) Colon Ascending, transverse, descending, and sigmoid colon Right colic flexure (hepatic flexure), left colic flexure (splenic flexure), and sigmoid flexure Rectum Anal canal Anal columns Anus (anal orifice) Internal anal sphincter External anal sphincter Teniae coli Haustra Physiology of The Gastrointestinal Tract (GI tract) – alimentary canal I. Oral or buccal cavity A. Functions of oral cavity 1. oral cavity a. Analysis of material b. Mechanical processing c. Lubrication d. Limited Digestion i Carbohydrates ii Lipids Melissa Gonzales McNeal --- Page 5 of 11 2. Tongue a. Functions i Mechanical processing ii Assist in chewing and swallowing iii Sensory analysis iv Secretion Lingual lipase mucins - glycoproteins for lubrication 3. Salivary Glands a. Composition and functions of saliva i Wet food Mucins ii Dissolves food iii Bicarbonate ions buffer acidic food iv Chemical digestion Salivary amylase v Protects mouth from infections Lysozyme Rinsing action b. mumps c. regulation of salivation i increase salivation - parasympathetic ii stop salivation – sympathetic 4. Teeth (dentition) a. Functions of teeth i Incisors ii Cuspids or canines iii Bicuspids or premolars iv Molars b. Dental succession i Deciduous teeth ii Secondary dentition iii Eruption (emerge) Impacted teeth B. Digestion in oral cavity 1. Mechanical digestion – mastication or chewing a. Bolus 2. Chemical digestion a. Amylase – starch b. Lingual lipase – lipids II. Pharynx and esophagus A. Functions 1. pharynx a. Function: common passageway for solid food, liquid, and air 2. Esophagus a. Function: carry solid foods and liquid to somach b. Histology i Muscosa and submucosa have large folds for expansion B. Deglutition 1. buccal phase 2. pharyngeal phase Melissa Gonzales McNeal --- Page 6 of 11 3. esophageal phase III. Stomach A. Functions 1. Bulk storage of ingested food a. Pylorospasm b. Phyloric stenosis 2. Mechanical digestion 3. Chemical digestion 4. Production of intrinsic factor B. Histology of the Stomach 1. Mucosa a. Simple columnar epithelium b. Gastric pits i Mucous cells – alkaline mucous ii Gastric glands (body and fundus of stomach) (a) Parietal cells Intrinsic factor for vitamin B12 absorption Hydrochloric acid Carbonic anhydrase Alkaline tide (b) Chief cells Pepsinogen Gastric lipase iii Pyloric glands (pylorus of stomach) (a) Enteroendocrine glands G cells: gastrin Stimulates secretion of parietal and chief cells Stimulates contraction of gastric wall D cells: somatostatin Inhibits gastrin 2. Submucosa 3. Muscularis – longitudinal, circular, oblique 4. serosa C. Digestion in the stomach 1. Mechanical digestion - peristalsis 2. Chemical digestion a. Proteins i HCl - denaturation of protein molecules ii Pepsin – breaks peptide bonds b. Milk fats i Gastric lipase ii Primarily in infant stomachs D. Absorption of nutrients in the stomach 1. some electrolytes 2. Drugs: aspirin, alcohol a. Alcohol dehydrogenase E. Regulation of gastric activity 1. Cephalic phase 2. Gastric phase 3. Intestinal phase Melissa Gonzales McNeal --- Page 7 of 11 V. Pancreas A. Functions 1. Hormone production 2. Digestive enzyme production 3. Buffer production B. Histology of the pancreas 1. Pancreatic acini (acinar) – pancreatic juice 2. Pancreatic islets (islets of Langerhans) – insulin C. Regulation of pancreas 1. nervous system control – parasympathetic NS 2. endocrine control a. CCK b. GIP c. Secretin VI. Liver A. Functions 1. Metabolic regulation 2. Hematological regulation 3. Bile production B. Histology 1. Hepatocytes 2. Lobules a. Interlobular septum b. Sinusoids c. Central vein d. Kupffer cells (stellate reticuloendothelial cells) i Phagocytes for pathogens, cell debris, damaged blood cells ii Storage (a) Iron (b) Some lipids (c) Heavy metals 3. Portal area/hepatic triad a. Hepatic portal vein b. Hepatic artery proper c. Small branch of bile duct C. Flow of bile through liver 1. Bile canaliculi 2. Bile ductules 3. Bile ducts 4. Right and left hepatic ducts 5. Common hepatic duct 6. Cystic duct 7. Common bile duct (bile duct) VII. Gallbladder A. Functions 1. Bile storage 2. Bile modification B. Gallstones VIII. Small Intestine A. Functions 1. Chemical digestion is completed Melissa Gonzales McNeal --- Page 8 of 11 B. C. D. E. F. 2. Nutrient absorption Histology of Small Intestine 1. Structures that increase surface area a. Plica circularis (circular folds) b. Villi i Intestinal glands, intestinal crypts or crypts of Lieberkuhn ii Goblet cells iii lacteals c. Microvilli – brush border 2. Submucosa a. Duodenal glands (Brunner’s glands) Hormones of small intestine 1. Cholecystokinin (CCK) 2. Enterocrinin 3. Gastrin 4. Glucose-dependent insulinotropic peptide (Gastric inhibitory peptide) 5. Secretin 6. Vasoactive intestinal peptide (VIP) Digestion in the small intestine 1. Mechanical digestion a. Peristalsis b. Segmentation 2. Chemical digestion a. Enzymes from small intestine: Brush Border Enzymes i Carbohydrases ii Dipeptidases and peptidases iii Enterokinase b. Enzymes from pancreas i Pancreatic amylase ii Pancreatic lipase iii Pancreatic nucleases iv Protein digestion (a) Proteases: break apart large protein complexes (b) Peptidases: break small peptide chains into individual amino acids (c) Released as proenzymes that are activated in small intestine (d) Enzymes Trypsinogen Chymotrypsinogen procarboxypeptidase v Trypsin inhibitor c. Bile from liver Absorption in small intestine 1. Lipids 2. Amino acids 3. Water 4. Ions 5. Vitamins Regulation 1. Small intestine a. Parasympathetic and sympathetic NS b. Myenteric reflexes Melissa Gonzales McNeal --- Page 9 of 11 c. Gastroileal reflex IX. Large Intestine A. Functions 1. Reabsorption of water and compaction of intestinal contents into feces 2. Absorption of vitamins produced by bacteria 3. Storage of fecal material B. Histology 1. Mucosa a. Intestinal glands i Simple columnar cells ii Goblet cells 2. Submucosa 3. Muscular layer a. Internal circular layer of smooth muscle is normal b. Outer longitudinal muscle i Taeniae coli ii Haustra 4. Serosa filled with fat C. Hemorrhoids I. Large intestine A. Digestion 1. Mechanical digestion a. Peristaltic waves b. Haustral churning 2. Chemical digestion a. No enzymes secreted b. Bacterial actions i Fermentation ii Vitamin production B. Absorption in large intestine 1. Some electrolytes 2. Water 3. Bile salts 4. Vitamins 5. Organic wastes C. Regulation of large intestine 1. Gastroilial reflex 2. Gastrocolic (gastroenteric reflex) and duodenocolic reflexes a. responds to stretch receptors in stomach and duodenum 3. Stimulates motility and secretion in colon 4. Spinal reflex 5. Limited voluntary control Explain where the hormones are released. Explain what stimulates release of the hormones. List the target(s) for each of the hormones. Explain the action(s) of the hormone. 1. Intrinsic factor 2. Gastrin 3. Somoatostatin Melissa Gonzales McNeal --- Page 10 of 11 4. 5. 6. 7. 8. Cholecystokinin Enterocrinin Gastric Inhibitory peptide Secretin Vasoactive intestinal peptide (VIP) Clinical applications: Peptic ulcer Gallstones – cholecystitis Pancreatitis Acites Chrohn disease Diverticulitis Dysphagia Hiatal hernia Ulcerative colitis Mumps Diarrhea Constipation Gastroesophageal reflux disease Pylorospasm Pyloric stenosis Lactose intolerance Dental caries Gingivitis Heartburn Hemorrhoids Impacted molars Periodontal disease Bulimia Melissa Gonzales McNeal --- Page 11 of 11
 0
0
advertisement
Download
advertisement
Add this document to collection(s)
You can add this document to your study collection(s)
Sign in Available only to authorized usersAdd this document to saved
You can add this document to your saved list
Sign in Available only to authorized users