Optochin Disk Procedure - University of Nebraska Medical Center
advertisement

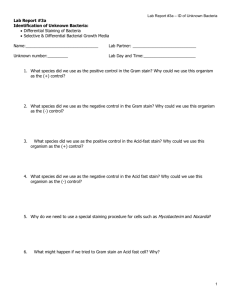
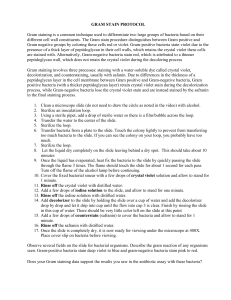
For student use only University of Nebraska-Medical Center Clinical Laboratory Science Program Gram Stain Procedure Principle: The differential staining seen with the Gram stain occurs because the two types of bacteria differ significantly in their cell envelope composition. The cell envelopes of both gram-positive and gram negative bacteria contain a cell wall (also known as the murein layer) and a cytoplasmic membrane. In addition, the cell envelopes of gram-negative bacteria contain a periplasmic space (between the cell wall and cytoplasmic membrane) and an outer membrane. It is the murein layer, or cell wall, that causes the differential staining seen with the Gram stain. The murein layer, which is composed of a peptidoglycan macromolecule, is much thicker in gram-positive bacteria than in gram-negative bacteria. Also, the cell walls of gram-positive bacteria contain teichoic acids and mycolic acids which fortify the murein layer. The thin cell walls of gram-negative bacteria, on the other hand, contain lipopolysaccharides which are extracted during decolorization. In the Gram stain procedure the slide is flooded with crystal violet (the primary stain), followed by Gram’s iodine (the mordant), which chemically bonds the alkaline crystal violet to the cell wall. The slide is then decolorized most commonly with a mixture of acetone and absolute alcohol. The decolorizer substantially damages the thin cell walls of gram-negative bacteria and allows the crystal violet-iodine complex to wash out, whereas the thicker cell walls of gram-positive bacteria are more resistant to damage and therefore retain the stain complex. In the final step, the slide is flooded with safranin (the counterstain), which stains the decolorized gram-negative bacteria pink or red. Specimen Collection and Preparation The Gram stain is used routinely and as requested in the clinical microbiology laboratory for the primary microscopic examination of specimens submitted for smear and culture. It is ideally suited for those specimen types in which bacterial infections are strongly suspected, but it may be used to characterize any specimen. Cerebrospinal fluid, sterile fluids, expectorated sputum or bronchoalveolar lavages, and wounds and exudates are routinely stained directly. Urine specimens may not be routinely stained directly. Stool specimen for gram stain is performed only to evaluate the presence or absence of polymorphonuclear cells. Samples sent for focused screening cultures usually are not stained. The Gram stain is regularly used to characterize bacteria growing on culture media. Specimen Gram stain preparation: 1. Roll swab, taken from representative areas of specimen, gently across slide to avoid destruction of cellular elements and disruption of bacterial arrangements. 2. If only one swab received, roll on sterile swab to sterile slide for gram stain inoculate media plates, then place swab in the broth last. 3. Biopsies and tissue specimens. A “touch prep” preparation may be used. Homogenizing or grinding tissue specimens before preparing smear will often destroy characteristic cellular entities and bacterial arrangements. • Mince with sterile scissors or scalpel. • Prepare a “touch prep.” Use sterile forceps to hold pieces, and touch the sides of one or more of the minced fragments to a sterile glass slide, grouping touches together for easier examination. Colonies from media preparation: 1. Place a drop of sterile saline on slide. 2. Transfer a small portion of colony with a sterile applicator stick, wire needle, or loop. 3. Gently mix to emulsify. For student use only University of Nebraska-Medical Center Clinical Laboratory Science Program Reagents and Supplies 1. Gram Crystal Violet Solution: Approximately 0.4% crystal violet in aqueous alcohol/acetone (3:1 ratio, respectively) solution 2. Gram Iodine Solution (stabilized): Approximately 13% polyvinylpyrrolidone-iodine complex in 1.9% aqueous potassium iodine 3. Gram Decolorizer Solution: Denatured ethyl alcohol and acetone, approximately one part to one part 4. Gram Safranin Solution: Approximately 0.25% safranin in 20% ethyl alcohol 5. Glass slides 6. Slide warmer Storage 1. Keep all reagents at room temperature. 2. Protect the Gram’s iodine reagent from the light when not in use. Quality Control Run controls daily using 18-24 hour cultures of known gram-positive and gram-negative microorganisms. 1. The following QC organisms should be used: Positive control – Staphylococcus aureus Negative control – Escherichia coli 2. Expected results: Staphylococcus aureus – stains as gram positive cocci (dark blue to blue-black) Escherichia coli – stains as gram negative bacilli (pink-red) Procedure 1. Using either heat or methanol, fix the specimen onto the slide. Heat fixation: Place on a slide warmer for 1 minute. Caution: Do not overheat. Overheating can cause over-decolorization. Methanol fixation: Flood the slide with 70%-95% methanol for 1 minute. The methanol is then drained off, and the slides are air-dried. 2. Place the slide on a slide holder rack at the sink. You may wish to wear latex gloves to protect your skin from the stain reagents. 3. Flood the slide with crystal violet. Allow to remain 30 seconds. Rinse with water. Caution: Avoid excessive rinsing. This can cause over-decolorization because crystal violet is not bound to the cell until Gram’s iodine is added. 4. Flood the slide with Gram’s iodine. Allow to remain 30-60 seconds, then rinse with water. 5. Decolorize the slide with the acetone-alcohol mixture. Pick up slide and carefully apply decolorizer solution (1-2 quick squirts) just until no more color is being washed from the smear. Quickly rinse off any remaining decolorizer with tap water. Caution: Avoid prolonged decolorization or excessive rinsing. These can wash the crystal violet-iodine complex from gram-positive cells. 6. Flood the slide with safranin for 30-60 seconds. Rinse gently with water. Caution: Do not leave the counterstain on longer than 1 minute. This can make gram positive organisms appear gram-negative. 7. Blot slide dry with paper towel. Carefully wipe excess stain from the back of the slide. 8. Let the slide dry completely before adding immersion oil and examining microscopically. For student use only University of Nebraska-Medical Center Clinical Laboratory Science Program Reading Gram stains: • Scan on low power (10x) to locate correctly stained areas • Read gram stain on oil immersion • Note the cellular morphology, arrangement and Gram stain reaction. Interpretation of Test Gram-positive bacteria stain dark blue to blue-black. All other elements stain safranin red. Individual structures absorb a different amount of safranin, so some will have prominent staining (strong avidity) and others will be weakly stained (low avidity). Among the gram-negative bacteria the enterics have strong avidity and stain a bright red; pseudomonads are less avid and stain moderately well. Anaerobic bacilli and other thin-walled gram-negative organisms, such as Borrelia, Legionella, and Spirillum, stain weakly. Always check the quality of the stain before moving to interpretation. Reporting Gram stains: (NOTE: scale may vary at your clinical site) • Gram reaction (gram positive = GP, gram negative = GN, gram variable = GV) • Morphology (bacilli or rod = R, cocci = C, coccobacilli = CB) • Arrangement GNR GPC GPR GNC large single spores diplococci (DC) thin pair large fusiform chains palisading tiny clusters branching tetrads • Other descriptive terms (i.e. pleomorphic, lancet-shaped, etc.) When looking at SPECIMEN Gram Stains, also include the following: • Sputum >25 squamous epithelial cells per low power field – REJECT specimen and do not do gram stain. • Type and amount of cells (if a specimen gram stain) None/NCS no cells seen Rare (1+) < 1 per oil immersion field Few (2+) 1-5 per oil immersion field Moderate (3+) 5-10 per oil immersion field Many (4+) >10 per oil immersion field • Enumerate the types of organisms as follows (if a specimen gram stain): None/NOS no organisms seen Rare (1+) <1 per oil immersion field Few (2+) 1-10 per oil immersion field Moderate (3+) 11-25 per oil immersion field Many (4+) >25 per oil immersion field Modifications Common modifications of the classic Gram stain procedure involve variations in fixation method, reagents, and timing. Fixation, which attaches the specimen to the slide before staining, can be done with heat or methanol. In heat fixation, the slide is gently warmed so that all moisture evaporates from the material. In methanol fixation, the slides are flooded with 70%-95% methanol for 1 minute. The methanol is then drained off, and the slides are air-dried. Although more labs use heat fixation, methanol fixation is superior for 5 reasons: 1. It preserves bacterial and human cell morphology. 2. It preserves red blood cells, which makes it especially useful with bloody specimens. 3. It provides greater control over the decolorization process, because organisms fixed with methanol are more resistant to decolorization. 4. It prevents liquid specimens from washing off the slide. 5. It leaves a clearer background. For student use only University of Nebraska-Medical Center Clinical Laboratory Science Program Common variations in reagents involve the decolorizer and the counterstain. Slides can be decolorized with acetone, absolute alcohol, or a mixture of the two. Acetone works more rapidly, but the slide must be rinsed with water as soon as the purple color disappears to avoid overdecolorization. Slides are usually counterstained with safranin, but neutral red or dilute carbolfuchsin, which better stains anaerobes, are used sometimes. Some microbiologists also advocate adding a fast green and tartrazine step before the final counterstain with safranin to give a better contrast between gram-negative organisms and background material. Finally, the duration of the steps in the Gram stain procedure may vary somewhat. Because anaerobes tend to stain weakly, they may stain better if the counterstain is left on for 1 minute instead of 30 seconds. Precautions Pitfalls in the Gram stain include both inherent limitations and technical errors. The Gram stain will not detect organisms which exist within host cells (e.g., Chlamydia spp), organisms with no cell wall (e.g., Mycoplasma spp and Ureaplasma spp), and organisms too small to be seen with light microscopy (e.g., spirochetes). Mycobacteria usually will not stain, and Legionella spp stain only when taken directly from culture. Gram-negative bacteria that stain poorly with safranin include Campylobacter spp, Legionella spp, Bacteroides spp, Fusobacterium spp, and Brucella spp. Certain conditions are known to damage the cell wall, causing gram-positive bacteria to falsely appear gram-negative or gram-variable. These include antibiotic treatment, cultures more than 48 hours old, inflammatory responses in the host, and autolytic enzymes (e.g., S. pneumoniae). To minimize ambiguous results, specimens should be collected before the patient begins antibiotic therapy. Also, Gram stains should be performed on colonies taken from culture media that do not contain antibiotics, preferably on colonies that are 18-24 hours old. Finally, correct interpretation of Gram stains requires a theoretical background of bacteria and their morphology, because improper technique or suboptimal reagents can cause unreliable results. Errors in technique which can alter Gram stain results include the following: • Fixation with excessive heat alters cell morphology and makes organisms more susceptible to over-decolorization. • Low concentrations of crystal violet make gram-positive organisms more susceptible to overdecolorization. • Insufficient exposure to iodine and lack of available iodine can prevent crystal violet from bonding firmly with the cell wall, thus making gram-positive organisms more susceptible to overdecolorization. To ensure reliable Gram stain results, only fresh iodine should be used. • Prolonged decolorization, especially with acetone, can cause gram-positive bacteria to appear gram-negative. Insufficient decolorization can make gram-negative organisms falsely appear gram positive. • Insufficient counterstaining can fail to stain gram-negative bacteria and background material, whereas excessive counterstaining will leach the crystal violet-iodine complex from gram positive bacteria and stain them with safranin, thus making them falsely appear gram-negative. • Prolonged washing between any of the steps can cause over-decolorization. References: Mahon & Manuselis, Textbook of Diagnostic Microbiology, Second edition, 2000. Pages 267-268. http://www.api-pt.com/pdfs/2004Bmicro.pdf