Modern Corneal Surgery - Minnesota Optometric Association
advertisement

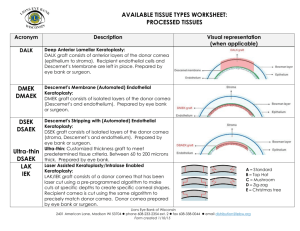
1/9/2015 Financial disclosures Modern Corneal Surgery • Formerly a paid research scientist for Alcon Laboratories Inc. (2006) • Travel and consulting services for Essilor Laboratories (2010) • Honoraria from Contact Lens Spectrum for publication submission (2014) Derek J. Louie, MSc, OD, FAAO Clinical Associate Professor, Ophthalmology Video presented with permission from Winston Chamberlain, MD, PhD Objectives Basic corneal anatomy • Review corneal anatomy • Understand the variations and indications of corneal surgery • Understand when to refer to corneal surgeon for assessment and treatment Epithelium & limbal stem cells Epithelium & limbal stem cells • Stem cells are necessary for intact and functioning epithelium • Epithelial cells migrate from the limbus to central cornea then are sloughed off – 5-7 cell layers thick, ~50µm total • Epithelium acts as barrier tissue to prevent fluid movement from tears to stroma • Epithelium is necessary to provide smooth refractive surface 1 1/9/2015 Corneal stroma Corneal endothelium • Thickest layer of cornea • Approximately 500µm • Regular distribution of collagen fibers produces destructive interference producing a clear tissue • Scars happen here • Monolayer of cells acting as pump to restrict water into the stroma • Aqueous leaks across the endothelium to provide glucose, amino acids and other nutrients to the cornea • 2500-3000 cells/mm2 in average adult cornea – 0.6% decrease/year • 300-600 cells/mm2 leads decreased barrier function and possibly edema • Fuch’s endothelial dystrophy Reasons for cornea surgery • Excessive scarring/opacity • Excessive ectasia/thinning (<200 µm) • Excessive loss of endothelium/endothelial function TYPES OF CORNEAL PROCEDURES Penetrating Keratoplasty (Conventional) Penetrating Keratoplasty PKP or PK Full thickness keratoplasty • • • • • Approximately 40,000/year in US ~20% rejection/year Lifetime of risk Does not require blood/tissue match May or may not improve vision – Decrease/remove scar – Increase thickness 2 1/9/2015 Suture patterns Suture Patterns IntraLase Enable Keratoplasty • Necessary for most corneal surgery • Surgeon dependent • IEK • Femtosecond Laser Assisted Keratoplasty– “FLAK” – Running – single suture and knot – Interrupted – multiple sutures and knots – Combo • Selective removal (or application) may help alleviate irregularity – Topography guided removal 3 1/9/2015 Shapes Shapes • TopHat • Zigzag • Mushroom • Christmas Tree • Standard • Zig Square Anterior Lamellar Keratoplasty • ALK • Not full thickness – Bladed or laser options How a Flap or Free Cap is Created 4 1/9/2015 Femtosecond Laser Assisted ALK Deep Anterior Lamellar Keratoplasty • DALK • “Big Bubble” – dissection technique Zigzag incision clear on OCT Zigzag incision clear on OCT Zigzag incision clear on OCT Zigzag incision clear on OCT 5 1/9/2015 DALK Tough Case with Multiple RK Incisions After Surgery 6 1/9/2015 Endothelial Keratoplasty • Descemet Stripping and (Automatic) Endothelial Keratoplasty • Includes basement membrane • DSEK and DSAEK Deep Lamellar Endothelial Keratoplasty • DLEK • Usually doesn’t require sutures • Held in place by air bubble What about transplanting a single cell layer ?? 7 1/9/2015 Descemet Membrane Endothelial Keratoplasty (DMEK) DMAEK in the Eye Bank Viscodissection Limbal Stem Cell Deficiency Intralase assisted Air dissection Causes of Limbal Stem Cell Deficiency • Congential – Aniridia – Ectodermal Dysplasia – Keratitis Ichthyosis Deafness (KID) Syndrome – Autoimmune Polyglandular Syndrome • Autoimune/Inflammatory – Stevens Johnson Syndrome – Ocular Cicatricial Pemphigoid (Mucous Membrane Pemphigoid) • Acquired Conditions – Pterygia – – – – – – – Drug toxicity/topical medications Chemical/thermal burns Herpes Virus Contact lens Limbal tumors Radiation Keratopathy Sequelae of Mustard Gas exposure – Multiple surgeries 8 1/9/2015 Stem cell deficiency in one eye. Total or Diffuse limbal stem cell deficiency Partial limbal stem cell deficiency Sectoral conjunctival scraping to remove conjuctival epithelium from corneal surface ± AMT Poor tear production and/or keratinized surface • KLAL Allogeneic limbal stem cell transplant ± conjunctiva from living related donor (lrCLAL) with systemic immunosuppression OR Autologous limbal stem cell transplant ± conjunctiva from healthy other eye Keratolimbal Allograft Allogeneic limbal stem cell transplant ± conjunctiva from 1-2 cadaver eyes (KLAL) with systemic immunosuppression Keratoprothesis Boston K-Pro I or II, AlphaCor, Oculaid, Osteo-odontokeratoprosthesis KLAL—Keratolimbal Allograft Keratolimbal allograft in corneal reconstruction E M Espana, M Di Pascuale, M Grueterich, A Solomon and S C G Tseng Boston Keratoprosthesis Type I 56 y.o Farmer – KPRO type I POM #4--20/30 Pre surgical--Hand Motion from Eastern Washington with history of bilateral corneal alkali burn 9 1/9/2015 Boston Keratoprosthesis Type I 58 y.o male 20/4000 --Counting fingers vision at 2 feet 20/25 vision with Scleral Contact Lens h/o Stevens Johnson Syndrome—Chronic ocular findings Indications for Boston Keratoprosthesis • Multiple failed corneal transplants • Extensive corneal blood vessels • Total or severe limbal stem cell deficiency Keratoconus • • • • • Non-Inflammatory corneal ectatic disease Progressive steepening and thinning Irregular astigmatism 1:2000 patients Treatment – Contact lens – Penetrating keratoplasty – Deep anterior lamellar keratoplasty • Life long risk of rejection (with PK and DALK) Keratoconus • 2nd most common reason for cornea surgery • Full thickness was the only option until ~1015 years ago • Scleral lenses have help reduce the need for surgery • Intra-corneal ring segments (ICRS) can help with mild corneal irregularity – INTACS® • Cross linking maybe the answer 10 1/9/2015 Intracorneal Ring Segments INTACS® • Flatten the steep part of the cornea or cone to reduce distortions • Does not stop ectasia or progression • Made of PMMA • Intrastromal placement – Can be femtosecond laser assisted • Removable Crosslinking stiffens the cornea 365nm Better Picture? 11 1/9/2015 Cross-linking Switzerland Switzerland CBM Vega X-- BON OPTIC – ITALY TECHNIQUE • • • • Sterile conditions Topical anesthesia Debride central epithelium 7-9 mm of cornea. Treat surface with 0.1% solution Riboflavin (in 10 ml dextran 20% solution) for 30 minutes starting 5 minutes before the start of irradiation. • UVA radiation of 365 or 370 nm wavelength for 30 min TECHNIQUE • Accelerated cross-linking study – 15 mW/cm2 for 8 min – 30 mW/cm2 for 4 min – 45 mW/cm2 for 2 min 40 sec – irradiance of 3 mW/cm2 at distance of 1 cm from the cornea – dose of 5.4 J/cm2 • Prophylactic antibiotic drops • Bandage contact lens • Follow-up visits (1day, 7 day, 1 month, 3 months) Topographic Changes Long term stabilization • METHODS: Four hundred eighty eyes of 272 patients with progressive keratoconus were included in this long-term retrospective study. The maximum follow-up was 6 years. At the first and all followup examinations, refraction, best corrected visual acuity (BCVA), corneal topography, corneal thickness, and intraocular pressure were recorded. • RESULTS: The analysis included 241 eyes with a minimum followup of 6 months. The steepening decreased significantly by 2.68 diopters (D) in the first year, 2.21 D in the second year, and 4.84 D in the third year. The BCVA improved significantly (R1 line) in 53% of 142 eyes in the first year, 57% of 66 eyes in the second year, and 58% of 33 eyes in the first year or remained stable (no lines lost) in 20%, 24%, and 29%, respectively. Two patients had continuous progression of keratoconus and had repeat crosslinking procedures. Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135(5):620-7. J Cataract Refract Surg 2008; 34:796–801 12 1/9/2015 Nature.com • In conclusion, in this systematic review and meta-analysis, we found that CXL may be effective in halting the progress of KC for at least 12 months under certain conditions. The effects of CXL on visual acuity improvement are also remarkable. With long-term follow-up (after 18 months post-CXL), a significant decrease in Kave and MRSE was observed, and BCVA also significantly increased compared with the pre-CXL values. However, no statistical difference in CT after CXL was found during long-term follow-up. Further research from randomized trials is necessary to confirm these findings. Other Applications Post Refractive Surgery Ectasia Hafezi F, Kanellopoulos J, Wiltfang R et al. Corneal collagen crosslinking with riboflavin and ultraviolet A to treat induced keratectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2007;33(12):2035-40. Kymionis GD, Diakonis VF, Kalyvianaki M et al . One-year follow-up of corneal confocal microscopy after corneal cross-linking in patients with post laser in situ Keratosmileusis ectasia and keratoconus. Am J Ophthalmol. 2009;147(5):774-8, 778. Infectious melting keratitis Iseli HP, Thiel MA, Hafezi F et al. Ultraviolet A/riboflavin corneal cross-linking for infectious keratitis associated with corneal melts. Cornea. 2008;27(5):590-4. Bullous Keratopathy Corneal collagen cross-linking in keratoconus: A systematic review and meta-analysis, Jul10, 2014. Nature.com Tian Chunyu, Peng Xiujun, Fan Zhengjun, Zhang Xia & Zhou Feihu Wollensak G, Aurich H, Wirbelauer C et al. Potential use of riboflavin/UVA cross-linking in bullous keratopathy. Ophthalmic Res. 2009;41(2):114-7. Ehlers N, Hjortdal J. Riboflavin-ultraviolet light induced cross-linking in endothelial decompensation. Acta Ophthalmol. 2008;86(5):549-51. Summary • Multiple corneal surgeries available • Lamellar keratoplasty has become the approach to most types of corneal pathology • Severe corneal disease requires more heroic intervention • Femtosecond lasers are fine tuning the surgeon maneuvers, but can’t do everything • Familiarity with different corneal procedures is essential in helping patients make informed decisions regarding their vision and eye health Thank you for staying awake (or at least not snoring…) louied@ohsu.edu 13