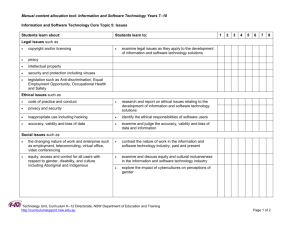
Research Activity Report 2012
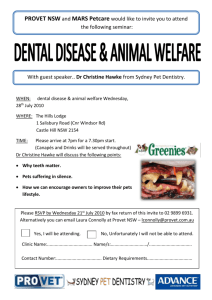
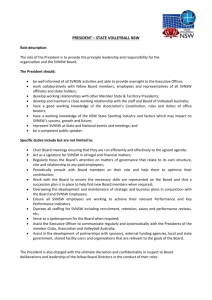
advertisement

Research Activity Report 2012 Contents Message from the Board Chair . . . . . . . . . . . . . . . . . . . . . . 2 Our highlights . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4 Fifteen years of cancer research . . . . . . . . . . . . . . . . . . . . . 6 Our research strategy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7 Who we are . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8 Prevention . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9 Changing skin cancer prevention worldwide . . . . . . . . . . 10 Making healthy food choices the easiest choices . . . . . . 12 Addressing liver cancer . . . . . . . . . . . . . . . . . . . . . . . . . . . 13 Diagnosis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14 Better cervical cancer screening . . . . . . . . . . . . . . . . . . . 16 Treatment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18 Understanding the gap in Aboriginal cancer survival . . . . 19 Radiation’s effects on neighbouring cells . . . . . . . . . . . . . 20 New invention simplifying radiotherapy treatment verification . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21 One treatment discovery impacting two cancers . . . . . . 22 Survivorship . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 23 Supporting those faced with the unknown . . . . . . . . . . . . 24 The factors influencing prostate cancer outcomes . . . . . . 25 Appendices Staff . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 26 Grants . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 28 Publications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 32 Board and committees . . . . . . . . . . . . . . . . . . . . . . . . . 36 Contact . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 37 Our vision Cancer defeated Our vision will be realised when lives are not cut short nor the quality of life diminished by cancer. Our mission To defeat cancer through engaging the community Cancer Council NSW connects people and organisations to the cancer cause. Together we can build insights into the significance of cancer in our lives and contribute our talents towards the vision of cancer defeated. We work across all cancers. The impact from our work together will be visible in changing: • The lives of cancer patients and carers • Scientific knowledge • Community understanding and behaviour • Society, policy and practice to advance cancer control. Increasingly, people will work in organisations and live in families and social settings which advance the control of cancer and where resources (people, ideas, services and funds) are developed globally and locally to meet the challenges of cancer. Message from the Board Chair “We want to know the ‘whys’ of cancer, so that we can best understand how to positively improve the lives of those with the disease, their families and the wider community.” Mr Bruce Hodgkinson SC Chair of the Board 2 Message from the Board Chair At Cancer Council NSW, we fund research that significantly impacts the cancer landscape through the investigation of cancer prevention, diagnosis, treatment and survivorship. Research and Cancer Council NSW We want to know the ‘whys’ of cancer, so that we can best understand how to positively improve the lives of those with the disease, their families and the wider community. We focus on those cancers that are the most lethal yet underfunded, such as brain, pancreatic and liver cancer. We also focus on disadvantaged groups, such as Aboriginal communities – among whom the cancer mortality rate is up to 60% higher than among non‑Aboriginal Australians – and seek to rectify such inequalities. To realise our vision of cancer defeated, Cancer Council NSW must seek out opportunities to improve our collective knowledge about cancer. This understanding does not just lead to better diagnostics and treatments, but is also used to encourage healthy behaviours in community members, to persuade governments to develop better policy, and to provide programs and services to support people through each step of their cancer journey. In the last fifteen years, we have awarded well over $120 million to Australia’s best and brightest cancer researchers. As the largest non-government funder of cancer research in NSW, we are able to invest strategically in research, and contribute to sustaining research momentum. Our research has found that major advances in screening, prevention and treatment have resulted in thousands of cancer deaths being avoided today compared to rates 20 years ago. More than 61,000 people are alive in Australia today thanks to knowledge that has been uncovered and put into practice over this time. All of this work is achieved in collaboration with the best universities, institutes and researchers throughout Australia and across the globe. These partnerships create greater leverage and opportunities than any single organisation could achieve on its own. Cancer Council NSW has solid foundations on which to build and grow. By combining scientific review with the assessments of our trained research consumers, we are able to determine which areas of research will best serve the wider community. Recent research discoveries The researchers that we fund have made some remarkable discoveries over the last 15 years. One of our recent breakthroughs is the creation of new drugs to fight neuroblastoma and pancreatic cancer that could slow cancer progression by 50%. We also contribute funding to groups at the Kinghorn Cancer Centre and Melanoma Institute Australia, who are on their way to mapping both the pancreatic and melanoma cancer genomes. This will dramatically improve our understanding of these cancers, paving the way for new discoveries and more personalised treatments. Our funded researchers have invented a new device that will make radiotherapy safer and more effective. They have also discovered that vitamin B3 could be used to prevent skin cancer, which may stop thousands of people from being diagnosed every year. And they have made hundreds of discoveries about the way cancers work, behave and spread that move us ever closer to defeating cancer. Thank you to the community In the pages that follow, you will be presented with a snapshot of just some of our research programs, both those that Cancer Council NSW runs, and those to which we contribute vital funding. We share the stories of people whose lives have been affected by cancer, highlighting the very reason that we fight this fight each and every single day. All of this is possible thanks to the support of the community, who contribute 96% of our funding, assist with our research funding decisions, participate in our research studies, and help spread the message about our work. Thank you. Mr Bruce Hodgkinson SC Chair of the Board Cancer Council NSW Research Activity Report 2012 3 Our highlights Total funding $14.9m research We fund all types of cancer research We provided $14.9 million* in funding to support research this year. We currently fund research into more than 15 different cancer types. Almost half our research funding is devoted to projects that will benefit all cancers. Fundamental – 25% Causes – 10% Prevention – 8% Types of research funded in 2012 Detection – 15% Treatment – 27% Survivorship – 10% Cancer Council NSW is dedicated to driving major advances in research, ensuring no cancer is ignored. Model systems – 6% What we funded 160 75 researchers institutions Investment 49 projects The five cancers we invested in most heavily were: 1 2 $1.4m* 3 $1.2m* Pancreatic 4 4 Leukaemia 5 $790k* *2011/12 financial year $860k* Melanoma Breast $760k* Brain We are dedicated to our vision of a society where lives are not cut short nor the quality of life diminished by cancer. Achievements Discovered that vitamin B3 could prevent up to 50% of non-melanoma skin cancers Changed the landscape of liver cancer prevention in Australia page 13 page 10 Created new drugs to fight neuroblastoma and pancreatic cancer that could slow cancer progression by 50% Invented a new device that will make radiotherapy safer and more effective page 21 who selects Grants page 22 Cancer patients, survivors and carers help us decide what research to fund. Feedback from community members is as important as the assessments of our scientific review panels. Together, these two groups determine which projects we fund each year. Global capabilities Our researchers have global collaboration and reach We have hundreds of collaborations with academics, organisations, networks and communities around the world, which enhance our research capabilities. Cancer Council NSW Research Activity Report 2012 5 Fifteen years of cancer research Fifteen years of cancer research Cancer Council NSW has focused on cancer research since our inception in 1955. Better treatments, improved diagnostics and other innovations over the past 15 years have transformed the cancer landscape, saving the lives of many thousands of people. Our ageing population and better detection mean that the number of people diagnosed with cancer has risen dramatically over the last 15 years – diagnoses in NSW alone increased by 25% between 1997 and 2012. Yet thanks to the tireless efforts of oncologists, researchers, GPs and the support of the community, the risk of dying from cancer actually dropped by 20% in those 15 years. Four of the most common cancers – prostate, melanoma, breast and thyroid – now have survival rates of 90% or higher. Cancer Council NSW’s research Cancer Council NSW is committed to research as key to understanding the causes of, and developing treatments for, cancer. We provided more than $120 million in funding to support research over the last 15 years. Under the tenure of the outgoing CEO, Dr Andrew Penman, research thrived and expanded at Cancer Council NSW, with our annual investment in research more than tripling since 1997, to just under $15 million in 2011/12. As a community-funded organisation, it is vital that this investment is dedicated to projects that positively impact the community. To ensure this, we bring community members to the decision-making table to help us decide which projects to fund. This sees us at the forefront of an important movement, where those suffering from cancer and researchers striving to control it can work together. Since 2005, every grant awarded by Cancer Council NSW has been assessed by patients, survivors and carers. Involving the cancer community in every funding decision ensures that we remain responsive to the priorities and needs of the community who fund us. 6 Research achievements Research into practice From unlocking the secrets to cancer cell immortality to developing new diagnostics, researchers funded by Cancer Council NSW have made many significant and exciting breakthroughs. Making sure that these research breakthroughs are translated into improvements for patients is a fundamental part of our work. Our funded researchers have developed two new treatments for brain and pancreatic cancer that target the power source of the cells, and could be 200 times more effective than current chemotherapy. New methods of targeting radiotherapy have been developed and the death rate from leukaemia has reduced. Researchers have begun to sequence the pancreatic and melanoma cancer genomes, and have also discovered how some types of bowel cancer are passed on in families. These findings build on hundreds of other discoveries into how cancer develops and spreads, and the best ways to detect and treat it. Many of Cancer Council NSW’s key internal research projects were established under Dr Penman’s leadership. Since 2006, the Cancer Lifestyle and Evaluation of Risk (CLEAR) Study has recruited close to 9,000 people to help understand the causes of cancer. ‘B Positive’, a project designed to enhance prevention and treatment of liver cancer, has documented the cost-effectiveness of liver cancer prevention; developed liver cancer treatment guidelines and a wide range of community resources; and established disease registries for hepatitis B and liver cancer. Our researchers were also the first to show just how significant the differences in mortality are between Aboriginal and non-Aboriginal Australians, particularly in breast and lung cancer. A significant addition to our funding portfolio over the last decade was the creation of Strategic Research Partnership grants, which aim to advance research with the potential to directly impact cancer control policy and practice. These allow Cancer Council NSW to actively partner with researchers to reduce the time between research discovery and real-world application. The research we fund and conduct has had a substantial impact on policies across the world. The work of our internal researchers on the human papillomavirus (HPV) vaccination for prevention of cervical cancer has changed vaccination and cervical screening policy in Australia, New Zealand, China and the United Kingdom. Research we funded into liver cancer has improved Australian screening policies and an investigation into radiotherapy has led to improved protocols being used as far away as Ireland and Canada. The research we fund and conduct has led to many significant achievements in the continuing fight against cancer. The benefits of this key investment speak for themselves: in 2012, Cancer Council NSW researchers estimated that more than 61,000 people are alive today who would have died from cancer during the last 20 years were it not for the lessons learnt from rigorous research. Our research strategy Our research strategy Cancer Council NSW has funded and conducted cancer research for more than 50 years. Our experiences and successes, and the collaborative relationships formed during this time, allow us to work strategically in the fight against cancer. Strategic thinking One of Cancer Council NSW’s Strategic Priorities is to drive major advances in research, ensuring no cancer is ignored. Our rigorous and transparent governance processes rely on the input of internationally recognised research leaders, as well as the community that funds us. This ensures that every dollar allocated to cancer research is invested in projects that are not only of the highest scientific merit, but are also of value to the community who support us. As we look to the future of research at Cancer Council NSW, our strategy will build upon our established solid foundations: • We will continue to combine rigorous scientific review with the judgements of our trained consumers to reach our funding decisions. • We will prioritise funding to tumour types and disadvantaged community groups which are under-resourced and underserved, and where clear inequities exist. • We will develop and nurture key research and funding collaborations, ensuring we can leverage our efforts against the efforts of all those who share our goals and objectives. • We will continue to systematically measure the benefit to the community of the research we support, ensuring that it makes a real difference, not only to scientific knowledge but also to the policies and clinical practices that shape the lived experience of cancer prevention, diagnosis, treatment and survivorship. • We will continue to strive for international ‘best practice’ research leadership, collaborating with those who can ensure that the research we fund will ultimately help us to achieve our vision of cancer defeated. Our international collaborations Our research capabilities and reach are also enriched by our international network, with hundreds of collaborations with academics, organisations, alliances and communities. Our internal researchers are contributing to ambitious and influential international projects, such as the InterSCOPE study into oesophageal cancer, the biobank stability study, and the skin health study. Our national and international collaborations enable us to extend our capabilities and accelerate breakthroughs in ways to prevent, diagnose, treat and manage cancer. Community involvement We are a community-funded organisation, so it is important that the community has a say in the research we fund. Cancer Council NSW ensures that cancer survivors and carers have input into every one of our research funding decisions, based on their understandings of which projects will best serve the community. They receive training to prepare them for this role, and their assessments are as important to our final funding decisions as those of the scientific panels who review each application. We thank each of our cancer consumers for their fundamental contribution to our funding process, as well as the many community members who assist our research projects. 90 % or higher survival rates for four of the most common cancers. 20 % drop in the risk of dying from cancer between 1997 and 2012. Cancer Council NSW Research Activity Report 2012 7 Who we are We are an independent and forward-thinking community of people, where ideas and charity come together to make a difference in the fight against all cancers. What we do By funding and conducting world-class research into prevention strategies and better treatments, as well as providing advocacy and support to those affected by cancer, we are working towards realising our vision of a society where lives are not cut short nor the quality of lives diminished by cancer. Our research We courageously prioritise previously underfunded areas of research, including pancreatic, oesophageal, liver, lung and brain cancer; and we judiciously invest in bold ideas with the potential to create significant impact. 8 We collaborate through partnerships with other funding bodies to create greater opportunities than a single organisation alone can achieve; and with leading researchers and institutions, recognising that researchers, policymakers, clinicians and service providers must unite to ensure the translation of research breakthroughs into real differences in cancer policy and clinical practice. Our financial independence ensures that we are accountable only to the cancer cause and the needs of our community, and can therefore support our Strategic Priorities and actively respond to research opportunities and needs. The rapidly evolving world of cancer research means we must be forward thinking to anticipate new discoveries and support the development of future breakthroughs. This is demonstrated by our longstanding and significant investment in cancer genetics and our commitment to long-term, population-based infrastructure studies, including our own Cancer Lifestyle and Evaluation of Risk (CLEAR) Study and the Sax Institute’s 45 and Up Study. Prevention “... You’re supposed to go home and get on with your life. How can you do that?” “I was a truck driver, working long hours, when a mole on my ankle started scabbing up and bleeding. The GP took one look at it and said it had to come out. Once melanoma gets more than 1mm deep it can get into the bloodstream, and mine was 1.95mm deep – they had to take out 14 lymph nodes from my groin plus some tissue from my stomach. I had 44 staples from my stomach all the way down to my thigh. Then I got the call – one lymph node was positive for melanoma. “We rushed our wedding through so we could have it before I started immunotherapy. My wife’s been my rock – she kept me on my feet. My melanoma was a result of my solarium use, and I don’t want other people to suffer what I have been through. Eight months after I was diagnosed, a friend of mine suggested I call Helpline. They eased my fears and put me onto support and advocacy groups. Cancer Council has played a big part in my journey, and I’m forever grateful for it.” Jay Allen Melanoma survivor and advocate Cancer Council NSW Research Activity Report 2012 9 Changing skin cancer prevention worldwide In a breakthrough that could dramatically reduce the number of skin cancers, Professor Diona Damian and Professor Gary Halliday have found that vitamin B3, a non-toxic and inexpensive vitamin, has a range of anti-cancer effects just by being rubbed into the skin or taken as a pill. The vitamin helps to reduce existing pre-cancerous skin lesions, reduced numbers of new non-melanoma skin cancers in a series of pilot studies, and may even help to prevent melanoma, one of Australia’s most deadly cancers. Lead researchers: Professor Diona Damian and Professor Gary Halliday, University of Sydney The need More than 60% of Australians develop skin cancer during their lifetimes – it is six times more common than all other forms of cancer combined. The vast majority of skin cancers rarely spread throughout the body, but if left untreated, they can cause extensive tissue destruction. Although they are less deadly than many other cancers, non-melanoma skin cancers are by far Australia’s most expensive cancer, with costs predicted to rise to more than $700 million by 2015. Sun exposure is the biggest risk factor for skin cancer: 90% of non-melanoma skin cancer and 65% of melanomas can be traced back to exposure to ultraviolet (UV) radiation from the sun. UV radiation causes cancer by damaging the genes of skin cells and by suppressing the immune system, which normally protects against skin cancer. 60 % of Australians develop skin cancer during their lifetimes. 6x more common than all other forms of cancer combined. 10 Achievements Professor Diona Damian and Professor Gary Halliday, from the University of Sydney, have made a remarkable discovery that could change skin cancer prevention worldwide. Both UVB (the type of light that is usually associated with sunburn) and UVA suppress the immune system when they hit the skin. This is important because the immune system is a big part of the body’s defence against cancer. Unusual cells, or cells that are growing incorrectly, are often targeted by the immune system and destroyed before they can develop into actual cancers. If the immune system is weakened, it means that the damage caused by sunlight isn’t repaired as quickly and is more likely to cause cancer. Vitamin B3 is protective because it replenishes cellular energy, helping cells to repair the damage caused to their DNA by sun exposure. This means that vitamin B3 could both protect against new skin cancers and also help heal existing sun damage. For example, actinic keratoses are pre‑cancerous lesions, normally appearing on chronically sun-exposed skin as red, scaling areas. If left untreated, many progress into non-melanoma skin cancer. The researchers found that applying vitamin B3 to the skin of people with these lesions accelerated their regression within a few months. They also found that simply taking a vitamin B3 supplement twice daily reduced the number of keratoses by 35% compared to people taking a placebo. But perhaps the biggest benefit from this discovery is the fact that vitamin B3 actually seemed to prevent new skin cancers (see Figure p.11). Of the patients taking a placebo, 32% developed a new skin cancer within 4 months. Of those taking the vitamin, only 8% did. Overall, there was an 80% reduction in numbers of new skin cancers in patients taking vitamin B3 in these Phase II studies. This substantial fall in cancers, thanks to a readily available vitamin, could dramatically change the number of people diagnosed with non‑melanoma skin cancer in Australia every year. The researchers are suggesting including it in sunscreen, especially because it helps to fight the adverse effects of UVA, which is less effectively blocked by normal sunscreen. The researchers have also found a number of other uses for vitamin B3. It helps to prevent the immunosuppressive effects of photodynamic therapy, which is often used for skin cancer treatment. This could boost cure rates after this therapy. It also reduces DNA damage after arsenic exposure, and could work to fight arsenic‑induced skin cancer. This is a major problem, affecting millions of people in areas like Bangladesh and West Bengal, where there are high levels of arsenic in the groundwater. Prevention Vitamin B3 may help to prevent melanoma. 50 % of non-melanoma skin cancer could be prevented. The most exciting aspects of this research may be yet to come. Comprehensive testing of the effects of vitamin B3 on skin cancers is ongoing. Professor Damian is working to complete a Phase III trial of its effects in preventing non‑melanoma skin cancer in 400 people at high risk of developing it. This trial is currently in the final stages of recruitment, with more than 300 participants enrolled to date. This multicentre study will provide enough evidence to show whether the vitamin should be recommended for all people at high risk of skin cancer. Until the Phase III trial is complete vitamin B3 is not recommended for the prevention of skin cancer. Preliminary results of this research have also shown that vitamin B3 may help to prevent melanoma, by helping melanocytes in the skin to repair their DNA more efficiently after UV exposure. This could potentially greatly improve the number of lives saved, as melanoma is by far the most deadly of the skin cancer types. If the non-melanoma skin cancer trial is successful, the next step will be the development of a clinical trial to test whether vitamin B3 can also prevent melanoma. The effect of vitamin B3 on skin cancers 25 20 Number of cancers Future work 15 10 5 0 Placebo Vitamin B3 Oral vitamin B3 given to 37 heavily sun-damaged patients significantly reduced the number of new skin cancers. Impact Australia has the highest incidence of skin cancer in the world. If, as the researchers estimate, including vitamin B3 in sunscreen could prevent 50% of non-melanoma skin cancers, this research has the potential to dramatically improve skin cancer prevention. It can also help to heal existing pre-cancerous lesions, and may even prevent melanoma and arsenic-induced skin cancer. Research team: Dr Andrew Chen, Dr Devita Surjana, Dr Benjamin Thompson, Dr Georgia Frost, Dr Sula Thanos, A/Professor Fergal Moloney, Dr Joohong Park, Dr Geetha Sivapirabu, Dr Eleni Yiasemides, Dr Malene Vestergaard, Dr Clare Patterson, Professor Ross Barnetson, Dr Anne Kricker and Dr Andrew Martin, University of Sydney; Dr Patricia Lowe, A/Professor Josette Eris and Mr Branko Radojkovic, Royal Prince Alfred Hospital Disclaimer: Information in this article is not meant to replace medical advice. As vitamin B3 is still being tested in clinical trials, we do not currently recommend it as a cancer prevention measure. Cancer Council NSW Research Activity Report 2012 11 Prevention Making healthy food choices the easiest choices Obesity rates are on the rise in Australia, putting more people at risk of developing obesity-related cancers. To help combat this, Cancer Council NSW researchers are investigating new labelling systems for food, and scrutinising the fast food industry by analysing its products, nutrition information and marketing practices. This can help Australians to make healthy choices and reduce levels of obesity and chronic disease. Lead researchers: Lyndal Wellard and Wendy Watson, Cancer Council NSW The need More than half of Australian adults are overweight or obese, increasing their risk of heart disease, type 2 diabetes and cancer. There is convincing evidence that overweight and obesity are risk factors for cancers of the bowel, kidney, pancreas, oesophagus, endometrium and breast. Obesity has overtaken smoking as the leading cause of premature death and illness in Australia. Healthy food choices are an essential part of combating rising obesity levels. Currently, reliable nutrition information and ingredients lists appear in fine print on the back or the side of food packages, while nutrition claims such as ‘97% fat free’ and ‘no added sugar’ appear prominently on the front – grabbing consumers’ attention. Fast food also has a big part to play in obesity, with research showing that we are increasingly eating away from home and that eating fast foods regularly can lead to weight gain. Achievements Cancer Council NSW has investigated multiple ways to improve food packaging to make it easier to identify healthier choices. Our researchers have conducted a number of studies to demonstrate to policymakers that adding simple nutrition information to the front of food labels will influence the choices people make. Our 2012 study asked 4,357 grocery shoppers to use a range of labelling systems to identify healthier foods. Those packs without front-of-pack labelling did not rate as well as those with information about sugar, fat and sodium. This research has informed Cancer Council’s advocacy to develop an effective front-of-pack labelling system. With Australians spending almost one-third of their household food budget on eating out, researchers also looked at the healthiness of fast food meals. Not surprisingly, fast food meals made for children were generally unhealthy, often exceeding the recommended levels of energy (kilojoules), saturated fat, sugar and sodium for both 4- and 8-year old children. Alarmingly, some meals exceeded a 4–8-year-old child’s recommended sodium and saturated fat intake for an entire day. No meals containing a cheeseburger were rated a healthy choice, despite being the default in many fast food children’s meals. Another study looked at the popularity of meals promoted as ‘healthy’ choices at one major fast food chain. Few people actually chose these healthier options, with less than 1% of the 1,448 meals observed being healthier selections. Given that consumers do not purchase the one or two items that are offered as ‘healthy’ choices, the next step is to see firm commitment from both industry and government to reformulate standard menu items to make them healthier. Less than 1% of the 1,448 meal choices observed were healthy options. Impact Cancer Council NSW uses this research to persuade the Government to act to reduce the impact that unhealthy food and the food industry have on chronic diseases and obesity rates in Australia. Our advocacy in this area aims to improve people’s ability to make healthy choices in the supermarket and when eating out. Cancer Council NSW sits on a working group that is advising Federal and State Health Ministers about the best food labelling system to implement - with our research demonstrating that front-of-pack labelling has a clear benefit to the public. Research team: Clare Hughes, Kathy Chapman and Colleen Glasson, Nutrition Unit, Cancer Council NSW; Dr Bridget Kelly, School of Molecular and Bioscience, University of Sydney; Dr Debra Hector and Lesley King, Prevention Research Collaboration, University of Sydney; and Jennifer Crawford and John Sergeant, Curly Questions, Sydney 12 Addressing liver cancer Over the last three decades, liver cancer diagnoses have steadily risen, bringing this cancer into the top 10 causes of cancer deaths – a trend which is expected to continue beyond 2020. As infection with the hepatitis B or C viruses are the key causes of liver cancer, Australians born in countries where these infections are endemic bear the brunt of this disease. Fewer than 1 in 5 people are alive five years after a liver cancer diagnosis, so researchers focus on disease prevention and early detection to improve these dismal statistics. Lead researchers: Professor Jacob George, Westmead Millennium Institute; and Dr Monica Robotin and Mamta Porwal, Cancer Council NSW The need Deaths from liver cancer are increasing faster than any other cause of cancer death in Australia, yet these deaths are largely preventable. The key causes of liver cancer are infections with the hepatitis B or C viruses, which are preventable and treatable. Despite the fact that hepatitis B increases the risk of liver cancer by more than 200 times, and is treatable, it is estimated that only 65% of infected people know that they have the disease. So far, more than 600 patients are being followed up in the liver cancer Registry. Achievements Cancer Council NSW has funded both the ‘B Positive’ Program and a Strategic Research Partnership grant to better understand liver cancer and hepatitis B, and to improve their diagnosis and treatment. To achieve this, researchers and clinicians work on a range of projects. They have developed liver cancer treatment guidelines, assisted clinicians in managing liver cancer, and helped establish Westmead and Royal Prince Alfred hospitals as centres of excellence for managing this disease. As a direct result of this program, more than 600 people are being followed up in the liver cancer Registry, and more than 500 have their hepatitis B infection followed up according to clinical guidelines, to prevent disease complications. The majority of people infected with hepatitis B are from non-English speaking backgrounds. Therefore, developing a variety of culturally appropriate information resources and engaging with these communities are critical to disease prevention. The ‘B Positive’ Program delivers community talks and programs in a number of relevant languages, and has developed a range of in-language audiovisual resources – such as a hepatitis B ‘travelling library’, flip charts, videos, cartoons, posters and flyers – demystifying the disease and explaining strategies for disease prevention. In the coming year, researchers will work to identify the information needs of people affected by liver cancer as a step towards developing relevant resources to address these needs. Impact This program directly helps to prevent liver cancer by educating communities, promoting screening programs, and identifying those at high risk of liver cancer. With many hundreds of people screened and treated as part of this effort, and through awareness-raising in high-risk communities and among their treating clinicians, we have real potential to reduce the impact of this largely preventable cancer. Research team: Debbie Nguyen, Anne Fraser and Ximena Masgoret, Cancer Council NSW Cancer Council NSW Research Activity Report 2012 13 “I’d never been a hypochondriac, but now whenever I get a little cough or stomach pains, I think, ‘This is it’.” “I’d just had twins when I was diagnosed with cervical cancer. I remember pushing the stroller down the street, screaming, ‘No, no!’ in my head, while trying not to show the kids. People refer to it as a battle; that you’re a fighter, but you’re not really. You’re feeling very helpless. “Then, the same year, one of my boys was diagnosed with leukaemia. That was shattering. Though the Children’s Hospital was spectacular – because I was worried that one twin was getting more attention than the other, they’d treat them both the same, giving pretend X-rays and blood tests; even a pretend lumbar puncture. He made it, and I’m so thankful for the amount of research done into cancer. Twenty years earlier, my child might not have survived. You just can’t be grateful enough.” Robyn Bransby Cervical cancer survivor 14 Diagnosis Cancer Council NSW Research Activity Report 2012 15 Diagnosis Better cervical cancer screening Cervical cancer screening with Pap tests has been in place for many years in most developed countries. However, new vaccines for the human papillomavirus (HPV, the virus that causes cervical cancer) have changed the prevention landscape. In 2012, Cancer Council NSW’s Cancer Modelling Group made important discoveries in their assessments of various options for cervical screening and diagnosis. They estimated that cervical screening cost $195 million in 2010 in Australia alone, and found that HPV testing for women who have had pre-cancerous lesions removed is likely to improve outcomes. By looking at differences in screening uptake and outcomes for migrant women, the researchers also identified areas where screening could still be improved. Lead researcher: Associate Professor Karen Canfell, Cancer Council NSW/University of New South Wales The need Thanks to the success of Pap test screening programs in many developed countries, cervical cancer is no longer the scourge it once was, although it is still one of the most common cancers in women in the developing world. However, the introduction of HPV vaccination changes the landscape for cervical cancer prevention. Cervical screening is being re-evaluated to take account of these changes in order to ensure that screening and vaccination work together as complementary preventative mechanisms. At the same time, HPV testing, which can be used at different points in the screening and diagnostic pathway, requires further evaluation. Cervical cancer is no longer the scourge it once was, although it is still one of the most common cancers among women in the developing world. 16 Achievements Cancer Council NSW researchers, led by Associate Professor Karen Canfell, have a comprehensive research program that investigates the outcomes and cost-effectiveness of different screening options for cervical cancer. The researchers use mathematical models to predict the effects of various future scenarios for cervical screening and HPV vaccination. These tools are then used to answer questions such as ‘How often should women be screened for cervical cancer?’ and ‘What is the most effective and cost-effective way to prevent cervical cancer?’ One of the group’s most important contributions in 2012 was to evaluate HPV testing for the surveillance of women following treatment for pre-cancer of the cervix. Previously in England, women were screened every year for 10 years after treatment of pre-cancerous lesions. Using data from 6 sites across England, they found that this traditional method led to 29 cases of recurring lesions per 1,000 women treated, while using the new HPV test led to 8 fewer recurring lesions. In addition, HPV testing was also more cost-effective, because this test is better at detecting those at risk of the disease recurring. The researchers found that this could save approximately £9,388 per 1,000 women treated, and would also result in fewer unnecessary medical examinations. These findings, along with the results of pilot site evaluation, have helped inform policy change in England. With the collaboration of Professor Bruce Armstrong at the University of Sydney, a PhD student in the Modelling Group, Nayerreh Aminisani, also conducted two studies looking at cervical screening in migrant women. The first found that migrant women from Asian and Middle Eastern countries are less likely to participate in cervical screening. However, the second study found that most (but not all) groups of migrant women experienced a reduction in cervical cancer since screening was implemented in 1991. The researchers surmise that the results for those groups who did not appear to benefit from the organised screening program in Australia may be explained by a recent rise in migration from countries with high rates of cervical cancer. Together, the findings reinforce the importance of addressing barriers to screening in migrant groups. Associate Professor Karen Canfell’s work in modelling cervical cancer prevention began at the University of Oxford and continued at Cancer Council NSW for seven years, from 2005 to 2012. Associate Professor Canfell and her team of 10 researchers have now relocated to the Lowy Cancer Research Centre at the University of New South Wales, where they continue their work. We wish them well in their future endeavours and look forward to continuing collaborations. In 2010 the cost of the National Cervical Cancer Screening Program was $195m Finally, the team estimated just how much Australia’s current cervical cancer screening program costs. Their study revealed that the National Cervical Cancer Screening Program cost $195 million in 2010, with half of this cost related to delivery of routine screening tests. These estimates are a benchmark for future assessment of the screening program, and will help to determine how changes to the screening program (prompted by the introduction of the cervical cancer vaccination) might affect costs in Australia. “Modelling is a key factor in our ability to best use the cancer resources available in our community. Our cervical cancer modelling has already opened the door to a wide range of opportunities to improve cancer prevention here and around the world.” – Associate Professor Karen Canfell. Cytology testing vs. HPV testing for detecting recurrent pre-cancers after treatment Predicted cases of pre-cancerous lesions (per 1,000 women treated) Demonstrating the international collaborations that make Cancer Council NSW a thriving research hub, the researchers have also undertaken a number of studies into cervical cancer in China. The most recent piece of research estimated the aggregated costs associated with cervical cancer screening, diagnosis and treatment in rural China. Due to economies of scale, diagnostic costs were similar to screening costs when the numbers of people being screened were high, but when they looked at smaller numbers of people the diagnostic costs increased. The study’s findings will help cost-effectiveness evaluation and budget planning for cervical cancer prevention initiatives in China. 30 25 20 15 10 5 0 0 1 2 3 4 5 6 7 8 9 10 Time since treatment (years) Cytology only follow-up HPV testing: sentinel sites Extended HPV follow-up protocol Reference: Legood R et al. BMJ 2012;345:bmj.e7086 Impact The work of the Cancer Modelling Group continues to directly influence policy decisions in cervical screening in several countries. Improving our understanding of screening rates in migrant communities, as well as how much screening costs, will help to inform policy and guidelines in the future. Research team: Megan Smith, Jie-Bin Lew, Robert Walker, Ming Xu, Dr Kate Simms, Dr Michael Caruana, Yoon Jung-Kang, Jessica Darlington-Brown and Luke Testa, University of New South Wales Cancer Council NSW Research Activity Report 2012 17 Treatment “Nearly every Aboriginal person I speak to knows someone that’s got cancer or died from cancer.” “I’ve had two aunts on dad’s side and three on mum’s side die of cancer. There’s always been cancer there, but you never think about it. My dad has cancer and he’s in denial – I was there when he was told and he just said to the doctor, ‘I haven’t got that dirty disease that killed my sisters’. But he does. “People have no idea what a lot of Aboriginal people have to deal with in their own country. I really believe we need more black faces in the cancer arena and more culturally appropriate ways to access the services. I’m so happy that Cancer Council is doing this research and that we’re finally getting somewhere. There’s a long way to go, but at least something’s happening for our people.” Veronica Saunders Community Liason Officer 18 Understanding the gap in Aboriginal cancer survival Cancer is the second most common cause of death for Aboriginal people, and they are 60% more likely to die from their cancer than non-Aboriginal Australians. Cancer Council NSW researchers are investigating how to close this gap. They have found evidence that there may be barriers preventing Aboriginal people from receiving the best care, and that more research is required to fully understand these barriers and to close the gap between Aboriginal and non-Aboriginal cancer outcomes. Lead researchers: Professor Dianne O’Connell and Raj Supramaniam, Cancer Council NSW The need In 2006, Cancer Council NSW researchers found that Aboriginal people were 60% more likely to die from cancer compared to non-Aboriginal people. Exactly why this difference exists and what can be done to reduce it are the issues that the Aboriginal Patterns of Cancer Care (APOCC) team is investigating. Aboriginal people were less likely to receive surgery, which might contribute to poorer outcomes. Achievements Following this pioneering work comparing Aboriginal and non‑Aboriginal cancer death rates, Cancer Council NSW researchers released results in 2012 relating to prostate cancer, breast cancer, colorectal cancer and non-small cell lung cancer – some of the most common cancers in Australia. For each study, the researchers examined the cancer survival rates of Aboriginal people compared to non-Aboriginal people, and looked into why these differences existed. For all four cancers, Aboriginal Australians had lower survival rates than non-Aboriginal Australians. However, the exact reasons for this were difficult to identify. Some problems identified could be the source of some of the differences for specific cancer types. For lung cancer and breast cancer, Aboriginal people were less likely to receive surgery, which might contribute to poorer outcomes. Yet by contrast, Aboriginal people with bowel cancer were just as likely to receive surgery, but were still 30% more likely to die from their disease. For prostate cancer, even after the researchers accounted for a range of additional factors, including surgical treatment, location and socioeconomic disadvantage, Aboriginal men were still 45% more likely to die from their cancer. Further research is required into factors such as follow-up after surgery, access to coordinated care, and the impact of other diseases limiting cancer treatment options. The researchers have already begun new research projects to learn more about these reduced survival rates for Aboriginal people with cancer. One investigation is the Pathways to Diagnosis Study, which is looking at the lives and healthcare of Aboriginal people in the lead-up to a cancer diagnosis. Impact The discovery that, compared to non-Aboriginal Australians, Aboriginal people diagnosed with prostate cancer, breast cancer, colorectal cancer or non-small cell lung cancer all have significantly lower survival rates has highlighted the pressing need for better access to cancer care for Aboriginal people to help close this gap. Cancer Council NSW is now extending its reach into Aboriginal communities to work with healthcare providers and community groups to further advance this research and support the implementation of solutions. Research team: Professor Phyllis Butow and Mr Anthony Dillon, University of Sydney; Professor Bruce Armstrong, Royal Prince Alfred Hospital; Professor Carla Treloar and Dr Christy Newman, University of New South Wales Cancer Council NSW Research Activity Report 2012 19 Treatment Radiation’s effects on neighbouring cells By identifying a better way to use radiotherapy machines to treat cancer, Associate Professor Natalka Suchowerska and her team have found a way to improve the quality of life of patients. They discovered that cancer cells hit with radiation communicate with the cells around them, affecting the outcome of radiotherapy. This means they can design a better way of administering radiotherapy using equipment already found in hospitals across the world. Lead researcher: Associate Professor Natalka Suchowerska, University of Sydney The need Radiotherapy is a common cancer treatment and uses high-energy beams of radiation to blast tumour cells, while avoiding and sparing normal tissue. Current radiotherapy techniques assume that only cells that have been directly hit by the radiation will be killed. Previous work by Associate Professor Suchowerska and her team discovered that the likelihood of a cancer cell dying is also influenced by damage to neighbouring cells. 20 % more cancer cells can be killed with the same dose of radiotherapy given in 5 minutes, instead of 20 minutes. Understanding this ‘bystander’ effect is essential to improving radiotherapy techniques and minimising its side-effects. Achievements Building on their earlier work, the researchers discovered that up to 40% of cell death from radiation might be due to bystander signalling, but the effect isn’t as straightforward as they thought. Being next to an irradiated cell has two opposite effects on the surrounding cells – it can help them grow or cause them to die, even if the bystander cells weren’t actually hit by radiation at all. Crucially, this outcome is determined by how the radiation was administered and the time since the treatment. These researchers have determined how much irradiated cells communicate to the surrounding cells, and how treatments are affected. Armed with this knowledge, they developed a new mathematical model that can predict the most effective way to administer radiotherapy treatment. This new model will allow for the maximum effect on a tumour with the minimum of side effects. Another of their key findings is that giving the same amount of radiotherapy in a shorter period of time can be much more effective. For instance, the same dose of radiotherapy given in 5 minutes, rather than the traditional 20 minutes, can kill 20% more cancer cells. This research could make a substantial difference to patients undergoing radiotherapy. The radiotherapy machines currently in use in Australian hospitals can rapidly deliver extremely complex dose distributions, but weren’t being used at their full capacity, because accurate models of what would happen did not exist. This research means that clinicians are able to tailor treatment dose rates and distributions, making more effective use of existing radiotherapy machines and improving patient quality of life. Follow up research is now investigating how bystander signalling applies to other types of radiation treatment, in the hope that other radiotherapy techniques can be improved. Impact This research has changed our understanding of tumours’ response to radiation with a direct impact on radiotherapy techniques across Australia and around the world. The experimental protocols the researchers developed have been utilised internationally, most notably by the Queen’s University Belfast in Ireland. This research has also been awarded several prizes including the Institute of Physics and Engineering in Medicine Roberts Prize for best paper in Physics in Medicine and Biology, and the Australasian College of Physical Scientists and Engineers in Medicine Omega Prize. Research team: Professor David McKenzie, University of Sydney; A/Professor Martin Ebert, Sir Charles Gairdner Cancer Centre; Ms Elizabeth Claridge, Dr James Bewes and Mr Atirak Taychasiraprapakul, Royal Prince Alfred Hospital 20 New invention simplifying radiotherapy treatment verification A new technology developed by researchers at Liverpool Cancer Therapy Centre and the University of Sydney has the potential to improve the safety and effectiveness of radiotherapy. Dr Philip Vial has invented a new detector that can track the exact location and dose of radiotherapy as it is being delivered, substantially improving the accuracy of the treatment. Lead researcher: Dr Philip Vial, Liverpool Cancer Therapy Centre The need External beam radiotherapy, used to treat up to 50% of cancers worldwide, must be very accurate in both the position and quantity of the dose delivered. Too much or too little radiation, or a beam in the wrong place, can reduce the effectiveness of the treatment and cause significant side effects. This makes it essential to verify that the treatment is accurate, especially as radiotherapy becomes increasingly complex. At the moment, clinicians can track where the radiation hits, but can’t confirm exactly how much radiation is delivered. Achievements This research group, led by Dr Philip Vial, has developed a new technology to solve this issue. They have invented a next-generation detector, which can accurately detect both how much radiation is delivered during a radiotherapy session, and where it is delivered. Preliminary experiments using a prototype detector have demonstrated its effectiveness, with excellent performance as a dosemeasuring device and promising performance in detecting location. This will not only improve patient safety by helping to prevent errors in treatment, it will also allow for the correction of inaccuracies in treatment that currently go undetected. One of the most important aspects of this device is its broad scope – it can be used to assist with any radiotherapy treatment, regardless of the complexity or the aim of the therapy. detection methods, but it may have further applications. As one of the most sophisticated detector models of its kind in the world, it has already shed new light on the physics behind existing radiotherapy machines. Research is ongoing, and based on these encouraging results, the research team is building a second prototype, which they hope to test in 2013. As one of the most sophisticated detector models of its kind in the world, it has already shed new light on the physics behind the existing machines. The researchers are also working on a computer model of radiotherapy which could improve the way current treatments are delivered. The initial aim of the model is to test whether the new detector is significantly better than the existing radiotherapy Impact A new invention that improves radiotherapy techniques has the potential to help many thousands of radiotherapy patients a year in Australia alone. As this can apply to all radiotherapy treatments, no matter how complex, it can improve the safety of advanced radiation therapy across a range of cancers. The modelling work has already delivered significant insights into how existing radiotherapy detectors work, and has the potential to underlie further discoveries as it is more widely applied. Research team: Dr Lois Holloway, Dr Samuel Blake, Dr Aimee McNamara and A/Professor Zdenka Kuncic, University of Sydney; A/Professor Peter Greer, University of Newcastle; Professor Michael Barton, University of New South Wales Cancer Council NSW Research Activity Report 2012 21 Treatment One treatment discovery impacting two cancers A new drug that may slow tumour progression by 50% has been identified by Dr Tao Liu at the Children’s Cancer Institute Australia for Medical Research. This drug, which may be able to treat both pancreatic cancer and neuroblastoma, works by targeting a protein that encourages cancer cells to grow and spread. Lead researcher: Dr Tao Liu, Children’s Cancer Institute Australia for Medical Research The need Pancreatic cancer and neuroblastoma are both devastating diseases. Pancreatic cancer is the fourth leading cause of cancer death in adults, and neuroblastoma is the most common solid tumour of early childhood. What ties these cancers together is that many of them are partially caused by the same protein, called Myc oncoprotein. Myc helps the cancers grow and spread throughout the body by accelerating the rate at which the cancer cells divide. Although the role of Myc in cancer has been known for some time, researchers have had little success in targeting it to stop cancers from growing. Achievements Dr Liu and his team have discovered a new way of reducing the amount of Myc in cells by targeting a different, related protein. This prevents the cancer from spreading, and could have important implications in the treatment of these cancers. The researchers found another protein, called SIRT, which increases the amount of Myc. By creating a new drug that blocks SIRT, the researchers were able to reduce the amount of Myc, which stopped the cancer from growing. These new drugs reduced the amount of Myc in all the cancer cell lines in which they were tested, and had a remarkable effect. Treating cancers caused by Myc with these new drugs reduced the extent of tumour progression by approximately 50%. In addition, the researchers have shown that the drugs partially prevent cancers from developing in the first place. Interestingly, the new drugs had another effect – increasing the amounts of two other proteins (called MKP3 and NEDD4). As low levels of these proteins are known to be related to poor outcomes for neuroblastoma patients, this is a good sign that the drugs could improve the lives of those diagnosed with this type of cancer. Building on this significant breakthrough, the important next step is to create a version of the drug that is suitable for therapeutic use in cancer patients. 50 % reduction in the amount the tumours progressed. Impact Given the dangerous nature of both pancreatic cancer and neuroblastoma, the creation of a new drug that may slow their progression by 50% is a remarkable discovery. There is further hope that the drug may be able to help prevent these cancers in the first place, which could improve treatments for the thousands of people diagnosed with these cancers every year. With a few modifications, the researchers hope to test these drugs in clinical trials in the near future. Research team: Professor Andrew Biankin and Dr Chris Scarlett, Garvan Institute of Medical Research 22 Survivorship “The post-operative pain means I’m reminded of my cancer every day.” “In January 2012, I found a lump under my jaw, like a pea under my skin. After all available tests, the doctors said that it was the secondary cancer, and that there was no sign of the primary. I started to get very concerned, thinking, ‘How can they treat my cancer correctly if they don’t know where it is?’ “It’s classified as cancer of unknown primary, or CUP. It’s difficult – if you have been diagnosed with breast or lung cancer, you can picture where it is, but with CUP the cancer could be anywhere so you have no idea what to picture. My friends ask me when I will be in remission and the honest answer is probably never, because they haven’t found all the cancer. There’s a great need for more awareness, support and funding for CUP, and I want to help others get through it.” Robyn Wagner Cancer of unknown primary survivor Cancer Council NSW Research Activity Report 2012 23 Survivorship Supporting those faced with the unknown With the help of a grant from Cancer Australia, Cancer Council NSW researchers created a project to better understand the unique experiences of people affected by cancer of unknown primary, and the support and information they most need. Using insights gained from this project, the researchers developed resources designed to inform, empower and provide hope to those affected by this cancer. Lead researchers: Gillian Batt, Amelia Beaumont, Helen Gooden and Kath Skinner, Cancer Council NSW; and Associate Professor Penelope Schofield and Dr Anna Ugalde, Peter MacCallum Cancer Centre The need Cancer of unknown primary, or CUP, is cancer that has spread from somewhere in the body other than where it is found at diagnosis, and where the location of the primary cancer cannot be identified. By definition, it is a diagnosis of advanced cancer. Knowing where the cancer started can be important to help decide the appropriate therapy that should be used. CUP is the seventh most common cause of cancer deaths in NSW, and although there are exceptions, it generally has a poor prognosis. Before this project was conducted, information and support resources specifically designed for people affected by CUP were virtually non-existent in Australia. Achievements To fill this gap, a team of Cancer Council NSW researchers worked with colleagues from the Peter MacCallum Cancer Centre, the Flinders Medical Centre, the University of Sydney, the University of New South Wales and the University of Newcastle to carry out both phone interviews and surveys with CUP patients and carers. This research provided vital insights into the experience of people affected by a CUP diagnosis, and their information and support needs. The team then worked closely with health professionals who treat CUP patients to develop a suite of information and support resources, including a booklet; a dedicated CUP information webpage; a space created for a CUP online community to provide peer support via the Cancer Connections website; and a DVD and online video resources. The DVD consists of four related videos that draw on the remarkable insights gained through the interviews of patients and carers. The themes identified in the research led directly to the content of the videos. They provide information about the diagnosis, prognosis, intent of treatment, and lived experience of those affected by CUP, and explain how people can access a range of support and information. Patient and carer stories are featured heavily, because research has shown that people learn not only from their own experiences, but also by observing the actions of others and the results of those actions. These videos are available free‑of‑charge in a variety of formats to make sure that they are available to those who need them. Before this project was conducted, information and support resources specifically designed for people affected by CUP were virtually non-existent in Australia. Impact Thanks to this research project, CUP patients and carers now have dedicated resources to help them understand that they are not alone in facing this difficult diagnosis. An online community gives patients and carers a place to connect and receive support from people in similar situations; and the booklet, video and online resources provide information and stories specific to this cancer. Previously, resources of this kind were virtually non-existent, making this project even more important. Research team: Professor Sanchia Aranda, Cancer Institute NSW; Ms Jane Barrett, consumer representative; Ms Nadine Hackl, Cancer Institute NSW; Dr Chris Karapetis, South Australia; Dr Sylvie Lambert, University of Newcastle; Dr Monica Robotin, Cancer Council NSW; Professor Martin Tattersall, University of Sydney; and A/Professor Claire Vajdic, University of New South Wales 24 The factors influencing prostate cancer outcomes With the rate of prostate cancer having rapidly increased in the last decade, Cancer Council NSW researchers have developed a comprehensive program investigating a range of factors influencing patient outcomes. This research includes looking at the link to sun exposure, examining the use of complementary therapies, and investigating whether the adverse side effects of treatment outweigh the benefits. Lead researcher: Associate Professor David Smith, Cancer Council NSW The need Prostate cancer is now the most common cancer in Australia (aside from non-melanoma skin cancer), with Cancer Council NSW research recently predicting that the number of men living with prostate cancer will more than double in a decade. This will place a substantial burden on the health system, and makes research into better prevention and treatment all the more important. 5x Men who spent more time in the sun on weekends had up to 5 times greater risk of prostate cancer. Achievements To meet the needs of this growing number of patients, researchers at Cancer Council NSW, led by Associate Professor David Smith, are working on a program of research to improve the understanding and prevention of prostate cancer, as well as treatments for the disease. In one investigation, researchers have shown that high sun exposure – in addition to increasing the risk of skin cancer – may also increase the risk of prostate cancer. After looking at the records of more than 1,000 men with prostate cancer, they found that men who spent the most time in the sun on weekends had up to five times greater risk of prostate cancer than men with the least sun exposure. Other studies suggest that too little sun exposure can also be harmful – so, as is often the case, the key is moderation; and further investigation is required to clarify the risks. Another study found that long-term survivors of prostate cancer often turn to complementary or lifestyle therapies. This work showed that up to one quarter of survivors used dietary supplements and modifications, meditation, prayer, and/or exercise changes to help manage their cancer. However, those who do use these therapies tend to be at opposite ends of the spectrum: either anxious about their disease, or confident that they can control their cancer. If doctors discuss the use of these therapies with their patients, they are more likely to identify men who are anxious and may benefit from counselling, and help those with more confidence to make additional healthy lifestyle changes. A further piece of research investigated the difficult question of how much treatment is too much? Prostate cancer grows very slowly, and for some men the side effects can outweigh the benefits of the treatment. Deciding on treatments is difficult, as patients want increased probability of survival, but don’t want to endure diminished quality of life during this time. After interviewing men with prostate cancer, the researchers found that incontinence, bowel problems and erectile dysfunction were the side effects that most affected patients although this depended on the severity of the illness. With further research, this knowledge will develop a shared decision-making model for doctors and their patients, acknowledging the impact of treatment on the quality, as well as duration, of their survival. Impact By influencing how men are treated for prostate cancer, this research will increase the quality of life of patients and more accurately characterise the likely outcomes. Helping doctors to more effectively weigh up the benefits and side effects of treatment will prevent unnecessary trauma for patients; while identifying patients in need of counselling will help combat the devastating mental toll of the disease. Research team: Dr Visalini Nair-Shalliker, Professor Dianne O’Connell, Suzy Hughes, Sam Egger, and Albert Bang, Cancer Council NSW; Professor Bruce Armstrong and Professor Madeleine King, University of Sydney Cancer Council NSW Research Activity Report 2012 25 Staff Staff Research Strategy Unit Cancer Research Division Kathy Chapman, BSc, MNutrDiet Director, Health Strategies Division A/Professor Freddy Sitas, BSc, MSc(Med), MSc(Epidemiology), DPhil Director, Cancer Research Division Dr Libby Topp, BSc(Psychol)(Hons1), PhD Manager, Research Strategy Unit Dr John Williams, BSpSc, MPH, PhD Research Governance Officer Sam Thorp, BCom/BSc(Hons1) Research Communication and Community Engagement Officer Nicci Bartley, BPsych(Hons) Project Officer Jane Bennett Volunteer Naomi Crain, BA, AdvDipFamTh Executive Assistant to Director Kate Christian, BSc Operations Manager Professor Dianne O’Connell, BMaths(Hons 1), PhD Division Manager and Senior Epidemiologist A/Professor Karen Canfell, BE(Hons), DPhil Senior Research Fellow A/Professor David Smith, BA, MPH, PhD Research Fellow ‘B Positive’ Program Dr Marianne Weber, BA(Hons), PhD Research Fellow Dr Monica Robotin, MBBS, FRACS, MBA, MIH, MAppEpid Medical Director Dr Xue Qin Yu, MPH, PhD Research Fellow Mamta Porwal, BHMS, MPH Project Coordinator Ximena Masgoret, GDipOphth Research Assistant Yumi Patton, MBiostat Research Assistant Annie Fraser, BSc Hepatitis B Community Educator Debbie Nguyen, BHlth Hepatitis B Community Educator Dr Michael Caruana, BSc, DPhil Post-doctoral Research Fellow Dr Carolyn Nickson, BA, GDipEpidBiostats, PhD Post-doctoral Research Fellow Dr Ju Fang Shi, MD, MPH, PhD Post-doctoral Research Fellow Dr Kate Simms, BSc(Hons), PhD Post-doctoral Research Fellow Dr Louiza Velentzis, BSc(Hons), MSc, PhD Post-doctoral Research Fellow Dr Eleonora Feletto, BBus/BA(IntlStudies), DPhil Post-doctoral Research Fellow Dr Visalini Nair-Shalliker, BSc(Hons), MSc, MPH, PhD Post-doctoral Research Fellow Program Managers Megan Smith, BE, MPH(Merit) Program Manager – Cancer Modelling Rajah Supramaniam, BSc, MPH(Hons) Program Manager – Aboriginal Studies Verity Hodgkinson, BSc, MSciMan Program Manager – Biobanking Katie Armstrong, BAppSc(HIM) Research Data 26 Statisticians Research Assistants Albert Bang, BCom Maria Albania, BSc/BEd Sam Egger, BSc, MBiostat Karen Allison, BBehavHlthSc Alison Gibberd, BSc(Hons), MStats May Chiew, BPharm, MHP(Professional Practice) David Goldsbury, BSc(Hons), MPH(Merit) Devisri Dharmaraj, BTech, MBiotech Qingwei Luo, BSc, MAppStats Bonnie Nixon, BMedSc Project Coordinators Geane Sharman Kate Blacker, BSc(Nurs) Susan Spratley, BPsych(Hons) Leighna Carmichael, BA, MSc Administration Jessica Darlington-Brown, BSc(Population Health), MPH Pinya Leeder, BA, MProfAcct Suzanne Hughes, BSc(Hons), MNutrDiet Elle McGlynn, BA Clare Kahn, BMus(Hons), MMus(Perf) Brodie Clarke, BPubHealth Michael Revius, BSc Annelouise Wells Jenny Rodger, BA(Hons), MSc Postgraduate Students Data Managers Nayerreh Aminisani, BSc(Nurs), MSc(Epid), PhD (awarded 2012) Sarsha Yap, BSc(Hons) Johnson Yuan, BSc, BEd(Teach) Research Programmers Jie Bin Lew, BSc(Bioinformatics) Robert Walker, BSc Ming Xu, BEng(Mech)(Biomed), BMedSci Laboratory Manager Janis Jansons, BSc, MSc Aboriginal Community Liaison Officer Veronica Saunders APOCC Communications Coordinator Leonardo Simonella, BA, MPH, PhD (awarded 2012) Yoon-Jung Kang, BA, MPH(Hons), (PhD candidate, submitted 2012) Qingwei Luo, BSc, MAppStats, (PhD candidate) Usha Salagame, BSc(Microbiol), PostgradCertBioinformatics, MSc(Biotech), (PhD candidate) Maria Albania, BSc/BEd, (MBiostats candidate) Albert Bang, BCom, (MBiostats candidate) Jie Bin Lew, BSc(Bioinformatics), (MPH candidate) Elle McGlynn, BA, (MBA candidate) Joanna Jarrald, BA(Hons)(Comm) Sarsha Yap, BSc(Hons) (MBiostats candidate) Senior Research Assistants Julia Stanbury, BMedSc, MHP, (MPhil candidate) Christina Christou, BHS, MPH, DipNat Kristie Weir, BSc(Population Health) Laboratory Research Assistant Mahboobeh Hosseini, BEng Cancer Council NSW Research Activity Report 2012 27 Grants Grants Grants awarded to Cancer Council NSW Cancer Information and Support Services Division New grants in 2012 Porwal M, Hillman B, Robotin M Empowering CALD youth to reduce the burden of liver cancer in high-risk communities Cancer Institute NSW 2012–2013 $100,000 Robotin M, Danta S, Porwal M Animated films as a medium to raise hepatitis B community awareness in high-risk communities in SW Sydney Gilead Australia Fellowship Research Grants Program 2013–2014 $20,000 Robotin M, George J, Porwal M, Strasser S Applied medical education on health disparities: chronic hepatitis B infection and liver cancer in Asian communities in NSW University of Sydney Divisional Strategic Teaching Enhancement Project Scheme (STEPS) grant 2012–2013 $35,000 Robotin M, Porwal M, Batt G, Bartels R, George J Developing multimedia resources for liver cancer for CALD communities Cancer Australia 2012–2014 $160,000 Robotin M, Porwal M, Penman A Supporting primary care providers to identify and optimally manage patients with chronic hepatitis B to prevent liver cancer NSW Ministry of Health 2012–2014 $183,400 Evaluation of Cancer Council Legal Referral Service Law and Justice Foundation Grant 2011–2012 $33,462 Condon J, Garvey G, Baade P, Valery P, Brotherton J, Lokuge K, Cunningham J, O’Connell D, Canfell K Cervical screening participation and outcomes for Indigenous Australian women NHMRC Project Grant 2013–2016 $576,701 Cancer Research Division Independent Research Institutes Infrastructure Support Scheme NHMRC Independent Research Institutes Infrastructure Support Scheme 2013 $151,476 Cancer Research Division NHMRC Research Administering Institution Add-On Grant NHMRC Research Administering Institution Add-On Grant 2013 $7,464 Garvey G, Cunningham J, Centre for Research Excellence in Discovering Indigenous O’Connell D, Valery P, Thompson S, Strategies to improve Cancer Outcomes via Engagement, Condon J, McGrath P, Adams M, Research Translation and Training (DISCOVER-TT) Sabeson S, Brands J NHMRC Centre of Research Excellence in Health Services Research Grant 2012–2016 $2,499,998 Smith D, Batt G A Survivorship Action Partnership (ASAP) Movember Funds 2013–2015 $6,250,000 (to be split between many collaborators) Yu XQ School of Public Health Travel Grant to present findings to the Karolinska Institutet, Stockholm, Sweden University of Sydney 2012 $3,000 Yu XQ Travel Grant to present findings at the International Association of Cancer Registries Conference in Cork, Ireland Australasian Epidemiological Association 2012 $3,000 Canfell K Evaluation of future cervical cancer prevention strategies in Australia NHMRC Career Development Award 2011–2014 $384,160 Canfell K Evaluation of the cost-effectiveness of colorectal cancer screening in Australia Cancer Council NSW 2011–2012 $200,000 Canfell K, Clements M, Nickson C, Evaluation of primary HPV testing for cervical Brotherton J, Castle P, Schiffman M, screening in Australia Lord S, Shi JF NHMRC Project Grant 2011– 2013 $677,522 Canfell K, Smith M, Walker R Analytical services for National Cervical Screening Program Monitoring Reports National Screening Unit, New Zealand Ministry of Health 2011–2014 Chambers S, Baade P, Youl P, Aitken J, Dunn J, Garvey G, Valery P, O’Connell D The effects of stigma and nihilism views on lung cancer outcomes Cancer Australia Request for Tender 2011–2013 $588,112 Chambers SK, Smith D, Berry M, Lepore S, Foley E, Occhipinti S, Frydenberg M, Gardiner RA A randomised controlled trial of mindfulness intervention for men with advanced prostate cancer Cancer Australia 2011–2013 $706,243 Haines M, O’Connell D, Young J, Smith D, Kneebone A, Brooks A, Watt H Improving evidence-based care for locally advanced prostate cancer: a randomised phased trial of clinical guideline implementation through a clinical network NHMRC Partnership Project Grant 2011–2013 $533,442 (NHMRC); $537,674 (PCFA) Ingham J, O’Connell D, Phillips J, Davidson P, Girgis A, Wilkinson A, Piza M, Pigot M, Goldsbury D Last days of life linkage study: patterns of health services use and experiences of adult NSW residents in the year prior to death from illness Cancer Institute NSW 2011–2012 $83,748 Continuing grants in 2012 Boyes A, Zucca A Cancer Research Division New grants in 2012 Continuing grants in 2012 28 Neale R, O’Connell D, Janda M, Merrett N, Goldstein D, Beesley V, Wyld D, Gooden H Patterns of care and quality of life in patients with pancreatic cancer NHMRC Project Grant 2010–2012 $655,213 O’Connell D, Butow P, Armstrong B, Treloar C, Knight R, Dillon A, Newman C, Supramaniam R Patterns of cancer care for Indigenous people in NSW NHMRC Health Services Research Grant 2007–2013 $1,580,755 O’Connell D, Chambers S, Moxey A, Smith DP Use of complementary and lifestyle therapies by men with prostate cancer: a population-based study Prostate Cancer Foundation of Australia 2009–2012 $137,766 O'Connell D, Supramaniam R, Dillon A, Ingham J, Fernando P Cancer comorbidity, treatment, survival and end-of-life care for Aboriginal people in NSW Cancer Institute NSW 2011–2013 $280,688 Shi J (supervisor Canfell K) Cost-effectiveness evaluation of cervical cancer prevention strategies in China American Cancer Society International Fellowships for Beginning Investigators, UICC/ACSBI Fellowship 2009–2012 Sitas F, Armstrong B, Banks E, Kricker A, Weber M, Pawlita M Infectious and lifestyle determinants of non‑melanoma skin cancer NHMRC Project Grant 2009–2013 $953,200 Sitas F, Canfell K, O’Connell D, Banks E, Ward R, Baron M The NSW Cancer Lifestyle and Evaluation of Risk (CLEAR) Study Cancer Council NSW 2006–ongoing $3,000,000 to date Yu XQ Projecting prevalence by phase of care for colorectal, lung, breast and prostate cancer in New South Wales NHMRC Training Fellowship 2009–2012 $279,000 Freeman R, Chapman S, Kelly B, King L, Chapman K, Baur L, Gill T Online food and beverage marketing to children and adolescents Australian National Preventive Health Agency 2012–2015 $259,159 Nutrition Unit Grant to assist in the delivery of the Eat It To Beat It fruit and vegetable promotion program in the Greater Western Sydney Region Nepean Blue Mountains and Western Sydney Local Health Districts Project Grant 2012–2015 $180,000 Nutrition Unit Grant to support our strategic food policy research examining nutrition information in fast food outlets and the promotion of fast foods, consumer understanding of nutrition information food labels, the extent of children’s exposure to food marketing and influence of digital media, and food advertising complaints NSW Ministry of Health 2012–2013 $70,000 Nutrition Unit Grant to support the promotion of the NSW Ministry of Health Get Healthy Coaching and Information Service NSW Ministry of Health 2012 $21,685 Sanson-Fisher R, Tang A, Carey M, Bryant J, Tzelepis F, Chapman K, Vallentine P, Doran C, McElduff P Improving cancer treatment systems: a randomised controlled trial of a consumer action model for cancer patients receiving chemotherapy Australian Research Council Linkage Grant 2012–2014 $249,408 (including $24,000 contribution from CCNSW as the industry partner) Health Strategies Division New grants in 2012 Grants awarded by Cancer Council NSW New Research Project Grants in 2012 A/Prof Tracy Bryan Involvement of helicase DHX36 in human telomere maintenance University of Sydney 2012–2015 $292,524 Dr Scott Cohen Structure and inhibition of the human telomerase enzyme complex University of Sydney 2012–2015 $360,000 Dr Sue Firth IGFBP-3 enhances autophagy to promote breast cancer cell survival during stress University of Sydney 2012–2015 $360,000 Dr Beric R Henderson Novel regulation of beta-catenin intracellular transport and its role in cell polarity and migration University of Sydney 2012–2015 $360,000 Dr Megan Hitchins The mechanistic basis for prediction of response to alkylating chemotherapy in high-grade glioma patients by molecular markers of MGMT activity University of New South Wales 2012–2015 $311,175 A/Prof Geraldine M O'Neill A sting in the tail: focal adhesion targeting and mechanotransduction University of Sydney 2012–2015 $326,169 A/Prof Stuart G Tangye Mechanisms underlying impaired anti-EBV immune responses in the absence of SAP Garvan Institute of Medical Research 2012–2015 $357,140 Dr Nicole M Verrills Activating a tumour supressor for leukaemia therapy (co-funded with Cure Cancer Australia Foundation) University of Newcastle 2012–2015 $360,000 Continuing Research Project Grants in 2012 Prof Mark Baker A colorectal cancer ‘interactome’ paradigm that influences patient survival Macquarie University 2010–2012 $300,000 Prof Robert C Baxter Targeting IGFBP-3 signalling pathways as a novel therapeutic approach in triple-negative breast cancer University of Sydney 2011–2013 $358,886 Dr Linda Bendall The role of sphingosine-1-phosphate in haematopoietic stem cell egress from the bone marrow University of Sydney 2010–2012 $360,000 A/Prof Tracy Bryan G-quadruplex stabilisers as cancer therapeutics University of Sydney 2011–2013 $292,524 A/Prof Tracy Bryan Recruitment of human telomerase to telomeres University of Sydney 2010–2012 $368,750 Cancer Council NSW Research Activity Report 2012 29 Grants Dr Megan Chircop Dynamin as a new drug target for the treatment of glioblastoma University of Sydney 2011–2013 $360,000 A/Prof Anna DeFazio Pathways of malignant progression in ovarian cancer University of Sydney 2010–2012 $354,575 A/Prof Peter Greer Does the initial treatment plan predict doses delivered to normal tissues during prostate radiation therapy? University of Newcastle 2011–2013 $349,794 A/Prof Peter Greer Real-time dose monitoring for patient safety in radiation therapy University of Newcastle 2010–2012 $360,000 Dr Beric R Henderson Regulation of APC intracellular dynamics and function University of Sydney 2011–2013 $360,000 Dr Viive Howell New opportunities for the study of ovarian cancer through characterisation of mouse models University of Sydney 2011–2013 $315,016 A/Prof Maija Kohonen-Corish Functional characterisation of the putative tumour suppressor gene MCC in colorectal cancer Garvan Institute of Medical Research 2010–2012 $360,000 Dr Tao Liu Targeting Myc onco-protein degradation for the treatment of Myc-induced malignancies Children’s Cancer Institute Australia for Medical Research 2010–2012 $319,500 Dr Tao Liu The critical role of the histone demethylase JMJD1A in cancer Children’s Cancer Institute Australia for Medical Research 2011–2013 $330,750 Dr Richard Lock Predicting the in vivo sensitivity of paediatric acute lymphoblastic leukaemia to BH3-mimetic drugs University of New South Wales 2011–2013 $329,250 Dr Guy Lyons Restoring epithelial differentiation to squamous cell carcinomas University of Sydney 2010–2012 $360,000 Dr Karen MacKenzie The prognostic and therapeutic significance of dyskerin and telomerase enzyme activity in neuroblastoma University of New South Wales 2011–2013 $352,524 Prof Finlay Macrae The effects of butyrylated high-amylose maize starch on polyposis in FAP volunteers Melbourne Health 2011–2013 $345,617 Prof John Rasko Dissecting the multicomponent machine that controls chromatin architecture University of Sydney 2011–2013 $359,324 Prof John Rasko The role of small non-coding RNAs (sncRNAs) in alternative splicing University of Sydney 2011–2013 $360,000 Dr Philip Vial A next-generation detector for radiotherapy treatment verification with dual capability for simultaneous imaging and dosimetry University of Sydney 2011–2013 $336,125 Prof Robyn Ward Laterally spreading tumours of the colorectum: an alternative pathway of colorectal cancer development in the Western world University of New South Wales 2011–2013 $360,000 Prof Xu Zhang Targeting pro-survival mechanisms to sensitise human melanoma to immunotherapy University of Newcastle 2011–2013 $359,250 New Priority-driven Collaborative Cancer Research Scheme grants in 2012 (co-funded through Cancer Australia) Dr Kerrie L McDonald Mechanisms underpinning how brain cancer cells respond to drugs University of New South Wales 2012–2015 $486,175 Prof Anna Nowak Phase III trial of concurrent and adjuvant temozolomide chemotherapy in non-1p/19q non-deleted anaplastic glioma. The CATNON Intergroup Trial University of Western Australia 2012–2015 $369,000 A/Prof Gianluca Severi Risk and prognostic factors for glioma in Australia Cancer Council Victoria 2012–2015 $600,000 Continuing Priority-driven Collaborative Cancer Research Scheme grants in 2012 (co-funded through Cancer Australia) A/Prof Bettina Meiser Too much, too soon? The impact of treatment-focused genetic testing in patients newly diagnosed with breast cancer University of New South Wales 2010–2012 $21,149 Prof Robyn Ward Role of dietary compounds on PGC-1alpha methylation in colorectal cancer University of New South Wales 2011–2013 $321,261 Continuing Research Program Grants in 2012 Prof Philip Hogg Metabolism inhibitors for the treatment of brain and pancreatic cancer University of New South Wales 2011–2015 $2,250,000 A/Prof Lisa Horvath Building capacity in pharmacogenomics across NSW: PRIMe (Pharmacogenomic Research for Individualised Medicine) University of Sydney 2010–2015 $1,498,668 Prof Murray Norris Toward cure of childhood ALL: improved diagnostics, therapeutics and prevention strategies University of New South Wales 2011–2015 $2,250,000 A/Prof Chris Ormandy Personalising breast cancer management by discovering the transcriptional basis for tumour phenotype Garvan Institute of Medical Research 2011–2015 $2,249,976 Prof Roger Reddel Alternative lengthening of telomeres: from basic biology to drug discovery Children’s Medical Research Institute 2011–2015 $2,250,000 30 Continuing Strategic Research Partnership (STREP) grants in 2012 Prof Andrew Biankin Genotype-guided cancer therapy (genomic theranostics) Garvan Institute of Medical Research 2011–2015 $1,500,000 Prof Jacob George Epidemiology, prevention and management of liver cancer in NSW: towards a strategic research partnership University of Sydney 2008–2012 $1,250,000 Dr Kerrie McDonald Australian Genomics and Clinical Outcomes of High Grade Glioma: AGOG University of New South Wales 2008–2012 $1,238,114 Laureate Prof Rob Sanson-Fisher Behavioural Science Strategic Research Partnership: the Newcastle Cancer Control Collaborative (New-3C) University of Newcastle 2011–2013 $1,200,000 Prof David Whiteman PROBE-NET: Progression of Barrett’s Esophagus to Cancer Network Queensland Institute of Medical Research 2008–2012 $1,246,165 International Cancer Genome Consortium (ICGC) in 2012 Prof Andrew Biankin Australian Pancreatic and Ovarian Cancer Genome Initiative Garvan Institute of Medical Research 2010–2014 $2,500,000 Prof Graham Mann Melanoma Genome Project Melanoma Institute Australia 2012–2015 $479,428 Continuing Innovator Grants in 2012 Dr Anthony Don Developing sphingosine kinase 2 inhibitors to block glioblastoma cell proliferation University of New South Wales 2011–2012 $8,648 Prof Jacob George Novel molecular targets for treatment of hepatocellular cancer (HCC) University of Sydney 2011–2012 $100,000 Prof Georges Grau Deep sequencing of glioma-derived microparticles University of Sydney 2011–2012 $100,000 Prof Michael Murray Pharmacogenomic approaches to minimise sorafenib toxicity in patients with liver cancer University of Sydney 2011–2012 $97,730 A/Prof Wayne Phillips Using familial genetics to identify genes involved in the biology of Barrett’s oesophagus Peter MacCallum Cancer Centre 2011 2011–2012 $100,000 Dr Nicholas Shackel Discovering novel non-invasive diagnostic and prognostic markers in hepatocellular carcinoma University of Sydney 2011–2012 $100,000 Dr Sarah Thompson Sentinel lymph node biopsy in oesophageal adenocarcinoma – improving staging accuracy and optimising treatment The Royal Adelaide Hospital 2011–2012 $94,255 Dr Kathy Willowson The role of imageable microspheres in radioembolisation treatment planning for HCC University of Sydney 2011–2012 $3,217 St Vincent’s Centre for Applied Medical Research 2011–2012 $50,000 Continuing Clinical Trials Protocol Grant in 2012 Prof Reginald Lord Randomised trial of endoscopic radiofrequency ablation versus complete mucosectomy with stent for Barrett’s high-grade dysplasia or intramucosal adenocarcinoma Commissioned Research Grants in 2012 Consumer testing of front-of-pack food labelling 2012 $40,000 Skin cancer prevention in outdoor workers – an investigation of knowledge, attitudes and behaviours 2011–2012 $30,000 Sun protection attitudes and behaviours among first generation Australians with skin type lV 2011–2012 $40,000 The construction and experience of fertility in the context of cancer: patient, partner and health professional perspectives 2012 $30,000 The Quit Smoking Support for Young People project 2011–2012 $15,000 Cancer Council NSW Research Activity Report 2012 31 Publications Publications Cancer Information and Support Services Cancer Research Division Fitz-Gerald L, Balakrishnan S, Orchard J. Little assurance for overseas students’ health insurance. Aust Health Law Bull. 2012;20(9):136-45. Aminisani N, Armstrong BK, Canfell K. Cervical cancer screening in Middle Eastern and Asian migrants to Australia: a record linkage study. Cancer Epidemiol. 2012;36(6):e394-400. Fraser A, Masgoret X, Robotin M, Porwal M. Using hepatitis B registry data to improve liver cancer prevention at primary care level. Asia Pac J Clin Oncol. 2012;8 Suppl 3:180. [A408] Aminisani N, Armstrong BK, Egger S, Canfell K. Impact of organised cervical screening on cervical cancer incidence and mortality in migrant women in Australia. BMC Cancer. 2012;12:491. Olver I, Robotin M, editors. Perspectives on complementary and alternative medicine. London: Imperial College Press; 2012. Cairns BJ, Travis RC, Wang XS, Reeves GK, Green J, Beral V; Million Women Study Collaborators (including Canfell K). A short-term increase in cancer risk associated with daytime napping is likely to reflect preclinical disease: prospective cohort study. Br J Cancer. 2012;107(3):527-30. Porwal M, Hillman B, Russell M, Robotin M. Engaging youth in reducing the burden of liver cancer in culturally and linguistically diverse communities. Asia Pac J Clin Oncol. 2012;8 Suppl 3:180. [A408] Robotin M. From traditional medicines to drug discovery. In: Olver I, Robotin M, editors. Perspectives on complementary and alternative medicine. London: Imperial College Press; 2012. p.157-86. Robotin M. Randomised controlled trials in the primary treatment of hepatocellular carcinoma. In: Qiao L, Li Y, Yan X, George J, editors. Molecular aspects of hepatocellular carcinoma. Sharjah UAE, Oak Park Il USA, Bussum The Netherlands: Bentham Science Publishers; 2012. p.174-95 Robotin M, Holliday C, Bensoussan A. Defining research priorities in complementary medicine in oncology. Complement Ther Med. 2012;20(5):345-52. Robotin M, Patton Y, Kansil M, Penman A, George J. Cost of treating chronic hepatitis B: comparison of current treatment guidelines. World J Gastroenterol. 2012;18(42):6106-13. Canfell K, Chesson H, Kulasingam SL, Berkhof J, Diaz M, Kim JJ. Modeling preventative strategies against HPVrelated disease in developed countries. Vaccine. 2012;30 Suppl 5:F157-67. [Invited peer-reviewed paper] Chambers SK, Dunn J, Occhipinti S, Hughes S, Baade P, Sinclair S, Aitken J, Youl P, O’Connell DL. A systematic review of the impact of stigma and nihilism on lung cancer outcomes. BMC Cancer. 2012;12:184. Chiew M, Weber MF, Egger S, Sitas F. A cross-sectional exploration of smoking status and social interaction in a large population-based Australian cohort. Soc Sci Med. 2012;75(1):77-86. Clements MS, Roder DM, Yu XQ, Egger S, O’Connell DL. Estimating prevalence of distant metastatic breast cancer: a means of filling a data gap. Cancer Causes Control. 2012;23(10):1625-34. Collaborative Group on Epidemiological Studies of Ovarian Cancer (including Sitas F). Ovarian cancer and smoking: individual participant meta-analysis including 28,114 women with ovarian cancer from 51 epidemiological studies. Lancet Oncol. 2012;13(9):946-56. Collaborative Group on Hormonal Factors in Breast Cancer (including Sitas F and Canfell K). Menarche, menopause and breast cancer risk: individual participant meta-analysis, including 118 964 women with breast cancer from 117 epidemiological studies. Lancet Oncol. 2012;13(11):1141-51. 32 Goldsbury D, Harris MF, Pascoe S, Olver I, Barton M, Spigelman A, O’Connell D. Socio-demographic and other patient characteristics associated with time between colonoscopy and surgery, and choice of treatment centre for colorectal cancer: a retrospective cohort study. BMJ Open. 2012;2:e001070. Goldsbury DE, Armstrong K, Simonella L, Armstrong BK, O’Connell DL. Using administrative health data to describe colorectal and lung cancer care in New South Wales, Australia: a validation study. BMC Health Serv Res. 2012;12:387. Green J, Roddam A, Pirie K, Kirichek O, Reeves G, Beral V; Million Women Study Collaborators (including Canfell K). Reproductive factors and risk of oesophageal and gastric cancer in the Million Women Study cohort. Br J Cancer. 2012;106(1):210-6. Kahn C, Simonella L, Sywak M, Boyages S, Ung O, O’Connell D. Pathways to the diagnosis of thyroid cancer in New South Wales: a population-based cross-sectional study. Cancer Causes Control. 2012;23(1):35-44. Kahn C, Simonella L, Sywak M, Boyages S, Ung O, O’Connell D. Post-surgical pathology reporting of thyroid cancer in New South Wales, Australia. Thyroid. 2012;22(6):604-10. King MT, Viney R, Smith DP, Hossain I, Street D, Savage E, Fowler S, Berry MP, Stockler M, Cozzi P, Stricker P, Ward J, Armstrong BK. Survival gains needed to offset persistent adverse treatment effects in localised prostate cancer. Br J Cancer. 2012;106(4):638-45. Legood R, Smith M, Lew JB, Walker R, Moss S, Kitchener H, Patnick J, Canfell K. Cost effectiveness of human papillomavirus test of cure after treatment for cervical intraepithelial neoplasia in England: economic analysis from NHS Sentinel Sites Study. BMJ. 2012;345:e7086. Litchfield MJ, Cumming RG, Smith DP, Naganathan V, Le Couteur DG, Waite LM, Blyth FM, Handelsman DJ. Prostate-specific antigen levels in men aged 70 years and over: findings from the CHAMP study. Med J Aust. 2012;196(6):395-8. Mayosi BM, Lawn JE, van Niekerk A, Bradshaw D, Abdool Karim SS, Coovadia HM; Lancet South Africa Team (including Sitas F). Health in South Africa: changes and challenges since 2009. Lancet. 2012;380(9858):2029-43. Nair-Shalliker V, Fenech M, Forder PM, Clements MS, Armstrong BK. Sunlight and vitamin D affect DNA damage, cell division and cell death in human lymphocytes: a cross-sectional study in South Australia. Mutagenesis. 2012;27(5):609-14. Nair-Shalliker V, Smith DP, Egger S, Hughes AM, Kaldor JM, Clements M, Kricker A, Armstrong BK. Sun exposure may increase risk of prostate cancer in the high UV environment of New South Wales, Australia: a case-control study. Int J Cancer. 2012;131(5):E726-32. Plummer M, Peto J, Franceschi S; International Collaboration of Epidemiological Studies of Cervical Cancer (including Canfell K and Sitas F). Time since first sexual intercourse and the risk of cervical cancer. Int J Cancer. 2012;130(11):2638-44. Sewram V, Sitas F, O’Connell D, Myers J, Klaassen L. Esophageal cancer in South Africa. In: Eslick G, editor. Esophageal cancer: epidemiology, diagnosis and treatment. New York: Nova Science; 2012. p. 53-76. Shi JF, Canfell K, Lew JB, Qiao YL. The burden of cervical cancer in China: synthesis of the evidence. Int J Cancer. 2012;130(3):641-52. Shi JF, Chen JF, Canfell K, Feng XX, Ma JF, Zhang YZ, Zhao FH, Li R, Ma L, Li ZF, Lew JB, Ning Y, Qiao YL. Estimation of the costs of cervical cancer screening, diagnosis and treatment in rural Shanzi Province, China: a micro-costing study. BMC Health Serv Res. 2012;12(1):123. Shi JF, Kang DJ, Qi SZ, Wu HY, Liu YC, Sun LJ, Li L, Yang Y, Li Q, Feng XX, Zhang LQ, Li J, Li XL, Yang Y, Niyazi M, Xu AD, Liu JH, Xiao Q, Li LK, Wang XZ, Qiao YL. Impact of genital warts on health related quality of life in men and women in mainland China: a multicenter hospital-based cross-sectional study. BMC Public Health. 2012;12(1):153. Sitas F, Egger S, Urban MI, Taylor PR, Abnet CC, Boffetta P, O’Connell DL, Whiteman DC, Brennan P, Malekzadeh R, Pawlita M, Dawsey SM, Waterboer T, Webb PM, Green AC, Hayward NK, Zaridze D, Holcatova I, Mates D, Szeszenia-Dabrowska N, Ferro G, Janout V, Curado MP, Menezes AM, Koifman S, Islami F, Nasrollahzadeh D, Hu N, Goldstein AM, Gao Y, Ding T, Kamangar F. InterSCOPE Study: associations between esophageal squamous cell carcinoma and human papillomavirus serological markers. J Natl Cancer Inst. 2012;104(2):147-58. Nair-Shalliker V, Armstrong BK, Fenech M. Does vitamin D protect against DNA damage? Mutat Res. 2012;733(1-2):50-7. Cancer Council NSW Research Activity Report 2012 33 Publications Smith M, Walker R, Canfell K. Independent Monitoring Report Number 33 for January-June 2010: National Cervical Screening Programme. Report to the NZ National Screening Unit. National Screening Unit: New Zealand; 2012. Smith M, Walker R, Canfell K. Independent Monitoring Report Number 34 for July-December 2010: National Cervical Screening Programme. Report to the NZ National Screening Unit. National Screening Unit: New Zealand; 2012. Swart A, Burns L, Mao L, Grulich AE, Amin J, O’Connell DL, Meagher NS, Randall DA, Degenhardt L, Vajdic CM. The importance of blood-borne viruses in elevated cancer risk among opioid-dependent people: a population-based cohort study. BMJ Open. 2012:2(5):e001755. Urban M, Banks E, Egger S, Canfell K, O’Connell D, Beral V, Sitas F. Injectable and oral contraceptive use and cancers of the breast, cervix, ovary, and endometrium in black South African women: case-control study. PLoS Med. 2012;9(3):e1001182. Walker R, Nickson C, Lew JB, Smith M, Canfell K. A revision of sexual mixing matrices in models of sexually transmitted infection. Stat Med. 2012:31(27):3416-32. Wang JB, Jiang Y, Liang H, Li P, Xiao HJ, Ji J, Xiang W, Shi JF, Fan YG, Li L, Wang D, Deng SS, Chan WQ, Wei WQ, Qiao YL, Boffetta P. Attributable causes of cancer in China. Ann Oncol. 2012;23(11):2983-9. Yu XQ, Baade PD, O’Connell DL. Conditional survival of cancer patients: an Australian perspective. BMC Cancer. 2012;12:460. Health Strategies Division Deacon RM, Topp L, Wand H, Day CA, Rodgers C, Haber PS, van Beek I, Maher L. Correlates of susceptibility to hepatitis B among people who inject drugs in Sydney, Australia. J Urban Health. 2012;89(5):769-78. Glasson C, Chapman K, Gander K, Wilson T, James E. The efficacy of a brief, peer-led nutrition education intervention in increasing fruit and vegetable consumption: a wait-list, community-based randomised controlled trial. Public Health Nutr. 2012;15(7):1318-26. Hull P, Salmon A, O’Brien J, Chapman K, Williams K. Can social and community service organisations embrace tobacco control for their disadvantaged clients? Health Promot J Aust. 2012;23(3):183-7. Islam M, Topp L, Conigrave KM, van Beek I, Maher L, White A, Rodgers C, Day C. The reliability of sensitive information provided by injecting drug users in a clinical setting: clinician-administered versus audio computerassisted self-interviewing (ACASI). AIDS Care. 2012; 24(12):1496-503. Islam M, Topp L, Conigrave K, White A, Reid S, Grummet S, Haber P, Day C. Linkage into specialist hepatitis C treatment services of injecting drug users attending a needle syringe program-based primary healthcare centre. J Subst Abuse Treatment. 2012;43(4):440-5. Islam M, Topp L, Day CA, Dawson A, Conigrave KM. Primary healthcare outlets that target injecting drug users: opportunity to make services accessible and acceptable to the target group. Int J Drug Policy. 2012;23(2):109-10. Islam M, Topp L, Day CA, Dawson A, Conigrave KM. The accessibility, acceptability, health impact and cost implications of primary healthcare outlets that target injecting drug users: a narrative synthesis of literature. Int J Drug Policy. 2012;23(2):94-102. Iversen J, Topp L, Wand H, Maher L. Individuallevel syringe coverage among Needle and Syringe Program attendees in Australia. Drug Alcohol Depend. 2012;122(3):195-200. Kelly B, Baur LA, Bauman AE, King L, Chapman K, Smith BJ. Restricting unhealthy food sponsorship: attitudes of the sporting community. Health Policy. 2012;104(3):288-95. 34 King L, Watson WL, Chapman K, Kelly B, Louie JCY, Hughes C, Crawford J, Gill TP. Do we provide meaningful guidance for healthful eating? An investigation into consumers’ interpretation of frequency consumption terms. J Nutr Educ and Behav. 2012;44(5):459-63. Larney S, Topp L, Indig D, O’Driscoll C, Greenberg D. A cross-sectional survey of prevalence and correlates of suicidal ideation and attempts in prisoners in New South Wales, Australia. BMC Public Health. 2012;12:14. O’Brien J, Bonevski B, Salmon A, Oakes W, Goodger B, Soewido D. An evaluation of a pilot capacity building initiative for smoking cessation in social and community services: the Smoking Care project. Drug Alcohol Rev. 2012;31(5):685-92. O’Brien J, Salmon A, Penman A. What has fairness got to do with it? Tackling tobacco among Australia’s disadvantaged. Drug Alcohol Rev. 2012;31(5):723-6. Pettigrew S, Roberts M, Chapman K, Quester P, Miller C. The use of negative themes in television food advertising. Appetite. 2012;58(2):496-503. Pettigrew S, Roberts M, Pescud M, Chapman K, Quester P, Miller C. The extent and nature of alcohol advertising on Australian television. Drug Alcohol Rev. 2012;31(6):797-802. Roberts M, Pettigrew S, Chapman K, Miller C, Quester P. Compliance with children’s television food advertising regulations in Australia. BMC Public Health. 2012;12:846. Scully M, Wakefield M, Niven P, Chapman K, Crawford D, Pratt IS, Baur LA, Flood V, Morley B; NaSSDA Study Team. Association between food marketing exposure and adolescents’ food choices and eating behaviors. Appetite. 2012;58(1):1-5. Topp L. ATS use and risk-taking behaviours. In: Allsop S, Lee N, editors. Perspectives on amphetamine-type stimulants. Melbourne: IP Communications; 2012. p. 69-82. Wand H, Iversen J, Wilson D, Topp L, Maher L. Developing and validating a scoring tool for identifying people who inject drugs at increased risk of hepatitis C virus infection. BMJ Open. 2012;2(1):e000387. Wellard L, Glasson C, Chapman K. Fries or a fruit bag? Investigating the nutritional composition of fast food children’s meals. Appetite. 2012;58(1):105-10. Wellard L, Glasson C, Chapman K. Sales of healthy choices at fast food restaurants in Australia. Health Promot J Australia. 2012;23(1):37-41. Cancer Council NSW Research Activity Report 2012 35 Board and committees Board and committees Cancer Council NSW Board of Directors Mr Bruce Hodgkinson SC (Chair) Barrister, Denman Chambers Ms Jill Boehm OAM (Deputy Chair) Prof Stephen Ackland Senior Staff Specialist, Medical Oncology, Calvary Mater Newcastle Hospital A/Prof Michael Back Director, Northern Sydney Cancer Centre Prof Reginald Lord AM Professor and Head, Gastroesophageal Cancer Research Program, St Vincent’s Centre for Applied Medical Research Mr John Moroney Consumer Representative Dr Monica Robotin Medical Director, Cancer Council NSW Ms Mary Chiew CEO, Giorgio Armani Australia A/Prof Natalka Suchowerska Head, Research and Education (Medical Physics), Department of Radiation Oncology, Royal Prince Alfred Hospital Mr Paul Lahiff Consultant Regina Sutton CEO, Cancer Council NSW Mr Stephen Roberts Consultant Prof Kate White Professor of Cancer Nursing, University of Sydney Cancer Nursing School, Royal Prince Alfred Hospital Mr Robert Sendt Consultant and former NSW Auditor-General Mr John Stubbs Executive Director, CanSpeak Australia Cancer Council NSW Ethics Committee Mr Jim Grainda Consumer Representative Dr Monica Robotin Medical Director, Cancer Council NSW A/Prof Freddy Sitas Director, Cancer Research Division, Cancer Council NSW Consumer Reviewers Mr James Butler (Chair) Project and STREP panels Ms Gillian Begbie Project Grant panel Ms Jane Bennett Project Grant panel Ms Linda Christenson Project Grant panel Ms Margaret Johnson Project Grant panel Ms Mara Lidums Project Grant panel Ms Meghan Carruthers (Chair) Lawyer, HWL Ebsworth Mr Dez Maule Project Grant panel Ms Melanie Trethowan Consultant Dr John Sanders (Deputy Chair), Layman Mr Tony Maxwell Project Grant panel Cancer Council NSW Cancer Research Committee Dr Megan Brock Religious Representative Ms Mary Potter Project Grant panel Prof Michelle Haber AM (Chair) Executive Director and Head of Experimental Therapeutics Program, Children’s Cancer Institute Australia for Medical Research Prof Bill McCarthy AM Medical Graduate with Research Experience Ms Bridget Whelan Project Grant panel Prof Mark Baker Professor of Proteomics, Macquarie University Ms Joanne Muller Lawyer Reverend John Neasey Religious Representative Ms Jane Bennett Consumer Representative Mr Felix Ratcliff Allied Health Professional Prof Andrew Biankin Professor and Head, Pancreatic Cancer Research, Garvan Institute of Medical Research Dr Monica Robotin Medical Graduate with Research Experience A/Prof Anna DeFazio Head, Gynaecological Oncology Research Group, Westmead Millennium Institute for Cancer Research at Westmead Hospital. Prof Sandra Jones Professor and Director, Centre for Health Initiatives, University of Wollongong 36 Ms Frances Taylor Laywoman Research Review Committee Prof Louisa Jorm (Chair) Research Director, Sax Institute Ms Gillian Batt Director, Cancer Information and Support Services Division, Cancer Council NSW Mr Jeff Winter Project Grant panel Ms Robyn Bransby STREP grant panel Ms Barbara Dawson STREP grant panel Mr James Falk STREP grant panel Mr John Moroney STREP grant panel Ms Jan Mumford STREP grant panel Contact Cancer Research Division Research Strategy Unit Cancer Council NSW PO Box 572 Kings Cross NSW 1340 Cancer Council NSW PO Box 572 Kings Cross NSW 1340 P: (02) 9334 1837 F: (02) 8302 3550 E: crd@nswcc.org.au P: (02) 9334 1993 E: research@nswcc.org.au FSC details to be inserted by printer Designed by Cobe Design Printed by SOS Print + Media Photography by Christian Trinder © Cancer Council NSW 2013 ABN 51 116 463 846 CAN2038 06/13 153 Dowling Street Woolloomooloo NSW 2011 feedback@nswcc.org.au www.cancercouncil.com.au facebook.com/cancercouncilnsw twitter.com/cancercouncil youtube.com/cancercouncilnsw1 @cancercouncil or #cancercouncil to show us yours linkedin.com/company/cancer-council-nsw pinterest.com/cancercouncil