- American Journal of Orthodontics and Dentofacial
advertisement

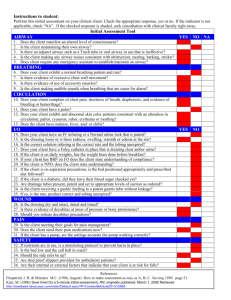
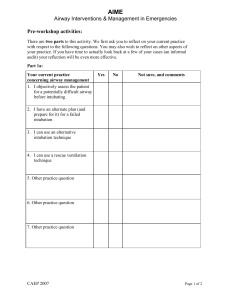
ONLINE ONLY Three-dimensional analysis of pharyngeal airway in preadolescent children with different anteroposterior skeletal patterns Yoon-Ji Kim,a Ji-Suk Hong,a Yong-In Hwang,a and Yang-Ho Parkb Seoul, Korea Introduction: In growing patients with skeletal discrepancies, early diagnosis, evidence-based explanations of etiology, and assessment of functional factors can be vital for the restoration of normal craniofacial growth and the stability of the treatment results. The aims of our study were to compare the 3-dimensional pharyngeal airway volumes in healthy children with a retrognathic mandible and those with normal craniofacial growth, and to investigate possible significant relationships and correlations among the studied cephalometric variables and the airway morphology in these children. Methods: Three-dimensional airway volume and crosssectional areas of 27 healthy children (12 boys, 15 girls; mean age, 11 years) were measured by using cone-beam computed tomography volume scans, and 2-dimensional lateral cephalograms were created and analyzed. The subjects were divided into 2 groups based on their ANB angles (group I: 2 # ANB # 5 ; group II: ANB .5 ), and cephalometric variables, airway volumes, and cross-sectional measurements were compared. Results: There were statistically significant differences in the following parameters: height of the posterior nasal plane (P \0.05), pogonion to nasion perpendicular distance (P \0.01), ANB angle (P \0.01), mandibular body length (P \0.01), facial convexity (P \0.01), and total airway volume (P \0.05). No statistically significant differences between the 2 groups were found in the cross-sectional area and the volumetric measurements of the various sections of the airway except for total airway volume, which had larger values in group I (P \0.05). Conclusions: The mean total airway volume, extending from the anterior nasal cavity and the nasopharynx to the epiglottis, in retrognathic patients was significantly smaller than that of patients with a normal anteroposterior skeletal relationship. On the other hand, differences in volume measurements of the 4 subregions of the airway were not statistically significant between the 2 groups. (Am J Orthod Dentofacial Orthop 2010;137:306.e1-306.e11) T he effects of respiratory function on craniofacial growth have been studied for decades, and most clinicians now understand that respiratory function is highly relevant to the orthodontic diagnosis and the treatment plan. In 1907, Angle1 showed that his Class II Division 1 malocclusion is associated with obstruction of the upper pharyngeal airway and mouth breathing. Clinical features related to impaired breathing have been observed by some authors, and Ricketts2 presented the main characteristics of the respiratory obstruction syndrome as adenoid and tonsil hypertrophy, From the Department of Orthodontics, Kangdong Sacred Heart Hospital, Hallym University Medical Center, Seoul, Korea. a Resident. b Associate professor. The authors report no commercial, proprietary, or financial interest in the products or companies described in this article. Reprint requests to: Yang-Ho Park, Department of Orthodontics, Kangdong Sacred Heart Hospital, 445 Gil-Dong, Gangdong-Gu, Seoul, Korea, 134-701. e-mail, dentpark64@hanmail.net. Submitted, May 2009; revised and accepted, October 2009. 0889-5406/$36.00 Copyright Ó 2010 by the American Association of Orthodontists. doi:10.1016/j.ajodo.2009.10.025 crossbite, open bite, narrow external nares, and tongue thrusting. Predisposing factors of nasal obstruction can include adenoid and tonsil hypertrophy, polyps, allergies, infections, and nasal deformities. A common cause of mouth breathing arises from the adenoids, which are a conglomerate of lymphatic tissues located in the posterior pharyngeal airway. Infection and inflammation of the adenoids leads to upper airway obstruction, and the term ‘‘adenoid facies’’ is often used to describe a possible aberrant craniofacial growth pattern related to mouth breathing characterized by lip incompetency, underdeveloped nose, increased anterior facial height, constricted dental arches, and proclined maxillary incisors with a Class II occlusal relationship.3,4 In addition to studies that affirm nasal obstruction as the major factor responsible for dentofacial anomalies, other studies refute a significant relationship between airway obstruction and the frequency of malocclusion. In a study of 500 patients with upper airway problems, Leech5 discovered that 60% of the mouth-breathing patients were Class I and concluded that mouth breathing 306.e1 306.e2 Table I. Kim et al American Journal of Orthodontics and Dentofacial Orthopedics March 2010 Sample characteristics Group I Subjects (n) Age (y) (mean 6 SD) Range (y) Group II Male Female Male Female Total 7 11.46 6 0.69 10.50-12.58 7 11.71 6 0.86 10.67-12.92 5 10.23 6 0.73 9.42-12.33 8 11.09 6 1.03 9.08-12.17 27 11.19 6 1.28 9.08-12.92 has no influence on craniofacial growth. Similarly, Gwynne-Evans6 determined that facial growth is constant regardless of the mode of breathing. Additionally, Humphreys and Leighton7 found no significant difference in the anteroposterior relationship of the jaws between nose and mouth breathers. In growing patients with skeletal discrepancies and clinical signs of adenoid facies, early diagnosis, evidence-based explanations of etiology, and assessment of the functional factors might be vital for the restoration of normal craniofacial growth and the stability of treatment results. Morphometric evaluation of the pharyngeal airway has been mostly performed on lateral cephalometric headfilms, by identifying specific landmarks and measuring various lengths and areas in the pharyngeal region.8-10 Despite the vast amount of research concerning airway anatomy and its influence on craniofacial growth and development, most studies have been 2-dimensional (2D) and have used lateral or frontal cephalograms with limited evaluation of lengths and areas. New 3-dimensional (3D) technology of computed tomography (CT) has expanded diagnostic capacities, making volumetric analysis and accurate visualization of the airway possible. Most 3D studies of the airway used multislice CT to evaluate the airway; this has the advantage of high-quality images to discern hard- and soft-tissue anatomies, but, because of the high radiation dose, it is restricted to patients with severe craniofacial deformities and those undergoing orthognathic surgeries.11,12 Recently, cone-beam CT (CBCT) systems have been developed specifically for the maxillofacial region. Because a CBCT scan uses a different type of acquisition than traditional multislice CT, radiation is reduced and can be used in a wider range of patients, eg, those having maxillofacial surgery, implantology, and orthodontics.13 Cross-sectional and volumetric investigations of the pharyngeal airway have been possible by using CBCT scans to analyze the complex airway anatomy, and previous studies have confirmed that volumetric measurements of airways with CBCT are accurate with minimal error.14 The aims of our retrospective, cross-sectional study were (1) to compare the 3D pharyngeal airway volumes in healthy children with a retrognathic mandible and those with normal craniofacial growth and (2) to investigate possible significant relationships and correlations among the studied cephalometric variables and the airway morphology in these children. MATERIAL AND METHODS Pharyngeal airway structures were studied in 27 healthy children (12 boys, 15 girls) with a mean age of 11.19 6 1.28 years (Table I) who were referred to the Department of Orthodontics of Kangdong Sacred Heart Hospital, Hallym University Medical Center, Seoul, Korea, for treatment. Those who had symptoms of upper respiratory infection, pharyngeal pathology such as adenoid hypertrophy and tonsillitis or a history of adenoidectomy or tonsillectomy were excluded. The study protocol was approved by the Ethics Review Committee of the hospital (IRB 09-57). CBCT volume scans of all subjects were obtained by using the Master 3D dental-imaging system (Vatech, Seoul, Korea), and the imaging protocol used a 12-in field of view to include the entire craniofacial anatomy. The axial slice thickness was 0.3 mm, and the voxels were isotropic. Patients sat upright with natural head position, and their jaws were at maximum intercuspation with the lips and tongue in a resting position. The patients were asked not to swallow and not to move their heads or tongues. Almost all 3D imaging modalities (eg, conventional CT or magnetic resonance imaging) require patients to be supine; this causes significant morphologic changes of the airway, since gravity affects the soft tissues surrounding the oropharyngeal cavity.15 It might be reasonable to examine patients in the supine position for diagnosing such disorders as obstructive sleep apnea. In most cases (including orthodontic diagnosis and treatment planning), however, patients do not need to be analyzed in the supine position. Recent advances in CBCT permit the acquisition of axial CT images in the upright sitting position, which is more valid for our study. The axial images were imported to InVivoDental software (Anatomage, San Jose, Calif), and volumetric American Journal of Orthodontics and Dentofacial Orthopedics Volume 137, Number 3 Kim et al 306.e3 Fig 1. A volumetric rendering of a subject’s craniofacial skeleton: A, lateral view right; B, frontal view; C, lateral view left. Fig 2. For the horizontal reference plane, the FH plane was constructed from the right and left porions and the right orbitale, which was set as the origin. rendering was done for airway and cephalometric analysis (Fig 1). To standardize the measurements and minimize errors, the 3D image was reoriented, by using the Frankfort horizontal (FH) plane as its reference plane. The FH plane was constructed from the right and left porions located in the most laterosuperior point of the external auditory meatus and the right orbitale (Fig 2). Cho16 proposed a 3D analysis system from a CBCT volumetric image with a set of landmarks, reference lines, and reference planes. In his system, the 3D image is reoriented according to the nasofrontozygomatic plane and the FH plane. Lagravère et al17 designated reference points such as the midpoint between the foramen lac- erum and the middorsum foramen magnum, since they are easily viewed in the 3D images. The 2D cephalometric images were derived from the 3D CT scans by creating an orthogonal projection with parallel rays, and the images were imported into V-ceph software (Osstem Implant, Seoul, Korea) for conventional 2D analysis. Landmark identifications and physical measurements were performed by the same investigator (Y.J.K). For the cephalometric analysis, 13 conventional hard-tissue cephalometric landmarks were identified, and 5 anteroposterior and 5 vertical measurements were calculated (Table II, Fig 3). The subjects were assigned to 2 groups based on their ANB angles: 14 subjects (7 boys, 7 girls) whose ANB angles ranged from 2 to 5 were allocated to group I, and 13 subjects (5 boys, 8 girls) who had ANB angles greater than 5 were allocated to group II (Table I). Five cross-sectional planes (2 frontal and 3 axial sections) and 5 volumes of the pharyngeal airway were developed in this study based on the FH plane and soft-tissue landmarks (Table III; Figs 4 and 5). Cross-sectional planes of the nasal cavity are perpendicular to the FH plane, whereas the pharyngeal cross-sections are parallel to the FH plane. Although these crosssections are not directly perpendicular to the long axis of the airway, the FH plane was used as a reference plane to standardize the plane orientation and minimize error in identifying the studied cross-sectional planes of the subjects. Various dimensions of the airway were calculated by the same examiner. Cross-sectional measurements including width, length, and area were calculated in the sectional views (frontal and axial) because they provide precise 2D visualization and linear accuracy of 2D measurements (Fig 5). 306.e4 Table II. Kim et al American Journal of Orthodontics and Dentofacial Orthopedics March 2010 Two-dimensional cephalometric variables used in this study Variable Vertical skeletal pattern Gonial angle AFH PFH FMA AFH/PFH Anteroposterior skeletal pattern A to N-perp Pog to N-Perp ANB Mn body length Facial convexity Definition The angle formed by the junction of the posterior and lower borders of the mandible Distance between nasion and menton Distance between sella and gonion The angle formed by the FH plane and the mandibular plane (Go-Me) Ratio of AFH to PFH The linear distance from Point A to nasion perpendicular The linear distance from pogonion to nasion perpendicular The difference between SNA and SNB The linear distance of the mandibular plane (Go-Me) The angle fomed by nasion, Point A, and pogonion the selected airway region. Finally, the volume of the designated airway was calculated in cubic millimeters. Lateral cephalometric variables and airway dimensions of 15 randomly selected CT scans were remeasured by the same investigator 2 weeks after the first measurements. A paired t test was used to estimate systemic error, and all measurements were free of systemic error.18 Random error was estimated by using Dahlberg’s formula19 (ME2 5 Sd2/2 n). Random errors varied from 0.49 to 2.24 mm in linear measurements, from 11.33 to 36.12 mm2 in area measurements, and from 57.36 to 91.37 mm3 in volume measurements. Descriptive statistics including the mean and standard deviation for each group were calculated by using SPSS for Windows software (version 12.0, SPSS, Chicago, Ill). Differences between groups I and II, and between the sexes, were tested by using independent t tests. Pearson’s correlation coefficient test was used to detect any relationship of different parts of the airway and between airway volume and 2D cephalometric variables. Fig 3. Landmarks, anteroposterior measurements, and vertical measurements used in this study. RESULTS Volumetric renderings of the subjects’ CT scans were acquired with the InVivoDental software, and we proceeded with volumetric analysis of the defined airways. Since airway is void space surrounded by hard and soft tissues, inversion of the 3D-rendered image is required; this converts a negative value to a positive value, and vice versa. This process removes the hard and soft tissues of the image and embodies the airway spaces of the craniofacial region including the paranasal sinuses and other empty spaces. Then sculpting was dpme to isolate the desired airway section by removing unnecessary structures; subsequently, threshold values were adjusted to eliminate imaging artifacts and refine Means and standard deviations for cephalometric, cross-sectional, and volumetric variables were compared by sex; since no sex differences were found in any measurement, the subjects were combined for subsequent analysis. Table IV gives the comparison results of groups I and II. There were statistically significant differences in the following parameters: height of the posterior nasal plane (P\0.05), pogonion to nasion perpendicular distance (P \0.01), ANB (P \0.01), mandibular body length (P \0.01), facial convexity (P \0.01), and total airway volume (P \0.05). According to the lateral cephalometric analysis, group II had retruded mandibles and a greater skeletal anteroposterior discrepancy, as evidenced by the pogonion to nasion Kim et al 306.e5 American Journal of Orthodontics and Dentofacial Orthopedics Volume 137, Number 3 Table III. Cross-sectional planes and volumes of the 3D pharyngeal airway Landmark Definition Cross-sectional plane Anterior nasal plane Ana plane Posterior nasal plane Pna plane Upper pharyngeal plane Uph plane Middle pharyngeal plane Mph plane Lower pharyngeal plane Lph plane Volume Nasal airway Superior pharyngeal airway Middle pharyngeal airway Inferior pharyngeal airway Total airway A frontal plane perpendicular to the FH plane passing through ANS A frontal plane perpendicular to the FH plane passing through PNS An axial plane parallel to the FH plane passing through PNS An axial plane parallel to the FH plane passing through the caudal margin of the soft palate An axial plane parallel to the FH plane passing through the superior margin of the epiglottis Airway formed by the Ana and Pna planes Airway formed by the Pna and Uph planes Airway formed by the Uph and Mph planes Airway formed by the Mph and Lph planes Airway extending from Ana plane to Lph plane perpendicular distance, ANB, and facial convexity values. No statistically significant difference between the 2 groups was found in the cross-sectional area and volumetric measurements of the different parts of the airway. However, total airway volume, which is the sum of the 4 separate volumes of the airway, was significantly greater in group I (P\0.05). The linear measurements of the cross sections indicated that the height of the posterior nasal plane was the only significant mean found, with greater values in group I (P \0.05). Tables V and VI show the correlations among the studied variables. Table V shows the correlations of sections of the airway with each other, and Table VI shows correlations between the 2D cephalometric variables and the 3D volumetric measurements of the airway. The nasal airway volume and the superior pharyngeal airway volume had a positive correlation (P \0.01). Some analyses from the lateral cephalograms tended to be correlated with airway volume. The anterior facial heights showed positive correlations to all volumetric measurements except the middle pharyngeal airway volume. Posterior facial height showed significant correlations with total airway volume and inferior pharyngeal airway volume (P \0.05). Additionally, total airway volume was significantly correlated with ANB angle and mandibular body length (P \0.05). DISCUSSION Although the impact of respiratory function on craniofacial growth and its relevance in orthodontics has long been a controversial issue, many clinical studies have presented good evidence with sound data supporting this hypothesis. To evaluate the airway, nasal resis- tance and airflow tests, nasoendoscopy, and lateral cephalometry have been the primary means used for the last few decades.20,21 As new-generation CBCT supplements the diagnosis and treatment planning of orthodontic patients, 3D analyses of the maxillofacial skeleton and the soft tissues are possible. Our study of the pharyngeal airway with CBCT produced anatomically true images that are 3D reconstructed without magnification or distortion, allowing accurate measurement in all 3 dimensions (sagittal, frontal, and transverse) to understand fully the pharyngeal morphology in growing children.22-24 Because of the retrospective design of this study, direct examination of the patients’ nasopharyngeal functions was not possible; selection of subjects was based on previous clinical chart information at their diagnoses for orthodontic treatment, and CBCT images were used additionally to screen subjects with severe adenoid and tonsillar hypertrophy. Area measurements of adenoids in lateral cephalograms have been reported to have clinically useful correlations with gold standards such as actual tissue volumes obtained by adenoidectomy and direct observations through endoscopy.25-27 However, Aboudara et al28 found that 2D measurements of the nasopharyngeal airway area lacks much of the structural information, since the 3D structure is compressed into a 2D image. In our study, subjective grading of the adenoid and tonsil sizes in the 3D image was done, and patients with severe adenoid or tonsillar hypertrophy were considered as having infections or allergies, and they were excluded in this study. As a result, we confirmed that our patients were free of clinical signs and symptoms related to pharyngeal pathology and had no history of treatment intervention (eg, tonsillectomy or 306.e6 Kim et al American Journal of Orthodontics and Dentofacial Orthopedics March 2010 Fig 4. Five cross-sectional planes of the pharyngeal airway used in this study: A, right lateral view and B, frontal view of volume rendered images. a, Anterior nasal plane (Ana); b, posterior nasal plane (Pna); c, upper pharyngeal plane (Uph); d, middle pharyngeal plane (Mph); e, lower pharyngeal plane (Lph). C, The cross-sectional planes are shown in the lateral cephalogram. adenoidectomy) in the pharyngeal area. Thus, we assumed that the subjects were relatively healthy and showed normal patterns of nasorespiratory function. Obviously, this method of patient selection is not ideal, and we could have included patients with mild pharyngeal diseases that could not be detected. According to a study by Laine-Alava and Minkkinen,29 however, a history or symptoms of upper respiratory diseases have no influence on variables related to nasorespiratory function when the measurements are made during an asymptomatic period. The nasopharyngeal airway is mainly influenced by the adenoids, which are known to follow the lymphoid growth curve shown by Scammon et al.30 They increase rapidly from infancy, reach a peak before adolescence, and then gradually decrease to their adult sizes. Subtelny and Baker31 concluded that the growth peak of the adenoids varies from 9 to 15 years of age. In our study, children aged 9 to 12 years were selected. According to the curves of general growth of Scammon et al,30 which the maxillomandibular growth is known to follow, this period is the end of the second phase of growth when the growth rate is steady and constant before the adolescent growth spurt. Therefore, children at these preadolescent ages can have adenoids that have reached their maximum size, and considerable facial growth has occurred to reflect functional influences because they might be predisposed to the natural anatomic conditions of narrower nasopharyngeal airways. The 2D lateral cephalometric images were created from the CBCT scans primarily to assign the subjects to the 2 groups and also to ascertain significant correlations among the cephalometric variables and the airway volumes. Linear accuracy of the CBCT-derived lateral cephalometric images has been studied.32-34 Moshiri et al35 compared linear measurements of lateral cephalograms derived from CBCT with those of conventional cephalograms and direct measurements on a dry human skull, which was considered to represent the anatomic truth. For most linear measurements calculated in the sagittal plane, they found that the CBCT-derived 2D lateral cephalograms were more accurate than conventional lateral cephalograms. Moreover, generation of 2D cephalometric images from CBCT data prevents unnecessary irradiation of the patients. Regarding patient positioning, Hassan et al33 compared linear measurements on 3D surface-rendered images, 2D tomographic multiplanar reformatted slices, and 2D projection images in both ideal and rotated positions of dry human skulls. They concluded that linear measurements on all 3 images were accurate in the ideal skull position; however, the rotated skull provided linear accuracy only for 3D surface-rendered images and 2D tomographic slices. To classify the subjects based on their anteroposterior skeletal relationships, Korean norms for the ANB angle were used.36 Several reports about the ANB angle have indicated its lack of clinical significance and reliability in the determination of the anteroposterior jaw position. Hussels and Nanda37 showed that the ANB angle is influenced by rotation and vertical growth of the jaws, anteroposterior position of the nasion, and vertical American Journal of Orthodontics and Dentofacial Orthopedics Volume 137, Number 3 Kim et al 306.e7 Fig 5. Cross-sectional views of the pharyngeal airway in the 5 planes: a represents the length (axial slice) or height (frontal slice) of the airway defined by the greatest distance in the anteroposterior or vertical direction of the airway cross section; b is the width of the airway defined by the greatest distance in the right and left directions of the airway cross section. The colored region indicates the cross-sectional area of the airway. distance between Points A and B. Ferrario et al38 suggested that the orthodontic diagnosis should be based on more than 1 anteroposterior appraisal. However, the ANB angle is a commonly used cephalometric parameter in clinical orthodontics,39 and Ishikawa et al40 corroborated that it is reliable for determining the anteroposterior relationship of the jaws. Additionally, these authors showed that the ANB angle and the angle of convexity in the prepubertal assessment have high prediction accuracy for postpubertal jaw relationships. In our study, the anteroposterior analyses displayed statistically significant differences except Point A to nasion perpendicular distance, reaffirming the reliability of the ANB angle, which was used to classify our subjects. The number of subjects in our study was limited and, therefore, this investigation should be considered a pilot study. Because of the small number of subjects, data from both sexes were collected, and, fortunately, no sexual dimorphism in any cross-sectional and volumetric measurements was observed. These findings agree with those of Ceylan and Oktay41 and Freitas et al.42 Vertical cephalometric means of the 2 groups were within normal limits, and no statistically significant differences in the vertical measurements between groups I and II were observed (Table IV), eliminating the possible effects of the vertical skeletal pattern that might have contributed to the variations of the airway dimensions. In the longitudinal study of Akcam et al,43 upper and lower pharyngeal airways were measured in preadolescents according to the different rotation types, and hyperdivergent subjects had narrower lower pharyngeal airways. All cross-sectional area and volumetric measurements of the subregions of the pharyngeal airway were greater in group I. However, they were not statistically significant, indicating that segmental airway capacities are not related to mandibular deficiencies (Table IV). This agrees with previous 2D studies that claimed no association of airway dimensions with malocclusion types.12,41,42 Ceylan and Oktay41 asserted that, as skeletal anteroposterior relationship changes, pharyngeal structures undergo postural modifications, and hence the size of the airway remains constant. Interestingly, total airway volume, the sum of the 4 subregions of the airway from the nasal cavity and the nasopharynx to the oropharyngeal region above the 306.e8 Kim et al Table IV. Descriptive statistics of groups I and II American Journal of Orthodontics and Dentofacial Orthopedics March 2010 Group I (n 5 14) Ana plane Pna plane Uph plane Mph plane Lph plane Cephalometric analysis Airway volume Height Width Cross-sectional area Height Width Cross-sectional area Length Width Cross-sectional area Length Width Cross-sectional area Length Width Cross-sectional area Gonial angle AFH PFH PFH/AFH FMA Point A to nasion perpendicular Pogonion to nasion perpendicular ANB Mandibular body length Facial convexity Nasal airway Superior pharyngeal airway Middle pharyngeal airway Inferior pharyngeal airway Total airway Group II (n 5 13) Mean SD Mean SD Intergroup difference P 44.62 16.48 263.51 22.15 25.85 292.93 22.98 29.72 494.93 18.25 25.38 321.86 17.34 29.63 427.68 125.94 116.02 73.09 0.63 29.72 –1.15 –6.84 2.42 68.22 5.04 13479.62 2620.77 1581.23 3278.00 20959.62 6.03 1.55 71.47 1.17 2.14 70.77 5.61 5.55 159.05 5.65 5.68 129.11 4.96 3.12 183.11 5.90 5.06 5.61 0.04 4.05 2.87 5.05 1.10 4.99 3.33 2547.12 899.23 509.83 1101.55 3611.26 40.32 14.91 216.92 19.42 25.40 258.04 22.45 28.63 467.64 15.44 23.57 250.96 16.18 28.72 363.66 125.30 111.96 69.32 0.62 32.22 –1.16 –12.79 5.85 63.10 12.10 11124.00 2138.38 1402.92 2498.77 17164.08 8.67 3.07 95.07 2.01 2.25 77.46 4.64 5.12 161.03 4.44 4.11 99.99 5.39 4.14 148.17 5.26 6.81 5.49 0.02 2.25 2.29 3.91 1.15 3.03 3.18 3302.82 658.27 662.49 1095.03 4238.46 0.16 0.11 0.17 0.03* 0.61 0.24 0.79 0.61 0.67 0.17 0.36 0.13 0.57 0.53 0.34 0.77 0.10 0.10 0.41 0.06 1.00 0.01* \0.01† \0.01† \0.01† 0.06 0.13 0.45 0.08 0.02* Linear measurements (mm), area measurements (mm2), volumetric measurements (mm3), angular measurements ( ). *P \0.05; †P \0.01. epiglottis, appeared to be significantly greater in group I. From these contrasting results, we inferred that each subregion of the upper airway does not specifically represent a patient’s whole upper airway capacity, and, therefore, comprehensive assessment of the entire upper airway is needed in patients who require functional examination. Further studies with larger samples are needed to investigate certain airway subregions that might be significantly correlated to other skeletal patterns such as mandibular prognathism and vertical growth pattern. Additionally, evaluation of discriminating capacities of airway parts limited by different anatomic landmarks might show specific regions of the airway that are responsible for significant relationships between the airway and the craniofacial structures. Linear analysis of the cross-sections showed that the nasal airway dimension is influenced by skeletal pattern. The height of the posterior nasal cavity was significantly greater in group I, and the rest of the crosssectional dimensions showed greater values in group I, but they lacked statistical significance. Alves et al12 compared 3D airways of adult skeletal Class II and Class III patients, and concluded that nasal cavity width had statistical significance between the 2 groups, whereas the height of the nasal cavity did not. In contrast, Kikuchi11 found in his 3D airway study that the oropharyngeal region of the airway was influenced by the skeletal pattern. He maintained that airway morphology, rather than size, is influenced by the anteroposterior position of the mandible and suggested that airway volume remains constant by horizontal and vertical compensation mechanisms of the muscles adjacent to the pharynx. Nasal airway volume and superior pharyngeal airway volume were positively correlated (Table V), indicating a close relationship of the anterior and posterior parts of the upper airway. Located above the hard palate, these 2 sections of the airway are not only anatomically adjacent, but also their volumetric dimensions have a direct relationship. Linder-Aronson3 studied the Kim et al 306.e9 American Journal of Orthodontics and Dentofacial Orthopedics Volume 137, Number 3 Table V. Correlations among airway volumes Nasal airway Superior pharyngeal airway Middle pharyngeal airway Inferior pharyngeal airway Pearson correlation P value Pearson correlation P value Pearson correlation P value Pearson correlation P value Nasal airway Superior pharyngeal airway Middle pharyngeal airway Inferior pharyngeal airway 1 0.542 0.004* 1 0.343 0.086 0.199 0.330 1 0.159 0.437 0.362 0.069 0.375 0.059 1 ˙ 0.542 0.004* 0.343 0.086 0.159 0.437 ˙ 0.199 0.330 0.362 0.069 ˙ 0.375 0.059 ˙ *P \0.01. Table VI. Correlations between cephalometric variables and airway volumes Gonial angle AFH PFH PFH/AFH FMA Pt A to N perp Pog to N perp ANB Mn body Facial conv Nasal airway Pearson correlation P value Superior pharyngeal Pearson airway correlation P value Middle pharyngeal Pearson airway correlation P value Inferior pharyngeal Pearson airway correlation P value Total airway Pearson correlation P value 0.01 0.57 0.37 0.00 0.00 –0.12 0.05 –0.36 0.33 –0.28 0.95 –0.13 \.01† 0.07 0.51 0.39 0.99 0.07 0.99 –0.10 0.56 –0.09 0.80 –0.07 0.07 –0.14 0.10 0.33 0.16 –0.09 0.53 0.15 \.01† 0.06 0.33 0.19 0.74 –0.04 0.63 –0.01 0.67 0.07 0.73 0.21 0.49 –0.31 0.10 0.22 0.66 –0.25 0.83 0.18 0.95 –0.37 0.73 –0.15 0.31 0.06 0.13 –0.32 0.27 0.32 0.23 –0.34 0.12 –0.42 0.11 0.42 0.09 –0.35 0.03* 0.08 0.46 –0.33 0.10 0.41 0.36 0.39 0.10 –0.08 0.03* 0.04* 0.66 0.47 0.39 0.05 0.06 –0.12 0.46 –0.13 0.77 0.07 0.70 \.01† 0.02* 0.80 0.57 0.52 0.74 0.03* Pt, Point; N, nasion; perp, perpendicular; Pog, pogonion; Mn, mandibular; conv, convexity. *P \0.05; †P \0.01. relationship of the upper and lower parts of the airway, and reported that a smaller nasopharyngeal airway is accompanied by a larger oropharyngeal airway. Ricketts2 and Dunn et al44 stated that oral breathing is related to a narrow nasopharyngeal airway width because it is easily blocked by adenoid enlargement. In our study, no significant correlations were found among the rest of the airway volumes below the hard palate. The relationship of conventional cephalometric analyses and airway volumes were evaluated; anterior and posterior facial heights were positively correlated to nasal, superior pharyngeal, and inferior pharyngeal airways, as well as to total airway volume (Table VI). This indicates that patients with vertical growth patterns are likely to have an expanded airway; this is inconsistent with studies that reported an inverse relationship between pharyngeal volume and vertical facial height.2,3,42,44,45 However, the variables used to assess vertical craniofacial patterns are different from those used in previous studies; this makes the comparison less compatible. Interestingly, anterior facial height showed strong correlations (P \0.01) to the upper part of the airway, and the nasal and superior pharyngeal airway; this agrees with Freitas et al,42 who noted that vertical growth patterns have significant correlations with the upper part of pharyngeal airways. Anteroposterior discriminants such as ANB angle and mandibular body length showed significant correlations with total airway volume, supporting the intergroup comparison of different anteroposterior skeletal patterns in this study. The negative correlation of the ANB angle and the total airway can be explained by group I (2 #ANB#5 ) having significantly greater airway volume than group II (ANB .5 ). Mandibular body length and total airway volume were both significantly greater in group I (Table IV), demonstrating a positive correlation. Hwang et al46 reported that a constricted nasopharyngeal airway is associated with retruded mandible and maxilla. On the other hand, Abu Allhaija and Al-Khateeb47 concluded that 306.e10 Kim et al anteroposterior pharyngeal airway dimensions were not affected by changes of the ANB angle. Since these previous studies were based on lateral cephalograms, more 3D studies are needed to clarify this conflicting issue. The standard deviations of the airway dimensions were significantly large in cross-sectional area and volumetric measurements. This agreed with the findings of Ozbek et al,48 who analyzed airway dimensions including width, area, and angulation in lateral headfilms of skeletal Class II growing children. The area measurement of the oropharnynx had large standard deviations, whereas the rest of the measurements such as airway width and angulation showed narrow ranges. The wide ranges of certain airway data were also evident in another study of airway morphology in skeletal Class II and Class III adults.12 Whereas angular and linear measurements on the 3D airway model were typical of the designated lengths and angles, cross-sectional areas and volumes showed markedly large standard deviations in both skeletal types. In a comparative study of the nasopharyngeal airway size using a lateral cephalometric headfilm and a CBCT scan, Aboudara et al14 found that volume has a much wider range than area of the same region of the airway, asserting that determination of airway volume from 2D lateral cephalograms is inaccurate because of inconsistencies of the 3D airway anatomy. Determined as percentages of the means, the standard deviations of the area and volume in our study ranged from 24% to 43% and 17% to 47%, respectively, indicating great variability in both parameters. Since a CBCT scan provides the most accurate dimensional analysis, it could be interpreted that much anatomic information is lost when the imaging modalities are 2D, and linear and angular measurements do not give enough information about the targeted structure.14,22-24 We showed that healthy preadolescent children with retruded mandibles have decreased total pharyngeal airway volumes. Therefore, orthodontists should be aware of the pharyngeal morphologies that might predispose these children to impaired craniofacial growth. Future investigations of longitudinal airway changes in patients with different skeletal patterns and assessment of their craniofacial growth with 3D superimpositions will allow better understanding of the relationship between respiratory function and craniofacial morphology. CONCLUSIONS The number of subjects available for this investigation was small; therefore, it should be considered a pilot study. It was conducted to examine a possible significant relationship between airway size and maxillom- American Journal of Orthodontics and Dentofacial Orthopedics March 2010 andibular growth patterns in healthy preadolescent children without evident pharyngeal pathology. According to our results, we can conclude the following. 1. 2. 3. 4. Accurate volumetric determination of 3D pharyngeal airway is possible in preadolescents by using CBCT scans. There is no sexual dimorphism in the 2D lateral cephalometric analysis or the 3D airway measurements of preadolescents. The mean total airway volume, extending from the anterior nasal cavity and the nasopharynx to the epiglottis, of retrognathic patients was significantly smaller than that of patients with a normal anteroposterior skeletal relationship. On the other hand, differences in volume measurements of the 4 subregions of the airway were not found to be significantly different between the 2 groups. In preadolescents, volumetric measurements of the airway are significanlty correlated to anteroposterior and vertical cephalometric variables, mainly anterior facial height and ANB angle. We thank Kyung-Min Oh for her contributions to data collection for this study. REFERENCES 1. Angle E. Treatment of malocclusion of the teeth. Philadelphia: SS White Manufacturing Company; 1907. 2. Ricketts RM. Respiratory obstruction syndrome. Am J Orthod 1968;54:495-507. 3. Linder-Aronson Adenoids S. Their effect on mode of breathing and nasal airflow and their relationship to characteristics of the facial skeleton and the denition. A biometric, rhino-manometric and cephalometro-radiographic study on children with and without adenoids. Acta Otolaryngol Suppl 1970;265:1-132. 4. Moore A. Observations on mouth breathing. Bull N Z Soc Periodontol 1972;9-11. 5. Leech H. A clinical analysis of orofacial morphology and behavior of 500 patients attending an upper respiratory research clinic. Dent Pract 1958;9:57-68. 6. Gwynne-Evans E. Discussion on the mouth-breather. Proc R Soc Med 1958;51:279-82. 7. Humphreys HF, Leighton BC. A survey of antero-posterior abnormalities of the jaws in children between the ages of 2 and 5 1/2 years of age. Br Dent J 1950;88:3-15. 8. Arun T, Isik F, Sayinsu K. Vertical growth changes after adenoidectomy. Angle Orthod 2003;73:146-50. 9. Kirjavainen M, Kirjavainen T. Upper airway dimensions in Class II malocclusion. Effects of headgear treatment. Angle Orthod 2007;77:1046-53. 10. Martin O, Muelas L, Viñas MJ. Nasopharyngeal cephalometric study of ideal occlusions. Am J Orthod Dentofacial Orthop 2006;130:436.e1-9. 11. Kikuchi Y. Three-dimensional relationship between pharyngeal airway and maxillo-facial morphology. Bull Tokyo Dent Coll 2008;49:65-75. 12. Alves PV, Zhao L, O’Gara M, Patel PK, Bolognese AM. Three-dimensional cephalometric study of upper airway space in skeletal American Journal of Orthodontics and Dentofacial Orthopedics Volume 137, Number 3 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. Class II and III healthy patients. J Craniofac Surg 2008;19: 1497-507. Ludlow JB, Davies-Ludlow LE, Brooks SL, Howerton WB. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3 G and i-CAT. Dentomaxillofac Radiol 2006;35:219-26. Aboudara C, Nielsen I, Huang JC, Maki K, Miller AJ, Hatcher D. Comparison of airway space with conventional lateral headfilms and 3-dimensional reconstruction from cone-beam computed tomography. Am J Orthod Dentofacial Orthop 2009;135:468-79. Battagel JM, Johal A, Smith AM, Kotecha B. Postural variation in oropharyngeal dimensions in subjects with sleep disordered breathing: a cephalometric study. Eur J Orthod 2002;24:263-76. Cho HJ. A three-dimensional cephalometric analysis. J Clin Orthod 2009;43:235-52. Lagravère MO, Hansen L, Harzer W, Major PW. Plane orientation for standardization in 3-dimensional cephalometric analysis with computerized tomography imaging. Am J Orthod Dentofacial Orthop 2006;129:601-4. Houston WJ. The analysis of errors in orthodontic measurements. Am J Orthod 1983;83:382-90. Dahlberg G. Statistical methods for medical and biological students. London, United Kingdom: G: Allen & Unwin; 1940. Major MP, Flores-Mir C, Major PW. Assessment of lateral cephalometric diagnosis of adenoid hypertrophy and posterior upper airway obstruction: a systematic review. Am J Orthod Dentofacial Orthop 2006;130:700-8. Vig KW. Nasal obstruction and facial growth: the strength of evidence for clinical assumptions. Am J Orthod Dentofacial Orthop 1998;113:603-11. Parks ET. Computed tomography applications for dentistry. Dent Clin North Am 2000;44:371-94. Mah J, Hatcher D. Three-dimensional craniofacial imaging. Am J Orthod Dentofacial Orthop 2004;126:308-9. Ziegler CM, Woertche R, Brief J, Hassfeld S. Clinical indications for digital volume tomography in oral and maxillofacial surgery. Dentomaxillofac Radiol 2002;31:126-30. Maw AR, Jeans WD, Fernando DCJ. Inter-observer variability in the clinical and radiological assessment of adenoid size, and the correlation with adenoid volume. Clin Otolaryngol Allied Sci 1981;6:317-22. Holmberg H, Linder-Aronson S. Cephalometric radiographs as a means of evaluating the capacity of the nasal and nasopharyngeal airway. Am J Orthod 1979;76:479-90. Jeans WD, Fernando DC, Maw AR. How should adenoidal enlargement be measured? A radiological study based on interobserver agreement. Clin Radiol 1981;32:337-40. Aboudara CA, Hatcher D, Nielsen IL, Miller A. A three-dimensional evaluation of the upper airway in adolescents. Orthod Craniofac Res 2003;6:173-5. Laine-Alava MT, Minkkinen UK. Should a history of nasal symptoms be considered when estimating nasal patency? Angle Orthod 1999;69:126-32. Scammon RE, Harris JA, Jackson CM. The measurement of man. Minneapolis: University of Minnesota Press; 1930. Subtelny JD, Baker HK. The significance of adenoid tissue in velopharyngeal function. Plast Reconstr Surg 1956;17:235-50. Kim et al 306.e11 32. Brown AA, Scarfe WC, Scheetz JP, Silveira AM, Farman AG. Linear accuracy of cone beam CT derived 3D images. Angle Orthod 2009;79:150-7. 33. Hassan B, van der Stelt P, Sanderink G. Accuracy of three-dimensional measurements obtained from cone beam computed tomography surface-rendered images for cephalometric analysis: influence of patient scanning position. Eur J Orthod 2009;31: 129-34. 34. Kumar V, Ludlow J, Soares Cevidanes LH, Mol A. In vivo comparison of conventional and cone beam CT synthesized cephalograms. Angle Orthod 2008;78:873-9. 35. Moshiri M, Scarfe WC, Hilgers ML, Scheetz JP, Silveira AM, Farman AG. Accuracy of linear measurements from imaging plate and lateral cephalometric images derived from cone-beam computed tomography. Am J Orthod Dentofacial Orthop 2007;132: 550-60. 36. Joo MJ. Analysis of the dento-facial complex in Koreans. Korean J Orthod 1970;1:21-7. 37. Hussels W, Nanda RS. Analysis of factors affecting angle ANB. Am J Orthod 1984;85:411-23. 38. Ferrario VF, Sforza C, Miani A Jr, Tartaglia GM. The use of linear and angular measurements of maxillo-mandibular anteroposterior discrepancies. Clin Orthod Res 1999;2:34-41. 39. Del Santo M Jr. Influence of occlusal plane inclination on ANB and Wits assessments of anteroposterior jaw relationships. Am J Orthod Dentofacial Orthop 2006;129:641-8. 40. Ishikawa H, Nakamura S, Iwasaki H, Kitazawa S. Seven parameters describing anteroposterior jaw relationships: postpubertal prediction accuracy and interchangeability. Am J Orthod Dentofacial Orthop 2000;117:714-20. 41. Ceylan I, Oktay H. A study on the pharyngeal size in different skeletal patterns. Am J Orthod Dentofacial Orthop 1995;108: 69-75. 42. de Freitas MR, Alcazar NM, Janson G, de Freitas KM, Henriques JF. Upper and lower pharyngeal airways in subjects with Class I and Class II malocclusions and different growth patterns. Am J Orthod Dentofacial Orthop 2006;130:742-5. 43. Akcam MO, Toygar TU, Wada T. Longitudinal investigation of soft palate and nasopharyngeal airway relations in different rotation types. Angle Orthod 2002;72:521-6. 44. Dunn GF, Green LJ, Cunat JJ. Relationships between variation of mandibular morphology and variation of nasopharyngeal airway size in monozygotic twins. Angle Orthod 1973;43: 129-35. 45. Behlfelt K, Linder-Aronson S, McWilliam J, Neander P, LaageHellman J. Cranio-facial morphology in children with and without enlarged tonsils. Eur J Orthod 1990;12:233-43. 46. Hwang YI, Lee KH, Lee KJ, Kim SC, Cho HJ, Cheon SH, et al. Effect of airway and tongue in facial morphology of prepubertal Class I, II children. Korean J Orthod 2008;38:74-82. 47. Abu Allhaija ES, Al-Khateeb SN. Uvulo-glosso-pharyngeal dimensions in different anteroposterior skeletal patterns. Angle Orthod 2005;75:1012-8. 48. Ozbek MM, Memikoglu TU, Gogen H, Lowe AA, Baspinar E. Oropharyngeal airway dimensions and functional-orthopedic treatment in skeletal Class II cases. Angle Orthod 1998;68: 327-36.