medication - Australian Commission on Safety and Quality in Health
advertisement

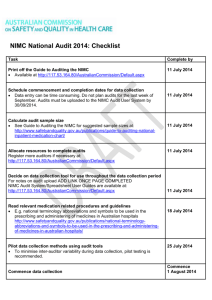
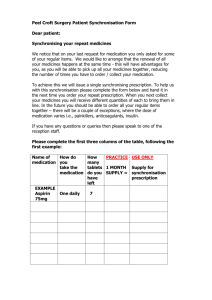
MEDICATION SAFETY The Australian Commission on Safety and Quality in Health Care Included in this issue: ISSUE 7 • FEBRUARY 2012 will not need to complete an expression of interest form to participate in phase 2. • NIMC VTE Pilot Phase 2 Now open • User-applied Labelling Recommendations • National Tall Man Lettering • New medication reconciliation resources • NIMC 2010 National Audit prescribing section will be piloted. Currently there • NIMC in psychiatric facilities are gaps between VTE prophylaxis evidence and • Dabigatran: Risk of bleeding practice and evidence suggests that point of About the NIMC VTE Pilot A draft National Inpatient Medication Chart (NIMC) with a pre-printed venous thromboembolism (VTE) risk assessment and prescribing prompts increase the rate of VTE risk NIMC VTE Pilot Phase 2 assessment and prophylaxis prescribing. The Australian Commission on Safety and Quality The aim of the NIMC VTE Pilot is to evaluate the in Health Care (ACSQHC) invited Australian hospitals to participate in the NIMC VTE Pilot efficacy and safety of a pre-printed VTE risk assessment and prescribing section in the NIMC Phase 2. on VTE risk assessment documentation and The NIMC VTE Pilot Phase 2 will pilot a draft NIMC mechanical) in adult patients admitted to with pre-printed VTE prophylaxis section and will run from March to the end of November 2012. Detailed information is provided in the expressions of interest invitation document which is available on the ACSQHC web site at http://www.safetyandquality.gov.au/internet/saf ety/publishing.nsf/Content/NIMC_006_NationalAu prophylaxis prescribing (pharmacological and hospital. The first phase of piloting involved 19 hospitals in three states and was conducted from August 2010 to February 2011. This pilot demonstrated a significant increase in the documentation of VTE risk assessment and prescribing of dit pharmacological prophylaxis. The rate of Hospitals interested in participating should read unchanged. The Phase 1 three month post- the invitation to understand what is required and whether they are eligible to participate. Expressions of interest should be submitted on the NIMC VTE Pilot Phase 2 Expression of Interest form mechanical prophylaxis ordering was implementation evaluation report is available on the ACSQHC web site. NIMC VTE Pilot Phase 2 will build on the results from on the web site. phase 1. Hospitals will use a draft version of the Completed expression of interest forms can be been modified to address issues identified in the emailed to mail@safetyandquality.gov.au Enquiries can be directed to Ms Helen Stark on 02 9126 3521. Closing date for expressions of interest is 29 February 2012. NIMC VTE Pilot Phase 1 sites NIMC with a VTE prophylaxis section that has first phase of the pilot. Pending the pilot final report, a revised version of the NIMC with a VTE prophylaxis section is expected to be available for introduction nationally in mid-2013. National Recommendations for Userapplied Labelling of Injectable Medicines Implementation of the National pre-printed sheet of sterile labels for use on the perioperative sterile field and results are expected to be reported in April 2012. Recommendations for User-applied Labelling of South Australia is developing an online e-learning Injectable Medicines, Fluids and Lines (Labelling tool for educating nursing staff about the Recommendations) is progressing in hospitals and Labelling Recommendations, available labels and health services. Implementation resources for the how to use them. This education tool will be Labelling Recommendations are available at available on the ACSQHC web site with a self- http://www.safetyandquality.gov.au/internet/saf assessment tool. ety/publishing.nsf/Content/PriorityProgram- ACSQHC recognises the importance of stability for 06_UaLIMFL national standardisations within the context of a In addition to the implementation guide, slide quality assurance process. However, it has been presentation and posters, implementation necessary to make a single change to the resources have been updated to include: container labels effective from November 2011. A • third patient identifier (date of birth) has been A set of frequently asked questions in which implementation issues are addressed; • An issues register in which referred national implementation issues are listed with decisions and resulting actions; • A poster demonstrating application of the Labelling Recommendations alongside included on container labels to comply with the National Safety and Quality Health Service Standard: Patient Identification and Procedure Matching. Container labels have been revised to include date of birth as shown below. Example of label including patient date of birth labelling standard AS/NZS4375 in perioperative areas; and • Gap analysis and audit tools from South Australia and Victoria to assist with implementation. Implementation of the Labelling Recommendations is an evolving process and ACSQHC invites health services to contact us for matters not addressed by the FAQs and the Issues Register by email on mail@safetyandquality.gov.au Anaesthesia, intensive care, perioperative and emergency services, in particular, continue to raise important issues in relation to identification of medicines and implementation of the Labelling Recommendations. ACSQHC has established the Labelling Recommendations Reference Group to advise on maintenance of the Labelling Recommendations and the group will hold an initial meeting in March 2012. Decisions of the group will be reported through the Issues Register. Establishing a practical suite of sterile, durable, pre-printed labels for the perioperative sterile field has proven difficult. The Calvary Wakefield Hospital, a major tertiary hospital with a strong focus on neurosurgery, cardiac services and orthopaedic surgery, is testing the suitability of a The revision is valid immediately and will be implemented as existing label stocks are exhausted. Label manufacturers and suppliers have been informed of the revision. The revised print-ready labels are available on the ACSQHC web site with updated posters for use by health facilities. Suppliers of custom procedure packs have been asked to ensure that labels included in packs to identify route of administration and medicines used on the sterile field, e.g. operating rooms and catheter labs, comply with the Labelling Recommendations. Please contact mail@safetyandquality.gov.au if you represent a label manufacturer or supplier of custom packs including labels and require further information on the Labelling Recommendations. National Tall Man Lettering The Commission has developed a standard list of Tall Man names to reduce the risk of drug selection error by health professionals when prescribing, dispensing and administering medicines with look-alike sound-alike names. The list and supporting documents are available at http://www.safetyandquality.gov.au/internet/saf ety/publishing.nsf/Content/PriorityProgram06_NTMS Tall Man lettering is designed solely for use by health professionals. For example, it should be applied in electronic medication management systems, on printed labels used for inpatient dispensing, shelving in pharmacies, ward medicines cupboards and in drug libraries for smart pumps. It is NOT designed for handwriting or for printed labels intended for consumers. having a formal medication reconciliation process. The MMP form, the new training presentation and other MMP implementation resources are available from the ACSQHC web site at http://www.safetyandquality.gov.au/internet/safet y/publishing.nsf/Content/PriorityProgram06_MedRecon Medicines list iPhone App Patients and carers with iPhones can now keep an up to date medicines list on their iPhone and email and print the list. The new Medicines List iPhone App, developed by NPS: Better Choices, Better Health, also allows people to schedule reminders which prompt them to take their medicine. This is an exciting use of technology to help patients maintain an accurate list of their medicines and for the information to be available when they present to hospital or visit their Standards Australia’s Health Informatics (IT-014) community health care provider. For more Committee has been asked to consider information on the NPS Medicines List iPhone App developing National Tall Man Lettering into an visit http://www.nps.org.au/iphonemedicineslist Australian standard. The request will be considered by the committee in the context of NIMC 2010 National Audit the large body of work it has been charged with undertaking in the near to medium future. No decision on incorporating Tall Man lettering into the Australian Medicines Terminology (AMT) has yet been made. However the National EHealth Transition Authority Ltd recently undertook an AMT roadmap survey to understand what additional information should be part of a national medicines terminology. The issue of Tall Man and AMT as a possible future development was included in the survey. Details of the survey are available from the NEHTA web site at http://www.nehta.gov.au/media-centre/featurestory/945-australian-medicines-terminologyimplementation-plan-roadmap-survey New medication reconciliation resources: National MMP training presentation A new online training presentation is available to assist healthcare professionals use the National Medication Management Plan form (MMP). The presentation uses voice over to describe how to obtain and document a complete and accurate medication history. It provides an introduction to the four steps of medication reconciliation and highlights the evidence for, and the benefits of, The National Inpatient Medication Chart (NIMC) reduces the risk of prescribing and administration errors in acute care The NIMC standardises medication information communication between doctors, nurses and pharmacist with the aim of reducing harm to patients from medication errors. The NIMC 2010 National Audit of medication charts was undertaken by nurses and pharmacists in seven jurisdictions from August to December 2010. The audit included 2,591 patients with 3,720 medication charts and 30,005 medication orders from 69 hospitals (including two private facilities). As in the 2009 audit, the 2010 audit found that some aspects of prescribing practices have improved since the introduction of the NIMC in 2006 and 2007, with a corresponding potential to Table 2: Examples of prescribing error rates reduce medication errors and possible adverse drug events. However in some areas there has Audit results (%) Criteria for missing, been little change and even a decline in the incorrect 2006 post 2009 2010 NIMC pilot audit audit N= N = 30,005 9,047 orders safety of prescribing, particularly in the use of or unclear medication audit error-prone abbreviations. Overall 11% of doses orders N= 15,416 were omitted or their administration not signed for. orders orders Unclear medication The 2010 audit report will be available shortly on names 3.0 7.6 4.0 the ACSQHC web site. Route errors (missing, 6.5 13.3 10.3 4.3 18.4 14.2 15.5 20.0 19.6 32.2 35.6 46.2 N/A 22.6 24.6 unclear, incorrect) Table 1: Rate of compliance in selected NIMC safety features Dose errors missing, unclear, incorrect Criteria for safe prescribing Rate of compliance (%) 2006 post 2009 2010 NIMC audit audit pilot N=864 N=2,591 audit 19.8 frequency errors (missing, unclear, incorrect) - PRN frequency errors Error prone abbreviations N=1,234 * Patient identification Regular, PRN, Variable 31.3 32.8 used completed (all patients) Indication documented 22.8 14.5 20.2 Patients’ weight Orders ceased correctly N/A 24.1 49.5 documented • all patients • paediatric patients Complete details of 19.1 29.4 23.1 24.4 75.7 N/A NIMC National Audit 2012 62.7 77.3 Nationally coordinated NIMC auditing will begin previous ADR documented in 2012 and take place from 1 August to 30 (drug name and reaction September. National auditing will occur every two or nil known) Warfarin orders with target 70 69.6 95.7 34.3 62.1 70 11.0 10.0 12.6 INR documented Indication for warfarin documented Warfarin education for patients documented Patients with drugs years thereafter at the same time of year. Hospitals using the NIMC are invited to participate in the audit to identify areas of practice requiring improvement, to compare with peer hospitals and to track practice over time. Hospitals can collect audit data using the paper- 0.9 1.6 0.9 based NIMC Audit Form, the NIMC Audit prescribed of a similar class Spreadsheet or enter directly into the NIMC Audit (duplication) System at Medicines prescribed by 73.0 80.2 78.8 generic name Sustained release forms of www.safetyandquality.gov.au/nimcaudit. For more information on the NIMC 2012 National 37.7 46.4 61.3 drugs identified Audit, visit the ACSQHC web site at http://www.safetyandquality.gov.au/internet/saf ety/publishing.nsf/Content/NIMC_2012- * N = number of patients Table 2 shows prescribing error rates compared to previous audits. Areas where there is significant room for improvement include use of approved abbreviations and the frequency of PRN orders. NationalAudit or email Ms Angela Wai at the ACSQHC on nimc.audit@safetyandquality.gov.au You can also contact your local State or Territory representative, or quality coordinator, for further information on participating in the NIMC 2012 National Audit. NIMC in psychiatric facilities The Commission is researching NIMC use in psychiatric acute care facilities. The research is looking at NIMC issues raised by a number of health professionals working in psychiatric acute services and to assess if any additional implementation resources are required to assist safe and standard use of the NIMC in that setting. Dabigatran (Pradaxa) is one of three new oral anticoagulants approved for the prevention of venous thromboembolism after major orthopaedic surgery of the lower limb (elective total hip or knee replacement). The other agents are rivaroxaban (Xarelto) and apixaban (Eliquis). Dabigatran is also approved for prevention of stroke and systemic embolism in patients with atrial fibrillation. Incidents have been reported An ACSQHC survey of health professionals where patients admitted to hospital taking working in psychiatric acute services was held dabigatran have been commenced on other from July to November 2011. Preliminary results anticoagulants on admission to hospital as indicate that there are some specific practice prescribers were not aware that the drug was an issues in psychiatric acute services which affect anticoagulant. NIMC use and that standardised ordering of certain medicines, particularly clozapine, present difficulties. There is no antidote or specific reversal agent for these agents. Health services should ensure prescribers are aware of: • New anticoagulants; • Risks associated with their use; • Monitoring requirements; • Management in the peri-operative period; and • Management of bleeding. Links to state safety notices on the new oral A report on the ACSQHC survey, and other anticoagulants have been posted on the research, will be considered by the Health ACSQHC web site at Services Medication Expert Advisory Group in http://www.safetyandquality.gov.au/internet/saf February along with recommendations. The ety/publishing.nsf/Content/NIMC_005_Medicatio report, and meeting outcomes, will be available n-Safety-Alerts on the ACSQHC web site shortly after. Adverse events associated with the new oral anticoagulants should be reported to the TGA at Safety advisory on dabigatran (Pradaxa): Risk of bleeding http://www.tga.gov.au/safety/problemmedicine-report-adr.htm On 3 November 2011 the Therapeutic Goods Administration (TGA) updated the safety advisory on the risk of bleeding relating to the use of the oral anticoagulant dabigatran. The update, available at http://www.tga.gov.au/safety/alertsmedicine-dabigatran-111005.htm includes new recommendations for monitoring kidney function when prescribing the drug. From June 2009 to 0ctober 2011, TGA received 297 reports of adverse events with dabigatran; 196 of them serious of which 70 were bleeding events. National Safety and Quality Health Service Standards ACSQHC has developed ten National Safety and Quality Health Service (NSQHS) Standards to drive the implementation and use of safety and quality systems and improve the quality of health service provision in Australia. The NSQHS Standards were selected because they address areas where: • The effect is on a large number of patients; • There is a known gap between the current situation and best practice outcomes; and • Improvement strategies exist that are A number of other standards contain criteria that evidence-based and achievable. are relevant to medication safety including From early 2013 hospitals and day procedure services will be assessed against the NSQHS Standards as part of their accreditation processes. Medication Safety is standard 4. The aim of the medication safety standard is to ensure competent clinicians safely prescribe appropriate medicines to informed patients and carers. Patient Identification and Procedure Matching, Clinical Handover and the two overarching standards; Governance for Safety and Quality in Health Service Organisations and Partnering with Consumers. The NSQHS Standards, fact sheets and other information to support health services implement the NSQHS are available from the ACSQHC web site. Guides to implementation are in development and will be available shortly. http://www.safetyandquality.gov.au/internet/saf ety/publishing.nsf/Content/PriorityProgram-07 Safer Naming, Labelling and Packaging of Medicines Round Table A report on the National Round Table on Safer Naming, Labelling and Packaging of Medicines is available on the Commission web site at The standard includes 5 criteria: • Governance for medication safety; • Documentation of patient information; • Medication management processes; • Continuity of medication management; and • Communicating with patients and carers. A full copy of the Medication Safety Standard is contained in the NSQHS Standards. It includes the criteria, items and actions required for health services to meet the Standard. ACSQHC tools and resources to assist health services implement the Medication Safety Standard include: http://www.safetyandquality.gov.au/internet/saf ety/publishing.nsf/Content/PriorityProgram06_SaferNaming The report contains recommendations for future activity and will guide national activity. The round table was held in Sydney on 24 May 2011. Co-hosted by ACSQHC and the Therapeutic Goods Administration (TGA), the round table brought together the pharmaceutical industry, regulators, policy-makers and consumers. The aim of the round table was to improve patient safety in relation to medicines naming, labelling and packaging through agreement and coordination amongst key stakeholders. Review of labelling and packaging • NIMC and support materials; • National Terminology, Abbreviations and packaging regulatory framework for prescription Symbols to be used in the Prescribing and medicines, over the counter medicines and Administering of Medicines in Hospitals; complementary medicines. A public consultation National Medication Management Plan form paper is expected to be released in early 2012. • • The TGA has initiated a review of the labelling and and support materials; Information on the review is available from National Recommendations for User-applied review.htm Labelling of Injectable Medicines, Fluids and Lines; • National Tallman Lettering List; and • Medication safety alerts. http://www.tga.gov.au/industry/labelling-