Glaucoma and refractive error
advertisement

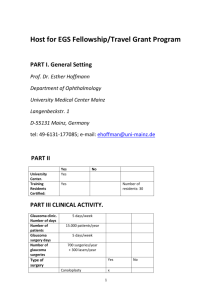
Refractive Error and Correction Options Pharmacy Society Australia Presentation The Vision Initiative Professional Education Program Outline Vision 2020 Australia The Vision Initiative Common causes of blindness and vision impairment Refractive Error Correction of Refractive Error Pharmacy’s role in prevention of avoidable blindness How to refer to vision services Vision 2020 - The Vision Initiative Save Your Sight – Get Tested The key message of The Vision Initiative Funded by the Victorian Department of Human Services Implemented by Vision 2020 Australia and members such as Optometrists Association Australia and RANZCO Victoria’s public health response to the National Framework The Vision Initiative Victorian Partner Service Providers Able Australia Blind Citizens Australia Brotherhood of St Laurence Centre for Eye Research Australia Diabetes Australia – Vic Glaucoma Australia Guide Dogs – Victoria International Diabetes Institute Kerataconus Australia Macular Vision Loss Support Society of Australia Optometrists Association Australia (Victorian Division) Orthoptic Association of Australia Retina Australia – Vic The Royal Australian and New Zealand College of Ophthalmologists Royal Victorian Eye and Ear Hospital Seeing Eye Dogs Australia St Vincent’s health Victorian College of Optometry Vision Australia Causes of vision impairment 80% vision impairment and blindness is caused by five conditions: Under-corrected refractive error (62%) Cataract (14%) Age-related Macular Degeneration (AMD) (10%) Glaucoma (3%) Diabetic eye disease (2%) Structure and function of the eye Structure and function of the eye Retinal blood vessels Macula (fovea in centre) Optic nerve Age-related Macular Degeneration (AMD) Progressive condition affecting the central area of the retina Age-related maculopathy (ARM) in the early stages If disease progresses to AMD, irreversible loss of central vision occurs, usually in both eyes Advanced AMD View with Age-related Macular Degeneration AMD Prevention Tobacco use Physical Activity Adequate intake of fruit and vegetables - Dark leafy green vegetables - Fish (Omega 3) Reduce saturated fat, use sparingly in cooking American reports implicating margarine may not be relevant to Australia Diabetic Retinopathy Complication of longstanding diabetes 25 times more vision loss than those without Elevated sugar levels damage the sensitive blood vessels at the back of the eye 90 % of those with diabetes will develop some changes in their eyes Painless loss of vision due to leaky blood vessels or scar tissue formation in the retina Diabetic Retinopathy Healthy retina Broken blood vessels Cause scaring and loss of vision Diabetic Retinopathy Prevention Early detection and treatment essential Regular review and coordinated care approach by GP and other eye care practitioners Target levels for blood sugar levels < 7.0 blood pressure < 130/80 Cholesterol (LDL ideal) < 2.6 mmol/L Cataract Progressive age related change Opacification of the internal lens of the eye Symptoms include - Painless blurring and ‘dullness’ of vision - Increased awareness of glare e.g. car lights - Reduced contrast sensitivity Vision unable to be corrected with glasses Mature Cataract Glaucoma Topic of the second part of tonight’s presentation 50% suffers undetected! So… Save Your Sight – Get Tested for the ‘sneak thief of sight’ Refraction is the passage of light through the ocular media to focus an image onto the retina Under-corrected refractive error - focus defect Long-sightedness (hyperopia) Light focuses behind the retina Trouble with near - effort (& possibly distance vision) Short-sightedness (myopia) Light focuses in front of the retina Trouble with distance vision Astigmatism (oval shaped eye) Distance and/or near focus difficulty Presbyopia (age related near focus difficulty) >40 yrs should have eye test, incidence increases with age Types of Refractive Error Long-sightedness (hyperopia) Near Vision blur, asthenopia &/or headache with near vision tasks Print ‘runs together’ Short concentration for near tasks Associated with esotropia (one eye turning in) Types of Refractive Error Short sightedness (myopia) Distance vision blur, squinting in distance, TV and night Driving difficulties Poor concentration for board based learning in school Headache and eyestrain less likely Types of Refractive Error Astigmatism (oval shaped eye) Can be of myopic or hyperopic or mixed type causing dist &/or near problems Strong association of headache and eyestrain, squinting of eyelids for dist &/or near Types of Refractive Error Presbyopia (age focus difficulty) Symptoms similar to hyperopia except >40 YOA Holds near objects at arms length should have eye test as incidence of most diseases increases with age Correction Options for Refractive Error Spectacles § § Contact Lenses Refractive Surgery Corneal Onlays / Inlays Spectacles Convenient, non-invasive, easily updated Protective – trauma & radiation Sunsmart – slip, slop, slap Problematic in some environments – fogging, perspiration, smudging Restrict peripheral vision, Bi/Multifocals zone dependent Not ideal for physical activity – damage, dislodgement Ready-mades (“Magnifying Glasses”) Won’t ‘damage your eyes’ but asthenopia & headaches possible Neglecting eyecare leads to vision loss through non-detection or late detection Giving good advice with each sale Save Your Sight – Get Tested Contact Lenses Less convenient than specs, mildly invasive, easily updated if disposable Some splash protection, can be UV absorbing Problematic in dusty dirty environments, allergies & atopy Danger of infection – pseudomonas aeruginosa, acanthamoeba, fungal keratitis Good for sports Contact Lens Problems minor vs. medical emergency Sign/Symptom Less Serious More Serious Pain bilateral unilateral CL removal reduces persists or Photophobia Redness mild surface conjunctival none to mild due to lacrimation severe in sunlight deeper tissues ring or sector around iris profound > 2 lines on letter chart Vision loss Refractive Surgery Radial Keratotomy (RK) -> <- Photorefractive Keratectomy (PRK) Laser-Assisted In Situ Keratomileusis (LASIK)-> <-Corneal Onlays / Inlays Experimental Presbyopic Inlay Pharmacy’s Role in Prevention of Avoidable Blindness Engage clients on eyecare issues Over 40? Change in vision? Family History of Eye Disease? Diabetes? Wearing / Buying Ready-mades? Save Your Sight – Get Tested The Victorian Eyecare Service (VES) Provides low cost eye care and glasses to holders of Pensioner Concession Cards (PCC) and Health Care Cards (HCC) Funded by the Department of Human Services Staffed by qualified optometrists Glasses start from $33.00 a pair – get Tested! Consultations are bulk billed to Medicare Operates throughout Victoria Contact details: - Corner of Cardigan and Keppel Street Carlton - Telephone: 9349 7400 - www.optometry.unimelb.edu.au/clinicalservices/index.htm Low vision service providers Low vision organisations and some optometrists provide low vision services These services help people to adjust to vision impairment by learning new ways to carry out daily tasks They assist people in making the most of their remaining vision Referring to low vision service providers Able Australia Telephone: 1300 ABLEOZ (1300 225 369) Website: www.ableaustralia.org.au Email: info@ableaustralia.org.au Guide Dogs Victoria www.guidedogs.asn.au Ph: 9854 4467 Email: referrals@guidedogs.asn.au Seeing Eye Dogs Australia www.seda.org.au Ph: 1800 037 773 Vision Australia www.visionaustralia.org.au Ph: 1300 VISION (1300 847 466) Management of Glaucoma • An overview of Glaucoma • Practical aspects for Pharmacists • Ophthalmologists’ management • Ways Pharmacists can assist Glaucoma • • Glaucoma can be considered a generic name for a group of diseases causing optic neuropathy and visual field loss, usually in the presence of raised intraocular pressure. Glaucoma is often asymptomatic until late stages as the peripheral vision is often lost first causing a “tunnel vision” effect Glaucoma It is estimated that visual impairment due to glaucoma will double over the next two decades Year Age 60-69 70-79 80-89 >90 2004 2010 2014 2020 2024 1,191 1,487 1,853 2,083 2,225 3,069 3,259 3,653 4,793 5,616 8,669 10,268 10,924 12,387 14,176 813 1,081 1,229 1,359 1,489 Total VI 13,741 16,096 17,658 20,623 23,507 Total blind 8,561 9,890 11,289 12,595 Prevalence of visual impairment from Glaucoma Source: Access Economics Pty Limited From VIP, BMES and ABS population data Glaucoma in Australia Demographic distribution of glaucoma in Australians over 40 10 9 8 7 6 Undiagnosed Diagnosed 5 4 3 2 1 0 40-49 50-59 60-69 70-79 80-89 >90 Age It is estimated only half of Australians currently living with glaucoma have been diagnosed Source: Taylor (2001) Glaucoma risk factors • • • • • • • • Family history (4 times increased risk) Age (increased risk after age 40) Corneal thickness (thin) High myopia Diabetes Race (African descent) Hypertension History of eye trauma QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. Glaucoma Disease Prevention • Often no “early signs” of disease • All methods of current treatment rely on the reduction of intraocular pressure • No current medication has consistently proven itself as neuro-protective or to favourably influence optic nerve perfusion Examinations for Glaucoma • • • • • Tonometry Ophthalmoscopy Perimetry Gonioscopy Retinal nerve fibre analysis Normal Abnormal Examinations for Glaucoma • Tonometry • Brief and painless procedure where the intraocular pressure is measured (normal range is 10-21mmHg) Diagnosing Glaucoma • Ophthalmoscopy • Allows for detailed examination of the retina and optic nerve head with cup:disc ratio and vessels • Gonioscopy • A slit lamp and gonioscopic mirror allows evaluation of the anatomy of the angle where the cornea meets the iris Visual field loss in Glaucoma • • • The longer treatment is delayed the greater the loss in vision Visual field changes are imperceptible at first and more rapid as time progresses Visual field loss shows after 50% of nerve firbres are damaged Diagnosing Glaucoma • Glaucoma vs. ocular hypertension • OHT = IOP of up to 30mmHg with normal optic discs and full visual fields • IOP above 30mmHg has increased risk of central retinal vein occlusion • Need evidence of progression and structural changes to confirm diagnosis • HRT retinal nerve fibre layer analysis is useful in closely monitoring these patients Primary open-angle glaucoma (POAG) • • • • Makes up more than 70% of all glaucoma cases Impairment of aqueous drainage through the trebecular meshwork Results in excavation and atrophy of the optic nerve head Visual field abnormalities Other types of glaucoma • Angle closure glaucoma • One of the few types that causes symptoms • Severe pain, red eye, nausea or vomiting • Extraordinarily high IOP, often 40-70mmHg • Low tension glaucoma • Rarer form of disease where optic nerve damage and vision loss occur despite normal intraocular pressure PI in Angle closure glaucoma Secondary Glaucomas • Pigmentary Pigment granules from the back of the iris flake off and slowly block drainage channels and increase IOP • Traumatic Blunt trauma to the eye tears ciliary body and resulting in blood and other debris blocking the drainage and increasing IOP • Neovascular Tissue which accompanies new blood vessels growing near the trabecular meshwork blocks drainage and increases IOP Management of Glaucoma • Topical medication for treatment of POAG – Prostaglandin analogs – Beta-blockers – Alpha-agonists – Carbonic anhydrase inhibitors – Miotics Glaucoma Medications • Beta blockers Generic Name Timolol maleate 0.5% • Drug Interactions Adverse Reactions Adrenaline, reserpine Asthma, bradycardia, depression, erectile dysfuntion Betaxolol HCl 0.25%, 0.5% Beta Blockers, Adrenaline Levobunolol HCl ophthalmic solution, USP 0.25%, 0.5% Oral Beta Blockers, Adrenaline Asthma, bradycardia, depression, erectile dysfuntion Asthma, bradycardia, depression, erectile dysfuntion Decrease production of intraocular fluid Glaucoma Medications • Prostaglandin Analogs Generic Name Drug Interactions Adverse Reactions nil Pro-inflammatory reaction of HSV/HZO, eyelash pigment changes, dry eye Bimatoprost 0.03% nil Pro-inflammatory reaction of HSV/HZO, eyelash pigment changes, dry eye Latanoprost 0.005% Eye drops containing thiomersal Pro-inflammatory reaction of HSV/HZO, eyelash pigment changes, dry eye Travaprost 0.004% • Increases drainage of intraocular fluid Glaucoma Medications • • Alpha Agonist Generic Name Drug Interactions Adverse Reactions Brimonide tartrate 0.1%, 0.15% MAOIs, CNS depressants, alcohol Oral dryness, hyperaemia, irritation Works to both decrease production of fluid and increase drainage Glaucoma Medications • • Carbonic Anhydrase Inhibitors Generic Name Drug Interactions Adverse Reactions Brinzolamide ophthalmic suspension 1% nil Blurred vision, dry eye, transient discomfort Dorzolamide HCl 2% (drops) nil Allergic reactions, ocular irritation, bitter taste Acetazolamide (oral) Salicylates, folic acid antagonists, hypoglycaemics Metabolic disturbances, fatigue, kidney stones, tingling, taste disturbance Decreases production of intraocular fluid Glaucoma Medications • • Combined Generic Name Drug Interactions Adverse Reactions Dorzolomide HCl Timolol maleate Beta Blockers, Ca channel blockers Ocular irritation, taste perversion, lacrimation Lantanaprost Timolol maleate Eye drops containing theomersal, Beta Blockers, prostaglandins, antidiabetic agents Increased iris pigmentation, irritation, eyelash changes Combination of beta blocker and carbonic anhydrase inhibitor Practical aspects for pharmacists Compliance with eye drops is a frequent issue Glaucoma patients’ medications are often modified or increased if monotherapy fails • Techniques to maximise legibility of medication labels for patients: – Large print labels – Large print medication lists – Encourage to wear their spectacles – Bold and black typeface not red How Pharmacists can assist • Liaison with GPs and eye healthcare providers • Checking for drug interactions • Eg. Topical + systemic Beta Blockers – • Alert Ophthalmologist if this occurs Discussing instillation technique • Emphasising importance of compliance • Sitting/lying down to instill drops • Having partner instill the drops for you • Pressing on tear duct • Waiting 5 minutes between using different drops Laser treatments for Glaucoma • Selective Laser Trabeculoplasty (SLT) and Argon Laser Trabeculoplasty (ALT) Laser is applied in evenly spaced spots of the trabecular meshwork Laser burns cause shrinkage and contraction of the collagen meshwork to create openings and increase aqueous outflow Laser treatments for Glaucoma • Selective laser trabeculoplasty (SLT) uses a low-energy, large-spot, very brief pulse to the trabecular meshwork SLT ALT Laser treatments for Glaucoma • Perpheral Iridotomy – Typically performed to treat narrow angle or angle closure glaucoma – YAG laser is focused on the iris root, creating an opening for the aqueous fluid to move through – Usually holes are in superior part of the iris which is covered by the upper eyelid • Less problems with glare • No double vision from “new pupil” Trabeculectomy • • Mechanical formation of an aqueous outflow channel through the sclera and into the subconjunctival space Aqueous pools into the “bleb” fluid sac and reduces IOP OCT image of bleb Save Your Sight week An integrated campaign by The Vision Initiative will promote the importance of regular eye tests for people over 40 Activity includes television, radio and newspaper advertising, media PR and a series of public events from 11-16 March Health Professionals- what can you do to help? Awareness of the campaign with increased knowledge of common eye conditions, and referral options Support the campaign by accepting and displaying promotional materials, posters, post cards in your setting Please tick box on registration sheet for us to send you materials for display. Vision 2020 Australia would like to thank John Clemens from the Optometrists Association Australia and Dr. David McKnight from the Royal Australian and New Zealand College of Ophthalmology for this presentation For more information please contact: Robyn Wallace Vision 2020 Australia (03) 9656 2020 rwallace@vision2020australia.org.au www.saveyoursight.org.au www.vision2020australia.org.au Vision 2020 Australia wishes to acknowledge the Victorian Department of Human Services for funding The Vision Initiative