Lecture Notes for Lecture 1: From Fertilization to Gastrulation
advertisement
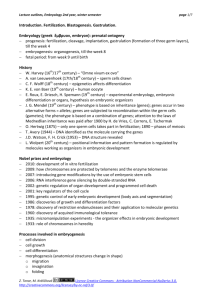
Lecture 1: From Fertilization to Gastrulation Slide 1: Title slide: From Fertilization to Gastrulation Main points: Covers Chapter 3 (First Week of Development: Ovulation to Implantation), Chapter 4 (Second Week of Development: Bilaminar Germ Disc), and Chapter 5 (Third Week of Development: Trilaminar Germ Disc) Slide 2: List of reasons for learning embryology Main points: 1. This list provides students with some of the facts about birth defects. 2. In addition to those listed, birth defects are a major contributor to our health care costs. Just to get a newborn infant with spina bifida home from the hospital can run up to $300,000, and then there are additional costs for the lifetime needs of the individual. 3. There is almost no measure for the amount of human suffering birth defects can cause, both for the affected child and his or her family. It is a very stressful situation for a family; divorce rates among those with children with birth defects are high. And if a couple thinks they are not going to get pregnant, they should remember that 50% of all pregnancies are unplanned. Slide 3: Graph showing when most structural birth defects are induced. Main points: 1. This slide is one of those “take-home message” types. It is crucial for everyone to understand that development happens fast and early in pregnancy even before women realize they are pregnant. 2. During the embryonic period (3-8 weeks; see slide), the primordia of each organ system is established, and it is at this time that each organ is most sensitive to the induction of a birth defect. It does not mean that the rest of gestation (week 9 to birth) can be ignored from a birth defects standpoint, however. For example, the brain continues to develop even postnatally and remains sensitive to insult from many factors, including drugs like alcohol (alcohol exposure during gestation is the leading cause of mental retardation), but the baby is less likely to have a major structural defect induced after the eighth week. Therefore, since most women do not go to their first prenatal visit until the eighth week (i.e., after the period of greatest sensitivity), it is imperative that birth defects prevention programs begin prior to conception! 3. Another issue is calculating embryonic age. On this slide and throughout the text, embryonic age is calculated from fertilization. Most physicians calculate the age as gestational or menstrual age and use the Last Normal Menstrual Period (LNMP) as the starting point. This practice is very inaccurate since only 50% of women ovulate within a 7-day period around the midpoint of their cycle. Some actually ovulate within 3-4 days of the end of their last menstrual period. In any case, since fertilization is supposed to occur at the midpoint of the cycle, the LNMP method Sadler, T.W.: Langman’s Medical Embryology, 11e © Lippincott Williams & Wilkins, 2010 begins 2 weeks prior to actual fertilization. Therefore, converting fertilization age to LNMP age requires adding 2 weeks. Slide 4: Cross section of a uterus, uterine tube, and ovary Main points: 1. Fertilization occurs in the ampullary region of the uterine (Fallopian) tube, and embryonic development begins immediately. 2. Development continues as the embryo moves down the tube toward the uterus. By 3 days, the morula (mulberry) stage is attained; by 4-5 days, the blastocyst stage is observed, and the embryo enters the uterine cavity. 3. At 5-6 days, the blastocyst implants. Interesting point: The process is not efficient. Approximately 50% of embryos are spontaneously aborted regardless of a woman’s nutritional, economic, or other status. Of those embryos that are lost, 50% will have a serious chromosomal defect. Slide 5: Morula stage and compaction Main points: 1. "Morula" means mulberry and is a stage attained at 3 days with 8-16 cells. Each cell is capable of forming a complete embryo (totipotent). 2. Compaction begins when cells on the outside seal themselves from the external environment by forming tight junctions. Fluid is pumped toward the inside and begins to displace the inner cells. At this stage, outer cells begin to be committed to forming trophoblast (placental) cells, while cells on the inside will form cells for the embryo. Slide 6: Blastocyst stage and implantation Main points: 1. As fluid accumulates in the center of the conceptus due to compaction and cells pumping the fluid inward, a blastocyst is formed. This structure is like a tennis ball with a liquid center. Cells on the outside form the outer cell mass or trophoblast; while cells on the inside at one pole form the inner cell mass or embryoblast. Cells from the embryoblast will develop into the embryo and represent the source of embryonic stem cells used (or not) in research. They are nearly totipotent and can differentiate into virtually any type of cell or tissue given the right growth factors and environment. This characteristic is what makes them so valuable clinically. These are the cells that the United States Government has declared off limits from funding by federal resources. 2. Implantation begins with attachment to the uterine epithelium. This process is affected by receptors on the epithelial cells that recognize specific proteins on the surface of the trophoblast cells. The process is similar to that involved in leukocytes sticking to the walls of blood vessels. 3. At approximately 6 days, the blastocyst implants. Implantation elicits an antibody response by the uterine epithelium because the embryo is a foreign body (half its genes come from dad). Normally, the embryo blocks this response, but in Sadler, T.W.: Langman’s Medical Embryology, 11e © Lippincott Williams & Wilkins, 2010 autoimmune diseases like systemic lupus erythematosus, the process may not function properly, possibly resulting in infertility. 4. The trophoblast is the invading tissue, and it differentiates into two cell types: the syncytiotrophoblast, which forms a syncytium and is actively invasive and secretes hormones like human chorionic gonadotropin (hCG), the basis for pregnancy tests; and the cytotrophoblast, which provides a proliferative pool of cells that move into the syncytiotrophoblast. 5. The invasion of the blastocyst is similar to growth of a tumor and can sometimes become unregulated. The result is formation of a hydatidiform mole. (See next slide.) Slide 7: Characteristics of hydatidiform moles Main points: As listed Interesting point: Regulation of the growth of moles is by the paternal genome. Thus, during the earliest stages of development, paternal genes regulate differentiation of the trophoblast (placenta), while maternal genes regulate growth of the embryoblast. Slide 8: Repeat of the fertilization slide (slide 3) Main point: 1. Implantation occurs at the end of the first week and usually takes place along the anterior or posterior walls of the uterus. Sometimes, however, it may occur at ectopic sites. (See next slide.) Slide 9: Sites for ectopic pregnancies Main points: 1. The most common site is in the uterine tube, but other sites may occur. 2. Ectopic pregnancies are due to the invasive nature of the trophoblast and abnormal transport or recognition of the blastocyst. 3. They are dangerous because development may proceed for several weeks or months before rupture of the site, including blood vessels, occurs, which can result in severe hemorrhaging and maternal and fetal death. Slide 10: Example of a tubal pregnancy Main points: 1. This is the most common site for an ectopic pregnancy. Slide 11: Ectopic pregnancy in the rectouterine pouch Main points: 1. This is the most common site for an ectopic pregnancy in the peritoneal cavity. The embryo falls to this position because it is the lowest site in the cavity. Slide 12: Assisted reproductive technologies (ART) Main points: Sadler, T.W.: Langman’s Medical Embryology, 11e © Lippincott Williams & Wilkins, 2010 1. The next series of slides provides some information about assisted reproductive technologies (in vitro fertilization). They are relevant because 1% of all births in the United States arise from these procedures, and there are significant complications with these pregnancies. Slide 13: Graph showing incidences and births from ART procedures Slide 14: Adverse outcomes from ART Slide 15: Graph of adverse outcomes from ART Main points: 1. There is an increase in low birth weight, very low birth weight, and premature births among ART babies. Most of this is due to the fact that the techniques often result in multiple birth pregnancies, which are always high risk. Slide 16: Graph showing low birth weight in ART singletons Main points: 1. Even in singleton ART pregnancies, there is an increased risk for low birth weight, possibly suggesting that something inherent in the procedures is having an adverse effect. Slide 17: ART and birth defects Main points: 1. There is an increase in birth defects among ART pregnancies, yet most centers do not warn people about this possibility. 2. There are beginning to be some long-term follow-up studies of ART infants in which it appears that there may be some developmental issues that have not been detected at birth. Slide 18: Continued differentiation of the trophoblast and embryo Main points: 1. About 1 or 2 days after implantation, the embryo and trophoblast each begin to differentiate into two layers: The embryoblast differentiates into a dorsal layer, the epiblast, and a ventral layer, the hypoblast; the trophoblast forms the syncytiotrophoblast and cytotrophoblast. 2. Placental development continues as the syncytiotrophoblast burrows deeper into the uterine tissue. Slide 19: Cross sections through implantation sites. The slide is used for a demonstration of both early placental and embryonic development. Main points (placenta): 1. Trophoblast cells contribute to the fetal portion of the placenta. 2. On the ninth day, spaces (lacunae) form in the invading syncytiotrophoblast. Sadler, T.W.: Langman’s Medical Embryology, 11e © Lippincott Williams & Wilkins, 2010 3. Within a few days, these spaces fill with maternal blood as the syncytiotrophoblast erodes uterine vessels. 4. As the spaces fill with blood, finger-like projections of syncytiotrophoblast covering a core of cytotrophoblast project into the blood-filled regions. These represent primary villi, and most form on the embryonic pole. 5. Another layer, the extraembryonic mesoderm, forms around the embryo and yolk sac and inside the cytotrophoblast. Initially, this layer is solid, but soon spaces appear causing a separation into two layers: extraembryonic splanchnopleuric mesoderm (splanchnic or visceral layer) around the yolk sac and embryo, and extraembryonic somatopleuric mesoderm (somatic or parietal layer) lining the inside of the cytotrophoblast. (All of these terms are potentially confusing. Therefore, it is perhaps best to refer to these layers as visceral and parietal because these are the terms that will be used later for all other layers that relate to organ systems. For example, the layer on the external surface of an organ is the visceral layer [visceral pleura, visceral peritoneum, etc.], whereas the layer along the body cavity or wall is called the parietal layer [parietal pleura, parietal peritoneum, etc.]. Similarly, the mesoderm layer that lies adjacent to the embryo and yolk sac is the visceral layer, while the layer adjacent to the trophoblast is the parietal layer). The parietal layer eventually is referred to as the chorionic plate or chorion, and the space between the layers is called the chorionic cavity. Both layers are continuous at the connecting stalk and will be important for forming blood vessels. Slide 19: Repeat to talk about the embryo's development Main points (embryo): 1. During the second week, the embryoblast forms two layers: a dorsal epiblast and a ventral hypoblast. The structure is like an Oreo cookie without the icing. Epiblast cells will form all of the embryonic tissues and cells. The hypoblast will be important for early signaling to establish the cranial-caudal axis but will eventually be displaced. 2. Two cavities are formed: the amnion and the yolk sac. Amnioblasts proliferate from the edges of the epiblast and secrete amniotic fluid. Yolk sac (endoderm) cells proliferate from the edges of the hypoblast to form the yolk sac. 3. Nobody knows whether or not the yolk sac is involved in embryonic nutrition, but later, it will provide the first blood cells and the germ cells (eggs and sperm) for the embryo. Slide 20: Illustration of sagittal section of the embryo and membranes that summarizes events of the second week Main points: 1. At the end of the second week, we are like a chick embryo with the embryonic disc (Oreo cookie) sitting on top of a yolk sac. 2. The second week can be called the "week of two’s." (See slide.) Also, there are three cavities formed: amniotic, yolk sac, and chorionic. Slide 21: Dorsal view of the embryonic disc (Oreo cookie) at the beginning of the third week Sadler, T.W.: Langman’s Medical Embryology, 11e © Lippincott Williams & Wilkins, 2010 Main points: 1. Two features appear in the epiblast: 1) the primitive streak, a shallow groove at the caudal end of the embryo; and 2) the oropharyngeal membrane, a disc-shaped region of tightly adhering epiblast and hypoblast cells. This is the primitive membrane between the oral cavity and the pharynx. It will eventually degenerate by programmed cell death to create an opening into the pharyngeal portion of the gut. 2. These two features demonstrate that the head (cranial) and tail (caudal) ends of the embryo have been established. Slide 22: Illustration showing a midsagittal section through the embryonic disc Main points: 1. Establishment of the cranial-caudal axis requires molecular signals from two regions. First, the anterior visceral endoderm (AVE), consisting of hypoblast cells at the cranial end of the embryonic disc, expresses head-forming genes. These signals are reinforced by those from a region (a shallow circular depression) at the cranial end of the primitive streak called the node. The main head-inducing gene from this region is goosecoid (a transcription factor). 2. Other signals from the node specify dorsal and ventral regions of the embryo by interacting with bone morphogenetic protein (BMP). This protein is secreted as a growth factor in all regions and cells at this stage of development. If this protein is not inhibited, then mesoderm becomes “ventralized” to form intermediate mesoderm (urogenital system) and lateral plate mesoderm (limbs and ventral body wall). If it is inhibited, then mesoderm becomes “dorsalized” and forms paraxial mesoderm (somites [vertebrae]) and notochord. Genes expressed in the node inhibit BMPs. Goosecoid upregulates chordin (a growth factor), while noggin, follistatin, and nodal (all growth factors) are secreted by the node, and all of these proteins inhibit BMPs. Slide 23: Example of conjoined twins Main points: 1. In frogs, overexpression of goosecoid causes double-headed tadpoles. Perhaps one way for this type of conjoined twins to form is by the same mechanism, whereby too much signaling from goosecoid induces additional head regions. Slide 24: Dorsal views of the embryonic disc at day 15 when laterality is established Main points: 1. Not only does the early embryo know its head from its tail, it also knows its left from its right. 2. First fibroblast growth factor (FGF) is secreted by cells in the node. This causes the growth factor nodal to be secreted by the node and then concentrated to the left side by the action of cilia on cells in the node. The ciliated cells establish a polarized beat to the left side by some unknown mechanism (maybe electrical). 3. Concentration of nodal on the left initiates a cascade of gene expression on that side, culminating in expression of the transcription factor PITX2; the master gene for establishing left-sidedness. Sadler, T.W.: Langman’s Medical Embryology, 11e © Lippincott Williams & Wilkins, 2010 4. Mechanisms to establish the right side are not clear but may involve expression of snail. Slide 25: Abnormalities resulting from problems establishing sidedness Main points: 1. Situs inversus is a complete reversal of the organs and sidedness, which is not usually a problem clinically. Individuals with situs inversus typically do not have other abnormalities. 2. 20% of people with situs inversus have Kartagener syndrome, which includes a problem with abnormal cilia function. Thus, their situs inversus probably relates to a cilia problem at the beginning of the third week when cilia in the node should have swept nodal to the left side. 3. As each organ is formed, it too expresses the cascade of genes that regulates sidedness, for example when the heart loops or the liver or spleen is formed. 4. People whose organs do not express this cascade properly have laterality sequences in which one or more organs are on the wrong side but not all of them. (They do not have complete situs inversus.) If the abnormality is primarily on the right, they have polysplenia (the spleen is a right-sided organ) or if the abnormality is primarily leftsided, they have asplenia. They also have a higher chance of having other congenital malformations (unlike people with complete situs inversus). Slide 26: Dorsal views of the embryonic disc showing initial stages of gastrulation Main points: 1. Gastrulation is the process of making the three germ layers from the epiblast by cell migration. It transforms the embryonic disc from a bilaminar structure (Oreo cookie without the icing) to a trilaminar structure (Oreo cookie with the icing). 2. Gastrulation begins when cells of the epiblast proliferate and migrate toward the primitive streak (arrows). Slide 27: Dorsal view of the embryonic disc and a cross section through the primitive streak showing the process of gastrulation Main points: 1. Cells of the epiblast move toward the streak, turn inward, detach from their epiblast neighbors, and migrate beneath the remaining epiblast cells to establish two new cell layers. 2. Some of the first cells to migrate into the streak displace the hypoblast cells, such that the hypoblast layer will be completely replaced with a new set of cells. Thus, the hypoblast does not contribute any cells to the embryo’s development; all of them arise from the epiblast. 3. Additional cells assume an intermediate position between the ventral cells, replacing the hypoblast and cells that remain in the epiblast. This middle (icing) layer makes the embryo trilaminar. Slide 28: Dorsal view of the embryonic disc showing direction of migrating cells and a sagittal section through the midline showing prenotochordal and notochordal cells Sadler, T.W.: Langman’s Medical Embryology, 11e © Lippincott Williams & Wilkins, 2010 Main points: 1. Cells move in through all regions of the primitive streak, including the node. As they move through the streak, their fates are specified. For example, cells moving through the most cranial aspect of the primitive node will form prechordal and notochordal cells; just lateral to this region, cells will form heart cell precursors and so on. 2. Some cells move through the cranial aspect of the node and migrate in the midline directly toward the oropharyngeal membrane. These cells will form prechordal and notochordal cells that will be critical for inducing the brain and establishing the midline. Slide 29: Sagittal (A) and cross sections (B and C) showing notochord development Main points: 1. Sagittal section showing midline location of the prechordal and notochordal cells and the cut lines for B and C. 2. As cells that will form the notochord move through the node, they first intercalate themselves into the hypoblast to form the notochordal plate (B). 3. As differentiation continues, these cells detach from the hypoblast and form a continuous line of cells called the notochord. This structure is critical for establishing the midline and the axis of the embryo. It eventually forms the nucleus pulposus of each intervertebral disc. Slide 30: Cross section through the trilaminar embryonic disc showing the 3 germ layers Main points: 1. The result of gastrulation is formation of a trilaminar (Oreo cookie complete with icing) embryo, and the three layers are called the germ layers because they will “germinate” all of the tissues and organs of the embryo. 2. The three layers include ectoderm, formed from cells that remain in the epiblast; mesoderm, formed from cells that migrate in through the primitive streak to form the middle germ layer, including the prechordal plate and notochord; and endoderm, formed by cells migrating through the streak and displacing the hypoblast cells. 3. Gastrulation progresses in a cranial to caudal direction. Thus, the head region becomes trilaminar first, then the neck, thorax, and so on down the body axis. The process starts at the beginning of the third week and continues until near the end of the fourth week. 4. Ectoderm basically represents tissues that come in contact with the outside world, such as the skin, brain and spinal cord, and eyes and ears. 5. Mesoderm forms the heart and urogenital system and the tissues that hold everything together (most bones and connective tissue). 6. Endoderm is related to the gut and its derivatives. Sadler, T.W.: Langman’s Medical Embryology, 11e © Lippincott Williams & Wilkins, 2010