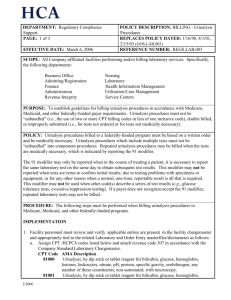
Billing: Urinalysis Procedures
advertisement

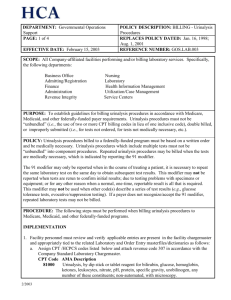
DEPARTMENT: Regulatory Compliance Support PAGE: 1 of 3 POLICY DESCRIPTION: BILLING - Urinalysis Procedures REPLACES POLICY DATED: 1/16/98, 8/1/01, 2/15/03 (GOS.LAB.003); 3/6/06; 5/1/08; 6/12/08 EFFECTIVE DATE: May 15, 2010 REFERENCE NUMBER: REGS.LAB.003 APPROVED BY: Ethics and Compliance Policy Committee SCOPE: All Company-affiliated facilities performing and/or billing laboratory services. Specifically, the following departments: Business Office Admitting/Registration Finance Administration Revenue Integrity Nursing Laboratory Health Information Management Case Management Shared Services Centers PURPOSE: To establish guidelines for billing outpatient urinalysis procedures in accordance with Medicare, Medicaid, and other federally-funded payer requirements. Urinalysis procedures must not be “unbundled” (i.e., the use of two or more CPT billing codes in lieu of one inclusive code), double billed, or improperly submitted (i.e., for tests not ordered or for tests not medically necessary). POLICY: Urinalysis procedures billed to a federally-funded program must be based on a written order and be medically necessary. Urinalysis procedures which include multiple tests must not be “unbundled” into component procedures. Repeated urinalysis procedures may be billed when the tests are medically necessary, which is indicated by reporting the modifier 91. Modifier 91 may only be reported when in the course of treating a patient, it is necessary to repeat the same laboratory test on the same day to obtain subsequent test results. This modifier may not be reported when tests are rerun to confirm initial results; due to testing problems with specimens or equipment; or for any other reason when a normal, one-time, reportable result is all that is required. This modifier may not be used when other code(s) describe a series of test results (e.g., glucose tolerance tests, evocative/suppression testing). If a payer does not recognize/accept modifier 91 and the payer has not provided you with their specific billing guidance for repeated laboratory tests, these tests may not be billed. CMS has established Medically Unlikely Edits (MUE) and National Correct Coding Initiative (NCCI) edits. MUEs may trigger when units of service on a given claim line item exceed the established limit for that HCPCS code. NCCI edits may trigger when there are restrictions on code combinations reported on a single date of service. MUEs and/or NCCI edits may supersede information within this policy. PROCEDURE: The following steps must be performed when billing urinalysis procedures to Medicare, Medicaid, and other federally-funded programs. IMPLEMENTATION 1. Facility personnel must review and verify applicable entries are present in the facility chargemaster and appropriately tied to the related Laboratory and Order Entry masterfiles/dictionaries as follows: 4/2010 DEPARTMENT: Regulatory Compliance Support PAGE: 2 of 3 POLICY DESCRIPTION: BILLING - Urinalysis Procedures REPLACES POLICY DATED: 1/16/98, 8/1/01, 2/15/03 (GOS.LAB.003); 3/6/06; 5/1/08; 6/12/08 EFFECTIVE DATE: May 15, 2010 REFERENCE NUMBER: REGS.LAB.003 APPROVED BY: Ethics and Compliance Policy Committee Assign CPT /HCPCS codes listed below and attach revenue code 307 in accordance with the Company Standard Laboratory Chargemaster. CPT Code AMA Description 81000 Urinalysis, by dip stick or tablet reagent for bilirubin, glucose, hemoglobin, ketones, leukocytes, nitrate, pH, protein, specific gravity, urobilinogen, any number of these constituents; non-automated, with microscopy. 81001 Urinalysis, by dip stick or tablet reagent for bilirubin, glucose, hemoglobin, ketones, leukocytes, nitrate, pH, protein, specific gravity, urobilinogen, any number of these constituents; automated, with microscopy 81002 Urinalysis, by dip stick or tablet reagent for bilirubin, glucose, hemoglobin, ketones, leukocytes, nitrate, pH, protein, specific gravity, urobilinogen, any number of these constituents; non-automated, without microscopy 81003 Urinalysis, by dip stick or tablet reagent for bilirubin, glucose, hemoglobin, ketones, leukocytes, nitrate, pH, protein, specific gravity, urobilinogen, any number of these constituents; automated, without microscopy 81005 Urinalysis; qualitative or semiquantitative, except immunoassays 81007 Urinalysis; bacteriuria screen, except by culture or dipstick 81015 Urinalysis; microscopic only 81020 Urinalysis; two or three glass test 2. Business Office/Service Center personnel must verify that edits are present in the electronic billing system which identifies occurrences of more than one urinalysis procedure per outpatient per date of service for federally funded programs. 3. Laboratory and Business Office/Service Center personnel must educate all staff associates responsible for ordering, charging, or billing laboratory services on the contents of this policy. 4. Monitoring activities must be completed in accordance with the Billing – Monitoring Policy, REGS.GEN.001. DAILY 1. It is recommended but not required that laboratory personnel review daily charge reports (e.g., Ancillary Charge Report, NPR charge reports, etc.) to verify compliance with this policy as follows: a. Duplicate urinalysis procedures which are not medically necessary are not billed to federallyfunded programs for the same patient on the same date of service. If more than one urinalysis procedure has been charged, bill the most comprehensive procedure. (See example 1 below.) b. Repeated urinalysis procedures are billed to federally funded payers only when medically necessary. 2. Business Office personnel must review electronic billing edit / error reports daily and perform the 4/2010 DEPARTMENT: Regulatory Compliance Support PAGE: 3 of 3 POLICY DESCRIPTION: BILLING - Urinalysis Procedures REPLACES POLICY DATED: 1/16/98, 8/1/01, 2/15/03 (GOS.LAB.003); 3/6/06; 5/1/08; 6/12/08 EFFECTIVE DATE: May 15, 2010 REFERENCE NUMBER: REGS.LAB.003 APPROVED BY: Ethics and Compliance Policy Committee following: a. Bundle urinalysis components to the most comprehensive procedure code. b. Identify the presence of more than one urinalysis procedure per patient on the same date of service and determine if documentation is present to support medical necessity. i. Append modifier 91 to repeated urinalysis procedures which are medically necessary. ii. Eliminate repeated tests/panels which are not medically necessary. Modify number of units and related charges in the electronic billing vendor system to reflect the appropriate charge for the procedure being billed. The Facility Ethics and Compliance Committee is responsible for implementation of this policy within the facility. EXAMPLES: 1. A. Perform and report automated UA no micro. B. Dr. adds a microscopic order later in the day. BILL: CPT code 81001 - Automated UA, with microscopic 2. A. Perform a manual UA with microscopic, with abnormal bilirubin results. B. Perform a bile confirmation test. BILL: CPT code 81000 only. 3. A. Perform and report automated UA with micro and pregnancy test. BILL: CPT code 81001 and 81025 Special Considerations: All confirmation testing is included in the urinalysis procedure and therefore are not billed separately. Refer to company policy Laboratory - Reflex Orders REGS.LAB.010 for guidelines related to reflex testing. REFERENCES: 1. American Medical Association, Urinalysis, CPT codes and nomenclature 2. Medicare Claims Processing Manual, Chapter 16, Section 90 3. Medicare Reimbursement Manual for Clinical Laboratory Issues; National Edition, 1997. Washington G-2 Reports, Washington D.C. Page 1.20 4. CMS website - National Correct Coding Initiative edits 4/2010