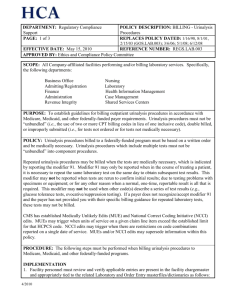
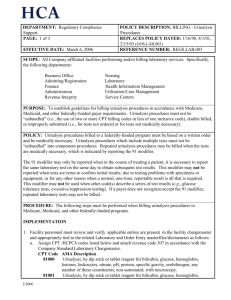
Billing: Urinalysis Procedures
advertisement

DEPARTMENT: Governmental Operations Support PAGE: 1 of 4 EFFECTIVE DATE: February 15, 2003 POLICY DESCRIPTION: BILLING - Urinalysis Procedures REPLACES POLICY DATED: Jan. 16, 1998; Aug. 1, 2001 REFERENCE NUMBER: GOS.LAB.003 SCOPE: All Company-affiliated facilities performing and/or billing laboratory services. Specifically, the following departments: Business Office Admitting/Registration Finance Administration Revenue Integrity Nursing Laboratory Health Information Management Utilization/Case Management Service Centers PURPOSE: To establish guidelines for billing urinalysis procedures in accordance with Medicare, Medicaid, and other federally-funded payer requirements. Urinalysis procedures must not be “unbundled” (i.e., the use of two or more CPT billing codes in lieu of one inclusive code), double billed, or improperly submitted (i.e., for tests not ordered, for tests not medically necessary, etc.). POLICY: Urinalysis procedures billed to a federally-funded program must be based on a written order and be medically necessary. Urinalysis procedures which include multiple tests must not be “unbundled” into component procedures. Repeated urinalysis procedures may be billed when the tests are medically necessary, which is indicated by reporting the 91 modifier. The 91 modifier may only be reported when in the course of treating a patient, it is necessary to repeat the same laboratory test on the same day to obtain subsequent test results. This modifier may not be reported when tests are rerun to confirm initial results; due to testing problems with specimens or equipment; or for any other reason when a normal, one-time, reportable result is all that is required. This modifier may not be used when other code(s) describe a series of test results (e.g., glucose tolerance tests, evocative/suppression testing). If a payer does not recognize/accept the 91 modifier, repeated laboratory tests may not be billed. PROCEDURE: The following steps must be performed when billing urinalysis procedures to Medicare, Medicaid, and other federally-funded programs. IMPLEMENTATION 1. Facility personnel must review and verify applicable entries are present in the facility chargemaster and appropriately tied to the related Laboratory and Order Entry masterfiles/dictionaries as follows: a. Assign CPT /HCPCS codes listed below and attach revenue code 307 in accordance with the Company Standard Laboratory Chargemaster. CPT Code AMA Description 81000 Urinalysis, by dip stick or tablet reagent for bilirubin, glucose, hemoglobin, ketones, leukocytes, nitrate, pH, protein, specific gravity, urobilinogen, any number of these constituents; non-automated, with microscopy. 2/2003 DEPARTMENT: Governmental Operations Support PAGE: 2 of 4 EFFECTIVE DATE: February 15, 2003 POLICY DESCRIPTION: BILLING - Urinalysis Procedures REPLACES POLICY DATED: Jan. 16, 1998; Aug. 1, 2001 REFERENCE NUMBER: GOS.LAB.003 81001 b. Urinalysis, by dip stick or tablet reagent for bilirubin, glucose, hemoglobin, ketones, leukocytes, nitrate, pH, protein, specific gravity, urobilinogen, any number of these constituents; automated, with microscopy 81002 Urinalysis, by dip stick or tablet reagent for bilirubin, glucose, hemoglobin, ketones, leukocytes, nitrate, pH, protein, specific gravity, urobilinogen, any number of these constituents; non-automated, without microscopy 81003 Urinalysis, by dip stick or tablet reagent for bilirubin, glucose, hemoglobin, ketones, leukocytes, nitrate, pH, protein, specific gravity, urobilinogen, any number of these constituents; automated, without microscopy 81005 Urinalysis; qualitative or semiquantitative, except immunoassays 81007 Urinalysis; bacteriuria screen, except by culture or dipstick 81015 Urinalysis; microscopic only 81020 Urinalysis; two or three glass test Remove charge explosions from urinalysis procedures. 2. Business Office personnel must verify that edits are present in the electronic billing system which identify occurrences of more than one urinalysis procedure per outpatient per date of service for federally funded programs. 3. Laboratory and Business Office personnel must educate all staff associates responsible for ordering, charging, or billing laboratory services on the contents of this policy. 4. Monitoring activities must be completed in accordance with the Billing – Monitoring Policy, GOS.GEN.001. 5. Business Office personnel must identify intermediary interpretations which vary from the interpretations in this policy. Specific documentation from the intermediary related to the variance(s) must be obtained and provided to the Billing Help Line at 1-888-735-3669. DAILY 1. It is recommended but not required that laboratory personnel review daily charge reports (e.g., Ancillary Charge Report, NPR charge reports, etc.) to verify compliance with this policy as follows: a. Duplicate urinalysis procedures which are not medically necessary are not billed to federallyfunded programs for the same patient on the same date of service. If more than one urinalysis procedure has been charged, bill the most comprehensive procedure. (See example 1 below.) b. Repeated urinalysis procedures are billed to federally funded payers only when medically necessary. c. Any exceptions noted on the daily charge reports should be corrected on the individual patient accounts. This will ensure that your accounts receivable system remains updated with actual billing data. 2/2003 DEPARTMENT: Governmental Operations Support PAGE: 3 of 4 EFFECTIVE DATE: February 15, 2003 POLICY DESCRIPTION: BILLING - Urinalysis Procedures REPLACES POLICY DATED: Jan. 16, 1998; Aug. 1, 2001 REFERENCE NUMBER: GOS.LAB.003 2. Business Office personnel must review electronic billing edit / error reports daily and perform the following: a. Bundle urinalysis components to the most comprehensive procedure code. b. Identify the presence of more than one urinalysis procedure per patient on the same date of service and determine if documentation is present to support medical necessity. i. Append the 91 modifier to repeated urinalysis procedures which are medically necessary. ii. Eliminate repeated tests/panels which are not medically necessary. Modify number of units and related charges in the electronic billing vendor system to reflect the appropriate charge for the procedure being billed. c. It is recommended but not required to modify number of units and related charges in the Accounts Receivable system to match the corrected claim in electronic billing system. (Note: Utilize ancillary charge codes rather than correcting claims with adjustment codes. Corrections made subsequent to final bill should be processed through your patient accounting system late charge cycles.) This will ensure that your accounts receivable system remains updated with actual billing data. The Facility Ethics and Compliance Committee is responsible for implementation of this policy within the facility. EXAMPLES: 1. A. Perform and report automated UA no micro. B. Dr. adds a microscopic order later in the day. BILL: CPT code 81001 - Automated UA, with microscopic 2. A. Perform a manual UA with microscopic, with abnormal bilirubin results. B. Perform a bile confirmation test. BILL: CPT code 81000 only. 3. A. Perform and report automated UA with micro and pregnancy test. BILL: CPT code 81001 and 81025 Special Considerations: All confirmation tests are included in the urinalysis procedure and therefore are not billed separately. REFERENCES: CMS (formerly known as HCFA) Publ. 14-3, Trans. No 1554, (Nov. 01, 1996) 2/2003 DEPARTMENT: Governmental Operations Support PAGE: 4 of 4 EFFECTIVE DATE: February 15, 2003 POLICY DESCRIPTION: BILLING - Urinalysis Procedures REPLACES POLICY DATED: Jan. 16, 1998; Aug. 1, 2001 REFERENCE NUMBER: GOS.LAB.003 Medicare Intermediary Man., Section 3628, as revised by Trans. No 1686, Sept. 1996 American Medical Association, 1996. Urinalysis, CPT codes and nomenclature Hospital Insurance Manual Section 437. Billing For Clinical Diagnostic Laboratory Services Other Than to Inpatients Medicare Reimbursement Manual for Clinical Laboratory Issues; National Edition, 1997. Washington G-2 Reports, Washington D.C. Page 1.20 2/2003