skin - Gmu
advertisement

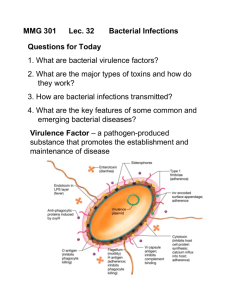
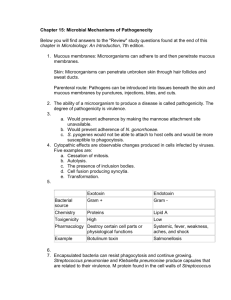
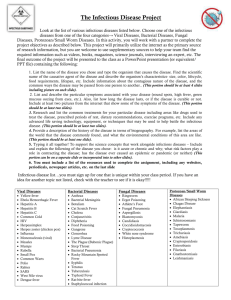
MECHANISMS of PATHOGENESIS Part I Host-Microbe Relationships and Disease Processes Chapter 14 Definitions NORMAL FLORA or MICROBIOTA • HOST – any organism that harbors another organism • NORMAL FLORA - permanent and usually not pathogenic microorganisms – RESIDENT FLORA – always present on or in the human body – TRANSIENT FLORA - come & go – For a few hours to a few months • In utero - germ-free • Birth - microorganisms being to establish themselves – Lactobacilli from mother’s vagina – Feeding and breathing - colonization of URT and GIT NORMAL FLORA • HOST & NORMAL FLORA exist together – The normal flora live in SYMBIOSIS with the human body • SYMBIOSIS – association between two or more species • COMMENSALISM = one organism benefits - the other is not affected – EX: Staphylococcus epidermidis - on our skin – The normal flora usually benefits the host by prevents pathogens from overgrowing NORMAL FLORA - HOST INTERACTIONS • MUTUALISM = both organisms benefit – EX: E. coli in intestines produce vitamin K & some B vitamins • ANTAGONISM = competition between the microorganisms – Active competition ie between normal flora & pathogen – BACTERIOCINS = proteins secreted by E. coli in the large intestine to inhibit other bacteria • PARASITISM = one organism (microorganism) benefits - the other is harmed – EX: Any successful pathogenic microorganism NORMAL FLORA INTERACTIONS • SYNERGISM = the effect of 2 organisms acting together is greater than the effect of either one acting alone – EX: Mycoplasma fermentans & HIV - if 1 cell is infected by both the cell will die much faster than when infected by either one alone OPPORTUNISTS • • OPPORTUNISTIC ORGANISMS = do not usually cause a disease but can become pathogenic under certain circumstances OPPORTUNITY KNOCKS: – – – – – Normal flora disrupted /destroyed Host defense mechanisms compromised Normal protective barriers of host are disupted EX: S. aureus - causes toxic shock syndrome (TSS) EX: Pneumocystis carinii - causes pneumonia in AIDS patients Evidence of Disease • Symptoms: changes in body functions such as pain and malaise .Signs: changes that can be seen by an observer such as rash, fever, swelling .Syndrome: specific symptoms and signs associated with a disease TYPES of DISEASES • INFECTIOUS – Caused by bacteria, viruses, fungi, protozoa and helminths • COMMUNICABLE INFECTIOUS DISEASES – Contagious – can be spread from one host to another • NON-COMMUNICABLE INFECTIOUS DISEASES – Caused by: individual’s normal flora; ingestion of pre-formed toxins; organisms found in the environment – Not “caught” from another person • NON-INFECTIOUS – Caused by any other factor than infectious organisms Occurrence of Diseases • Sporadic: occurs occasionally in a population • Endemic: a disease that is always found in the region • Epidemic: a disease that many people acquire in a very short period of time • Pandemic: is an epidemic that occurs worldwide CLASSIFYING INFECTIOUS DISEASES: DURATION • ACUTE DISEASES = short duration (flu, cold) • CHRONIC DISEASES = longer duration (AIDS, leprosy) • SUBACUTE DISEASES = intermediate duration • LATENT DISEASES = causative agent becomes latent – Characterized by a period of time of no symptoms – VZV - chicken pox then shingles SPREAD of INFECTION • THE INFECTIOUS AGENT: – WHERE DOES IT COME FROM? – HOW DOES IT GET INTO THE BODY? – HOW DOES IT GET OUT OF THE BODY? • HOW IS IT TRANSMITTED? • WHERE IS IT BETWEEN & DURING DISEASE? • Many pathogens can not survive outside the host long enough to serve as a source of infection – There must be sites where the pathogen can persist and maintain infectivity • RESERVOIR = a continual source of the disease causing organisms, it can be living or inanimate objects LIVING RESERVOIRS of INFECTION • HUMAN RESERVOIRS: – May transmit M/O directly or indirectly – Carriers (asymptomatic people) • AIDS, diptheria, typhoid fever, hepatitis, gonorrhea – Convalescing patients • ANIMAL RESERVOIRS: – Wild and/or domestic – ZOONOSES = a disease that occurs PRIMARILY in animals but that CAN BE TRANSMITTED to HUMANS – ~150 are known: anthrax, bubonic plaque, Lyme disease – Transmitted: bites, contaminated hides/feathers, food, insect vectors NONLIVING RESERVOIRS of INFECTION • SOIL – Many fungal diseases – Clostridium tetani, Bacillus anthracis • WATER – HAV, pathogenic E. coli, polio and various gastrointestinal diseases, typhoid fever MODES of DISEASE TRANSMISSION • New cases of infectious diseases – • Pathogen must leave reservoir or portal of exit portal of entry in the new host Three categories: – – – Contact transmission Vehicle transmission Vector transmission CONTACT TRANSMISSION • DIRECT: person-to-person – HORIZONTAL transmission = from one person to another OR from one part of the host to another part of the host • Kissing, sexual contact, touching sores, shaking hands; direct fecaloral transmission – VERTICAL transmission = from parent to offspring • In egg or sperm; placenta; breast milk; birth canal • INDIRECT TRANSMISSION: – FOMITES ie nonliving object • Syringe, drinking glass, contaminated linens, toys • DROPLET TRANSMISSION: – Coughing, sneezing, talking VEHICLE TRANSMISSION • Is transmission through a medium A non-living carrier of an infectious agent from its reservoir to a susceptible host WATER – Often due to fecal contamination • Ex: Cholera, shigellosis, leptospirosis FOOD – Often due to incompletely cooked food or improperly refrigerated foods food poisoning • Ex: Botulism, typhoid fever AIR – Mucus droplets – can travel a long distance • Ex: Histoplasmosis, the flu, measles, tuberculosis BODY FLUIDS – • • • • VECTOR TRANSMISSION • Usually an arthropod (insect) • Transfer of M/O from feet or other body parts of insects to food or skin of person – Or person can be bitten by insects that are harboring these M/O and thus introduce them to the body • BIOLOGICAL transmission – M/O replicates in vector (or at least part of the M/Os replicative cycle occurs in the vector) • Ex: Lyme disease, malaria • MECHANICAL transmission – Passive – no replication of M/O within vector – Ex: shigellosis, typhoid fever Emerging Infectious Diseases • Diseases that are either new or changing • Many different factors – – – – – – – A new strain of pathogen that is more virulent Overuse of antibiotics promotes resistant strains Global warming increases survival of reservoirs and vectors Modern transportation Natural disasters Animal control measures increase # of animals that carry microbes Failure to comply with public health measures AGE OF ANTIBIOTICS = NO DISEASE? • EMERGING INFECTIOUS DISEASES • New or changing diseases – – – – – E. coli O157:H7 HIV Ebola virus Hepatitis C Virus Drug resistant T.B. • http://www.cdc.gov/ncidod/eid/eid.htm NOSOCOMIAL INFECTIONS • Hospital or other medical facility acquired – 5-15% of patients affected • ~2 million (10%) in American Hospitals • 20,000 or more patients die/year • THREE FACTORS: – M/O in hospital – Patient’s general health – Chain of transmission NOSOCOMIAL MICROORGANISMS • Often the most pathogenic will be in the hospital – – – – S. aureus - urinary & respiratory infections Pseudomonas aeruginosa - burns & surgical wounds E. coli - urinary tract, neonatal meningitis Enterococcus - urinary tract & wound • Many M/O contain R plasmids = antibiotic resistance • Endogenous infections – Caused by opportunistic M/O among patient’s own normal flora • Exogenous infections – Caused by M/O that enter the patient through the environment HOSPITAL PATIENTS • Host is usually immunocompromised • Resistance to infection is reduced – Broken skin or mucous membranes – Surgery, burns, catheters • Suppressed immune system – Drugs, diabetes, stress, HIV etc CHAIN of TRANSMISSION • • • • • Hospital staff ---> patient Patient ---> patient Fomites ---> patient Ventilation system ---> patient CONTROL: – Educate personnel – Practice good techniques – Monitor for drug resistance HOW VIRUSES CAUSE DISEASE • Evade host immune system – Sometimes can destroy cells of the immune system (cytocidal) • CPE: Cytopathic Effects – Abnormalities in the host cell induced by virus • Inhibition of DNA, RNA and protein synthesis – Inclusion bodies • Small granules containing viral nucleic acids & proteins; found in nucleus and cytoplasm – Syncytia formation (giant cells) • Cause several host cells to fuse together EXTENT of HOST INVOLVEMENT • SEPTICEMIA – “blood poisoning” – Pathogens are present and multiplying in the blood • BACTEREMIA - presence of bacteria in the blood – Bacteria are being transported but are NOT multiplying in the blood • VIREMIA - presence of viruses in the blood – Viruses are being transported but are NOT multiplying in the blood • TOXEMIA - presence of toxins in the blood causing symptoms Definitions • PATHOGENICITY: Is the ability of an organism to cause disease • VIRULENCE: Is the degree of pathogenicity PORTALS of ENTRY • • • • Organisms need to ENTER to establish disease – – These portals of entry differ for different M/O Some M/O have only 1 portal and some have several portals – Respiratory, GI, & genitourinary tracts, conjunctiva (eyes) – Largest organ & outermost protective layer – Deposition directly under the skin into the tissues beneath skin or mucous membranes • Bites, burns, injections etc. MUCOUS MEMBRANES SKIN PARENTERAL ROUTE ENTRY of M/O into HOST • PREFERRED PORTALS of ENTRY – Route of entry that is required for establishment of disesase • NUMBERS of INVADING M/O – Number required for disease may vary from person to person • ADHERENCE – To tissue surfaces to establish infection – ADHESINS = surface molecules on the pathogen that bind to RECEPTORS on the surface of the host cell/tissues – Can be found on capsules, fimbriae, capsid, or envelope of a virus PORTALS of EXIT • Usually pathogens leave host with body fluids or feces • Gastrointestinal tract – Diarrhea, vomitting • Urogenital tract – Sexual contact, urine • Blood – Insects, needles – Wounds • Respiratory tract – Coughing, sneezing, speaking ESTABLISHMENT of DISEASE • • • • • To cause an infection or disease, microorganisms need to: ENTER the organism (Portal of Entry – Chpt 15) ADHERE to tissues PENETRATE the tissues DAMAGE CELLS to establish disease HOW BACTERIA CAUSE DISEASE • VIRULENCE FACTORS – characteristics that help M/O cause infection and disease – Structural: pili for adhesion – Physiological: enzymes help to evade host defenses; toxins • DIRECT ACTIONS by BACTERIA – Adhesins – proteins/glycoproteins allow M/O to adhere to host cells – Colonization – growth of M/O on epithelial cell surfaces (skin, mucous membranes) – Invasiveness – degree to which a M/O can invade and grow in host tissues – related to virulence factors – Toxins – any substance poisonous to other organisms HOW BACTERIA CAUSE DISEASE • VIRULENCE FACTORS – characteristics that help M/O cause infection and disease – Structural: pili for adhesion – Physiological: enzymes help to evade host defenses; toxins • DIRECT ACTIONS by BACTERIA – Adhesins – proteins/glycoproteins allow M/O to adhere to host cells – Colonization – growth of M/O on epithelial cell surfaces (skin, mucous membranes) – Invasiveness – degree to which a M/O can invade and grow in host tissues – related to virulence factors – Toxins – any substance poisonous to other organisms BACTERIAL VIRULENCE FACTORS • CAPSULES – resist host defenses – Phagocytosis and complement • CELL WALL COMPONENTS – some may help – Streptococcus pyogenes - protein M – Mycobacteria – waxes (mycolic acid) • ENZYMES – extracellular enzymes – Help to breakdown and dissolve material found between/around cells • Hyaluronidase – “spreading factor” – Streptococci produce - digests hyaluronic acid • Coagulase – increases clotting (coagulation) – Staphylococcus aureus produces – keeps organism from spreading BUT also walls off M/O from immune system BACTERIAL VIRULENCE FACTORS cont’d • Streptokinase – dissolves clots (digests fibrin) Streptococcus pyogenes- pathogens trapped in clots free themselves to spread to other tissues • Collagenases – breaks down collagen – Produced by some Clostridia • Hemolysins – hemolyze RBCs – Alpha – partially digests hemoglobin greenish color – Beta – completely digests hemoglobin clear area – Staphylococci, Streptococci, Clostridium perfringes • Streptolysin O (SLO) is sensitive to oxygen • Streptolysin S (SLS) is not sensitive to oxygen • Leukocidins – destroys neutrophils – A type of WBC important for phagocytosis – – Produced by Staphylococci and Streptococci BACTERIAL TOXINS • TOXINS: poisonous substances produced by some M/O – Some produce fever, cardiovascular disturbances; neurological disturbances; diarrhea, shock • INTOXICATION – Diseases due to ingestion of the toxin (vs the M/O) • EXOTOXINS – Produced by bacterial and released into the surrounding medium • ENDOTOXIN – Lipid A portion of LPS released from cell wall of Gram –ve bacteria BACTERIAL ENDOTOXIN • • • • ENDOTOXIN – Causes chills, fever, weakness, aches & sometimes shock and death Two outcomes possible: Fever or pyrogenic response Septic shock ENDOTOXIN & the PYROGENIC RESPONSE • • • • Pyrogenic or Fever Response Macrophage phagocytosis Gram -ve cell Cell degraded releasing endotoxin Endotoxin stimulates macrophage to secrete IL-1 – IL-1 = INTERLEUKIN 1 (Endogenous pyrogen) • IL-1 causes the hypothalamus of brain to produce prostaglandins • PGs causes the body temperature to rise ENDOTOXIC (SEPTIC) SHOCK #1 • Reaction is due to a cascade of events • Fairly high fatality rate – 100,000 die / year (USA) – 13th leading cause of death in the USA • Macrophage may also secrete tumor necrosis factor (TNF) or cachetin in response to endotoxin • TNF + IL-1 activate other cells in the immune system which release MEDIATORS – Constriction of small blood vessels & increased permeability of capillaries – Rapid decrease in blood pressure (HYPOTENSION) – Impaired blood flow to the kidneys ENDOTOXIC (SEPTIC) SHOCK #2 • RESULTS: Chills, fever, vomitting, diarrhea, rapid decrease in b.p., convulsions, shock death • NORMAL? - a low level response allows for cells of the immune system to leave the blood and enter the site of infection • MAJOR PRODUCERS – – – – – – P. aeruginosa E. coli Klebsiella Proteus Enterobacter Salmonella typhi BACTERIAL EXOTOXINS #1 • EXOTOXINS – – – – – • • • • Usually proteins and enzymes, mainly produced by Gram +ve bacteria Genes often carried on plasmids or bacteriophages Easily diffuse to blood & lymph Exotoxins can be destroyed by heat or chemicals to become TOXOIDS.used as vaccines Three categories of exotoxins based on effect: CYTOTOXINS - Kill cells & affect their function NEUROTOXINS - Interfere with normal nerve impulses ENTEROTOXINS - Affect the GI tract BACTERIAL EXOTOXINS #2 • DIPTHERIA Toxin - Corynebacterium diptheria – Infected with a lysogenic phage – Cytotoxin that inhibits protein synthesis, AB toxin • Polypeptide B binds to cells; Polypeptide A inhibits protein synthesis • ERYTHROGENIC Toxin – Streptococcus pyogenes – 3 types: A, B and C – Damages blood capillaries under the skin rash of Scarlet Fever • BOTULINUM Toxin – Clostridium botulinum – Neurotoxin acts at neuromuscular junction • Prevents impulses from nerve muscle and inhibits release of acetylcholine flaccid paralysis BACTERIAL EXOTOXINS #3 • TETANUS Toxin – Clostridium tetani – Neurotoxin (tetanospasmin) – inhibits nerve cell impulses for muscle relaxtion uncontrollable muscle contractions • VIBRIO Enterotoxin (Cholera Toxin) – Vibrio cholerae – AB toxin • Polypeptide B binds to cells; Polypeptide A induces formation of cAMP release of large amounts of fluid & electrolytes “rice water stools” • STAPHYLOCOCCAL Enterotoxin – Affects intestinal tract similar manner to cholera toxin • STAPHYLOCOCCAL TSS Toxin – Toxic Shock Syndrome Toxin EXOTOXINS vs. ENDOTOXINS • • • • • Gram positive and gram negative bacteria Protein Neurotoxin, cytotoxin, enterotoxin Destroyed by heat Can be made into TOXOID, neutralized by antitoxin • • • • • • Only gram negative bacteria Lipid Found in LPS of gram negative cells, LIPID A Fever, toxic shock Cannot be destroyed by heat Cannot be made into toxoid, no neutralizing Ab. PLASMIDS, LYSOGENY & PATHOGENICITY • R factors - antibiotic resistance increases pathogenicity • Plasmids that code for virulence factors – Staph enterotoxin – Certain fimbriae of E. coli – Tetanus toxin • LYSOGENY = incorporation of a phage into a bacterial chromosome often containing gene for toxins – C. diptheriae - prophage beta codes for diptheria toxin – Streptococcus pneumoniae - phage codes for capsule