Macroeconomics and Health Nepal
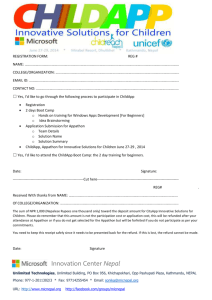
advertisement

WHO/SDE/CMH/04.10 Macroeconomics and Health Nepal Situational analysis Maria Paalman1 April 2004 World Health Organization 1 Senior Health Advisor, Royal Tropical Institute (KIT), Netherlands; Consultant, WHO Geneva Table of contents Acronyms .............................................................................................................. 5 Executive summary .............................................................................................. 7 Introduction ............................................................................................................................................... 7 Nepal Context ........................................................................................................................................... 7 The Health Sector ..................................................................................................................................... 8 Poverty and Health .................................................................................................................................... 9 External Development Partners .............................................................................................................. 10 Macroeconomics and Health ................................................................................................................... 10 Conclusion and recommendations .......................................................................................................... 11 Macroeconomics and Health ..................................................................................................... 12 Assignment ................................................................................................................................. 12 Nepal Context ...................................................................................................... 13 Physical ................................................................................................................................................... 13 Demographic ........................................................................................................................................... 13 Administrative .......................................................................................................................................... 13 Political .................................................................................................................................................... 13 Economical.............................................................................................................................................. 14 Social ...................................................................................................................................................... 14 Religion ................................................................................................................................................... 15 Ethnic ...................................................................................................................................................... 15 Education ................................................................................................................................................ 15 Poverty .................................................................................................................................................... 15 Security .................................................................................................................................................. 16 Government finance ................................................................................................................................ 16 The Health Sector ............................................................................................... 18 Ministry of Health ........................................................................................................................ 18 Policies, strategies and plans ................................................................................................... 18 National Health Policy 1991 .................................................................................................................... 19 Second Long Term Health Plan 1997-2017 ............................................................................................ 19 Strategic Analysis to operationalise the SLTHP ...................................................................................... 20 WB study - Nepal: operational issues and prioritization of resources in the health sector....................... 21 Medium Term Strategic Plan (MTSP) ...................................................................................................... 22 Medium Term Expenditure Programme (MTEP) ..................................................................................... 22 Medium Term Expenditure Framework for Health (MTEF-H) .................................................................. 23 Objectives ............................................................................................................................................... 24 Health Sector Strategy (HSS) ................................................................................................................. 24 Tenth 5-year Development Plan .............................................................................................................. 24 Nepal Health Sector Programme – Implementation Plan 2003-2007 (NHSP-IP) .................................... 26 PRSP and JSA ........................................................................................................................................ 27 Conclusion on policies, strategies and plans ........................................................................................... 28 Provision of health services ...................................................................................................... 28 Public health facilities .............................................................................................................................. 28 Utilisation................................................................................................................................................. 29 Human Resources................................................................................................................................... 29 Devolution of health services .................................................................................................................. 30 Private sector and NGOs ........................................................................................................................ 31 Implications of Maoist insurgency ........................................................................................................... 31 MEH/Nepal/Situational Analysis, April 2004 2 Health financing .......................................................................................................................... 31 Public Expenditure Review...................................................................................................................... 31 Budget for 2003/2004 .............................................................................................................................. 33 National Health Accounts ........................................................................................................................ 33 Taxes ...................................................................................................................................................... 33 User fees ................................................................................................................................................. 34 Insurance ................................................................................................................................................ 34 Health Management Information System ................................................................................. 35 Health indicators and targets .................................................................................................... 35 MDGs (HSS June 2002).......................................................................................................................... 36 Tenth Plan ............................................................................................................................................... 36 MDG Progress Report ............................................................................................................................. 36 Health Sector Strategy ............................................................................................................................ 36 Essential health interventions ................................................................................................... 36 Conclusion .............................................................................................................................................. 38 Research ...................................................................................................................................... 38 Capacity ....................................................................................................................................... 38 Relationship poverty – ill health ........................................................................ 40 External Development Partners ......................................................................... 42 Multilateral and bi-lateral donors .............................................................................................. 42 International NGOs ..................................................................................................................... 42 National NGOs............................................................................................................................. 42 Macroeconomics and Health ............................................................................. 45 Commitment ................................................................................................................................ 45 Commitment to poverty reduction............................................................................................................ 45 Commitment to Macroeconomics and Health .......................................................................................... 45 Commitment of external development partners ....................................................................................... 46 Institutional arrangements ......................................................................................................... 46 CMH calculations for Nepal ....................................................................................................... 47 Opportunities for scaling up/reaching the poor ...................................................................... 48 Non-financial constraints to scaling up/reaching the poor .................................................... 48 Financial constraints to scaling up/reaching the poor ........................................................... 49 Sources ................................................................................................................................................... 49 Expenditures ........................................................................................................................................... 50 Recommendations and conclusions ................................................................. 51 Annexes ............................................................................................................... 53 MEH/Nepal/Situational Analysis, April 2004 3 Annex 1 Policies and Plans ................................................................................................. 54 Annex 2 Tenth Plan Chapter 24 – Health .......................................................................... 59 Annex 3 Nepal Health Sector Programme – Implementation Plan (2003 – 2007) .......... 60 Annex 4 Health and Financing paragraphs in the PRSP ................................................. 61 Annex 5 People met in Nepal during mission 16/12/03 – 06/01/04 .................................. 67 Annex 6 Bibliography MEH situational analysis Nepal .................................................... 68 MEH/Nepal/Situational Analysis, April 2004 4 Acronyms Aamaa AIDS ALOS ARI BNMT BoD CBR CDR CHI CMH CMR CPR CRS CTC DALY DD DDC DFID DHO DoHS DOTS EDP EHCS FP FPAN FR FY GDP GTZ HDI HEFU HIV HMG HMGN HMIS HP HR HSS IEC ILO IMCI IMF IMR INF INGO JICA KIT Aamaa Milan Kendra (Mother’s Club) Acquired Immune Deficiency Syndrome Average Length of Stay Acute Respiratory Infections Britain Nepal Medical Trust Burden of Disease Crude Birth Rate Crude Death Rate Community Health Insurance Commission on Macroeconomics and Health Child Mortality Rate Contraceptive Prevalence Rate Nepal Contraceptive Retail Sales Company Close-to-Client Disability Adjusted Life Year Diarrhoeal Disease District Development Committee Department of International Development (British Govt) District Health Office Department of Health Services Directly Observed Treatment, Short-course External Development Partner Essential Health Care Services Family Planning Family Planning Association of Nepal Fertility Rate Fiscal Year Gross Domestic Product Gesellschaft für Technische Zusammenarbeit (German Development Organisation) Human Development Index Health Economics and Financing Unit MoH Human Immuno-deficiency Virus His Majesty’s Government His Majesty’s Government of Nepal Health Management Information System Health Post Human Resources Health Sector Strategy Information, Education and Communciation International Labour Organisation Integrated Management of Childhood Illness International Monetary Fund Infant Mortality Rate International Nepal Fellowship International Non-Governmental Organisation Japan International Cooperation Agency Royal Tropical Institute Amsterdam MEH/Nepal/Situational Analysis, April 2004 5 LE LIC MCHW MDGs MEH MMR MoF MoH MSI MTEF MTEF-H MTEP NGO NHA NHEICC NHRC NHSP-IP NLSS NPC NRCS OR P-1/2/3 PAF PER PHC PP&IC PPP PRSP RH SDC SHI SHP SLTHP STD SWAp TB TBA UMN UN UNDP USAID VAT VDC VHW WB WDR WHO Life Expectancy Low-income country Maternal and Child health Worker Millenium Development Goals Macroeconomics and Health Maternal Mortality Rate Ministry of Finance Ministry of Health Marie Stopes International Medium Term Expenditure Framework Medium Term Expenditure Framework – Health Medium Term Expenditure Programme/Plan Non Governmental Organisation National Health Accounts National Health Education, Information and Communication Centre National Health Research Council Nepal Health Sector Programme – Implementation Plan Nepal Living Standard Survey National Planning Commission Nepal Red Cross Society Occupancy Rate Priority 1/2/3 Poverty Alleviation Fund Public Expenditure Review Primary Health Care Policy, Planing and International Cooperation Purchasing Power Parity Poverty Reduction Strategy Paper Reproductive Health Swiss Agency for Development and Cooperation Social health Insurance Sub Health Post Second Long Term Health Plan 1997-2017 Sexually Transmitted Disease Sector-wide Approach Tuberculosis Traditional Birth Attendant United Mission Nepal (INGO) United Nations United Nations Development Programme United States Agency for International Development Value Added Tax Village Development Committee Village Health Worker World Bank World Development Report World Health Organization MEH/Nepal/Situational Analysis, April 2004 6 Executive summary Introduction The Government of Nepal requested WHO to provide technical assistance to take forward the Macroeconomics and Health (MEH) agenda. The Royal Tropical Institute in Amsterdam (KIT) was selected to provide this support during the preparatory phase (around 6 months). The support will consist of the production of a situational analysis, facilitation of establishing the institutional mechanisms for taking the work forward, support for the organisation of a national meeting and facilitation of a workshop to produce a proposal for the planning phase. The consultant visited Nepal from 16 December 2003 to 6 January 2004 to collect information, discuss options and further work as input for the situational analysis. This report is the situational analysis. Nepal Context Nepal is a relatively small (population 24 million) land-locked country, bordered by the two biggest countries in the world, India and China. Its renowned physical beauty makes it very fragmented and many parts are inaccessible by modern transport and lack of communication facilities. There are few cities and 86% of the population live in rural areas. The country is divided into 5 development regions, 14 zones and 75 districts and almost 4000 Village Development Committees and 58 municipalities. Nepal was never colonised, is a constitutional Hindu monarchy and has a multiparty bicameral parliamentary democracy. However, since October 2002 the King has taken over power. Since 1996 an ever increasingly violent Maoist insurgency has thrown the country into civil war. Road blocks, abductions, forced protection and fighting are increasingly making the country outside the capital Kathmandu an insecure place to live and travel. Underlying the insurgency is (among other things) a pervasive poverty. The country’s GDP per capita is only $250 and 38% of the population live below the poverty line. There are large inequalities. The poorest people live in the remote mountainous areas or belong to the lowest caste, the Dalits, in particular in the Western part of the country. This is also the part where the Maoists are strongest. While only 15% of households is connected to the electricity grid, 80% have access to safe water. Unemployment is a big problem, and many work abroad, bringing more money into the economy than toursim, foreign aid and export together. Illiteracy is very high, with around 40% of men and 75% of women not able to read or write. Nepal is still a very traditional country, hierarchical, linked to a caste system, strong religious and family traditions and a feudal structure. Favouritism is institutionalised, corruption rife. On the positive side civil society is well developed with numerous NGOs, including human right organisations, and a diverse and free press. Two braod ethnic groups can be subdivided into some 60 different groups, with their own culture and language, but there is only one official language: Nepali. Total government expenditure over FY 2002/2003 was $48 per capita, being 19% of GDP. Two-thirds of that is regular budget,one third development budget. 11% of government expenditure was used for debt repayment. The government budget for 2003/2004 is almost 20% higher. Around 60% of that comes from domestic revenues, 15% is expected to come in as foreign aid and 25% will be borrowed. The real percentage of foreign aid to Nepal is much higher, as a substantial percentage does not go through the MoF and is not accounted for in MEH/Nepal/Situational Analysis, April 2004 7 the so-called Red Book. In the health sector this percentage is even 90%. Maybe this is the reason why the expected government expenditure 2003/2004 for the health sector is so low, both compared to education (3x as much) and as compared to other countries: only 5.1% of total government budget, being $2,94 per capita and 1.18% of GDP is publicly spent on health. The Health Sector The central section of the MoH is responsible for policy making, and planning, financing, international cooperation, human resources, monitoring and evaluation, as well as for the central and zoanl hospitals. The Division for policy, planning and international cooperation is rather weak, but the health economcis and financing unit has become strong. The Department of Health Services is responsible for the provision of all health services at the district level and below and produces very informative annual reports. Regional Health Directors are responsible for technical backstopping as well as programme supervision. Their role seems to become less clear under the decentralisation process. At the district level and below, District and Village Development Committees are responsible for the delivery of health services. Over the years many policies and plans have been produced. It seems that more or less simultaneously two sets of documents were developed, one government driven and related to the 5-year development plan cycle, the other EDP driven. It seems that the detailed work done by the MoH jointly with the EDPs has to some extent informed the development of the documents for the Tenth 5-year Plan. The problem seems to be that the most current, prevailing documents have somewhat different objectives, strategies and activities. The main government document in force is the Tenth Plan, the health chapter and budget of which are organised by priority programme and/or organisational centre, probably following present budget lines. The NHSP-IP, more donor-driven, is organised by objectives, outputs and activities in a logical framework and does not have a budget yet. The PRSP, supposed to be a summary of the Tenth Plan, contains elements of both the Tenth Plan’s Health Chapter and the NHSP-IP, but also includes new activities. It is therefore not clear at this point which document the MoH is implementing and using to monitor its activities. Officially the MoH is bound by the Tenth Development Plan and its MTEF. It would be helpful, if a detailed comparison was made between the IP, the Tenth Plan and the PRSP, after which the MoH, NPC and MoF could sit together with the EDPs and decide which activities they will implement together. From all these plans however it is clear that Nepal is highly committed to poverty reduction and also sees health as a major driving force for economic growth. The MoH has identified essential health care services and the main objective of the health sector relates to scaling these up to reach more people. The EHCS package is very similar to the globally agreed priorities of maternal and child care, RH and infectious diseases, consistent with the MDGs and the package that the CMH advised. However, it is not clear which concrete activities are included. The NHSP-IP has outputs, broad actions, but no detailed activities for each output. The Tenth Plan includes prioritised programmes, but does not include the kind of detail, that sheds light on which parts of these programmes, or which activities, belong to the prioritisation. This obviously makes the costing very difficult. The MoH further has objectives to partner with the private and NGO sector, to decentralise resources and responsibility to village levels and to improve quality of services. Alternative sources of financing and exemption schemes for user fees will be developed. The health information system will be changed in such a way that the impact of the health strategy on the MEH/Nepal/Situational Analysis, April 2004 8 health status of the poor can be monitored. As in so many countries the implementation is the problem, utilisation of public health services is low, staff does not want to work in rural and remote areas, supplies and drugs are inadequate etc. The MoH website gives an astonishingly candid and comprehensive summary of the health status of the population and its determinants: “The Mortality and morbidity rates especially among women and children are alarmingly high. Acute preventable childhood diseases, complications of child birth, nutritional disorders and endemic diseases such as malaria, tuberculosis, leprosy, STDs, rabies, and vector borne diseases continue to prevail at a high rate. Determinants of such conditions are associated with pervasive poverty, low literacy rates, poor mass education, rough terrain and difficult communications, low levels of hygiene and sanitary facilities, and limited availability of safe drinking water. These problems are further exacerbated by under-utilization of resources; shortages of adequately trained personnel; underdeveloped infrastructure; poor public sector management; and weak intraand inter-sectoral co-ordination”. Another major problem is that money does not follow agreed policies. While the MTEF for the health sector, produced by the MoH in preparation for the Tenth Plan, set aside 57.6% of the budget for Priority-1 programmes and the Tenth Plan itself even 70%, the Public Expenditure Review of the health sector showed that actual funding going to Priority-1 programmes decreased from 58% to 50% over the last 3 years, while funding for priority-3 programmes increased. Also running counter to plans, is the fact that the share of the funding going to rural areas decreased, the expenditures for RH drastically decreased, and the share of health expenditures for children under 5 wasonly 4,7%, while they bear around 50% of the burden of disease. Provision of public sector health services is basically financed from taxes and user fees. Both are regressive, as the taxes are mainly indirect (VAT) and the user fees are a fixed amount, meaning that the poor pay relatively more than the rich, if and when they make use of public services at all. There are virtually no insurance schemes in place. People pay around $10 per capita out-of-pocket per annum. A pilot with community health insurance is planned for this year. Public services are mostly used by the middle income groups, while the rich go to the private sector and the poor don’t go at all. The ongoing Nepal Living Standard Survey will give more information on utilisation of health services in the rural areas. Poverty and Health Data from different sources have been analysed to get a grasp on the relationship between poverty and health and reveal great disparities in both health outcomes and intermediate indicators. Differences between the richest and poorest income quintiles in attended delivery, antenatal care, immunization coverage, malnutrition, total fertility rate and use of modern contraceptives are 2-10 fold. Infant and child mortality rates are much higher in rural areas and in particular in the mountains, coinciding with income differentials. A relation between the educational level of the mother (often in itself income related) and major health indicators has also been clearly established, as well as a relation between health care seeking behaviour and poverty. Geographical focus of reaching the poor should be on the Mid-and Far-West Regions, where 22% of the population live, who have the worst health indicators of the country and where hence great health gains can be made. As these are also the strongholds of the Maoist groups, this is far from simple. MEH/Nepal/Situational Analysis, April 2004 9 External Development Partners In Nepal 6% of external aid is spent on health. Donor expenditure in the health sector has more than tripled over the last 3 years and amount to about 40% of total public expenditures, translating in $2 per capita per annum. The biggest donors at the moment in the health sector are Japan and the UK, together good for half the external aid, with UNICEF, WHO, UNFPA, Germany, the US and Switzerland making up most of the remainder. The WB recently reduced its IDA grants to Nepal, but might be coming back soon. The financial inputs by indigenous and international NGOs are less well documented. The donors and the MoH have jointly developed the Health Sector Strategy and its Implementation Plan. Although this plan is a move towards a sector-wide approach, most donors are not in favour of fundpooling (yet), except DFID and the WB. At present all support is still organised in the form of projects or programmes and almost all funds go directly to the MoH or are self-executed by partners. The bulk of the donor funds go to essential health care or system development/strengthening. Macroeconomics and Health HMG of Nepal is very committed to poverty reduction, as is evident from all major policy and planing documents, but less so to health, as is evident from the low budget made available for the health sector (which might be related to the large direct flows of funding from the donors to the MoH). Within the health sector the MoH is on paper equally committed to reachng the poor with health services, but also hear money does not follow policy and the transfer of large amounts from Priority-3 to Priority-1 programmes must be considered unrealistic in such a short period. Nepal attended both global consultations on Macroeconomics and Health in Geneva and established a Sub-Commission on Macroeconomics and Health under the National Commission for Sustainable Development. The Sub-Commission met only once and appointed a working committee of 3 people, headed by the Chief of the Division for Policy, Planning and International Cooperation, Dr. B.b. Karki. This working committee made a Plan of Action for the preparatory phase of Macroeconomics and Health work, which was submitted to WHO. A revised version has been approved in March 2004. It remains to be seen whether the Sub-Commission will continue to be active, now that Dr. B.B. Karki has left Nepal for the USA. On the basis of the calculations by the CMH and the available information in Nepal the consultant estimated that total health expenditures in Nepal would have to double by 2007. HMG of Nepal would at least need to double its investment in health before 2007 and the donors would need to increase their share with $17 per capita, an eigth-fold increase from the present $2. Possibilities to channel the $10 that people now spend on health care out-ofpocket into pre-paid schemes need to be studied. Recently (during pre-consultative meetings of the Nepal Development Forum in April 2004) most donors have made restoration of democracy and conflict resolution conditionalities to future aid. Some donors advocated co-operating with the rebels in order for service delivery to continue. Therefore the present political situation could hamper scaling up efforts, in as far as both HMG of Nepal and donors do not seem willing and/or able to put more resources into health in the current situation. MEH/Nepal/Situational Analysis, April 2004 10 Conclusion and recommendations There are many achievements and developments in Nepal that forebode well on the possibility to scale up essential health interventions and specifically reach the poor. The opportunities have been summarised on page 47. However, there are also a considerable number of non-financial and financial constraints, which are summarised on pages 48/49. The main constraints are of a political nature and lie outside the health sector, namely the insecurity due to the conflict and the instable bureaucracy, resulting in lack of continuity in governance. Recommendations include: aligning the different operational plans, collecting (income poverty) disaggregated data for key indicators, adapting District Health Plans on the basis of detailed District Health and Poverty Profiles, focusing on interventions that address the burden of disease experienced by the poor and on actually reaching the poor with these interventions, studying options to contract out to NGOs and/or private sector, contract in or link up with existing services or schemes in other sectors ensuring that costing of the EHCS includes all system costs related to scaling up and is based on real local costs finding out how the P-1 programmes relate to the EHCS and how much of present expenditure is used to finance EHCS doubling HMG’s health budget increasing donor health budget using the full increase on scaling up EHCS for the poor including evaluation of community health insurance pilot in the proposal for the planing phase establishing research needs on the basis of the inventory made during the preparatory phase and the information gaps to be agreed during the national meeting and workshop in June 2004. Together with the working committee for Macroeconomics and Health and the WHO office the consultant adapted the Plan of Action and drafted ToR for a number of local consultants to carry out the desk review of local studies relevant to Macroeconomics and Health, to make district health and poverty profiles, and to organise a national advocacy meeting and workshop to draft a proposal for the planing phase. These activities are elaborated in the Plan of Action, last version dated 3 March 2004. MEH/Nepal/Situational Analysis, April 2004 11 Introduction Macroeconomics and Health The Commission for Macroeconomics and Health showed that investing substantially more in health will result in great economic returns. Disease creates poverty, but effective health care, especially targetted to the poor, will create economic growth. The health sector no longer only consumes resources, it can be a productive economic sector with very high returns on investment, if resources are used for prioritised interventions and targeted to those in greatest need. The Macroeconomics and Health agenda focuses on: 1. Achieving better health for the poor, thereby reducing poverty and stimulating economic growth 2. Eliminating financial constraints by increasing investments in health 3. Eliminating non-financial constraints to providing a package of essential interventions to the poor Assignment The Government of Nepal requested WHO to provide technical assistance to take forward the Macroeconomics and Health (MEH) agenda. The Royal Tropical Institute in Amsterdam (KIT) was selected by WHO Geneva, in consultation with the Regional Office, the WHO country office and the MoH Nepal, to provide this support during the preparatory phase (around 6 months). The support will consist of the production of a situational analysis, facilitation of establishing the institutional mechanisms for taking the work forward, support for the organisation of a national meeting and facilitation of a workshop to produce a proposal for the planning phase. This report is the situational analysis. The consultant visited Nepal from 16 December 2003 to 6 January 2004. Initial briefing took place by the WR, Dr. Klaus Wagner, and the WHO Health Planner, Dr. Lin Aung. The consultant was introduced to Dr. Benu Behadur Karki, Chief Policy, Planning and International Cooperation in the MoH. He was the driving force in Nepal to get the Macroeconomics and Health agenda implemented and was my main counterpart during the consultancy. A list of people met is provided as Annex 5 and a list of documents consulted in Annex 6. The consultant attended a meeting of the main donors in the health sector and gave a brief presentation on Macroeconomics and Health in general and the ToR for the consultancy in Nepal. A meeting was also organised by WHO and the MoH to meet with the core members of the National Commission for Macroeconomics and Health, with whom the first findings of the mission and the Plan of Action for the preparatory phase were discussed. At the end of the misson a debriefing took place at the MoH, where the consultant gave a power point presentation, which was provided to WHO in Geneva and Nepal for further dissemination. MEH/Nepal/Situational Analysis, April 2004 12 Nepal Context2 Physical Nepal is a landlocked country. The Himalaya mountain range in the north is bordering China (Tibet actually) and a flat jungle belt (terai) in the south is bordering India, with hills in the middle. The country is very fragmented by mountains and rivers. Due to its physical isolation, Nepal only opened to the outside world in 1951. Even today a large part of the country remains inaccessible by modern transport and communications. The environment is very fragile and an increasing population causes deforestation, erosion and pollution problems. Each year the summer rains cause landslides. Nepal is also earthquake prone. Demographic Nepal has 24.2 million inhabitants (estimate 2003) 1,5 million of which live in the Kathmandu valley (23x12 km) 1.8 million (7.4%) live in the mountains, which make up 35% of the land area 10.8 million (44.6%) live in the hills, which make up 42% of the land area 11.6 million (48%) live in the terai, which make up 23% of the land area 14 % of the population lives in urban and 86% in rural areas Population growth is presently 2.27% TFR is 4.1 (DoHS 2001) Administrative 5 development regions divided into 14 zones and 75 districts: Eastern Region has 16 districts and a population of 5.7 million (23.6%) Central Region has 19 districts and a population of 8.2 million (33.9%) Western Region has 16 districts and a population of 4.9 million (20.2%) Mid-Western Region has 15 districts and a population of 3.2 million (13.2%) Far Western Region has 9 districts and a population of 2.2 million (9.1%) Districts are divided into total of 205 electoral constituencies and 3,995 Village Development Committees (VDC) and 58 municipalities. Each VDC has 9 wards and each ward comprises 3-5 villages. District Development Committees (DDC) are responsible for the political and economic development of their respective districts. The Local Self Governance Act 1999, empowers the DDC to function as an integrated development institution in line with the national decentralization policy. Furthermore, this act delegates development authority to the respective municipalities and villages. Political Nepal was never colonised It is constitutional hindu monarchy Nepal has a multiparty bicameral parliamentary democracy since 1990: a Lower House with 205 members and an Upper House with 60 members. The country is very politically unstable. In October 2002 the King dismissed parliament and later government, and appointed a Prime Minister. At present 5 ministers run 20 ministries. 2 Nepal, Landenreeks. KIT Publishers 2002, Annual Report MoH 2001/2002, PER Health Sector MoH 2003 MEH/Nepal/Situational Analysis, April 2004 13 During the consultants’s stay in December 2003 fierce student protests broke out, supported by the 6-7 major political parties. They demanded the King’s decision be repealed, democracy be restored and dialogue with the Maoist groups, which were broken off in August 2003, be resumed. Because of the aphno manche system every change of government means replacement of a large number of government officials, not only at the central level, but also at lower levels, causing severe problems with administrative capacity and lack of continuity in policies and governance in general, resulting in inefficiency. The country also suffers from a high level of corruption. Payment of baksheesh is standard practice. An increasingly large percentage of civil servants and politicians are brahmins or chetris (98% of civil servants). In December 2003 a proposal was filed stipulating that at least 20% of seats in parliament should be reserved for women, 10% for dalits (the lowest caste) and 5% for ethnic groups. Economical One of the poorest countries in the world and the poorest on the Eurasian continent with GDP of around $250 p/c (2003) or PPP $1310 (2001) The currency is the Nepalese Rupee. In December 2003 US$1 buys around 73 Nepalese Rupees. Inflation has been 8-10% per year over recent years3. Almost entirely economically dependent on other countries, mainly India. 80% of population works in agriculture, being the largest economic sector, followed by small-scale industry. Unemployment causes many people to find work abroad, sending home 1 billion euro a year, more than tourism, foreign aid and export together bring into the economy. Large inequalities: 13% of the population earns 50% of the national income. Average income in Kathmandu is 4-5 times that in the rural areas. Only 15% of households is connected to the electricity grid. 80% of the population has access to safe water (UNDP 2001) Nepal has entered the World Trade Organisation in 2003. Social Human development index 2001: 0.499 Gender Development Index 2001: 0.479 Very patriarchal, hierarchical society, linked to the caste system, strong religious and family traditions and a feudal structure. The Nepalese caste system is made up of some 100 different castes. People from the same caste/family favour each other (aphno manche) and citizens often show their loyalty to influential persons by visiting them, in the hope to be rewarded at some point in the future (chakari). Women are supposed to be and often are subordinate to men, have to work longer hours, doing heavy physical labour. Abortion was illegal and punished with life-long imprisonment until abortion for medical reasons was legalised in 2002. Most marriages are still arranged. The modern world has definitely arrived in Kathmandu, but outside the capital many people still live without running water, electricity, telephone, radio and tv. The country has one official language: Nepali, the language of the brahmin and chetri castes, but Nepal harbours 20 languages and many more dialects. 3 Oral information MoF Shyam Nidhi Tiwari MEH/Nepal/Situational Analysis, April 2004 14 Civil society is well developed. There are many indigenous and international NGOs, a diverse and free press and human rights organisations, many of them also externally funded. Religion Hindu 60%, Buddhist 30% with animist, muslim and christian making up the remaining 10% So far little or no religious unrest. Ethnic Two main population groups can be distinguished: Mongol (35%) and Indo-Aryan (65%). The Mongols live mainly in the north, speak Tibeto-Birmese languages and are mainly buddhist The Indo-Aryan population live in the middle belt and the south, speak a Sanskrit language and are hindu. Both brahmins and chetris belong to the hindu Indo-Aryan population groups. These two broad ethnic groups can be subdivided into some 60 different ethnic and caste groups each with their own language, culture and religious rituals. Some population groups contain different castes and ethnicities. Education Adult illiteracy is very high, with almost 40% of men and 75% of women not able to read or write (UNDP 2003). Only 2/3 of children go to primary school, of the dalits only 1/3. In the budget speech for FY 2003/2004 the Minister of Finance announced that all the children from Dalit families admitted in primary schools will be provided with scholarships. An amount of Rs. 81.7 million has been earmarked for this purpose. Poverty Poverty is widespread. An estimated 38% of the population live below the poverty line ($1 a day), in rural areas 41.4%, in urban 23.9%, in the mountains 56%, among dalits 90% (partly UNDP 2001). This percentage has not changed much during the last 25 years, meaning that the absolute number of people living in poverty has increased. The target for the MDGs is 17%. Income poverty is more common in rural areas, where 90% of the poor live, in the mid-western and far western development regions, among mountain villagers, women, certain ethnic groups, called Janajati, and the lowest castes (Dalits). While the poverty rate for Kathmandu is 4%, it is as high as 72% in the remote areas of the Mid-Western and Far-Western hills and mountain regions. Poverty is most intense/severe among the mountain populations. Similar disparities exist for literacy rates, life expectancy, percentage op population having access to drinking water and the Human Development Index (HDI) in general. Breakdowns are generally given by ecological area, urban/rural, and development region. Whether they are also available by district, needs to be checked. Factors contributing to persistent poverty, mentioned in the PRSP, are limited resource endowment, ill health, rugged terrain, isolation, a high population growth rate of 2.2% per annum. Economic growth over the past decennium has largely bypassed the rural poor. MEH/Nepal/Situational Analysis, April 2004 15 Security The country is torn by a conflict between Maoist groups and the government security forces, which started in February 1996 and escalated in November 2001, after several months of peace talks broke down. The Maoist goal is to replace the present polity with a “people’s republic” and finds its justification in the deep poverty and social exclusion of large parts of the population, grievances about poor governance, corruption, lack of land reform, caste discrimination, control by economic and political elites etc.4 A cease-fire was agreed in January 2003, and peace talks began once more, but were broken off again in August 2003. The Maoist groups are in control of most remote hilly areas, particularly in the western part of the country. In those areas they have developed parallel or replacement structures, following government withdrawal. In Rukum district they have held elections, established a people’s court and tax offices5. Their methods of gaining influence have become more violent over time and security is seriously threatened in many parts of the country. They impose strikes, even in schools, organise roadblocks, abduct people and use methods of forced protection. Government staff cannot travel in government cars to numerous districts. Between August 2003 and December 2003 alone around 500 people have been killed in the conflict. Maoists abduct over 2,000, abduction results in exodus The Maoist rebels on Monday abducted over 2,000 people from the south-east part of Kanchanpur district, various dailies Thursday said. According to the Nepal Samacharpatra, the rebels abducted over 2,000 youths and students from Tribhuvan Basti, Parasan, Shripur, Laxmipur, Raikbarbichuwa, Baisebichuwa, Shankearpur, Kalika and Beldandi VDCs in Kanchanpur district. The rebels took them away in 28 tractortrailers to unidentified locations. With the Maoists escalating their abduction campaign in the district, 5,000 youths from the district have started fleeing their villages to neighboring Indian towns, Rajdhani daily said Thursday. nepalnews.com April 08 2004 Maoists abduct over 60 teachers in Taplejung Over 60 teachers from Singam VDC in Taplejung district were abducted by armed Maoist rebels on Tuesday to force them to participate in the ‘peoples’ oriented education’ campaign, reports said. nepalnews.com Apr 15 2004 Government finance In his budget speech on 17 July 2003 the Minister of Finance announced that the revised estimate of income and expenditure over the FY 2002/20036 shows a total expenditure of Rp 84.6 billion, 67% on the regular and 33% on the development budget. Recurrent costs made up 75% of the expenditures, capital costs 25%. Of total expenditures Rp 9.5 billion or 11% was used for repayment of principal debts. The sources of financing consisted of Rp 55.3 billion from domestic revenues and Rp 8.4 billion from foreign grants. The deficit of Rp 21 billion was borrowed, Rp 9 billion from multilateral donors and Rp 12 billion from domestic sources. The total expenditure translates into $48 per capita7. This is 19% of the estimated GDP per capita of $250. 4 Karki, AK (2002) A radical reform agenda for conflict resolution in Nepal, May, 2002. Cited in Collins et al 2003. 5 Philipson, L (2002) Conflict in Nepal: perspectives on the Maoist Movement, May 2002. Cited in Collins et al 2003. 6 Nepal’s FY runs from 16 July – 15 July. 7 84.6B NR/pop24.2M/exchange rate73=$47.89 MEH/Nepal/Situational Analysis, April 2004 16 The estimate of government revenue for FY 2003/2004 is 62.2 billion on a total budget of Rp 102.4 billion. The main sources of domestic revenue are indirect (61%) and direct taxes (17%).The main earners from indirect taxes are import duties,VAT and excise duties; the main earner from direct taxes is corporate income tax. Revenue from excise duty on cigarettes is Rp 2.3 billion, from alcohol Rp 2.5 billion, together good for 7.7% of domestic revenue and 4.7% of the total budget. Remuneration tax brings in Rp 1.3 billion only (2.1% of domestic revenue and 1.25 % of total budget). Foreign grants are expected to increase to Rp 15.5 billion (15.1% of the resource envelop), mainly due to a doubling of grants by bilateral donors. The foreseen deficit of Rp 24.6 billion is expected to be financed by foreign and domestic loans on a 50/50 basis. The amount of foreign grants only includes the funds that go through the MoF (the socalled Red Book). The real amount of external funds is much higher, as a substantial percentage of foreign aid goes directly to the other ministries, the districts, or through NGOs. Personal income tax is progressive, with the first 80,000 Rupees per year for a single and the first 100,000 Rupees for a couple being exempt (0%). The next 75,000 Rupees are taxed at 15%, any higher income than 175,000 is taxed at 25%. Only people in formal employment with government, larger companies or organisations pay income tax. VAT is 10% for all items that are taxed, but many items are VAT exempt, such as unprocessed food, lifestock and basic commodities such as oil, water, kerosine, salt etc. Domestic revenue is largely used to meet regular, recurrent expenditure (53% of the recurrent budget is for salaries), while development expenditure is increasingly dependent on domestic borrowings and foreign assistance. Of the 41.8 billion development budget for FY 2003/2004 75% is destined to be spent at the central level and 25% will go to the districts. The development budget for the poor Mid-and FarWestern regions has been increased by 34% to 6.5 billion Rupees. 17.1% of the total budget (24% of the recurrent budget) will be used for domestic and external debt servicing. Nepal does not qualify for the Heavily Indebted Poor Countries (HINPC) scheme, so no savings from debt relief are foreseen. Compared to the Rp 15.5 billion budget for the education sector, the 2003/2004 budget for the health sector is small with Rp 5.2 billion, which is 5.1% of the total government budget, $2,94 per capita or 1,18% of GDP. Of this amount Rp 3.2 billion is for development expenditure. MEH/Nepal/Situational Analysis, April 2004 17 The Health Sector Ministry of Health The MoH has a central section and three Departments: Department of Health Services (DoHS), Department of Ayurveda (traditional medicine), and Department of Drug Administration. The central MoH is responsible for policy making, planning, financing, international cooperation, human resources, monitoring and evaluation, as well as for the central and zonal hospitals. According to the NHSP-IP in practice senior officials spend most of their time in personnel management and non-policy issues. The policy and planning division of the MoH has 9 staff, who on average have been there 2 years and their capacity is inadequate. The Health Economics and Financing Unit (HEFU), supported by DFID, is headed by an economist from the MoF and has (among other staff) two health economists with a degree from Chulalongkorn. The MoH, like all ministries, suffers from the frequent changes in government, frequent appointment of new leaders and/or transfer of staff. The DoHS is responsible for the provision of all health services at the district level and below and produces the Annual Report. Regional Health Directors are responsible for technical backstopping as well as programme supervision. Their role seems to become less clear under the decentralisation process. At the district level and below, DDCs and VDCs are functionally responsible for the delivery of health services. Policies, strategies and plans Over the years a number of policy documents and plans have been produced. It seems that more or less simultaneously two sets of documents were developed, one government driven and related to the 5-year development plan cycle, the other EDP driven. There are clear interlinkages between the two sets of documents, although there are also quite some differences. It seems that the detailed work done by the MoH jointly with the EDPs has to some extent informed the development of the documents for the Tenth 5-year Plan. Officially the MoH is bound by the Tenth Development Plan and its MTEF. Below a schematic overview of production of all the main papers is given on a timeline. The shaded ones relate to the Tenth Plan. Annex 1 contains a summary of the ones, that appear on the MoH website (downloaded on 3 January 2004). Timeline Document 1991 <><> 1999 National Health Policy MoH Second Long Term Health Plan 1997-2017 MoH/NPC/EDPs/private/NGOs 2000 Strategic Analysis Operational issues and prioritization of resources Medium Term Strategic Plan MoH/EDPs WB MoH/EDPs 2001 none 2002 Medium Term Expenditure Programme MEH/Nepal/Situational Analysis, April 2004 Main agencies involved MoH/NPC 18 2003 Medium Term Expenditure Framework Health Nepal Health Sector Strategy MoH/NPC MoH/EDPs Tenth Plan MTEF Nepal Health Sector Program Implement Plan 2003-2007 PRSP Public Expenditure Review of the health sector Joint Staff Assessment PRSP NPC/Sectoral ministries NPC/MoF MoH/EDPs NPC MoH (HEFU) WB/IMF Below each of these documents is briefly described; in particular those features that have a specific bearing on the Macroeconomics and Health work are highlighted. National Health Policy 1991 In 1991 a National Health Policy was adopted. It’s primary objective was to extend the PHC system to the rural population. In order to bring basic preventive, promotive and curative health services to the whole population the plan states that: Sub Health Posts will be established in all Village Development Committees and mobile teams would provide specialist services to remote areas. Priority will be given to reduction of infant and child mortality. Hospital capacity will be based on population and patient loads and hospitals will be integrated into District Health Offices. A referral system will be developed. Training institutions will be strengthened in order to deliver competent staff for all health facilities. Alternative ways to mobilise more resources will be explored, such as insurance, user charges and revolving drug schemes Community participation will be sought and activities will be coordinated with NGOs, private sector and other government sectors Planning and management will be decentralised to the district level Second Long Term Health Plan 1997-2017 The SLTHP, published in August 1999, is to serve as a resource document for the preparation of successive five-year development plans and annual plans and will be periodically reviewed on the basis of evaluations. The SLTHP focuses on improving the health status of ‘those whose health needs often are not met: the most vulnerable groups, women and children, the rural population, the poor, the underprivileged and the marginalized’8. Disparities in health status would be addressed, assuring equitable access for the poor and vulnerable groups, with full community participation and gender sensitivity. Government and EDP funding should focus on areas of greatest need. Given resource constraints priorities have been set. Based on the demographic and disease profile (likely from the burden of disease study 1997) a package of Essential Health Care Services will be delivered at the district level and below before HMG and donor resources are diverted to provision of tertiary care. The SLTHP specifically mentions that resources should be redirected from high-cost low-impact interventions to the low-cost high-impact EHCS , while also improving effectiveness and efficiency. 8 Depending somewhat on the definitions of some of these terms, these groups combined could easily cover 90% of the population. MEH/Nepal/Situational Analysis, April 2004 19 With regard to health financing, the Plan states that a ‘safety net’ will be maintained to ensure that the needy and underpriviliged populations are not deprived of necessary health care because of inability to pay. Information on central and district level expenditures will be made more transparent and base-line data on public budgets, private expenditures and cost-sharing will be collected at the district level. HMG intends to decentralise (devolve – MP) responsibility and budget for PHC services to the District Development Committee, which will also be allowed to generate and retain local resources. Capacity for planning, management, supervision, monitoring and evaluation will be strengthened. The SLTHP includes targets for major outcome indicators (see page 2 and 3 of Annex 1). As output target the Plan wants the EHCS at the District to be available to 90% of the population living within 30 minutes travel time. The SLTHP includes key issues and policy options for the following areas: burden of disease, EHCS at the district, HCS beyond the district, health service delivery system, human resources for health, health financing, inter- and intrasectoral collaboration and decentralisation, management and organisational constraints, quality assurance, essential national health research, as well as the changing trend in communicable and noncommunicable diseases. It also mentions a number of emerging health issues that have not been dealt with and need to be addressed in the upcoming Five-year development plans. In September 1999 the Cabinet approved the EHCS package as part of its approval of the second SLTHP (see page 5 of Annex 1). The SLTHP describes many interesting policy options, but only a few of these refer specifically to improving access to health care services for the poor, although the overall objective of the Plan is to improve the health status of the needy. There is for instance no mention of the need to expand or upgrade the number of facilities in rural and remote areas. As usual targets are national averages. In the context of the objectives it would also be more meaningful to have specific targets and indicators for the vulnerable, women, children, rural populations and specifically for the poor. To reflect this the health management information system would need to be adapted. It would be helpful to disaggregate information on health status and utilisation by gender and income quintile for example. Strategic Analysis to operationalise the SLTHP In the fall of 1999, immediately after the SLTHP was published, HMG of Nepal and the EDPs together made a strategic analysis of the health sector, which was published in May 2000. It replaced individual EDP reviews. Its main purpose was to map out the action needed to develop capacity in order to improve delivery of health services. It would also serve as input to the 10th Five-year Development Plan. Four technical working groups reviewed the institutional context and relationships with EDPs, the capacity to turn policies into plans, the capacity to deliver the EHCS package, the capacity to regulate the private sector, and the capacity to meet the needs of the poor. The commitment to equity and meeting the health needs of the poor regardless of ability to pay is repeated. The analysis mentions that there is lack of information on the extent of inequity in provision and access to services, as well as on the way in which policies and management systems affect equity. There are no guidelines with respect to exemption of user MEH/Nepal/Situational Analysis, April 2004 20 fees for the poor. It is noted that given the expected future level of finance the identified EHCS will need to be further prioritised and choices will have to be made as to which population groups will be supported by government to receive these services. It is further noted that, contrary to agreed policy, more funds are flowing towards secondary and tertiary level hospital services, while the share going to PHC fell from 77% in 91/92 to 57% in 97/98. Due to lack of staff, drugs, equipment and maintenance, as well as poor supervision, public facilities have lower utilisation rates than private and NGO ones. Overall government spending on health remains low and there is considerable donor dependence. The Strategic Analysis recommends the following actions that could specifically benefit the poor: Encourage the private sector and NGOs to provide EHCS and consider contracting out. Advocate for additional resources from HMG Develop alternative sources of financing Increase community participation Develop guidelines with respect to user fees (exemption rules) Strengthen training institutes and identify future need for health workers Link (integrated) budgets to priorities, performance and outcomes Move towards a SWAp in order to use funds more efficiently and decrease transaction costs, starting with a medium term health strategy and financing framework that all stakeholders will agree to Establish a monitoring system that will assess the impact of the health strategy on the health status of the poor WB study - Nepal: operational issues and prioritization of resources in the health sector A month later, in June 2000, the World Bank issues its own, often cited, study on the health sector. It was based on several studies and workshops done between 1996 and 1999, in conjunction with the formulation of the SLTHP. The report analyses the burden of disease in Nepal, investigates whether allocation of resources corresponds to the main health problems and what the main problems affecting the health delivery system are. The key findings of the report, all of which are consistent with the priorities of Nepal’s Second Long-Term Health Plan, include the following: Expected population growth of 60% in 20 years will mean that a corresponding increase in health services will be necessary just to sustain the current level of inadequate services. Regional disparities in health indicators and health care are large (e.g. life expectancy ranges from 37 to 74 years). Nepal’s burden of disease will remain dominated by infectious diseases and maternal, perinatal, and nutrition-related disorders during the next decade. These disorders represent 69% of the BoD in Nepal. Degenerative and non-communicable diseases account for 23% and injuries and accidents for 9%. Children <5 bear 51% of the BoD. Targeted interventions should be aimed at disadvantaged areas and the poor. Interventions outside the health sector-particularly efforts aimed at improving water, sanitation, and public hygiene-would have a strong influence on the burden of disease, in particular of the poor. Current public sector allocations for the health sector are low and poorly allocated. Quality-enhancing nonsalary recurrent budget allocations are woefully inadequate, and resources will remain constrained for years to come. MEH/Nepal/Situational Analysis, April 2004 21 Institutional weaknesses and ineffective programme management are at the root of poor service delivery. Capacity for strategic planning, policy development, resource mobilisation and coordination is very limited. Absorption capacity is therefor also low. The private and NGO sectors are active, unregulated and the care they provide is often poor quality. Recommendations suggest an increased political commitment, focusing on infectious diseases, maternal, and prenatal ailments, and nutrition deficiencies. In addition, institutional capacity should be developed, and better health care systems ensured through public-private partnerships. Priorities should be established through careful planning, appropriate management, and financial availability. Detailed recommendations include limiting the role of the public sector to basic preventive and essential clinical care, expand public infrastructure in underserved areas and decentralise facility management. Medium Term Strategic Plan (MTSP) The follow-up of the strategic analysis was the Medium Term Strategic Plan, a logical framework that was developed later in 2000 to provide operational support for the SLTHP. More specifically, the MTSP provided the strategic framework for developing the health component of the Tenth Five Year Plan (2002-2007). The objectives for the medium term (still operational) are: To develop an effective health system for the provision of affordable and accessible Essential Health Care Services (EHCS) To promote a public-private-NGO partnership for the provision of healthcare To decentralise the health system and ensure participatory approaches at all levels To improve the quality of health care provided through the public/private/NGO partnership by total quality management of human, financial, and physical resources. For each objective several outputs have been defined, whereby especially the outputs for the first objective refer to equity and reaching the poor. It mentions improved access to and utilisation of health services by the poor and vulnerable, as well as a safety net for providing them with access to services “beyond the EHCS”. Medium Term Expenditure Programme (MTEP) Probably in the first half of 2002 the MoH drafted an MTEP (written by a local consultant) to operationalise the first three years of the Tenth 5-year Plan under development by the National Planing Commission (NPC). It clearly draws on the Strategic Analysis and the Medium Term Strategic Plan and concisely sums up the vision, mission, policies, strategies and lists the 4 objectives, 8 outputs and identifies a number of activities per output. Separately17 key quantitative targets are listed. It is not clear how they relate to the outputs and activities. The document also gives an overview of priority levels for each MoH programme and organisational units and includes a cost estimate for 3 years per the same. Programmes and organisational units listed as Priority 1: 1. Child Health: regular immnization (excl. Hep B); national immunization day; CDD; Vit. A and micronutrient supplementation; 2. Family Planning; Safe Motherhood; RH; 3. Epidemiology and Disease Control: communicable disease; emergency preparedness and disaster management; 4. TB control programme MEH/Nepal/Situational Analysis, April 2004 22 5. 6. 7. 8. Leprosy Control Programme HIV/AIDS/STD Hospitals: Teku, Bir, Kanti Children’s, Maternity and Bhaktapur All district hospitals; PHC Centers; HCs; District Public Health Offices; Health Posts; SHPs 9. Organisation: MIS; NHTC; Medical & Inst. Supplies; Health Laboratory; Community Drugs; Health Insurance; Institutional Capacity Building in relation to Decentralisation; Health Poverty Alleviation Fund (PAF) The cost estimate was prepared expecting a 20% reduction in the health budget for 2002/2003 (Rps 3,802 billion as compared with the previous year 4,581), while for the 2 consecutive years an increment of 10% each is foreseen. This was probably based on advance information from the MoF about the available resources. Medium Term Expenditure Framework for Health (MTEF-H) This document was prepared by the MoH (5th draft in July 2002) for the first 3 years of the 10th Plan as input into the Tenth Plan. The MTEF-H was based on the above MTEP, but used higher budget estimates (2002/2003 allocation 4,872 billion). The MTEF-H reiterates the goal, vision, mission, policies, strategies and key reforms of earlier documents. The MTEF-H provides somewhat lower, probably more realistic targets for the 17 key indicators, with the 2002 status as a baseline. It also adjusts the priority levels, based upon burden of disease, implementation capacity, equity considerations and on whether the programme is directed at the poor and vulnerable. A number of programmes and all hospitals are prioritised down to level 2. On the other hand some programmes are included in total, while the MTEP specified certain components. The MTEF-H lists the following programmes as Priority 1: 1. National TB Center and National TB Programme 2. AIDS and STD Center 3. Population and Family Health 4. Family Planing and MCH Programme 5. National Immunization Programme 6. CDD and ARI 7. Nutrition Progamme 8. Epidemiology; Malaria and kala-azar; Natural Disaster management 9. Leprosy control 10. Drug supply 11. HMIS 12. NHEICC 13. Vector Borne Disease Research Training and Control 14. Community Drug and Health Insurance A Policy Matrix gives an overview of programmatic activities, indicators and targets for each of the 13 (rather than 8) outputs related to the 4 objectives. The MTEF gives 3-year and 5-year budget estimates broken down by regular and development budget (both further divided into recurrent and capital expenditure) and by priority level. In the following tables the breakdown is shown for the first 3 years. MEH/Nepal/Situational Analysis, April 2004 23 Budget breakdown by priority level in percentages of total health sector budget Priority level Expenditure 2001/2002 Budget estimate 2002/2005 1-highest 48 57.6 2-medium 7 27.2 3-low 45 15.3 Interestingly these drastic changes in breakdown are not gradual, but foreseen for the first year 2002/2003 immediately, which seems very unrealistic, as many hospital costs are included in the 3rd priority level, and they are notoriously difficult to downscale. It will soon be known in how far the MoH succeeded in this. The MTEF also gives a budget breakdown by objective and as can be seen below almost ¾ of the budget is reserved for the provision of the EHCS. Budget breakdown by objective in percentages of total health sector budget Objectives Budget estimate 2002/2005 Provision of EHCS 72.6 Promote PPP 9.2 Decentralisation/participation 9.1 Improve Quality of services 9.1 The revised expenditure for the health sector 2001/2002 as mentioned in the MTEF-H was 5.195 billion Rupees. The allocation for 2002/2003 is less: 4.872 billion. For the forecast for 2003/2004 and 2004/2005 the regular budget was increased with 3% per annum and the development budget with 10%. The target in the MTEF for health sector expenditure as a percentage of total HMG budget is 6.5, while in 2003/2004 the real MoF budget for the health sector was only 5.1% of the total government budget. As said this MTEF-H served as input into the Tenth 5-year Plan, which is the operational document that the MoH is bound to and includes the final budget. See below. Health Sector Strategy (HSS) On the basis of the joint Strategic Analysis of 1999, HMG, NGO and private sectors and EDPs in the mean time continue to work together in a series of workshops and consultations led by the Health Sector Reform Committee. In August 2002 the Health Sector Strategy is finalised. It (again) provides a concise situational analysis, lists 6 key issues with their strategic implications and goes on to formulate 3 programme outputs and 5 Sector Management outputs, based on the previously agreed 4 objectives. It announces that a costed sector plan will be drawn up to deliver this strategy, covering the Tenth 5-year Plan period and taking account of its MTEF, which is being developed at the same time. Although the latter gives the impression that the costed plan will be based on the available resource envelop, interestingly it is mentioned that “it will identify the additional financial and technical support needed for its implementation. Negotiations can then take place with EDPs as to how that support can be made available”. Tenth 5-year Development Plan This Plan of over 600 pages covers the years from mid-2002-mid 2007 and was approved by the Cabinet in Feb 2003. It took 2 years to develop. During this process it became clear that MEH/Nepal/Situational Analysis, April 2004 24 the fiscal situation was deteriorating and available resources for the Tenth Plan would be less than previously expected (38 billion, rather than 50 billion Rupees for the development budget). Therefore preparation of the MTEF was started by end 2001, so that the Plan could be scaled down as necessary, while protecting the key priorities. The principle was established that P-2 and P-3 activities would only be funded if funds would still be available after providing for the P-1 activities. It contains a 20-page chapter on health, written in a diferrent style and wording than any of the other documents mentioned above. It seems to be a truly Nepali product. Also the content is different from what the MoH produced before. The consultant does not have any information at this point how, why and by whom decisions on changes were made, but this seems to be important to find out for future planning. The Health Chapter starts out to compare progress of the Ninth Plan with its targets. Most targets have been met, except for delivery of obstetric care by trained health workers and child mortality. In the case of obstetric care this is probably due to a change in definition of what constitutes a trained health worker (local birth attendants – sudenis – are no longer counted as such). The overarching national objective for health as formulated in the Tenth Plan clearly links health to poverty reduction: “Reduce the magnitude of poverty among the Nepalese people substantially and sustainably by developing and mobilising the healthy human resource”. The two objectives deduced from this include improving quality of health services, access by the poor, especially in rural and remote areas, and specifically access to RH and FP services in rural areas to bring down population growth rates and improve maternal health. Bring down popualtion growth rates did not feature in any of the MoH policy documents before. Decentralisation and promoting public-private partnerships are not mentioned as objectives, but as strategies to reach the objectives. The chapter goes on to describe 7 strategies related to the 2 objectives and the policies related to the strategies in a fuzzy way. The relationship between goals, objectives, strategies and policies is not very logical, nor clearly quantified. The plan also lists 16 key health indicators for the Plan’s period, ending in 2007. They are based on the status in 2002 and targets are given for the general and the alternative growth scenario. See Annex 2. Fully consistent with the MTEF-Health the following programmes are labeled Priority 1: 1. Expanded vaccination and national polio vaccine 2. Control of ARI and DD 3. Nutrition 4. Safe motherhood and FP 5. RH of adolescents 6. Female community health volunteers and trained traditional birth attendants (sudenis) 7. Prevention and Control of malaria, kala-azar, tuberculosis, leprosy and HIV/AIDS/STDs 8. IEC 9. Natural disaster management 10. Centre for vector-borne diseases and their control, research and training 11. Supply management. MEH/Nepal/Situational Analysis, April 2004 25 12. Essential medicines 13. Health insurance 14. Information management Health training, some key hospitals as the children’s hospital, maternity hospital and infectious disease hospital, as well as auxiliary services, monitoring and evaluation and research, and urban health and ayurveda services have been given priority 2. A specific target for access to facilities is included: a health institution or outreach clinic should not be more than 2 km or one hour walking away. In line with poverty focus the Plan also promises special programmes in Far Western and Mid-Western Development Regions. In the context of disparity in the conditions of the health services mention is made of “an independent national Microeconomic (!) Health Commission, to be set up within the accepted structure of the national programme for poverty eradication”. The Plan includes a budget for each of the 43 programmes, divided over the priority levels, as shown in the table below. Under the expected average growth rate of 6.2%, the Tenth Plan allocates almost 5% more to P-1 programmes than the MoH did in their MTEF-Health, at the expense of P-3 programmes. Under the alternative average growth rate of 4.3% (which is the operational basis at present9), the P-3 programmes are scheduled to loose 90% of their funding, in order to keep the P-1 programmes fully operational. Given the fact that the average growth rate during the Ninth Plan was 3.6% even the lower alternative growth rate seems to be optimistic. And the realism of scaling down government support to P-3 programmes (mainly hospitals) with 90% is questionable. Source: Tenth Plan, Chapter 24.9 Nepal Health Sector Programme – Implementation Plan 2003-2007 (NHSP-IP) The Plan, based on the Health Sector Strategy of August 2002 and developed under the guidance of the Health Systems Reform Committee, is ready one year later, in August 2003, but without a financial paragraph. For each of the 8 outputs the IP describes which of the 24 longterm strategic objectives are supported by the output, and lists the activities that will be undertaken and their key indicators. New health reform actions are added to the existing activities EHCS programme (see Annex 3). In the accompanying logical framework also the means of verification and assumptions are included. Many targets (OVIs) do not carry a specific percentage however, but show X%. Whether this has not been agreed yet, or whether 9 PRSP para 177/page 65 MEH/Nepal/Situational Analysis, April 2004 26 the consultant had a non-final copy of the document is not clear. “The key focus of the IP is to increase the coverage and raise the quality of the EHCS, with special emphasis on improved access for poor and vulnerable groups”. Key new activities, relevant for this situational analysis, include: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. costing of and resources allocation for EHCS redefine institutional arrangements for delivering EHCS develop systems for priority access for poor and vulnerable groups introduce local management of sub-health posts establish district level health co-coordinating committees update inventory of existing private/NGO/public involved in health sector, by district define an appropriate public/private/NGO mix for each district strengthen regional and district management capacity building at central and district levels identification of health sector priorities and reallocation of resources to priorities services alternative financing arrangements, such as community health insurance, explored MoH to develop national guidelines for user fee practices and other payments in public facilities drug financing mechanisms strengthened to support increased and equitable availability of essential drugs A Programme Preparation Team estimated the resource envelope for the health sector over the Tenth Plan period. The most realistic scenario, based on 4.6% GDP growth, a revenue growth of 14%, foreign assistance at 4.6% of GDP, a budget deficit of 2.7%, a 5.2% share of the govt budget for health and 70% of that for the EHCS, comes to a total of $US 663 million over 5 years (1$ =78 rupees), which translates into $4.72 per capita annually. This includes donor funds in and outside the Red Book. The report concludes that this is a far cry from the $12 in the WDR 1993 and the $34 mentioned in the CMH report. However real costs might be less in Nepal, but cost information on the EHCS are not available, and the IP announces cost studies and cost estimations by key programmes, divisions and centres. The World Bank has in the mean time commissioned a study to cost the NHSP-IP and provide unit costs of the EHCS. The results of this exercise will be available in April 2004. The consultant received a draft report dated 25 February 2004, which seems to not include all costs involved in scaling up to meet needs and does not make use of real country data in many cases. The NHSP-IP also includes an Annual Planning Cycle timetable. It is intended as a move towards a SWAp, but as yet the majority of donors does not favour pooled funding. The Plan indicates a big move towards a joint vision however, and HMGN and EDPs have agreed to joint planning and review exercises. PRSP and JSA A “more sharply focused” summary of the Tenth plan functions as the PRSP, dated May 2002. It received a positive Joint Staff Appraisal in October 2003. The following health indicators made it into the key goals and targets in the PRSP: Infant mortality rate, total fertility rate, maternal mortality rate, contraceptive prevalence rate, obstetric services by trained manpower, average life expectancy. Annex 4 contains major paragraphs from the PRSP dealing with or relevant for health. Strangely enough many details are quite different from the health content of the Tenth Plan. For instance the PRSP clearly indicates expansion and upgrading of PHC centres and district hospitals and strengthening outpatient care in hospitals. These objectives have not been MEH/Nepal/Situational Analysis, April 2004 27 encountered in any preceding document. The Policy Matrix in logframe format also includes many different activities and indicators than the NHSP-IP. Conclusion on policies, strategies and plans Many good documents have been prepared by HMGN and the MoH in collaboration with EDPs. The problem seems to be that the most current, prevailing documents have somewhat different objectives, strategies and activities. The main govt document in force is the Tenth Plan, the health chapter and budget of which are organised by priority programme and/or organisational centre, probably following present budget lines. The NHSP-IP, more donordriven, is organised by objectives, outputs and activities in a logical framework and does not have a budget yet. The PRSP, supposed to be a summary of the Tenth Plan, contains elements of both the Tenth Plan’s Health Chapter and the NHSP-IP, but also includes new activities. It is therefore not clear at this point which document the MoH is implementing and using to monitor its activities. It would be helpful, if a detailed comparison was made between the IP, the Tenth Plan and the PRSP, after which the MoH, NPC and MoF could sit together with the EDPs and decide which activities they will implement together. Provision of health services Public health facilities The government of Nepal has constructed or upgraded a Health Post (HP) or Sub Health Post (SHP) in 97% of VDC areas and a PHC centre in 93% of electoral constituencies. There are 83 public hospitals over the kingdom. There are 4 districts without PHC level facilities and 4 districts without a hospital (not the same districts). In 2003 there are in total 4,439 public health facilities under Ministry of Health: 3,170 SHPs, 700 HPs, 190 PHCs/HCs, 67 district, 11 zonal and 5 central hospitals. At the lowest level 15,548 PHC outreach clinics are being operated from the HPs and SHPs. Government also operates 6 military hospitals, 1 police hospital, and a number of specialty and teaching hospitals. Despite these impressive numbers the NHSP-IP mentions that only 29% of the poor can reach a health facility within half an hour, while 57% of the wealthiest households can. The Strategic Plan for Human Resources in Health (see below) mentions that the public sector bed to population ratio is 1 bed to 5,435 people, providing 59% of total beds. Together with the 41% beds provided in the private sector (profit and not-for-profit) the bed to population ratio is 1 bed to 2,993 people. Around half of public beds are in acute tertiary care hospitals and longstay specialty hospitals, which have a 95% occupancy rate (OR), partly reflecting cases that could have been treated at a lower level health facility. District hospitals have an OR of 60% and Health Centres with beds only 10%. The OR for all public sector beds is 72%. The OR of private sector beds is 50%. The national ALOS was 4.2 days in 2001/200210. Like in many low-income countries government is not able to provide or guarantee the provision of basic health services to the population, as intended. The problem is the quality of care (equipment, drugs and supplies, as well as technical knowledge of staff) and the availability of health workers to work in the rural and remote areas. On the demand side there are problems such as lack of awareness, negatively influencing health seeking behaviour, distance to the health facility, and perceived low quality of public health services. The NLSS 2003 includes questions on what kind of amenities are present in the health facility, and which essential services are available. 10 page 391 Annual Report DHS 2001/2002 MEH/Nepal/Situational Analysis, April 2004 28 Utilisation According to the Nepal Living Standards Survey (NLSS) 1996 40% of rural cases and 13% of urban cases were treated at public PHC centres and HPs. When disaggregated by income quartile it became clear that 5% of the richest quartile and only 3% of the poorest quartile made use of public facilities. This means that the public services are mostly used by the middle income groups, while the rich go to the private sector and the poor don’t go at all. The PER 2003 concludes that there is a persistent inequity in the use of services by girls and women for non-maternity care. The difference in utilisation of health services is reflected in terms of per capita expenditure: the richest households spend 8.7% and the poorest households only 3.2% of their household expenditure on health care. The NLSS 2003 asks questions on why people do not visit government health facilities. A referral system does not exist yet, but will be introduced shortly. A feasibility study has been done, manuals have been developed and training conducted. The consultant visited a SHP in a village (pop. 4400 over 742 households) in the hills about 25 km from Kathmandu. It was a temporary housing, since the VDC intends to build a new one. The present SHP had two rooms (a waiting and a consultation room) with a corrugated iron roof, was very, very simple, with faded health education posters on the wall, wooden benches and a kerosine steriliser. A few drugs in stock in a locked cupboard. There was noone there, no staff, no patients. The village health profile was manually kept up-to-date on a chalk board in the waiting room. The previous VDC chairman, whom I met, indicated that the major health problems in this village are: low awareness of disease, ARI, alcohol abuse, pregnancy related problems and injuries. Girls marry very young at 14-15 years and have 3-4 children. Human Resources In April 2003 the Strategic Plan for Human resources for Health – 2003-2017, prepared by the PP&IC Division with support of GTZ, was published by the MoH. The Plan provides an analysis of the current situation, essential policies, objectives and targets for the future workforce, and training proposals. The total number of staff per population is low. While there is a deficiency in the middle technical grades, the high number of unskilled and semiskilled labour (70% of the total) will need to be reduced. While expansion of training middle level staff is needed, a surplus of medical officers is expected. Training is at present driven by individual initiative, but will have to be more managed. Role of managers vis-à-vis the administration remains ill-defined. The public sector has only one medical doctor for each 18,500 inhabitants (more of them sNPCialists than medical officers!) one nurse for 4000 people, a paramedic or health assistant for 4500 people, a VHW for 6000 people, an MCHW for 7500 people and one hospital bed for every 2000 people. Furthermore there are 54,000 Female Community Health Volunteers and 15,000 TBAs. Management information on HR deployment, vacancies, staff transfer etc. is not well developed. Human resource development will need to be professionally managed. The MoH is presently lacking the capacity to do this. Health workers in Nepal earn relatively well, but pay differentials between senior staff and unskileld workers are small. An Auxiliary Health Worker, running an SHP receives Rp 6,000 per month ($82). Doctors working in a PHC centre can earn as much as Rp14,000 per month ($192). Even so it has been difficult to find providers who are willing to serve in remote areas. The government has tried to get health workers out to remote areas by providing MEH/Nepal/Situational Analysis, April 2004 29 monetary and training incentives. The first has not worked, but the second has: after 5 years of service, of which one year in a very remote area or two years in a near remote area, the Health Act guarantees the health worker full time higher education. During this time the health worker will receive twice his regular salary. The NLSS will provide information on what kind and how many health workers are actually present for how many hours in each health facility. Relevant recommendation in the Strategic HR Plan for MEH: Expansion of staff will focus on SHPs and the related outreach clinics to strengthen the availability of primary care services. Devolution of health services By the District Development Act of 1992, later replaced by Local Self Governance Act of 1999 HMG of Nepal decided to decentralise management responsibility to lower levels. The mode of decentralisation is devolution. The process of devolution is phased in. Central and zonal hospitals are semi-autonomous and receive block grants, based upon number of beds and occupancy rate. District hospitals are financed by line item and all hospitals are still directly financed by the MoH. In the future they will be financed through the DDC by the MoF. At the moment the central MoH and the DOHS still decide the resource allocation from the central budget for each health facility lower than the district hospital. The basis for this allocation is catchment population, geographical coverage and utlisation data. Resources for PHC centres and below then go from the central level MoF directly to the District Development Committees (DDC), who passes them on as block grants to the PHC facilities and to the VDCs. Similar arrangements exist for grants form the Ministry of Education and the Ministry of Local Development. In the future the DDC will be able to decide the resource allocation over the different facilities. The District Health Officer is responsible for all publicly financed health activities in the district including the organization and management of the district hospital, PHCs, HPs and SHPs. Local Health Committees have been established, but they do not have a plan of action yet. Their capacity needs to be built up. The DHO also operates the bank account and is responsible for payment of salaries for all health workers in the district. With a bold policy the government has decided to transfer ownership of HPs and SHPs to the VDCs. This means complete privatisation, since property, equipment and staff are handed over. In 2002/2003 468 HPs and SHPs in 12 districts were handed over. In 2003/2004 another 700 will be handed over in 14 districts. The time-frame to complete hand-over of all health posts is 3-4 years (by the end of the Tenth Plan). The National Health Training Centre has conducted 1 week training for the facilities involved, using operational and financial manuals, supported by DFID, UNICEF, USAID/CARE International and GTZ, who have health care strengthening initiatives in the districts to be handed over. The Regional Health Offices officially have a supervisory task, but it seems that they are not functioning very well, at least partly due to the impossiblity to travel due to insecurity. Collins et al (2003) describe the implications of the insecurity for the devolution process (see below). Local elections, scheduled for July 2002, did not take place due to the security situation, and power was handed over to the lower level bureaucracy, rather than to elected local government officers, as mentioned above. How this hand-over relates to the parallel structures the Maoist have set up in many districts is not clear. MEH/Nepal/Situational Analysis, April 2004 30 Private sector and NGOs There is a growing and unregulated private-for-profit sector, that cannot be clearly distinguished from the public sector, as many doctors working in the public sector have a private practice on the side. A permission is necessary, but easily granted, in order to keep doctors in public service. As usual private practitioners are most dense in the urban areas, but the ongoing NLSS will shed more light on the number of private pharmacists and doctors throughout the country. There are 14 non-government teaching hospitals and 3 community run hospitals. As mentioned above 41% of hospital beds are in the private and NGO sector. 237 indigenous and international NGOs reported to the District Health Office (DHO), spread over all development regions, but 60% of them work in the Terai. In the Annual Report of the DOHS 2001/2002 it is mentioned that 54 private health institutions reported to the DHO. Although this is undoubtedly a minute fraction of the total, almost all of them were concentrated in the central and western regions. The policy of the MoH is to recognise the important contribution the private and NGO sector make in the delivery of health care services, to better coordinate with them, avoid duplication of efforts and to formalise partnerships by engaging into service delivery agreements. The PRSP specifically mentions in the policy matrix for health that the private sector and NGOs have a role in environmental and occupational health, as well as in sanitation facilities. The NLSS also asks about NGO activities in each ward. NGOs used to need approval for their activities, but now they only hve to register. NGO coordination is weak, but the Council of Social Welfare has a list of NGOs. Implications of Maoist insurgency Also the delivery of health services has been affected by the Maoist insurgency. The MoH informally estimates absenteeism to reach 50% and many health workers cannot carry out their duties without harassment, intimidation and interference by both Maoist and government forces. There are reports of destruction of SHPs, blockades of essential drugs, difficulties in supervision and monitoring visits by regional and district health officers, disruption of the cold chain, all of which impact negatively on the delivery of the EHCS11. Health financing Public Expenditure Review A Health Economics and Financing Unit (HEFU) was established in the MoH in July 2002. They produced a Public Expenditure Review of the health sector in July 2003 (supported by British Council and DFID), covering the period 1999/2000 to 2001/2002. Sources of finance In the FY 2001/2002 public expenditure in the health sector, including donor spending was Rp 398 or $5.1 per capita12. 11 12 Collins et al, 2003 An exchange rate of Rp 78 to the US dollar was apparently used. MEH/Nepal/Situational Analysis, April 2004 31 The central government contributed 50.6%, donors 39.7%, SOEs 7% and local governments 2.5%. All domestic resources together financed 60% of the health expenditures or Rp 239 or $3.10 and the donors $2 per capita, together being 2.2% of GDP at the time (1.3% and 0.9% respectively). The central government share was Rp 201 or $2.58 per capita, being 1.1% of GDP The share of locally raised funds by DDCs and VDCs is still low, but growing. Allocations of funds In 2001/2002 74% of HMG and EDP indirect funding was spent on recurrent costs, 26% on capital costs. Of the recurrent costs 55% was spent on salaries, i.e. 40.7% of total spending. Spending on care provided at district level and below made up 60% of expenditures, zonal and regional level care 7% and tertiary level care 24%. The remaining 9% was used for the employees medical benefits scheme The share of funding going to the rural areas decreased somewhat over the 3 years The share of funding going to Priority 1 programmes (as defined in the 10th Plan and the MTEF) has decreased from 58% to 50% over the last 3 years, whereas the expenditures on Priority 3 programmes increased from 33% to 40% (the targets are 71% on P-1 programmes, 28 on P-2 and only 1% on P-3 programmes under the 4.3% GDP growth scenario) The expenditure share on interventions that address infectious diseases, MCH and nutritional deficiencies (Group 1 diseases, accounting for 68% of the burden of disease) is 60% Although 85% of the population live in rural areas and likely have higher health needs than the urban population, health spending on rural areas accounts for only 51% of total expenditures, and spending on urban areas for 32%. The remainder is spent on national programmes that cover both urban and rural areas. The trend over the last 3 years is one of decreasing expenditures in rural areas and increasing expenditures in urban areas The share of RH in total public expenditure decreased drastically from 14 to 3% due to the closure of the population and Family Health Project, while maternal mortality remains high The share of health expenditures for children under 5 (>12% of the population) was only 4.7%, while they bear the major share of the burden of disease The PER further revealed the following important information: The MoH spent 82% of the public health budget, the MoF 13% and other ministries the rest EDPs changed their funding channels and increased their direct funding (not through MoF, the so-called Red Book) to 90% in 2001/2002 (up from 56% 2 years earlier) DFID and JICA are the biggest donors to the health sector, together good for around 50% of all donor aid While the regular budget of HMG was fully used, only 27% of EDP development budget was used in 2001/2002 (from 61% two years earlier) MEH/Nepal/Situational Analysis, April 2004 32 Budget for 2003/2004 The official 2003/2004 public budget for the health sector is Rp 5.2 billion13. This translates into 5.1% of the total public budget, including foreign grants and loans going through the MoF. On a per capita basis this is Rp 215, or $2.95, being 1.2% of GDP per capita ($250). If we assume that donor aid for the health sector through the MoF stays at 10% of total donor grants, the true domestic central share of the public health budget will be Rp193.50 or $2.65, being 1.06% of GDP/capita. This represents a decrease of Rp7.50 as compared with 2001/2002 expenditures and given inflation of around 8-10% per year, a real decrease of Rp 9 or 4.5% per capita, compared to expenditures of 2001/2002. National Health Accounts HEFU is developing a system of NHA for which they are carrying out several surveys: INGO/NGO survey Private company expenditure survey Private health providers survey Public health facility survey Drug expenditure survey The first round of NHA data will be available in April 2004. Total health expenditure per capita is preliminarily estimated at around $1514. Given that total health expenditures of HMG and EDPs is currently around $5, the OOP expenditures are estimated to be 2/3rd of total expenditures at $10 per capita per annum. Taxes While income tax is progressive and poor people are unlikely to pay income tax at all, the main taxes that individuals pay are VAT and excise duties on tobacco and alcohol, both of which are regressive in nature, compensated somewhat by the exemption from VAT of basic commodities. In theory this means that public services which are financed from government revenues are relatively more expensive for the poor than for the rich. In the case of the really poor, it is unlikely that they consume many products that have VAT or excise duties levied on them, so in practice they probably hardly contribute to government revenue at all. As of the present FY, a portion of excise duty on cigarettes and alcohol will be earmarked through the budget to support programs for preventing tobacco-related diseases. Fifty percent of the earmarked budget will be used to support institutions engaged in the prevention of cancer, while the remaining 50 percent will be used to assist institutions engaged in the prevention of heart and tobacco-related diseases and also in running anti-smoking and alcohol campaigns15. The consultant was informed that this health tax is only 40 paisa (Rp 0.4) per pack of 20 cigarettes16. The consultant could not find out how much the total excise duty per pack of cigarettes is. But since the revenue from excise duty on tobacco and alcohol is Rp 4.8 billion, this total amount is more than the entire health budget that comes from central domestic revenue sources for FY 2003/2004 (Rp 5.2 billion minus 10% EDP funds going through the MoF is Rp 4.68 billion). Forty paisa per pack of cigarettes seems therefore very low and the MoH could make a strong case for a much higher share of the excise duty. 13 Whether this is the budget for the MoH only, or also includes the allocations for other ministries is not clear from the budget speech, but the consultant takes it to mean that it does include the allocations for all ministries . 14 Oral communication Tanka Mani Sharma 15 Budget speech 16 Oral communication Anil Mishra MEH/Nepal/Situational Analysis, April 2004 33 User fees Nepal introduced user fees 20-30 years ago. All public health facilities are allowed to charge fees. The level of the fees at the HP and SHP service level is set by the Local Health Committee. The PHC centres and hospitals charge higher fees. The facilities can retain all of the fees and are not required to report the amount they have received. So this source of income is not well documented. Since 2002-2003 the MoH is requesting this information however. As user fees are a fixed amount, they are income regressive and the poor pay relatively more than the rich. There are exemption schemes. Hospitals for example have been instructed to allocate 5% of the centrally provided grant and 5% of their other income to treating the poor, marginalised and disadvantaged. Also community drug programmes have an exemption scheme. However, the exemption schemes are said not to work properly, because there is no incentive for providers to exempt people. Besides formal fees, health providers also charge informal fees, although the extent to which this happens is unknown. Insurance Government operates a security fund for its 300.000 civil servants from which predefined health benefits for employees are paid if and when needed. Care to be paid from the fund can only be provided in public facilities. Government pays a maximum of 12, 18 and 21 monthly salaries for all officers, support staff and lower staff respectively into the fund, while employees themselves do not contribute. For the current budget year, government has increased the fund to enable costly medical treatment when civil servants fall seriously ill. An additional Rp 40.000 each was made available for an estimated 3000 people needing hospitalisation and Rp 200.000 each for an estimated 200 people needing ‘special treatment’. The management of the fund is contracted out to an insurance company, external to government. HEFU is looking into the possibilities to establish Social Health Insurance for salaried employees and Community Health Insurance (CHI) for people not formally employed. HEFU believes that SHI is at present premature, because the formal sector is too small. Instead they want to look into the possibility to link up specific companies with hospitals, whereby the companies would contract the hospitals to provide health services to their employees without a third party involved. From the company survey that they did it became apparent that some of them already have an internal scheme, whereby the company pays the health care costs of its employees. Community Health Insurance Schemes will shortly be introduced on a pilot basis in Morang, Dhading, Nawalparasi, Banke, Gorkha, Lamjung, Kailali and Solukhumbu districts17. This is easier to set up, because no legal framework is required, as is the case for SHI. The CHI would be centered around a facility. HEFU estimates that 20-25% of the catchment area will be poor. These people will get a card and their premium will be subsidised by the government. They would pay a small percentage themselves. Once a year the ward officer would have to re-estblish the poverty level of card-holders. HEFU might want to look into the possibility to set up a re-insurance system to increase the risk pool. A CHI coordination commission, consisting of government, donors, NGOs and ILO, has been set up. At present the government does not have any technical assistance in setting up this CHI pilot, but would 17 Budget speech 2003/2004 MEH/Nepal/Situational Analysis, April 2004 34 like to make use of 1 local and 1 international consultant to evaluate the pilot. This could possibly be financed through the budget for the Macroeconomics and Health planning phase. Dr. Aviva Ron, private consultant for ILO, is working on a masterplan for social insurance, which would incorporate formally employed and self-employed people and their dependents. The insurance systems should be big enough to pool sufficient funds and cover both PHC and hospital costs. As said HEFU does not think this is feasible at present. Health Management Information System The DoHS publishes very detailed annual reports with an overview of the health policies and strategies, population and health facilities, sections on child and family health, disease control, in- and outpatient care statistics, morbidity and mortality data, health education, training programmes, availability of drugs, laboratory services, management of logistics, administration and finance. It also includes sections on the contribution of EDPs. An effort is being made to capture information of NGOs and private sector, but this is still scanty. Most key data are available per district. Health indicators and targets As mentioned above in Annex 2 the health status per 2002 and targets for the Tenth Plan period is given for 16 key indicators. The main causes of mortality and morbidity cannot be found in the Annual Report. A small leaflet published by the MoH contains top 10 morbidity figures, but it is not clear whether these are based on hospital in- or outpatient data or on PHC data. Based on data from 1996, the Burden of Disease Study18 showed that infectious diseases, maternal and perinatal ailments, and nutritional deficiencies (Group 1 diseases) together account for 50% of all deaths, 80% of deaths of children under 5, and 69% of the total burden of disease. Degenerative and non-commnicable diseases account for 23% and injuries and accidents for 9% of the total burden. The number of DALYs lost in Nepal is much higher than in India or China, the neighbouring countries. The BoD is higher for females than for males, particularly for group 1 diseases, suggesting gender bias in health seeking behaviour. Children under 5 carry half the disease burden. Leading causes of BoD in the 0-4 age group are perinatal diseases, acute respiratory infections, diarrhoea and measles. The leading causes of DALYslost for women are maternal illness, tuberculosis, burns and psychiatric disorders. For men diseases influenced by lifestyle were more important, such as ischemic heart disease, cirrhosis, alcohol dependency and injuries and accidents. Projections for the next 10 years show that Group 1 diseases will keep accounting for the main part of the BoD. The study recommends to give priority to Group 1 diseases, focus on children and safe motherhood programmes, increase the focus on tuberculosis, improve sanitary conditions, control risk factors for non-communicable diseases (such as hypertension and diabetes), reduce smoking and drinking, and target underserved areas. As these data are somewhat dated, there is a clear need to compile an up-to-date overview of morbidity and mortality and compare this to the EHCS package. 18 Nepal, operational issues and prioritization of resources in the health sector. WB, June 8, 2000 MEH/Nepal/Situational Analysis, April 2004 35 MDGs (HSS June 2002) In February 2002 HMG of Nepal together with the UN published a Progress Report on the MDGs. The conclusion is that it is unlikely that the MDGs will be reached, with a possible exception for the reduction of child mortality. The targets to be reached differ in different documents, that were all published in 2002: Status and targets for child mortality rate (CMR) and maternal mortality rate (MMR) Status Target 2015 Tenth Plan CMR 91 (2001) 74 MMR 415 (?) 315 MDG Progress Report CMR 91 (2001) 54 MMR 539 (1996) 129 or 213 Health Sector Strategy CMR 91 (2001) 30 MMR 539 (1996) 134 The HSS document seems to have mistakenly calculated the targets with 2001 as a baseline, rather than 1990. The Tenth Plan seems to have taken into account that the set targets were not realistic and has probably adapted them. Child mortality reduced over the past decade from 162/1000 live births in 1990 to 91 per 1000 now. The MDG target is 54 per thousand (74 in the Tenth Plan). Mortality is highest in rural areas and the mountain region in particular. MMR is currently high at about 539 per 100000 live births. The target is 129 or 213 (dependent on which baseline data for 1990 are used) and 315 in the Tenth Plan. No info on geographical spread. Data on HIV is scarce but the infection rate is rising. Estimated prevalence is 0.29% but it is much higher in at risk groups. Malaria fatality rates have declined dramatically –from 92 per 100,000 in 1992 to 29 in 1997. However it is still a problem and adequate control programmes will have to continue. Tuberculosis is a major challenge. Though the rate has increased from 92 to 106 cases per 100,000 from 1995 to 1998 this is due to better reporting systems. Effective programmes are in place but the strategy will need to reach the 15% not yet covered by the DOTs programme. Essential health interventions The disease profile indicated that: Children under 5 account for half of the total disease burden, with the leading causes of mortality and morbidity being perinatal conditions, ARI, DD and measles. The disease burden of females is higher than of males, primarily due to high maternal mortality and morbidity. Infectious diseases, maternal and perinatal disorders and nutritional deficiencies will still dominate the BoD pattern throughout the first decennium of the next millenium. MEH/Nepal/Situational Analysis, April 2004 36 Realisation of scarce resources led to a prioritisation attempt on the basis of the 1996 Burden of Disease study. In September 1999 the Cabinet approved a package of Essential Health Care Services at the district level as part of its approval of the Second Long Term Health Plan. Twenty broad areas of intervention were identified, with the bold intent to ‘redirect resources from high-cost-low-impact interventions to those that can substantially reduce mortality, morbidity and disability without increasing expenditures’. By 2017 these EHCS should be available to 90% of the population within 30 minutes travel time. The list is included in Annex 1. Specific targets were included for important indicators such as IMR, <5MR, MMR, LE, CBR, CDR,TFR, CPR, attended deliveries and weight of newborns. These need to be compared with the MDGs, as they use about the same timeframe. The HSS of August 2002 acknowledges that the whole package of essential health care services is not immediately affordable. Initially therefore the focus will be on four main areas of essential care: safe motherhood and family planning, child health, control of communicable diseases, and strengthened out patient care. The delivery the EHCS will mainly focus on personal preventive and curative services. It will however be supported by a national programme to increase knowledge about common illnesses and cost effective interventions particularly in the four priority areas, targeting both consumers and providers in the informal sector e.g. rural shopkeepers and pharmacists. Although the ECHS will not initially give priority to non-communicable diseases it is essential that the BCC programme in the first five years includes programmes aimed at reducing tobacco and alcohol abuse. HMGN will also consider what legislative and taxation policies could be effective in this latter area. The HSS continues to state that “The first task will be to identify and cost the resources necessary to delivery the package across all districts. Prioritising these services at VDC/sub heath post level will require a major transfer of resources. The staff and skills mix at that level will need revision, regular and timely provision of drugs and equipment will be required and service protocols and quality standards will need to be established to build confidence and awareness. This will draw on the work already done in these priority areas by the DOHS. The role of the district hospital in supporting the EHCS needs to be further developed, particularly their role in providing essential obstetric care. Clear policies for financing and providing care outside the priority programmes will have to be in place with exemption mechanisms for the very poor”. Phasing of scaling up is foreseen: “Fifteen districts will be targeted initially to achieve full coverage of the essential services at all levels within three years. They will be selected to ensure maximum coverage of the poor and vulnerable. Over years four and five extension across a further twenty districts will be targeted”. Partnerships form a key feature in order to deliver the services: “A key feature will be integrating programmes in these areas being supported by EDPs. Where appropriate NGOs and private providers will be contracted to provide the services”. Both outcome and process/output indicators will be monitored, as well as utilisation of and satisfaction with the services: “Indicators of progress will include the rate of increased coverage, the MDGs, the increase in budget both real and proportionate given to the EHCS, community perception of services available and accessed, and direct health impact”. MEH/Nepal/Situational Analysis, April 2004 37 Conclusion Although the EHCS package has been further prioritised, it is not clear which concrete activities are included. The NHSP-IP has outputs, broad actions, but no detailed activities for each output. The Tenth Plan includes prioritised programmes, but does not include the kind of detail, that sheds light on which parts of these programmes, or which activities, belong to the prioritisation. This obviously makes the costing very difficult. Research The consultant visited the National Health Research Council (NHRC), established in 1991 to promote and facilitate medical and health research. They coordinate, collect and disseminate information, operate a library, strengthen capacity, ethically and technically assess and approve study proposals, and give training. Each Regional Health Directorate has a focal point for research. They get 25 laks (1 laks =100,000 Rupees) or around $33,000 core funding from the government and a yearly contribution of $40,000 from WHO, and have a 5-year grant of $200,000 from Mary Knolls. A 3-year $200,000 project funded by the Rockefeller Foundation finished in 2003. Research in Nepal is done by the MoH, medical schools, NGOs, EDPs, but there is no special research institute or School of Public Health. The Council made a bibliography of all medical and health-related research done in Nepal. It shows that a number of studies relevant for Macroeconomics and Health work seem to have been done. Unfortunately the overview does not contain abstracts, meaning that the original studies will have to be traced to asses their quality and relevance. A major survey, the Nepal Living Standard (Measurement) Survey, done by the Central Bureau of Statistics, will yield preliminary results in 2004. The consultant looked at the questionnaires used, in particular for the rural areas, and found that the survey will produce much relevant information, that can be used for targeting interventions to the poor. The Chairman of the Council, Dr. Sachey Kumar Pahari, thinks research should be done into why public policies and plans have not been implemented in Nepal. Capacity Technical capacity vis-à-vis essential interventions (diagnosis, treatment, counseling) The consultant was not able to assess this. Planning, management and monitoring capacity at different levels The planning capacity at the central MoH is weak, but the monitoring and data collection by the DOHS seems to be good quality and linked to policies and targets. The MDGs are monitored by a UN Team Group together with the Government. How the administrative and management capacity at the regional and district levels is, is not clear, but in all likelyhood needs to be upgraded. Financial management capacity at different levels The capacity of the HEFU in the MoH has substantially increased due to DFID support and capable leadership. Supervision arrangements MEH/Nepal/Situational Analysis, April 2004 38 Several policy documents mention the inadequacy of supervision by the regions to the district. While this may partly reflect lack of capacity, is it at present undoubtedly also due to the increased insecurity to travel. Research capacity Seems to be reasonable, but needs to be verified and specified for different areas of health research, in particular for health systems, financial and operational research. A quick search in Pubmed learned that there are a good number of publications in peer-reviewed international journals that have Nepalis as first author. Health education and promotion capacity Still to be assessed. Important, because the often mentioned ow awareness of the population on health and disease issues. Absorption capacity Due to the failing bureaucracy and constant transfers of staff, absorption capacity is less than it could be. MEH/Nepal/Situational Analysis, April 2004 39 Relationship poverty – ill health Just like in the economy at large, there are great inequalities in health status of people. The health gap between the poor and the rich remains. Health data are available by district, and some by gender and age. The breakdown by district will give some idea of (in)equity, because they can be linked to economic indicators for the districts. A Living Standard Measuring Survey was done in 1996 and is presently being done again by the Central Bureau of Statistics. This survey, the data of which will be available soon, has breakdowns by income quintiles. Tirtha Rana (WB Kathmandu) compiled some data on health indicators by income quintile from different sources19: It is clear that all indicators are strongly and gradually related to income. The greatest disparity between the poorest and richest quintile is for attended delivery: poor women have twice as many children as rich women, but the number of them that receive antenatal care is three times less and the number that have their deliveries professionally attended to is 11 times less. The number of children underweight is 5 times as high among the poorest quintile than among the richest one, while the number immunized is half that of rich children. Percentages of people in each income quintile for important health indicators Poorest 20% 2.9 5.2 6.4 9.1 Attended Delivery 21.5 34.7 35.6 43.5 ANC 32.4 34.6 40.8 51.0 Immunization coverage1 2 20.1 19.6 17.6 14.1 Severe malnutrition 6.2 5.0 4.7 4.4 TFR3 15.7 21.2 23.2 26.6. Use of modern contraceptives Richest 20% 33.7 66.5 71.1 4.4 2.9 44.9 1 % children under 2 receiving all vaccinations % children underweight 3 % births per 1000 women age 15-49 (this is a wrong definition – TFR is number of children the average woman gives birth to during her lifetime -MP) 2 The Nepal HSS shows the differences in infant and child mortality rates between urban and rural areas and between the three ecological regions. The children that live in the mountains clearly have the highest mortality, followed by those in the terai. The hilly regions and in those the urban areas have the lowest rates. Infant and Child Mortality by Area of Residence Area of Residence Infant Mortality Rate Urban 60.4 Rural 100.2 Mountains (North) 132.3 Hills (Middle) 85.5 Terai (jungle in the South) 104.3 Under 5 Mortality Rate 93.6 147.0 201.0 131.3 147.3 Source: Nepal Health Sector Strategy, draft June 2002 19 From Living Standard Measuring Survey, Demographic Health Survey (2001), HMIS MoH, UNDP Report 2001 MEH/Nepal/Situational Analysis, April 2004 40 In February 2002 The MoH organised a National Seminar on Health and Poverty Reduction, sponsored by WHO/SEARO, with reference to the CMH report. Bishwambher Pyakuryal, professor in Economics at the Tribhuvan, gave a presentation on the links between Education & Health and Poverty & Health in Nepal. His findings: 1. There is a clear relationship between the education level of the mother and major health indicators. When the mother’s educational level increases: Percentage receiving antenatal care increases Percentage receiving tetanus toxoid injections increases Percentage receiving skilled attendance at delivery increases Infant and child mortality rates decrease sharply Percentage of children fully immunized increases sharply Percentage of children underweight decreases Relevant in this context is that of the 8429 respondents in the 1996 Nepal Family Health Survey, on which the above results are based, 80% had no education, that is had never been to school. 2. There is a clear relationship between income poverty and health indicators. When the level of per capita consumption increases: Access to a health post increases (measured by time taken to reach the nearest health post) Health care seeking behaviour increases (measured by consultation of in particular a doctor) Percentage of fully immunised children increases Prevalence of chronic illness decreases 3. There is a clear relationship between poverty rate and health indicators (IMR, CMR and % of attended deliveries) for different areas of the country: Comparing urban and rural areas, mortality rates are much higher and percentage of attended deliveries much lower in rural areas, which are also poorer. Comparing Mountains, Hills and Terai, all three indicators are worse in the poorest areas, being the mountains. Comparing regions, indicators are worse in the Mid and Far West Development Regions, where poverty is also much higher than in the other regions. The disparities are big indicating that great health gains can be made. Focus should be on the Mid and Far West Development Regions, where 22% of the population live, who have the worst health indicators of the country. According to the information the consultant was able to collect, studies on catastrophic health care costs have not been done yet in Nepal. MEH/Nepal/Situational Analysis, April 2004 41 External Development Partners According to UNDP 2001 6% of external aid is spent on health, another 6% on water and 9% on education, 9% on rural development, while 28% is spent on energy and 19% on transportation. An overview of Technical Assistance by multilateral and bilateral agencies over all sectors in the Fiscal Year 2003/2004 is available from the MoF. The table includes titles of current projects and programmes, areas of Nepal in which the activities are being implemented, type of technical assistance and budget. A similar overview of all INGO-supported programmes for the Fiscal Year 2003/2004 is also available from the MoF. The health projects can be distilled from these overviews. See bibliography. The MoH Annual Report gives detailed overviews of support to the health sector by the main multilateral and bilateral partners, as well as international and national NGOs, and the achievements in a given year. Also the MoH website provides EDP information. Multilateral and bi-lateral donors The main multilateral agencies active in the health sector are UNICEF, WHO and UNFPA. Main bilateral donors are JICA/DRF, DFID, GTZ/KWF, USAID and the Swiss Development cooperation. The lack of governance, slow implementation of reforms and level of corruption was the main reason that the WB greatly reduced it’s IDA grants to Nepal in FY 2001/2002. For the health sector the IDA expenditure fell from 464 and 406 million Rupees in 2000 and 2001 to only 52 million Rupees in 2002. The PER gives an overview of donor expenditure in the health sector for 1999/2000-2001/2002. The share of EDP funds going through the Red Book of the MoF has declined over the years from 44% to only 10%. At present 90% of EDP funds for health go directly to the Ministry of Health or are self-executed by partners. The donors have regular meetings, chaired by the WHO Representative. As mentioned above all support is still organised in project/programme form, in some cases by several donors jointly. Most donors are however not (yet) in favour of pooling funds in a sector-wide approach, although all of them now subscribe to the jointly developed Health Sector Strategy and its Implementation Plan. Given the substantial differences between this strategy and plan on the one hand and the Tenth Plan, to which the MoH is nationally committed, on the other hand, it is not clear how the MoH will seek to reconcile the two paths. International NGOs The main INGOs active in health are United Mission to Nepal (UMN), Save the Children UK and US, Marie Stopes Inernational (MSI), International Nepal Fellowship (INF), Netherlands Leprosy Relief (NLR), The Asia Foundation Nepal (TAF) and the Britain Nepal Medical Trust (BNMT). National NGOs The main national NGOs involved in health are the Family Planning Association of Nepal (FPAN), Aamaa Milan Kendra (Mother’s Club), Nepal Contraceptive Retail Sales Company (CRS), the Nepal Red Cross Society (NRCS) and the National Vitamin A programme. MEH/Nepal/Situational Analysis, April 2004 42 The EDPs are active in the following areas: Safe motherhood, RH and FP (UNFPA, UNICEF, DFID, USAID, GTZ, TAF, Save US, MSI, Aamaa, FPAN, CRS) Child Health (EPI, CDD, ARI, IMCI, Vit A & Iron Supplementation, salt iodisation and deworming) (UNICEF, JICA, Save US, Nat Vit A progr) Priority disease programmes (TB, polio, leprosy, HIV/AIDS/STDs, malaria, kala-azar, Japanese encephalitis) (WHO, USAID, DFID, JICA, UMN, Save US, Save UK, INF, NLR) Provision of community health care or PHC (UMN, BNMT, NRCS) Provision of health services in conflict affected areas (DFID, Save UK, NRCS) Provision of hospital services (UMN, NRCS) Nursing (UMN) School and community health (JICA) Health education, information and communication (UNFPA, Physical assets and Drug management (GTZ) Construction, extension and rehabilitation of facilities (KfW) Procurement of essential drugs, equipment, contraceptives, vaccines (KfW, JICA) Integration of health in general development and poverty reduction programmes (WHO) Human Resource Development (WHO, GTZ) Strengthening District Health Systems (WHO, GTZ, DFID, SDC, INF) Health financing (DFID) Tobacco control (WHO, JICA) WHO is also involved in non-priority areas such as mental health, non-communicable diseases, blindness, deafness, oral health, disaster preparedness, blood safety, laboratory technology, environmental protection etc. UMN is also active in some of these areas. The NRCS is responsible for the blood safety in Nepal and runs 51 blood transfusion centres throughout the country. The organisation is becoming more involved in providing some health care services, operates an ambulance service in 43 districts. They have 27 warehouses around the country. It is further worth mentioning that the NRCS has a youth volunteer programme, in which almost 800,000 children and young adults participate. They are involved in First Aid, HIV/AIDS/RH information and water & sanitation programmes. Given their huge national network, reaching into very remote areas, they could be an interesting partner in providing the EHCS package to remote and poor populations. Capacity building and developing/strengthening management, financial and information systems (including disease surveillance) is part of most programmes/projects. Most donors are involved in supporting development of policies and strategic plans, decentralisation, health sector reform etc. Some projects are nationwide, others focus on a number of districts. The EDPs that support programmes in certain districts, usually support a wide range of activities, including maternal and child health, RH, infectious diseases, iec, drug schemes etc. With a few exceptions there was little mention of research activities. An inventory needs to be made which studies have been done by EDPs that are relevant for the macroeconomic and MEH/Nepal/Situational Analysis, April 2004 43 health agenda. It was agreed that this would be done as part of the Plan of Action for the first phase of Macroeconomics and Health work. The consultant did not receive information about mechanisms by which NGO coordination takes place, either among themselves or with the MoH. In how far the EDPs work with poor/remote/vulnerable populations should be assessed by comparing their district work with economic indicators and studying their programmes in detail. This can be done as part of the planning phase of the macroeconomic and health work. Latest news Nepali Times 16-22 April 2004 The pre-consultative meetings of the Nepal Development Forum (NDF) have brought heightened donor concern about Nepal’s parliamentary crisis and the conflict to the fore. Most donors have made restoration of democracy and conflict resolution conditionalities to future aid, with some even including respect for human rights by the security forces as a pre-requisite. Government officials admit the crises have made it difficult to ask for more aid, but say they need to know the level of program, sectoral and project support to plan future activities. Some bilateral donors have placed their programs under the UN umbrella while others have started work without associating themselves with government networks to avoid Maoist confrontation. Some donors have argued again that service delivery should be attempted in Maoist-held areas, even if it means working with the rebels. But by far the major disagreement between the government and donors is over making specific aid commitments. Government officials want donors to commit before the main conference on 5-6 May. Donors have been saying that there has to be adequate discussion on aid policy first, while the government has been insisting that they ease their conditions. MEH/Nepal/Situational Analysis, April 2004 44 Macroeconomics and Health Commitment Commitment to poverty reduction The Government of Nepal is very committed to poverty reduction, as is evident from all major policy and planning documents related to development. The PRSP20 mentions that a Nepal Dalit Commission and a National Academy for the upliftment of indigenous people will be created. A Poverty Alleviation Fund has already been created to strengthen local ownership and coordinate special programmes by line ministries at the local level and to involve NGOs and CBOs. The NPC has furthermore created a central monitoring unit and poverty mapping will also be initiated. A key question of course is whether finance follows this political commitment. For the health sector the PER showed that some trends in expenditures over the last 3 years actually go against the agreements or intentions (more detail under Health Financing above): The share of funding going to the rural areas, to Priority 1 programmes and to RH have all decreased. This shows that agreements on policies without calculating the budgetary consequences, and especially agreeing on disinvestments to free up resources for the priority investments, is not good enough. It also shows that it might not be politically feasible to really transfer large amounts of resources from one programme to another. In the CMH Report this was taken into account, when the recommendation was made that more funds were needed, to finance additional investment for scaling up essential services for the poor, keeping the present nonessential services at the same level. Commitment to Macroeconomics and Health Already in June 1992 Dr. Suniti Acharya from the MoH and Dr. Bal Gopal Baidya from the National Planning Commission attended the International Conference on Macroeconomics and Health in countries in greatest need, held at WHO Geneva. Dr. Acharya (now WR in Bangladesh) co-authored a chapter in the proceedings21. Nepal also attended both recent WHO consultations on Macroeconomics and Health. Mr Mahendra Nath Aryal, Secretary MoH, Mr Madhav Prasad Ghimire, Joint Secretary MoF and Mr Ram Krishna Tiwari, Joint Secretary NPC attended the first consultation in June 2002, while, according to the official participants list the following persons attended the second consultation in October 2003: Mr Kamal Thapa, Minister of Health, Ministry of Health, Kathmandu Mr Bhoj Raj Ghimire, Member-Secretary, National Planning Commission, His Majesty’s Government of Nepal, Kathmandu Mr Bijay Raj Bhattarai, Secretary, Ministry of Health, Kathmandu Mr Surendra Mani Tripathi, Under Secretary, Ministry of Finance, Kathmandu Dr H.N. Acharya, Member of the Executive Board of the World Health Organization and Chief Public Health Administrator, Ministry of Health, Kathmandu Mr Gyan Chandra Acharya, Ambassador, Permanent Mission of Nepal to the United Nations Office and other International Organisations at Geneva Dr B. Datt Chataut, Director-General, Department of Health Services, Kathmandu Nepal has submitted a thoughtful Plan of Action for the preparatory phase to WHO. 20 21 PRSP: pages 57 and 58 Acharya et al. 1993 MEH/Nepal/Situational Analysis, April 2004 45 Commitment of external development partners The consultant gave a short presentation on the key messages and strategies of WHO’s Macroeconomics and Health agenda during a donor meeting on 30 December 2003. The plans for the preparatory phase were also briefly indicated. The biggest concern of the donors is how the Macroeconomics and Health work will fit into existing strategies and plans. The consultant stressed that the work would not duplicate any ongoing activities, but complement them. According to GTZ there is more suspicion than representatives of donors showed during the meeting, so this point will need continuous attention. Intense cooperation with the EDPs during the planning phase is warranted. Institutional arrangements Under the National Commission on Sustainable Development, chaired by the Prime Minister, a Sub-Commission on Macroeconomics and Health (SCMH) was formed, co-chaired by the Ministers of Health and Finance. The following persons serve on the SCMH: Member of National Planning Commission responsible for Health Member of National Planning Commission responsible for Finance, Commerce and Industry Secretary, Ministry of Finance Secretary, National Planning Commission Secretary, Ministry of Health (as member secretary of the SCMH) A woman representative from NGO having significant contribution to macroeconomics and health ( Mrs. Meena Acharya) Health economist ( Dr. Badri Raj Pandey ) Chief of Policy, Planning and International Cooperation Division, Ministry of Health During its first meeting the SCMH has formed 3 people working committee consisting of one representative each from MoH (Dr. Benu Bahadur Karki), MoF (Mr. Lal Shankar Ghimire) and NPC (Mr. Ram Krishna Tiwari). Together with WHO this committee has identified a number of issues to be addressed in relation to Macroeconomics and Health work and made a Work Plan for 2003-2004, which contains actions to be taken during the preparatory phase, but also 2-3 actions that would be part of the planning phase. The Work Plan with a budget of $50,000 was submitted to WHO in September 2003. The consultant met with the working committee on 29 December 2003 and some adaptations in the Work Plan (=Plan of Action for preparatory Phase) and budget were agreed. This adapted plan, albeit with a lower budget still, has in the mean time been accepted by WHO. The commitment of Nepal to macroeconomics and health is threatened by the departure of Dr. B.B. Karki22 and the frequent change in people in key positions. The WR Office is trying to minimise this threath by constantly briefing new staff and involving them in meetings. Even so it is likely that any process, including macroeconomics and health activities, will take longer in Nepal due to the instability of the bureaucracy. 22 Dr. Karki, who has been the leading force on Macroeconomics and Health so far, has left the MoH and Nepal. Most likely, his direct chef, the Chief Specialist Dr. Bishnu Pandit, will become the focal point for Macroeconomics and Health in the MoH. MEH/Nepal/Situational Analysis, April 2004 46 CMH calculations for Nepal The Commission on Macroeconomics and Health calculated that scaling up a package of 49 essential interventions in 5 priority areas (see page 174 of CMH Report) to target levels at the close-to-client (CTC) level would cost an additional $11 per person per year on average for least-developed countries by 2007 and an additional $16 by 2015. But this is not enough, because in order to scale up services at the CTC level, system expansion is also needed. The CMH therefore also estimated the additional costs for requirements for the process of scaling up. This includes improving management above the CTC level, improving absorptive capacity, improve the quality of current services, and increase the number of staff as well as their salaries. These costs were estimated to be another $11 and $16 per capita for the least developed countries on average. The total additional costs would therefore be $22 per capita for 2007 and $32 for 2015. These costs are over and above the baseline expenditure, which was estimated to be $13 per capita in 2002. The total health expenditure required would therefore be around $34 per person per year by 2007 and >$40 by 2015. The CMH thinks that the least developed countries (including Nepal) should be able to domestically mobilise around $15 per person per year by 2007 and $20 by 2015 (around 5% of per capita income). The EDPs would have to close the gap of $19 per capita per year in 2007 and $21 in 201523. Efforts are underway in Nepal to estimate the total health expenditure from all sources. The results of the first round of NHA calculations will be available in March/April 2004. According to preliminary estimates Nepal’s total health expenditure is around $15 at present 24 Roughly 1/3rd of this amount is public expenditure, including HMG of Nepal budget and EDP funds, and the other 2/3rd is private out of pocket expenditure. This means that total health expenditure would have to more than double by 2007 in order to provide an essential package to the whole population, as calculated by the CMH. On the basis of a 4-5% growth scenario the estimated income per capita in 2007 would be around $300 (at present $ value). If we agree that it is reasonable to expect 5% of per capita income to go to health care costs, this would be $15 per person per year (again at present value), that would have to be raised domestically. At present Nepal’s domestic spending is around $13 p/c (only $3 government and $10 OOP). The EDPs spend just over $2 per capita, If we assume that: Nepal indeed needs an additional $21 per person (as calculated by the CMH for the average least developed country) per year to finance a scaled up EHCS package non-EHCS are not expanded donor investment in the health sector would need to increase very substantially with $17 per capita per person per year ($34-$15-$2=$17), being an eight-fold increase of present investment. The EHCS package established by HMG of Nepal (11 areas of interventions) is being costed at the moment by a consultant of the WB (unit costs, zero-based budgeting, for limited scaling up). The results will be available in April 2004. It is as yet not known whether upgrading of the system, facilities, personnel etc. is included in the costing. It is further not exactly known how much of the present domestic expenditures is actually spend on the EHCS. Part of of this amount, especially the OOP part spent in the private sector, might be spent on non-effective 23 24 US$ 2002 (executive summary CMH report page 11 and Tables A2.4, A2.5 and A2.6 in Appendix 2) Oral communication Mr. Tanka Mani Sharma, Chief HEFU, MoH. MEH/Nepal/Situational Analysis, April 2004 47 interventions. Most of the EDP contribution likely does go to EHCS and related system development costs. As the impact of scaling up EHCS within the Macroeconomics and Health framework is expected to come in particular from reaching the poor with the EHCS, we will also need to assess how much of present expenditures actually benefit the poor. It is also very likely that most of the $10 OOP average per capita expenditures on health are paid by the middle and higher income classes. The poor will be able to spend less, and will need to be subsidised, by large-scale pooling of funds and risks between the rich and the poor, an income related contribution system and/or through direct subsidisation of the poor by the government. Therefore it is very likely that the part of HMG of Nepal’s share in the financing of health care will have to be substantially increased. With how much would depend on the ability and willingness of the poor to contribute, on the willingness of the middle-and higher income groups to subsidise the poor through a progressive contribution system, and on the feasibility to set up operational pre-paid schemes without the risk of adverse selection. Opportunities for scaling up/reaching the poor There are many achievements and developments in Nepal that forebode well on the possibility to scale up essential health interventions and specifically reach the poor: Strong pro-poor policies and plans are in place as well as commitment to the macroeconomics and health agenda. Nepal has a well-developed and in principle functional administrative structure, and a good coverage of public health facilities. Health care workers earn relatively well (as compared with the average per capita income and with health worder salaries in other low-income countries) A decentralisation/devolution process is well under way, which will mean more local ownership and possibilities to target interventions to local needs and vulnerable groups, if local political commitment to poverty reduction is present and health is seen as an important issue, both in its own right and as a vehicle for development. Essential Health Care Services have been identified and further prioritised. The unit cost of some EHCS are being calculated. A first PER of the health sector has been made and a system of NHA is being set up, which will further improve availability of data on financial flows, necessary to monitor macroeconomic and health work. New community financing schemes will be piloted in 2004. Results of a new Living Standard Survey will soon be available, including information on health facilities, personnel and health care seeking behaviour. It will be possible to link the data to income and poverty statistics at district level. This will be a very powerful data source for detailed planning, necessary to reach the poor with essential services. The HMIS is excellent and the DoHS produces very useful data on key indicators per district, which can also be used to monitor progress towards targets. Donors are willing to support Nepal and have also indicated their willingness to increase their support. Non-financial constraints to scaling up/reaching the poor A considerable number of non-financial constraints are described in the documents mentioned above under Policies, strategies and plans. MEH/Nepal/Situational Analysis, April 2004 48 Geographical constraints exist because is Nepal is very fragmented, hampering transport and communication. Because of this there are relatively many remote areas in this relatively small country. And it is in those areas that most of the poor live. Institutional constraints include a lack of planning and coordination capacity within the Ministry of Health, lack of clarity of roles and responsibilities between the MoH and the Directorate of Health Services, the need to strengthen intersectoral collaboration, and the need to integrate several disease based programmes. The HMIS does not allow disaggregation of key indicators by income or poverty status. Absorptive capacity is weak; utilisation of funds has been lower than in other ministries, especially for the development budget. Supply side constraints include a lack of staff in rural and remote areas, weak supervision of service delivery, a need for quality assurance, but also for improving attitudes of staff. Facilities need to be upgraded and supply of drugs and medical supplies ensured. Demand side constraints include lack of awareness among the public about health and disease and inability to pay the user fees, while exemption schemes do not work well. Supply and demand side constraints together lead to a low utilisation of the public facilities, especially by the poor. Partnership constraints include the lack of mechanisms to regulate the private sector and probably lack of coordination with international and national NGOs. A particular issue is collaboration between HMGN and the EDPs. This has improved over recent years but there is still considerable work to do in increasing coordination of donor resources within a national strategy. In particular not all EDP expenditure is notified to the Government. Political constraints include the present political instability, due to the Maoist insurgency, and the frequent change of key staff at all levels in the MoH (and elsewhere in the public service). The implications of the insurgency on the delivery of health services are increasing, with reports of destruction of SHPs, blockades of essential drugs, difficulties in supervision and monitoring visits by regional and district health officers, disruption of the cold chain etc. The conflict makes it even more difficult te find staff willing to serve in the areas under control of the Maoist forces. The frequent changes in the civil service lead to lack of institutional memory and continuity in policy and planning. But also to lack of proper skills for any particular job, because by the time an officer has acquired the knowledge for a specific job is becoming productive, s/he is being transferred again. While lack of good governance, corruption and slow implementation of agreed reforms were still a reason for the WB to minimise its financial contributions to Nepal in 2002, according to the WB CAS Progress Report made end of 2002, the government has become increasingly more serious about reform implementation (under the Immediate Action Plan – IAP). Financial constraints to scaling up/reaching the poor Sources Nepal is the poorest country on the Eurasian continent with 38% of the population living below the poverty line and a per capita income of just $250 per annum. People do not have enough money to buy health services. HMG of Nepal has problems raising enough revenues. The government does not have enough money to invest enough in basic services to make an impact on health status. MEH/Nepal/Situational Analysis, April 2004 49 Even so, compared to other low-income countries, HMG of Nepal spends very little on health: the national government spends only 193.5 million Rupees on health, being $2.65 or 1.06% of GDP. HMG of Nepal also spends relatively little on health as the health budget 2003/2004 is only 1/3rd of the education budget. The health budget has increased less than the general budget over the last years. The domestic share of the national public health budget has decreased with 4.5% in real terms since 2001/2002. People pay 3-4 times more out-of-pocket for health than the government does. Health services are mostly financed from direct taxes and user fees. As these are regressive, the poor pay relatively more for health services than the rich and often get less. Pre-paid plans hardly exist. Expenditures Expenditures have not followed policies: Spending on PHC slightly decreased over the last years Spending on health services in the rural areas decreased in favour of urban areas Spending on priority-1 programmes decreased, while those on priority-3 programmes increased Spending on RH drasticially decreased and those on child diseases is very low, compared to the burden of disease MEH/Nepal/Situational Analysis, April 2004 50 Recommendations and conclusions 1. Nepal has good pro-poor policies and plans in place and quite some work relevant to Macroeconomics and Health is ongoing. However, some of the major constraints can only be solved politically. The security situation in particular seems to be getting worse and might seriously hamper necessary work, both in the planning and implementation phase. 2. It is needed that objectives and targets/indicators of NHSP-IP and those in the Tenth Plan and in the PRSP are compared and differences discussed. It would be highly desirable that all three sets of objectives, outputs and targets would be streamlined. It cannot be that the MoH has to work with three pretty different plans. 3. As usual, targets in the HSS and the NHSP-IP, as well as in the Tenth Plan and the PRSP are national averages. In the context of the development objectives it would be more meaningful to have specific targets and indicators for the vulnerable, women, children, rural populations and specifically for the poor. To reflect this the health management information system would need to be adapted. 4. Rather than national solutions we might have to look for local solutions in this fragmented, inaccessible country. This would also align well with the devolution process that is gaining momentum. Therefore the consultant has recommended to produce District Health and Poverty Profiles. In order to speed up work, this was included in the Plan of Action for the preparatory phase. The NHRC has been requested to implement this activity. These profiles will subsequently serve as a basis for adapting the existing District health Plans into District Health and Poverty Plans during the planning phase. 5. Focus should be on interventions that address the burden of disease experienced by the poor and on actually reaching the poor with these interventions, ensuring that health and other systems serve them more effectively. To this end a number of options should be studied in detail in each district as part of the district profile, such as: Analysis of the burden of disease among the poor, disadvantaged and marginalised Utilisation of public services and barriers to utilisation Given the big impact of clean water and sanitation services on the burden of disease of the poor, the availability of these should be included in the district profiles Linking up with existing public or private organisations that are on the ground/have network, such as the Nepal Red Cross, which has an extensive network, but also organisations in other sectors, such as the Annapurna Conservation Area Project and the Hills Leasehold Forestry and Forage Development Project Operating outreach/mobile services Organise transport to health facilities Telemedicine Linking up with microcredit schemes for community financing Linking up with user groups, such as farmers group, water user association, forestry user group (more than 10,000 all over the country), credit group, women in development group etc. 6. The methodology of the costing of the EHCS done by the WB recently needs to be studied in more detail in order to ensure that all costs of system expansion and the process of scaling up are included, also those at the higher levels. Final costing should be based on real local costs, not literature based. MEH/Nepal/Situational Analysis, April 2004 51 7. The PER calculated the expenditure on priority-1 programmes, probably by ministerial budget lines for programmes and centres. But these do not necessarily coincide with the EHCS, as these are defined by activities and the priority programmes probably also undertake activities that would not be included in the EHCS. Moreover the EHCS have been further prioritised since 2001/2002. There is a need to find out how the P-1 programmes relate to the EHCS and how much of present expenditure is used to finance EHCS. 8. HMG of Nepal should consider doubling the health budget by 2007, as it spends very little on health, both compared with other social sectors in Nepal and compared with other LICs. The present trend in resource allocation goes against the agreed policies. Resource allocation should improve and follow priorities. 9. Donors should also consider to substantially increase their health budget. 10. The full increase (of both HMG and donors) should be used for scaling up EHCS for the poor. 11. Because of the regressive forms of financing of the health sector and low utilisation by the poor, the urban and wealthier people pay relatively less and get more benefits, whereas the poor pay more and get less benefits. People in Nepal spend 3-4 times as much OOP as HMG spends on health. A plan to channel these OOP contributions into pre-paid plans should be developed. The handing over of HPs and SHPs to VDCs offer opportunities for CHI to be introduced. The MoH is planning a few pilot projects. The evaluation of the CHI pilots could be included in the Macroeconomics and Health planning phase proposal. 12. Research should be focused on generating answers to questions and options that will facilate pro-poor strategic planning. MEH/Nepal/Situational Analysis, April 2004 52 Annexes MEH/Nepal/Situational Analysis, April 2004 53 Annex 1 Policies and Plans 1. NATIONAL HEALTH POLICY 1991 The National Health Policy was adopted in 1991 (FY 2048 BS) to bring about improvement in the health conditions of the people of Nepal. The primary objective of the National Health Policy is to extend the primary health care system to the rural population so that they benefit from modern medical facilities and trained health care providers. The National Health Policy addresses the following areas: 1. Preventive Health Services Priority is given to programmes that directly help reduce infant and child mortality rates. Services are to be provided in an integrated manner throughout the health system to sub health posts at the local level. 2. Promotive Health Services The programmes that enable people to live healthy lives will be given priority. 3. Curative Health Services Curative health services will be made available at all health institutions-central, regional, zonal and district hospitals; primary health care centres (PHCC), health posts (HP), and sub health posts (SHP); and, at health institutions at all levels of the healthcare system. Hospital expansion will be based on population density and patient loads. Mobile teams will be organised to provide specialist services to remote areas. A referral system will be developed to direct the rural population to well-equipped institutions. 4. Basic Primary Health Services Sub Health Posts will be established in phased manner in all Village Development Committees (VDC). One Health Post in 205 electoral constituencies will be upgraded in a gradual manner and converted to a Primary Health Care Centre. 5. Ayurvedic and other Traditional Health Services The ayurvedic system will be developed and other traditional health systems (such as Unani, homeopathy, and naturopathy) will be encouraged. 6. Organisation and Management Improvements will be made in the organisation and management of health facilities at the central, regional and district levels. This will include the integration of the district hospitals and the public health offices into District Health Offices. 7. Community Participation in Health Services Community participation will be sought at all levels of healthcare through the participation of female community health volunteers (FCHV), traditional birth attendants (TBA) and leaders of various local social organisations. VDCs will provide sites for the location of SHPs. 8. Human Resources for Health Development (HRH) Technically competent human resources will be developed for all health facilities. Training centres and academic institutions will be strengthened. 9. Resource Mobilisation in Health Services National and international resources will be mobilised and alternative concepts (such as health insurance, user charges, and revolving drug schemes) will be explored. 10. Private, Non-Governmental Health Services and Inter-sectoral Co-ordination The Ministry of Health will co-ordinate activities with the private sector, non-governmental organisations (NGOs), and non-health sectors of HMG. The private sector and NGOs will be encouraged to provide health services. 11. Decentralisation and Regionalisation Decentralisation and regionalisation will be strengthened; peripheral units will be made more autonomous. District Health Offices (DHO) will have a prominent role in the planning and management of curative and promotive health services from district to village levels. 12. Blood Transfusion Services The Nepal Red Cross Society will be authorised to conduct all programmes related to blood transfusion. The practice of buying, selling, and depositing blood will be prohibited. 13. Drug Supply Improvements will be made in the supplies of drugs by increasing domestic production and upgrading the quality of essential drugs through effective implementation of the National Drug Policy. 14. Health Research Health research will be encouraged for better management of health services. MEH/Nepal/Situational Analysis, April 2004 54 2. SECOND LONG TERM HEALTH PLAN, 1997-2017 The Ministry of Health of His Majesty's Government of Nepal developed a 20-year Second Long-Term Health Plan (SLTHP) for FY 2054-74 (1997-2017). The aim of the SLTHP is to guide health sector development in the improvement of the health of the population, particularly those whose health needs are not often met. The SLTHP addresses disparities in healthcare, assuring gender sensitivity and equitable community access to quality healthcare services. The aims of the SLTHP are to provide a guiding framework to build successive periodic and annual health plans that improve the health status of the population; to develop appropriate strategies, programmes, and action plans that reflect national health priorities that are affordable and consistent with available resources; and to establish co-ordination among public, private and NGO sectors and development partners. The SLTHP vision is a healthcare system with equitable access and quality services in both rural and urban areas. The system would encompass the concepts of sustainability, full community participation, decentralisation, gender sensitivity, effective and efficient management, and private and NGO participation. 2.1 OBJECTIVES The objectives of the SLTHP are as follows: To improve the health status of the population of the most vulnerable groups, particularly those whose health needs often are not met-women and children, the rural population, the poor, the underprivileged, and the marginalized population. To extend to all districts cost-effective public health measures and essential curative services for the appropriate treatment of common diseases and injuries. To provide the appropriate numbers, distribution and types of technically competent and socially responsible health personnel for quality healthcare throughout the country, particularly in under-served areas. To improve the management and organisation of the public health sector and to increase the efficiency and effectiveness of the healthcare system. To develop appropriate roles for NGOs, and the public and private sectors in providing and financing health services. To improve inter-and intra-sectoral co-ordination and to provide the necessary conditions and support for effective decentralisation with full community participation. 2.2 TARGETS The targets of the SLTHP are as follows: To reduce the infant mortality rate to 34.4 per thousand live births; To reduce the under-five mortality rate to 62.5 per thousand; To reduce the total fertility rate to 3.05; To increase life expectancy to 68.7 years; To reduce the crude birth rate to 26.6 per thousand; To reduce the crude death rate to 6 per thousand; To reduce the maternal mortality rate to 250 per hundred thousand births; To increase the contraceptive prevalence rate to 58.2 percent; To increase the percentage of deliveries attended by trained personnel to 95%; MEH/Nepal/Situational Analysis, April 2004 55 To increase the percentage of pregnant women attending a minimum of four antenatal visits to 80%; To reduce the percentage of iron-deficiency anaemia among pregnant women to 15%; To increase the percentage of women of child-bearing age (15-44) who receive tetanus toxoid (TT2) to 90%; To decrease the percentage of newborns weighing less than 2500 grams to 12%; To have essential healthcare services (EHCS) in the districts available to 90% of the population living within 30 minutes' travel time of facilities; To have essential drugs available at 100% of facilities; To equip 100% of facilities with full staff to deliver essential health care services; and To increase total health expenditures to 10% of total government expenditures. 3. STRATEGIC ANALYSIS In October-November 1999 the Ministry of Health, in collaboration with external development partners (EDP), conducted a strategic analysis of the health sector with a view to developing an effective planning approach. The aim of the strategic analysis was to initiate a process for analytical decision-making in planning. During the analysis it became apparent that despite policy commitment, equity in access to healthcare remained elusive. Of further concern was that compared with investments achievements were lower than expected. The following issues were identified: weak management of public sector health facilities and institutions; inadequate compliance with existing guidelines and quality of care protocols; lack of clear roles and responsibilities for health authorities (central and district level) regarding decentralisation; the absence of an effective system to ensure quality and fair pricing of private sector services; and the lack of policies for human resource development and management. The outcome of the strategic analysis was the Medium Term Strategic Plan (MTSP), which was formulated to provide operational support for the SLTHP. More specifically, the MTSP provides a strategic framework for developing the Tenth Five Year Health Plan (2002-2007). MEH/Nepal/Situational Analysis, April 2004 56 4. MEDIUM TERM STRATEGIC PLAN (MTSP) Aims To develop an effective health system for the provision of affordable and accessible Essential Health Care Services (EHCS) To promote a public-privateNGO partnership for the provision of healthcare To decentralise the health system and ensure participatory approaches at all levels Outputs Delivery of prioritised Essential Health Care Services (EHCS) elements according to National Standard Guidelines Provision of services beyond EHCS, ensuring a safety net for poor and vulnerable groups Improved access to and utilisation of health services by the vulnerable population (poor, disadvantaged, women and children) Defined and strengthened roles of public-private-NGO providers in the provision of health services A regulatory framework for the private sector An effective partnership management system Developed and implemented financial mechanisms for public-private-NGO involvement Enhanced participatory planning and management capabilities at all levels in the spirit of devolution ensuring gender balance Functional health management committees (HMCs) at all levels including the central level To improve the quality of health care provided through the public/private/NGO partnership by total quality management (TQM) of human, financial, and physical resources. Defined and operational roles and responsibilities for all stakeholders Mobilised communities with lifestyles developed to increase service utilisation and to see the practice these lifestyles at home An adequate and appropriate mix of HRH developed and deployed at all levels and systems Quality assurance mechanisms in place in public/private/NGO sectors for provision of quality services Assurance of availability and proper utilisation of financial resources Availability and use of adequate and reliable information for management decision making Development and implementation of a national healthcare technology strategy Supplies of drugs and medical consumables of approved quality available throughout the year MEH/Nepal/Situational Analysis, April 2004 57 5. DELIVERY OF ESSENTIAL HEALTH CARE SERVICES The Second Long Term Health Plan indicated that priority be given to health promotion and prevention activities based on Primary Health Care principles. It identified Essential Health Care Services (EHCS) that address the most essential health needs of the population and that are highly cost-effective. EHCS are priority public health measures and are essential clinical and curative services for the appropriate treatment of common diseases. The EHCS for Ayurveda and other traditional systems of medicines are defined separately. Essential Care Services for the Modern System of Medicine * Main Interventions* Health Problems Addressed Appropriate treatment of common diseases and injuries Common Diseases and injuries Reproductive health Maternal and Peri-natal The expanded programme on immunisation (EPI) and Hepatitis B Vaccine Diphtheria, Pertusis, TB, Measles, Polio, Neonatal Tetanus, Hepatitis B Condom promotion and distribution STD/HIV, Hepatitis B, Cervical Cancer Leprosy control Leprosy Tuberculosis control Tuberculosis Integrated Management of Childhood Illness (IMCI) Diarrhoeal Disease, Acute Respiratory Infection (ARI), Protein Energy Malnutrition (PEM) Nutritional supplementation, enrichment, nutrition education and rehabilitation PEM, Iodine Deficiency Disorders, Vitamin A Deficiency, Anaemia, Cardiovascular Disease Prevention, Diabetes, Rickets, Perinantal Mortality, Maternal Morbidity, Diarrhoeal Disease, ARI Prevention and control of blindness Cataracts, Glaucoma, Pterygium, Refractive Error, and other Preventable Eye Infections Environmental sanitation Diarrhoeal Disease, Acute Respiratory Infection, Intestinal Helminthes, Vector Borne Diseases, Malnutrition School health services Diarrhoeal Disease, Helminthes, Oral Health, HIV, STDs, Malaria, Eye and Hearing Problems, Substance Abuse, Basic Trauma Care Vector borne disease control Malaria, Leishmaniasis, Japanese Encephalitis Oral health services Oral Health Prevention of deafness Hearing Problems Substance abuse, including tobacco and alcohol control Cancers, Chronic Respiratory Disease, Traffic Accidents Mental health services Mental Health Problems Accident prevention and rehabilitation Post Trauma Disabilities Community-based rehabilitation Leprosy, Congenital Disabilities, Post Trauma Disabilities, Blindness Occupational health Chronic Respiratory Disease, Accident, Cancers, Eye and Skin Diseases, Hearing Loss Emergency preparedness and management Natural and Man-made disasters. Main Interventions are listed in priority order MEH/Nepal/Situational Analysis, April 2004 58 Annex 2 Tenth Plan Chapter 24 – Health MEH/Nepal/Situational Analysis, April 2004 59 Annex 3 – 2007) Nepal Health Sector Programme – Implementation Plan (2003 Output 1: Prioritised EHCS 1. costing of and resources allocation for EHCS 2. redefine institutional arrangements for delivering EHCS 3. develop systems for priority access for poor and vulnerable groups 4. strengthen outpatient services 5. additional behaviour change and communication (BCC) activities Output 2: Decentralised health management 1. introduce local management of sub-health posts 2. create hospital autonomy and initiate resource mobilisation Output 3: Private and NGO sector developed 1. formally establish committees and workgroups for specific programme areas to coordinate the work of government, donor and I/NGO groups 2. establish district level health co-coordinating committees 3. update inventory of existing private/NGO/public involved in health sector, by district 4. define an appropriate public/private/NGO mix for each district 5. set quality standards and regulatroy emchanisms for private and NGO delivery Output 4: Sector management 1. strengthen joint MoH/donor annual planning, programming, budgeting and monitoring cycle 2. strengthen ongoing MoH/donor programmatic collaboration 3. strengthen sector management at the central level 4. strengthen regional and district management 5. capacity building at central and district levels 6. systematic assessment of institutional and organisational arrangements 7. redefinition of roles throughout the health system Output 5: Financing and resource allocation 1. identification of health sector priorities and reallocation of resources to priorities services 2. alternative financing arrangements, such as community health insurance, explored 3. MoH to develop national guidelines for user fee practices and other payments in public facilities 4. drug financing mechanisms strengthened to support increased and equitable availability of essential drugs Output 6: management of physical assets 1. product selection and quality improved 2. commodity distribution improved 3. drug financing mechanisms strengthened 4. national drug policy better implemented 5. logistics management information sytsem (LMIS) strengthened 6. disaster relief commodities management strengthened 7. quality and safety policies and systems to be established Output 7: Human resource development 1. the MoH will reform its HRD unit and locate it in an appropriate place 2. the MoH will improve its personnel management 3. in-service training coordination and quality will be improved 4. new training for identified needs 5. better coordination between the MoE, MoH and CTEVT for pre-service education Output 8: Integrated MIS and QA policy 1. develop and establish integrated MIS 2. establish and implement QA Policy MEH/Nepal/Situational Analysis, April 2004 60 Annex 4 Health and Financing paragraphs in the PRSP Health paragraphs in the PRSP (page 54/55) 145 The health sector is of critical importance for human development, improving living standards in rural areas and for mainstreaming marginalized groups and communities. Despite significant progress in recent years, service delivery in the health sector remains weak. Although an extensive network of primary healthcare centers has been constructed nationwide, it has not been functioning well in many rural areas due to lack of trained staff, drugs and medicines, etc. The sector's overall performance has suffered due to inadequate funding for essential recurrent expenditures, misallocation of resources and limited capacity for supervision and, for co-ordination of the activities of other agencies providing health care services. 146 To address the health sector needs, the government formulated a Health Sector Strategy in August 2002, which provides a coherent strategic framework to involve all the stakeholders. The key sector objectives are: (i) Extending essential health care services to all, with special emphasis on the poorer population living in rural areas; (ii) Management of the growing population by enhancing the accessibility of rural population to family planning services and expanding maternal and child health services; and (iii) Ensuring effective control of communicable diseases, such as Malaria, and Tuberculosis, as well as HIV/AIDS. 147 The Tenth Plan has adopted a number of strategies to achieve these objectives: (i) Expansion of primary health centers and district hospitals, and strengthening out-patient services in hospitals; (ii) Development and retention of trained health personnel in rural areas; (iii) Increased supply of essential drugs and vaccines; (iv) Improved delivery of health services, publicly, through decentralized management/delivery, through increased participation of the private sector, INGOs and NGOs, or through public -private partnerships; (v) Improved regulatory mechanisms to ensure the quality and accessibility of health services; and (vi) improving human resource development and management and health care financing. 148 The major policies and programs to implement these strategies include, among others, the following: As noted, primary health centers and outpatient facilities in hospitals will be expanded. In order to mainstream the marginalized groups and regions, efforts will be made to ensure access to a facility within one hour's walk to all, and to initiate special programs in the Mid and Far Western regions. Given the inadequate staffing and quality of health facilities in rural areas, the government will make recruitment and transfer process of health workers transparent; and adopt an incentive mechanism to encourage them to work in remote areas. The policy of transferring the management of sub-health posts and health posts to local communities will be further intensified; and recruitment of health workers and procurement of drugs will be done at the local level. The community drug program and human resources development program to produce trained health manpower will be further expanded. Focus programs particularly for immunization, safer motherhood and control and prevention of communicable diseases such as HIV/AIDS, as well as a Health Insurance Scheme will be initiated. Family planning and nutrition programs will be expanded and made more effective. MOH is also developing an annual work plan within the framework of the MTEF and the Tenth Plan that would help implement these key reform actions identified in the Health Sector Strategy as a part of a sector-wide approach to improve performance. It is expected that with effective implementation of these policies and programs, the existing infant mortality rate will come down to 45 and life expectancy will increase to 65 years from the current 61.9 years. All sub-health posts, some of the health posts, and some hospitals will be managed by local bodies/communities by the end of the Plan. 149 The new implementation modalities in the education and health sectors should be seen as a logical extension of the decentralization process. Indeed, they represent the operationalization of the commitment the government made two years ago to transfer increased functions and responsibilities to local governments and communities, starting with education, health, rural roads and agricultural extension services. While the management of MEH/Nepal/Situational Analysis, April 2004 61 primary schools and primary health centers in specified areas are being transferred to community management committees, funding for them will be channelled through local governments—DDCs and VDCs. The community management committees will be answerable to, and be monitored by the DDCs/VDCs for ensuring effective use of and accountability for resources, while technical support for the management committees will be provided by the district offices of the line departments, since the DDCs and VDCs do not have sufficient capacity in this regard at present. Moreover, in both education and health, the pace of transferring management to the communities will be gradual, taking into account the management capacity and readiness of communities to take on such responsibilities, the degree of availability of support through NGOs and CBOs, and implementation constraints created by the domestic disorder. As conditions improve, particularly as peace and a degree of normalcy return to the affected areas, it would be possible and necessary to develop new implementation modalities involving local groups, NGOs and CBOs in order expand the community management approach to those areas also. Finance paragraphs in the PRSP (page 64-66 en 72/73) 177 Accordingly, the rest of this section briefly reviews the Tenth Plan's strategy with regard to its financing. It starts with the "normal case"—what the government would like to do, if resources are available. Even here though, the program for the first year has been sharply reduced, (reflecting the present resource constraints), but picks up quickly thereafter. Recognizing that the resolution of the present fiscal and socio-political constraints may take more time and the Plan's targets and expenditure programs may have to be scaled down for a longer period, a “lower case” scenario, (which is really a base case) is then presented. The lower case scenario is indeed the operational basis at present, and will be adjusted every year through the MTEF as resource availabities and development needs change, (for example as may be required with the progress of the peace negotiation process). And, as and when resource availabilities improve, the Government will try to move up to the normal case scenario to the extent possible. The remainder of this section will discuss how future expenditure adjustments will be made in practice, (through the MTEF, expenditure prioritization etc); as well as the actual adjustments that have been made so far in this year's budget to firmly anchor the Tenth Plan to resource availability and to protect its poverty reduction priorities through the MTEF. A third "low case" scenario is not separately discussed, because these built-in mechanisms will help reduce the Plan expenditures further in a systematic way, if needed. Macro-economic Framework 178 The macro-economic framework of the Tenth Plan has been set taking into account the economic growth target, the financial resources required to meet that target, and the incremental capital output ratio estimated at 4.3:1. Given the fact that resource availability, implementation capacity and Plan outcome will be heavily influenced by the law and order situation in the country, the macro economic framework has been designed on the basis of two scenarios for targeted economic growth. The first—Normal Case—assumes that restoration of peace within the first year of the Plan would provide room for a GDP growth of 6.2 percent per annum. The investment requirement to attain this growth, given the incremental capital-output ratio, would be about Rs. 610 billion for the entire Plan period. As private sector is expected to contribute about 72 percent of this investment, the required government investment for attaining the growth target would be Rs. 170 billion for the Plan period. The corresponding development outlay by the Government would be Rs. 234 billion. The annual decomposition of this development outlay is in line with the MTEF, which was formulated in FY 2003. Starting from Rs. 32.5 billion in the first year of the Plan, development expenditure would reach Rs. 51.5 billion in the third year of the Plan. 179 In case the restoration of sustainable peace takes a longer time, the 'normal' economic growth would be difficult to attain. A risky investment climate for the private sector, resource constraints in the public sector and constrained Plan implementation capacity would hamper the growth potential. Accordingly, economic growth in the constrained environment is expected to be confined to only 4.3 percent per annum under this alternative 'low case' scenario. The investment required to attain the lower growth target would be Rs. 457 billion. Of this, the investment to be made by the government would be Rs. 129 billion; and the MEH/Nepal/Situational Analysis, April 2004 62 corresponding development expenditure level would be Rs. 178 billion for the five year Plan period. Accordingly, from Rs. 29 billion in the first year, the development expenditure will rise to Rs. 40.5 billion in the third year of the Plan. 180 The key assumptions underlying these two scenarios are discussed in some detail below. However, it is worth noting that maintaining a sustainable macroeconomic framework and ensuring macroeconomic stability are built in as key imperatives under both scenarios. The major differences between the two scenarios are with regard to the scope for mobilization of government revenue and domestic/national savings, (both of which will be closely related to the levels of economic activity/growth), and the feasible levels of external assistance inflows. Under both scenarios, prudent monetary, fiscal and exchange rate policies designed to keep domestic inflation at around 4.5% p.a. and foreign exchange reserves at comfortable levels (nine months' imports equivalent) will be pursued; and the overall fiscal deficit (after grants) is expected to remain at a sustainable level of about 5 percent of GDP throughout the Plan period. Much of this deficit would be financed by concessional external loans; and domestic borrowing will average only about 2.0 percent of GDP per annum over the Plan period. Such a fiscal deficit would not pose any serious threat to price and balance of payments stability of the country. Financing this defic it through the planned level of domestic borrowing also will not lead to a substantial rise in the debt burden of the government. Debt servicing will remain within affordable limits. The Normal Case 181 The Normal Case Scenario is based on a number of critical assumptions: (i) The security situation will improve beginning in the second half of 2002/03, helping to bring about a modest revival in tourism and domestic economic activities. (ii) The agriculture sector is expected to grow at a modest rate. These will help the economy to achieve a 3.3% growth rate in 2002/03. (iii) Global economic conditions will also improve in 2003/04, helping to achieve faster GDP growth from then on—-6.1% in 2003/04, rising to 7.5% in 2006/07. (iv) Lower revenue growth will initia lly constrain development spending in 2002/03 to only about Rs. 32.5 billion; but will recover strongly after that. (The revenue/GDP ratio will rise from 12.0% in FY 2002 to 14.0% in FY 2007). (v) Savings and investment rates, after a slow start in 2002/03, are expected to grow by 11% and 9% per annum respectively during the Plan period. (National savings will rise from 17.4% of GDP in FY 2002 to 23.1% in FY 2007). (vi) Prioritization of projects and improved monitoring will increase the effectiveness of public expenditure and bring positive results; and (vii) Accelerated reforms will help attract more foreign assistance and raise growth rates further, especially during the last 2 years of the Plan period. The Alternative Case 189 Recognizing that some of these risks outlined above may indeed materialize and constrain resource availability and the potential for economic recovery and growth, the Tenth Plan incorporates an alternative lower case scenario to indicate how the government will deal with such a situation (Table 15). The key assumptions of the lower case scenario include the following: (i) The security situation will improve late in (beginning in the last quarter of) 2002/03; (ii) The recovery in the domestic economy will be slower and take longer, with a slower rate of growth in exports and remittances reflecting slower recovery of the international economy also. (iii) Revenue growth will be slow, reflecting the continuing weakness in the economy. The revenue/GDP ratio, after an initial decline (from 12.0% in 2001/02) to 11.8% in 2002/03, will rise slowly to 13.0% by 2006/07, averaging only 12.4% p.a. for the Tenth Plan period. (iv) Current expenditures will decline marginally from 11.7% in 2001/02 and 12.6% in 2002/03 (reflecting the need to sustain some security-related expenditure) to 11.1% of GDP by 2006/07, and average 11.9% p.a. of the Tenth Plan period. (v) Gross aid inflows will increase only modestly (from 4.7% of GDP in 2001/02 to 5.7% in 2006/07); (vi) but, the government will continue to limit domestic borrowing to limit the debt burden; and such borrowing will fall steadily from 3.2% of GDP in 2002/03 to only 0.8% in 2006/07. (vii) The cumulative effects of these assumptions are that resource availability for financing development spending by the government will remain very tight. For example, in 2002/03 development spending is assumed to be only Rs. 29 billion (equivalent to 6.5% of GDP) compared to a budget target of Rs. 38.3 billion and actual spending ratio of 7.6% in 2001/02. Moreover, development expenditure/GDP ratio will rise only gradually to 8.4% by MEH/Nepal/Situational Analysis, April 2004 63 2006/07, averaging 7.6% of GDP p.a. over the Plan period. (viii) Under this scenario domestic/ national savings and overall investment levels in the economy will decline below the 2001/02 levels, refle cting a sharp decline in these variables during the current year (2002/03), followed by a very modest recovery in the next few years. Thus, national savings are expected to reach only 16.1% of GDP by 2006/07, and total investment in the economy only 21.8% by 2006/07 (Table 15). Therefore, to attain a growth rate of 4.3% p.a. over the Plan period, a significant improvement in the efficiency of the use of resources will be required. This is of course what the Tenth Plan strategy tries to do by prioritizing expenditures, focusing on quick returns and results in terms of output and service delivery and improving accountability and monitoring. 190 Given these assumptions, the economy’s performance in terms of GDP growth, social and infrastructure development and poverty reduction will be significantly lower under the Lower Case than under the Normal Case (Table 12, last column). For example, GDP growth will be only about 2.0% in 2002/03, and rise slowly thereafter to 4.0% and 4.5% in the next two years, though picking up thereafter to 6.0 % by 2006/07. For the Tenth Plan period as a whole, GDP growth will average 4.3% p.a., permitting per-capita income growth of about 2.0 % per annum. This is still better than the GDP and per capita income growth rates of 3.6% and 1.3% respectively achieved during the Ninth Plan, but not good enough from a macroeconomic perspective to achieve significant progress in poverty reduction. Not surprisingly, development programs, activities and results in virtually every area would be constrained. Medium Term Expenditure Framework (MTEF) 191 Recognizing the fiscal deterioration and the need to revise the Tenth Plan accordingly, the Government initiated the preparation in parallel of a Medium Term Expenditure Framework (MTEF) in late 2001. The key objective of the MTEF was to begin to implement the Tenth Plan from the beginning of the fiscal year 2002/03, without waiting for the formal finalization of the Plan. Accordingly, the key projects/programs and activities that are considered essential for achieving the Tenth Plan's poverty reduction goals and their resource requirements for the next three years were to be identified, and were to be given priority in terms of budget allocations in the 2002/03 budget. Additional considerations guiding the MTEF, in view of the fragility of the fiscal situation, were: (i) How to streamline the budget which was already overextended well beyond resource availability, with over 600 ongoing activities/budget lines? (ii) How to protect the Tenth Plan's key priorities in the event of further shortfalls in resource availability? and (iii) How to ensure that the resources allocated and released for priority activities would be effectively utilized? The MTEF was expected to be the principal instrument for operationalizing the Tenth Plan, by prioritizing the proposed Plan activities according to the changing resource situation, and firmly linking the annual budget process and the Plan. 192 Thus, a three year MTEF was prepared in early 2002 by virtually the same line ministry teams responsible for Tenth Plan preparation, using similar methodology for ranking and prioritizing activities, (but with a sharper focus on implementability, short term financing needs and results). On the basis of the MTEF, (i) the 2002/03 development budget was initially set at a significantly lower level—Rs. 38 billion, compared to Rs. 50 billion in the 2001/02 budget; and the number of budget lines were reduced from over 600 to 430. (ii) Even more importantly, all activities were classified into three groups according to their priority (P1 being the highest priority and P3 being the lowest); and (iii) The principle was established that the priority classification would be strictly followed in releasing funds for development activities. Thus, P1s will receive first priority in budget releases; and P2 and P3 will get funded only if funds are still available after providing for P1s. This has established clear criteria and methodology for adjusting resource allocations on the basis of Tenth Plan's priorities, in line with changes in the resource situation. (iv) Finally, resource allocation was linked to expenditure reporting and performance, in order to ensure satisfactory results. Thus, under the new system that has been evolved, activities which do not provide statements of expenditures (SOEs) for the preceding trimester will not be given additional funds, until they provide the SOE's. (Section VII discusses these in more detail). MEH/Nepal/Situational Analysis, April 2004 64 From Table 18 page 85 Key indicators/actions for Health MEH/Nepal/Situational Analysis, April 2004 level of analysis frequency Source of data collection responsible agency 65 PRSP: Policy Matrix for Health MEH/Nepal/Situational Analysis, April 2004 66 Annex 5 People met in Nepal during mission 16/12/03 – 06/01/04 1. Dr. Klaus Wagner, WHO Representative Nepal 2. Dr. Lin Aung, Health Planner, WHO Nepal 3. Dr. Bhakta Raj Dahal. National Operation Officer WHO. 4. Dr. Benu Bahadur Karki, Chief Policy, Planning & International Cooperation, MoH (core member Subcommittee Macroeconomics and Health) 5. Dr. Dr. Bishnu Prasad Pandit, Chief Specialist, MoH 6. Dr. Rita Thapa, Senior Public Health Policy Adviser, MoH 7. Mr. Tanka Mani Sharma, Under Secretary Finance, Chief Health Economics & Financing Unit (HEFU) MoH 8. Mr. Ram Krishna Tiwari, Joint Secretary National Planning Commission (core member Subcommittee Macroeconomics and Health) 9. Mr. Lal Shankar Ghimire, Under Secretary Foreign Aid Coordination Division, MoF (core member Subcommittee Macroeconomics and Health) 10. Dr. Umesh Prasad Dhakal, Director Health Service Department, Nepal Red Cross Society 11. Mr. Ramesh Kumar Sharma, Chairman Nepal Red Cross Society 12. Mr. Badri Khanal, Executive Director, Nepal Red Cross Society 13. Dr. Sachey Kumar Pahari, Executive Chairman Nepal Medical College/Teaching Hospital, Chairman Nepal Health Research Council 14. Dr. Anil K. Mishra, Member Secretary Nepal Health Research Council 15. Mrs. Chetna Thapa, publication officer Nepal Health Research Council 16. Dr. Tirtha Rana, Senior Health Specialist, WB Nepal 17. Dr. Aviva Ron, Consultant Health Policy (Masterplan Social Health Insurance Nepal -ILO) 18. Dr. Angelika Schrettenbrunner, Programme Manager Health Sector Support Programme GTZ 19. Ramji Dhakal, GTZ 20. Sheila Lutjens, Director Office of Health and Family Planning, USAID 21. Dr. Hernando Agudelo, Deputy Representative UNFPA 22. Mr. Harka Bahadur Thapa, Project Manager Rural Health Development Project, SDC 23. Mrs. Susan Clapham, Health Advisor DFID. MEH/Nepal/Situational Analysis, April 2004 67 Annex 6 Bibliography MEH situational analysis Nepal 1. Action Plan for Essential Health Care Package. Annex to unknown document. Contains specific targets per programme for scaling up between 2003-2005. 2. Annual Report 2001/2002. MoH, Department of Health Services, February 2003 3. Annual Report July 2002-2003. Rural Health Development Project. HMG/SDC. 4. Budget speech. MoF. 17 July 2003. 5. Costing of NHSP-IP with Unit Cost of EHCS. Second draft. 25 February 2004. 6. Country Assistance Strategy Nepal. Progress report. WB, Jan 2003 7. Description of INGOs Supported programmes (Fiscal Year 2003/2004). Website MoF. Not dated. 8. Description of Technical Assistance (Fiscal Year 2003/2004). Website MoF. Not dated. 9. Developing Health Sector Decentralisation in Nepal: Collaborative Policy Development. Charles Collins et al. British Concil Nepal, 2003. 10. DFID Nepal. Summary of projects funded in the health sector. November 2003. 11. Health information in brief. MoH, 2002 12. Important issues related to Macroeconomics and Health in Nepal. Unknown author, not dated. 13. Links between Macroeconomics and Health Sector in the SEA Region. Abusaleh Shariff. August 2003 14. Living Standard Measurement Survey rural and urban questionnaires. CBS, 2003. 15. MacroEconomics and Health – Nepal. Draft project proposal MoH, cleared 2 September 2003 16. MacroEconomics and Health – Nepal. Plan of Action for the Preparatory Phase. Revised proposal cleared 6 January 2004. 17. MDG Progress Report 2002. HMG of Nepal and the UN Country Team. February 2002. 18. Medium Term Expenditure Framework FY 2002/3 – 04/05 5.2 Health. MoH, July 2002. 19. Medium Term Expenditure Programme (MTEP) to operationalize 1 st three years of 10th five-year plan’s health programmes. Kalyan Raj Pandey for the MoH (not dated) 20. Memorandum of Understanding for Collaboration between the South East Asia Regional Office of the World Health Organization and the International Federation of Red Cross and Red Crescent Societies. DRAFT 2 (revised on 20.2.2003) 21. MoF Nepal. Description of Technical Assistance Fiscal Year 2060/2061. 22. National Seminar on Health and Poverty Reduction in Nepal. Kathmandu, 14-15 February 2002 23. Nepal and Senegal: initial support for Macroeconomics and Health work. Proposal. Royal Tropical Institute Amsterdam, June 2003 24. Nepal country strategy paper. DFID, October 1998 25. Nepal Health Sector Programme – implementation plan (NHSP-IP) 2003-2007. MoH, August 2003 26. Nepal Health Sector Strategy: an agenda for change. Draft June 2002 27. Nepal Joint Staff Assessment of the PRSP. IDA/IMF, 16 October 2003 28. Nepal Red Cross Society. Several brochures. 29. Nepal. Operational Issues and prioritization of resources in the health sector. WB HNP Unit South Asia Region, June 8, 2000 30. Nepal’s Health Sector Study on meeting the MDGs. Kiran Dev Pant, Nepal Health Economics Association. Not dated 31. Organograms MoH and DoHS. MoH, 19 August 2003 MEH/Nepal/Situational Analysis, April 2004 68 32. Overview of German Support to HMG/N Health Sector. GTZ and KfW, December 2003. 33. Poverty reduction and governance. Nepal Human Development report 2001. UNDP, 2002 34. Pro-poor health strategies in Nepal – challenges and opportunities. WB ppt presentation, 25 September 2003 35. Public expenditure review of the health sector. HMG Nepal, MoH, Health Economics and Financing unit. July 2003 36. S. Acharya,G. Carrin, A Herrin. The macro-economy and health sector financing in Nepal: a mediumterm perspective. Chapter 11 in Macroeconomic Environment and Health – with case studies for countries in greatest need. WHO Geneva, 1993. 37. Second Long Term Plan 1997-2017. Executive summary. MoH, August 1999. 38. Selected Indicators Nepal. Website WHO March 2004. 39. Socio-economic differences in health, nutrition, and population in Nepal. Gwatkin et al. WB, May 2000. 40. Strategic Analysis to Operationalise Second Long Term Plan. MoH, May 2000. 41. Strategic Plan for Human Resources for Health 2003-2017. MoH Nepal April 2003. 42. Summary information on policies and plans. MoH Nepal Website: www.moh.gov.np 43. Summary of Income and Expenditure 2001/2, 2002/03; Estimates of government revenue 2003/04; Summary of budget estimate 2003/04. MoF, 2003. 44. Terms of reference for costing of the EHCS. WB consultancy end 2003/early 2004 45. The Tenth Plan 2002-2007 (PRSP). NPC, Kathmandu, May 2003. 46. The Tenth Plan 2002-2007. Chapter 24 Health. NPC, Kathmandu, February 2003. 47. Understanding the access, demand and utilisation of health services by rural women in Nepal and their constraints. WB Nepal, June 2001. MEH/Nepal/Situational Analysis, April 2004 69