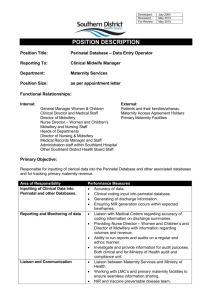
Maternity Services Literature Review DPHQA Final 06.07
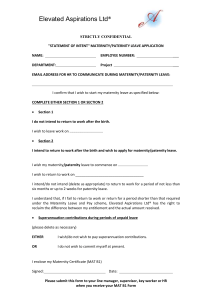
advertisement

Maternity Services Literature Review Author: Sian Ap Dewi, Principal Public Health Officer, Siobhan Jones, Consultant in Public Health, Rob Atenstaedt, Consultant in Public Health Medicine, Jo Charles, Associate in Public Health, Gill Richardson, Executive Director Public Health Aneurin Bevan Health Board, Andrew Jones, Executive Director Public Health Date: July 2011 Version: 1 (Final) Publication/ Distribution: Internet Purpose and Summary of Document: To answer the question: What is the current evidence base on the delivery of safe and sustainable maternity services? MATERNITY SERVICES LITERATURE REVIEW ................................ 1 1 SUMMARY OF KEY MESSAGES ................................................. 3 2 BACKGROUND ......................................................................... 6 2.1 Methodology ........................................................................ 7 2.2 Introduction ......................................................................... 7 2.3 Factors that impact on the health of mothers and babies ........... 9 2.4 Why is maternity care important? .......................................... 11 2.5 What do we mean by Maternity Services? ............................... 12 2.6 Access to Maternity Services ................................................. 13 2.7 Barriers to access ................................................................ 14 3 DEVELOPMENTS WITHIN MATERNITY SERVICES .................. 15 3.1 The Challenges .................................................................... 15 3.2 Maternity Dashboard ............................................................ 18 3.3 Antenatal Care .................................................................... 18 3.4 Supporting women through childbirth ..................................... 20 3.5 Role Definition ..................................................................... 20 3.6 Midwife led care................................................................... 24 3.6.1 Midwifery led Units (MLU) ..................................................... 26 3.6.2 Home Births ........................................................................ 28 3.7 Evidence from the Netherlands .............................................. 30 4 SAFER CHILDBIRTH .............................................................. 32 4.1 What should a Birth Setting look like? .................................... 33 4.2 Guidance on decision to delivery intervals for emergency caesarean section ................................................................ 33 5 RECOMMENDATIONS ARISING FROM THE LITERATURE ........ 35 5.1 Recommendations for the Maternity Service for Wales .............. 35 5.2 Recommendations for the New Local Health Boards from the Wales Audit Office Maternity Services report .................................... 36 6 APPENDIX: SEARCH STRATEGY ............................................. 38 7 REFERENCE LIST ................................................................... 45 Date: July 2011 Version: 1 Page 2 of 49 1 Summary of Key Messages Prevention and Early Intervention Strengthening maternity services will benefit entire health care systems. Maternal and newborn care services are the cornerstone of public health services. Care of pregnant women can be the entry point for health services to the family and community (World Health Organisation) Future maternity services must be planned to ensure safe and high quality maternity services are provided that meet the needs of the population. Services should seek to reduce inequalities and inequities and improve outcomes Current policy documents highlight the current risks to maternal and child health from preventable factors such as maternal smoking and maternal obesity. The important role that maternity services can play in improving the health and well being of individuals and communities is identified (Strategic Vision for Maternity Services in Wales & Midwifery 2020) Challenges Maternal age has Wales appears to maternal age and does the risk of treatment). All of service need The key challenges for medical cover of secondary care maternity services across Wales have been identified as; - The effect of the European Working Time directive on the provision of junior and senior medical service - Training and continuing professional development, shorter medical training periods requiring more organised training opportunities and supervised clinical experience - Recruitment difficulties in nearly all the professions involved - The geographical Date: July 2011 risen in many areas of the western world and be following this trend. Fertility decreases with the rate of chromosomal anomalies increases as multiple births (as a consequence of infertility these factors have the possibility of increasing challenges to Version: 1 achieving consistent clinical Page 3 of 49 Public Health Wales Maternity services literature review standards of care including access/travel times (Welsh Medical Committee ‘Maternity Service’ report) The WMC report recommended that where service reconfiguration is proposed, professional advice is sought from Royal Colleges and advisory groups early in the planning stage, and that any impacts on medical training be considered Staffing levels, training, access to services, information systems, high caesarean section rates in Wales, clinical negligence claims, the need for a common data set and increased post natal support are key themes that emerged from the Wales Audit Office (WAO) 2009 report on Maternity Services in Wales. Recommendations in relation to these areas were made by WAO Midwifery led care To achieve the vision set out in the Midwifery 2020 strategy, midwives should be the lead professional for healthy women with straightforward pregnancies. For women with more complex pregnancies they should act as the key coordinator of care (Midwifery 2020) Women classified as low or mixed risk, receiving midwife–led models of care were found to have: reduction in regional analgesia, fewer episiotomies and instrumental births, less likely to experience antenatal hospitalisation, less likely to lose babies before 24 weeks gestation and shorter length of hospital stay. Midwife-led care increased the chance of having a spontaneous vaginal birth and initiating breastfeeding. There were no statistically significant differences in Caesarean birth rates. (Cochrane review). The new Maternity Services Strategy for Wales currently out for consultation, supports a greater focus on midwifery led births, and proposes that this care is delivered in a range of settings including home, hospital or midwife led units appropriate to the needs of the mother and family Midwifery led units A structured review of birth centres (term used interchangeably with midwifery led units for purpose of this report) found that due to the limitations of the available data, there was no reliable evidence about either clear benefit or harm associated with birth centres compared with any other type of intrapartum care offered Date: Feb 2011 Version: 0j Page: 4 of 49 Public Health Wales Maternity services literature review in the NHS. (National Perinatal Epidemiology Unit: Structured Review of birth centre outcomes) There was substantial support for the service from women accessing care, their families and maternity care health professionals as the service is clearly differentiated from an obstetric-led maternity service. There are also benefits to the NHS in having a tiered service for deliveries reserving expensive obstetric care for those that really need it (National Perinatal Epidemiology Unit: Structured Review of birth centre outcomes) Women were transferred from midwifery led units (MLU) to obstetric led maternity units (OLMU) in 14-16% of cases and neonates were transferred in up to 4% of cases in one UK evaluation (24) More high quality evidence is needed on whether there are important differences in experiences and outcomes for women and babies between alternative locations and systems of care The Evaluation of Maternity Units in England (EMU), due to report in March 2011, is a programme of research designed to examine the role of midwifery led units and generate high quality evidence. Home Births The Royal College of Midwives (RCM) and the Royal College of Obstetricians and Gynaecologists (RCOG) support home birth for women with uncomplicated pregnancies provided the appropriate local infrastructures and risk assessment framework are in place to support such a system A Cochrane Collaboration review of home versus hospital births concluded as follows: There is no strong evidence to favour either planned hospital birth or planned home birth for low risk pregnant women The change to planned hospital birth for low risk pregnant women in many countries during this century was not supported by good evidence Planned hospital birth may even increase unnecessary interventions and complications without any benefit for low risk women Date: Feb 2011 Version: 0j Page: 5 of 49 Public Health Wales Maternity services literature review Several studies have been conducted to evaluate the obstetric system in Netherlands, which has a different system of maternity care to the UK. Low risk women give birth at home or in primary care under supervision of midwives. There is conflicting evidence from these studies on outcomes and perinatal mortality in relation to place of birth and travel times to hospital. Organisation and delivery of care in Labour - 2 The Safer Childbirth report (2007) gives detailed advice of staffing roles within maternity services. In particular they advise: Increase in appropriately trained maternity support workers to support role of midwife Availability of Supervisor of midwives 24/7, with a ratio of 1 supervisor to every 15 midwives. Labour ward shift coordinator should be supernumerary 40 hour consultant cover on labour ward for units with <2500 births/year. 60 hour consultant cover for units with 2500-4000 births Guidance exists in relation to decision to delivery intervals for emergency caesarean section. A decision to delivery interval describes the time between an obstetrician in a consultant led unit deciding that a caesarean section should be undertaken, and the delivery. A decision to delivery interval of less than 30 minutes is not in itself critical in influencing baby outcome but remains an audit standard for response to emergencies within maternity services (NICE Clinical Guideline) Background The purpose of this report is to provide information to support the North Wales Review of Maternity, Neonatal, and Gynaecology and Child Health services. The aim of the review is to describe the optimum service delivery model that will ensure safe, sustainable and efficient maternity, neonatal and paediatric health services are provided for the population of North Wales. The future model of service delivery will seek to improve population health and optimise health and well-being outcomes for women and children. Date: Feb 2011 Version: 0j Page: 6 of 49 Public Health Wales Maternity services literature review In order to ensure that discussion and debate are as well-informed as possible, this paper seeks to provide: An understanding of the background to the current situation A summary of key guidance and recommendations made by national bodies and authorities Findings from a targeted review of key sources An indication of the key aspects of safety, quality and sustainability against which proposed options generated within the review process may be viewed. 2.1 Methodology Due to the short timescales involved in undertaking this review, a method drawn from an approach known as Rapid Appraisal has been used. Searches were undertaken of core databases, topic specific databases and meta search engines for recently-published (since 2000) evidenceinformed material. Here the phrase “evidence-informed” is used purposefully to distinguish it from the more familiar term “evidencebased”. Use of the term evidence-based would imply 1. a systematic review approach to ensuring all relevant literature is identified; 2. reference to a “hierarchy of evidence”; and 3. structured critical appraisal of the individual pieces of literature. This review has used a structured approach to identify relevant reports and papers, many of which are summaries of available evidence with recommendations for good practice. The most important sets of recommendations are reproduced in full in the penultimate section. The initial searches were undertaken by the Public Health Wales Library and Knowledge Management Services Team, and their full search strategy is listed as an Appendix. 2.2 Introduction The priority for modern maternity services as identified in the “Maternity Matters” report prepared by the Department of Health is to provide a choice of safe and high quality maternity care for all women and their partners. This is to enable pregnancy and birth to be a safe and satisfying process for both mother and baby and to support and enable new parents to have a confident start to family life (2). Date: Feb 2011 Version: 0j Page: 7 of 49 Public Health Wales Maternity services literature review The “Towards better births” review of maternity services in England highlighted that the National Service Framework emphasised the need for woman centred, individualised care (3). The report recognised that a women’s reaction to her birth experience can influence her emotional well being, her relationship with her baby and future parenting. Women should have a good experience and positive view of the support provided to them during the three stages of maternity care: pregnancy, labour and birth and the post natal period. Women their partners and their families should, according to the NICE guidelines on Antenatal Care, always be treated with kindness, respect and dignity (4). The views, beliefs and values of the woman, her partner and her family, in relation to the care of her baby, should be sought and respected at all times. Good communication between healthcare professionals and women is essential. This should be supported by evidence based, written information tailored to the woman’s needs. Care and information provided should be culturally appropriate, and all information should also be accessible to women with additional needs such as physical, sensory or learning disabilities, and to women who do not speak or read English (4). The Wales Audit Office report on maternity services stated that maternity services need to be planned in such a way that they meet the needs of the local population. The report also suggested that it is important that services meet national standards to help ensure consistency in the quality of maternity services provided across Wales. The Wales Audit Office report noted that the Welsh Assembly Government had not set any national performance targets for maternity services and whilst the office was not recommending the implementation of targets, it did note that the absence of national performance targets for maternity services had resulted in other service areas being given higher priority (5). Infant mortality rates are higher in more deprived areas of the country and in more vulnerable and disadvantaged groups (2). The “Why Mothers Die” report found a higher risk of maternal death in women from minority ethnic groups, women who were socially disadvantaged, poor attenders and women with a history of psychiatric illness (6). Date: Feb 2011 Version: 0j Page: 8 of 49 Public Health Wales Maternity services literature review Future maternity services must therefore be planned to reduce inequalities and inequities and improve outcomes for the most disadvantaged and vulnerable families. The challenges of the reduction in working hours of doctors as a result of the introduction of the working time directive needs to be addressed, as do the changes brought on by demographic and lifestyle changes. However the principle should remain that pregnancy and birth are natural events which should be supported by midwives (2). 2.3 Factors that impact on the health of mothers and babies Research work undertaken in Great Britain has shown that more deprived families are likely to have overall higher levels of the following: Perinatal and infant mortality, including sudden infant death Low birth weight babies (less than 2500g) Teenage pregnancy. Conversely mothers in less deprived circumstances are more likely to start their families at a later age, have more babies with a higher birth weight than 4000g, and have teenage pregnancies ending in a termination (7). There is a strong association in Wales between the proportion of low birth weight babies and the relative social deprivation of the area in which they live. The more deprived the area then the higher the proportion of low birth weight babies. Teenage pregnancy rates also tend to be higher in the more deprived areas of Wales (7). Babies born with low birth weight (less than 2500g) are more likely to die in the first few weeks of life or to develop certain chronic diseases in childhood. Very low birth weight (‹1500g) is associated with significant disability. Poorer survival and the association with deprivation can be demonstrated in Wales (7). In recent years maternal age has risen in many areas of the western world and Wales appears to be following this trend. A woman giving birth at an Date: Feb 2011 Version: 0j Page: 9 of 49 Public Health Wales Maternity services literature review older age is associated with relative affluence and better maternal educational achievement. There is some evidence of this in Wales (7). However fertility decreases with maternal age and the rate of chromosomal anomalies increases as does the risk of multiple births (probably as a consequence of infertility treatment). All of these factors have the potential to increase service need (7). The most recent annual report by the Congenital Anomaly Register and Information Service highlights high rates of Isolated Cleft Palate in North West Wales. Although detailed analysis of the data has not identified a reason for this increase, there are some important public health messages to communicate around risks of congenital anomalies. In particular, the risks in relation to smoking, alcohol, substance misuse and obesity in pregnancy. The use of folic acid and the importance of preconceptual care are also highlighted (49). Improved care for serious childhood illness, including cancer and congenital heart conditions has permitted increasing numbers of women to reach their childbearing years after surviving major health problems; and these women are more likely than other women to need additional support during pregnancy and labour. Less common conditions like tuberculosis are also on the rise and can pose a threat to women in pregnancy (8). There are a number of groups within society who although small in number carry an increased vulnerability to social exclusion and economic disadvantage. People within these groups have a greater risk of adverse health outcomes. Groups include those with learning disabilities or physical disabilities, people with mental health problems, young adults who are leaving care, victims of domestic abuse, people who are homeless, travelling families, refugees, people with substance misuse problems or people leaving prison (7). For women in such groups pregnancy might bring with it particular challenges, however at present no comprehensive data exists to describe the health status of women and their babies in these groups across Wales. WHO note the benefits of strengthening maternity services (9) and the importance of ensuring the availability of high quality safe universal services for the whole population that can also be flexible to meet the specific needs of vulnerable groups. Current policy documents highlight the important role of maternity services in improving the health and well being of individuals and families (53, 54). The public health role of the Date: Feb 2011 Version: 0j Page: 10 of 49 Public Health Wales Maternity services literature review midwife is also highlighted as vital, needing to be protected and strengthened (53,54) 2.4 Why is maternity care important? The World Health Organisation identified in their strategic approach document for making pregnancy safer (2008) that women and babies in European countries are still dying an unfair and unnecessary death, and suffering unnecessary illness and disabilities (9). The report argued that although evidence based interventions are well known, many European countries have stagnated and regressed in their efforts to reduce maternal and perinatal mortality (9). Obtaining the highest attainable standards of health is a human right and all women and newborns regardless of their socio – economic status, culture, race or origin have the rights to these standards of health (9). Women play an irreplaceable role as citizens, mothers, and caretakers and are frequently the family’s breadwinners. Therefore if a woman dies from complications of pregnancy, or becomes ill or disabled, then the well being of the whole family is severely affected (9). Investing in maternal health is a powerful way of improving the lives of poor and marginalized women. The “Making Pregnancy Safer” Regional strategy for Europe argued that no single intervention on its own was sufficient. Maternal and newborn deaths can, however, be reduced significantly using low cost and effective interventions (9). The regional strategy stressed the importance of strengthening capacity within health systems in order to identify best practice for programme development. Emphasis needs to be placed on planning implementing and evaluating interventions, including the identification of subpopulations with higher levels of needs (9). The health of the newborn is directly linked to the health of the mother and avoiding complications that affect the mother will improve perinatal outcomes (9). The World Health Organisation argue that strengthening maternity services will benefit entire health care systems as maternal and newborn Date: Feb 2011 Version: 0j Page: 11 of 49 Public Health Wales Maternity services literature review care services are a cornerstone of public health services. The care of pregnant women can be the entry point for health services to the family and community to prevent and treat for example STIs, HIV, and introduce family planning, ensure immunizations, provide nutritional advice or act as a conduit to the introduction of other health programmes (9). 2.5 What do we mean by Maternity Services? Maternity services were defined by a multi professional maternity services group in 2010 in the document A Maternity Service for Wales (10), as those services delivered chiefly by Midwives, Obstetricians, Anaesthetists, Paediatricians and Neonatologists. The Maternity Service aims to be a cohesive service providing care for women at both high and low risk of complications. The medical specialities are also a part of the core service specialities. The role of GPs in the provision of mainstream maternity services has diminished considerably within the last decade, but continues usually at a lower level most often in the period before pregnancy and after delivery. Midwives are involved in the care of all pregnant women irrespective of their risk status and their involvement in the Maternity Service is ubiquitous (10). A recent policy document recommends that midwives should be the lead professional for healthy women with straightforward pregnancies. For women with more complex pregnancies they should act as the key coordinator of care within the multidisciplinary team (53) Much of the care provided to women is provided in the home or community. When a women’s risk status changes from one of low risk to a higher risk during pregnancy then it becomes necessary to involve one or more of the medical specialities in addition to midwifery care. This higher level of care is provided in hospital consultant or obstetric units with the majority forming part of the secondary sector, with the midwife remaining as the coordinator of care (53). The Royal Colleges have set out the requirements for providing obstetric led care and obstetric anaesthesia, while the British Association of Perinatal Medicine (BAPM) sets out the standard of care for newborn babies. The Maternity Services also represent an interdependent network across Wales; especially where more advanced care at tertiary centres is required for critically ill babies or their mothers. It was noted within A Maternity Service for Wales that the Welsh maternity services network is a virtual one, and as such has never been subject to formal organisation (10). Date: Feb 2011 Version: 0j Page: 12 of 49 Public Health Wales 2.6 Maternity services literature review Access to Maternity Services The “Access to Maternity Services” research report highlighted inequalities in access to maternity services and identified a number of groups who were less likely to access ante and post natal services. The report found that women’s attitudes towards managing their health and accessing maternity services often reflected their circumstances (11). Some women from minority ethnic groups and communities preferred to use expertise and support that was available within their community groups, and only used general health services when necessary (11). Other “hard to reach” groups, such as those individuals dependant on drugs or alcohol and homeless women, found it difficult to access health services as a result of the complexity of their problems, limited understanding of the health service and issues relating to their transient lifestyle (11). The NICE guidelines relating to Pregnancy and Complex Social Factors note that pregnant women who misuse substances may be overwhelmed by the involvement of multiple agencies and that those women need supportive and coordinated care during their pregnancy (12). Although teenagers and women with learning difficulties were more likely to access services, along with other groups they often lacked the confidence to engage fully with services as they feared that they would be labelled or would face discrimination (11). As well as attitudes towards pregnancy, other barriers, such as those relating to practical access, cultural relevance and understanding of the role and value of the services meant that none of these “hard to reach” groups used maternity services to their full extent (11). Attendance at antenatal classes was limited and most care focused on scans and check ups. Many were late receiving antenatal care and consequently felt ill prepared for motherhood. Patterns of post natal care were more consistent as contact was relatively easy for health visitors to follow up after the birth (11). Date: Feb 2011 Version: 0j Page: 13 of 49 Public Health Wales 2.7 Maternity services literature review Barriers to access The Access to Maternity Services report found that women from “hard to reach” groups found it difficult to access maternity services targeted at the general population for the following reasons (11): Fear of discrimination or prejudice and referral to either social services or immigration agencies Cultural sensitivities relating to the need to be treated by a female and with discretion Personal circumstances that made it difficult to acknowledge and accept their pregnancy Practical difficulties relating to low levels of literacy, transient lifestyle (which meant that they were not always registered with a G.P) cost of travel, fixed appointment times and language difficulties. Misconceptions about their eligibility for the service and its elements. These barriers demonstrate the need for maternity services to cater more effectively to the needs of specific, vulnerable groups through a more tailored service. Active steps are needed to counter misconceptions and build a better understanding of the service offered. The importance of sensitivity when dealing with women from hard to reach and vulnerable groups was highlighted within the report as was the need to provide information and guidance in order to prevent confusion (11). These recommendations are also repeated within the NICE guidelines relating to Pregnancy and complex social factors (12) which recommended that Women should be told why and when information may need to be shared with other agencies To allow for discussion of sensitive issues each woman should be provided with a one to one consultation without partners, family members or legal guardians present on at least one occasion Hand-held Maternity Notes should be kept up to date with a full record of care received and contain all test results (12) Date: Feb 2011 Version: 0j Page: 14 of 49 Public Health Wales Maternity services literature review Post natal services were appreciated for the practical strategies provided but women from these “hard to reach” groups often felt that the services failed to provide them with much needed emotional support and reassurance (11). Successful engagement with maternity services usually resulted from flexible provision, targeted information, and continuity of staff who were experienced or familiar with working with specialist audiences (11). 3 Developments within Maternity Services There have been many changes in maternity services over the last twenty years. Some of these changes are the result of technical advances while others are the result of the application of the findings of sound scientific studies. The introduction of screening for aneuploidy (which identify one or more chromosomes above or below the normal chromosome number), better ultra sound imaging and the creation of the sub-specialty of fetal medicine are all examples of this (13). Another development has been that of senior clinicians specializing in obstetrics alone. This is recognised by the Royal College of Obstetricians in their report The Future role of the Consultant (14). 3.1 The Challenges There have been a number of challenges identified to providing a safe coordinated Maternity Service in Wales: The Welsh Medical Committee’s “Maternity Service” (10) report noted that the risk of potential collapse of the medical elements of the service within one or two years were identified through The effect of the European Working Time directive on the provision of junior and senior medical service, training and continuing professional development. Shorter medical training periods requiring more organised training opportunities and supervised clinical experience to achieve completion of competence- based training. Date: Feb 2011 Version: 0j Page: 15 of 49 Public Health Wales Maternity services literature review Recruitment difficulties in nearly all the professions involved, with unplanned pressure to replace junior services provision 24/7 but without a suitable source of suitably trained practitioners Attempts to deal locally with the difficulties of ad hoc mergers for example, without a broader view of the effect on neighbouring and centralised (tertiary) services. Geographical challenges to reaching clinical standards of care including access/travel times Reorganisation of the health service in Wales presents excellent opportunities to address these concerns but there is also the potential to overlook them or for deterioration in quality of service if these challenges are not addressed. The Wales Audit Office 2009 report on Maternity Services in Wales (5) identified a number of key themes that needed to be addressed;- Staffing levels in some trusts were not always adequate. Some trusts were identified as failing to meet recommended midwifery staffing levels, and whilst some of the data related to consultant staffing was unclear, in some trusts there was insufficient consultant obstetrician presence on the delivery suite. Training provided for maternity staff varied considerably within Wales, with some trusts having very low levels particularly in areas such as skills for handling emergencies and in monitoring the progress of labour. The Wales Audit report (5) noted that not all obstetricians had received core training within the recommended timescales. Accessing Services- Most women accessed ante natal services within the initial 12 weeks of pregnancy in line with recommended timescales. However it was noted in the report that although the National Service Framework promotes the midwife as the appropriate first point of contact for pregnant women, 69% of those surveyed for the Wales Audit Office report first went to their GP. This is because although some midwives have clinics in GP surgeries most are only accessed via the GP (5). Date: Feb 2011 Version: 0j Page: 16 of 49 Public Health Wales Maternity services literature review Information The Wales Audit report noted that in some trusts the information provided to pregnant women was not effective in informing them of what they could expect from maternity services, thus enabling the women to make informed choices about their care. The example of ante natal classes was cited as they provide a unique opportunity for health professionals to engage with women and provide information. The proportion of women who said they had wanted to attend antenatal classes and were then able to do so vary considerably between trusts, with low attendance rates in a number of trusts. Caesarean Sections- There were a higher level of Caesarean sections within Wales than in England and there were inconsistencies in the practices that trusts employ to prevent unnecessary Caesareans (5). The typical rate of normal births in Wales was 40 percent which is considerably lower than the recommended level. There was variation identified in the rates of intervention (i.e. induction, ventouse or forceps delivery) between trusts (5). Clinical negligence claims for obstetrics had more than doubled between 2003-4 and 2007-8 with £28.4 million paid out by the Welsh Risk Pool in 2007-8 (5). However the Wales Audit office report suggested that the culture in some trusts may not be conducive to learning from such incidents. Common data set -the lack of a common data set for maternity services in Wales prevents meaningful benchmarking of performance amongst trusts in Wales. It was also identified that maternity services have a range of groups for gathering feedback on performance but that there could be improvements in how these were used to drive forward service improvement (5). Recommendations from the “Maternity Services in Wales” (5) report are that maternity services should seek to achieve high levels of satisfaction as well as providing high quality care that meets prescribed standards of good practice. Post natal support -the importance of the NHS maintaining contact with mothers for a short period of time after they return home from hospital in order to monitor the progress of both mother and baby was identified. It Date: Feb 2011 Version: 0j Page: 17 of 49 Public Health Wales Maternity services literature review was noted that wide variation exists within Wales in the number of visits that are made, which suggested a lack of consistency in the way that trusts provided post natal support. 3.2 Maternity Dashboard The Maternity Dashboard is a tool recommended by the Royal College of Obstetricians and Gynaecologists that can be employed to monitor the implementation of principles of clinical governance “on the ground”. It can be used as a means of benchmarking activity and can help monitor performance against locally agreed standards for the maternity unit on a monthly basis (18). The maternity dashboard can help identify patient safety issues in advance so that an appropriate course of action can be undertaken. It follows the principle of a car dashboard which provides contemporary information about the fuel in the tank, speed, state of the battery, and temperature of the engine so that that appropriate action can be taken if the car breaks down. Similarly the maternity dashboard will provide contemporary information about resources, clinical management issues, risk management issues and user views (18). In any unit the various parameters of clinical performance and the workforce delivering should be known and should be constantly monitored and the maternity dashboard assists this process. This tool has now been adopted by health boards across Wales as part of performance monitoring processes. 3.3 Antenatal Care The updated NICE guidelines relating to Antenatal care identified a number of new key priority areas for implementation (4). Antenatal information should be offered to women on the basis of current available evidence and should include where they will be seen, and who will undertake their care. Screening for haematological conditions such as sickle cell and thalassaemia should be offered to all women as early as possible in pregnancy and ideally by 10 weeks. Date: Feb 2011 Version: 0j Page: 18 of 49 Public Health Wales Maternity services literature review Screening for foetal anomalies and the participation in regional congenital anomaly registers and /or UK National screening approved audit systems is strongly recommended in the NICE guidelines to facilitate the audit of detection rates (4). Screening for Down’s syndrome using the combined test (nuchal translucency, beta human chorionic gonadotrophin, pregnancy- associated plasma protein-A) should be offered between 11 weeks 0 days and 13 weeks 6 days. For women who book later in pregnancy the most cost effective serum screening test (triple or quadruple test) should be offered between 15 weeks 0 days and 20 weeks 0 days. Screening for gestational diabetes using risk factors is recommended in a healthy population (4). Women with certain risk factors should be offered testing for gestational diabetes. Gestational age assessment - pregnant women should be offered an early ultrasound scan between 10 weeks 0 days and 13 weeks 6 days to determine gestational age and to detect multiple pregnancies. This will ensure a consistent approach for gestational assessment and reduce the incidence of the induction of labour for prolonged pregnancy. Lifestyle factors and pregnancy- The NICE guideline regarding antenatal care has an updated section relating to alcohol consumption in pregnancy(4). At the first contact with the pregnant woman staff are encouraged to discuss smoking status, provide information about the risks of smoking to the unborn child and the hazards of exposure to second hand smoke and refer to specialist services (4). This would also include explaining the risk of giving birth to a low weight or pre term baby. Mental health disorders- The updated NICE Antenatal guidelines also note that in all communications (including the initial referral) with maternity services that healthcare professional should include information regarding any relevant history of mental disorder (4). Health professionals should ask at their first contact about past or present severe mental illness including schizophrenia, bipolar disorder, and psychosis in the post natal period and severe depression. After identifying a possible mental disorder in a woman during pregnancy or the postnatal period then further assessments should be considered, in consultation with colleagues if necessary. Date: Feb 2011 Version: 0j Page: 19 of 49 Public Health Wales Maternity services literature review All Maternity Services need to have the appropriate systems in place to provide this level of ante natal care. Because of the unique impact of lifestyle factors on the unborn child, action to support the woman in addressing these issues is particularly importance during pregnancy. A failure to address lifestyle issues during pregnancy can lead to poorer outcomes for both mother and baby which in turn lead to increased costs to the service. 3.4 Supporting women through childbirth Historically women have been attended and supported by other women during labour. However in recent decades in hospitals around the world the continuous support of women through the process of childbirth has become the exception rather than the routine. This has raised concerns that the process of childbirth has become dehumanized, and that modern obstetric care frequently subjects women to institutional routines which may have an adverse effect on the way that labour progresses. A Cochrane collaboration review of continuous support for women during childbirth noted that supportive care during labour may enhance normal labour processes as well as women’s feelings of control and competence and thus reduce the need for obstetric intervention (19). The review included 16 trials from 11 countries, involving over 13,000 women in a wide range of different birth settings and circumstances. The review concluded that women who received continuous labour support were more likely to give birth “spontaneously” i.e. give birth with neither Caesarean nor vacuum nor forceps (19). In addition women were less likely to use pain medication, were more likely to be satisfied, and have slightly shorter labours. In general labour support appeared to be most effective when it was provided by women who were not part of the hospital staff and when support commenced early in labour. The authors of the review suggested that it may be possible to increase access to one to one continuous labour support worldwide by encouraging women to invite a family member or friend to commit to being present at the birth and assume the supportive role. No adverse effects were identified within the review (19). 3.5 Role Definition The following section will therefore go on to clearly define the roles that may be called upon to support a woman through the process of childbirth Date: Feb 2011 Version: 0j Page: 20 of 49 Public Health Wales Maternity services literature review whilst seeking to define each role’s unique contribution to the birth experience. Midwives-it is recognised that regardless of the place of birth that women will be cared for by midwives. The role of the midwife, her function and scope of practice is established in statute and cannot be delegated to anyone else. The midwife has a role in caring for all women in labour irrespective of their risk category or the type of unit in which she is practising (38). Midwives expertise lies in the care of normal childbirth and in their diagnostic skills in identifying deviations from the normal birth experience which can lead to a referral when indicated. When obstetric or other medical involvement is necessary the midwife continues to be responsible for the provision of holistic support to the expectant mother promoting pregnancy and labour as normal physiological processes as far as is possible (38). The role of the midwife immediately after birth encompasses the care of the newborn, with responsibility for newborn resuscitation, the establishment of skin to skin contact, organisation of Vitamin K prophylaxis and the initiation of breastfeeding. Midwives are also responsible for alerting other team members usually paediatricians, to potentially important aspects of maternal or foetal history which may require urgent intervention (38). All midwives have a major public health role and have a key role in teaching and mentoring student midwives, junior doctors and medical students. It is essential that the midwifery establishment reflects this (38, 53). The head of midwifery services provides strategic and organisational leadership, and is accountable for the quality of midwifery services within their organisation (2). The role combines the effective promotion of professional expertise in women and children’s health, overarching responsibility for the operational and strategic general management, Date: Feb 2011 Version: 0j Page: 21 of 49 Public Health Wales Maternity services literature review professional leadership and being an advocate for women. Specific aspects of the role include budgetary control, human resources, strategic planning, clinical governance and quality of midwifery care; this should be reflected in the organisational structure (38). The term consultant midwife is the one which has replaced that of clinical midwife lead and more accurately fulfils the clinical leadership role without managerial responsibilities. The role provides clinical leadership in conjunction with the lead consultant obstetrician and complements the role of head of Midwifery. Consultant midwives contribute to effective leadership, training and mentoring, as well as having specific responsibilities such as promoting normal childbirth or reducing inequalities. Consultant midwives are able to drive service improvement through working with colleagues in health and other agencies to develop effective care pathways or specific services for specific client groups (2). Maternity Support Workers who are appropriately trained and supervised can carry out a range of duties including clerical duties, supporting women with breastfeeding, helping to run parent craft classes and supporting post natal care. Wales has developed a national curriculum for Maternity Support Workers to develop this element of the workforce (53, 54) Specialist Midwives include practice development midwives, lecturer practitioners and antenatal screening coordinators, who effectively contribute to the maternity team and can drive forward enhancements to services (2). The Supervisor of Midwives has a statutory role which is undertaken on behalf of the local supervising authority. A supervisor of midwives is an experienced midwife who has received additional training, who is able to contribute to the development of the maternity strategy. There should be one supervisor of midwives to every 15 midwives and their role is to protect the public through the provision of evidence based midwifery care. Supervisors of midwives should be represented at all local maternity communication forums such as the maternity services liaison committee, risk management, perinatal audit meetings and the labour ward forum and should have a direct line of communication to the executive team. A supervisor of midwives is to be available 24 hours a day and may be contacted by any member of the maternity team for support and guidance (38). Date: Feb 2011 Version: 0j Page: 22 of 49 Public Health Wales Maternity services literature review The Labour ward manager has a crucial role to play in the smooth and efficient management of the labour ward and in providing advice support and guidance. This includes Resource management, ensuring that there is a supportive, positive environment that encourages learning and development of all staff Ensuring a quality service through evidenced based guidelines, a robust risk management framework, safe and effective resourcing of equipment and support systems for mentoring new and junior midwives and students. The Safer childbirth report which provides minimum standards for the organisation and delivery of care in labour suggests that the minimum requirement for a labour ward manager presence is one whole time equivalent (38). To ensure 24 hour managerial cover each labour ward must have a rota of senior midwives as labour ward shift coordinators supernumerary to the staffing requirements for one to one care. Their role is a pivotal one in facilitating clear communication between professionals and in overseeing the appropriate use of resources (38). Student midwives are supernumerary to the midwifery establishment numbers. But as they provide direct care to women, under the mentorship and support of midwives their role in contributing to the care of women cannot be overlooked (38). Obstetricians -The role of the consultant obstetrician on the labour ward is to ensure a high standard of care for women and their babies with complex medical or obstetric needs and to be available for the acute, severe and often unpredictable life-threatening emergencies which are a feature of obstetric practice. There is some evidence linking the absence of consultants from labour wards in the night, with less favourable outcomes (38). The role of the consultant obstetrician on the labour ward is clearly defined in the Safer Childbirth report (38) as Providing clinical leadership and leading by example Training and educating staff in a multi disciplinary team Date: Feb 2011 Version: 0j Page: 23 of 49 Public Health Wales Maternity services literature review Ensuring effective teamwork Developing and implementing standards of obstetric practice and having a major role in risk management Bringing experience to clinical diagnosis Auditing the effectiveness of practice in order to modify it if required. Consultants in obstetrics and gynaecology are increasingly appointed with a special interest to complement the skills of the existing team. Maternity units may benefit from having a person appointed with a consultant lead role in areas such as labour ward management, early pregnancy assessment, diabetes and prenatal diagnosis (2). Subspecialists in feto-maternal medicine work in tertiary centres and have the expertise to provide specialised care for more complex problems and ensure comprehensive care within a network (2). 3.6 Midwife led care In many parts of the world midwives are the main providers of care for childbearing women. Elsewhere medical doctors or family physicians have the main responsibility for care or the care of the woman may be shared between doctors and midwives. The new Maternity Services Strategy for Wales consultation document, supports a greater focus on midwifery led births, and proposes that this care is delivered in a range of settings including home, hospital or midwife led units as appropriate to the needs of the mother and family (54). Midwives should be the lead professional for healthy women with straightforward pregnancies. For women with more complex pregnancies they should act as the key coordinator of care within the multi disciplinary team (53). Midwife–led care has an underpinning philosophy that birth is a normal experience with continuity of care provided to the mother. The mother is supported and cared for by a midwife whom she knows and trusts during labour. There is an emphasis in midwife-led care on the natural ability of women to experience birth with minimum intervention. Some models of midwife-led care provide a service through a team of midwives sharing a Date: Feb 2011 Version: 0j Page: 24 of 49 Public Health Wales Maternity services literature review caseload and this is often described as “team” midwifery (20). Another model of care is “caseload midwifery” where the aim is to provide greater continuity of caregiver throughout the episode of care. Caseload midwifery aims to ensure that the woman receives all her midwifery care from one midwife or her/his practice partner (20). All models of midwife-led care are provided in a multi disciplinary network of consultation and referral with care providers. A Cochrane review of midwife–led versus other models of care for child bearing women compared models of medical led care and shared care, and identified 11 trials involving 12,276 women (20). Midwife-led care was associated with several benefits for women and had no identified adverse effects. The main benefits to women were a reduction in regional analgesia, with fewer episiotomies and instrumental births. Midwife-led care also increased the chance that women were cared through the birth by a midwife that they knew. This increased the chance of feeling in control during labour and of having a spontaneous vaginal birth and initiating breastfeeding (20). However there were no statistically significant differences in Caesarean birth rates. The Cochrane review identified that women who were randomised to receive midwife-led care were less likely to lose their baby before 24 weeks gestation, although there were no differences in the risk of losing the baby after 24 weeks or overall. In addition the babies of women who were randomised to receive midwife-led care were more likely to have a shorter length of hospital stay (20). The review concluded that most women should be offered midwife led models of care, although caution should be exercised in applying this advice to women with substantial medical or obstetric complications (20). Midwifery led care during labour can be delivered through different systems such as home, hospital or in stand alone midwifery led units. The following sections summarise evidence around these different systems of care. Date: Feb 2011 Version: 0j Page: 25 of 49 Public Health Wales 3.6.1 Maternity services literature review Midwifery led Units (MLU) During the past twenty years there has been a policy emphasis on increasing choice in relation to the place of birth. As a result women in England and Wales are able to make a choice between giving birth at home or in hospital. In addition to these two options women in some parts of England and Wales have the additional choice of giving birth in a midwifery led unit which may be geographically separate from or adjacent to, a hospital obstetric unit (21). Midwife led maternity units (MLMU) are units which are organised and run by qualified midwives offering midwifery care to women during the antenatal, intrapartum and postnatal period (22). The units provide an alternative model of care to traditional obstetric led care, and are aimed at women who are considered to be at low risk of developing complications during pregnancy and childbirth. Midwife led maternity units may be located adjacent to or integrated with obstetric led maternity units or they may be freestanding (22). These units are also sometimes referred to in the literature as birth centres. This section will use the term Midwifery led unit and birth centre interchangeably to describe the system of midwifery led care that is delivered in a separate unit that may or may not be geographically separate from or adjacent to, a hospital obstetric unit. The report “Structured review of birth centre outcomes” set out in its review to achieve an overview of the evidence base from published reports about clinical, psychosocial and economic outcomes in developed country settings about women who plan to give birth or had given birth in birth centres (21). The report noted that overall data were of poor quality and derived from small scale observational studies. Outcomes were inconsistently defined and reported with a high likelihood of bias. It was likely that there was a disproportionate publication of positive or negative results (21). The “Structured review of birth centre outcomes” concluded that birth centre care can offer the possibility of accessible, appropriate, personal maternity care for women and their families. There is substantial support for this service from women accessing care, their families and maternity care health professionals as the service is clearly differentiated from an obstetric-led maternity service (21). Date: Feb 2011 Version: 0j Page: 26 of 49 Public Health Wales Maternity services literature review It is important to note however that no reliable evidence about either clear benefit or harm associated with birth centre care compared with any other type of intrapartum care offered in the NHS was identified in the review (21). The review recommends that a large scale pragmatic randomised controlled trial be conducted as a matter of urgency to provide high quality evidence in maternal and neonatal outcomes by place of birth. Walsh and Downe (23) found in their review that women labouring on a MLMU compared to an Obstetric Led Maternity Unit (OLMU) had higher rates of normal vaginal birth and lower rates of caesarean section, demonstrating that women delivering in an MLMU are ideally matched to the remit of a MLMU in terms of risk. Intact perineum rates were found to be high in both MLMU and in OLMU. However episiotomy rates were found to be variable in both types of unit. Failure to progress in the first stage of labour was found to be the main reason for intrapartum transfer to an OLMU (23). Muthu and Fischbacher (24) found in their study that events such as maternal and neonatal morbidity and mortality were rare in both MLMU and OLMU. Pethidine injection and epidural anaesthesia were less common in a MLMU than in an OLMU. Women in a MLMU were more likely to have an intact perineum than those women labouring in an OLMU. These findings may be expected in a MLMU setting where births likely to be less complex. Women were transferred from MLMU to OLMU units in 14-16% of cases and neonates were transferred in up to 4% of cases. Another study evaluating outcomes of the first midwife led centre in Italy found caesarean section rates to be 6.1% (87/1438) and intrapartum transfers were 14.1% (46). Postpartum transfers due to haemorrhage or retained placenta were 2.4%. There were no perinatal deaths. There was one maternal death, but there was no power to calculate a maternal mortality rate due to the sample size of the study (n= 1438). It is important to note that there is ongoing debate in relation to the evidence on the different systems within which care is delivered (47, 48). In 2005, the National Perinatal Epidemiology Unit concluded that more high quality evidence was needed about whether there are important differences in experiences and outcomes for women and babies in these alternative locations and systems (47). Date: Feb 2011 Version: 0j Page: 27 of 49 Public Health Wales Maternity services literature review In response to this, work is currently being undertaken to evaluate maternity units in England. The Evaluation of Maternity Units in England (EMU) is a programme of research designed to examine the role of midwifery led units and generate high quality evidence. The publication date for the review is anticipated to be March 2011. It is anticipated that the findings will add to the evidence base relating to midwife led maternity units. 3.6.2 Home Births The Royal College of Midwives (RCM) and the Royal College of Obstetricians and Gynaecologists (RCOG) support home birth for women with uncomplicated pregnancies (25). Their home births joint statement states that there is no reason why home births should not be offered to women who have a low risk of complication and state that it may confer considerable benefits for them and their families (25). The Royal Colleges report suggests that there is ample evidence showing that labouring at home increases a woman’s likelihood of a birth that is both satisfying and safe. The National Childbirth trust in their briefing document relating to home births (26) suggest that planned home birth is a positive choice for many parents, particularly women who are healthy, have no history of medical conditions or maternity complications and have had a straightforward pregnancy and previous delivery. The National Childbirth Trust argues that being able to access a home birth is important because women have the greatest autonomy in their own home (26). In comparison to the institutional environment which can limit their privacy, intimacy and freedom (26). A review of literature on the place of birth concluded that there is some evidence , although not conclusive that women and their babies do better and women are more satisfied with their care when cared for out of an institutional setting (27). The Department of Health Maternity Standard states that several large studies on home birth have concluded that it appears safe for women who have been appropriately assessed (28). Home births should be offered within a risk management framework with adequate local infrastructure and support (28). Van Weel described risk Date: Feb 2011 Version: 0j Page: 28 of 49 Public Health Wales Maternity services literature review selection as “delicate” (29). One study argues that adverse events may occur if too few or too many women are referred, or if referrals are made too early or too late. If women are not referred in time then perinatal outcomes may be worse in primary midwife led care compared with obstetrician led care. On the other hand unnecessary referrals may increase the risk of unnecessary obstetric interventions (29). A Cochrane Collaboration review (1) of home versus hospital births originally published in 1998 and assessed as up to date in 2006 concluded as follows That there is no strong evidence to favour either planned hospital birth or planned home birth for low risk pregnant women. That there is no strong evidence about the benefits and safety of planned home birth compared to planned hospital birth for low risk pregnant women. The change to planned hospital birth for low risk pregnant women in many countries during this century was not supported by good evidence Planned hospital birth may even increase unnecessary interventions and complications without any benefit for low risk women (1) The Royal College of Obstetricians and Gynaecologists do support home births in cases of low-risk pregnancies provided the appropriate infrastructures and resources are present to support such a system. It is however important to note that the issue of home births remains a contested one and the American, Australian and New Zealand colleges of obstetricians and gynaecologists oppose home birth. However the Royal College of Midwives in the United Kingdom, Australia New Zealand and Canada all support home birth in uncomplicated pregnancy (32). The rate of home births within the U.K remains low at approximately 2% (33-35) but it is believed that if women had true choice the rate would be around 8-10% (36). Date: Feb 2011 Version: 0j Page: 29 of 49 Public Health Wales Maternity services literature review It has been argued that the development of maternity policies over the last four decades combined with the regular reorganisation of service structures have impacted on the availability of home birth to the point that birth is now focused in hospital settings (25). The Royal College of Obstetricians and Gynaecologists suggest that reasons for this appear to include Financial constraints The values and beliefs of organisations about maternity care A lack of staff with the appropriate competencies (25) In any discussion about home birth it is important to distinguish between women who plan for a home birth and those who have an unintended home birth, as unintended home births and/or women who received no antenatal care are linked to a higher rate of both maternal and perinatal complications (37). A proportion of women who plan for home birth are transferred to hospital most commonly for slow progress or needing pain relief not available at home, such as epidural anaesthesia (25). The Royal College of Obstetricians and Gynaecologists state that women need to be counselled on the unexpected emergencies (such as cord prolapse, foetal heart rate abnormalities, undiagnosed breech, prolonged labour and postpartum haemorrhage) which can arise during labour and can only be managed in a maternity hospital (31). Such emergencies would always require the woman to be transferred to a hospital by ambulance as extra medical support is only present in hospital settings and would not be available to them when they deliver at home (31). 3.7 Evidence from the Netherlands Several studies have been conducted to evaluate the obstetric system in Netherlands, which has a different system of maternity care to the UK. Women are assessed as either high or low risk with low risk women giving birth at home or in primary care under supervision of midwives, and high risk women delivering in hospital under supervision of obstetricians. There is conflicting evidence from these studies on outcomes and perinatal mortality in relation to place of birth and travel times to hospital. This Date: Feb 2011 Version: 0j Page: 30 of 49 Public Health Wales Maternity services literature review section summarises some of the evidence on the maternity system in the Netherlands. One study from the Netherlands undertook an analysis of 529,688 low risk women who were in primary midwife led care at the onset of labour (30). The study analysed national perinatal and neonatal registration data over a period of seven years. This study concluded that planning a home birth does not increase the risks of perinatal mortality and severe perinatal morbidity among low risk women. This is provided that the maternity care system facilitates this choice through the availability of well trained midwives, and through a good transportation and referral system (30). A very recent study from the Netherlands conflicts these findings (49). The Netherlands have an obstetric system which classifies women into low and high risk categories. Low risk women receive midwife led care in primary care or at home and high risk women receive consultant led care in hospital. This prospective study found that infants of pregnant women at low risk whose labour started in primary care under the supervision of a midwife had a higher risk of delivery related perinatal death and the same risk of admission to the NICU compared with infants of pregnant women at high risk whose labour started in secondary care under the supervision of an obstetrician. The authors note the study used an aggregated large birth registry database and could not adjust for confounders, which was a key limitation. However they note that this was a surprising finding that conflicts findings from other similar studies on the Netherlands’ maternity care system and requires further evaluation. A further recent large registry based cohort study from the Netherlands which evaluated the effect of travel times at the start of and during labour from home to hospital found that a travel time from home to hospital of 20 minutes or more by car is associated with an increased risk of neonatal mortality and adverse outcomes in women at full term (50). This finding conflicts two UK studies, which found no association between adverse outcomes and increased travel time to the nearest or second nearest healthcare facility (51, 52), although sample sizes in these studies were much smaller. A strength of the Netherlands study is that a large registry database was used (n751 926) and the study did control for some confounders. However there were some key confounders that were not controlled for such as body mass index and smoking, it is therefore not possible to exclude the possibility that residual confounding could explain some of the statistically significant results in the study. The authors note Date: Feb 2011 Version: 0j Page: 31 of 49 Public Health Wales Maternity services literature review that further research is needed to investigate the policy implications of the findings of this study. When considering the evidence from the Netherlands, it is important to note that the system of maternity care is very different to the UK and this may limit the generalisability of the findings to the UK setting. 4 Safer Childbirth Maternity care can range from looking after women through a very natural birth process with little medical intervention through to highly technical emergency care which has more in common to the services provided by an accident or emergency department or intensive care unit. The King’s Fund Safe Births report noted that nowhere have the negative aspects of patient safety been more emphasised than in maternity services, which have been subject to frequent reviews often accompanied by media commentary. Pregnancy and birth are normal physiological processes but the transition from routine to emergency can occur rapidly and unexpectedly. Because pregnancy and birth do not normally involve ill health, the expectation of safety is particularly high and the obligation of the health system to do no harm is an even higher imperative than normal (8). Safety is more than focusing on recording, investigating, and analysing failure. It also has the dimension of striving to maintain a system that is geared to success. The King’s Fund report succinctly describes safety being as much a matter understanding how success is achieved as of understanding how failure happened (8). Clinical and managerial leaders at all levels have important roles to play in ensuring patient safety. They can be proactive in promoting safer practice, monitoring standards of care and improving safety measures where necessary (8). The King’s Fund Safe Births report (8) identified that the skills required to lead maternity teams at different levels need to be clearly defined. The development of shared objectives and a shared understanding of roles may offer a means of promoting effective team working within maternity service. Date: Feb 2011 Version: 0j Page: 32 of 49 Public Health Wales 4.1 Maternity services literature review What should a Birth Setting look like? A good working relationship between the multidisciplinary team made up of medical ancillary and managerial staff and the women for whom they care is crucial to ensure optimal birth outcomes (38). The “Safer Childbirth” report suggested this is best achieved with a team approach based on mutual respect, a shared philosophy of care and a clear organisational structure for both midwives and medical staff with explicit and transparent lines of communication (38). The minimum standards for the organisation and delivery of care in labour in relation to the senior management of an acute unit are set out in the “Safer Childbirth” report (38). Safer childbirth highlights the importance of the environment in which women give birth. Facilities in all settings should be at an appropriate standard and take account of the woman’s needs by being less clinical, non threatening and more like home wherever possible (38). Facilities should be audited and reviewed every two years. 4.2 Guidance on decision to delivery intervals for emergency caesarean section A decision to delivery interval describes the time between an obstetrician in a consultant led unit deciding that a caesarean section should be undertaken and the delivery. The National Institute for Clinical Excellence clinical guidelines relating to caesarean section (39) state that emergency Caesarean section delivery for maternal or foetal compromise should be accomplished as quickly as possible. This is reflected in the guidelines on electronic foetal monitoring as cited in the report of the National Collaborating Centre for Women’s and Children’s Health (40). The NICE clinical guidelines for caesarean section do however take into account that rapid delivery has the potential to do harm (39). However the most compromised babies are most predisposed to poorer outcomes and are also often delivered with the least delay and this confounding needs to be taken into account when assessing the effects of a rapid delivery (41). Date: Feb 2011 Version: 0j Page: 33 of 49 Public Health Wales Maternity services literature review A decision to delivery interval (DDI) of less than 30 minutes is not in itself critical in influencing baby outcome, but has been an accepted standard for response to emergencies within maternity services (39). The evidence on this audit standard is mixed. The National Sentinel Caesarean Section report produced by the Royal College of Obstetricians and Gynaecologists (42) noted that in some cases the priority of ensuring maternal safety may conflict with concerns about the baby. Delivery should be accomplished as far as possible without endangering the condition of the mother. Rapid decision making has the potential to cause adverse effects and the report acknowledges that rapid decision making in stressful circumstances may generate anxiety for all involved (42). Delays in delivery can possibly associate with poor outcomes. Delays have been attributed to poor communication and the sentinel report acknowledges that rapid and precise communication between health professionals may reduce delays (42). The good practice guidance developed by the Royal College of Obstetricians and the Royal College of Anaesthetists suggested that in certain cases such as cord prolapse a DDI of 15 minutes was feasible (43). The guidance goes on however, to suggest that in certain circumstances, delivery within 75 minutes does not appear to raise the risk of compromise, while delivery within 30 minutes may not always result in a good neonatal outcome (43). Once a decision to deliver has been made delivery should be carried out with urgency appropriate to the risk to the baby and the safety of the mother. Units should strive to design guidelines that result in the shortest safely achievable DDI. Undue haste to achieve a short DDI can introduce its own risk, both surgical and anaesthetic with the potential to cause harm to either the mother or baby (43). It is suggested that the speed of intervention is only one aspect to be considered, and that the anticipation and identification of early threatening conditions for both baby and mother were important (44). Date: Feb 2011 Version: 0j Page: 34 of 49 Public Health Wales Maternity services literature review 5 Recommendations literature arising from the 5.1 Recommendations for the Maternity Service for Wales The report “A Maternity Service for Wales” (10) sought to provide maternity service planners with a consensus view from the lead professional groups on what issues need to be taken into consideration. The recommendations made fall under two broad headings: Service Reconfiguration The Multidisciplinary Professional Project Group recommended that the ultimate goal should be the development of a sustainable, safe service which is acceptable to the users: pregnant women and their families. Therefore where service mergers are proposed, professional advice should be sought at the planning stage from all the Royal Colleges and advisory groups involved. The group also recommended that the “Standards for Maternity Care” hosted and published in 2008 by the Royal College of Obstetricians and Gynaecologists’ for all maternity speciality groups should set the standard for any change in care structures (10). When service changes have been made they should be monitored regularly against the Joint Colleges’ standards for Maternity Care. Training The Maternity Service for Wales report (10) recommended that the impact of a merger, closure, or service change to a unit on other providers be considered with especial regard to training. The maternity service should allow for high quality training of those medical specialists who will be providing services in the future The Midwifery 2020 Delivering Expectations report (45) as part of its vision for midwifery training states that midwifery education will be rooted in normality whilst preparing midwives to care for all women including those with complex medical, obstetric and social needs. It will prepare and develop midwives to be skilled and safe, empathic and trustworthy with Date: Feb 2011 Version: 0j Page: 35 of 49 Public Health Wales Maternity services literature review increased emphasis on the principles of autonomy and accountability within multidisciplinary and multi agency teams. 5.2 Recommendations for the New Local Health Boards from the Wales Audit Office Maternity Services report The Wales Audit Office report “Maternity Services” (5) made a series of recommendations directed at the new Local Health Boards in Wales. Staffing The new LHBs need to strengthen the consultant job planning process in order to clearly identify the consultant time spent on obstetrics as opposed to gynaecology. This improvement would help ensure that Boards have appropriate consultant cover. Where the presence of consultant obstetricians on delivery suites fall below recommended levels that the new LHBs should undertake an adequacy assessment of their consultant staffing requirements for delivering safe and high quality services. Where midwifery staffing levels fall below recommended levels the new LHBs should undertake an assessment of the adequacy of their staffing requirements for delivering safe and high quality services That the new LHBs review whether they have sufficient numbers of maternity support workers in order to release midwives to focus on the more specialist care and treatment, and to support the national training programme to ensure all support workers have all the appropriate skills. Training That the new LHBs ensure that all maternity services staff are trained to the required level. That the training programmes implemented by LHBs should be reviewed in order to ensure a sufficient focus on the principles of respect, well being, choice and dignity for women. Date: Feb 2011 Version: 0j Page: 36 of 49 Public Health Wales Maternity services literature review The Woman’s Experience That the new LHBs work harder to gather the views of service users and consider the views expressed when planning services. That the LHBs promote midwives as the most appropriate first point of access for pregnant women, and publicise broadly the services available locally That the new LHBs should review their processes for deciding on the appropriate number of ante natal check ups to ensure this is based on need and evidence based standards. That LHBs should explore the reasons behind low attendance at ante natal classes, and that information gained from surveys should be acted upon in order to give every woman an opportunity to attend classes if they wish. In order to improve care during labour and birth that processes are put into place by LHBs to ensure that women’s preferences for pain relief are formally recorded by the clinicians caring for them. That the new LHBs should provide locally accessible community locations that can function as antenatal drop-in centres run by midwives. That the new LHBs carry out local audits to assess the appropriateness of their caesarean rates including a comparison rate between individual consultants. Where high rates are identified that the Caesarean toolkit developed by the NHS Institute for Innovation and Improvement which aims to reduce section rates be implemented That the LHBs should ensure that the necessary support is available to support women to breastfeed and that the advice and support provided is consistent. Safety In order to improve safety the Wales Audit Report recommended that the LHBs standardise the criteria for incident reporting by promoting a culture of openness and by putting into place mechanisms for learning from incidents That the recommendations contained within the Welsh Risk Pool Maternity Project should be implemented by LHBs as they address the problems in the use of electronic foetal monitoring that is a Date: Feb 2011 Version: 0j Page: 37 of 49 Public Health Wales Maternity services literature review common feature in a large number of high-value obstetric clinical negligence claims Acknowledgments The authors would like to acknowledge the invaluable contribution from Dinah Roberts and Ken Jones from the Public Health Wales’ Library Knowledge and Management Service in the development of this report 6 Appendix: Search Strategy Main search: maternity services Additional searches: emergency caesarean section; transfer times; home births Topic: Maternity services Search question: What is the current evidence base on best practice in relation to the delivery of safe and sustainable maternity services? By: Dinah Roberts Date : 3 August 2010 Updated: 18 August 2010 Methodology Search terms :-Keywords, Free text Models of service Service models Service delivery Service provision Service redesign Service reconfiguration Service rationalisation Models of care Access to services Provision of services Maternity services Maternity hospitals Hospitals, maternity Obstetric led maternity units OLMU Maternal health services Maternity health services Maternity units Maternity wards MMU Date: Feb 2011 Version: 0j Page: 38 of 49 Public Health Wales Maternity services literature review Midwifer* –led units Midwife-led birth centre* MLMU Designated midwifery unit Local maternity care Birthing centres Intra-partum Pregnancy services Ante-natal services MESH HMIC BNI Obstetric and Gynecology Department, Hospital maternity health services/ma/og/st/tr/ut Maternal health services Maternal care Maternity clinics Maternity units General practitioner maternity units Obstetric clinics Obstetric care Midwifery services Change management Health provision Health service development Health service delivery Health service evaluation Health service management Health service organisation Health service planning Health service utilisation "hospital planning and design" Models Nursing models Organisational change Patient safety Service delivery Service demand Service development Service needs Service planning Service relocation Service standards Service utilisation Staffing levels Unit management Ward organisation Workforce Workforce planning Publication types Database searches filter = Systematic reviews, RCTs, Meta analysis , reviews Limitations Language Date: Feb 2011 English only Version: 0j Page: 39 of 49 Public Health Wales Maternity services literature review Dates covered/period of publication 2000- Exclude Include Developing countries Topic: Emergency caesarean section Search question: What is the current evidence base on decision-to-delivery time of 30mins in emergency caesarean section? By: Sian King, LKMS Swansea Date : 27/09/10 Methodology Search terms headings, :-Keywords, HMIC, BNI MESH Publication types Limitations Language Dates covered/period of publication Non UK Date: Feb 2011 subject Caesarean adj2 emergenc* C$esarean adj2 emergenc* Caesarean section Caesarian section (BNI) Birth delivery Emergencies Emergency care Emergency surgery Labour: complications Labor complications (CINAHL) Obstetric emergencies Decision making Clinical decision making Medical decision making Time Cesarean section Emergency care Emergency surgery Emergency treatment Emergencies Decision making Time factors Systematic reviews, reports, guidelines, articles English 2000-2010 Yes Version: 0j Page: 40 of 49 Public Health Wales Maternity services literature review Topic: Maternity services Transfer times from midwifery led units to consultant led unit in relation to obstetric emergencies and maternal/neonatal outcomes? Search question: By: Dinah Roberts Date : 29 September 2010 Topic: Home births Search question: What are the increased risks associated with home births compared to hospital births? By: Sian King, LKMS Swansea Date : 07/10/10 Methodology Search terms :-Keywords, Free text MESH HMIC BNI etc Publication types Limitations Language Date: Feb 2011 Home birth$ Home adj2 birth$ Home childbirth Pregnancy Outcome Pregnancy, High Risk Risks Risk factors Patient transfer Home confinement Home delivery Confinement: Place (BNI) Birth delivery Fetus risk Risks Adverse outcome Clinical outcomes Fetal outcomes Health outcomes Outcomes and prognoses Outcomes Pregnancy outcome Pregnancy: complications Labour: complications Labor complication(s) Patient safety Systematic reviews, reports, guidelines, articles English Version: 0j Page: 41 of 49 Public Health Wales Maternity services literature review Dates covered/period of publication Other limitations 2000-2010 Exclude Include Developing countries Personal experience stories 2. Sources (i.) Core databases/sources BNI CINAHL Clinical Evidence Pre 2000 included Cochrane Library √ EMBASE HMIC MEDLINE NICE √ Library catalogue & knowledge base √ PsycINFO X (ii.) Topic specific databases, sources Databases Child data MIDIRS X POPLINE Map of medicine Department of Health (inc: Children, Young People & Services) NSF for Maternity Department for Health & Children [Ireland] Department of Health, Social Services & Date: Feb 2011 Version: 0j Page: 42 of 49 Public Health Wales Maternity services literature review (ii.) Topic specific databases, sources Public Safety [NI] NHS Institute Improvement for Innovation and NHS Quality Improvement Scotland (inc. Findings – CH & Maternity Services & Reproductive health) NHS Scotland NHS Quality Improvement Scottish Government (for Services Action Group reports) Maternity Welsh Assembly Government (inc: NSF for Children, Young People & Maternity Services) CMACE (Centre for Maternal and Child Enquiries) √ NPSA NIHR-SDO √ Health select Committee √ Welsh Audit Office √ National Audit Office National Perinatal Epidemiology Unit Maternity Evidence Birmingham] √ [University of √ King’s Fund – maternity topic National Collaborating Centre for Women's and Children's Health NHS Evidence (specialist collections) - health management – Maternity services √ Royal College of Midwives Royal College of Paediatrics & Child Health Royal College Gynaecologists of Obstetricians & √ Royal College of Surgeons Date: Feb 2011 Version: 0j Page: 43 of 49 Public Health Wales Maternity services literature review (ii.) Topic specific databases, sources AIMS (Association for Improvements in the Maternity Services) European Foundation Newborn Infants for the Care of MARCH (Centre for Maternal Reproductive and Child Health) Maternity Action National Childbirth Trust National Maternity Support Foundation Independent Midwives Association Warwick Infant and Family Wellbeing Unit Child Health and Maternity Partnership CHAMP *** ChiMat √ Maternity Liaison Committees International Gyn. (iii) Meta search engines Federation of Obstetrics and Google/Google Scholar √ √ Intute SUMsearch TRIP Date: Feb 2011 Version: 0j Page: 44 of 49 Public Health Wales 7 Maternity services literature review Reference List (1) Olsen O, Jewell D. Home versus hospital birth. Cochrane Database of Systematic Reviews 2009;Art. No.: CD000352. DOI: 10.1002/14651858.CD000352(3). (2) Department of Health. Maternity Matters: Choice,access and continuity of care in a safe service. London: Department of Health; 2007. (3) Healthcare Commission. Towards better births; A review of maternity services in England. Healthcare Commission; 2007. (4) National Institute for Health and Clinical Excellence. Antenatal Care. NICE; 2008. Report No.: Clinical guideline CG62. (5) Coleman J, Body G, Davies T, Lisle S. Maternity Services. Wales Audit Office; 2010 Jan. (6) Confidential Enquiry into Maternal and Child Health (CEMACH). Why Mothers Die 2000-2002: Sixth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. London: CEMACH; 2004. (7) Greenacre J. The health and social circumstances of children in Wales. Cardiff: National Public Health Service for Wales; 2004 Jan. (8) The King's Fund. Safe Births: Everybody's business. London: The King's Fund; 2008. (9) World Health Organization. European strategic approach for making pregnancy safer: Improving maternal and perinatal health. World Health Organisation; 2008. (10) Welsh Medical Committee. A Maternity Service for Wales. 2010. (11) Dartnall L, Ganguly N, Baatterham J. Access to Maternity Services: Research Report. Department of Health; 2005 Jan. (12) National Institute for Health and Clinical Excellence. Pregnancy and Complex Social Factors. NICE; 2010. Report No.: Clinical guidelines CG110. (13) Clement Jones M., Scholefield H. Obstetrics:what we need in the future. British Journal of Hospital Medicine 2008;69(2):81-3. Date: Feb 2011 Version: 0j Page: 45 of 49 Public Health Wales Maternity services literature review (14) Royal College of Obstetricians and Gynaecologists. The Future Role of the Consultant. London: RCOG; 2005. (15) Healthcare Commission. Investigation into 10 maternal deaths at, or following delivery at Northwick Park Hospital, North West London Hospitals NHS Trust between April 2002 and April 2005. London; 2006. (16) Royal College of Obstetricians and Gynaecologists, Royal College of Midwives. Towards Safer Childbirth: Minimum Standards for the Organisation of Labour Wards. London: RCOG/RCM; 1999. (17) Arulkumaran S, Wells M. Lessons learnt from the reorganization of maternity services. British Journal of Hospital Medicine 2008;69(2):74-7. (18) Royal College of Obstetricians and Gynaecologists. Maternity Dashboard :Clinical Performance and Governance Score Card. 2008. Report No.: Good Practice No. 7. (19) Hodnett ED, Gates S, Hofmeyr GJ, Sakala C. Continuous support for women during childbirth. Cochrane Database of Systematic Reviews 2007;Reviews 2007(3). (20) Hatem M, Sandell J, Devane D, Soltani H, Gates S. Midwife-led versus other models of care for childbearing women (Review). The Cochrane Database of Systematic Reviews 2009;Reviews 2008(4). (21) Stewart M, Mc Candlish R, Henderson J, Brocklehurst P. Report of a structured review of birth centre outcomes. Oxford: National Perinatal Epidemiology Unit; 2004. (22) NHS Quality Improvement Scotland. Safety and risk associated with free standing midwife led maternity units (MLMU). 2007. Report No.: Evidence Note 18. (23) Walsh D, Downe SM. Outcomes of free standing, midwife led birth centres: a structured review. Birth 2004;31(3):222-9. (24) Muthu V, Fischbacher C. Free standing midwife-led maternity units: a safe and effective alternative to hospital delivery for low risk women? Evidence Based Health Care and Public Health 2004;8(6):325-31. (25) Royal College of Obstetricians and Gynaecologists, Royal College of Midwives. Home Births: Joint Statement No 2. 2007. (26) National Childbirth Trust. Home Birth. National Childbirth Trust; 2008. Date: Feb 2011 Version: 0j Page: 46 of 49 Public Health Wales Maternity services literature review (27) Henderson J, Davidson L, Chapple J, Garcia J, Petrou S. Pregnancy & Childbirth. Health care needs assessment: The epidemiologically based needs assessment reviews. 3rd series ed. 2000. p. 769. (28) Department of Health. Maternity Standard, National Service Framework for Children, Young People and Maternity Services. 2004. (29) van Weel C, van der Velden K, Lagro-Janssen T. Home births revisited: the continuing search for better evidence. British Journal of Obstetrics and Gynaecology 2009;116(9):1149-50. (30) de Jonge A, van der Goes BY, Ravelli ACJ, Amelink-Verburg MP, Mol BW, Nijhuis JG, et al. Perinatal mortality and morbidity in a nationwide cohort of 592,688 low risk planned home and hospital births. British Journal of Obstetrics and Gynaecology 2009;116(9):1177-84. (31) Royal College of Obstetricians and Gynaecologists. RCOG statement on the paper on perinatal mortality and morbidity rates by de Jonge and published in BJOG on 15 April 2009. 2009. (32) Mc Lachlan H, Forster D. The safety of home birth: Is the evidence good enough? Canadian Medical Association Journal 2009 Jan;181(6-7):359-60. (33) Department of Health. The National Service Framework for Children and Young People Maternity Services. Standard 11. London: Department of Health; 2004. (34) Scottish Executive. A Framework for Maternity Services in Scotland. Edinburgh: Scottish Executive; 2001. (35) Welsh Assembly Children's Health and Social Care Directorate. National Service Framework for Children Young People and Maternity Services in Wales. Cardiff: Welsh Assembly Government; 2005. (36) Department of Health. Changing Childbirth: Report of the Expert Maternity Group. London: HMSO; 2003. (37) Maternal and Child Health Research Consortium. Confidential Enquiry into Stillbirths and Deaths in Infancy. 5th Annual Report Focus Group Place of Delivery. London; 1998. (38) Working Party of the Royal College of Obstetricians and Gynaecologists. Safer Childbirth: Minimum Standards for the Organisation and Delivery of Care in Labour. RCOG; 2007. Date: Feb 2011 Version: 0j Page: 47 of 49 Public Health Wales Maternity services literature review (39) National Institute for Clinical Excellence. Caesarean Section. NICE; 2010. Report No.: Clinical Guideline 13. (40) National Collaboration for Women and Children's Health. Caesarean Section. 2004. (41) Thomas J, Paranjothy S, James D. National cross sectional survey to determine whether the decision to delivery interval is critical in emergency caesarean section. British Medical Journal Online First 4 A.D. March 15bmj.38031.775845.7C (42) Clinical Effectiveness Research Unit of Royal College of Obstetricians and Gynaecologists. The National Sentinel Caesarean Section Report. Royal College of Obstetricians and Gynaecologists; 2001. (43) Royal College of Obstetricians and Gynaecologists, Royal College of Anaesthetists. Classification of Urgency of Caesarean Section- a Continuum of Risk. 2010. Report No.: Good practice No. 11. (44) Huissoud C, Dupont C, Canoui Poiytrine F, Touzet S, Dubernard G, Rudigoz RC. Decision to delivery interval for emergency caesareans in the Aurore perinatal network. European Journal of Obstetrics, Gynaecology, and Reproductive Biology 10 A.D.;149(2):159-64. (45) UK Chief Nursing Officers. Midwifery 2020 Delivering Expectations. London: Department of Health; 2010 Sep 9. (46) Morano S, Fiorenza C, Mistrangelo E, Pastorino D, Benussi M, Constantini S, Ragni N. Outcomes of the first midwife-led birth centre in Italy: 5 years' experience. Arch Gynecol Obstet 2007, 276: 333-337 (47) Page L, Drife J. Do we have enough evidence to judge midwife led maternity units safe? BMJ 2007, Vol 335, 642- 643 (48) Tuffnell D. Place of delivery and adverse outcomes. BMJ 2010; 341: c5560 (49) Congenital Anomaly Register and Information Service for Wales. CARIS Review 2010. http://www.wales.nhs.uk/sites3/home.cfm?OrgID=416 (50)Ravelli ACJ, Jager, KJ, de Groot MH, Erwich JJHM, Rijninks-van Driel GC, Tromp M, Eskes M, Abu-Hanna A, Mol BWJ. Travel time from home to hospital and adverse perinatal outcomes in women at term in the Netherlands. BJOG 2010;1-9 (51) Dummer TJ, Parker L. Hospital accessibility and infant death risk. Arch Dis Child 2004;89:232-4 Date: Feb 2011 Version: 0j Page: 48 of 49 Public Health Wales Maternity services literature review (52) Parker L, Dickinson HO, Morton-Jones T. Proximity to maternity services and stillbirth risk. Arch Dis Child Fetal Neonatal ed 2000;82:F167-8 (53) Midwifery 2020 Programme. Midwifery 2020: Delivering Expectations. Sept 2010 (54) Welsh Assembly Government. A Strategic vision for Maternity Services in Wales Draft Strategy Document. Consultation January 2011 Date: Feb 2011 Version: 0j Page: 49 of 49