Beth Bailey, PhD: “Prematurity and Low Birth Weight in Appalachian
advertisement

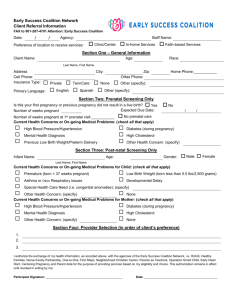
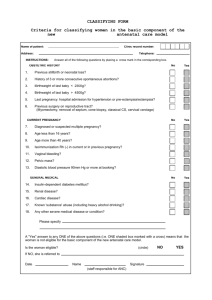
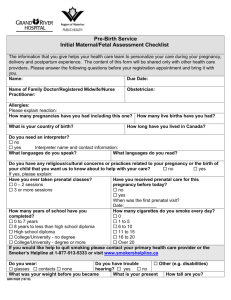
Beth Bailey, PhD: “Prematurity and Low Birth Weight in Appalachian Tennessee: The Roles of Smoking and Domestic Violence” Pregnancy smoking, intimate partner violence (IPV), and low birth weight and prematurity are thought to occur at exceptionally high rates in Northeast Tennessee. This project examined the prevalence of pregnancy smoking and intimate partner violence (IPV) in a Southern Appalachian sample, as well as the rates of adverse newborn outcomes. Of interest were the associations among these variables. The ultimate aim of the project was to develop evidence-based recommendations for the design of prenatal interventions to reduce the incidence of poor newborn outcomes in Northeast Tennessee. The following disparities were the focus of this project: 1. Pregnancy Smoking – Nationally, 11.4% of pregnant women in the United States are smokers. In Tennessee, the rate is 17.1%, the second highest in the nation. In the 6-county area in Northeast Tennessee, pregnancy smoking rates range from 23.2% to 39.0%. 2. Pregnancy IPV – Estimates of IPV during pregnancy range from around 15% for physical violence and as high as 36% for psychological victimization. Many reports suggest that rural women, and women in Appalachia in particular, may be at significantly increased risk of pregnancy IPV. Pilot data from a project in Bristol revealed that 70% of pregnant patients were experiencing psychological abuse, while 25% reported physical violence. 3. Preterm Births and Low Birth Weight – In the U.S., preterm births account for 12.1% of live births. Rates in Tennessee are higher, at 13.8%, the fifth highest rate in the nation. Low birth weight births (LBW) account for 7.8% of births nationally. The rates of LBW births are 18% higher in Tennessee (9.2%), which represents the sixth highest rate in the nation. Pilot data from a project in Bristol revealed that nearly 20% of births are preterm or LBW. Eighty-five women receiving prenatal care at a family practice center in Bristol, TN participated in the project. Women were interviewed during their third trimester, and practice and hospital/newborn medical records were reviewed. Project findings related to these disparities include: 1. Pregnancy Smoking – 65% of the participants entered prenatal care as smokers, with 49% continuing to smoke during pregnancy. Thus, the pregnancy smoking rate was 4.3 times the national average. 2. Pregnancy IPV – 70% of participants reported some type of psychological victimization at the hands of an intimate partner during pregnancy, with 35% reporting some type of physical violence during pregnancy. Thus, the rate of psychological victimization in the current sample was twice that reported in other studies. The rate of physical victimization was 2.3 times that reported in other studies. 3. Preterm Births and Low Birth Weight – 15.7% of the births to participants were preterm, while 10.8% were LBW. Thus, significantly increased rates of both prematurity and LBW were evident in the current sample. This is especially troubling since all participants were deemed to have pregnancies of low medical risk upon entry into prenatal care. 4. Other important findings - Both pregnancy smoking and IPV were associated with multiple adverse newborn outcomes. Babies born to smokers and women experiencing violence were at significantly increased risk for LBW, preterm birth, decreased birth head circumference, the need for oxygen at birth, decreased Apgar scores, and increased length of hospital stays. Additionally, pregnancy smoking and IPV were associated in that women who experienced IPV during pregnancy were significantly less likely to quit smoking during pregnancy than women not experiencing IPV. 5. As a result of project findings, the following recommendations were developed: a. Due to the exceptionally high rates of pregnancy smoking, much more needs to be done in the region to decrease this negative health behavior b. A reduction in pregnancy smoking in the region will likely lead to improved newborn outcomes, increasing the health of children in the region, and decreasing health care costs c. In order to be successful, efforts to help women stop smoking must also address life stressors such as intimate partner violence. A. Peer Reviewed Publications in Professional Journals 1. Bailey B. Factors predicting pregnancy smoking in Southern Appalachia. American Journal of Health Behavior, 30(4), 413-421, 2006. 2. Bailey B, Byrom A. Factors predicting birth weight in a low-risk sample: The role of modifiable pregnancy health behaviors. Maternal and Child Health Journal, 11(2), 173-179, 2007. 3. Bailey B, Daugherty RA. Intimate partner violence during pregnancy: Incidence and associated health behaviors in a rural population. Maternal Child Health Journal, in press. 4. Bailey B. IPV assessment in clinical settings: Finding the most valid measure. Manuscript in progress. 5. Bailey B. Smoking and health during pregnancy. In Smoking and Women’s Health Research, in preparation. B. National Professional Conference Presentations 1. Bailey B. Factors predicting smoking cessation during pregnancy: Results from a rural cohort with a high smoking prevalence. Society for Research on Nicotine and Tobacco annual meeting, February 2006, Orlando, FL. 2. Bailey B, Daugherty RA. Pregnancy smoking cessation: The role of intimate partner violence. Society for Research on Nicotine and Tobacco annual meeting, February 2007, Austin, TX. 3. Bailey B, Daugherty RA. Pregnancy smoking and intimate partner violence. To be presented at the National Conference on Tobacco or Health, October 2007, Minneapolis, MN. 4. Bailey B, Daugherty RA. Maternal health and health behavior disparities in Southern Appalachia. To be presented at Community Connections: Using Research Results to Reduce Health Disparities, June 2007, Wintergreen, VA. 5. Bailey B. Prematurity and low birth weight in Appalachian Tennessee: The roles of smoking and domestic violence. To be presented at Community Connections: Using Research Results to Reduce Health Disparities, June 2007, Wintergreen, VA. C. Regional/Local Professional Conference Presentations 1. Bailey B, Daugherty RA. Intimate partner violence during pregnancy: Incidence and associated health behaviors in a rural population. Presented at Primary Care Research Day, Johnson City, TN, September 2006. 2. Bailey B, Daugherty RA. Maternal health and health behaviors: Disparities in Northeast Tennessee. Presented at Primary Care Research Day, Johnson City, TN, September 2006. 3. Daugherty RA, Bailey B. Are Appalachian obstetric patients receiving adequate breastfeeding education? Presented at Primary Care Research Day, Johnson City, TN, September 2006, and at the Women’s Health Across the Lifecycle Conference, Johnson City, TN, February, 2007. 4. Daugherty RA, Bailey B, Click I. Pregnancy depression in Appalachia. Presented at Primary Care Research Day, Johnson City, TN, September 2006, and at the Women’s Health Across the Lifecycle Conference, Johnson City, TN, February, 2007. D. Dissemination to Community Members (i.e. defining health care professionals as the “community”) 1. “Smoking and Domestic Violence During Pregnancy: Results and Recommendations from Research at Bristol Family Practice Center.” Noon conference presentation on 3/9/06 at Bristol Family Practice Center. Attended by 38 health care professionals (faculty physicians and psychologists, family medicine residents, and nursing staff). Feedback from attendees focused on their need and request for additional training and support in the areas of pregnancy smoking cessation and domestic violence (see 2 below; also provider training was subsequently incorporated into later funding requests) 2. “Prenatal Care Didactic: Learning the 5 A’s.” Half day training session teaching a brief intervention for smoking cessation on 7/13/06 at Bristol Family Practice Center. Attended by 32 faculty, residents, and nursing staff from ETSU family medicine sites, as well as 2 members of the Regional March of Dimes Program Services Committee, and 4 Sullivan County Health Department Staff. This training was offered in response to (1) above. Attendees provided considerable feedback on practical implementation of the 5 A’s and the need for someone to work more intensively with the pregnant women that they provide prenatal care to. This suggestion led to the incorporation of a request for support for case managers in all future related funding requests. 3. Report to the March of Dimes. This was a presentation to the Regional March of Dimes Program Services Committee on the project and the findings (MOD funded the prenatal case manager who assisted with project data collection) on 8/23/06. Attendees included health department workers, neonatal nurses, NICU family members, ETSU nursing faculty, and other health professionals. Most noteworthy feedback from this session was that larger-scale smoking cessation interventions are needed in this area, and that such interventions need to coordinate with existing services (ex: quit lines, other health department services). These suggestions were incorporated into subsequent requests for funding. 4. OB-GYN Grand Rounds. Findings, recommendations, and the recently funded intervention project will be presented at ETSU OB-GYN Grand Rounds on August 22, 2007 at the Center for Women’s Health Labor and Delivery conference room. Expected attendees are OB-GYN faculty, residents, and medical students, as well as labor and delivery and NICU nurses. 5. Psychiatry Grand Rounds. Long-term psychiatric effects of prenatal tobacco exposure will be presented at ETSU Psychiatry Grand Rounds in December 2007. Expected attendees are Psychiatry and psychology faculty, residents, medical students, psychology interns, and other interested professionals 6. Northeast Tennessee Regional Health Council. The findings of this project and the newly funded intervention/evaluation project will be presented to this group on 4/9/2007. Expected attendance will be approximately 35 community health leaders from 8 counties in Northeast Tennessee. 7. Project findings and recommendations were also presented as part of other presentations/meetings including family medicine department faculty meetings, ACTRID project meetings, and a solicitation of advice from Governor Bredesen’s office. E. Dissemination to Community Members (i.e. defining pregnant women/new mothers as the “community”) 1. Report to the March of Dimes (3 above) included parents of premature babies, many of whom smoked or experienced other risks during pregnancy. 2. New/Expectant Mom Support Groups. In the course of the research interviews, many participating women talked about social isolation and the desire to network with other expectant or new mothers. As a result, the research assistant on the project went about enthusiastically setting up a support group for the participants. Meetings were held biweekly over a 4 month period (April through July, 2006). Sessions were held at a community center and time was divided between informal group discussions and an “expert” speaker. Food and childcare were provided. At two of the sessions, presentation of findings and ideas from the project were the “expert” portion. Significant feedback was obtained regarding the usefulness of the support group and suggestions for defining and solving pregnancy issues in Southern Appalachia. Feedback was incorporated into ideas for service provision and applications for future funding. As a result of the findings of this project, the PI has sought to expand the study as well as apply the findings to improve health in the region. The PI has put together and presented a training session for family physicians and residents focusing on helping them help their prenatal patients quit smoking. This training will continue to be offered to other groups of physicians. From these efforts and the need to do more research on the effectiveness of interventions, the PI has developed multiple proposals for funding. In 2006 an R03 application was submitted to NIH for funding of a pregnancy smoking intervention and evaluation. While the proposal received positive feedback, it was not funded. In working with the project mentor (Dr. Sandy Martin), the proposal was revised for submission in 2007. In the meantime, however, another funding opportunity presented itself and the PI was awarded funding to implement and evaluate a pregnancy smoking cessation program. In January 2007 she received a $1.44 million grant from the State of Tennessee to implement and evaluate the Tennessee Intervention for Pregnancy Smoking (TIPS) project, which she designed based on project findings and the current state of knowledge in the field. This program will involve training all prenatal care providers in a 6 county area in Northeast Tennessee in the 5 A’s, and provide them support for continued use of this intervention. In addition, money is available to provide more intensive case management services to about half of the pregnant smokers in the region. The primary focus of this project will be to conduct a thorough evaluation of the TIPS program, including factors affecting its implementation and effectiveness. The ultimate goal of this four year project will be to refine the TIPS program for use state-wide.