Business Architecture Document
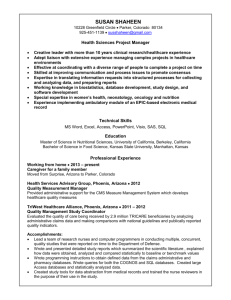
advertisement
HealthConnect Business Architecture version 1.9 November 2004 Foreword We have already seen one revolution in health, as computers have become used in all areas of healthcare. We are now on the verge of a second revolution, as improved communication technology makes it possible to share data between computer systems. Information vital to a patient’s care can now be made available when and where it is needed. HealthConnect is a cooperative venture between the Australian, state and territory governments. The core of HealthConnect is a national system of sharable electronic health records, established to collect, store and exchange consumer health information. Information will be transferred using a secure network with strict privacy safeguards. Summaries of health events such as community consultations, hospital interventions, prescribing history and recent test results can be made available when and where they are needed – to the advantage of both consumers and health professionals. For the past three years HealthConnect has conducted research, trials and extensive community consultations. The business architecture is based on that work; it defines a workable and achievable solution for stage 1 of HealthConnect and provides a framework for future development, implementation and operational activities. HealthConnect is moving closer to becoming a national reality with whole of state implementations underway in Tasmania and South Australia. Significant development projects are underway in several states. The business architecture and other technical documents to be released shortly are providing the basis for this work to proceed. Another important development is the establishment of the National e-Health Transition Authority (NEHTA) to drive the national IM&ICT strategic priorities such as clinical data standards, identification standards and provider directories. These will provide important national components to HealthConnect. This draft business architecture is being made available to provide the basis for comment. Feedback from consumers and the broader health community will guide the preparation of version 2.0 of the business architecture and also guide its ongoing development. There are important new elements of this version of the business architecture that are designed to support the everyday operation of HealthConnect such as the introduction of the eHealth Message Bank service for communication of referrals, prescriptions and diagnostic tests between providers. Nowhere else in the world has an extensive, truly national electronic health record system been established. We are embarking on a long journey that we know will be complex and challenging. HealthConnect will evolve substantially during this journey, but we are confident the destination will provide significant benefits in improved health care and health status for all Australians. On behalf of the HealthConnect Board, I look forward to receiving your comments. Dr Robert Wooding Chair, HealthConnect Board 22 October 2004 i Contacts and Further Information If you require further information, or wish to comment on this document or any other aspect of HealthConnect, please contact the HealthConnect Program Office at: The HealthConnect Program Office Australian Government Department of Health and Ageing MDP 25 GPO Box 9848 CANBERRA ACT 2601 Fax: (02) 6289 8295 Email: healthconnect@health.gov.au Alternatively, please contact your nearest interstate HealthConnect office, as follows: Joanna Kelly New South Wales Ph: (02) 9391 9090 Fax: (02) 9391 9015 Ernest Higgs Victoria Ph: (03) 9616 2083 Fax: (03) 9616 8559 Karen Gibson Queensland Ph: (07) 3131 1679 Fax: (07) 3131 1687 Alan Nankivell South Australia Ph: (08) 8237 8276 Fax: (08) 8237 8070 Des Hutchinson Western Australia Ph: (08) 9222 4379 Fax: (08) 9222 2449 Garry Hulme Tasmania Ph: (03) 6233 2483 Fax: (03) 6233 2899 Gloria Baillee Northern Territory Ph: (08) 8999 2629 Fax: (08) 8999 2419 Wendy Mossman Australian Capital Territory Ph: (02) 6244 3870 Fax: (02) 6285 2099 ii Business Architecture V1.9 - Table of Contents Business Architecture V1.9 - Table of Contents ............................................................. iii HealthConnect Business Architecture version 1.9 - An Overview .................................. 1 Part A – Introduction to the HealthConnect Business Architecture version 1.9 .............. 9 1. Introduction ............................................................................................................ 11 1.1 The HealthConnect Project............................................................................. 11 1.2 Phase 1 & 2 Achievements ............................................................................. 12 1.3 HealthConnect Business Architecture ............................................................ 14 1.4 Finding Your Way around the Business Architecture .................................... 15 Part B – HealthConnect Business Context ..................................................................... 19 2. The HealthConnect Business Drivers ..................................................................... 21 2.1 The Business Need ......................................................................................... 21 2.2 HealthConnect Objectives .............................................................................. 22 2.3 The HealthConnect Concept........................................................................... 23 2.4 The Business Case .......................................................................................... 26 3. HealthConnect Principles ....................................................................................... 29 3.1 Scope of HealthConnect ................................................................................. 29 3.2 Participation in HealthConnect ....................................................................... 30 3.3 Information Management Principles .............................................................. 33 3.4 Technology Principles .................................................................................... 34 4. The HealthConnect Solution .................................................................................. 37 4.1 HealthConnect Context .................................................................................. 37 4.1.1 HealthConnect Scope ............................................................................. 37 4.1.2 The HealthConnect Participants ............................................................. 38 4.1.3 HealthConnect Service Roles and Services ............................................ 39 4.2 HealthConnect System ................................................................................... 40 4.2.1 The HealthConnect EHR ........................................................................ 41 4.2.2 The HealthConnect EHR Repository ..................................................... 41 4.2.3 Core HealthConnect EHR Functionality ................................................ 42 Part C – HealthConnect Participant Involvement .......................................................... 49 5. Consumer Participation .......................................................................................... 51 5.1 Benefits of HealthConnect to Consumers ...................................................... 51 5.2 Consumer Consent to Participate ................................................................... 52 5.2.1 Consent Principles .................................................................................. 52 5.2.2 Current Consent Model .......................................................................... 52 5.2.3 Access Control Arrangements ................................................................ 56 5.2.4 Privacy of Consumer Records ................................................................ 57 5.2.5 Consumer Responsibilities ..................................................................... 57 5.3 Consumer Registration ................................................................................... 58 5.3.1 Identification of Consumers ................................................................... 58 5.3.2 Initial Registration Process ..................................................................... 58 5.3.3 Establishing the Initial Health Profile .................................................... 59 5.3.4 Ongoing Identification ............................................................................ 60 5.3.5 Cancelling Registrations ......................................................................... 61 5.4 Consumer Interaction with HealthConnect .................................................... 61 5.4.1 HealthConnect Consumer Access Services ............................................ 61 5.4.2 Consumer Access to their Health Record ............................................... 62 5.4.3 Consumer Direct Interaction .................................................................. 62 iii 5.5 HealthConnect Consumer Access Portal ........................................................ 63 5.6 Consumer Value Added eHealth Services ..................................................... 65 5.7 Consumer Scenarios ....................................................................................... 67 Scenario 1. HealthConnect – Value Add for Accident Victims. ............................ 67 Scenario 2. HealthConnect – Value Add for the Young Family. ........................... 68 Scenario 3. HealthConnect – Value Add for those with Chronic Disease. ............ 69 6. Healthcare Provider/Organisation Participation ..................................................... 72 6.1 Benefits of HealthConnect to Provider/ Organisations .................................. 72 6.2 Provider Participation Boundaries .................................................................. 73 6.2.1 Scope of Provider Participation .............................................................. 73 6.2.2 Provider Organisations and Individual Providers ................................... 73 6.2.3 Provider Identification ............................................................................ 75 6.2.4 Provider Registration .............................................................................. 75 6.2.5 Authorisation of Providers...................................................................... 76 6.2.6 Provider Authentication .......................................................................... 76 6.2.7 Provider Responsibilities ........................................................................ 77 6.2.8 Privacy and Confidentiality .................................................................... 77 6.3 Provider Interaction with HealthConnect ....................................................... 78 6.3.1 Provider eHealth Access Services .......................................................... 78 6.3.2 Provider Clinical Information System Interfaces ................................... 79 6.3.3 HealthConnect Provider Access Portal................................................... 80 6.3.4 Value Added eHealth Services ............................................................... 81 6.3.5 eHealth Message Bank Service .............................................................. 81 6.4 Key Work Practice Implications..................................................................... 82 6.4.1 Creating Event Summaries ..................................................................... 82 6.4.2 Retrieving EHR information .................................................................. 83 6.4.3 Authorising Diagnostic Test Results ...................................................... 83 6.4.4 Maintaining EHR Lists ........................................................................... 84 6.4.5 Receiving Notifications .......................................................................... 85 6.4.6 Creating the Initial Health Profile .......................................................... 85 6.4.7 First Presentation at Healthcare Setting ................................................. 86 6.4.8 Managing Emergency Access ................................................................ 87 6.5 Provider Scenarios .......................................................................................... 87 Scenario 1 – HealthConnect – Value Add for the GP ............................................ 87 Scenario 2 HealthConnect – Value Add for the Busy Specialist ........................... 88 Scenario 3 – HealthConnect – Value Add for the Ancillary Health Workers ........ 89 Scenario 4 – HealthConnect – Value Add for the Community Health Nurse ........ 90 7. Secondary Users Participation ................................................................................ 92 7.1 Scope of Secondary Uses ............................................................................... 92 7.1.1 Secondary Users ..................................................................................... 92 7.1.2 Areas Secondary Uses will Support ....................................................... 92 7.1.3 Examples of Secondary Uses ................................................................. 93 7.2 Benefits of Secondary Uses ............................................................................ 94 7.3 Consent and Responsibilities .......................................................................... 95 7.3.1 Consent for Secondary Uses ................................................................... 95 7.3.2 Responsibilities of Secondary Users ...................................................... 95 7.4 Governance of Secondary Uses ...................................................................... 96 7.4.1 Governance Structure ............................................................................. 96 7.4.2 Secondary Uses Approval Process ......................................................... 97 7.4.3 Information Access Process.................................................................... 98 7.5 Secondary User Scenario ................................................................................ 98 iv Scenario – HealthConnect – Value Add for the Population ................................... 98 Part D – Description of HealthConnect Components................................................... 101 8. HealthConnect Context and Roles........................................................................ 103 HealthConnect Participants .......................................................................................... 105 8.1 Consumers .................................................................................................... 105 8.2 Providers ....................................................................................................... 105 8.2.1 Types of HealthConnect Provider ........................................................ 105 8.2.2 Provider Access to HealthConnect ....................................................... 106 8.2.3 Provider Processes ................................................................................ 107 8.3 Secondary Users ........................................................................................... 107 Core HealthConnect Roles ........................................................................................... 108 8.4 HealthConnect Governance .......................................................................... 108 8.4.1 HealthConnect Governance - Functions and Processes ....................... 108 8.5 HealthConnect EHR Repository................................................................... 110 8.5.1 The Federated Model for HealthConnect Delivery .............................. 110 8.5.2 HealthConnect Records System (HRS) ................................................ 111 8.5.3 Approved EHR Manager (AEM) ......................................................... 111 8.5.4 HRS/AEM – Processes ......................................................................... 112 8.6 National Data Store ...................................................................................... 113 8.7 HealthConnect Metadata Repository ............................................................ 113 8.8 Consumer Registration and Management..................................................... 114 8.9 HealthConnect Consumer Index ................................................................... 116 8.10 HealthConnect Consumer Access Services .................................................. 117 8.11 Provider Registration and Management ....................................................... 118 8.12 Provider eHealth Access Services ................................................................ 120 8.13 eHealth Message Bank Service .................................................................... 122 8.14 Value Added eHealth Services ..................................................................... 122 8.15 National Health InfoStructure ...................................................................... 123 8.15.1 National Health Identifier ..................................................................... 123 8.15.2 National Health Provider Directory...................................................... 124 8.15.3 National Health Metadata Repositories ................................................ 124 8.15.4 Health Information Standards, Terminologies and Data Sets .............. 125 8.16 Supporting ICT Infrastructure ...................................................................... 126 9. Information Components ...................................................................................... 128 9.1 Introduction .................................................................................................. 128 9.2 HealthConnect EHR Repository................................................................... 129 9.3 HealthConnect Electronic Health Record (EHR) ......................................... 129 9.4 The CEN EHR Reference Information Model ............................................. 130 9.5 HealthConnect National Data Store ............................................................. 131 9.6 HealthConnect Event Summary ................................................................... 132 9.7 EHR Views ................................................................................................... 135 9.8 EHR Lists ..................................................................................................... 136 9.9 EHR Query/Response ................................................................................... 137 9.10 HealthConnect Notifications ........................................................................ 139 9.11 Consumer Details ......................................................................................... 139 9.12 Access Control List ...................................................................................... 141 9.13 EHR Access Logs and Audit Trails.............................................................. 141 9.14 HealthConnect Reports ................................................................................. 142 9.15 HealthConnect Consumers and Providers .................................................... 143 9.15.1 HealthConnect Consumer Index ........................................................... 143 9.15.2 HealthConnect Provider Directory ....................................................... 144 v 9.16 HealthConnect Metadata .............................................................................. 144 9.17 HealthConnect Registration Objects ............................................................ 146 9.18 National Information Repositories ............................................................... 146 9.19 eHealth Communication Messages .............................................................. 147 10. HealthConnect Business Processes .................................................................. 148 10.1 High Level Business Process Context .......................................................... 148 10.2 Major Business Processes............................................................................. 150 11. Technology Components .................................................................................. 154 11.1 Systems Overview ........................................................................................ 154 Part E – Managing and Implementing HealthConnect ................................................. 159 12. Managing HealthConnect ................................................................................. 161 12.1 HealthConnect Governance Structure .......................................................... 161 12.1.1 The Governance Approach ................................................................... 161 12.1.2 Ongoing Management Governance Structure ...................................... 162 12.1.3 Project Implementation Governance Structure .................................... 163 12.1.4 National eHealth Transition Authority ................................................. 165 12.2 HealthConnect Privacy Issues ...................................................................... 165 12.2.1 Need for Strict Privacy Control ............................................................ 165 12.2.2 Existing Privacy Frameworks............................................................... 166 12.2.3 HealthConnect Privacy Framework...................................................... 167 12.3 HealthConnect Legal Issues ......................................................................... 168 13. Implementing HealthConnect ........................................................................... 169 13.1 HealthConnect Implementation Approach ................................................... 169 13.1.1 Implementation Drivers ........................................................................ 169 13.1.2 Provider and Consumer Take-up .......................................................... 170 13.1.3 HealthConnect Capabilities Compliance .............................................. 171 13.2 Current Implementation Activities ............................................................... 172 13.2.1 HealthConnect Version 1 ..................................................................... 172 13.2.2 Stage 1 HealthConnect Implementations ............................................. 172 13.2.3 Current HealthConnect Trials............................................................... 173 Glossary of Terms ........................................................................................................ 175 HealthConnect Business Architecture – Glossary of Terms ....................................... 176 vi HealthConnect Business Architecture v1.9 HealthConnect Business Architecture version 1.9 - An Overview HealthConnect Business Architecture v1.9 HealthConnect Business Architecture v1.9 Overview of the HealthConnect Business Architecture What is the HealthConnect Vision? Healthcare services in Australia are provided by a wide range of government and non-government organisations. A key theme that has emerged in healthcare reform over the last decade is the need to integrate and better coordinate the delivery of care across the full range of healthcare settings. HealthConnect is being developed as Australia’s national health information network. It is a cooperative venture between the Australian, State and Territory Governments. It involves the collection, storage and exchange of consumer health information via a secure network and within strict privacy safeguards, to facilitate better integration of care and to improve outcomes across the health care system. HealthConnect will help make Australia a world leader in what many experts believe is currently the most significant contributor to health care reform – better, more timely health information. The first phases of HealthConnect involved intensive research, design and development, including HealthConnect trials, to define the policies, technologies, infrastructure and management structure needed to underpin the nation-wide implementation of HealthConnect. These activities have delivered significant findings that are enabling the HealthConnect concept to be distilled into practical reality. Why develop a Business Architecture? The HealthConnect Business Architecture is the means of communicating the scope and longer term vision of a workable national solution for HealthConnect. It provides a compliance framework for initial HealthConnect implementations, identifies requirements for further research and provides a vehicle for stakeholder review and participation in refining the HealthConnect solution. The current version of the Business Architecture differs significantly from the earlier version published in 2002. Since then, there has been extensive consultation with stakeholders throughout Australia and HealthConnect trials in a number of States - these activities have significantly refined the HealthConnect concept and have provided valuable input to the development of the current Business Architecture. The Business Architecture is now able to explain in much more detail how HealthConnect is to work. What is the HealthConnect model? The core of HealthConnect is a national system of sharable electronic health records, which will be established to receive, store, retrieve and deliver consumers’ electronic health record (EHR) information via secure eHealth communications with strict privacy safeguards for use in the delivery of health care. A consumer’s EHR will consist of a series of event summaries, each containing key information about a specific health care event such as a general practitioner consultation, hospital admission or discharge, community health centre visit, pathology test or a pharmacy dispensing a prescription. 1 HealthConnect Business Architecture v1.9 The figure below illustrates the components considered fundamental to the development of HealthConnect, namely: HealthConnect Participants, HealthConnect Event Summaries, EHR Repository, EHR Lists, EHR Views and EHR Reports. HealthConnect Participants For example: · Consumers · · · · · · · Event Summaries HealthConnect Repository General Practitioners, Specialists Community nurses Event Summaries including: · Healthcare consultations Private allied health care providers eg. physiotherapists, podiatrists, optometrists Community pharmacists EHR Views Hospital clinicians · · · Diagnostic test results Hospital discharge information Immunisation information Emergency department clinicians Aged care workers EHR Lists including: · Current medications Secondary Users · Researchers · Managers//Planners · Evaluators · · Principal diagnoses Allergies and alerts EHR Reports Figure 1 – Key Components of HealthConnect Once a consumer has given consent to participate in HealthConnect, each time the consumer has contact with the health system, an event summary may be created and sent electronically by the consumer’s health service provider for inclusion in the consumer’s HealthConnect EHR. These event summaries will then be available to those users of HealthConnect that the consumer has authorised access to the EHR. With the consumer’s authorisation, access to the HealthConnect EHR will be available to registered provider organisations at the time health services are delivered to the consumer. The availability of EHR information is to assist clinical decision making with a view to improving both quality of care and consumer safety. HealthConnect will not replace providers’ own clinical records or clinical information systems. Providers will continue to maintain their own consumer health records but may choose to incorporate selected HealthConnect EHR information in their records or clinical information systems. HealthConnect will support secondary use of HealthConnect EHR information for research and planning of health service delivery, in line with strict privacy policies, appropriate legislative requirements and monitoring of such use. What other services will HealthConnect provide/support? For HealthConnect to work, there will need to be considerable investment in the establishment of national health messaging services and communications networks with 2 HealthConnect Business Architecture v1.9 high levels of security and capacity. Building on this requirement provides the opportunity for HealthConnect to support wider eHealth communications including the transmission of messages between participating providers. This service is referred to as the eHealth Message Bank service and might be used for delivery of referrals, prescription processing, diagnostic test requests and results. Being a separate support service rather than an integral part of HealthConnect, the eHealth Message Bank can be used for more efficient clinical communication about any Australian health care consumer, not just HealthConnect participants. HealthConnect will also encourage development of new value-added services by the health sector and will enhance the decision-support ability of provider clinical information systems by ensuring that the information about the consumer being treated is more complete than otherwise possible. HealthConnect implementations will support, use, and facilitate the development of health infostructure such as the national provider directory, national health identifier, health metadata repositories, health information standards, approved terminologies and health data sets. While this infostructure may not be available for the early implementations, HealthConnect will need to be able to accommodate and use these infostructure components as they become available. Who will participate in HealthConnect? HealthConnect’s primary users will be consumers and those seeking consumer health record information to assist in decision making related to the provision of health services - specifically: health service providers (including doctors, nurses, pharmacists, allied health, community health, Aboriginal and Torres Strait Islander health and public health practitioners); and consumers reviewing and adding to their own health records. There will also be a range of secondary users including researchers, planners and managers, and evaluators. How will consumer participation be managed? Enrolment in HealthConnect will be available to all Australian citizens and residents of Australia. Early implementation will focus on those consumers with ongoing health care needs – those suffering chronic diseases, populations with high morbidity and infants. Consumer participation in HealthConnect will be voluntary and nondiscriminatory. The consumer must have given informed consent before their EHR and other personal information can be collected, accessed, used or disclosed by HealthConnect. Consumer consent arrangements and practical measures for managing consent have proven some of the most difficult and sensitive aspects of HealthConnect to date and are some of the most heavily researched. The proposed consent model covers: consent for establishment and use of the consumer’s HealthConnect EHR, the nomination of agents and legal representatives to act on behalf of the consumer, amendment, correction and withdrawal of information, deregistering from HealthConnect and the complaints process. A key aspect of the consent process is the creation and maintenance of a list of provider organisations authorised to access the consumer’s HealthConnect record. Organisations not identified on the consumer’s access list will not be able to access the consumer’s 3 HealthConnect Business Architecture v1.9 EHR, unless using the emergency override facility. At any time, the consumer will be able to nominate or change the provider organisations that may access their EHR. In the future, there may also be the opportunity to control access through features such as restriction by provider type and the ‘secure envelope’ concept which allows more restricted access for sensitive information, although these are subject to the findings of further research. How will consumers use HealthConnect? HealthConnect Consumer Access Services (HCCAS) will be established to assist and support customer interaction with HealthConnect. These may also offer additional services of interest to consumers. Consumers will have access to HealthConnect to view their EHR information. A web browser facility will be created for this purpose. Future implementations of HealthConnect are expected to include consumer contribution to their records, following resolution of medico-legal and workflow concerns. How will provider participation be managed? Provider participation in HealthConnect will be voluntary and available to all providers and provider organisations involved in the chain of health care delivery. While the initial focus is likely to include medical practices, pharmacies, hospitals, diagnostic services, health and aged care facilities and those practitioners currently participating in HealthConnect initiatives, this scope will be extended through arrangements with representatives of each provider group. Participation in HealthConnect occurs at the level of individual providers (for example, medical practitioners, diagnostic specialists, community clinicians, pharmacists) who may be contributing to HealthConnect and provider organisations accessing HealthConnect. Both will need to register with HealthConnect. As part of registration with HealthConnect, providers will be required to sign an agreement that includes an acknowledgement that their access to consumer information through HealthConnect will be only for the purpose of delivering health services to the consumer. How will providers use HealthConnect? Provider eHealth Access Services (PeHAS) will be available to providers and provider organisations as the means of accessing HealthConnect services, via a message handling and transport system and for obtaining front line support to assist them in using HealthConnect. Providers will interact with HealthConnect primarily through their clinical information systems. In the initial stages, a web portal will be available for providers who do not have clinical information systems able to create event summaries. This will allow them to enter event summary data directly; however, this is not seen as the preferred method of event summary entry for the long term. HealthConnect information will be available to providers via specially designed views that bring together key aspects of a consumer’s health record, such as medications, 4 HealthConnect Business Architecture v1.9 allergies and alerts, problems and diagnoses. Providers will send requests for information to HealthConnect and will be able to use the resulting information as part of their local decision making processes. Though it is recognised that access to HealthConnect entails additional processes, a high priority will be placed on effective integration with provider systems in order to streamline the process and minimise the impact on provider work practices. How will secondary user participation be managed? HealthConnect will support secondary uses of HealthConnect information for improvement of health service delivery and for research purposes, in line with national privacy legislation, the research and ethics best practice guidelines of the National Health and Medical Research Council (NHMRC) and with transparent monitoring of use. A key role in HealthConnect will be to manage the process of granting access to HealthConnect information for agreed secondary purposes. HealthConnect’s governance structures will contain arrangements for the independent and transparent monitoring of the role of HealthConnect in authorising and managing access to information for secondary uses. How will privacy be managed? The success of HealthConnect will depend on individual providers, health service organisations and consumers having confidence and trust that their health information is kept confidential and secure. To this end, a robust privacy framework, together with the strongest available security measures, is required. Providers participating in HealthConnect will be obliged to abide by existing privacy legislation and by specific HealthConnect privacy protocols, covering access and use of information from consumers’ HealthConnect records, and contributing information to these records. What functions will be needed to deliver HealthConnect? There are many roles and functions associated with the delivery of HealthConnect services including both roles performed within HealthConnect itself and roles performed within associated entities (such as providers and consumers). The figure overleaf presents the major roles; the core HealthConnect roles are shaded. These core HealthConnect roles include those for registration of consumers and providers, maintaining the HealthConnect EHR repository, managing the structure and content of EHR information, and for governance of HealthConnect. The ICT infrastructure necessary for the operation of HealthConnect includes secure networks, IT processing platforms, clinical applications and the organisations that support these services. Ministers have endorsed the establishment of the National eHealth Transition Authority (NEHTA) to drive the national IM&ICT priorities to June 2005, at which stage a longer term strategy will be determined. NEHTA has established a work program focussing on 5 HealthConnect Business Architecture v1.9 the areas of clinical data standards, identification standards, directories, supply chain procurement standards, consent models, secure messaging and information transfer, and technical integration standards. These initiatives will be critical to supporting the future development and implementation of HealthConnect. National Health InfoStructure National Health Identifier Service (Consumers) Health Information Standards, Terminologies and Data Sets National Health Metadata Repositories National Health Provider Directory Secondary User HealthConnect Governance HealthConnect Metadata Repository HealthConnect EHR Repository National Data Store Consumer Consumer Registration & Management HealthConnect Consumer Access Services HRS/ AEM ... HRS/ AEM Provider Registration & Management Provider Health Connect Provider Directory HealthConnect Consumer Index Provider eHealth Access Services Value Added eHealth Services Health Registries eHealth Message Bank Service Supporting ICT Infrastructure Processing Platforms Clinical Information System Support Clinical Applications Secure Communications Networks Figure 2 – Role Map for Delivery of HealthConnect Services How will the EHR information be structured? Each HealthConnect EHR will comprise a collection of ‘event summaries’ that contain a summary of information about healthcare events related to the ongoing care of a consumer in a standardised, machine readable form. Separate event summaries can be submitted for each healthcare event or one event summary may cover a number of related treatments. Different types of event summaries will be developed over time in line with business needs. The information within the event summaries will be structured as data groups. Some key data groups will be stored as EHR ‘lists’ which are collections of similar EHR items describing key aspects of a consumer’s health, formed to serve a specific purpose. Examples of EHR lists which HealthConnect will automatically derive from event summary information are prescribing/dispensing history, procedure/treatment history, and recent health services. Examples of EHR lists which need to be maintained by a 6 HealthConnect Business Architecture v1.9 provider are current medications, active problems/diagnoses, adverse reactions and warnings. Users of HealthConnect will access data using pre-defined ‘views’ suited to the specific needs of consumers and providers. The priority views identified to date are the primary (or ‘critical’) view; and the health profile view. Secondary users will access data through ‘reports’ that are extracts of EHR information that have been predefined as part of the HealthConnect secondary use approval process. What are the key technology components? HealthConnect will establish an EHR repository based on a national network of HealthConnect Records Systems (HRS). Each HRS will hold and manage the shared electronic health records (EHR) for many consumers. Whilst the HealthConnect EHR repository may be distributed across a number of federated elements, it is intended that it be available as a single national resource from the viewpoint of access, interoperability, reporting and inquiry. Hence each HRS service must support a common interoperability framework that enables standard HealthConnect interactions with provider systems, national HealthConnect infrastructure and health infostructure components. A copy of the EHR material will to be transmitted to the National Data Store (NDS) for archiving and long-term retention. This National Data Store will be used to support all secondary use of HealthConnect EHR data for research and planning purposes, while all operational interaction with a consumer’s EHR will occur through the HRS. Access to the NDS will be tightly controlled. HealthConnect will complement rather than replace providers’ systems. The focus will be on sourcing event summaries from these systems and providing information required for the selected views. All communications between an HRS and user applications are conveyed as messages via the message handling and transport system that manages communications between HealthConnect participants and other individuals and organisations. The message handling and transport system and HRS services will rely on the HealthConnect consumer index and HealthConnect provider directory for information needed to identify HealthConnect participants and to route messages to and from the appropriate HRS and other application components in the federated HealthConnect environment. For consumers, and providers whose clinical information systems cannot interact with HealthConnect, web-based portals will be developed for entry of event summaries, viewing of EHR information and maintenance of registration information. How will HealthConnect be implemented? The procurement, development and implementation of a complete, sustainable solution as a long-term platform for HealthConnect will be based on version 2 of the HealthConnect Business Architecture. Given that some of the longer term requirements are still being finalised, it is likely to be several years before this solution is implemented. 7 HealthConnect Business Architecture v1.9 There is an immediate need to make progress and to build on the successes and the momentum of the first HealthConnect trials. HealthConnect is therefore undertaking a staged approach to implementations. The Stage 1 implementations will not be extensions of the trials, though they will make use of components and lessons from the trials. There are also significant development projects underway in other states as part of the HealthConnect trial program, some of which are intended to become part of the longer-term HealthConnect program. Implementation is therefore three pronged, with: stage 1 implementations in three jurisdictions; continuation of trials still under development in some other states and the development and implementation of a complete, sustainable HealthConnect solution for the longer-term. How will HealthConnect be managed? It is proposed that the ongoing management of the HealthConnect program at the national level be vested in a dedicated organisational entity on behalf of all the participating governments and other stakeholders. This organisational entity is commonly referred to as the HealthConnect governing body. The functions which this governing body would be expected to cover include: overseeing the implementation and operation of HealthConnect, providing clinical governance, maintaining approval mechanisms to assess requests for secondary uses of HealthConnect data, overseeing registration process for both consumers and providers, determining the rules and standards applicable to HealthConnect activities, establishing contractual and licensing arrangements with various HealthConnect participants and suppliers, and monitoring of compliance throughout the network. In the short term, the governance arrangements for project implementation activities will be based on the current HealthConnect Board, Steering Committee and Advisory Group arrangements. HealthConnect is also being progressed regionally through HealthConnect state/territory implementations and the ongoing HealthConnect trials. 8 HealthConnect Business Architecture v1.9 Part A – Introduction to the HealthConnect Business Architecture version 1.9 HealthConnect 1. Business Architecture v1.9 Introduction 1.1 The HealthConnect Project Australian health ministers are committed to improving the delivery of health services and achieving better health care outcomes through the use of information and communications technologies. To this end, health ministers established the National Health Information Management Advisory Council (NHIMAC) in July 1998 to develop a national action plan for information management in the health sector. In turn, NHIMAC established the National Electronic Health Records Taskforce in 1999 to develop a coordinated approach to electronic health records in Australia. In July 2000, the taskforce presented its report, A Health Information Network for Australia,1 to the health ministers. They endorsed its recommendation to create a national health information network supporting electronic health records (EHR) - now known as HealthConnect. HealthConnect will, with consumer consent, allow the electronic exchange of clinical information between health care providers. HealthConnect is a cooperative venture between the Australian, State and Territory governments. The Taskforce proposed that HealthConnect be developed in three phases over a six to ten year period, as follows: · Phase 1 & 2: Research and development work (years 1-4); · Phase 3: Construction and initial operation (years 3-6); and · Phase 4: Subsequent growth and expansion (years 6+). Phase 1 of HealthConnect commenced in July 2001 with a mix of research, development and design activities and in July 2003 was extended for a further two years to enable the conduct of further trials and for the results of these activities to be assessed and incorporated into the design of HealthConnect. In March 2004, the Australian government announced the national implementation of HealthConnect, providing $128 million over the next four years towards the implementation, which will commence in Tasmania, South Australia and the Northern Territory. The Australian Health Information Council (AHIC) and the National Health Information Group (NHIG), to which the HealthConnect Board reports, are jointly developing a national IM&ICT strategy due to be completed at the end of 2004. Ministers have endorsed the establishment of the National eHealth Transition Authority (NEHTA) to drive the national priorities over the next 12 months. The longer term strategy will then be determined, potentially including the establishment of an independent legal entity. The directories and standards work to be conducted by NEHTA will be critical to supporting the future development and implementation of HealthConnect. 1 A Health Information Network for Australia, National Electronic Health Records Taskforce, July 2000 11 HealthConnect Business Architecture v1.9 1.2 Phase 1 & 2 Achievements The first phases of HealthConnect involved extensive research, design and development, including a program of HealthConnect trials and accelerated programs of work to define the policies, technologies and infrastructure, and management structure needed to underpin the national implementation of HealthConnect. Many of the preliminary outcomes were presented in the HealthConnect Interim Research Report2, published in August 2003. Significant outcomes have been derived from the HealthConnect Trials, MediConnect Field Test and research deliverables. Each of these is discussed below. HealthConnect Trials The HealthConnect trials are a significant achievement for the project and have been the principal mechanism for testing the HealthConnect concept. Each of the trial sites focuses on a particular health issue or population group where HealthConnect arrangements might reasonably be expected to, in the future, yield some benefit to both consumers and providers. In October 2002, ‘fast track’ trials commenced in Clarence municipality near Hobart in Tasmania and in the Katherine region of the Northern Territory. The Tasmanian trial, subsequently extended to cover Southern Tasmania and now nearing completion, focuses on adults with diabetes and involves health care providers from general practice, pathology and the Royal Hobart Hospital, as well as a range of diabetes specialists and educators. The Northern Territory trial has expanded to become a full implementation covering services to indigenous and remote communities across the Katherine region, with a view to further expansion across the Territory in the future. Two longer-term HealthConnect trials have been established in Queensland in the second half of 2003. The North Queensland HealthConnect trial, which went live in December 2003, focuses on the peri-operative assessment and preparation of consumers travelling to undergo elective surgery at Townsville Hospital. This trial has now been extended for a further 12 months. The Brisbane Southside HealthConnect trial, commenced in late 2004, focuses on testing new openEHR software technology for managing health records for consumers with diabetes. The New South Wales Health-e-Link initiative currently under development is also considered a HealthConnect trial. The project will test HealthConnect infrastructure in two pilot sites. The Child Health Information Network (CHIN) will operate in Greater Western Sydney and includes the Children’s Hospital at Westmead. The Chronic Disease Management System project will operate in the Hunter Valley and includes the John Hunter Hospital in Newcastle. These two pilots are expected to go live in mid2005. MediConnect Field Test MediConnect, formerly known as the Better Medication Management System (BMMS), has been combined with HealthConnect and now forms the medications component of HealthConnect. 2 The HealthConnect Interim Research Report, August 2003. 12 HealthConnect Business Architecture v1.9 A field test has been conducted at two locations, Ballarat and Launceston, as part of the MediConnect program. MediConnect was aimed at improving quality and safety in prescribing, dispensing and managing medication by using online technology to enable prescribers, dispensers and the consumer to have more timely access to more complete information about the consumers’ medication. The HealthConnect trials and MediConnect field test are providing first-hand experience that has proven valuable to HealthConnect in understanding the practical application of EHR concepts, their impacts on clinical workflow and the challenges of sharing EHR information between different clinical settings. Research Deliverables Phase 1 of HealthConnect addressed the key HealthConnect research questions and commenced important technical design work, much of which has resulted in the production of substantial research reports and planning documents. The key reference documents are: · HealthConnect Interim Research Report3, which included version 1 of the HealthConnect Business Architecture, following its refinement through widespread public consultation; · Outputs of the HealthConnect systems architecture project, including: the HealthConnect Architecture Overview and the HealthConnect Systems Architecture v0.94; · Reports of the Clinical Information Project (CIP)5 which specify the information content and structure of HealthConnect health event summaries, lists and views; · A series of discussion papers on HealthConnect business requirements. These papers were circulated to the HealthConnect Board, Program Office and Trial Managers and address: privacy; consent; registration and identification of HealthConnect participants; processing and storage of health information; security and access control; and user interfaces, messaging and transport; · HealthConnect Indicative Benefits Report6; · A proposed National Health Privacy Code and accompanying discussion paper, which was developed by the AHMAC Privacy Working Group and has now been forwarded to Health Ministers for their consideration; · Work by National InfoStructure Development Section facilitating the development of Australian Standards and International Standards on healthcare messaging, EHR architecture, terminologies, discharge summaries and referrals, patient (consumer) identification, provider identification and other areas that will benefit both HealthConnect and the health sector generally; and 3 The HealthConnect Interim Research Report, August 2003. HealthConnect Draft Systems Architecture v0.9, July 2003. 5 www.health.gov.au/healthconnect/building_blocks/cip.html 6 Indicative Benefits Report, Fujitsu Consulting, February 2004 4 13 HealthConnect · Business Architecture v1.9 Research and evaluation studies of HealthConnect trials in Tasmania and Northern Territory and preparation for trials in New South Wales and Queensland. These documents, together with feedback from the trial and evaluation documents, have been instrumental in shaping the HealthConnect solution described in this Business Architecture. 1.3 HealthConnect Business Architecture In 2002 the HealthConnect Business Architecture version 1 was issued. While an effective communication tool, it was not possible to resolve all the business issues at that time. Since the initial version, the lessons learned from the trials and research and the development of the draft systems architecture have informed the requirements. Hence a review of the Business Architecture and the development of an update were required. This document, version 1.9 of the HealthConnect Business Architecture, represents the results of the review. The purpose of this version of the HealthConnect Business Architecture is to: · Communicate HealthConnect in a way that is understandable to a range of different audiences; · Identify the scope of the longer-term HealthConnect solution, based on the findings of HealthConnect research and development work and extensive consultation; · Determine a workable, achievable and cost-effective scope for stage 1 HealthConnect implementations, recognising current technical, legal and environmental considerations; · Provide the framework to which the stage 1 implementations will need to comply; · Identify potential business requirements for further research, and possible inclusion in later versions, of HealthConnect; and · Provide a suitable vehicle for stakeholder review and acceptance of the initial and longer-term HealthConnect solution. This version of the HealthConnect Business Architecture seeks to address and reconcile the many different positions on HealthConnect held by Australian, state and territory health jurisdictions, consumer and privacy advocates, health service delivery organisations, healthcare providers and the health software industry. As such, the Business Architecture seeks to define the requirements for the end-point to which those currently proposing to provide EHR solutions need to aspire for Australia to succeed in its endeavour of having a single national system of health records, albeit composed of many disparate, interoperating parts. 14 HealthConnect Business Architecture v1.9 Approach to Developing the Business Architecture As indicated the HealthConnect Business Architecture is based on extensive clinical and consumer consultation, research and trial lessons. Preparation of this version of the Business Architecture (version 1.9) was also based on a staged program of activities that involved: · Reviewing existing HealthConnect work programs, including the HealthConnect trials, MediConnect field test, HealthConnect architectures, HealthConnect business requirements and the work of the Clinical Information Project; · The development and circulation of a range of position papers to the Program Office and recognised experts. These papers addressed topics such as: eHealth communications; clinical decision support; the nature of the summary record; HealthConnect front-end processing; the passive store paradigm; secondary uses of HealthConnect data; the federation paradigm, EHR architectures for HealthConnect and the use of EHR standards; · Widespread consultation on HealthConnect business requirements and matters raised in the position papers - including conduct of two national workshops; · Discussions at HealthConnect Trial Manager Forums, HealthConnect Stakeholder Reference Group and HealthConnect Board meetings and consultation with state and territory health jurisdictions, and the HealthConnect Program Office; · Consultation with consultants and project managers reviewing other aspects of HealthConnect, specifically, benefits realisation, implementation and legal issues; and · Contact with the broader health informatics community and industry experts, and obtaining updates on relevant developments in the eHealth environment and the activities of government and non-government organisations. Following broad consultation and feedback on version 1.9, it is proposed that an updated final version 2.0 of the Business Architecture will be released following approval by the HealthConnect Board. As implementations proceed, it is proposed that the HealthConnect business architecture will continue to be developed in line with the changing business requirements, under the guidance of the body responsible for on-going management of HealthConnect. 1.4 Finding Your Way around the Business Architecture Structure of the Business Architecture The main content of the Business Architecture is divided into five parts as follows: · Part A - Provides background on the HealthConnect project and the development of this business architecture. 15 HealthConnect Business Architecture v1.9 · Part B - Develops the HealthConnect concept – the business drivers for undertaking HealthConnect, the key principles on which HealthConnect implementation is based; · Part C – Discusses the operation of HealthConnect from the viewpoints of different types of participants – consumers, providers and secondary users; · Part D – Provides a structured description of the business and systems components that make up HealthConnect and how they interoperate – based on considerations raised by the Federal Enterprise Architecture Framework (FEAF); and · Part E – Provides detail on governance, legal and implementation issues associated with realising HealthConnect. Using the Business Architecture The HealthConnect Business Architecture contains a variety of material intended for a broad audience including: Australian, state and territory health jurisdictions; consumer representatives; peak bodies and professional associations representing healthcare providers and the health IT industry; health ministers, their advisers and other policy makers; those working on implementation of HealthConnect; other involved agencies; and interested stakeholders. Where more selected reading is required, the following guidance may be helpful in finding the most appropriate material: 7 · Those with no prior knowledge of HealthConnect may find it helpful to refer first to some of the introductory HealthConnect materials (including the most recent HealthConnect overview7) that are available from HealthConnect offices, or HealthConnect staff in each state and territory or to view the HealthConnect website at www.healthconnect.gov.au · Those seeking a general overview of HealthConnect and its specific scope should refer to Parts A and B of this document. · Those primarily interested in the impact of HealthConnect from a consumer perspective should refer to Section 5 in Part C of this document. · Those primarily interested in the impact of HealthConnect from the perspective of a healthcare provider or provider organisation should refer to Section 6 in Part C of this document. · Those interested in access to HealthConnect information for research, health planning or policy development, should refer to Section 7 in Part C of this document. · Those seeking more detailed information on HealthConnect requirements and proposed functions should refer to Part D of this document. HealthConnect – An Overview, May 2004, Australian Department of Health and Ageing. 16 HealthConnect Business Architecture v1.9 · Those seeking information on HealthConnect implementation issues including governance and stakeholder engagement arrangements should refer to Part E of this document. · A glossary of terms is provided to assist understanding. 17 HealthConnect Business Architecture v1.9 Part B – HealthConnect Business Context 19 HealthConnect 2. Business Architecture v1.9 The HealthConnect Business Drivers This section addresses the business drivers associated with the exchange of health information and a proposed solution based on a national system of shared electronic health records. The Business Drivers are discussed below in relationship to the: · Business need, a statement of the background to the business drivers and a statement of the primary and secondary business problems; · Business objectives, a statement of the business goals, purposes, outcomes of the system; · System concept, a statement of the concept of what the system is; and · Business case, a high level statement of the HealthConnect business case. 2.1 The Business Need A key theme that has emerged in healthcare reform in Australia over the last decade is the need to integrate and better coordinate the delivery of care across the full range of healthcare settings. Achieving such integration, where healthcare services are provided by a wide range of government and non-government organisations, depends upon relevant information about individual consumers being more readily available at every point of care. Currently, health records are kept in a variety of formats at different locations across the system – i.e. in ‘information silos’. The situation is further compounded by existing organisational and professional boundaries that impede information sharing. Lack of ready access to critical information can result in: · adverse events, including drug interactions, duplicated medications and inappropriate therapy based on less complete information; · diagnostic tests being undertaken unnecessarily due to previous results not being available and there being insufficient information to assist diagnosis; · consumers and providers spending additional time retrieving information that could be readily available at the point of care; and · individuals falling through ‘cracks’ in the system and not receiving appropriate health care due to information not being effectively communicated. Clearly, inadequate sharing of information is a quality and safety issue that needs to be addressed through a system-wide approach. Technologies, such as an electronic health records network, offer unprecedented opportunities to improve the flow of information across the health system. If successfully implemented, such systems have the potential to ensure that the consumers and providers have access to the information they need for better decision making. 21 HealthConnect Business Architecture v1.9 As stated in version 1 of the Business Architecture: The primary business problem that HealthConnect aims to address is to facilitate access by consumers and providers to timely, relevant, summary information relating to the health status, treatment and events of consumers, at the time of care, to assist decision making. This has the potential to enable consumers to take an increasing role in self management. The secondary problems that HealthConnect is intended to assist with resolving include: · creating a best practice, evidence-based health system through generation of new knowledge and better education and professional development of healthcare providers, planners and policy makers; · improving utilisation of health resources and access to health services through implementation of better, more targeted health initiatives and better planning; · improving safety of healthcare services through activities such as enabling rapid response to treatment and device failures; · supporting research and education; and · detecting outbreaks of disease. 2.2 HealthConnect Objectives In 1999, the Australian Health Ministers endorsed Health Online: A Health Information Action Plan for Australia and a national strategy was developed which included a key recommendation to develop a national framework for the use of electronic health records. The Australian Health Ministers subsequently endorsed the recommendations of the National Electronic Health Records Taskforce to establish HealthConnect - a health information network overseeing the development of a national electronic health record. In its July 2000 report to Health Ministers8, the National Electronic Health Records Taskforce outlined the following objectives for achieving this national EHR network, namely: "Improved delivery of healthcare and better continuity and quality of care, consumer safety and health outcomes for all Australians while enhancing the privacy and respecting the dignity of health consumers by: · empowering consumers to be able to take a greater responsibility for their own healthcare and be better informed about the choices available to them in respect of their healthcare; · ensuring better decision-making which is shared by both consumers and health providers at the point of care; 8 A Health Information Network for Australia, National Electronic Health Records Taskforce, July 2000 22 HealthConnect Business Architecture v1.9 · providing a flexible, seamless and integrated process of care through the improved delivery of healthcare and better continuity and quality of care, consumer safety and sharing and better exchange of information; · providing better access to healthcare, particularly in rural and remote areas; · building a best-practice, evidence based health system; · encouraging better, more targeted health initiatives; and · informing research, learning and training; through developing a nationally coordinated and distributed system of electronic health records, which is based on the greater use of online technologies." Building on the Taskforce’s objectives for a national EHR network, a HealthConnect Project Proposal was developed and endorsed by the HealthConnect Board in September 2001. This project proposal identified the specific goals, purposes and objectives of HealthConnect to be: Goal(s) Improved health outcomes. (ie the higher order objective(s) to which the project contributes) Improved healthcare delivery. Purpose(s) Improved knowledge creation and employment of same. (ie the direct effect(s) or impact(s) of the project) More informed consumers. Improved participant (consumer and sectoral stakeholders) satisfaction with the health system. Less time and resource wastage, including reduction in duplication of information/tests. More appropriate healthcare delivery and decision making. Better informed, planned and coordinated care. More empowered providers, consumers and planners. More effective targeting of resources (people, services, dollars etc). Outcome(s) A national system of EHR available to authorised consumers and providers. (the deliverables of the project) Availability of the best health information (clinical, evidence and service) to the right people, at the right time and place, and in appropriate forms – targeting the needs of a range of end-users ie consumers, healthcare providers, managers. Confidence in a national health information network in Australia (privacy, information storage and retrieval, governance etc). Improved quality (scope and nature) of health data holdings. A sustainable business model (eg incentives framework). Better equipped health workforce – ie information use, decision making etc. 2.3 The HealthConnect Concept In 2000, the National Electronic Records Taskforce defined an EHR (Electronic Heath Record) as: “An electronic, longitudinal collection of personal health information, usually based on the individual, entered or accepted by health care providers, which can 23 HealthConnect Business Architecture v1.9 be distributed over a number of sites or aggregated at a particular source. The information is organised primarily to support continuing, efficient and quality health care. The record is under the control of the consumer and is stored and transmitted securely.” In the context of HealthConnect, a consumer’s EHR will consist of a series of event summaries (subsets of the complete information recorded by providers for a given health event and not aimed at replacing local health records). The event summary is analogous to a document containing key information for a specific health care event such as general practitioner consultation, hospital admission or discharge, pathology test or a pharmacy dispensing a prescription. HealthConnect is a cooperative venture between the Australian, State and Territory Governments to implement a national EHR solution which will operate seamlessly and consistently across Australia, with the same rules for privacy, identification, registration and consent applying everywhere. Each time a consumer has contact with the health system (including at a general practitioner’s surgery, specialist rooms, hospital, community health centre, pharmacy), a standard event summary will be created and sent, subject to consent arrangements, electronically to a HealthConnect repository. These event summaries form a summary health record for the consumer which will then be available when it is required to help with making decisions about the consumer’s healthcare. HealthConnect’s primary focus is to improve the availability of relevant consumer information in the delivery of healthcare so as to achieve better continuity and quality of care, consumer safety and health outcomes. HealthConnect’s primary function is to receive, store, retrieve and deliver electronic health record (EHR) information for use in the delivery of health care. HealthConnect will also provide simple notifications. HealthConnect will provide the information needed to support other functions, such as clinical decision support, but will not itself provide these functions. HealthConnect will support secondary use of EHR information for improvement of health service delivery and research purposes, in line with strict policies, appropriate legislative requirements and monitoring of such use. A number of components are considered fundamental to the development of HealthConnect, namely: · HealthConnect Participants · HealthConnect Event Summaries · EHR Repository · EHR Lists · EHR Views · EHR Reports These components are illustrated in the figure below. 24 HealthConnect Business Architecture v1.9 HealthConnect Participants For example: · · · · Event Summaries Consumers HealthConnect Repository General Practitioners, Specialists Community nurses Event Summaries including: · Healthcare consultations Private allied health care providers eg. physiotherapists, podiatrists, optometrists Community pharmacists · · · · EHR Views Hospital clinicians · · · Diagnostic test results Hospital discharge information Immunisation information Emergency department clinicians Aged care workers EHR Lists including: · Current medications Secondary Users · Researchers · Managers//Planners · Evaluators · · Principal diagnoses Allergies and alerts EHR Reports Figure 2.1 Key Components of HealthConnect · Consumer participation in HealthConnect will be voluntary and nondiscriminatory. Non-participation must not limit the availability of any health service to the consumer. · Enrolment in HealthConnect is available to all Australian citizens and residents of Australia. While HealthConnect is for all Australians, early implementation will focus on those likely to get greatest long-term benefit – those suffering chronic diseases, populations with high morbidity and infants. · Provider participation in HealthConnect will be encouraged and will be made available to all providers involved in the chain of health care delivery. While the initial focus is likely to include medical practices, pharmacies, hospitals, diagnostic services, health and aged care facilities and those practitioners currently participating in HealthConnect initiatives, this scope will be extended through arrangements with representatives of each provider group. · Each consumer EHR will comprise a collection of ‘event summaries’ which provide summarised information about healthcare events that are relevant to the ongoing care of a consumer. These event summaries will be produced according to defined metadata covering format, data items and allowable code sets. · The HealthConnect EHR repository is expected to comprise multiple health record systems (HRS). The EHR of each registered consumer will reside on one HRS. · HealthConnect will include the maintenance of EHR lists of critical information such as current medications, diagnoses and alerts. 25 HealthConnect Business Architecture v1.9 · Users will access data from the stored event summaries for an individual consumer through a series of pre-defined EHR views. Views will be developed to address specific needs of consumers and providers taking into account specific practice areas, conditions and treatment regimes. · Users will access data from event summaries across consumers, i.e. relating to populations, through EHR reports which will be extracted from the EHR databases in line with predefined requirements and strict approval processes; The underlying principles of HealthConnect are discussed more extensively in Section 3 HealthConnect Principles and the scope and functionality of the HealthConnect solution is detailed in Section 4 HealthConnect Solution. HealthConnect support for the Business Need HealthConnect, as a national EHR network, will address and support the business problems described above by: · The provision of timely information about consumers, available at the point of care, including emergency situations; · The provision of information that supports safer healthcare delivery, such as improved medication information during prescribing; · The provision of information supporting coordinated and shared care through increased recognition of the involvement of multi disciplinary healthcare providers and the availability of information at key transition points in service provision, such as during care handover between participating healthcare services; and · The provision of information for research, education, service planning and policy development. 2.4 The Business Case Extensive research and consultation has shown that, while there are significant costs associated with HealthConnect, there are considerable benefits to be realised and that, to the extent that quantifiable information is available, a sufficiently strong business case exists for proceeding with HealthConnect as the national EHR solution. The key benefits and costs are summarised below. Benefits of HealthConnect According to the draft HealthConnect Benefits Realisation Framework9, the implementation of HealthConnect in Australia is expected to deliver benefits that will accrue to consumers, providers and to the Australian health sector more generally. By improving access to a consumer’s health information across health care settings, HealthConnect would deliver benefits though increased coordination of care, enabling healthcare providers to provide a better quality of care to their consumers, and even a reduced number of adverse reactions, which would lead to improved health outcomes. 9 HealthConnect Benefits Realisation Framework V1.0 October 2004 26 HealthConnect Business Architecture v1.9 Moreover, the availability of HealthConnect records should reduce the amount of time providers spend chasing patient information, enabling their business to become more efficient. Financial Benefits of HealthConnect The HealthConnect Indicative Benefits Report (February 2004)10 analysed potential financial benefits attributable to HealthConnect. The report took a conservative approach to estimating benefits. After removing potential areas of double counting, the cost offsets from the implementation of HealthConnect were estimated to be in the order of $396m per annum should there be a 100% take up by consumers and providers. While it is recognised that a near 100% take up is not likely to happen for many years if ever, the analysis provides an indication of the level of benefits that could be achieved. The report also concluded that when fully deployed additional direct financial benefits could accrue giving a total indicative benefits range of $554m to $604m per annum. Cost of HealthConnect An analysis of the cost of HealthConnect was conducted as part of the research activities and summarised in the HealthConnect Interim Research Report (2003)11. The cost modelling of HealthConnect demonstrates that the overall cost is highly dependent on the registration process and to a lesser extent on the technical solution adopted. The one-off establishment costs are highly dependent on the approach to registration employed by HealthConnect. An intensive registration would require hundreds of millions of dollars, but a self-managed approach is expected to become the standard if HealthConnect were offered as a mainstream service. The major establishment components outside registration are expected to be: infrastructure deployment ($140 million); the change management program ($90 million, including training, support, and the organisational change studies); and system integration ($60 million). These establishment costs would be spread out over a number of years and therefore would be in the order of $30 million per annum over 10 years. Within this there would be an initial loading in years 0–5. It is anticipated that annual recurrent costs, including registration, would be in the order of $160 million. The major components of the ongoing cost are information technology operations ($100 million), information technology infrastructure replacement and application development ($35 million), registration ($5 million) and governance and management ($20 million). This would be a shared cost among all jurisdictions and, potentially, private sector partners. Indirect Costs of HealthConnect There are also indirect costs that are necessary to provide the underpinning structure of HealthConnect. The indirect costs of HealthConnect include development and implementation of: privacy, security and identification arrangements; information technology and data standards; computing infrastructure within participating 10 The HealthConnect Indicative Benefits Report was prepared by Fujitsu (formerly DMR Consulting) for the HealthConnect Program Office in February 2004. 11 The HealthConnect Interim Research Report, August 2003. 27 HealthConnect Business Architecture v1.9 organisations; workflow changes; and telecommunications infrastructure. These costs are substantial, (in the order of $2–3b). However, these costs will be incurred/are already being incurred with, or without, HealthConnect. Funding HealthConnect Based on the research undertaken, it is has been stated that it cannot be assumed that the private information technology industry sector will take on a substantial role as an investor/funder in the first few years of implementing HealthConnect, notwithstanding the substantial role of the private health care sector in providing the source systems feeding into HealthConnect. As evidenced by experiences with other e-government projects, the private sector is likely to invest in HealthConnect only after a proven business case for the private sector has emerged. And, as evidenced by overseas experiences, government needs to take a leadership role for implementation on a national scale, particularly with respect to standards and infrastructure development. The assumption at this point in time is that the majority of funding support in the early years would be provided by the public sector. Notwithstanding this, the implementation plan needs to allow for subsequent private sector involvement possibly through public private partnership models. There is also a major funding issue with private sector providers, many of which do not have the infrastructure and resources required for them to participate in HealthConnect. The need to encourage investment in areas such as infrastructure for general practitioners, specialists and private hospitals, will be addressed as part of implementations. 28 HealthConnect 3. Business Architecture v1.9 HealthConnect Principles This section presents high level principles which encapsulate the intent of HealthConnect, guide the development of its processes and systems and inform proposed implementation activities. These high-level guiding principles are grouped according to whether they relate to: · The Scope of HealthConnect; · Participation in HealthConnect; · HealthConnect Information Management; and · HealthConnect Technology Principles These high-level guiding principles have been adopted in the contemporary conceptual design of HealthConnect and are reflected, to the maximum extent reasonably possible, in the more detailed material presented in the various parts of this business architecture. 3.1 Scope of HealthConnect · HealthConnect’s primary focus is to improve the availability of relevant consumer information in the delivery of healthcare so as to achieve better continuity and quality of care, consumer safety and health outcomes. · HealthConnect will support a whole-of-health perspective encompassing private and public providers and continuity of care across primary, secondary and tertiary care settings including preventive health. · HealthConnect’s primary function is to receive, store, retrieve and deliver electronic health record (EHR) information for use in the delivery of health care and to support rather than provide additional functions, such as clinical decision support, other than simple notifications. · HealthConnect will not replace providers’ own clinical records or clinical information systems. Providers will continue to maintain their own consumer health records but may choose to incorporate selected HealthConnect EHR information in their records or clinical information systems. · HealthConnect will encourage development of value-added services. HealthConnect’s contribution to improving health outcomes can be greatly enhanced by stimulating development of other complementary systems and services such as clinical decision support and health call centres. · HealthConnect will support secondary use of HealthConnect EHR information for improvement of health service delivery and research purposes, in line with strict privacy and ethical protocols, appropriate legislative requirements and monitoring of such use. 29 HealthConnect Business Architecture v1.9 · To the maximum extent possible, HealthConnect implementations will support, use, and facilitate the development of national health infostructure and work closely with the National eHealth Transition Authority (NEHTA) and the longer term entity. Key infostructure areas include the national provider directory, national health consumer identifier, health metadata repositories, health information standards, approved terminologies and health data sets such as the Australian Catalogue of Medicines. · From stage 1 onwards, the scope of HealthConnect will expand to encompass new types of providers and information. Core HealthConnect systems and services for receiving, storing, retrieving and delivering EHR information must be able to accommodate this expansion with minimal redevelopment or replacement. · HealthConnect will potentially support registers through the provision of information such as diagnosis and treatment information on which specialist registries may be built. In the future it may also support registers such as notifiable diseases databases. · Any changes to the business boundaries of HealthConnect, required over time, will be controlled and be on a national basis. This would potentially include changes to the definition of core services to reflect evolving business requirements. A number of issues requiring future decisions have already been identified; these include the scope of consumer contributions to their health record. · Ongoing management of the HealthConnect program at the national level will be vested in a dedicated organisational entity on behalf of all the participating governments and other stakeholders. This organisational entity is commonly referred to as the HealthConnect governing body. 3.2 Participation in HealthConnect Consumer Participation · Enrolment in HealthConnect is available to all Australian citizens and residents of Australia. While HealthConnect is for all Australians, early implementation will focus on those likely to get greatest long-term benefit – those suffering chronic diseases, populations with high morbidity and infants. · Each consumer and their EHR information will be uniquely identified within HealthConnect by use of a single unique identifier able to be linked to any future National Health Identifier. This is currently being researched by the National eHealth Transition Authority (NEHTA). · Consumer participation in HealthConnect will be voluntary and nondiscriminatory. Non-participation must not limit the availability of any health service to the consumer. · The consumer must have given informed consent before their EHR and other personal information can be collected, accessed, used or disclosed by HealthConnect. This will form part of the initial consumer consent process. 30 HealthConnect Business Architecture v1.9 · Consumers will be free to deregister from HealthConnect at any time, without suffering discrimination in terms of access to healthcare. · Consumer consent for participation in HealthConnect remains valid until deregistration. · Consumers will have control over who may access their HealthConnect EHR. At any time, the consumer will be able to nominate (and to vary or revoke the nomination of) provider organisations that may access their EHR. · Consumers will have access to HealthConnect to view and, in the future, contribute to their EHR information and, also, to review the access log for their EHR and to set preferences that control access to the EHR. To do this, the consumer must be identified to HealthConnect – usually by giving their unique HealthConnect identifier and another form of identification (eg a PIN). · Each consumer will be able to nominate (and vary or revoke the nomination of) one or more agents capable of accessing HealthConnect on behalf of the consumer. An agent may be any person formally nominated by the consumer and capable of being identified to HealthConnect. Other persons able to access the EHR on behalf of a consumer include legal representatives such as parents (for a child), a legal guardian or person with power of attorney over the consumer’s health care. · Consumers will, as part of the sign up process, consent to an “emergency access override” facility. This would entail their EHR being accessed by any provider delivering clinical care in an emergency, where the consumer is not in a position to otherwise give their consent e.g. where consumer is unconscious or otherwise unable to provide immediate consent at the time of service. This type of access be tightly controlled, and will be closely monitored with audit trails and follow up processes being maintained. · Consumers, at the time of a consultation, may require personal information to be withheld from HealthConnect. The provider will, on request, not send the event summary or delete the information prior to sending the event summary. Provider Participation · Provider participation in HealthConnect will be encouraged and will be made available to all providers involved in the chain of health care delivery. While the initial focus is likely to include medical practices, pharmacies, hospitals, diagnostic services, health and aged care facilities and those practitioners currently participating in HealthConnect initiatives, this scope will be extended through arrangements with representatives of each provider group. · A person practising as a health service provider who is recognised for professional registration in an Australian jurisdiction will be eligible to register with HealthConnect as an individual provider. This will require their professional registration body to have been previously recognised and registered with HealthConnect. · A registered business (including a sole trader) that delivers health services using the services of one or more individual providers will be eligible to register with HealthConnect as a “provider organisation”. This could range 31 HealthConnect Business Architecture v1.9 from small general practitioner practices to major hospitals and area health services. · Provider participation in HealthConnect will be voluntary and will remain active until the provider gives HealthConnect a request to deregister or the provider is no longer eligible to participate in HealthConnect (as determined by the rules governing the operation of HealthConnect). · Individual providers and provider organisations will be required to sign HealthConnect agreements outlining their responsibilities at time of registration. · Each provider (individual or organisation) will be uniquely identified within HealthConnect by use of a single unique identifier linked, in the future, to the National Provider Directory. · HealthConnect will allow any registered individual provider acting on behalf of a provider organisation that has been authorised by the consumer to access the consumer’s EHR for the purpose of providing health services to the consumer. · A provider’s organisation must have the consumer’s consent prior to an individual provider accessing a consumer’s HealthConnect EHR. This consent would typically be set up at registration or the first time the consumer presents at the provider organisation’s premises. · Provider access to view a consumer’s HealthConnect EHR implies that the provider requires access to the information for clinical purposes. All access will be audited and providers may be requested to provide reasons for an access event. · Each provider organisation will be responsible for controlling its personnel’s use of HealthConnect information and for ensuring that the individual provider (or any other person) accessing the consumer’s EHR on behalf of the provider organisation does so for valid clinical reasons, and that the provider/person is identified to HealthConnect. · Providers once authorised will be able to access all parts of the consumer’s HealthConnect EHR. HealthConnect will not determine which parts of the EHR are relevant to any individual health encounter and therefore not restrict access. As the range of providers widens there will need to be a review of this principle; this will be based on additional research and policy work to be undertaken as part of the implementation phase. · All access to a consumer EHR will be logged and able to be tracked back to individual - provider, consumer or other authorised person. · HealthConnect participants will be obliged to abide by privacy legislation and by specific HealthConnect privacy rules. The National Health Privacy Code will be used when it has been implemented, until then privacy arrangements will be tailored to suit each jurisdiction for each implementation, with a view to progressing towards a single national solution. 32 HealthConnect · Business Architecture v1.9 Providers are responsible for the security of any EHR information integrated into their clinical information systems. Once HealthConnect EHR information has been entered into a local system, the owner of that system has responsibility for the security of the information. 3.3 Information Management Principles · Each HealthConnect EHR will comprise a collection of ‘event summaries’ which provide a subset of information about healthcare events that are relevant to the ongoing care of a consumer. These event summaries will be produced according to defined metadata covering format, data items and allowable code sets as developed by the Clinical Information Project. · Separate event summaries will be submitted for each healthcare event e.g. a hospital stay, an emergency department presentation, a community nurse visit, pathology test(s). An event may cover a number of treatments e.g. a series of chemotherapy treatment events may be represented by an admission summary and a discharge summary. Different types of event summaries will be developed over time in line with business needs. · Event summaries should be available as soon as possible after a health event and hence, as far as practicable, should be submitted directly following the completion of an event. Failure to do so may adversely impact on some of the functions of HealthConnect such as the provision of script information to pharmacists at the time of dispense. · Users will access data from the stored event summaries for an individual consumer through a series of pre-defined ‘views’. Views will be developed to address specific needs of consumers and providers taking into account specific practice areas, conditions and treatment regimes. · Users will access data from event summaries across consumers, i.e. relating to populations, through ‘reports’ which will be extracted from the EHR databases in line with predefined requirements and appropriate approval; · HealthConnect will not perform any clinical validation of the data in the event summary. It will take reasonable steps to ensure that any personal health information held is accurate, up to date and relevant to the HealthConnect functions and activities by validating the type of information contained in the event summaries, but not assessing the clinical content. · HealthConnect will promote a focus on data quality checking in source systems. Improving the quality of data at the time of entry is critical to ensuring that the HealthConnect EHR information is meaningful and useful in assisting healthcare delivery. · HealthConnect will include the maintenance of ‘lists’ of critical information such as current medications, diagnoses and alerts. · Information, once submitted to HealthConnect, may not be deleted or altered; however corrections or amended information may be included in the EHR by issuing revised versions of the information which will be used in place of the earlier versions with appropriate annotations. Access to view an event 33 HealthConnect Business Architecture v1.9 summary can be removed. Operational based changes to maintain database integrity will be closely managed and controlled. · Each entry in a consumer’s HealthConnect EHR must be attributed to an individual provider, on behalf of an authorised provider organisation, the consumer or another person authorised to add information to the EHR. The event summary formats will control the type of information which can be added. Requests for information from the EHR will also be attributable to an individual. · The EHR data will be permanently recorded and preserved subject to legal constraints. Upon a consumer’s death, processes will be put in place to limit access to those with a need eg for activities in relation to death certificate issue, autopsy or coroner investigation and for secondary uses. Rules controlling these processes will be established by HealthConnect in line with privacy legislation. · If a consumer deregisters from HealthConnect, the information in their HealthConnect record will be withdrawn from view, but will not be deleted. It will continue to be available for de-identified secondary reporting uses. · Each implementation of HealthConnect must fully support: (a) use of the HealthConnect consumer identifier to identify consumers and their EHR information; and (b) use of the HealthConnect provider identifier for authentication of event summaries and control of access to EHR information. · All implementations of HealthConnect HRS services must support interoperability. This requires that all implementations must be able to perform the core functions of HealthConnect, and be able to handle standard HealthConnect interactions with provider systems and national HealthConnect infrastructure throughout Australia. Any implementations not able to achieve full interoperability in the short term must have clearly defined migration paths aimed at achieving the required level of interoperability. · The use of standard terminologies in the provider source systems will be heavily promoted. This will be critical to the grouping of key data into meaningful lists and for the provision of appropriate information to support clinical decision making. · The HealthConnect data model must be extensible to accommodate evolution of the content and format of EHR information over time. 3.4 Technology Principles Integration with clinical systems · Providers will interact with HealthConnect primarily through their clinical information systems. A standard web-browser interface to HealthConnect will be available for consumers. A provider web-browser interface will also be available for providers whose systems do not have the capacity to interact with HealthConnect. This will be phased out over time. 34 HealthConnect · Business Architecture v1.9 HealthConnect will aim for access to HealthConnect to be integrated into the providers’ clinical information systems and as far as practicable streamline access and keep to a minimum impact on provider work practices. Standards and conformance · HealthConnect will use existing health informatics standards and seek to cater for emerging standards to support local and national perspectives, and in the future the potential sharing of EHR data on a global scale. · HealthConnect will support standards proven and supported by industry. · The structure of messages must conform to Australian standards accepted for use within HealthConnect and these standards must be supported by all systems participating in HealthConnect. · Participating organisational systems and personal provider IT devices must be demonstrably compliant with appropriate published security policies and standards that have been endorsed by HealthConnect. · Software developed to interact with HealthConnect records systems will be tested and accredited to the standard endorsed by HealthConnect. Storage and Access · The entire EHR of each registered consumer will reside on one and only one HRS. · HealthConnect will receive EHR information sent by providers and consumers and provide information in response to requests from users. Providers and consumers will initiate and control their interactions with HealthConnect; however standing requests for notifications related to specified consumer EHRs will be supported where the provider organisation has access to the EHR. · For participation in HealthConnect, a HRS must allow any provider registered with HealthConnect acting on behalf of a provider organisation that has authority to access the consumer’s EHR information stored on that HRS. This includes access both for viewing and update of the EHR. · Each HealthConnect Records System will aim for continuous availability. A target of 99.9% availability is being sought. · Systems and services for receiving, storing, retrieving and delivering HealthConnect EHR information should be extensible i.e. designed to adapt to the growth of HealthConnect in terms of provider types and clinical information content. The capacity and capability of HealthConnect will grow in terms of provider types, event summaries, views and lists and facilities must be flexible enough to cater for this change without replacement. · HealthConnect data structure, systems and processes must be designed to maintain backward compatibility and integrity of the stored data so that information may be reproduced through time. 35 HealthConnect Business Architecture v1.9 Other Initiatives · Implementations of value added services are outside core HealthConnect functionality. Individual implementations of HealthConnect may include optional value added functionality to address local requirements. While these will be encouraged, they are related systems and must be implemented such that they do not affect the compatibility of the HealthConnect implementation with the national standards. · Implementations of HealthConnect are likely to build on the messaging service it requires and conduct, as an adjunct to the core service, an implementation of a wider eHealth message bank service to support other health communications. 36 HealthConnect Business Architecture v1.9 The HealthConnect Solution 4. This section presents the HealthConnect solution from a business perspective. It addresses the: · Broad scope of HealthConnect; · Context of HealthConnect in terms of participants and roles; · National network of EHR repositories known as HealthConnect Records Systems (HRS); and · Key functions of the HealthConnect system and the associated information flows. Topics such as who uses the services, who provides the services or where the systems and services reside, will be discussed later in the document in Part C Participant Involvement and Part D Description of HealthConnect Components. 4.1 HealthConnect Context 4.1.1 HealthConnect Scope Over the last three years considerable effort has been focussed into research aimed at scoping HealthConnect. This research has concluded that HealthConnect should be kept relatively simple – focusing on the acceptance, validation and management of event summaries to construct an EHR for each consumer, and the use of EHR information to create views. Summarising the HealthConnect Principles, the scope of HealthConnect can be encapsulated in the statement: “HealthConnect will be a repository service for consumers’ lifetime health records.” HealthConnect will complement rather than replace providers’ systems. The focus will be on sourcing event summaries from these systems and providing information required for the selected views. HealthConnect will enhance the decision-support ability of provider clinical information systems by ensuring that the information about the consumer being treated is more complete than otherwise possible. At least in the initial stages of HealthConnect, for providers who do not have clinical information systems able to create event summaries, a web portal will be available for direct entry of event summary data; however, this is not seen as the preferred method of event summary entry for the long term. For consumers, a web based front end will be developed for ongoing use. HealthConnect, through the supply of EHR information, will act as an enabler to the development of other complementary systems and services such as clinical decision support and health call centres. HealthConnect implementations will support, use, and facilitate the development of national health infostructure such as the national provider directory, national health identifier, health metadata repositories, health information standards, approved terminologies and health data sets. It is recognised that this infostructure may not be 37 HealthConnect Business Architecture v1.9 available for the early implementations. HealthConnect will need the capability to link to them as they become available. HealthConnect will potentially support registers, such as the Australian Childhood Immunisation Register, through the provision of information, but will not of itself provide full registry functionality. 4.1.2 The HealthConnect Participants HealthConnect’s primary users will be those users seeking consumer health record information to assist in decision making related to the provision of health services, namely: · Providers (including doctors, nurses, pharmacists, allied health, community health, Aboriginal and Torres Strait Islander health and public health practitioners) and public and private provider organisations seeking information about the consumer they are treating; and · Consumers reviewing and adding to their own health records. There will also be a range of secondary users including: · Researchers seeking information to conduct research needed for improving health care and its delivery; · Planners and Managers (including administrators, strategic planners, policy makers, funding bodies) seeking information to assist management decision making; and · Evaluators seeking information directly related to monitoring the effectiveness of HealthConnect. The provision of data for secondary uses will only be allowed under strict privacy and ethical protocols, appropriate legislative requirements and monitoring of such use. Stakeholders In addition to these five broad groups of participant stakeholders, there is a sixth group which is key to the success of HealthConnect but will not generally be made up of direct users of the system. Members of this group include: · Consumer representative groups (eg Consumers’ Health Forum, National Aboriginal Community Controlled Health Organisations, Health Consumers of Rural and Remote Australia); · Provider representative groups (eg Australian Medical Association, Royal College of Nursing Australia, Australian Nursing Federation, Pharmacy Guild of Australia, Pharmaceutical Society of Australia, Society of Hospital Pharmacists of Australia, Australian Divisions of General Practice, Australian Physiotherapists Association, Medical Colleges including specialist colleges and the Royal Australian College of General Practice, Australian College of Rural and Remote Medicine); 38 HealthConnect Business Architecture v1.9 · The health IT industry, who will provide the applications, systems, services and staff to deliver HealthConnect functionality and support infrastructure (represented by groups such as the Medical Software Industry Association (MSIA) and Australian Information Industry Association(AIIA)); · Healthcare-related organisations such as the Australian, state and territory departments of health and/or human services, the Health Insurance Commission; and · Health information providers, academics, publishers and health libraries. 4.1.3 HealthConnect Service Roles and Services Figure 4.1 below illustrates the major roles/services associated with the delivery of HealthConnect services. This role map includes both roles performed within HealthConnect itself, roles performed by the associated national bodies and roles performed within associated participant entities. Those roles contained within the dotted lines are considered core HealthConnect roles. National Health InfoStructure Secondary User Consumer Consumer Registration & Management HealthConnect EHR Repository Provider Registration & Management HealthConnect Consumer Access Services Provider Provider eHealth Access Services Value Added eHealth Services eHealth Message Bank Service Supporting ICT Infrastructure Figure 4.1 Key HealthConnect Roles and Services Ongoing management of the HealthConnect program at the national level will be vested in a dedicated organisational entity, the HealthConnect governing body, acting on behalf of all the participating governments and other stakeholders. 39 HealthConnect Business Architecture v1.9 The roles/services associated with the delivery of HealthConnect may be grouped as follows: 1. HealthConnect participants - consumers, providers and secondary users. 2. Core HealthConnect roles, including those for: - registration and management of consumer and provider participation; - maintaining the HealthConnect EHR repository; including the individual Health Record Systems and the National Data Store , - managing the structure and content of EHR information, including the HealthConnect Metadata repository; - evaluating program performance; and - governing the interaction with HealthConnect. 3. HealthConnect Consumer Access Services that support customer interaction with HealthConnect and may also offer additional services of interest to consumers. 4. Provider eHealth Access Services that support providers interacting with HealthConnect. 5. eHealth Message Bank Services, an adjunct to the core services, to facilitate electronic information interchange for both HealthConnect and other purposes, such as electronic retrieval of prescriptions, referrals and notifications. 6. Supporting HealthConnect ICT infrastructure, which includes secure networks, IT processing platforms, clinical applications and the organisations that provide and support these services. 7. National Health Infostructure, which provides national repositories and information definitions that underpin the operation of HealthConnect. This includes the proposed National Health Identification Service (Consumers) and, national Provider Directory/Index; the National Health Metadata Repository and terminologies and data sets, such as the Australian Catalogue of Medicines. 8. Other contributors and recipients of information – specifically value-added eHealth services and (potentially) health registries. These roles are discussed in more detail in Part D Description of HealthConnect Components. 4.2 HealthConnect System Having discussed the context and scope of HealthConnect above, this section presents a high-level discussion of the HealthConnect EHR, the key functions of the HealthConnect system and the associated information flows from a business perspective. More detailed descriptions of HealthConnect components can also be found in Part D Description of the HealthConnect Components. 40 HealthConnect 4.2.1 Business Architecture v1.9 The HealthConnect EHR HealthConnect intends to complement the provider’s records by facilitating the sharing of summary healthcare information, in the form of standardised event summaries and composite views of information in event summaries, between providers that are involved in the care of a consumer. The EHR will also be accessible to the consumer, other people nominated by the consumer and those with a legal responsibility for the consumer’s health care. The HealthConnect EHR is not intended to replace the provider’s own detailed consumer records and health record systems, but should be able to supply information that can be stored and used by such systems to better support health care delivery. The EHR will contain clinical information that is of relevance to other providers. It is proposed that the EHR will be comprised of a series of event summaries, each of which will contain summary information relating to the services provided at a given healthcare event. Users will access data from multiple event summaries through a series of predefined views (relating to individuals) and reports (relating to populations). It is expected that views and reports will be developed for specific practice areas, conditions and treatment regimes. The Clinical Information Project, a major project contributing to HealthConnect, is developing the initial set of event summaries and views in consultation with consumer and provider representatives. HealthConnect will also send users notifications based on analysis of the type of event summary or the information contained in the event summary. Notifications based upon clinical content will not be supported initially. 4.2.2 The HealthConnect EHR Repository HealthConnect will establish a shared electronic health record (EHR) for consumers and a national network of secure EHR repositories known as HealthConnect Records Systems (HRS). HealthConnect is to be implemented as a federation of HealthConnect Records Systems (HRS) supported by common services at a national level, with each consumer’s EHR being stored in a single HRS. A copy of the EHR material is to be transmitted to the National Data Store for archiving and long-term retention. Together, the EHR information held in each HRS and the National Data Store will comprise the HealthConnect EHR repository. Whilst the HealthConnect EHR repository may be distributed across a number of federated elements, it is intended that it be available as a single national resource from the viewpoint of access, interoperability, reporting and inquiry. Within this framework, it is proposed that the National Data Store be used to support all secondary use of HealthConnect EHR data for research and planning purposes, while all operational interaction with a consumer’s EHR will occur through the HRS. Access to the National Data Store will be limited and will generally be for de-identified record analysis. This will be tightly controlled. Each HRS is a system that provides EHR storage services. The HRS will act as a library of EHRs, storing event summaries on behalf of the consumer and ensuring that the entire record is accessible 24 hours a day in accordance with the consumer’s privacy 41 HealthConnect Business Architecture v1.9 rights and the nationally-agreed security and access control policies. The primary functions of the HRS are: · to store event summaries that are contributed to the EHR by participating consumers and providers; · to maintain the confidentiality, integrity, availability and non-repudiation of an individual consumer’s EHR; · to present views of the EHR in response to requests by participating consumers and providers, subject to the consumer’s consent and the privacy, security and access control policies established by HealthConnect. For participation in HealthConnect, an HRS must allow any provider registered with HealthConnect acting on behalf of a provider organisation that has authority to access the consumer’s EHR information stored on that HRS. This includes access both for viewing and update of the EHR. It is envisaged that there will be a limited number of HRS implemented across Australia each of which may be operated by public or possibly private organisations referred to as “Approved EHR Managers” (AEMs). Further details of the system environment are presented in Part D Description of HealthConnect Components. 4.2.3 Core HealthConnect EHR Functionality The focus of HealthConnect is to be kept relatively simple – focusing on the acceptance, validation and management of event summaries, the maintenance of the consumer’s EHR and the use of EHR information to create views and reports. HealthConnect will provide information in standardised electronic formats that may be more readily used by clinical information systems and newer applications external to HealthConnect such as expert clinical decision support systems. The figure below illustrates the boundaries of the key HealthConnect functions (contained within the dotted line) and relationships to the receipt and provision of EHR information, followed by brief descriptions. The main functions discussed in this section are: A. Create Event Summaries B. Manage access to EHR Information C. Incorporate into Local Records D. HealthConnect Notifications E. Secondary Uses F. eHealth Value Added Services G. eHealth Message Bank Services 42 HealthConnect Business Architecture v1.9 As indicated in Figure 4.2 the main function of HealthConnect, apart from maintaining the EHR repository, is receiving and sending messages. The specific functions of creating event summaries, views, conducting clinical analysis etc are conducted by end user tools such as: · Provider clinical information systems, consumer access tools and registers; · Specialist clinical and consumer health tools; and · Research and planning tools The functions associated with the registration of consumers, providers and other users are discussed in Part C Participant Involvement. Via Provider systems, consumer tools A. Event Summaries Provider: · Hospital Discharge · Emergency Discharge · Pharmacy · GP Consultation · Specialist Consultation · Diagnostic tests (pathology, imaging etc) · Allied Health · Community Health etc Consumer (future): · Diary · Event summary Research/planning tools E. Secondary Uses · Clinical research · Health policy HealthConnect EHR Repository Provider eHealth Access Services D. Notifications Examples: · Admission/discharge · Registers Specialist clinical & consumer health tools F. eHealth Value Added Services Examples: · Medication management · Evidence based analysis G. eHealth Message Bank Services (related initiative) Eg: Referrals, results, prescriptions Via Provider systems, consumer tools B. EHR Views/Lists Examples: · Critical View (Composite) · Individual Event Views · List Views C. Incorporation into local health record Examples: · Script details · Event summary · Medications list · Allergies, alerts etc. Figure 4.2 Key HealthConnect Functions and Interactions A. Create Event Summaries Event summaries will typically be created in the providers’ clinical information system and then transmitted to HealthConnect, which will receive and store the event summaries in the consumer’s EHR. HealthConnect will not proactively extract data from operational systems but will receive event summaries sent by the operational systems at the discretion of the consumer and system user. HealthConnect will work with the vendors of the provider systems to investigate ways of integrating the process of creating and sending event summaries into their systems. From the research and trials conducted it is apparent that not all providers have clinical information systems and that many of the systems that are in use may not be able to create the required event summary messages in the short term. 43 HealthConnect Business Architecture v1.9 Stage 1 of HealthConnect will therefore include a web based access portal tool to enable providers without an appropriate clinical information system to create event summaries online. The preferred solution for the longer term is for commercial vendors to address this requirement for all providers. There is also a future requirement for consumers to be able to create and maintain health diaries, create and send event summaries and add comments to their EHR. A web based access portal tool will be provided for this purpose. In the future, HealthConnect compliant Consumer Health Tools are expected to become available as commercially viable products. However the HealthConnect provided consumer tool will still be available to consumers that require it. B. Manage Access to EHR Information Retrieval of consumers’ EHR information will be through the provision of EHR views. An EHR view is a subset of a consumer’s EHR information and may consist of one or more complete event summaries or a collection of lists of specific items derived from one or more event summaries. Users, in addition to being able to access individual event summaries, will be able to select from a range of predefined summary views or lists. The types of views of an EHR to be provided by the HRS will include a ‘critical’ view containing information such as basic demographic data, diagnoses, alerts, allergies, adverse reactions and current medications, and recent history. HealthConnect will be responsible for providing the requested EHR information to the user’s clinical information system. HealthConnect will need to be able to receive and interpret a request for information, and retrieve and send the information. HealthConnect will only send the information as a result of a request for the information. The composition of the information in some views will be targeted to a specific type of user. A key aspect of the definition of views will be the maintenance of the integrity of the information presented in the view and ensuring that important components of an EHR are always included so that information cannot be misinterpreted by being seen out of context. There will be a requirement to interface to a wide range of consumer and provider systems including: · clinical information systems – hospital, specialist, general practitioner systems; · provider group tools eg shared care, health call centre systems; and · consumer health tools eg consumer diary, self monitoring, and care management advice tools. As with the event summary creation, it is acknowledged that not all provider systems will be in a position to provide this functionality in the short term and that initially a web based ‘viewing’ tool will be provided as part of services available through the access portal. 44 HealthConnect Business Architecture v1.9 Within this model there are still opportunities for a level of integration with the clinical information system such as automatic initiation of a HealthConnect session upon opening a consumer record locally and transmission of clinical context information. The web-based HealthConnect consumer access tool will include development of ‘consumer-friendly’ viewing functions. Generalised ad-hoc query of information within a HealthConnect EHR will not be available from HealthConnect; (however, secondary uses will be facilitated through the provision of ‘reports’ – discussed below). The use of predefined EHR views (some of which are expected to include search parameters) will ensure that the results of requests represent clinically valid data and that the processing workload which would be required to service queries do not adversely impact performance of the overall HealthConnect system. C. Incorporation into Local Record Once the EHR view information has been delivered to a provider system, this may be stored temporarily and used when displaying the data. A user may wish to browse extensively through the available views of the EHR data, and possibly print out selected views, or even store a full copy in the same way they would store any externally supplied report, such as a referral. Alternatively, the user may wish to incorporate specific data into their local clinical information system, particularly for use in decision support systems for activities such as interaction checking. The type of information to be incorporated might be: · Individual event summaries stored as a report attached to the local record; or · Selected lists eg medications, diagnoses, allergies, alerts, adverse reactions incorporated into the appropriate part of the local database. This incorporation facility will depend on the capabilities of the clinical information system and may be set up within the system to take place automatically or as a result of a user initiated request. HealthConnect will encourage and support this functionality as it is seen to be important for realising key safety benefits. D. HealthConnect Notifications HealthConnect will support simple notifications relating to time, events and data codes, for example, admission notice, discharge notice or overdue notice. Notifications based upon interpreting the clinical content of an EHR will not be supported. Notifications can be sent to the provider organisations nominated in the consumer’s access control list. This list will be established and maintained as part of the consumer’s consent process. Organisations receiving these notifications will be responsible for actioning the notifications. The notification function could, if the business need is identified, also be extended to consumers; for example, to provide a Consumer Reminder Service for overdue appointments. 45 HealthConnect Business Architecture v1.9 HealthConnect could be developed to have the facility, should it be required, to provide a mechanism for facilitating the notification of notifiable events to national health registers. This would be particularly important for registers which require timely reporting, such as notification of infectious diseases. It should also improve collection of data for voluntary registers. Registers might include: disease specific eg cancer, implantable and other devices, organs, treatments, immunisations, births, deaths, research cohorts. While HealthConnect may provide limited support for some notifiable registers, it will not seek to replace any registers or become a registry service. This position will be reviewed in later years particularly if participation reaches very high proportions of the Australian population. HealthConnect will send all notifications on encountering the appropriate trigger without reference to any other notification that might have been sent. Any filtering to avoid double counting etc would need to be managed by the access service or the recipient (eg. a provider or register). E. Secondary Uses The HealthConnect repository will provide a valuable source of information which, under appropriate privacy and ethical protocols, can also be used for clinical research, policy making, planning and health outcome evaluation - collectively referred to as secondary uses. The provision of access to data for secondary uses will only be allowed under strict protocols. These will include information being aggregated or de-identified and ensuring authorisation has been given for the requested use. The focus of the secondary uses will be on analysis of de-identified data. Any research projects requiring access to identified information will only be allowed in accordance with current legislation detailed in the National Health and Medical Research Council (NHMRC) section 95 and 95A guidelines. These requests which may include epidemiological research, environmental research, and clinical research will be limited to special circumstances and subjected to stringent requirements, including assessment by appropriate ethics committees. Given the significant investment in the HealthConnect system, there will also be a need to monitor and evaluate the success of the system and seek ways to improve the quality of the service. As a minimum, this will require analysis of usage and outcomes to assess whether the overall objectives of HealthConnect are being met. The focus of the HealthConnect functionality will be on extracting the required information or ‘reports’ such that the analysis can be performed. Specialist research and planning tools used to analyse the data are outside the scope of HealthConnect. 46 HealthConnect Business Architecture v1.9 F. eHealth Value Added Services The functionality of the eHealth Value Added Services such as clinical decision support is outside the core HealthConnect functionality; however, interfacing to these systems and providing them with EHR data will be part of HealthConnect. Specifically HealthConnect will maintain lists such as current medications, prescribed medication, dispensed medication, current diagnoses and alerts and be able to provide these to provider clinical information systems to support clinical practice such as interaction checking and script processing functions. While not directly within scope, HealthConnect will be actively promoting the development and use of a range of eHealth value added services. G. eHealth Message Bank Service For HealthConnect to work, there will need to be considerable investment in the establishment of national health messaging services and communications networks with high levels of security and capacity. There has been extensive discussion about whether HealthConnect should build on this requirement to incorporate within its scope the provision of an eHealth Message Bank Service. This would particularly facilitate the provision of prescription details to pharmacies; a high-benefit service identified from the MediConnect field tests. If this requirement were to be addressed by means of an eHealth Message Bank Service developed in close association with HealthConnect, it would provide an opportunity for HealthConnect to support wider eHealth communications. Such a service could support transmission of messages between participating providers for services such as delivery of discharge summaries, prescription processing, referrals, diagnostic test requests and results. Being a service rather than an integral part of HealthConnect, it could also be extended to include all consumers of health care services and not just HealthConnect participants. Given the philosophy of containing the scope of HealthConnect, the HealthConnect business architecture does not include this wider eHealth Message Bank Service as part of the core functions to be provided by HealthConnect. It is however considered a critical adjunct service and the actual implementations of HealthConnect are expected to include coordinated implementation of these two major initiatives. 47 HealthConnect Business Architecture v1.9 Part C – HealthConnect Participant Involvement 49 HealthConnect 5. Business Architecture v1.9 Consumer Participation HealthConnect’s primary focus, as stated in the HealthConnect Principles, is to improve the availability of relevant consumer information in the delivery of healthcare so as to achieve better continuity and quality of care, consumer safety and health outcomes. To achieve this goal, a high level of consumer participation is required and considerable analysis into what being involved in HealthConnect will mean to consumers has been conducted. This section outlines the key elements of consumer involvement including: · Benefits of participation in HealthConnect; · Consumer consent arrangements for the stage 1 implementations of HealthConnect; · The process of consumer identification and registration; · Subsequent consumer interaction with HealthConnect; · Features of the HealthConnect Consumer Access Portal; and · Potential for value added eHealth services to consumers. 5.1 Benefits of HealthConnect to Consumers Analysis of consumer benefits have been conducted throughout the HealthConnect research and development activities, drawing on the experiences of the HealthConnect trials. A full analysis of the potential HealthConnect benefits is presented in the Benefits Realisation Framework12. In summary, the key benefits of HealthConnect specific to participating consumers include: 12 · the availability of critical consumer health information during a healthcare emergency; · facilitation of freedom of choice and freedom of movement, with the consumer’s heath record “following” the consumer; · the ability for a consumer’s health information to be brought together when it is needed – at the point of care; · the availability of consumer health information where consumers are not known to the provider, including first-time consultations and when working and travelling away from home; · more complete consumer medication records available to prescribers and dispensers, supporting greater medication interaction checking and fewer medication errors and associated adverse events; HealthConnect Benefits Realisation Framework V1.0 October 2004 51 HealthConnect Business Architecture v1.9 · reduced need for consumers to repeat their medical history to different care providers; · decreased incidence of unnecessary services; · better consumer care-coordination and care integration across providers, including more effective and efficient care transfer between care settings, through the availability of timely and accurate health information from participating providers; · decreased patient waiting and travelling time and fewer cancelled operations leading to increased patient satisfaction and increased health sector efficiency; and · gains from improvement in the provision of health services from the creation of new knowledge, more effective planning and allocation of resources. 5.2 Consumer Consent to Participate 5.2.1 Consent Principles A fundamental principle of HealthConnect is that consumers should give informed consent to participate in HealthConnect. This includes communicating clearly to consumers what HealthConnect is and what agreeing to participate means in practical terms. The key HealthConnect Principles relating to consumer consent are: · Consumer participation in HealthConnect will be voluntary and nondiscriminatory. Non-participation must not limit the availability of any health service to the consumer. · The consumer must have given informed consent before their EHR and other personal information can be collected, accessed, used or disclosed by HealthConnect. · Consumers will be free to deregister from HealthConnect at any time, without suffering discrimination in terms of access to any health service. · Consumer consent for participation in HealthConnect remains valid until the consumer deregisters. 5.2.2 Current Consent Model The following consent model, extracted from information provided in the consent business requirements, describes the arrangements to be implemented as part of the stage 1 HealthConnect implementation. Consumer consent arrangements, and how consent is managed, are probably the most sensitive aspects of HealthConnect. As such consent arrangements may evolve over time, though within the framework of the underlying principles. Considerable research has gone into the development of the consent model; any changes to the model that would require consumer re-consent would be prohibitively expensive. 52 HealthConnect Business Architecture v1.9 1. Consumer Registration Should a consumer choose to participate in HealthConnect they will need to register. As part of this process the consumer will need to sign a consent form specifically consenting to: (i) Conditions of participation Consumers will be given information about HealthConnect, how it will operate and how they can deregister at any time. (ii) Collection of initial health profile (optional) Consumer consent will be sought to gather background information about their health status in order to establish their HealthConnect record. Some of this information will be collected by directly asking the consumer questions (eg. social and lifestyle information) and some through retrieving information from their nominated provider’s electronic health systems. (iii) Nominate provider organisations Consumers will nominate service provider organisations who can access their HealthConnect records. Consent is at the provider organisation level, not the individual provider. Consumer nominations may be changed at any stage to reflect consumer choices. (iv) Emergency override Participation in HealthConnect includes allowing providers to have access to consumer HealthConnect records in an emergency situation where (a) consent has not previously been given, (b) the consumer is unable to consent and (c) no one else available to give consent. Where emergency override occurs, details of the access will be recorded in the access log and consumers will subsequently be advised of the emergency override. (v) Consent to secondary uses of data Consumers will be advised that consent to participate in HealthConnect will include consent for HealthConnect information to be used for approved secondary uses. For the majority of secondary uses de-identified data will be used; identified data may be used for limited research purposes, subject to independent scrutiny and National Health and Medical Research Council Guidelines. 2. Agents and legal representatives Each consumer will be able to nominate (and vary or revoke the nomination of) one or more agents capable of accessing HealthConnect on behalf of the consumer. An agent may be any person formally nominated by the consumer and capable of being identified to HealthConnect, including carers and family members. Other persons able to access the EHR on behalf of a consumer include legal representatives such as parents (for a child), a legal guardian or person with power of attorney over the consumer’s health care. 53 HealthConnect Business Architecture v1.9 Where the consumer is not able to sign the consent form or nominate their agents, the consent form can be signed on their behalf by a legal representative such as parent, guardian or someone who has power of attorney that extends to the right to make decisions about the consumer’s health care. Appropriate documentation will be required. Children will be able to consent on their own behalf if their medical practitioner provides a statement that the child has the requisite capacity to understand and make their own health decisions. Any nominated agent has the same access rights as the consumer themselves. Changes to a nominated and legal agent might occur at any stage. Policies and processes will be put in place to manage the potentially changing status of children’s consent. These are currently being investigated and are not yet finalised but might include: when a child reaches maturity giving them the option to withdraw from HealthConnect, and the option of making their parents/guardians their registered agents. Processes might include activities such as: sending out letters to children approaching maturity informing them of their rights; issue of separate cards, and expiry dates on registration of parents as agents such that it requires active renewal to stay valid. Policies and processes will be put in place to manage blocking of access for a parent or guardian should HealthConnect be instructed to do so and presented with official documentation such as a court order. 3. Subsequent episodes of care Consumers will be informed that they have the right to withhold information from HealthConnect at the time of the healthcare event. After the initial registration to join HealthConnect, summaries of all events occurring at registered provider organisations will be added to the consumer’s HealthConnect record unless: · the consumer requests that the provider not send the particular event summary, or request that part of the information be deleted before it is sent; and/or · the provider advises, and the consumer agrees, not to send the particular event summary or that part of the information be deleted before it is sent. An example might be a young teenager requesting that details of a particular consultation not be sent to their HealthConnect EHR to which their parents have access. Providers will need to assist the teenager in understanding the implications of sending or not sending the event summary. Hence, once a consumer has consented all event summaries generated by registered provider organisations will be sent to HealthConnect unless the consumer actively indicates otherwise. There is concern that not having access to all the facts may impede a provider’s ability to give appropriate care. It is assumed that the number of requests not to send information will be small, but that this feature is required to address consumer control and confidence issues. It will be provider’s responsibility to explain the implications to 54 HealthConnect Business Architecture v1.9 the consumer. Providers viewing the HealthConnect EHR will need to take into consideration that, as with manual records, the records cannot be considered 100% complete, but that the HealthConnect EHR provides a more complete picture. Indeed until HealthConnect is widely used there will be gaps in the record relating to providers who have not yet registered with HealthConnect. There have been discussions about the potential for establishing a ‘secret envelope’ section of the consumer’s EHR, where sensitive information can be placed with access restricted to certain providers. This functionality is not part of the scope for version 1 of HealthConnect. If further investigations identify that there is a strong business case for this requirement, and technical challenges related to its implementation particularly within provider organisations can be resolved, it will be considered for future implementations. 4. Amendment, correction and withdrawal of information from view Should clinical information on the record be considered incorrect, the consumer should raise the issue with the provider, or another provider from the organisation which submitted the original event summary. The provider may then if appropriate submit an updated version of the event summary containing the corrected information. The original and updated versions of the event summary will contain the identity of the provider submitting the event summary. Should factual information on the record be considered incorrect, the consumer will be able to request, via their HealthConnect Consumer Access Service, that it be changed. The rules determining whether a correction is made will be set out by the HealthConnect governing body and will be developed in consultation with appropriate organisations. A consumer will also be able to request that a comment be added to an event summary. The consumer may request that a particular event summary be withdrawn from view. This will mean that the information contained in the event summary will not be used to generate subsequent views of their HealthConnect information. In all cases the original information will be kept for medico-legal and audit purposes, but will no longer be disclosed by HealthConnect. 5. Deregistering from HealthConnect Consumers will be free to deregister from HealthConnect at any time, without suffering discrimination in terms of access to healthcare. 6. Complaints process The complaints process will be based on current practices, with private sector privacy complaints being directed to the Office of the Federal Privacy Commissioner and public sector privacy complaints to the Health Care Complaints Commissioner or state/territory body authorised to deal with privacy and health complaints in each jurisdiction. Health care related complaints will be referred to the relevant jurisdictional Health Care Complaints Commission. The possibility of a memorandum of understanding (MOU) with the Health Care Complaints Commissions is being investigated. If such an MOU 55 HealthConnect Business Architecture v1.9 is established, Health Care Complaints Commissions could investigate privacy complaints as well as health care complaints in the public and private sectors. A process will also be established for managing complaints about the operation of HealthConnect such as delays in registration processing. 5.2.3 Access Control Arrangements A key aspect of the consent process is the establishment of a list of provider organisations authorised to access the consumer’s HealthConnect record. It is expected that these provider organisations would generally be those routinely or potentially involved in the consumer’s care. Access control is at the provider organisation level, not the individual provider. Organisations not identified on the consumer’s list will not be able to access the consumer’s record, other than using the emergency override facility. Consumers will not be able, through HealthConnect, to deny access to an individual provider within an authorised provider organisation, though it may be possible for the consumer to address this requirement with the relevant provider organisation. It would be misleading to consumers to claim that denying access to the individual providers could be achieved unless organisational access control systems could also match the requirement. Once a provider from an authorised provider organisation has accessed the consumer’s record they may printout or download the information for incorporation into the local record. After this it is the responsibility of the provider organisation to control access. Providers registered with HealthConnect will be required to sign an agreement indicating that they will only access a consumer’s record as part of the process of delivering health care to the consumer. Within HealthConnect, all access includes the identity of the provider and provider organisation and the consumer will be able to review access logs and check whether who has accessed their record. Consumers will be able to change their HealthConnect access control arrangements in line with their changing healthcare needs, for example, changing their general practice or adding specialist groups to their list. The access control arrangements are without time limit and will remain in force until such time that the consumer changes them. Where access has been granted to cover some temporary situation, eg while on holiday, it is the consumer’s responsibility to remove the access rights when such access is no longer required. The potential for introducing time-limited access will be explored further in future versions of HealthConnect. Access control arrangements may be established and changed in a number of ways, including: · On enrolment in HealthConnect as part of the HealthConnect registration process; · At reception areas on first presenting to a healthcare organisation; · By attendance at nominated HealthConnect agency; 56 HealthConnect Business Architecture v1.9 · Directly by the consumer accessing their HealthConnect record through the HealthConnect web portal; and · By written instructions to HealthConnect. 5.2.4 Privacy of Consumer Records The success of HealthConnect will depend on consumers, providers and provider organisations having confidence and trust that health information is kept confidential and secure. To this end, a robust privacy framework, together with strong security measures, is required. Providers participating in HealthConnect will be obliged to abide by existing privacy legislation and by specific HealthConnect privacy protocols, covering access and use of information from consumers’ HealthConnect records, and contributing information to these records. Although a national health privacy framework is not yet in place, the National Privacy Principles and the proposed NHPC have informed the development of specific HealthConnect privacy common service principles. More detailed information on the privacy protocols is set out in Part E Implementing and Managing HealthConnect. 5.2.5 Consumer Responsibilities Consumer participation in HealthConnect comes with certain consumer responsibilities including: · making a decision whether to participate in HealthConnect; · maintaining consent arrangements so that providers from provider organisations of their choice can access their HealthConnect record when required; · being aware of the HealthConnect protocols that will operate in an emergency situation; · understanding the consequences of contributing to, or withholding information, from their HealthConnect record. It is important that consumers are aware that withholding information may directly impact the provision of healthcare services; · being informed on how to obtain access to their HealthConnect record and access log, including obtaining hard copies; how to complain or seek redress; and how to obtain more information on HealthConnect and its governance mechanisms; and · being responsible for the security and access control of any copies of their EHR information they may store on a local system. The consumer’s agents and legal representatives will have additional responsibilities in protecting the privacy of the record on behalf of the consumer. 57 HealthConnect Business Architecture v1.9 5.3 Consumer Registration 5.3.1 Identification of Consumers HealthConnect Principles state that: · Enrolment in HealthConnect is available to all Australian citizens and residents of Australia. While HealthConnect is for all Australians, early implementation will focus on those likely to get greatest long-term benefit – likely to be those suffering chronic diseases, populations with high morbidity and infants. · Each consumer and their EHR information will be uniquely identified within HealthConnect by use of a single unique identifier able to be linked to any future National Health Identifier. It is important that each consumer has only one HealthConnect identifier so clinical decisions can be made accurately and that information can be stored, retrieved and exchanged efficiently. Consumers will need to provide evidence of identification for registration to HealthConnect. Consumers will have the ability to change their identities on HealthConnect (for example, a change of name). Initially the criteria used for Medicare eligibility will be used as the criteria for consumers to participate in HealthConnect, though this will eventually be extended to accommodate consumers who are not eligible for Medicare. The same proof of eligibility documents accepted for Medicare registration will be used for HealthConnect enrolment. Where consumers have previously registered for a Medicare smartcard, this card will be sufficient evidence of both eligibility and identity for HealthConnect registration. 5.3.2 Initial Registration Process HealthConnect registration can occur in a number of ways, including: · registration at registration agencies acting on behalf of HealthConnect; · supported registrations, where additional time may be required for explaining HealthConnect concepts, for example, for elderly consumers, consumers with disabilities, or where registration occurs on behalf of another person; and · registration via a HealthConnect web based access tool (this would only be possible where consumers have previously registered for the Medicare smartcard and further identification is not required). The registration process will involve the consumer: · providing the evidence required to uniquely identify themselves; · providing written agreement to participate in HealthConnect, indicating an understanding of their rights as a consumer participating in HealthConnect, including consent arrangements; and 58 HealthConnect · Business Architecture v1.9 optionally, providing consent to collect initial health profile information to establish the health record. The HealthConnect agency will then: · issue a unique HealthConnect identifier and assign to the consumer a personal identification number (PIN), or equivalent, linked to the consumer’s HealthConnect identification number. This PIN will also allow consumers access to their HealthConnect records via web based systems; · set up the consumer’s HealthConnect record with consumer provided information and initial population of the list of provider organisations authorised to access the consumer record; and · initiate steps to collect the initial health profile information including obtaining information from the consumer and sending requests for information to the selected providers. All registration processes will be developed to facilitate access by people from a nonEnglish speaking background. Registration processes will also be developed to facilitate access by people with a disability. 5.3.3 Establishing the Initial Health Profile The collection of initial health profile information is initiated at the time a consumer registers with HealthConnect. This is an important part of establishing the record, particularly for consumers with chronic and complex conditions and where consumers have important allergies or alerts. For others, such as a predominantly healthy young adult, it is likely that only a simple initial health profile will be collected. All collection activities are subject to consumer consent with consumers being informed about the types of information and sources of information being sought. Consumers will subsequently be able to review the initial health profile and, if necessary, request changes. The initial health profile may comprise information from a number of sources such as: · family and social history information supplied by the consumer potentially through an on-line registration system; · information on recent events taken from the Medical Benefits Scheme (MBS) and Pharmaceutical Benefits Scheme (PBS) - what constitutes a recent event will be determined as part of the process; · summary information such as current diagnoses, allergies and medications, extracted from the systems of nominated providers, such as the consumer’s general practitioner or specialist; · details of inpatient and emergency presentations and procedures from hospital systems; and · selected records from registers such as the Australian Childhood Immunisation Register. 59 HealthConnect Business Architecture v1.9 While the information may come from multiple sources, only one source for each type of information will be permitted; HealthConnect will not include the ability to rationalise the data and resolve duplications and inconsistencies. The number and type of sources from which the information is sought will vary depending on the health status of the consumer. 5.3.4 Ongoing Identification After the consumer is registered there will be an ongoing need to identify the consumer to ensure appropriate and safe utilisation and management of their HealthConnect record. The main circumstances in which consumer’s identity will need to be authenticated are: · · Consumer-initiated - when the consumer or their authorised representatives wish to change registration and access control settings; - when the consumer or their authorised representatives wish to access their record or add information to their record; and Provider-initiated - when a provider organisation is requesting access to the record or wishing to add an event summary to the record. In the consumer-initiated situations the consumer will need to provide “two-tier” authentication. The specific details of the requirement will vary depending upon the setting and means of communication with HealthConnect. For example: · In a HealthConnect agency, through a kiosk, or at a provider organisation location with a smartcard reader available, the Medicare smartcard and consumer PIN will provide the required level of authentication; or · If accessing HealthConnect through a web browser the consumer’s HealthConnect identifier combined with the consumer PIN will serve the same purpose. Where a provider organisation is requesting use of the record, there is a necessary precondition that will need to be satisfied. That is, the consumer, or their nominated representatives, will need to have added the organisation to the consumer’s access control list. Upon the first presentation to the provider organisation, the consumer will inform the provider of their HealthConnect identifier either verbally or by producing the card. Where the smartcard and PIN are not used the provider organisation will need to follow an identification process as determined by HealthConnect to confirm the identity of the individual. The HealthConnect identifier can then be added to the consumer record in the provider’s system. The processes will be established to reduce the chance of incorrectly identifying the consumer or incorrectly entering the information. Once the provider organisation has been added to the consumer’s access control list and the consumer’s HealthConnect identifier is part of the consumer’s local record, the provider organisation’s system can access the consumer’s HealthConnect record. 60 HealthConnect Business Architecture v1.9 It will then be the organisation’s own identification processes which are relied upon to authenticate the consumer’s identity for any particular healthcare event. In this situation, the organisation is acting as a trusted agent of HealthConnect, with responsibilities set out in the organisation’s HealthConnect participation agreement. The HealthConnect Consumer Access Service will assist the consumer should they forget their PIN. Standard identification processes involving asking the consumer a series of questions including a ‘secret question’ will be used. These processes will also be used where a consumer has forgotten their smartcard or PIN when presenting to a provider organisation location for the first time to which they wish to give access. In the future additional processes will need to be put in place to manage the provision of access where the consumer is not present, and therefore not able to provide their smartcard. Situations of this type may include calls by the consumer to Health Call Centres. 5.3.5 Cancelling Registrations A consumer can deregister from HealthConnect at any time by completing and submitting the appropriate deregistration form. For consumers who cancel their registrations, information in their HealthConnect record will be withdrawn from view, but will not be deleted – this will be explained as part of the informed consent process. Any future event summaries submitted to HealthConnect will be rejected and providers will no longer be able to view the record. This information remains available for medico-legal purposes and, should the consumer wish to reinstate their HealthConnect participation at some stage in the future, the block on viewing could be reversed. Information in a ‘withdrawn from view’ record will also continue to be available for secondary reporting uses. Upon notification of a consumer’s death, processes will be put in place to allow access to those with a need eg for issue of death certificate, autopsy purposes or coroner investigation and for secondary uses. Procedures will also be put in place to handle the submission of any late and retrospective event summaries. When children reach maturity they may choose to cancel their registration, or possibly change their list of guardians and carers including to disable their parents’ access to their record. 5.4 Consumer Interaction with HealthConnect 5.4.1 HealthConnect Consumer Access Services HealthConnect Consumer Access Services (24x7) will be established to support customer interaction with HealthConnect and these may offer additional services of interest to consumers. The primary role of the HealthConnect Consumer Access Services (HCCAS) is to provide consumers with an effective means of accessing HealthConnect services and to give them front line support for using HealthConnect. Processes identified as being potentially associated with the HealthConnect Consumer Access Service role include: 61 HealthConnect Business Architecture v1.9 (a) Provide HealthConnect consumer access portal service (for consumers accessing HealthConnect via a web browser and via consumer health information systems) (b) Provide advice, assistance and training to consumers using or starting to use HealthConnect; (c) Provide consumer support to resolve HealthConnect access and usage problems; (d) Assisting to market HealthConnect to consumers and to facilitate consumer registration; and (e) Provide consumer access to value added services, potentially including supply of HealthConnect-compliant consumer health information systems. The key elements of the service – the HealthConnect Consumer Access Portal and the link to Value Added eHealth Services - are discussed in subsequent sections. 5.4.2 Consumer Access to their Health Record Consumers will have access to HealthConnect to view and, in the future, to contribute to their EHR information and, also, to review the access log for their EHR and to set preferences that control access to the EHR. This provision for consumers to access and contribute to their own electronic health record is a fundamental principle of HealthConnect. Empowering consumers and getting them more involved in the management of their own healthcare is an important objective of HealthConnect. There are a number of ways in which the consumer, or their nominated representative, could access their record, these include: · Directly through a HealthConnect Consumer Access Portal, which will be web based for version 1 of HealthConnect; · Via third party Value Added eHealth Services such as Consumer Health Tools or Shared Care Program Tools; · At any HealthConnect agency for specific tasks such as the provision of an audit trail report; · Using access points such as public kiosks, established at selected places such as HealthConnect agencies, hospitals and major health centres; and · Via written instructions to HealthConnect for specific tasks such as requesting the withdrawal from view of a particular event summary. 5.4.3 Consumer Direct Interaction Consumers may participate in HealthConnect simply so that their healthcare providers have access to their health information to assist in their treatment and management, and have no other ongoing interaction. Alternatively they may select greater levels of involvement, taking a more proactive role in HealthConnect and ultimately in their healthcare. 62 HealthConnect Business Architecture v1.9 Given that they have completed the registration process, signed the consent form, indicated which providers may access their EHR and been given a card and PIN, the type of interactions that consumers might have are: · (Necessary) Presenting their Medicare smartcard (or possibly in the future other HealthConnect smartcards) at the first presentation at a healthcare provider/organisation. The card will be read by the provider system and the PIN entered so that the details of the consumer’s HealthConnect number can be added to the local system and the consumer identified as a HealthConnect participant. The consumer will not need to present their card at subsequent visits to that particular health care provider organisation. Alternate processes will be put in place in the absence of a smartcard. · (Optional) Requesting an event summary is not sent to HealthConnect. At any stage a consumer may indicate to the provider they do not wish the details of the consultation to be sent to HealthConnect. The provider’s system will have the capability to accommodate this request. · (Optional) Updating access control preferences. This might be achieved by visiting HealthConnect agencies, writing to HealthConnect, or via the web based access portal provided by the HealthConnect Consumer Access Services. · (Optional) Using the web based access system, provided by a HealthConnect Consumer Access Services, to view or in the future to add to their record. · (Optional) Using the HealthConnect Consumer Access Services if they have any queries about HealthConnect operations. Consumers will need to take clinical queries to the relevant provider. · (Optional) Lodging of formal complaints through the appropriate HealthConnect complaints channels – a complaints procedure will be established. 5.5 HealthConnect Consumer Access Portal From the time of registration, consumers will have the ability to use a HealthConnect Consumer Access Portal to view and contribute to their HealthConnect record. This will initially be via a web browser system requiring the consumer’s HealthConnect identifier and PIN for access. The consumer’s nominated agents will also be able to use a Consumer Access Portal to access the consumer’s EHR by identifying themselves as an agent. This Portal may be accessed from their home computer or personal digital assistant (PDA), or possibly through third party systems such as information kiosks, work computers, Internet cafes or a relative’s or friend’s computer or PDA. Consumers may also download their record onto their computer and some consumers may purchase consumer orientated health software that allows them to maintain a local copy of their health record. Consumers will need to recognise that the local record will need to be updated as new event summaries are submitted to HealthConnect. The HealthConnect Consumer Access Portal will include the following functionality: 63 HealthConnect Business Architecture v1.9 1. Viewing and printing of their HealthConnect records, including: - Composite views that bring together key aspects of the consumer’s health information for ease of viewing. This might contain summary health status information such as current medications, diagnoses and alerts and recent investigation results; and - Individual event summaries, such as hospital discharge summaries, emergency department presentations, provider consultations and diagnostic results. 2. Consumer contributions to their HealthConnect records, which may in the future, include: - Creation of a consumer event summary. This might include direct entry of health information, for example self monitoring information such as weight, blood sugar levels and peak flows; - Addition of a consumer comment related to a specific event summary; and - Consumer diary functionality. The scope of these consumer contributions is discussed in more detail below. 3. Maintenance of consumer demographic and social information, important in an emergency situation, as well as for discharge planning following hospitalisation, including: - Contact details, including next-of-kin information; - Social circumstances, for example, independent living arrangements, family and work contacts; and - Social care agencies providing services to the consumer; 4. Maintenance of access control preferences that enable healthcare providers/organisations access the consumer’s HealthConnect record; 5. Consumer access control i.e. maintenance of PIN details; and 6. Audit review of access to the consumer’s HealthConnect record. This will include recording when and by whom information was viewed/printed. Additional consumer facilities may be provided through third party value added eHealth services as discussed below. Consumer Contributions The original HealthConnect business architecture suggests that consumers can submit their own event summaries to HealthConnect. Possible examples cited in the literature include consumer weight records, blood sugar readings, events such as “hypos”, pain management, lifestyle issues (diet and exercise), feelings/emotions, self-medication records and contributions to joint care-plans. Consumer contributions to their records were not included in the scope of the early trials, though the Tasmanian trial now allows consumers to submit event summaries. Therefore the requirements and issues in this area have not yet been defined and 64 HealthConnect Business Architecture v1.9 evaluated. Additionally, there are potential medico-legal issues with consumers contributing to their heath records, not least because of the expectation by consumers that their contributions will be reviewed, and acted upon by providers where necessary. Hence consumer submission of event summaries which are accessible to providers will not be included in the scope of the HealthConnect implementations at this stage. It is recognised that overseas experiences have demonstrated some successes in this area, and that it is likely that this type of functionality will evolve and become integrated into HealthConnect as the surrounding issues are resolved. Hence: · For version 1 of HealthConnect consumer access will be limited to viewing their EHR, and maintaining their personal details and access control list; · Subsequent implementations are likely to expand to include a consumer health diary, with the information within the health diary being owned by the consumer and intended to assist consumers in the management of their own healthcare. The consumer health diary information will not be available to providers as part of the consumer’s HealthConnect record, though mechanisms for access when the consumer is present may be established; and · Future implementations are expected to include consumer contribution to their records which can be accessed by providers; as the medico-legal and workflow concerns are resolved. The design of the health record systems should allow for this future requirement. 5.6 Consumer Value Added eHealth Services The HealthConnect Consumer Access Services will also provide mechanisms for linking to value added eHealth services which are outside the scope of HealthConnect. For example it is not proposed that the core HealthConnect functions include the provision of sophisticated consumer clinical decision making tools; though it is recognised that many of the benefits of HealthConnect will be realised through these systems/tools. Rather HealthConnect will promote the development of these tools by commercial and not-for-profit organisations and support their use by providing the required HealthConnect information on request and the promotion of the standards necessary to enable these tools to work safely and effectively. As in the US, these tools might be provided to consumers by private organisations to promote self monitoring and improve consumer management of their own healthcare. These facilities might be funded on a subscription basis or through reduced costs to healthcare providers. Consumer Health Tools Examples of these tools might include: · Consumer health tools which facilitate self monitoring and the collection of information such as weight, blood sugar levels and peak flows, access to knowledge bases, decision support tools and care management advice. These systems may also include facilities tailored to the specific needs of the consumer with certain clinical conditions; and 65 HealthConnect · Business Architecture v1.9 Shared-care tools which encourage consumers to actively contribute to their health records in conjunction with providers. A well-established shared-care tool is the personal health record used in the monitoring of child health developments from birth to five years. These systems will need to have the capacity to download information from the consumer’s HealthConnect record and the ability to create event summaries; The Need for Clinical Interpretation The information within a consumer’s HealthConnect record will primarily consist of clinical information which is often highly technical in content. This is inevitable, as the clinical information provided to HealthConnect is mainly generated by health providers communicating with other health providers involved in the consumer’s care. Consumer access to this information may require interpretation and possible representation in ways more meaningful to consumers. As with the clinical tools this is not core HealthConnect functionality. However the need of consumers to understand the technical content of their health records is an important issue which HealthConnect needs to include in its design. For example should a provider wish to include consumer friendly instructions in their event summary, HealthConnect must be able to accommodate this. The types of features to be addressed by consumer tools and services include: · Consumer-centric views of their health records, with a consumer look and feel, including the use of online help and navigation guides; · Consumer management instructions within individual provider event summaries that are written in plain English, to assist consumer compliance. This might include the incorporation or reference to context sensitive, consumerfriendly material supporting consumer self management and compliance with their healthcare regime; · Access to consumer-centric clinical guidelines and knowledge sources; · Clinical support services for consumers seeking clarification regarding the content of their HealthConnect record, or consumer requests for additional information. Such services could be operated by trained clinical staff capable of providing consumer advice based upon the clinical content of the consumer’s HealthConnect record. The extent to which these consumer-centric facilities will be made available depends upon how quickly commercial products and other initiatives such as health call centres are established to address the requirements, and the extent to which providers are able to incorporate consumer-centric elements within their event summaries. 66 HealthConnect Business Architecture v1.9 5.7 Consumer Scenarios Scenario 1. HealthConnect – Value Add for Accident Victims. The year is 2010 and John and Emily Craig, having retired last year, are three months into their planned twelve month motor home tour of Australia – having set out from Brisbane and explored NSW and Victoria – they are on the road heading for Adelaide. As part of their preparation for the trip they had been to see their GP for a thorough check up and on his advice had registered for HealthConnect, and had arranged for all their basic health information (past history, allergies, past illnesses and present diseases and treatment) to be uploaded into HealthConnect so that wherever they were in Australia this information could be retrieved if needed. Early one evening, just before the Craigs were to stop and rest for the evening, a large fuel tanker on its way from Adelaide to Melbourne jumped the median strip and sideswiped their oncoming motor home causing it to crash into a pole. In the accident, the tanker driver was uninjured but unfortunately John and Emily both sustained significant injuries. Using his mobile phone, the tanker driver informed rescue and ambulance authorities of the accident and did what he could for the Craigs until help arrived. Once the paramedics arrived at the accident scene they were able to access John’s HealthConnect record remotely (his card was in his wallet) and discover that because of his heart condition he needed to have the fluids given in transport carefully monitored. John was the most severely injured and it was decided that he would be flown to the Royal Adelaide Hospital (RAH). Besides a number of broken bones, John had suffered a significant head injury which left him quite confused. Fortunately his HealthConnect smartcard was passed on by the paramedics and using, the emergency override facilities within HealthConnect, the RAH emergency team were able to access his medical records swiftly and discover two key facts. Firstly, John had had severe allergic reactions to intravenous dye in the past and so would need to have special cover to prevent a recurrence during the urgent brain scan which he was about to undergo (where dye would routinely be used). Secondly, John was on a regular heart medication that needed to continue while he was treated for his head injury and other broken bones and that the fluids started by the paramedics needed to be carefully monitored during his further treatment. The record also showed that John had while travelling in remote NSW had a check up at a nursing post for his heart condition, and that he had run out of his heart medication. Emily on the other hand was not too badly injured – having just a couple of fractured ribs and a broken wrist. She was taken by road ambulance to a nearby district hospital where she was given pain relief, relevant precautionary X-rays were taken and her wrist was placed in plaster. The local hospital also contacted the Craig’s relatives and they arranged to all meet in Adelaide after the motor home was salvaged and accommodation close to the RAH was secured. Emily was able visit John the next day in the RAH’s Intensive Care unit and was greatly relieved to know that his brain scan had been completed quite safely – due mainly to the warning derived from the information obtained from HealthConnect – and that there was an excellent chance that both the head injury and the other injuries would heal successfully and that any deterioration in his heart condition would be avoided thanks again to HealthConnect. 67 HealthConnect Business Architecture v1.9 John was eventually discharged from the RAH some two weeks later to the attached rehabilitation unit – and it was really only then his local doctor in Brisbane discovered how valuable the information he had placed on HealthConnect had been, although he had been alerted of their admissions to the two different hospitals when they happened via a HealthConnect notification. The news came via the RAH Discharge Summary from HealthConnect - Dr Hall, not being on the RAH’s internal provider directory, would not normally have received this electronically. Dr Hall subsequently received a discharge summary from the rehabilitation unit. The discharge summaries highlighted the successful extra precautions taken to ensure John’s safety and what special care John needed once he returned home. The doctor had, of course, been aware of Emily’s progress much earlier as the smaller district hospital had transmitted a discharge summary with her treatment when she left the hospital the day after the accident. Once at home, John’s local physiotherapist was able to develop a targeted treatment plan assisted by looking at the imaging reports and the Adelaide allied health team reports on HealthConnect. The pleasing news is that four months later John and Emily are about to set out again to complete their trip – due in no small part to the help given by HealthConnect’s capabilities to move critical health information to where it is needed nationwide. Scenario 2. HealthConnect – Value Add for the Young Family. It is 2009 and HealthConnect has now registered over 70% of the adult population to have their health records managed and retrieved by HealthConnect - the Australian national electronic health record program. A few years ago in 2006, Amanda Duncan was an early registrant who decided to sign up to have her records and those of her children transmitted to HealthConnect – after she was thrilled to discover that she was pregnant with her daughter Emma who was born some seven months later. Amanda has been feeling a little ‘unusual’ for a couple of weeks and decides to arrange an appointment with her usual GP (Dr Ellen Grant) suspecting it just could be that she is pregnant a second time. On calling the surgery she is disappointed to find that Dr Grant is not available – being herself on maternity leave – and that her locum (Dr Phoebe Mills) is looking after the surgery. Amanda agrees to come and see Dr Mills who can as she works in the same practice access Amanda’s and Emma’s HealthConnect records so she can ‘get up to speed’ before they meet in a few days (when Dr Mills moves to work as a locum at a practice without authorisation, she will no longer have access to Amanda’s record). Had Amanda decided to go to a different practice she could have used her HealthConnect smartcard to provide access to her records for the doctor she was seeing if she so chose. On the day of the appointment, Dr Mills opened her Clinical Information System, requested Amanda’s and Emma’s HealthConnect records and downloaded them to her system. Here an advanced rule-based decision support system assessed information from each of the records. From this assessment it was identified that Amanda needed the routine early pregnancy checks should she indeed to turn out be pregnant and Emma was a couple of months overdue for her year three vaccinations. Dr Mills noted these 68 HealthConnect Business Architecture v1.9 findings and found stocks of the required vaccines were low and arranged for a delivery so she could be sure they were ready when her patients arrived. The only concern that was raised in the review of the records was a report relating to the previous pregnancy that Amanda had suffered from high blood pressure and it was important to ensure this had been fully resolved. Amanda’s blood pressure would need to be carefully tracked during this pregnancy. Later that day Amanda and Emma arrived for their appointment. Forewarned, Dr Mills had all the necessary vaccines ready for Emma (who was less than impressed at the prospect of a needle) and had the pathology forms ready so Amanda could be quickly checked for any unexpected complications in the event she was indeed pregnant. The rapid pregnancy test confirmed the good news that Amanda’s instinct was proved correct – blood was collected for the routine tests and after some general congratulations all around Amanda said she was keen to use the same obstetrician (whom she had previously authorised to access her HealthConnect record). An appropriately timed appointment and referral was made electronically – from Dr Mills computer to the appointment system of Dr Adrian (the obstetrician) making additional use of the HealthConnect communications network. Printed confirmation of the appointment was given to Amanda as she left, as well as another appointment with Dr Mills for one week’s time to review the test results and to ensure Amanda was happy will all the arrangements and had no pressing questions etc. For the next seven months Dr Mills and later Dr Grant (Amanda’s usual GP) received notifications and progress reports on her visits to the Obstetrician – along with some pictures of the ultrasound which was done at 18 weeks to confirm the status of the pregnancy and rule out major congenital deformities. Through HealthConnect these were available the day after they were done. This meant that when Amanda developed a nasty episode of the flu about 28 weeks into the pregnancy Dr Grant was on leave, but the temporary locum was able to catch up with the progress of the pregnancy and could give optimum care to both Mum and the expected baby. Amanda delivered a few weeks earlier than expected and needed minor operative intervention to ensure a healthy baby was delivered. On the day of the birth Dr Grant received a progress report via HealthConnect and later, on the day of discharge, a discharge summary from the Maternity Hospital. These enabled her to check and be confident that, if Amanda had any complications, she could offer informed assistance. As it turned out, Amanda and Troy (the new baby boy) had no problems but Amanda was greatly reassured that all those involved in her care knew exactly what the other was doing and could work in a co-ordinated effective way to ensure a healthy mother and baby - due at least in part to the capabilities of HealthConnect. Scenario 3. HealthConnect – Value Add for those with Chronic Disease. It is 2008 and HealthConnect has now become an important and accepted part of Jim Boyle’s life. Jim is now just over 60 and had been forced by worsening health to ease up on his previously very active life as a building tradesman and to devote a little more time to looking after himself, and planning for a healthier retirement. Jim’s health problems began in late 2004 when the combination of poor dietary habits, maybe a few too many beers after work and a move to more office work led to less 69 HealthConnect Business Architecture v1.9 exercise, weight gain, and eventually to a feeling of progressive tiredness and increasing difficulty getting around due to a gradually worsening pain in his right hip. It was thus, early in 2005, that Jim finally decided, with much prompting from his wife to visit his local GP for the first time in living memory! At the end of the first visit the GP (Dr Andrew Hall) had formed tentative diagnoses of Type II diabetes and slowly progressive osteoarthritis of the right and probably left hip. Fortunately for Jim, Dr Hall had recently signed up to HealthConnect as a provider and just before Jim left to have a range of tests, Dr Hall had explained to him that his care over the next few months and years could be streamlined should he decide to register as a consumer on the HealthConnect system and use the system to keep track of progress getting his diabetes under control and his weight down – to help lengthen his life and much improve the pain in his hip – deferring perhaps for years the need for more serious intervention such as surgery. Dr Hall explained to Jim that once he agreed to join HealthConnect it would be possible for Dr Hall to use HealthConnect to closely monitor the progress of Jim’s diabetes and reduce the number of times he actually had to go and see the doctor (something Jim hates). Dr Hall explained that he could use HealthConnect to keep an eye on how things were progressing and additionally could schedule routine visits around important scheduled checks of vision and foot health (which may deteriorate with diabetes). On Dr Hall’s advice Jim registered and consented to be a participating HealthConnect consumer at his local Medicare office. The next visit to Dr Hall a week later confirmed the diabetes as well as osteoarthritis of both hips (milder in the left) and, Dr Hall explained what Jim would now need to do in order to track and manage his condition. Being a moderately skilled person with good understanding of his situation Jim was given the option of piloting using HealthConnect or attending the surgery several times a week to track his condition. Jim took home the documentation from HealthConnect which explained how he and Dr Hall could use the HealthConnect system to enter and then keep track of his blood sugars, his home measured blood pressure and his weight between visits to the doctor. (This capacity to make use of information recorded by a patient is still being piloted and evolved by HealthConnect and presently needs Jim and Dr Hall to sign specific consents, but such facilities are in increasingly wide use overseas). Dr Hall also started Jim on an oral hypoglycaemic tablet (anti diabetic tablet) and pointed out to Jim that with weight reduction and careful dietary control, it was possible that, over time, his need for the tablet may be reduced or even cease. Each fortnight Dr Hall was able to access the records Jim created and ensure all was going to plan. When problems arose, and this was quite common in the early months, Dr Hall was able to contact Jim by phone or e-mail and, when Dr Hall’s clinical information system identified any additional tests or routine follow-up that was required. This was arranged at the same time. In this way both Jim and Dr Hall were able to ensure Jim’s health was improving and any required adjustments to Jim’s treatment could be simply arranged. Indeed, with Jim’s weight having dropped by 15 kilos and his HbA1C being within the normal range after six months, (demonstrating the overall effectiveness of his blood sugar control), Dr Hall was able to reduce the tablet dosage and reduce the frequency with which Jim needed to check his blood sugar – good news all around – less pain for Jim (in both his hips and fingers not having to sample his blood so often), less cost for medication and use of state-of-the art evidence-backed care all co-ordinated by HealthConnect and allowing both Jim and Dr Hall to do a better job 70 HealthConnect Business Architecture v1.9 more easily. In particular, through the use of HealthConnect, Jim was able to minimise the impact of his treatment on his employment and family life. Now in 2008, HealthConnect has been helping Jim live a longer and happier life for over three years while reducing the risk of complications of his diabetes and maybe even avoiding the need for hip surgery. No wonder Jim is a convert – convinced he now has control of his health, in co-operation with his doctor, back again! 71 HealthConnect 6. Business Architecture v1.9 Healthcare Provider/Organisation Participation The provision of timely, accurate and clinically useful information to healthcare providers at the point-of-care is one of the key objectives of HealthConnect. The availability of HealthConnect information will assist providers in delivering safe and effective healthcare, and the provision of HealthConnect event summaries by providers will facilitate on-going care provision. The ability of HealthConnect to integrate seamlessly within healthcare providers work practices will be critical in ensuring the success of HealthConnect. This section outlines what being involved in HealthConnect will mean to providers and provider organisations including: · Benefits to providers and provider organisations; · The process of provider identification and registration; · Provider privacy and consent responsibilities; · The interaction providers will have with HealthConnect; and · Use of value added eHealth systems which will interface with HealthConnect. 6.1 Benefits of HealthConnect to Provider/ Organisations Analysis of provider benefits have been conducted throughout the HealthConnect research and development activities, drawing on the experiences of the HealthConnect trials. In addition, a full analysis of the potential HealthConnect benefits is presented in the Benefits Realisation Framework13. The expected benefits of HealthConnect for participating providers include: · · 13 Support for Medication Management, including: - More informed medication management; - Fewer prescriptions written and dispensed; - Increased efficiency in dispensing prescriptions; and - Fewer dispensing errors. Assisting Decision Making and Care Coordination, including: - Better informed clinical decision-making; - Enhanced management of complex and chronic disease; - Improved knowledge about the existence of patient co-morbidities; - Reduced incidence of unnecessary services; - Improved coordination of patient care; and HealthConnect Benefits Realisation Framework V1.0 October 2004 72 HealthConnect · · Business Architecture v1.9 Increased efficiency and effectiveness of transfer of patients between care settings. Enhancing Service Delivery Efficiency, including: - Increased efficiency of outpatient services; - Increased efficiency of peri-operative processes; and - Decreased length of stay. Improved Information Management, including: - Increased efficiency of referrals from general practitioners to specialists; - Increased efficiency of information exchange between care providers; - Reduced time spent chasing paper-based records or dispersed electronic records; - Reduced duplication of effort in updating records; and - Improved accuracy of information. 6.2 Provider Participation Boundaries 6.2.1 Scope of Provider Participation The HealthConnect Principles relating to providers include: · Provider participation in HealthConnect will be voluntary and will remain active until the provider gives HealthConnect a request to deregister or the provider is no longer eligible to participate in HealthConnect (as determined by the rules governing the operation of HealthConnect.) · HealthConnect will support a whole-of-health perspective encompassing private and public providers and continuity of care across primary, secondary and tertiary care settings including preventive health. · Provider participation in HealthConnect will be encouraged and will be made available to all providers involved in the chain of health care delivery. While the initial focus is likely to include medical practices, pharmacies, hospitals, diagnostic services, health and aged care facilities and those practitioners currently participating in HealthConnect initiatives, this scope will be extended through arrangements with representatives of each provider group. Considerable efforts will be made in the implementation of HealthConnect to streamline the access process and keep to a minimum the impact on provider work practices and focus on delivering value to the provider. It is assumed that this approach, together with appropriate marketing and education, will result over time in a high participation rate. 6.2.2 Provider Organisations and Individual Providers Provider participation in HealthConnect occurs at the level of both individual provider and provider organisation. Provider organisations must be registered with HealthConnect and work is progressing on the requirements for individual provider participation. Hence: 73 HealthConnect Business Architecture v1.9 · A person practising as a health provider who is recognised for professional registration in an Australian jurisdiction will be eligible to register with HealthConnect as an individual provider. This will require their professional registration body to have been previously recognised and registered with HealthConnect. · A registered business (including a sole trader) that delivers health services using the services of one or more individual providers will be eligible to register with HealthConnect as a “provider organisation”. Individual providers will include general practitioners, specialist medical practitioners, diagnostic specialists including pathologists and radiologists, nurse practitioners and community nurses, pharmacists etc. Organisational providers potentially include any of the following: medical centres; general and specialist hospitals; community health centres, Aboriginal medical services, residential aged care facilities and nursing homes etc. Any individual provider operating as a sole trader or as a business enterprise will also be registered separately with HealthConnect as a provider organisation. Consumers consenting to providers accessing their HealthConnect records do so at the level of the provider organisation (for example, a hospital or a general practice). Thereafter, all personnel authorised by the nominated provider organisation will be able to access the consumer’s HealthConnect record. There is a requirement for HealthConnect to provide consumers with access to an audit trail detailing who has accessed which parts of their HealthConnect health information, necessitating both individual providers and provider organisations to be uniquely identifiable. The audit trail report will display the name of the organisation, the user who has accessed the information and the various parts of the participant’s health records that were accessed. The delivery of reports at this level of detail requires all personnel accessing the consumer’s record and the health care organisation from which access occurred to be uniquely identified. All information submitted for inclusion in a HealthConnect EHR will be attributable to an individual provider as well as to the provider organisation from which it originates. To submit entries for inclusion in the EHR, individual providers must already have been uniquely identified within the organisation so that they can be identified to HealthConnect. It is recognised that there are a group of clinical support staff who are not clinicians but will require access to HealthConnect as part of their current work practices. These clinical support staff include surgery receptionists, admissions and ward clerks, and junior clinical personnel. This group of users will not be individually registered on HealthConnect but will need to be identified to HealthConnect by the organisations to fulfil monitoring and audit requirements in a manner acceptable to consumers. Procedures to support this requirement are currently being developed. 74 HealthConnect 6.2.3 Business Architecture v1.9 Provider Identification Provider registration and identification requirements are defined together with consumer requirements in the Registration and Identification Business Requirements document14. · Each provider (individual or organisation) will be uniquely identified within HealthConnect by use of a single unique identifier linked, in the future, to the National Provider Directory. The National eHealth Transition Authority (NEHTA) has, as one of its strategic priorities, the development of a national solution for unambiguous identification of providers, known as the national provider directory (previously ProviderConnect). HealthConnect will, in due course, make use of the national provider directory in identifying and referencing HealthConnect providers. To provide interoperability, give longevity to the information being recorded in HealthConnect and to ensure that the entities are correctly identified, the identifier allocated to a provider or provider organisation will be compliant with all relevant national and international standards for health provider identification (for example, AS4846 - 2004 Australian Standard for Health Care Provider Identification). 6.2.4 Provider Registration A provider’s participation in HealthConnect will be subject to the provider having entered into a legal agreement with the HealthConnect governing body which will set out the obligations of the provider and provide the basis both for the provider’s use of HealthConnect and the protection of consumer privacy. Registration of provider organisations A health provider organisation employing individual health providers will be able to enrol in HealthConnect. The provider organisation must be a legal entity able to enter into an agreement with HealthConnect. Public and private hospitals, outpatient clinics, general practices, community health centres, pharmacies, aged care facilities and other non-government health agencies are examples of health provider organisations. Healthcare organisations wishing to participate in HealthConnect would need to: · enrol in HealthConnect; · acknowledge and support consumer preferences for participation in HealthConnect; · follow HealthConnect guidelines and procedures for the use of HealthConnect; · manage staff participation in HealthConnect; and · secure and authorise use of HealthConnect information within the organisation. The organisation’s representative or agent will be required to complete and submit to HealthConnect an assessment of the organisation’s eligibility as part of the enrolment 14 Registration and Identification Business Requirements V1.01 Aug 04 75 HealthConnect Business Architecture v1.9 process. The organisation must meet HealthConnect requirements on privacy and security in order to participate. Registration of individual providers Processes for individual provider enrolment with HealthConnect will be developed to complement existing and future professional registration processes and will be designed to have a minimal impact on the individual provider’s existing business processes. Providers wishing to participate in HealthConnect would need to: · enrol in HealthConnect including signing a HealthConnect agreement; · acknowledge and support consumer preferences for participation in HealthConnect; and · follow HealthConnect guidelines and procedures for the use of HealthConnect. 6.2.5 Authorisation of Providers Providers will only be able to access, view and contribute to the records of consumers for whom the provider organisation has been authorised. Provider organisation nomination will mainly be established by consumers in advance of a consultation, although the consumer may nominate provider organisation access at the time of the consultation. HealthConnect will also support access using emergency override. The HealthConnect Principles state that: · HealthConnect will allow any registered individual provider acting on behalf of a provider organisation that has authority to access the consumer’s EHR for the purpose of providing health services to the consumer. · A provider’s organisation must have the consumer’s consent prior to an individual provider accessing a consumer’s HealthConnect EHR. This consent would typically be set up at registration or the first time the consumer presents at the provider organisation’s premises. · Providers once authorised will be able to access all parts of the consumer’s HealthConnect EHR. HealthConnect will not determine which parts of the EHR are relevant to any individual health encounter. · All access to a consumer EHR will be logged and able to be tracked back to an individual provider or consumer. 6.2.6 Provider Authentication Stringent security and authorisation mechanisms will be put in place to ensure that only authorised providers can access consumer records. Different levels of authentication will apply depending on the access scenario: Where a provider wishes to access a consumer’s information using an endorsed healthcare IT system operating within a facility that is managed by a registered healthcare organisation, the provider’s identity shall be authenticated by the normal 76 HealthConnect Business Architecture v1.9 means used by that healthcare system. The individual provider’s HealthConnect identification will then be included in each access request. Where a provider wishes to access a consumer’s record using another device such (eg a PC, laptop or PDA) the provider’s identity shall be authenticated by at minimum of two factor authentication, for example a user defined PIN or equivalent and a token containing a personal digital certificate. 6.2.7 Provider Responsibilities Individual providers and provider organisations will be required to sign HealthConnect agreements outlining their responsibilities at time of registration. As participants of HealthConnect, provider responsibilities include: · Commitment to providing accurate information to HealthConnect. Providers will be able to review the event summary prior to it being submitted to HealthConnect; · Recognition of consumers rights as participants in HealthConnect (eg not sending an event summary to HealthConnect if requested not to do so). This includes a duty to assist consumers understand the implications of withholding information from their HealthConnect record or restricting access to their HealthConnect record, which may impact the ability of providers to deliver safe and effective healthcare; · Participation in line with the HealthConnect confidentiality and privacy arrangements. Providers must abide by privacy legislation and by specific HealthConnect privacy protocols; · Local procedures which comply with appropriate national standards, to meet HealthConnect privacy and security requirements. These will include processes to control access to, and audit the use of, the organisation’s information systems. Provider organisations will be responsible for controlling its personnel’s use of HealthConnect information and for ensuring that the individual provider (or any other person) accessing the consumer’s EHR on behalf of the provider organisation is identified to HealthConnect; · Using clinical information systems to access HealthConnect that comply with the technical requirements of HealthConnect; and · Maintaining security of any EHR information integrated into their clinical information systems. Once HealthConnect EHR information has been entered into a local system, the owner of that system has responsibility for the security of the information. 6.2.8 Privacy and Confidentiality The success of HealthConnect will depend on consumers, providers and provider organisations having confidence and trust that health information is kept confidential and secure. To this end, a robust privacy framework, together with strong security measures, is to be established as proposed in the HealthConnect Principles: 77 HealthConnect · Business Architecture v1.9 HealthConnect participants will be obligated to abide by privacy legislation and by specific HealthConnect privacy rules. The National Health Privacy Code will be used when it has been implemented, until then privacy arrangements will be tailored to suit each jurisdiction for each implementation, with a view to working towards a single national set of rules. Provider organisations and individual providers participating in HealthConnect will be obligated to abide by existing privacy legislation and by specific privacy protocols developed for HealthConnect – including when providers seek health information from HealthConnect, or when they add information to any HealthConnect record. The privacy framework will ensure that both consumer and provider privacy interests are managed. 6.3 Provider Interaction with HealthConnect The key HealthConnect Principles relating to provider interaction are: · HealthConnect will not replace providers’ own clinical records or clinical information systems. Providers will continue to maintain their own consumer health records but may choose to incorporate selected HealthConnect EHR information in their records or clinical information systems. · Providers will interact with HealthConnect primarily through their clinical information systems. A standard web-browser interface to HealthConnect will also be available for providers whose systems cannot initially link to HealthConnect. · HealthConnect will aim for access to HealthConnect to be integrated into the providers’ clinical information systems and as far as practicable streamline access and keep to a minimum impact on provider work practices. 6.3.1 Provider eHealth Access Services A central role in HealthConnect is that of provider eHealth access services (eHAS) whose primary function is to give providers effective means of accessing HealthConnect services and any front line support needed to help them in using HealthConnect. This role was highlighted in the HealthConnect Roles/Services diagram presented above in Section 4 - The HealthConnect solution. Functions identified as being potentially associated with delivery of provider eHealth access services include: (a) providing HealthConnect access portal and connection to the core HealthConnect message handling and transport system (for providers accessing HealthConnect via both clinical information systems and web browsers); (b) providing advice, assistance and training to HealthConnect providers using or starting to use HealthConnect; 78 HealthConnect Business Architecture v1.9 (c) providing eHealth support service to resolve HealthConnect access and usage problems; (d) providing access to eHealth message bank service and facilities that support secure transmission of eHealth messages (including prescriptions, referrals and notifications) between providers; (e) providing access to added-value services, potentially including supply of health information and clinical decision support services, HealthConnectcompliant clinical information systems, and associated consulting and advisory services; and (f) assisting to market HealthConnect to providers and facilitate provider registration. The functions of the Provider’s Clinical Information System, the Provider Access Portal, the Value Added eHealth Services and the eHealth Message Bank Service are discussed in the sections below. 6.3.2 Provider Clinical Information System Interfaces The longer term goal is that providers will, for the main part, access HealthConnect through their own clinical information systems, which will inter-operate with the HealthConnect message handling and transport system through nationally defined HealthConnect interfaces. The provider systems will generate and supply event summaries to HealthConnect. Providers will send provider-initiated requests for consumer health information views to HealthConnect and utilise the resultant information retrieved from HealthConnect. The HealthConnect information will be presented succinctly to providers via specially tailored EHR views/lists that bring together key aspects of a consumer’s health information, such as medications, allergies and alerts, problems and diagnoses. These provider clinical information systems will provide all aspects of the provider’s “user interface” to HealthConnect so that providers will not need to use HealthConnect directly. The HealthConnect interface to a provider’s clinical information system (CIS) will include the following functionality: 1. Provision of information to create views of consumer HealthConnect records such that the provider’s CIS can create the view. This will be subject to the provider’s organisation having been authorised as part of the consumer consent process. Views include: - Composite EHR views and lists that bring together key aspects of the consumer’s health information for ease of viewing. This might contain summary health status information such as current medications, diagnoses and alerts and recent investigation results; and - Individual event summaries, such as hospital discharge summaries, emergency department presentations, provider consultations and diagnostic results. 79 HealthConnect Business Architecture v1.9 The provider may elect merely to view the information or to incorporate the information into their local system. Within this functionality there will be support for specific information downloads, for example a pharmacist using the barcode on a printed script to download the prescription details to assist the dispensing process. 2. Receipt of the event summary containing predefined key aspects of the consumer consultation to HealthConnect, again subject to authorisation via consumer consent. This will be automatically generated and sent by the providers system, though the provider may elect not to send or all part of it, on request from the consumer. 3. Provision of Notifications regarding key consumer healthcare events including hospital admissions and discharges and emergency department presentations. 4. Provision of consumer demographic and summary health information – where a consumer presents for the first time and provides access using their HealthConnect identifier, HealthConnect will provide consumer demographic and summary health information which can be integrated into the provider’s local system. 5. Receipt of initial health profile information – provider systems may upon request create and send a message containing parts of the consumer’s initial health profile. 6.3.3 HealthConnect Provider Access Portal Where there are no clinical information systems in place, the Provider Access Portal will provide web based access to HealthConnect to providers to facilitate viewing records and creating event summaries. These facilities will be limited to core HealthConnect functions only (that is, there will be no “value-added” provider services such as medication management and clinical decision support). This web based access is considered an interim measure and not part of the core HealthConnect, and as such it will be phased out over time. The HealthConnect Provider Access Portal web-based access will include the following functionality: 6. 7. Viewing and printing of consumer HealthConnect records, subject to the provider’s organisation having been authorised as part of the consumer consent process, including: - Composite views and lists that bring together key aspects of the consumer’s health information for ease of viewing. This might contain summary health status information such as current medications, diagnoses and alerts and recent investigation results; and - Individual event summaries, such as hospital discharge summaries, emergency department presentations, provider consultations and diagnostic results. Creation and transmission of an event summary, according to a predefined event summary format appropriate to the provider type. 80 HealthConnect Business Architecture v1.9 8. Receipt of Notifications regarding key consumer healthcare events including hospital admissions and discharges and emergency department presentations. 9. Maintenance of provider preferences – it is anticipated that there will be the facility for providers to record and change preferences such as types of views they prefer to access, types of notifications they want to receive. 10. Provider logon access i.e. maintenance of security PIN or equivalent details. For some providers it may be that a combination of the two solutions (i.e. messaging access through their clinical information system and direct access using the access portal) would be required. For example, the provider’s system may be able to create and send event summaries but not initially have the capability to receive the EHR information and create the required views. 6.3.4 Value Added eHealth Services HealthConnect will make available health record information which will support clinical decision making. It will not itself perform clinical decision support; rather it will support providers’ local systems in performing these functions which include: · Medication management (including support for prescribing, medication interaction checking and dispensing); · Evidence based information; and · Sophisticated event notifications based on analysis of the clinical information within the event summaries. To support these value added services HealthConnect must be able to provide the information in an appropriate computable and interpretable form. The HealthConnect Principles state that: · 6.3.5 Implementations of value added services are outside core HealthConnect functionality. While individual implementations of HealthConnect may include optional value add functionality to address local requirements, these are related systems and must be implemented such that they do not affect the compatibility of the HealthConnect implementation with the national standards. eHealth Message Bank Service Though the eHealth Message Bank Service support for operational communications activities such as electronic referrals, investigation requests and investigation results is not part of the core functions of HealthConnect, it is expected to be established as a related service. The role of the eHealth message bank service is to provide a facility for handling eHealth messages between participating providers and relating to any health consumer (not just those who consent to participate in HealthConnect). 81 HealthConnect Business Architecture v1.9 Providers wishing to use this service will need to register with HealthConnect in order to formalise agreements and establish a provider identifier. This does not necessarily imply active use of the HealthConnect EHR. In the absence of a national identifier for consumers, use of the eHealth message bank service in stage 1 will be limited to HealthConnect consumer participants. Once a mechanism has been established for unique identification of non HealthConnect consumers, the service can be expanded. The HealthConnect Principles state that: · Implementations of HealthConnect are likely to build on the messaging service it requires and conduct, as an adjunt to the core service, an implementation of a wider eHealth message bank service to support other health communications. 6.4 Key Work Practice Implications For the main part, provider interaction with HealthConnect will comprise the creation of event summaries for each healthcare event for HealthConnect consumers and the retrieval of HealthConnect consumers’ EHR information via views. In addition to these core functions there are a number of specific functions which will impact provider work practices such as authorising diagnostic test results; maintaining current medications lists; receiving notifications and creating initial health profiles. These core and specific functions are discussed below. 6.4.1 Creating Event Summaries A critical aspect of the creation of event summaries is the quality and completeness of the information being entered into the provider’s clinical information system as part of their normal work practices. A key aspect of HealthConnect implementations will need to be focussed on change management activities to improve the quality of the data available in the local clinical information systems. Once the data has been entered into the provider’s system, the creation of event summaries should fit in with provider work practices. For example: · The hospital event summary will be created in parallel with the standard hospital discharge referral and sent to HealthConnect once authorised by the discharging clinician; · A general practitioner consultation event summary will be created by the doctor’s clinical information system based on information entered during the consultation. The doctor will have the opportunity to review and edit the event summary prior to its submission; and · A diagnostic test result event summary, or possibly a link to the result information, will be a by product of the standard electronic result message. In all cases providers will have the ability to, on request, not send the event summary or delete selected information prior to sending the event summary. To be considered HealthConnect compliant the providers’ clinical information systems will need to provide this facility. 82 HealthConnect Business Architecture v1.9 Where the provider uses the HealthConnect web based tool for event summary creation (a short to medium term solution) there will be a greater manual effort to set up the event summary. Vendors of provider systems will be encouraged to support the collection and checking of data required in the event summary. Similarly providers will be encouraged to enter this information as part of their normal work practices and increase the focus at the time of data entry on the quality and completeness of the information being collected. In this way the creation of an event summary will become a seamless by product of standard work practices. 6.4.2 Retrieving EHR information The first step in a provider retrieving information from HealthConnect is for the provider to access and open the relevant consumer’s EHR. The presentation of information received and the navigation pathways provided will depend on the provider’s own CIS functions (or on the Access Portal Application) rather than on HealthConnect itself. The starting point for most providers is expected to be the “primary/critical view” which provides information such as identification of the consumer; alerts, allergy and adverse reaction list; existing diagnosis/problems list; and latest medications. It will also contain secure links to further information such as relevant medication list; laboratory test results list; recent health events; and procedure/treatment history. Technology for reducing the impact of EHR systems operation on users is still in the early stages of development and refinement of these concepts is expected to be a major focus of the implementation architecture and of development work for stage 1 implementations. A potential mode of operation might be that when the CIS opens up with the consumer’s local record, it automatically establishes a communication session with HealthConnect and brings up the critical view in the background ready, should the provider so wish, to be viewed. Technologies such as the HL7 Clinical Context Object Workgroup (CCoW) initiative could be used to identify the consumer and provider to HealthConnect so that consent checking and creation of the view can be achieved without intervention from the provider. It is also anticipated that the provider’s CIS will put mechanisms in place to ensure that the provider does not spend time reviewing information already reviewed as part of a previous consultation. The CIS might, for example, highlight information which has changed since the provider last accessed the consumer’s EHR, and the provider may choose just to review that information. 6.4.3 Authorising Diagnostic Test Results There has been considerable debate about whether diagnostic test results should be submitted directly to HealthConnect or to the requesting provider for review and subsequent incorporation into an event summary. Diagnostic test results are critical parts of the EHR especially in an emergency and there is concern about any potential delays in their being available on the consumer’s record. 83 HealthConnect Business Architecture v1.9 The proposed solution is that: · All diagnostic test results for participating consumers will be sent to HealthConnect at the same time as being issued to the requesting provider, with the exception of diagnostic tests for hospital inpatients. · For inpatients it is considered that the test results will already be available to those involved with caring for the consumer during the hospital stay. Only at discharge will those tests deemed appropriate by the discharging clinician be sent to HealthConnect as part of the discharge summary referral. · Test results sent to HealthConnect directly will not be available for viewing until the requesting provider has reviewed the result and confirmed its release to HealthConnect (to allow providers the opportunity of discussing with consumers prior to general availability). Message functions will be established for this purpose. In the future a parameter may be established which sets a time period after which the results will become available whether or not the provider has released them. The latter is not the current model. · Emergency access to the record will include access to all results available in HealthConnect at the time, including non released tests. This emergency access includes emergency presentations where the consumer is able to give consent as well as the emergency override facility. 6.4.4 Maintaining EHR Lists An EHR list is a collection of similar EHR items describing a key aspect of a consumer’s health, formed to serve a specific purpose. Two types of lists have been identified - derived and maintained. A derived list is a list that can be automatically generated as an EHR view across all relevant health event summaries and requires no user intervention. Examples of derived EHR lists are prescribing/dispensing history, procedure/treatment history, and recent health services. A maintained list is a list which requires clinical judgement to determine if and when an entry should be removed from the list. This implies, in most cases, a need for some review process. Examples of maintained lists are current medications, active problems/diagnoses, adverse reactions and warnings. The current medication list is one of the most important aspects of HealthConnect. It is therefore important that mechanisms are set in place to ensure that this is accurate and up to date. Details of prescribed, dispensed and over the counter medications will be sent to HealthConnect as part of a wide variety of event summaries. HealthConnect will upon receipt of medication information add the details to relevant derived lists such as prescribed medications list, dispensed medication list and the maintained list for current medications. Through this process the current medication list will contain all newly prescribed and dispensed medications. The issue arises of how best to delete entries from the list either due to the medications no longer being current or there being duplicates on the list. 84 HealthConnect Business Architecture v1.9 The Tasmania HealthConnect trial takes the current medications list from the most recent general practitioner consultation event summary. Recent phases of the trial allow other clinicians to add to the current medications list. For ongoing maintenance, the current medication list contained in the general practitioner’s clinical information system is incorporated into the consultation event summary. Upon receipt HealthConnect uses this version to replace older versions. The Brisbane Southside HealthConnect trial operates in a similar manner except that the consumer’s nominated general practitioner maintains the current medication list. These solutions are not viable for the wider implementation of HealthConnect. For version 1 of HealthConnect it is proposed that HealthConnect provides the functionality for any clinician (such as general practitioners, specialists, hospital, community nurse practitioners) to review and amend a view of the current medication list as part of a health event. The resulting event summary will be structured to include information to confirm, delete, and/or add medications to the list. Amending rather than replacing the list will ensure that the integrity of the list is maintained, and that any linkages to event summaries relating to entries which are still current are retained. It is recognised that this review activity will need to be conducted consistently and involves changes to work practices, but that the additional effort is worthwhile due to the importance of these lists in the consumer’s healthcare activities. A possible approach might be to integrate the review of these lists into assessment consultations which are longer than standard consultations and where such matters are commonly addressed. It is also recognised that the introduction of a standard medication coding scheme will be required for this information to effectively support local clinical decision making. 6.4.5 Receiving Notifications HealthConnect will support simple notifications relating to time, events and data codes, for example, admission notice, discharge notice, overdue notice. Notifications based upon interpreting the clinical content of an EHR will not be supported. Determining which providers will be sent a notification about a consumer will be managed through the consumer access control parameters, set up as part of the consent process, which nominate specific provider organisations. It is anticipated that only a subset of the providers on the consumer’s access control list will be sent notifications. This will vary depending on the type of notification and consumer preferences, for example only the consumer’s nominated general practitioner might be sent a notification of hospital presentation and discharge. HealthConnect will send all notifications on encountering the appropriate trigger without reference to any other notification that might have been sent. Any filtering to avoid double counting would need to be managed by the recipient (eg. a provider or registry). 6.4.6 Creating the Initial Health Profile The process of the collection of initial health profile information is initiated at the time a consumer registers with HealthConnect. This is an important part of establishing the 85 HealthConnect Business Architecture v1.9 record, particularly for consumers with chronic and complex conditions and where consumers have important allergies or alerts. Subsequent to a consumer registering with HealthConnect, a provider may receive a request from HealthConnect to supply part of the initial health profile for a consumer they are treating. This might include summary information such as current diagnoses, allergies and medications. It is important to note that: · establishing an initial health profile is a one off activity conducted around the time of registration; · establishing a consumer’s initial health profile will not always require involvement from a provider; · where provider involvement is required, only one provider on the consumer’s access control list will receive a request to supply a particular type of information. HealthConnect will not include the ability to rationalise the data and resolve duplications and inconsistencies. Multiple sources might be used for different types of data; and · the initial health profile will be extracted from the provider’s CIS, presented for review and update and sent to HealthConnect as a specific type of event summary. Clinical validation of the data contained in the profile is particularly important to ensure that the consumer’s EHR is meaningful and useful. If the provider is regularly maintaining the type of information required in their CIS this process will be straightforward. In summary, the creation of the initial health profile is performed only once, for a subset of HealthConnect consumers; and for a subset of the consumers the provider is treating; and will be as automated as possible though clinical validation is required. 6.4.7 First Presentation at Healthcare Setting When a consumer attends a provider’s premises for the first time, they may be able to establish their record with the provider practice using their HealthConnect identifier. This would include: · the consumer’s HealthConnect identifier and PIN being entered. If the consumer has forgotten their HealthConnect identifier, a phone call to the consumer’s registration agency will be required. Processes for identifying the consumer including use of secret questions will be established; · having established the consumer’s identity, messages can be sent to HealthConnect to add the provider organisation to the consumer’s access control list. This is a one off activity and the access authorisation will remain valid until the consumer changes it; and · at this stage HealthConnect may send a predefined view of the consumer’s EHR containing consumer demographics and a health summary. This can, should the provider CIS have the capability, be incorporated into the provider’s local record. 86 HealthConnect Business Architecture v1.9 Hence HealthConnect can bring a direct benefit to providers when establishing records for new consumers. 6.4.8 Managing Emergency Access In the case of an emergency presentation where the consumer is unable to give consent for the provider access, the emergency override feature can be used. If the consumer has already included the provider organisation on their access control list, the emergency override is not required and standard provider access will be possible. This will be the case where the consumer has attended an emergency department previously and set up access. If the consumer is able to give consent to the provider, the smartcard and PIN can be used to set up the access. Once again this is not an emergency override situation, albeit that the provision of the healthcare services are considered an emergency. Only in those few cases where the consumer, or their agent, is not able to give consent and consent has not previously been given will the provider need to use the emergency override facility. If the HealthConnect consumer identifier is known (eg the consumer’s card is with them), the provider can enter the HealthConnect identifier and activate the emergency override to gain access. This type of access will be closely monitored. As with other non emergency access requirements, where the HealthConnect identifier is not known, processes will be put in place to ensure that the consumer may be correctly identified and the HealthConnect identifier and a temporary pass code given. The processes will include the ability for a provider organisation to phone a consumer registration agency or the HealthConnect registration service. 6.5 Provider Scenarios Scenario 1 – HealthConnect – Value Add for the GP In the five years since 2005 when the initial components of the HealthConnect project began to be implemented in his area, Dr Andrew Fergus has seen very substantial change in his work practices, greater use of computers to support his practice of medicine and increasing confidence in the quality of care he is providing. Prior to HealthConnect, Dr Fergus was like the vast majority of GP’s in the sense that he had a computer at the surgery front desk which handled patient registration, appointments and billing and, while he also had a computer screen in the consulting room, this was essentially used to print prescriptions and maintain medication histories on the patients under his care. In 2004 it was Dr Fergus’s view that further use of computers would slow his practice down, thus reducing his income potential while not making a positive difference to patient care. However, with the advent of HealthConnect, the value provided by his computer systems began to change and the effort involved in recoding patient details and encounters electronically became more worthwhile. One of the first benefits Dr Fergus began to greatly value was the access to event summaries providing a record of his patient’s encounters with specialists. Quick and 87 HealthConnect Business Architecture v1.9 easy online access to this information has made Dr Fergus’s role as the key co-ordinator of his patients’ care a great deal easier and more comprehensive. In parallel with this Dr Fergus has begun using information from HealthConnect and his own records to create patient summaries for current medications, current diagnoses allergies etc, especially for his more complex patients. He has found being able to send these summaries with his referrals to specialists has saved time in referring and usually improves the quality of the information coming back to him when the patient is seen. The benefits of having the medication summary maintained in HealthConnect have also risen as this summary can also be simply added to referral notes and of course downloaded to his local prescribing system ensuring accurate prescribing as well as effective local checking of drug interactions and so on. In addition, the medication summary can be used by the patient’s pharmacist to advise the patient on appropriate use of medication and the pharmacist can also see the reasons for a patient’s treatment in context from the patient summary resulting in fewer but more relevant, communications between the pharmacist and doctor over medication and better outcomes for the patient. With all this support Dr Fergus is much more confident he is less likely to make errors and he has no worries that the pharmacist can’t read his writing on the printed script! Enriched with information from HealthConnect, as well as being able to link to x-ray images from the radiologists report, Dr Fergus is finding his local clinical information system increasingly valuable as a tool in assisting his quality practice. The combination of information from HealthConnect – specialist reports, pathology results, discharge summaries, home nursing encounter reports and so on, when combined with the powerful local decision support capabilities and patient reminder systems in his desktop computer is just unbeatable and he now really wonders just how he managed to practice so effectively and safely before HealthConnect became available. Scenario 2 HealthConnect – Value Add for the Busy Specialist Dr Ted Aziz really enjoys practice as a specialist anaesthetist in his large regional centre serving patients from a wide area. The centre is large enough to mean there are 3 colleagues working at the same hospital which ensures a reasonable after hours roster while at the same time there is a wide variety of acute and elective surgery to ensure he has an interesting and fulfilling practice. The one thing Ted (and all the surgeons he works for) find frustrating are patients who are admitted for routine surgery and, when seen on the evening before the operation, are clearly not medically optimised to withstand the planned surgery and therefore have to be deferred or cancelled while their condition is improved and stabilised. This problem is annoying for all concerned (especially the patient) when they have travelled for many hours to be admitted and then have to go back home or find accommodation after being deferred. Enter HealthConnect and a dramatic improvement becomes possible. All the surgeons at the regional hospital have agreed that for any significant planned surgery the patient will be assessed in the first instance by their authorised GP who will send an event summary regarding the patient’s clinical status (including medications, recent tests etc as well as a specific pre-anaesthetic questionnaire) to the Hospital pre-admission clinic via HealthConnect. These records will then be reviewed by one of the specialist 88 HealthConnect Business Architecture v1.9 anaesthetists and, if necessary, treatment will be altered, referrals instigated and so on until it is clear the patient is ready to be admitted for their operation. The outcome of this pre-admission screening has been threefold. Unexpected last minute cancellations due to pre-existing medical conditions have almost been eliminated, patients have not had surgery unnecessarily delayed anywhere nearly as often and the average quality of pre-operative work up has been dramatically enhanced – due in large part to the improved clinical communication provided by HealthConnect. Better still, at least one aspect of ‘regional disadvantage’ is overcome as communication through HealthConnect leads to greater equality in the quality of care for patients in both large centres and small rural towns. Other benefits of HealthConnect for rural and regional patients flow directly from the speed and efficiency of communication of clinical information – so, for example, the distant local GP is alerted when his patient is discharged after surgery (at which time they can check the discharge summary on HealthConnect ) so early follow-up is possible and equally any changes made by the specialists to the patients medications and other treatments can be seamlessly continued when the patient reaches home. Scenario 3 – HealthConnect – Value Add for the Ancillary Health Workers HealthConnect has made a huge difference to the life of the consulting dietician over the years since it was made operational. Indeed Jenny Osmond, who is in private dietetic practice in the inner suburbs of Melbourne, suggests that the impact has been almost as large as that of the ‘obesity epidemic’ itself. Jenny says she remembers how things were back in 2003 when her practice was entirely paper-based and the potential impact of obesity and its health consequences were really only starting to be picked up by the public at large. Some five years later she finds her practice better integrated with both the needs of her clients and also the referring doctors as a result of HealthConnect. For her clients she now uses a Dietetic Information System (DIS) which permits her to undertake dietary assessments, set goals and provide the client with individualised evidence-based advice. Jenny can also use HealthConnect to obtain records of patient parameters which are important in her management of patients e.g. cholesterol levels, other blood lipids, calcium and vitamin D levels and so on. Better still, her DIS is able formulate an event summary for each patient and to send it to HealthConnect for those who are registered HealthConnect participants, so that she can keep the client’s GP up to date with both her initial assessment and ongoing progress reports. This service is much appreciated by the GP and assists Jenny in building her practice. Indeed a significant number of GPs are now using the closely related eHealth Message Bank to refer their patients and to arrange appointments electronically with Jenny while the patient is still in the doctor’s surgery. A year ago, in 2006, Jenny started her own client web site where registered clients can track their dietary intake and other relevant parameters like weight and general wellness. (Of course the web site also provides dietary information and advice for a wide range of dietary problems along with general recommendations as to how these problems should be addressed. Jenny hopes that soon such web services will be provided by HealthConnect to improve the integration and reliability of the patient provided 89 HealthConnect Business Architecture v1.9 information). This information is then transferred into the DIS and after review a summary of the client’s progress can be sent as an event summary when the patient is next seen. Jenny is now convinced she has, with the help of HealthConnect, reached a near ideal state in the quality and accessibility of the services she can offer her clients – to say nothing of the excellent service she offers her medical referrers and the satisfaction she derives from offering well documented evidence based care. Scenario 4 – HealthConnect – Value Add for the Community Health Nurse Nurse Jane Watson, an experienced community clinician, has seen many changes to the way healthcare services are delivered to the community in the last few years; one being the introduction of HealthConnect. These changes began in 2006 when it became increasingly common for patients who required continuing community health care to be registered with HealthConnect. This allowed the Community Nursing Service in the southern suburbs of Adelaide, with the client’s consent, to access their health record electronically, ensuring continuity and coordination of care across the inter-disciplinary team and multiple agencies providing services. These days Nursing Clinical Information Systems (NCIS) are used to provide client information, decision support and workload scheduling. New referrals (from GP’s, hospitals, and allied health services) predominately come via the eHealth Message Bank – though there are still one or two agencies (out of over 300) who have not yet moved with the times and telephone in with their requests for care. Each day clients are allocated by the service’s manager via the NCIS to individual clinicians for visits and care. When Jane arrives at work she logs onto her computer and reviews the clinical notes of the clients allocated to her. She regularly accesses HealthConnect to obtain the most recent clinical information and completes the occasional missing record from paper referrals, sending off a referral to the clerical staff to follow up these clients for information, consent and possible participation in HealthConnect. Jane is pleased that the number of clients where this is needed is dropping to the extent that by the end of 2007 she believes the need for manual entry of client details, with the risk of error and delay, will have virtually disappeared. As Jane is an endorsed Nurse Practitioner her clients tend to have more complex care needs and clinical decision making is needed to maximise their independence and ability to stay in community based care. Jane decides today because of her clients’ complexity levels that she will take her notebook computer with her rather than download data to a PDA which some of the other community clinicians prefer to do. With her notebook computer loaded with the necessary information Jane is able to plan her workflows taking into account client care needs, client appointment time preferences and the best route to minimise travel while seeing each patient. At each client visit she reviews case notes including current medications and pathology results and using her clinical judgement prescribes medication changes and orders pathology tests online. Details of these and her clinical notes from the NCIS are uploaded to HealthConnect as event summaries. With this done, the client, their GP, other community clinicians, and other members of the interdisciplinary team (who may have to, for example, treat Jane’s clients when she 90 HealthConnect Business Architecture v1.9 is on leave) can review each client’s progress, and the client’s healthcare needs can be integrated providing both more effective and safer care. As she leaves work for the day Jane reflects just how much better the services and care she can offer her clients is with continual interaction within the interdisciplinary team, compared with the days before HealthConnect. With the time saved Jane is able to comprehensively manage her complex client workload safety and is assisting more clients to remain in community based care then was ever possible before. In the past a hurried note or telephone call from a doctor, hospital or allied health professional was typically the only information source, and contact between clinicians was minimal for weeks at a time with little information sharing or care coordination except for the odd rushed telephone call. Often clients ended up in crisis, with urgent calls between clinicians, invariably resulting in her clients not being able to remain at home and independent in the community! 91 HealthConnect 7. Business Architecture v1.9 Secondary Users Participation The primary focus of HealthConnect is on recording and storing information about consumer heath care events, with this information being available to healthcare providers supporting healthcare delivery, greater coordination of care, safer care, and improved health outcomes for consumers. Over time, the HealthConnect data repository will become a highly valuable national information resource supporting important national initiatives and activities including clinical research, policy making and planning and health outcome evaluation, collectively referred to as secondary uses. This section outlines what being involved in HealthConnect will mean for secondary users such as researchers and planners. It includes: · Potential scope of secondary uses; · Benefits of participation in HealthConnect; · Consent arrangements and responsibilities of secondary users; and · Management and control of use of HealthConnect for secondary purposes. 7.1 Scope of Secondary Uses 7.1.1 Secondary Users In addition to consumers and providers, there will be a range of secondary users of HealthConnect. Secondary users are expected to include: · Researchers seeking information to conduct research needed for improving health care and its delivery; · Planners and Managers (including administrators, strategic planners, policy makers, funding bodies) seeking information to assist management decision making; and · Evaluators seeking information directly related to monitoring the effectiveness of HealthConnect. 7.1.2 Areas Secondary Uses will Support The “secondary use” of a healthcare record has been defined by the Clinical Information Project as: “Any legitimate use of a healthcare record other than the purpose of supporting the direct delivery of healthcare services to the subject of care. Examples of secondary uses include applying the record for medico-legal, quality management, clinical research, epidemiology, population health, health administration, financial, educational or health service planning purposes”. 92 HealthConnect Business Architecture v1.9 Specific areas for the secondary use of HealthConnect data could include support for: · clinical research; · analysis leading to improvements in clinical practice and health service delivery, including development of evidence-based clinical protocols and guidelines, evaluation of current clinical practice, and analysis of health outcomes. · health service delivery quality improvement mechanisms including clinical audit, continuous quality improvement studies, outcome analysis, benchmarking, resource utilisation reviews and accreditation; · provision of information for health policy development including performance monitoring, demand for health services, resource allocation and trend analysis; · improving consumer safety through healthcare product recalls (as an option of last resort, that is, where there are no other mechanisms available to identify atrisk consumers other than via HealthConnect); · detection of adverse clinical events dispersed in time and space; · clinical teaching; and · provision of information to national data collections where authorised. There is also a significant activity relating to the evaluation of HealthConnect. An ongoing program will be put in place to monitor and evaluate the success of the system and seek ways to improve the service. 7.1.3 Examples of Secondary Uses There are a wide range of reasons why secondary users may request access to HealthConnect. Examples of these include: Evaluation of HealthConnect Given the significant investment in the HealthConnect system, there will be a need to monitor and evaluate the success of the system and seek ways to improve the service. As a minimum, this will require analysis of usage and outcomes to assess whether the objectives of HealthConnect are being met. Using identified unit records to enhance consumer safety This includes developing reports listing consumers who fulfil certain criteria, for example, occurrences of: · certain procedures being performed (potentially for follow up or infection control); · certain prostheses or medication regimes (for safety recall purposes); or · given combination of medications and/or clinical conditions over a particular period. 93 HealthConnect Business Architecture v1.9 Reporting based on anonymised unit records This includes developing reports containing anonymised unit records for review and analysis such as: · occurrences of consumers that received a particular treatment regime (potentially to evaluate effectiveness of the regime); or · clinical audit and benchmarking studies. Statistical reporting of aggregated HealthConnect data There is a requirement for HealthConnect information to be used to produce performance and statistical reports on HealthConnect at regular intervals (monthly, quarterly, annually) and upon request. Subject to considerations relating to sample bias and population size, there is also considerable potential to use HealthConnect for the production of: · Indicative health statistics in specific HealthConnect populations; and · Casemix analyses. These types of uses, which are likely to be common, could be largely automated. 7.2 Benefits of Secondary Uses The ability to use HealthConnect information to support secondary uses is seen as a key benefit of HealthConnect by consumers, healthcare providers, clinical researchers and Australian Government, State and Territory health jurisdictions. A full analysis of the potential HealthConnect benefits is presented in the Benefits Realisation Approach15. While it is recognised that the benefits from secondary uses will be limited in the short term, there is considerable potential as participation rates, volume and type of data collected increases, to: 15 · use the information held in HealthConnect to improve the quality, effectiveness and efficiency of the Australian health care system; · establish a detailed picture of Australians’ health profile, leading to advances in the treatment of illnesses and improvements in the day-to-day and long-term care of all Australians; and · increase the amount of information available for research purposes to enable Governments to make more informed decisions about health sectors that should be targeted in the future. With better information, Governments can become more responsive to the community’s needs. HealthConnect Benefits Realisation Framework V1.0 October 2004 94 HealthConnect Business Architecture v1.9 7.3 Consent and Responsibilities 7.3.1 Consent for Secondary Uses The HealthConnect Principles state that: · HealthConnect will support secondary use of HealthConnect EHR information for improvement of health service delivery and research purposes, in line with strict privacy and ethical protocols, appropriate legislative requirements and monitoring of such use. · The consumer must have given informed consent before their EHR and other personal information can be collected, accessed, used or disclosed by HealthConnect. This will form part of the initial consumer consent process. Consumers and providers participating in HealthConnect will be informed that information will only be used for approved secondary uses, and in accordance with best practice guidelines and privacy protocols developed for HealthConnect, including being subject to independent scrutiny. The use of identified data (ie personal health information) will be in accordance with the Privacy Act and National Health and Medical Research Council (NHMRC) guidelines. The use of de-identified data will likewise be subject to approved guidelines, drawing on work underway at the national level to develop best practice in this area. At registration, consumers and providers will be informed: · that their information will be used for approved secondary purposes only, in accordance with strict privacy protocols and ethics committee scrutiny; · about the range of uses to which the health information might be employed; and · how they can access information about the HealthConnect approval process for secondary uses and the arrangements in place to safeguard consumer and provider privacy. 7.3.2 Responsibilities of Secondary Users The use of HealthConnect to support secondary uses will require high-levels of consumer and provider support and confidence that their health information will only be used in accordance with strict procedures including ethics approval. HealthConnect participants, researchers, planners and evaluators will have to abide by the privacy legislation and protocols. The HealthConnect Principles state that: · HealthConnect participants will be obliged to abide by privacy legislation and by specific HealthConnect privacy rules. The National Health Privacy Code will be used when it has been implemented, until then privacy arrangements will be tailored to suit each jurisdiction for each implementation, with a view to progressing towards a single national solution. As participants of HealthConnect, secondary users’ responsibilities include: 95 HealthConnect Business Architecture v1.9 · commitment to using the information only for the purposes stated, including commitment to take reasonable endeavours to ensure accurate interpretation of the information provided; · participation in line with the HealthConnect confidentiality and privacy arrangements; · commitment to abiding by HealthConnect processes for secondary uses including rules relating to circulating and publishing information; and · provision of a secure environment for storage of HealthConnect supplied information. 7.4 Governance of Secondary Uses 7.4.1 Governance Structure The HealthConnect Principles state that: · HealthConnect will support secondary use of HealthConnect EHR information for improvement of health service delivery and research purposes, in line with strict privacy and ethical protocols, appropriate legislative requirements and monitoring of such use. Hence a key role in HealthConnect will be that of managing the process of granting access to HealthConnect information for agreed purposes in line with national privacy legislation and the research and ethics best practice guidelines of the NHMRC. HealthConnect’s governance structures, yet to be finalised, will contain arrangements for the independent and transparent monitoring of the role of HealthConnect in authorising and managing access to information for secondary uses. Types of representation to be included are likely to be: · Consumers; · Professional bodies representing healthcare providers; · Other national agencies involved in the provision and use of national data collections (to ensure a consistent approach); and · National Health and Medical Research Council (NHMRC). Assistance will be sought from the Australian Health Ethics Committee (AHEC), established under the NHMRC Act 1992 to advise NHRMC on ethical issues relating to health and developing guidelines for the conduct of medical research involving humans. AHEC membership is specified in the Act and draws on experts in philosophy, the ethics of medical research, public health and social science research, clinical medical practice and nursing, disability, law, religion and health consumer issues. 96 HealthConnect 7.4.2 Business Architecture v1.9 Secondary Uses Approval Process The provision of access to data for secondary uses will only be allowed under strict protocols and subject to ethics committee approval. These will include ensuring authorisation has been given for the requested use; extracting the information; performing any aggregation and de-identification activities required. The specific processes have not yet been defined. It is recognised that these processes will need to be consistent for all requests for secondary uses with the associated procedures for approval being dependent on the type of information (and extent to which it might identify individuals or communities) and sensitivity issues of the secondary use being proposed. There are also expected to be reasons for secondary uses not yet envisaged and the process and procedures will need to be enhanced over time to accommodate these. Hence proposals for secondary use of HealthConnect data should be assessed against ethical and legal principles, which need to be established, rather than by specifying categories of permissible use. At a minimum, all such secondary uses will be subject to ethics committee assessment. Generation of and use of published aggregated data would not require very tight controls as long as it has been aggregated according to best practice processes (eg Australian Bureau of Statistics and AIHW). Management of “small cell” inference is one issue of particular concern. Ethics approval once given may be valid for ongoing production and use of regular reports eg disease type by age and sex. For more sensitive uses, HealthConnect may establish a process which includes: · a formal request to HealthConnect ; · the provision of evidence of local ethics committee approval (in line with the user’s clinical, academic or jurisdictional affiliations); and · a HealthConnect ethics approval process. This process is consistent with the approach used to access de-identified data from other national data collections, such as those held by the Australian Institute of Health and Welfare (AIHW), preventing any potentially identifiable data being released into the public domain. The use of identified data for research purposes will be assessed through a rigorous approval process, including ethics committee assessment. Such approved purposes will only be permitted according to strict criteria, and with agreements in place to govern the handling and security of stored data within an organisation and subsequent publication of the research findings to protect individual and community privacy. HealthConnect will not support any secondary uses that involve: · identification of individual HealthConnect consumers or providers explicitly through use of consumer and provider identification details, except in limited, approved circumstances as determined by the HealthConnect governing body; · identification of individual HealthConnect consumers or providers implicitly through small cell inference, for example, participants from small populations or local communities; or · uses that contravene national legislation or recognised best practice. 97 HealthConnect 7.4.3 Business Architecture v1.9 Information Access Process In most cases, requests for access to HealthConnect data for approved secondary uses will result in the provision of an authorised HealthConnect “report” (i.e. an extract of data) consisting of the required data set. The report will be issued to the requestor for use exclusively in the way defined by the approval process. HealthConnect will not provide the analytical tools required to process the data set, although HealthConnect will support requestors in the interpretation and use of HealthConnect data. As part of the approval, HealthConnect will have the right to scrutinize research prior to it being published to ensure compliance with the ethics approval guidelines. 7.5 Secondary User Scenario Scenario – HealthConnect – Value Add for the Population Dr Debra Fern is a consultant public health advisor to a number of Australian governments and has been carefully tracking the progress of HealthConnect since state implementations began in late 2005. She has been delighted with the progress she has seen in the last three years but is convinced the best is yet to come. She has seen the secondary uses of HealthConnect data deliver major benefits, especially in the areas of preventive care, improved patient safety and detection of systemic quality of care failures. Most especially Debra remembers the time before HealthConnect and similar systems were available when medication side effects, which were not picked up in standard clinical trials, could go unrecognised for years after initial product marketing because of the gaps in post marketing surveillance. Among the risks for which detection seems to have been significantly delayed, often with fatal consequences, but which are now know about are the risk of: · Suicide in young patients given some antidepressants to treat their depression; · Hyperkalemia and cardiac arrest in spironolactone treatment for some heart failure patients and; · Life threatening muscle problems associated with some of the cholesterol lowering medicines. Debra now sees a range of HealthConnect research applications in frequent use including: 1. A much enhanced post-marketing surveillance program for prescription, over the counter (OTC) and complementary medicines. Hospital discharge event summaries are now routinely searched for evidence of admissions related to side effects of drug therapies and medical practitioner and pharmacist event summaries are screened for evidence of out-of-hospital adverse events. Even with 20 per cent of the population registered to use HealthConnect, there is the capacity to detect the rarest of side effects 98 HealthConnect Business Architecture v1.9 (which may not have been found in clinical trials which typically involve less than a few thousand patients) quickly and ensure the proper warnings are given to doctors and the public promptly. Thus, despite the fact that not everyone is signed up for HealthConnect, this has resulted in a dramatic improvement in the quality of medicine safety surveillance for everyone. Better than this, in the event of a serious problem being identified in post marketing surveillance, press coverage and letters to practitioners can help to promptly alert people to take whatever remedial action is required for the whole population. 2. With effective coding of procedures and outcomes developed during 2006 HealthConnect has the capacity to very effectively monitor the quality of care delivered in a range of areas and to use well understood indicators to monitor patient safety in great detail. What may be monitored can include such parameters as: re-admission rates for particular diseases, unexpected re-admissions following surgery or medical treatment, medical device failures, use of crucial recommended treatment for specific illnesses etc. This allows early and effective responses to ‘health black spots’ and the difficult to recognise systemic health system failures. The detail of the information now available to ensure patients receive optimal treatment is genuinely amazing and really only possible with a national network like HealthConnect. 3. Daily tracking of prescribing patterns nationally now occurs routinely. Not only does this permit assessment of the various influences on prescribing and drug use patterns (advertising etc) but it also provides early warning of emerging epidemic diseases through monitoring of prescriptions for anti-flu or symptom-management medication. 4. Geographically linked prescribing data of the sort now available from HealthConnect also allows for assessment of regional variations in prescribing and medical device use to assist in identification of under and over use of expensive resources. HealthConnect now can also assist in ensuring all cases where a medical device of critical importance such as a heart valve or implantable defibrillator is used the fact is entered on a registry so adverse outcomes for those patients can be regularly assessed and the risk of failure identified and modified / acted upon if necessary. 5. HealthConnect event summaries can be aggregated over time to provide profiles of usage and resource consumption. These can augment that found in the Medicare statistics because they cover Medicare and non-Medicare transactions and contain more clinical information, which can provide a finer-grained view of what is driving resource use. 6. Linkage of event summaries associated with such diverse matters as cancer diagnosis and childhood vaccination is assisting to identifying areas of special need, concern or risk where further investigation and research may be warranted. 7. In special circumstances Debra is pleased to know it is even possible to check patients who have a diagnosis of potentially lethal clots in their legs to see if they had the diagnosis at a time when they had recently been overseas. This can be done with none of the patients being identified in any way – but can permit certainty as to just how risky flying overseas is and if necessary prompt extra study as to how this potentially lethal problem can be avoided and if it would be safe and effective to do so. Debra is very firmly of the view that, with careful planning, HealthConnect can make a major contribution to the reduction of risks which may not become obvious for months 99 HealthConnect Business Architecture v1.9 or years without its help, thereby improving the opportunity for earlier, better and more cost-effective intervention and cures. As well it can act as a very effective monitoring tool for the quality and patient safety of the whole health system and pin point problems well before too much harm is done. 100 HealthConnect Business Architecture v1.9 Part D – Description of HealthConnect Components 101 HealthConnect Business Architecture v1.9 This part identifies and describes key components of HealthConnect and its surrounding context with a focus on developing the links between the high-level business requirements discussed in previous parts and the more detailed descriptions of components required as part of an enterprise architecture that can support the development of HealthConnect. This work is informed by the Federal Enterprise Architecture Framework (FEAF) used in the development of both version 1 of the HealthConnect Business Architecture and version 0.9 of the HealthConnect Systems architecture and is intended to provide a foundation for subsequent work on the HealthConnect data, application and technology architectures. In this part, various HealthConnect components and their interrelationships are developed by use of process mapping, which considers the roles, processes, information and technology needed to support HealthConnect. The following sections discuss each of the identified components in more detail from the following perspectives: 1. Section 8 presents the analysis of HealthConnect roles and discusses the entities, processes, information and technologies used to perform the role. 2. Section 9 identifies the high-level information components needed to deliver HealthConnect (informing the HealthConnect data architecture). 3. Section 10 catalogues and discusses the business processes associated with the delivery of HealthConnect (forming a basis for the HealthConnect applications architecture and more detailed functional requirements). 4. Section 11 presents an overview of the major application systems and technology components needed to support HealthConnect (providing an input to the technology architecture). The functions and characteristics of these HealthConnect components are also developed in a separate attachment to this business architecture entitled Specification of HealthConnect Business Requirements. 8. HealthConnect Context and Roles Figure 8.1 on the following page presents a role map illustrating the major roles and functions associated with the delivery of HealthConnect services. The role map includes both roles performed within HealthConnect itself (indicated by the shaded zone) and roles performed within associated entities (such as providers and consumers). Roles associated with the delivery of HealthConnect are grouped as follows: 1. HealthConnect participants - consumers, providers and secondary users; 2. Core HealthConnect roles, including those for registration of consumers and providers, maintaining the HealthConnect EHR repository, managing the structure and content of EHR information, and for governance of HealthConnect, which includes regulating interaction with HealthConnect and evaluating HealthConnect performance; 103 HealthConnect Business Architecture v1.9 3. HealthConnect Consumer Access Services (HCCAS) that support customer interaction with HealthConnect and may also offer additional services of interest to consumers; 4. Provider eHealth Access Services (PeHAS) that support providers interacting with HealthConnect; 5. eHealth Message Bank Service, an adjunct to the core services, to facilitate electronic information interchange for HealthConnect and other purposes, such as electronic retrieval of prescriptions, referrals and notifications; 6. HealthConnect ICT infrastructure (for HealthConnect and other services), which includes secure networks, IT processing platforms, clinical applications and the organisations that support these services; 7. National health infostructure, which provides national repositories and information definitions that underpin the operation of HealthConnect; and 8. Other contributors and recipients of information – specifically value-added eHealth services and (potentially) health registries. National Health InfoStructure National Health Identifier Service (Consumers) Health Information Standards, Terminologies and Data Sets National Health Metadata Repositories National Health Provider Directory Secondary User HealthConnect Governance HealthConnect Metadata Repository HealthConnect EHR Repository National Data Store Consumer Consumer Registration & Management HealthConnect Consumer Access Services HRS/ AEM ... HRS/ AEM Provider Registration & Management Health Connect Provider Directory HealthConnect Consumer Index Provider Provider eHealth Access Services Value Added eHealth Services Health Registries eHealth Message Bank Service Supporting ICT Infrastructure Processing Platforms Clinical Information System Support Clinical Applications Secure Communications Networks Figure 8.1 – Role Map for Delivery of HealthConnect Services Each role is discussed in more detail on the following paragraphs with consideration being given to the entities that might carry out the role, and the processes, functions and information needed to perform the role. 104 HealthConnect Business Architecture v1.9 HealthConnect Participants 8.1 Consumers All Australian citizens and residents of Australia will be eligible to participate in HealthConnect as consumers. In stage 1 this participation is expected to be limited to those identified as being eligible to receive Medicare benefits but, in the future, this may be extended to other persons determined by the HealthConnect governing body. A consumer’s participation in HealthConnect will be subject to the consumer (or an appropriate agent) having given consent to participate and having completed the consumer registration process. Agents able to register a consumer include parents (for a child), a legal guardian or person with power of attorney over the consumer’s health care or a person specifically authorised by the consumer in accordance with HealthConnect rules. Each consumer’s EHR will be held by an Approved EHR Manager (AEM) on a HealthConnect Records System (HRS) and consumers will be able to access and interact with HealthConnect through one or more HealthConnect Consumer Access Services (HCCAS). The primary processes and functions which HealthConnect consumers may perform include: (a) Registering as a HealthConnect consumer, providing initial registration details; (b) Accessing HealthConnect as a consumer (including maintaining an access control list, reviewing EHR information and checking access by others); (c) Maintaining consumer registration details; (d) Seeking HealthConnect support assistance, where required; and (e) Accessing value added eHealth services (where available) through the consumer’s HealthConnect consumer access service. Consumer access to HealthConnect will typically be via web browser interface hosted by the relevant HealthConnect consumer access service and will be protected by a password/PIN. 8.2 Providers 8.2.1 Types of HealthConnect Provider Provider participation in HealthConnect occurs at the level of both: (a) an individual provider, and (b) a provider organisation. In the medium to longer term, HealthConnect must be able to service a broad range of individual providers, including: 105 HealthConnect Business Architecture v1.9 (a) General practitioners; (b) Specialist medical practitioners; (c) Diagnostic specialists including pathologists and radiologists; (d) Nurse practitioners and community nurses: (e) Pharmacists; (f) Physiotherapists, chiropractors, podiatrists, optometrists and dentists; (g) Other allied health workers delivering individual health care services, including: occupational therapists, speech therapists; dieticians; social workers and clinical counsellors; (h) Aboriginal and Torres Strait Islander (ATSI) health workers. Provider organisations may be either publicly or privately funded and include: (a) Any of the above individual providers, operating as a sole trader or as a business enterprise; (b) General practices and medical centres; (c) General hospitals and specialist hospitals; (d) Aboriginal Community Controlled Health Services (ACCHS); (e) Residential aged care facilities and nursing homes; (f) Community health centres, community care and shared care teams; (g) Clinical staff working in call centres providing health advisory services; and (h) Any similar type of service offering health services to consumers as individuals or as part of identified group of consumers within a health care program (such as a shared care program). Where the word "provider" is used without qualification in this part, it should be interpreted as encompassing both individual providers and provider organisations as appropriate to the context in which the word is used. 8.2.2 Provider Access to HealthConnect A provider’s participation in HealthConnect will be subject to the provider having entered into a legal agreement with the HealthConnect governing body which will set out the obligations of the provider and provide the basis both for the provider’s use of HealthConnect and the protection of consumer privacy. In the case of provider organisations, the agreements will place requirements on the provider with respect to its employee’s activities and the interoperation of its systems with HealthConnect and will identify the person responsible for the organisation’s use of HealthConnect. 106 HealthConnect Business Architecture v1.9 To facilitate an appropriate level of access control without presuming how provider organisations may register with HealthConnect, HealthConnect needs to allow major organisational units (such as a hospital or clinic) to be identified separately within HealthConnect while still recognising their link to the head provider organisation. Provider organisations will interact with HealthConnect through one or more provider eHealth Access Services (PeHASs), which provide communication pathways between the provider and the HRS/AEM in which a consumer’s EHR is held. Before permitting a provider organisation to access the consumer’s EHR, providing any confidential consumer identification details, or allowing any entry to be made in the EHR, the HRS/AEM must authenticate the initiating provider organisation’s access credentials against the consumer’s access control list. Each event summary submitted for inclusion in a consumer’s HealthConnect EHR must be attributable to a registered individual provider, even though entries will originate from within a provider organisation. All persons accessing a HealthConnect EHR on behalf of a provider organisation must be either a registered individual provider or a person (eg support staff and junior clinicians) authorised by the provider organisation and uniquely identified to HealthConnect by the provider organisation. Provider access to HealthConnect will be accommodated via a combination of access technologies including HL7 and/or XML-based web service messaging to and from the provider’s clinical information system and an option of providers using a limited web browser interface (hosted by the relevant PeHAS). 8.2.3 Provider Processes Specific processes identified as potentially being performed by providers include: (a) Register with HealthConnect as an individual provider and/or a provider organisation; (b) Retrieve/use consumer EHR information; (c) Update consumer EHR information; (d) Send/Receive eHealth communication; (e) Access value-added services; and (f) Seek HealthConnect support assistance. 8.3 Secondary Users Secondary users who access HealthConnect information for legitimate purposes other than direct care delivery to a consumer and are expected to include: (a) researchers, carrying out basic and applied research; (b) health managers and planners 107 HealthConnect Business Architecture v1.9 (c) HealthConnect evaluators; and (d) the HealthConnect management team, for purposes associated with management and control of HealthConnect itself. All secondary uses of HealthConnect must be subject to stringent approval including review and acceptance by an ethics committee and measures that protect the privacy of individuals and the confidentiality of their personal data. The HealthConnect governing body sets and enforces the policies and guidelines for secondary uses. Core HealthConnect Roles HealthConnect Governance 8.4 Details of the proposed governance structure for HealthConnect are being finalised in parallel with the documentation of this business architecture and are discussed in further detail in Part E below. While details are still being resolved, it is widely accepted that overall management of the HealthConnect program at the national level will be vested in a dedicated organisational entity on behalf of all the participating governments and other stakeholders. This organisational entity is commonly referred to as the HealthConnect governing body. HealthConnect is also being progressed regionally through HealthConnect trials and lead-state/territory implementations. Each of these initiatives currently has its own governance structure, which encompasses many of the same functions at a local/regional level as are proposed to be carried out by the HealthConnect governing body at a national level. For the short- to medium-term a significant proportion of HealthConnect management functions will be performed at a regional level. 8.4.1 HealthConnect Governance - Functions and Processes The HealthConnect governance role may be encapsulated by three high-level functions: · Administration of HealthConnect programs; · Management of HealthConnect participation; and · Establishment and operation of HealthConnect infrastructure. Identified processes for administering HealthConnect programs include: (a) Establish HealthConnect operational policies and standards (b) Establish arrangements for coordinated national delivery of HealthConnect (c) Procure HealthConnect systems and infrastructure (d) License HealthConnect consumer access and provider eHealth access services (e) Evaluate HealthConnect outcomes 108 HealthConnect Business Architecture v1.9 Processes for managing HealthConnect participation include: (a) Promote community awareness of HealthConnect (b) Engage with stakeholder bodies (c) Contract with health providers for use of HealthConnect (d) Agree HealthConnect supply terms for consumers (e) Manage approval and monitoring of secondary uses (f) Administer access to HealthConnect (g) Monitor access and audit/report usage (h) Handle consumer and provider complaints (i) Coordinate HealthConnect records management functions Processes for establishing and operating HealthConnect infrastructure include: (a) Promulgate metadata and standards for HealthConnect (b) Maintain National Data Store (c) Maintain HealthConnect Metadata Repository (d) Maintain HealthConnect Consumer Index (e) Maintain HealthConnect Provider Directory (f) Manage HealthConnect ICT infrastructure (g) Run HealthConnect operations (h) Organise clinical systems to inter-operate with HealthConnect There are many routine HealthConnect operational activities that will be managed through or on behalf of the HealthConnect governing body, these include: (a) Maintaining processes for the creation, update and distribution of HealthConnect metadata and for managing its application and use in HRS facilities and in HealthConnect interfaces. (b) Operation of the national data store and processing services to support secondary uses of HealthConnect data. (c) Oversight of message handling and transport operations. (d) HealthConnect registration operations. (e) Performing other management, technical and operational tasks delegated by the HealthConnect governing body from time to time. These functions may be undertaken by the HealthConnect governing body itself or, alternatively, they may be performed by other organisations contracted to perform them on its behalf. 109 HealthConnect Business Architecture v1.9 Until the HealthConnect governing body and its operational support arrangements are fully active, similar operational functions will be needed locally to support initial HealthConnect implementations. Longer-term integration of these functions into the national Program will need to be considered by the HealthConnect governing body and the relevant jurisdictions. Front-line HealthConnect registration functions may be carried out through various registration agencies; however, the following types of registration operations may be best handled through a HealthConnect registration centre operating at a national level: (a) Providing a contact point (potentially via a call centre) for consumers needing to modify their registration details or seeking information about participation in HealthConnect. (b) Providing a contact point (potentially via a call centre) for providers needing to modify their registration details. (c) Supervision of HealthConnect registration systems and processes, including management of the HealthConnect registration application system and overseeing the activities of HealthConnect registration agencies. (d) Ensuring the operational integrity of the Consumer Index and Provider Directory, including handling complex registration issues (such as resolution of duplicate identities). 8.5 HealthConnect EHR Repository 8.5.1 The Federated Model for HealthConnect Delivery HealthConnect is to be implemented as a federation of HealthConnect Records Systems (HRS) supported by common services at a national level, with the entirety of each consumer’s EHR being stored in only one HRS. All EHR information submitted to HealthConnect is received by the HRS on which the consumer’s EHR is held and, if valid, is incorporated into the consumer’s EHR. Within 24 hours of an EHR being updated (and preferably much earlier), a copy of the updated EHR material is to be transmitted in a standard format by the responsible HRS/AEM to the National Data Store for archiving and long-term retention. Together, the EHR information held in each HRS and the National Data Store comprise the HealthConnect EHR repository. Whilst the HealthConnect EHR repository is to be distributed across a number of federated elements, it is intended that it be available as a single national resource from the viewpoint of access, interoperability, reporting and inquiry. Within this framework, it is proposed that the National Data Store be used to support all secondary use of HealthConnect EHR data for research and planning purposes, while all operational interaction with a consumer’s EHR will occur through the HRS. Such a federated approach has the potential to relieve problems of scale and, depending on the implementation model adopted, may allow for a diversity of technology solutions. 110 HealthConnect Business Architecture v1.9 It has also been perceived as being more consistent with local strategies and the current regional nature of healthcare delivery. For HealthConnect to have seamless capability to accept, store and interchange standardised EHR information using the federated approach, each HRS must conform to a common EHR architecture, common interface standards and common specifications. It is important that each HRS validate, accept and be capable of delivering event summaries in accordance with national HealthConnect information standards – nonstandard records cannot be used by other HRS nodes, at the national level or by individual provider systems. Certainly, in the first few years, as the HealthConnect concept is developed through separate implementations in several jurisdictions, there will be differences in the role and function of each HRS. Reconciling these differences with the preferred approaches set out in this business architecture remains one of the key challenges facing HealthConnect as a national program and strategies for managing this issue need to be developed as a high priority. 8.5.2 HealthConnect Records System (HRS) Version 0.9 of the HealthConnect Systems Architecture proposed that the core element of HealthConnect be the HealthConnect Records System, or HRS, on which a consumer’s EHR is stored, with the HRS managing EHR updates and controlling access to the EHR. While the precise role and functions of an HRS have been refined considerably since they were documented in the HealthConnect Systems Architecture, the HRS continues to be the centrepiece of a HealthConnect implementation, performing the functions of EHR storage, update and access control. It also remains a core principle of HealthConnect that: “a consumer’s entire HealthConnect EHR should reside on one and only one HRS”. Each HRS is based on an HRS Application which is to provide functions in the following general areas: 8.5.3 (a) Controlling access to EHR and consumer information; (b) Maintaining consumer details and access control lists for those consumers holding their EHR on the HRS; (c) Processing event summary information into a consumer’s EHR (including maintaining managed lists and views); (d) Responding to (authorised) EHR information requests; (e) Interaction with the shared HealthConnect consumer index, provider directory and metadata repository; and (f) Keeping audit trails and access logs recording all access, outputs and changes involving consumer information held in the HRS. Approved EHR Manager (AEM) In the federated structure proposed for HealthConnect, service providers referred to as “Approved EHR Managers” (AEMs) will contract with the HealthConnect governing body to provide the functions of a HealthConnect data centre or service bureau. 111 HealthConnect Business Architecture v1.9 Under this version of the HealthConnect business architecture, the role of an AEM in managing an HRS has been identified as being different from the roles of a HealthConnect Consumer Access Service (HCCAS) and/or a Provider eHealth Access Service (PeHAS), although, for some implementations of HealthConnect all three roles may be performed by the one organisation. Each AEM will be responsible for the security and access control of EHR information held in the HRS that they operate. The AEM must protect the confidentiality, integrity and availability of the EHR, by: · providing a physically secure processing environment for the HRS with access restricted to personnel that have been vetted and are duly authorised; · authenticating the identity of all users or organisations that seek access to EHR information; · restricting access to an EHR (including any views and reports derived from the EHR) in accordance with the consumer’s consent settings and policies defined by the HealthConnect governing body; · managing, maintaining and administering the HRS databases, audit trails and access logs; · ensuring that the access log for each EHR is maintained, complete and accessible for review over an extended period; · ensuring that HRS applications, systems software and hardware are properly maintained to ensure integrity and performance of the service; · protecting the confidentiality and integrity of data communicated over public networks; · providing business continuity and disaster recovery for the EHR Repository (covering EHR information, access logs and audit trails); HRS/AEM – Processes 8.5.4 The following high-level processes were identified in the context of performing the role of an HRS/AEM, include: (a) Manage HRS databases and audit trails (b) Apply updates to consumer details and access control lists (c) Apply consumer preferences (d) Control access to EHR information (e) Update/maintain HRS Application software (f) Maintain compatibility with HealthConnect metadata (g) Maintain HRS processing platform and network environment (h) Apply and monitor ICT security measures 112 HealthConnect 8.6 Business Architecture v1.9 National Data Store The National Data Store (NDS) is managed by (or on behalf of) the HealthConnect governing body to provide a data storage and archiving service that aggregates EHR information sent from all HealthConnect EHR datasets to support: (a) Reporting across the national HealthConnect population for use in research, planning and management of the HealthConnect program; (b) Review, development and management of HealthConnect metadata; and (c) Maintenance of archival copies of each EHR to support recovery of records (if corrupted at an HRS), allow access for secondary use without impacting operational performance, and support ad-hoc access for specific enquiries. An access log is also to be maintained of all access to the National Data Store. Where access to an HRS (such as a query) results in new artefacts being added to an EHR, those artefacts will form part of the updated EHR material that the HRS supplies to the National Data Store. HealthConnect Metadata Repository 8.7 The role of the HealthConnect Metadata Repository is to maintain a long-term versioncontrolled collection of metadata implemented within HealthConnect and provide a single reference point that can be accessed by everyone needing authoritative metadata for: (a) interfacing with HealthConnect and supplying information for incorporation into the HealthConnect EHR repository; (b) validating the structure and content of EHR information submitted as event summaries; (c) interpretation, linkage and storage of EHR information; (d) accessing information held in the HealthConnect EHR repository; (e) production of meaningful views and lists spanning information submitted over time; and (f) interpreting HealthConnect EHR information in other applications, such as clinical decision support systems. The HealthConnect metadata repository will be centrally maintained by (or under the authority of) the HealthConnect governing body and each HRS/AEM will derive the structure, content and validation rules for event summaries, lists and views from locally applied versions of this metadata. The metadata will also form the authoritative source of information for the design of interfaces to HealthConnect. 113 HealthConnect Business Architecture v1.9 Maintenance of the HealthConnect metadata repository will be carried out in close cooperation with the Clinical Information Project, which will provide formalised metadata definitions for incorporation into the repository. There will also be close liaison with the AIHW, to ensure that HealthConnect definitions and structures comply as closely as possible with the definitions in the National Health Data Dictionary (NHDD) and are compatible with METeOR (the proposed new national health metadata repository). Maintaining the HealthConnect Metadata Repository is identified as one of the highlevel business processes required as part of the establishment and operation of the HealthConnect infrastructure – currently being performed by the HealthConnect Program Office in collaboration with the Clinical Information Project (CIP) but ultimately to be done under the auspices of the HealthConnect governing body. 8.8 Consumer Registration and Management Consumer registration and management is an important aspect of HealthConnect and has, justifiably, received a great deal of attention since the concept of a national system of electronic health records was first proposed in the National EHR Taskforce (NEHRT) report. At the national level, the HealthConnect governing body has responsibility for establishing and enforcing appropriate policies and procedures for managing the relationship between participating consumers and various elements of the overall HealthConnect solution. This includes rules for consumer registration, notification of consent and for deregistration from HealthConnect. The HealthConnect governing body also has responsibility for national awareness and marketing of the HealthConnect program to consumers, providers and the community at large. A consumer must be uniquely identified and registered in order to participate in HealthConnect. The avoidance of duplicate identities requires that, in most cases, the consumer will need to identify themselves personally to an authorised HealthConnect consumer registration agency. While some registration management functions can be performed online by electronic means, many, including initial registration for some consumers, will require face-to-face contact, at considerable cost to both the consumer and HealthConnect. To achieve high participation rates, HealthConnect Consumer registration and management functions need to be efficient and available in communities across Australia, close to the consumers themselves. Efficiencies in HealthConnect registration are anticipated through the implementation of a national health identifier, possibly coupled with the introduction of individual Medicare smartcards. The new smartcards will be issued to most Australians over the next few years as a replacement for their current magnetic stripe Medicare cards. Holders of the new smartcards will have a unique secure identity for accessing a wide range of health care benefits, including a separate identifier for registering with, and accessing, HealthConnect. Consumers that obtain the new smartcards will have already identified themselves to the Health Insurance Commission (HIC) through Medicare. 114 HealthConnect Business Architecture v1.9 It is not currently proposed that the HealthConnect governing body establish its own Australia-wide physical presence to perform consumer registration and management functions, but rather, that it will: (a) Allow consumers holding the new Medicare smartcard to register online by using the smartcard and other information (eg. a PIN) to identify themselves; and (b) Appoint one or more HealthConnect consumer registration agents to provide face-to-face registration services. Although Medicare outlets are ideally placed to provide HealthConnect registration services; this would be subject to resolution of jurisdictional issues and an agreement between HIC and the HealthConnect governing body. Subject to them having access to appropriate facilities (including the ability to access the registration application), there is no reason for other organisations not to be licensed to perform the HealthConnect consumer registration role – candidates include HealthConnect consumer access services, registration agencies established to support a state or regional HealthConnect initiatives, and organisations having a close relationship with various large groups of health consumers. The consumer registration and management role must be supported by a group of business processes to establish and maintain consumer registration, including: (a) Market HealthConnect to consumers (b) Register consumer with HealthConnect (c) Update/recover consumer registration details (d) Process consumer deregistration from HealthConnect (e) Manage tracking of consumer surrogates The process of registering a consumer with HealthConnect includes: (a) the allocation and activation of unique HealthConnect consumer identifier linked to the National Health Identifier (should it proceed); (b) capturing the consumer’s details and the provider organisations to be included on their access control list; (c) setting up the consumer with a record on an HRS/AEM; (d) providing or capturing a security code for accessing/authorising HealthConnect information; (e) entering the consumer’s identifier and personal details into the HealthConnect Consumer Index; and (f) arranging for information to be collected (eg. from the consumer and any treating practitioners) for the consumer’s initial health profile and loading it into the consumer’s EHR. 115 HealthConnect Business Architecture v1.9 The processes involved in establishing and maintaining consumer registrations and associated consumer details need to be supported by a single HealthConnect registration application available to all licensed HealthConnect consumer registration agencies. Local requirements may accommodate different registration processes, where required to meet particular local needs eg different registration processes for ATSI people. Once a consumer is registered with HealthConnect, their registration details can be maintained by online access, in person at any HealthConnect consumer registration agency or by telephone to a HCCAS or to the central HealthConnect registration centre. In all cases, the consumer must provide one of the forms of identification normally required for access to HealthConnect. Where a consumer has lost or mislaid their HealthConnect identification details or password/PIN, they would either visit a HealthConnect consumer registration agency in person or, alternatively, contact the HealthConnect registration centre so that the access could be reset, using other identifying information held in the HealthConnect registration system. 8.9 HealthConnect Consumer Index As a consumer is registered with HealthConnect, their HealthConnect identifier, their personal details, and a link to the HRS on which their EHR is held, are set up in the HealthConnect Consumer Index. The index will also hold a reference to their entry in the National Health Identifier system (should it proceed). The primary role of the HealthConnect Consumer Index is to provide the linkage information needed by HealthConnect message handling and transport applications to identify the appropriate HRS on which a registered consumer’s EHR is stored. In this way, a communication pathway can be established between an authorised provider (operating via a PeHAS) and the HRS so that the provider may retrieve and contribute to the consumer’s EHR information. Similarly, the Consumer Index provides flexibility for consumers to access their EHR via HealthConnect portals not directly associated with the HRS on which their EHR is stored. The master copy of the HealthConnect consumer index is to be maintained by (or on behalf of) the HealthConnect governing body as a national HealthConnect resource and this copy alone will hold information needed to re-establish the consumer’s HealthConnect identity should this be lost. Some information from the Consumer Index is expected to be replicated to access services to facilitate faster processing. The main function of the HealthConnect Consumer Index is to direct HealthConnect transactions to the HRS on which the consumer’s EHR and other information is held – not to validate a person’s right to access the consumer’s EHR information. Once a HealthConnect transaction arrives at the relevant HRS, the HRS is responsible for controlling access, using the access control list supplied by the consumer. The Consumer Index will hold sufficient information in secure form to enable a frontend application or HRS to confirm that the HealthConnect identifier matches the consumer’s password/PIN, thereby permitting the consumer to use their password/PIN to authenticate HealthConnect transactions online. 116 HealthConnect Business Architecture v1.9 HealthConnect Consumer Access Services 8.10 The primary role of HealthConnect Consumer Access Services (HCCAS) is to provide consumers with an effective means of accessing HealthConnect services and to give them front line support for using HealthConnect. Processes identified as being potentially associated with the HealthConnect Consumer Access Service role include: (a) Provide HealthConnect consumer access portal service (for consumers accessing HealthConnect via a web browser and via consumer health information systems) (b) Provide advice, assistance and training to consumers using or starting to use HealthConnect (c) Provide consumer hotline support to resolve HealthConnect access and usage problems (d) Assist with marketing HealthConnect to consumers (e) Facilitate consumer registration (f) Provide consumer access to value added services, potentially including supply of HealthConnect-compliant consumer health information systems (g) Monitor and report service delivery performance indicators Depending on decisions taken by the HealthConnect governing body, this business architecture does not restrict the organisations that can perform an HCCAS role. Potentially, consumers could obtain HealthConnect Consumer Access Services via a number of different approaches, including: · Directly via a national HealthConnect web portal organised directly by the HealthConnect governing body (for simple consumer access); · Via an organisation operating as a HealthConnect registration agency; · Via organisations offering value-added services to consumers, including health information service providers, health insurers, and associations providing targeted services to specific groups of health consumers (such as shared care programs); and · From a service originally established to support a regional implementation of HealthConnect. Those operating an HCCAS would have access to the Consumer Index and the HealthConnect message handling and transport applications. It is most important that HCCAS operators support standard HealthConnect interface protocols for accessing HRS and national HealthConnect services. To ensure that confidentiality of consumer personal information and the security of the HealthConnect ICT infrastructure is preserved, all HCCAS operators must be licensed by the HealthConnect governing body. As part of their being licensed, they must agree with reasonable conditions relating to compliance with HealthConnect policies, maintaining confidentiality and security of 117 HealthConnect Business Architecture v1.9 HealthConnect information, support of HealthConnect, technical protocols and standards and their relationships with consumers on behalf of HealthConnect. 8.11 Provider Registration and Management At the national level, the HealthConnect governing body has responsibility for establishing and enforcing appropriate policies and procedures for managing the relationship with participating providers, including rules for provider registration and for deregistration of providers from HealthConnect. The HealthConnect governing body also has responsibility for national awareness of HealthConnect and for marketing the program to providers (as well as to consumers and to the community at large). A provider’s registration with HealthConnect will be subject to the provider having entered into a legal agreement with the HealthConnect governing body which will set out the obligations of the provider and set out the basis both for the provider’s use of HealthConnect and the protection of consumer privacy. The roles of a provider organisation and as an individual provider are different, in particular: · Access to HealthConnect for retrieval and/or update of EHR information is only granted to registered provider organisations (even though, in many cases, this will be a one-person practice or business entity employing one or two staff). · Each entry submitted by a provider organisation for inclusion in a consumer’s HealthConnect EHR must be attributable to an individual provider registered with HealthConnect. HealthConnect will provide a simple, integrated registration process for small practices. It is required that each person accessing HealthConnect EHR information be uniquely identifiable. Support staff and junior clinicians who are not registered as individual providers may be authorised by a provider organisation, providing that the provider organisation uniquely identifies them and gives undertakings relating to their use of HealthConnect information. Provider organisations will need to agree to retaining a record of the identification of authorised staff. There are plans at the national level for providers to be registered in a single national provider directory/index. Efficiencies could be achieved if the HealthConnect provider registration could be facilitated by this directory. In the short- to medium-term and depending on the scope of the national provider directory, HealthConnect will need to maintain its own information on providers, to track their HealthConnect status and to efficiently manage their HealthConnect access privileges. Where a provider is entered on the proposed national provider directory, their national health provider identifier will be used to uniquely identify them to HealthConnect. Given the existing relationship between many healthcare providers and the Health Insurance Commission (HIC) through Medicare and with the States/Territories through licensing and professional registration, it is anticipated that processes for recruitment, 118 HealthConnect Business Architecture v1.9 identification and registration of providers will involve liaison with both HIC and State/Territory health authorities. It is proposed that the HealthConnect governing body establish a single integrated process for provider registration, but may appoint HIC and/or a small number of other provider registration agents (eg. state professional registration boards) to run the process on its behalf. To implement this approach, all provider registration agents would require access to appropriate facilities (including the ability to access the registration application). Although HIC is well placed to provide HealthConnect provider registration services; this would be subject to resolution of jurisdictional issues and an agreement between HIC and the HealthConnect governing body. The provider registration and management role must be supported by business processes to establish and maintain provider registration, including: (a) Market HealthConnect to providers (b) Register individual provider with HealthConnect (c) Register provider organisation with HealthConnect (d) Maintain provider registration details (e) Process deregistration of individual provider from HealthConnect (f) Process deregistration of provider organisation from HealthConnect The process of registering an individual provider or provider organisation with HealthConnect includes: (a) confirming (where relevant) an individual provider’s existing Medicare provider number, a provider organisation’s practice identifier and all providers’ National Provider Directory entries (if and when available); (b) capturing the provider’s details – contact details (including email address), additional security information to facilitate access, and profile for electronic exchange of information; (c) obtaining the provider’s consent for any publication of directory information to facilitate contact; (d) for a provider organisation, agreement to additional terms relating to access and use of HealthConnect information; ABN; responsible practice manager; (e) providing or capturing a security code for accessing/authorising HealthConnect information; and (f) entering the provider’s identifier, details and eHealth contact addresses into the HealthConnect Provider Directory. In addition to registered authorised providers, a provider organisation may authorise other staff to access HealthConnect on its behalf. The information that a provider 119 HealthConnect Business Architecture v1.9 organisation should retain in relation to those staff which are authorised to access HealthConnect should include: (a) the training program and agreements under which a staff member is authorised to access HealthConnect (which comply with any HealthConnect rules in this regard); (b) the individual identifier by which the person will be uniquely identified when accessing HealthConnect information; (c) the person's full name, title/role, and contact details within the organisation; and (d) the date of authorisation and the officer who approved the authorisation. The processes involved in establishing and maintaining registration of provider organisations and individual providers need to be supported by the HealthConnect registration application system. This application should be accessible by the HealthConnect registration centre and all HealthConnect provider registration agencies. Once a provider is registered with HealthConnect, their registration details can be maintained by online access, by personal contact with a HealthConnect provider registration agency or by telephone to the national HealthConnect registration centre. In all cases, the provider must provide one of the forms of identification normally required for access to HealthConnect. Where a provider has lost or mislaid their HealthConnect identification details or password/PIN, they would contact the HealthConnect registration centre so that the access could be reset, using other identifying information held in the HealthConnect registration system. Because access control is tied to provider organisation and some larger private and public health services have complex structures that change from time to time, the facility must exist within HealthConnect to have some provider organisations (eg individual hospitals) also being part of a larger provider organisation (eg a regional hospital group) to several levels of nesting. Administrative processes and systems functions will also be required to re-establish the status of organisational units and their responsibilities when provider organisations merge, split or change hands. 8.12 Provider eHealth Access Services The primary role of Provider eHealth Access Services (PeHAS) is to give providers effective means of accessing HealthConnect services and any front line support needed to help them in using HealthConnect. Processes identified as being potentially associated with delivery of eHealth access services include: (a) Provide HealthConnect access portal and message handling service (for providers accessing HealthConnect via both clinical information systems and web browsers); (b) Provide advice, assistance and training to HealthConnect providers using or starting to use HealthConnect; 120 HealthConnect Business Architecture v1.9 (c) Provide eHealth telephone and web-based support service to resolve HealthConnect access and usage problems; (d) Provide access to eHealth message bank service and facilities that support secure transmission of eHealth messages (including prescriptions, referrals and notifications) between providers; (e) Provide access to value-added services, potentially including supply of health information and clinical decision support services, HealthConnectcompliant clinical information systems, and associated consulting and advisory services; (f) Assisting to market HealthConnect to providers and facilitate provider registration; (g) Monitoring and reporting performance indicators on services delivered to providers; and (h) Assisting to market HealthConnect to providers and facilitating provider registration. Depending on decisions taken by the HealthConnect governing body, this business architecture does not restrict the organisations that can perform an PeHAS role; however, providers will be encouraged to access HealthConnect and submit event summaries through clinical information systems, interchanging information with HealthConnect via web-based access portals running the HealthConnect message handling applications, which are expected to including some portals operated and supported by independent organisations performing the PeHAS role. A HealthConnect web portal running a simple provider front-end application, will be available for web-browser access by providers and for simple administrative functions, such as updating registration details. Organisations possibly able to offer PeHAS capabilities include: · Organisations offering value-added services to providers, including vendors of health information services, clinical information systems and secure communications services; · State/Territory health departments, private hospital groups, or the larger nursing services who have the capability to offer this service to themselves, their own employees and associated private practitioners; · Peak bodies representing large groups of providers; · Organisations already providing electronic business services to large groups of health providers (eg. billing or supply services); and · Any service used to support a regional implementation of HealthConnect. Those operating a PeHAS facility would have access to the Consumer Index, the full Provider Directory, and the HealthConnect message handling and transport applications. It is most important that PeHAS facilities support standard HealthConnect interface protocols for accessing HRS and national HealthConnect services. To ensure that confidentiality of consumer personal information and the security of the HealthConnect 121 HealthConnect Business Architecture v1.9 ICT infrastructure are preserved, all PeHAS operators must be licensed by the HealthConnect governing body. As part of their being licensed, they must agree with reasonable conditions relating to compliance with HealthConnect policies, maintaining confidentiality and security of HealthConnect information, support of HealthConnect, technical protocols and standards and their relationships with providers on behalf of HealthConnect. 8.13 eHealth Message Bank Service The eHealth message bank service is an adjunct to the HealthConnect message handling and transport application. It provides facilities needed to receive, hold and forward eHealth messages being transmitted between participating providers for purposes such as electronic prescriptions, electronic referrals, and electronic notifications and, potentially, a range of other health-to-health and business-to-business transactions. The eHealth Message Bank Service role is to be developed in conjunctions with HealthConnect, and is needed to provide essential HealthConnect functions so it may have the full range of required functionality. In particular, there is a requirement for HealthConnect to be able to accept, hold and forward prescriptions in electronic form in order to incorporate functionality previously provided by the MediConnect system. If this functionality is provided purely within HealthConnect (and it could be) it would only be available for handling communication relating to consumers and providers participating in HealthConnect. Whereas the requirement for eHealth communication between providers is much wider and applies, whether a particular message contains information about a consumer participating in HealthConnect or not. This business architecture has therefore proposed that the eHealth Message Bank Service be specified as a separate component, to be developed in conjunction with HealthConnect. It is too early in the development of the eHealth messaging concept to define the organisation or organisations likely to provide the service or the supporting technologies. However, various proprietary services supporting various forms of health-to-health messaging need to be taken into account by developers of HealthConnect as they progress the development of the eHealth message bank concept. 8.14 Value Added eHealth Services Value Added eHealth Services encompass any service or function (including supply of an application system or product) that complements the use of HealthConnect and gives consumers, individual providers or provider organisations added value from participating in HealthConnect. Potential examples of value added eHealth services include: (a) Access to health information repositories and online knowledge bases containing reference information; (b) New online clinical decision support tools and applications that might emerge (with a capacity to use EHR information, such as that held in HealthConnect); 122 HealthConnect Business Architecture v1.9 (c) Consumer health information systems - allowing a consumer to monitor their general health and progress in managing specific conditions (particularly if the system can produce or use EHR information); (d) Health maintenance programs involving periodic personal recording of progress in maintaining or improving healthcare parameters; (e) Clinical Information Systems and applications specifically configured to make use of HealthConnect EHR information; and (f) Access to health transaction processing services - for handling provider billing or booking transactions. Adherence to mainstream international and global standards for the representation of EHR information is one of the key enablers for expanding the availability and use of value added eHealth services in conjunction with HealthConnect. 8.15 National Health InfoStructure National health infostructure work is being progressed to service a number of national priorities, including HealthConnect, but is not part of the HealthConnect program. The following areas of this work are of particular relevance to HealthConnect: (a) A proposed national health identifier (b) National health metadata repositories (c) National health data sets (d) Health information standards, terminologies and data sets (e) A proposed national provider directory 8.15.1 National Health Identifier Proposals for the introduction of a National Health Identifier (NHI) are currently being prepared for presentation to Australian health ministers and it is expected that over the coming years, consumers will be issued with a national health identifier that will uniquely identify them for several healthcare initiatives, including HealthConnect. The national consumer identification service is expected to include a client (consumer) master index linked to the consumer-held smartcard, which is available to replace the current Medicare magnetic stripe card. If approved by the ministers, and with appropriate regulatory backing, this initiative has the potential to impact on HealthConnect in the following ways: (a) It provides a unique identifier, usable for health applications, which can be checked to avoid duplicate registration of individual consumers within HealthConnect; (b) It provides a unique identification token, in the form of the smartcard, on which the healthcare identifier can be stored and which can be used by 123 HealthConnect Business Architecture v1.9 the consumer to identify themself and to facilitate the access to their HealthConnect information. (c) If developed in consultation with HealthConnect, the indexes supporting the National Health Identifier may be able to replace the HealthConnect consumer index. The entities that might provide such a service, or indeed the nature of the service itself, are matters to be determined as part of a major review to be completed by the end of 2004. 8.15.2 National Health Provider Directory Further investigation of a National Health Provider Directory (NHPD) is one of the high-priority initiatives currently being progressed for presentation to Australian health ministers and it is expected that it will provide the basis for providers being uniquely identified for several healthcare initiatives, including HealthConnect. If approved by the ministers, and with appropriate regulatory backing, this initiative has the potential to impact on HealthConnect in the following ways: (a) It provides a unique identifier, usable for health applications, which can be checked to avoid duplicate registration of individual providers within HealthConnect; (and depending on the scope of the NHPD may also avoid duplication of identifiers for provider organisations). (b) If developed in consultation with HealthConnect, indexes supporting the National Health Provider Directory may be able to replace the HealthConnect provider directory. How such a national service might be provided, and whether it is worthwhile, are matters to be determined as part of a major review to be completed by early 2005. 8.15.3 National Health Metadata Repositories To achieve its objectives, HealthConnect needs to collect and produce information in the most meaningful way, without imposing overheads on those who must supply the information. Given that HealthConnect is a recipient of EHR data from a wide range of sources, it is important that it is supported by national standards. For a long time, many organisations have been defining how health information is to be collected for use in health applications. These organisations include: the Australian Institute of Health and Welfare (AIHW), the Australian and state departments of health, specialised registries for clinical research and planning (such as cancer registries) and, more recently, the Clinical Information Project. In May 2004, the National Health Information Management and Information and Communications Technology Strategy prepared by Boston Consulting Group for the National Health Information Group (NHIG) and Australian Health Information Council (AHIC) identified over 70 groups developing health information standards and requirements across the entire spectrum of national, state, government, not-for-profit and private-sector areas. 124 HealthConnect Business Architecture v1.9 Well formed metadata supports the effective use of information by ensuring that it is properly defined by reference to an appropriate ontology and terminologies, structured by reference to information models (compiled with input from the subject domain) and is expressed in a format and using values that can be readily interpreted. It will be one of the tasks of the HealthConnect governing body to identify and promulgate the metadata that is to be used in collecting, processing and retrieving information for HealthConnect – and, more specifically, HealthConnect EHR information. Wherever possible, metadata selected for use with HealthConnect should conform to appropriate international, global and national standards to minimise the cost and maximise the potential for clinical systems to interoperate with HealthConnect. As an extension its ongoing role in maintaining the National Health Data Dictionary (NHDD), AIHW have released a specification for a new automated National Health Metadata Repository (to be called METeOR) supported by contemporary information management tools. The NHDD is also being extended to include an increasing array of clinical data items, which will be added to METeOR as they are developed. In consultation with stakeholders, the Clinical Information Project is developing the information models and defining the information structure and content of event summaries, lists and views to provide HealthConnect with well-formed metadata. This work is proceeding in collaboration with AIHW, the National InfoStructure Development Section and the HealthConnect Program Office and, as the outputs are endorsed by relevant authorities (currently the National Data Standards Committee – NDSC - on behalf of the Australian Health Ministers’ Council), it is proposed they become available as electronically interpretable XML specifications on METeOR. While all these developments are expected to influence HealthConnect strongly, HealthConnect will also need to accept a range of material in a recognised form not necessarily conforming to approved metadata registered in the national health metadata repository. HealthConnect also has a responsibility to ensure the long-term retention and availability of any metadata used to define EHR information stored in the HealthConnect EHR repository. In these key respects, the requirements of HealthConnect metadata repository may diverge from those of the national health metadata repository. Nevertheless, HealthConnect should ensure that the techniques it uses for metadata representation are harmonised with those used by the CIP and the National health metadata repository to allow speedy comparisons, automated processing and information sharing. As HealthConnect is developed, consideration also should be given to whether METeOR (or a derivative subsystem) can become the HealthConnect Metadata Repository. 8.15.4 Health Information Standards, Terminologies and Data Sets Without agreement on appropriate standards for representation and use of information, effective interchange and interpretation of information is not possible. It is therefore important that the development of HealthConnect be strongly guided by the substantial work currently being undertaken to identify and establish Health Information Standards, 125 HealthConnect Business Architecture v1.9 Terminologies and Data Sets. The specific factors bearing on HealthConnect in this regard include: (a) The national health standards agenda – establishing standards for the representation and interchange of EHR information; (b) Adoption and implementation of a standard terminology (or combination of terminologies ) for representation and coding of clinical concepts so that they can be unambiguously interpreted by automated clinical systems (including HealthConnect); and (c) Programs to establish and maintain key national data sets of clinically relevant information that will support accurate representation of clinical information and enhance the potential for interoperability. HealthConnect will follow and adopt the results of these national health infostructure programs and also make substantial contributions to their development, so as to ensure that they are informed by and can support HealthConnect’s own requirements. Specific initiatives of particular relevance to HealthConnect include: · Development of the Australian Catalogue of Medicines (ACoM) and a standard terminology for medications and medical devices; · Development of standard notifications for allergies and alerts and adverse reactions; · Australian input to CEN and HL7 standards development programs aimed at harmonisations of international standards for representation of EHR information; and · Formalisation of Australian Standards for implementation of HL7 messages, discharge summary and referrals. Where code sets are used to represent information submitted in event summaries, it is important that the update of these code sets be controlled with each new release being retained for the long term, so as to enable HealthConnect EHR information to be interpreted long into the future. 8.16 Supporting ICT Infrastructure Being engaged in the collaborative electronic sharing of information across the Australian health community, HealthConnect will interact with ICT infrastructure supplied, owned, operated and supported by a wide variety of organisations. Key ICT infrastructure elements identified as being required for the success of HealthConnect (in addition to the core HealthConnect applications) include: (a) Secure Communications Networks – maintaining a high level of open access, good response times, and effective security protection for messages flowing across interconnected networks supplied by different providers represents a significant challenge. 126 HealthConnect Business Architecture v1.9 (b) Clinical Applications – end-user applications are typically supplied by independent vendors selling to groups of providers - these must be maintained to comply with HealthConnect interface standards to effectively interchange EHR information with HealthConnect. (c) Processing Platforms - the very scale of HealthConnect represents a significant challenge to its ability to acquire, configure and manage underlying processing technologies for the long term. (d) Clinical Information System Support – the cooperation of suppliers of networking, applications and technology services, which is essential to achieving the other elements of the required ICT infrastructure. The success of HealthConnect will therefore not only depend on those elements which are under the direct influence of the HealthConnect governing body, but also on its ability to manage its interoperation with other systems and organisations. The technology components supporting core HealthConnect activities are discussed further in section 11 of this business architecture. 127 HealthConnect 9. Business Architecture v1.9 Information Components 9.1 Introduction This section identifies, classifies and discusses the information objects that are involved in the future delivery of HealthConnect and considers the relationship of these objects to each other. This task has been approached with a degree of formality with a view to informing the subsequent development of the HealthConnect Data Architecture. The following are the information objects discussed in this section: · HealthConnect EHR Repository: - HealthConnect Electronic Health Record (EHR) - HealthConnect National Data Store · HealthConnect Event Summary · EHR Views · EHR Lists · EHR Query/Response · HealthConnect Notifications · Consumer Details · Access Control List · EHR Access Logs and Audit Trails · HealthConnect Reports · HealthConnect Consumers and Providers - HealthConnect Consumer Index - HealthConnect Provider Directory · HealthConnect Metadata · HealthConnect Registration Objects · National Information Repositories · eHealth Communications Messages Note Descriptions of each of the above components and associated requirements are being developed as part of this business architecture in conjunction with the preparation of a detailed statement of business functional requirements. This section 9 will be progressively updated to reflect the results of this work as it becomes available. 128 HealthConnect Business Architecture v1.9 9.2 HealthConnect EHR Repository HealthConnect is designed to be capable of operation as a federated system in which the entire EHR for each consumer is held on one of a number of HealthConnect records systems (HRS), but is accessible by any health provider participating in HealthConnect anywhere in Australia. Each HRS also provides EHR extracts to the HealthConnect national data store (NDS) to allow reporting on a national basis. The HealthConnect EHR repository is therefore the sum total of the EHR information held in: · All Electronic Health Records held in HealthConnect records systems; and · The HealthConnect national data store. The information content of these objects and the associated processing is discussed below. 9.3 HealthConnect Electronic Health Record (EHR) The following definition of the term EHR (Electronic Health Record) is commonly used within HealthConnect and is taken from The National Electronic Health Records Taskforce report: “An electronic, longitudinal collection of personal health information, usually based on the individual, entered or accepted by health care providers, which can be distributed over a number of sites or aggregated at a particular source. The information is organised primarily to support continuing, efficient and quality health care. The record is under the control of the consumer and is stored and transmitted securely.” In HealthConnect, each EHR is a longitudinal collection of health information relating to a single consumer that is stored within the HealthConnect system itself. The logical contents of a HealthConnect EHR include: · Consumer identifier; · Consumer data – key demographic data about the consumer, including date of birth, sex, contact details, next of kin etc; · Access Control List, which identifies the providers which the consumer has allowed to access the EHR – associated with this is the option for authorised providers to request notification when specific types of event summary arrive for processing into the EHR; · A long-term collection of all Event Summaries incorporated into the EHR, each containing information received from points of care (eg. a GP surgery or hospital), typically providing salient information about one or more care event; · EHR Views –commonly referenced, clinically meaningful aggregations of EHR information drawn from one or more event summaries (eg. the “critical view” which shows problems, alerts and medications, care plan summary, or a microbiology sensitivity report); · EHR Lists –commonly referenced sets of similar clinically meaningful data items selected from the EHR, e.g. “active problems”, “current medications”, “therapeutic precautions”, “cumulative laboratory report”; and 129 HealthConnect · Business Architecture v1.9 EHR Version Log, Access Log and Audit Trail, which are logically part of each consumer EHR but may be implemented as part of a different physical database to the EHR itself. The structure and content of EHR components are to be formally expressed and maintained in HealthConnect metadata. An appropriate and consistent range of messages will also need to be defined for submission of event summaries (and other information such as consumer details) to HealthConnect Records System (HRS) nodes and for EHR query/response sequences to retrieve EHR information from them. 9.4 The CEN EHR Reference Information Model Following considerable international collaboration to secure convergence between those working on the European CEN standards and those working on US-based HL7 EHR standards, there is now substantial agreement as to what constitutes the reference model for an “EHR Extract” (or portion of an EHR that may be communicated between EHR systems). Figure 9.1 illustrates the broad structure of this converging EHR reference model. EHR Extract -Versioning -Consumer Demographics -Access Control List 1 1 Core EHR Extract Objects * * 1 1 1 Composition * Composition (Event Summary) * Folder EHR Compositions (Event Summaries) may be constrained at each of these levels by using Archetypes (CEN) or Templates (HL7) ─────────── Folder 1 * Section * * Entry * 1 Cluster 1 1 Element Optional EHR Organiser Objects * 1 Cluster Entry * * Element 1 * 1 1..* 1 Section Data Value Fig. 9.1. Simplified CEN EN 13606-1 Reference Model When applying this model, the “Composition” level is used for each discrete event summary submitted to HealthConnect (eg. a discharge summary). The observations (e.g. vital signs, a blood pressure measurement, APGAR score or pathology test result) are 130 HealthConnect Business Architecture v1.9 incorporated into the Event Summary as “Entries”. A composition may comprise a number of entries. It is a business requirement that HealthConnect have the capacity to accept, store and recognise EHR information which has been structured according to this model – including any more complex EHR event summaries which use the “optional” organiser levels (which may also be nested) and any of the many Data Value constructs. While localised EHR implementations are working towards support of a more restricted model (eg. for HealthConnect trials or EHR feeder applications), HealthConnect itself, as a national EHR system must support the converging EHR reference model fully. The object models used to fully describe the CEN 13606 and HL7 CDA reference models are quite complex and undergoing change as convergence progresses. At this time, the most developed, tested and definitive version of the converging EHR reference model is Part 1 of the draft CEN EN13606 EHR messaging standard. This Part is expected to be published as a full European standard by early 2005 and has been translated into a draft DMIM for use in the HL7 v3 messaging and CDA environment. Part 1 of the CEN EN13606 EHR messaging standard has therefore been selected as a starting point for defining the content of event summaries, recognising that HealthConnect must consider extensions and potential simplifications when using the model to structure the HealthConnect EHR and its components. This should not be misinterpreted as a requirement that all data submitted to HealthConnect must originally be structured according to this model, but all event summaries specifically developed for acceptance of structured information into HealthConnect will be developed by constraining this model. 9.5 HealthConnect National Data Store The HealthConnect National Data Store will hold archival copies of HealthConnect EHR information in a format complying with standard HealthConnect metadata to facilitate searching and the production of reports. Information held in the National Data Store will replicate information contained in, and received from, each HRS/AEM as EHR extracts - rather than being a reconstruction of the EHR from basic transactions. The HealthConnect data architecture and on-going metadata definitions will need to define the specific content of EHR material being supplied to the NDS and allow for both complete copies of each new version of an EHR and incremental updates of specific material (planned for later versions of HealthConnect). For this update process to succeed, all HRS implementations will need to be able to produce replicated EHR material in accordance with the appropriate HealthConnect standards, even if they themselves do not use these standards internally. EHR material provided by an HRS for incorporation into the National Data Store conforms to the CEN EN 13606 notion of an EHR Extract and, therefore, this standard is probably the most appropriate to apply to the transfer of this material. 131 HealthConnect Business Architecture v1.9 9.6 HealthConnect Event Summary The HealthConnect EHR will be largely made up of event summaries, which are central to the concept of HealthConnect. An event summary has been defined in the following terms: “Health information about one or more healthcare event(s), that is relevant to the ongoing care of a consumer/patient. The collection of health event summaries relating to a consumer/patient will constitute their (HealthConnect) shared EHR. Health event summaries define inputs to HealthConnect”.16 The intention is that an event summary should present a provider’s summary of key details relevant to the ongoing care of the consumer and would normally be produced at or near the end of a clinical encounter and at an appropriate level of detail to inform other providers involved in the current episode of care. Nevertheless, all separately attributed information headed for storage in the consumer’s HealthConnect EHR must be presented as an “event summary” and HealthConnect will need to be able to handle a wide range of inputs from a very simple observation through to complex clinical reports all within the paradigm of an event summary. For each event summary supplied to HealthConnect, the following information components are required: · The identity of the consumer (via the HealthConnect identifier); · The identity of the individual provider to whom the event summary is attributed (in line with the identification requirements of the National Provider Directory); · The identity of the provider organisation (in line with provider organisation’s registration details); · Other event summary header information, including the type of event summary, the date and time of the consultation and the date and time of submission to HealthConnect; and · The data elements or sections that make up the event summary in line with CIP event summary definitions. The Clinical Information Project (CIP) has been given the responsibility for researching, designing and recommending the information content and structure of HealthConnect event summaries. As a result of CIP Phase 1 and 2 work, prototypes of the following priority event summaries have been designed to capture information expected to be commonly exchanged in HealthConnect settings: 16 · Initial Health Profile (which captures a person's EHR information on initial enrolment with an EHR system and may need to be compiled from several sources); · GP Consultation; · Hospital Discharge Summary; · Diagnostic Imaging (report); and Clinical Information Project, Phase 1 Overview Report, March 2004 132 HealthConnect · Business Architecture v1.9 Pathology Test (report). Work on stage 1 has indicated that they will require a range of other event summaries not yet on the CIP work program, these include specific event summary formats for events arising in the following areas: · Pharmacy; · Clinical specialties; and · ATSI health. All HealthConnect implementations must support event summaries as they are developed and adopted by the HealthConnect governing body. The structure and content of each event summary is to be formally expressed and maintained in HealthConnect metadata. An appropriate and consistent range of messages will also need to be defined for submission of event summaries. Clinical Observations Within an event summary, each separate clinical observation (or set of observations) is represented as a “component” (usually at the level of an “Entry”), whose purpose, structure and content may be defined as HealthConnect metadata (such as by an archetype constraint on the Entry, Compound and/or Data Value classes of the EN 13606-1 reference information model). An overriding objective in constructing metadata for HealthConnect components (and archetypes in general) is to ensure that any clinical observation or concept is consistently represented using the same metadata in different types of event summaries so that HealthConnect can identify and relate the same types of information when found in different contexts. For example, considering the five prototype event summaries designed by CIP, a pathology test result may occur in an initial health profile, GP consultation, hospital discharge summary or (clearly) a pathology report – it is important that this result be characterised in the same way in each of these contexts to enable proper management and comparability of information. Other re-usable (or “spanning” components include medication prescriptions and dispensing; vital signs; care plans and health outcomes). Those working on archetypes have had a long-standing interest in the efficient specification and grouping of reusable EHR components, but a similar concept has also been more recently progressed through work in the HL7 community on “clinical statements”. The following specific EHR data elements were characterised by the CIP as part of its design of the five prototype HealthConnect event summaries. • Advance Directive • Adverse Reactions • Alert/Warning • Diagnostic Imaging • Family Clinical History • Functional Status, Social Circumstances • Immunisation • Lifestyle, Risk Factor • Medication • Problem / Diagnosis Presenting Complaint Reason for Encounter • Procedure/ Treatment History • Referral/ Care Team 133 HealthConnect • Discharge Summary Business Architecture v1.9 • Pathology The CIP is currently identifying further high-priority event summaries required for HealthConnect through consultations with HealthConnect trials, lead implementations and professional bodies. These priority event summaries will make up the CIP work for 2004 / 2005. Thereafter, the CIP will develop further event summaries and associated data elements in line with national priorities, including the priority requirements of HealthConnect. Structured and unstructured information in event summaries The extent to which HealthConnect should require the content of all event summaries to be structured is a topic that has been thoroughly examined through extensive consultation with stakeholders throughout this update of the HealthConnect business architecture. On one hand, there are strong arguments (backed up by cost-benefits identified in formal evaluation studies) that EHR systems only achieve significant improvements in health outcomes, where strongly structured data is used to enable applications such as clinical decision support. On the other hand, many feeder systems are not currently in a position to collect and deliver any significant amount of well-structured information to HealthConnect for quite some time. It has also been found that clinicians are more willing to participate, if there is an option of starting with relatively simple information, including free text entries. Based on these considerations, the following principles have been adopted: 1. HealthConnect should strongly encourage the submission of EHR information in a structured form that allows interpretation by automated systems. 2. HealthConnect event summaries should be progressively designed to encompass all common clinical statements in structured form. 3. Event summaries capable of being used with minimally structured content (eg. free text) or content expressed in a structure alien to HealthConnect must also be available but should not be used where a more structured event summary is available. 4. HealthConnect should require all medication lists, alerts and diagnoses/problems to be submitted in a structured form. 5. The level of structure in event summaries should be increased as terminologies, code sets and archetypes are developed for use with HealthConnect. Consumer-supplied HealthConnect event summaries Supporting consumer access and the ability of consumers to contribute to their own HealthConnect records has long been an important goal of HealthConnect. However, while stage 1 of HealthConnect will support consumer access, consumers will not initially be able to supply consumer event summaries for incorporation into the HealthConnect EHR until the associated medico-legal issues have been resolved. Nevertheless, stage 1 is required to be designed with capability for consumers to supply consumer event summaries for inclusion in their HealthConnect EHR. 134 HealthConnect Business Architecture v1.9 9.7 EHR Views From the viewpoint of the HealthConnect system, all information retrieved from the event summaries in a consumer’s EHR (other than for secondary uses) will be delivered as an EHR view, which may be defined as: “A pre-defined set of data items selected from the EHR, processed and returned in response to an EHR request”.17 The term “EHR view” can also be applied to the visual presentation of material received from HealthConnect in response to a user request. However, this presentation will normally be determined by the functionality and configuration of the application system used by each user, rather than by HealthConnect itself. Nevertheless, HealthConnect must anticipate and include functions that support the users’ interactions with EHR views delivered from HealthConnect. All EHR views will be defined by, and structured in accordance with, HealthConnect metadata. When a user issues a request for EHR information relating to a consumer (by means of an EHR query), the relevant HRS application will process the request and will return a response in the form of an EHR view containing the required information. For the present, HealthConnect will only support the retrieval of pre-defined (but parameterised) EHR views to ensure systems responsiveness and retain greater control over the clinical integrity of the responses provided. This contrasts with the approach whereby HealthConnect would offer users the ability to retrieve EHR information via more generalised ad-hoc query language. From a practical perspective in implementing HealthConnect, the CIP has identified the following advantages of pre-specifying standard EHR views: · It allows for prioritising the data sets that need to be specified; · Agreement can be reached on what data should be supplied, and therefore which health event summaries are needed to supply the information; and · Vendors of existing systems can be given a smaller set of specifications to incorporate into their systems. On the basis of CIP consultations to date, two priority views have been identified: · The Primary (or ‘Critical’) View; and · The Health Profile View. The Primary View is the first view delivered when a provider gains access to a consumer’s EHR. The information contained within the view is that considered to be the most critical and will contain links to EHR lists and other EHR views. In due course, a number of different primary views may evolve to serve the needs of different provider groups (eg. dispensing pharmacists, GPs, specialists, community nurses, emergency departments). 17 Clinical Information Project. Phase 2 Report: Part A – Clinical Information Framework, v1.0, s7.1. 135 HealthConnect Business Architecture v1.9 The Health Profile View displays the information provided from the Initial Health Profile Event Summary (used to initialise HealthConnect), which is updated via subsequent health event summaries. Much of the information within EHR views will be maintained within the EHR in the form of EHR lists (see below). From a technical viewpoint, the retrieval of subsidiary information that is identified but not presented in an initial EHR view (eg. subsidiary information obtained from drilling down into the EHR or by following links in EHR lists) also needs to be defined as an EHR request, followed by provision of an EHR view. A large amount of HealthConnect metadata will be needed to define the EHR queries and matching EHR views for retrieving these lower-level EHR components. Deciding what information ought to be presented in any particular EHR view is based on the needs identified by consumers and providers obtained through CIP consultation. The challenge will be to make the EHR views appropriate to the user – for example a specialist might be interested in complex disease management views, while consumer views will need to be more user-friendly. The priority EHR views will also need to maintain the integrity of the information by ensuring that important components of an EHR are always included so that information cannot be misinterpreted by being seen out of context. 9.8 EHR Lists An EHR list is a collection of similar EHR items describing a key aspect of a consumer’s health, formed to serve a specific purpose.17 An EHR List is a special form of the more general EHR View and carries with it some notion of persistence, completeness, currency, maintenance and/or order. All EHR lists will be defined by, and structured in accordance with, HealthConnect metadata. The CIP has identified two types of EHR lists: derived lists and maintained lists, which have the following characteristics. Derived EHR Lists Derived lists are those that can be automatically generated by querying all relevant event summaries. For efficiency reasons, it might be preferable for HealthConnect to build derived lists as the event summaries are entered, rather than to query a substantial amount of data to build the list dynamically at the time that it is requested. A derived list is the EHR view that results by running a predefined query against a consumer’s EHR information in accordance with parameters supplied as part of the query. Typically such lists will be constrained by some time window, (e.g. prescribing history or recent events) but may also be constrained in other ways (such as by test type for a pathology result list). 136 HealthConnect Business Architecture v1.9 Work by the CIP included the following as potential derived EHR lists: · Prescribing and dispensing history (a generated list of prescriptions and associated dispensing events); · Procedure/treatment History (a generated list of treatments or procedures); and · Recent Health Events (a generated list from recent event summaries). Maintained EHR Lists A “maintained list” is an EHR list maintained by a process of review and update by providers having knowledge of the consumer’s condition and treatment (see section 6.3.4). Even though the maintenance of such lists might be assisted by a high degree of automation, the ultimate decision on their content requires an element of clinical judgement or contemporary information, which is not readily available to automated processes operating within an HRS application. Typically, the maintenance of such a list might involve clinical judgement as to: · Whether an entry in the list is valid (e.g. "Is depression still an active problem for this patient?") · Whether an entry is still significant, or whether it can be removed in order to increase the relevance and reduce the size of the list (e.g. is a 10-year old X-ray to determine fracture of the femur of a patient aged 12 still a “significant investigation”?); or · In some cases, whether a new item of information is sufficiently significant to be added to the list. (eg. whether an acquisition of OTC Panadol to treat the symptoms of a minor headache needs to be added as “current medication”). Based on the above definitions, the CIP has identified the following as being maintained EHR lists: • Current Medications • Active Problems/Diagnoses • Adverse reactions • Warnings • Recent and/or Significant Tests and Investigations • Immunisations • Inactive Significant Problems/Diagnoses. It is an important characteristic that, when a maintained EHR list is updated, the updated version is the one used to produce any subsequent EHR view that contains the list. In this respect, the maintained EHR list differs from an event summary, each one of which persists in its own right as part of the current EHR. It should also be noted that a maintained EHR list may be retrieved and viewed by a user without it being updated. 9.9 EHR Query/Response Providers and consumers will access HealthConnect EHR information through applications that will interact with HealthConnect, by sending EHR queries to 137 HealthConnect Business Architecture v1.9 HealthConnect and receiving the HealthConnect responses in the form of EHR views (which include information provided as EHR lists). All such applications, whether they be a provider’s clinical information system or a web-based front-end application running in a HealthConnect access portal will use standards-based query/response messaging to interact with the HRS node on which the consumer's EHR is held. It is anticipated that many broad classes of EHR query (and associated EHR views in response) will be required to support interaction between normal users and HealthConnect. These include: (a) Initial EHR query to establish a user’s access to an EHR. If the user is authorised to access the consumer record, the initial EHR query should result in the allocation of an end-to-end HealthConnect session identifier. The provider nominated primary/critical view will be delivered to the user, from which the user may drill down to more detailed information in that consumer’s EHR. (b) An EHR query to enable retrieval of the EHR views predefined to support particular clinical functions. (c) Parameterised EHR queries to support selection and retrieval of each type of EHR component, including each type of event summary (by time/data, type or both) and each type of entry-level and event-level component (in context). (d) Parameterised EHR queries to support selection, retrieval and aggregation/summarisation of information contained in EHR lists. (e) An EHR query that will enable information specified via secure links in a previous EHR view to be efficiently retrieved from the HRS. (f) A category of EHR queries which retrieve trend data and measures (averages, maxima, minima, totals, counts etc) drawn from relatively small amounts of data from potentially large numbers of event summaries, entries and/or elements within an EHR. (g) A category of EHR queries (and potentially query/update transactions) that operate on information held in a consumer’s EHR other than that held in event summaries – such as consumer details, access log or audit trail. The structure and content of each EHR query and responses is to be formally expressed and maintained in HealthConnect metadata. An appropriate and consistent range of messages will also need to be defined for communication of both queries and responses. The HL7 v2.x request for patient clinical information (event I05 RQC/RCI) and request/receipt of clinical data listing (event I06 RQC/RCL) and/or v3 Find Act Reference Registry Entry Messages provide possible messaging frameworks for this purpose. 138 HealthConnect Business Architecture v1.9 9.10 HealthConnect Notifications The CIP defines notifications as: “a type of message or ‘flag’ sent between applications, users or systems to communicate about important occurrences – usually specified in terms of a condition or set of conditions that when satisfied, triggers a pre-defined response.” Two types of notifications have been identified for stage 1 of HealthConnect: · Provider Notifications regarding key consumer healthcare events including hospital admissions and discharges and emergency department presentations. These HealthConnect notifications are generated at the HRS when triggers maintained in the notification list within the consumer’s EHR are activated by an incoming event summary. Each provider with access to the EHR may set notification triggers, which will remain active for so long as the provider continues to have access (or until the provider de-activates them). When the consumer removes a provider’s access to the EHR, the triggers are retained (along with the provider details) but are de-activated. If the provider’s access is restored, the notification list is also restored. · Electronic lodgement of registry notifications. As a by product of processing certain specific types of event summary, official registries and data repositories such as births, deaths and notifiable disease registers may be approved to receive notifications from HealthConnect. The business rules for generating these registry notifications will primarily support statutory notifications and will be applied outside the context of an individual consumer EHR. The information content of a notification may include: a) the consumer’s HealthConnect identifier; b) the consumer’s name, date of birth and sex; c) the recipient’s HealthConnect identifier or other addressing details known to HealthConnect; and d) the type and details of the notification (for example, admission details, discharge details, emergency presentation details or birth notifications). 9.11 Consumer Details Once a consumer has been registered and their EHR has been allocated to an HRS, the consumer will be able to maintain many of their own consumer details by accessing the EHR or by asking an approved provider to make the changes on their behalf. The consumer details accessible as part of the consumer’s EHR are those which would be required in establishing practice records or for admission to a healthcare institution, including (to the extent provided by/for the consumer): (a) current HealthConnect name; 139 HealthConnect Business Architecture v1.9 (b) date of birth (fixed from registration); (c) sex (fixed from registration); (d) current address and contact details; (e) demographic information - ethnicity, language, religion, place of birth, ATSI status etc; (f) Medicare number; (g) National Health Identifier (fixed from registration) (h) next of kin with contact details; (i) previous address and contact details; (j) previous name(s) and aliases; (k) details of any consumer agent(s) (for example, parents, guardian, powers of attorney or informal carer); and (l) a list of other healthcare services and identifiers (eg private health insurer, state UPI number). In addition to being held in the EHR, a copy of this information, along with security information needed to re-establish lost identity is also to be maintained in a secure zone within the consumer’s entry in the HealthConnect consumer index, and maintained by the HealthConnect registration application. Consumers and providers have access to, and may update, the consumer details in the EHR but it is not intended that individual consumers or providers have access to the HealthConnect registration application, which will only be available to the HealthConnect registration centre and to licensed HealthConnect consumer registration agencies. Because some (but not all) consumer details will be accessible via the EHR and, also, held in the consumer index, the maintenance of consumer details will need to be carefully synchronised between HRS nodes and the registration system. This will include: (a) The registration application both loading initial consumer details to the restricted zone of the consumer index and passing them to the HRS when the consumer first registers with HealthConnect; (b) The registration application providing updated consumer details to both the consumer index and to the HRS when the consumer updates their details through a HealthConnect consumer registration agency; and (c) A means for consumer details in the registration application and the EHR to be updated simultaneously, when changes are made online by the consumer (or an authorised provider with access to the EHR). Some key identification details are normally fixed at registration and may not be changed by the consumer (or their agent) or by a provider other than by the consumer making special application to the HealthConnect registration centre; these include date 140 HealthConnect Business Architecture v1.9 of birth, sex, and national health identifier and the security information the consumer provides to assist in re-establishing their access in the event that they lose their HealthConnect security code. 9.12 Access Control List A key aspect of the consent process is the identification of provider organisations authorised to access the consumer’s HealthConnect record. It is expected that these provider organisations would generally be those routinely or potentially involved in the consumer’s care. The consumer access control list identifies the provider organisations that the consumer has authorised to access their EHR from time to time. The information to be retained in the consumer access control list includes: (a) the identities and HealthConnect identifiers of those provider organisations to which the consumer grants access; and (b) the person and means by which each grant and removal of access was made and the date/time at which each such event occurred. Whenever a provider organisation is displayed to the consumer or to HealthConnect agencies, the name, role and contact details of the provider organisation should also be provided. By changing entries in their access control list, consumers will be able to change their HealthConnect access control arrangements in line with their changing healthcare needs; for example, changing the general practitioner practice or adding specialist groups to their list. When the consumer removes a provider’s access to the EHR, the provider’s details and any notification list are retained but access is suspended. Providing consumers can identify themselves to HealthConnect, they may grant, review or reinstate a provider’s access at any time by using online access facilities, or through a HealthConnect consumer registration agency or at a HealthConnect provider’s premises. If they have lost their identification, they may obtain access by obtaining a temporary access code by identifying themselves to the HealthConnect registration centre. 9.13 EHR Access Logs and Audit Trails Access logs detail individual access to EHR records (including emergency override access) by providers, consumers, HealthConnect registration agencies and HealthConnect system administration functions. The EHR access log is to be available to the consumer for review at any time and is to be automatically updated by the HRS application whenever the EHR is accessed. Information to be recorded on the EHR access log and audit trail includes: (a) a unique sequence number for all transactions (including accesses); (b) the date and time of transaction/access; 141 HealthConnect Business Architecture v1.9 (c) a unique identifier for the person (and the identity of any individual provider) and, where relevant, the provider organisation from which the access was performed; (d) for EHR inputs: (e) (1) identification of the type of information inserted into the EHR including the type and version of any event summary; (2) the complete event summary transaction (including header information) for each and every event summary received by the HRS; and (3) the event summary status indicator for each event summary, indicating whether the event summary is a new event summary or a replacement event summary; and for EHR outputs (including notifications): (1) identification of the type of information retrieved from the EHR including the type and version of any query, view or trigger event and any query parameters; and (2) the complete output transaction (for example, the view, the list, the HealthConnect notification or the individual event summary); All changes to the consumer’s EHR data must be versioned and retained on the audit trail in such a way that previous versions of EHR information can be accessed. 9.14 HealthConnect Reports HealthConnect reports provide a view of EHR information aggregated across a collection of EHRs within the HealthConnect EHR repository. Reports will also be available to extract detailed information and metadata from individual EHR records to assist in analysing problems in the processing of HealthConnect EHR data. The principal function of the HealthConnect report will be to support secondary uses including various forms of approved research, and the management and technical development of HealthConnect. It is proposed that population-based reporting and aggregated reports across large numbers of consumers’ EHR take place using the HealthConnect national data store, rather than the EHR information held at operational HRS nodes. A formal query language informed by HealthConnect metadata will be needed to allow reports to be generated in response to report requests and this will need to be supported by tools that provide the means of parsing HealthConnect report queries and of, extracting, analysing, processing and compiling report information. HealthConnect reporting might also include: · Providing search-engine functionality to retrieve filtered lists of EHR entries, selected on a combination of metadata and content and processed to provide consolidated information derived from the records identified; and · Any query on populations of patients, including queries addressing either clinical (e.g. find all patients having a correlation between several characteristics) 142 HealthConnect Business Architecture v1.9 or administrative (find patients who have not received a certain recall for a given time) parameters. Access to these functions will be restricted with the HealthConnect governing body managing access and the processing of report queries (see Section 7.4.3). 9.15 HealthConnect Consumers and Providers Information on the principal participants involved in HealthConnect transactions – consumers and providers - is maintained by the registration application on: · The HealthConnect Consumer Index; · The HealthConnect Provider Directory. The information content of these objects and the associated processing is discussed below. 9.15.1 HealthConnect Consumer Index The HealthConnect consumer registration application sets up consumer index entries from information provided when the consumer registers with HealthConnect. Selected parts of the consumer’s personal information may subsequently be maintained by the consumer via online interaction with HealthConnect itself or a HealthConnect consumer registration agency. The main function of the HealthConnect Consumer Index is to direct HealthConnect transactions to the HRS on which the consumer’s EHR and other information is held. Once a transaction arrives at the relevant HRS, the HRS has responsible for controlling access, using the access control list supplied by the consumer. The information components associated with the HealthConnect Consumer Index include: · a unique HealthConnect consumer identifier; · the HRS on which the consumer’s EHR information is being held; · consumer PIN and/or password details in a secure form, And the following information in a more restricted, secure environment, not generally accessible to front-end applications or users: · potentially, the proposed national health identifier as unique identification; · consumer personal details including name, date-of-birth, sex, address, telephone and other contact details; · other information needed by an authorised helpdesk operator to help re-establish the consumer’s identity and access privileges, if the consumer loses their HealthConnect identifier or their password/PIN. 143 HealthConnect Business Architecture v1.9 The Consumer Index will hold sufficient information in secure form to enable a frontend application or HRS to confirm that the HealthConnect identifier matches the consumer’s password/PIN. The Consumer’s HealthConnect identifier, secure access key, summary identification information and linkage information will be available for replication so that relevant index entries may be held locally for faster access by those organisations licensed by the HealthConnect governing body to deliver HealthConnect access services. 9.15.2 HealthConnect Provider Directory The HealthConnect provider registration application sets up provider directory entries from information supplied when an individual provider or provider organisation registers with HealthConnect. Selected parts of the provider’s details may subsequently be maintained via online interaction with HealthConnect itself or via a provider service line at the HealthConnect registration centre. The information components of a provider directory for HealthConnect are likely to include: · unique identifiers for individual providers and provider organisations - linked to the provider’s existing Medicare provider number (where relevant), and/or National Provider Directory entry (if and when available) ; · the type of provider organisations (for example, individual practitioner, GP practice, public or private hospital, community pharmacy, aged-care facility); · an individual provider’s full name, title, role and clinical speciality (for example, General Practitioner, specialist, other medical practitioner, pharmacist, podiatrist); · the provider’s professional registration number(s) and professional registration body (or bodies); · records of agreement to additional terms relating to access and use of HealthConnect information; ABN; responsible practice manager; · additional security information to facilitate access; · the provider’s primary contact details, including address, phone, email, eHealth communications details and HeSA key; and · for provider organisations, the nominated contact person (for example, hospital administrator, GP practice manager or specialist’s receptionist) for receipt of HealthConnect related information. 9.16 HealthConnect Metadata All information used in HealthConnect, such as event summaries, views and lists must be defined in the form of metadata, which is to be retained indefinitely in the HealthConnect metadata repository. This metadata must be sufficiently extensible and 144 HealthConnect Business Architecture v1.9 flexible to accommodate changes in clinical practices and yet also needs to be available in many years time for reviewing and using contemporary information. HealthConnect metadata defines both the syntax and semantics of event summaries, EHR views, EHR lists and EHR queries by specifying some or all of: the structure, optionality, rules, conditions, bindings/relationships and value ranges applicable to these EHR components. These metadata resources are the key to HRS applications being interoperable with source systems and each other, as well as being adaptable and therefore economic in the long term. It can reasonably be expected that such metadata will need to accommodate emerging terminologies, vocabularies, templates and archetypes. HealthConnect metadata must therefore be extensible – that is, it must allow data definitions to change over time, without invalidating information already collected. Once developed, metadata can be rendered in different forms for distribution and application. The exact form of HealthConnect metadata has yet to be finalised but the use of archetypes to constrain an information model based on the CEN EN 13606-1 reference information model is considered the most likely approach. Metadata that CIP will deliver as specifications of event summaries, EHR views and EHR lists is proposed to comprise: · a standardised written specification based on ISO/IEC 11179; · a metadata definitions for registration and dissemination by the HealthConnect governing body (using a form of XML representation); and · usage notes to highlight potential data quality, implementation or other issues. Proposed principles for HealthConnect metadata include: 1. Archetypes, expressed in an appropriate XML syntax, should be used to represent HealthConnect metadata. 2. All HealthConnect metadata should be defined in both machine-readable and human-readable form and in accordance with the ISO 11179 standard. 3. HealthConnect must have a governance process for quality assurance and to oversee compliance of HealthConnect metadata. 4. Archetypes may be defined using languages such as ADL, OWL, RDF(2) and tools are becoming available to transform archetypes between representations. 5. While XML Schema Definition (XSD) may not be sufficiently comprehensive or structured to define and interpret HealthConnect metadata, archetypes may still be communicated as XML documents. 6. EHR views, EHR lists and EHR queries at any future point in time are likely to encounter data created under older metadata, hence backward compatibility of metadata (and also definitions of previous versions) need to be maintained. 7. EHR components must be tagged with the version of metadata they were created under and HealthConnect applications will require the flexibility to merge data 145 HealthConnect Business Architecture v1.9 from a number of versions of metadata in adding to an EHR or when forming a list or view. 8. 9.17 Incremental updating of metadata is needed, particularly in the case of large terminologies, should they be adopted in Australia. HealthConnect Registration Objects The processes of consumer registration and provider registration that will be carried out by the HealthConnect registration applications will involve a range of subsidiary registration objects required to maintain the HealthConnect consumer index and the HealthConnect provider directory. In addition to information contained in basic registration transactions, the registration application will manage the following types of information objects: (a) updates to consumer details including contact details, changed business parameters, voluntary and enforced deregistration; (b) audit trails and logs of all accesses and transactions processed by the registration application; (c) confidential questions used to assist in identifying consumers and providers and temporary access codes issued to allow an authorised user temporary access to an EHR; and (d) details of registration with professional registration boards in various jurisdictions including any change in status (particularly, suspension or cancellations of registration). 9.18 National Information Repositories HealthConnect business processes will make substantial use of national health infostructure now being developed. The following areas of this work are of particular relevance to HealthConnect: (a) A proposed national health identifier, which may provide a universally recognised unique health identifier for consumers that will underpin and may even replace the unique HealthConnect consumer identifier. (b) National health metadata repositories being established by the AIHW under the oversight of the inter-governmental National Data Standards Committee. (c) National health data sets – in particular the Australian Catalogue of Medicines (ACoM) (d) Health information standards and terminologies; (e) A proposed national provider directory, which may provide a universally recognised unique health provider identifier that may even replace the unique HealthConnect provider identifier. 146 HealthConnect Business Architecture v1.9 As these national infostructure components come to fruition, HealthConnect will harness these resources to assist with the identification of consumers and providers and to enhance the semantic interoperability of HealthConnect and supporting applications. Further information on the role and impact of each of these elements of the national health infostructure is provided in section 8.14. 9.19 eHealth Communication Messages The eHealth message bank service provides facilities needed to receive, hold and forward eHealth messages being transmitted between participating providers for purposes such as electronic prescriptions, electronic referrals, electronic notifications and, potentially, a range of other health-to-health (H2H) and B2B transactions. The information content for these messages is still being addressed, but is expected to include the following broad categories of information: · The provider organisation and/or individual provider from which the message originated; · The identity of the consumer (via the HealthConnect identifier); · The HealthConnect (or national provider directory) identifier for the receiving provider; · The type of eHealth communication message; · The message body – containing the clinical comments and information; and · Associated event summary header information. 147 HealthConnect Business Architecture v1.9 10. HealthConnect Business Processes 10.1 High Level Business Process Context The following process map illustrates the high-level groups of business processes associated with the delivery of HealthConnect: Secondary User A. Administer HealthConnect Programs Provider B. Manage HealthConnect Participation Consumer Consumer Registrations G. Access HealthConnect as a Consumer Provider Registration D. Establish & Maintain Provider Registration C. Establish & Maintain Consumer Registration E. Use HealthConnect Information for Health Service Delivery I. Provide HRS/AEM Services Consumer Transactions H. Deliver Consumer Access to HealthConnect J. Respond to EHR Information Request K. Process Event Summary into EHR F. Deliver Provider Access to HealthConnect L. Establish/Operate HealthConnect Infrastructure HealthConnect Processes Metadata Repository National Data Store Audit Trails Consumer Index Provider Directory Networks & Systems Provider Transactions eHealth Message Bank M. Maintain National Health Infostructure > Health Information Standards, Terminologies & Data Sets (eg ACOM) > National EHR Metadata > National Health Identifier Service > National Health Provider Directory/Index Figure 10.1 HealthConnect Process Map The process map identifies 13 aggregated process groups, which may be further broken down into processes, sub-processes and tasks. In many cases, execution of these processes involves participation by different entities and interaction between roles and it is the identification and management of such interactions which is necessary to have an effective design and implementation of HealthConnect. A. Administer HealthConnect programs B. Manage HealthConnect participation C. Establish and maintain consumer registration D. Establish and maintain provider registration E. Use HealthConnect information for health service delivery F. Deliver provider access to HealthConnect G. Access HealthConnect as a consumer H. Deliver consumer access to HealthConnect I. Provide HRS/AEM services J. Respond to EHR information request K. Process event summary into EHR L. Establish and operate HealthConnect infrastructure 148 HealthConnect M. Business Architecture v1.9 Maintain national health infostructure Within these high-level process groups, over 80 business processes were identified, which are addressed in more detail in the business requirements document produced as part of this business architecture. 149 HealthConnect 10.2 Business Architecture v1.9 Major Business Processes The following table shows the break-down of the aggregated process groups into the major business processes required for the development and operation of HealthConnect. 150 HealthConnect A. Administer HealthConnect programs Administer HealthConnect programs A1 Establish HealthConnect operational policies and standards Business Architecture v1.9 B. Manage HealthConnect participation B1 Promote community awareness of HealthConnect B2 Engage with stakeholder bodies A2 Establish arrangements for coordinated national delivery of HealthConnect B3 Contract with health providers for use of HealthConnect A3 Procure HealthConnect systems and infrastructure B4 Agree HealthConnect supply terms for consumers A4 Licence HealthConnect consumer access and provider eHealth access services B5 Handle applications for secondary use of HealthConnect data B6 Administer access to HealthConnect B7 Monitor access and audit/report usage B8 Handle consumer and provider complaints B9 Coordinate HealthConnect records management functions 151 HealthConnect Business Architecture v1.9 C. Establish and maintain consumer registration D. Establish and maintain provider registration C1 Market HealthConnect to consumers D1 Market HealthConnect to providers C2 Register consumer with HealthConnect D2 C3 Update/recover consumer registration details Register individual provider with HealthConnect C4 Process consumer deregistration from HealthConnect D3 Register provider organisation with HealthConnect C5 Manage tracking of consumer surrogates D4 Maintain provider registration details D5 Process deregistration of individual provider from HealthConnect D6 Process deregistration of provider organisation from HealthConnect F. Deliver provider access to HealthConnect F1 Provide HealthConnect access portal and message handling F2 Provide advice, assistance and training to HealthConnect providers E. Use HealthConnect information for health service delivery E1 Identify consenting consumer to HealthConnect E2 Retrieve/use consumer EHR information E3 Update consumer EHR information F3 Provide eHealth support service E4 Send/receive eHealth communication F4 E5 Access value-added services Provide access to eHealth message bank service E6 Seek HealthConnect support assistance F5 Provide access to added-value services F6 Monitor and report service delivery performance indicators F7 Assist to market HealthConnect to providers & facilitate provider registration H. Deliver consumer access to HealthConnect H1 Provide HealthConnect consumer access portal H2 Provide advice, assistance and training to HealthConnect consumers G5 Access value-added services H3 Provide consumer support service G6 Seek HealthConnect support assistance H4 Assist with marketing HealthConnect to consumers H5 Facilitate consumer registration H6 Provide consumer access to added-value services H7 Monitor and report service delivery performance indicators G. Access HealthConnect as a consumer G1 Maintain consumer access control list G2 Maintain consumer registration information G3 Retrieve/use EHR Information G4 Update/Annotate EHR information G7 Check access log 152 HealthConnect Business Architecture v1.9 I Provide HRS/AEM services J. Respond to EHR information request I1 Manage HRS databases and audit trails J1 Validate EHR information request I2 Apply updates to consumer details and access control lists J2 Provide EHR View/List I3 Control access to EHR information J3 Process EHR Query/Response I4 Update/maintain HRS Application software J4 Produce EHR Report J5 Maintain access log I5 Maintain compatibility with HealthConnect metadata I6 Maintain HRS processing platform and network environment K. Process event summary into EHR K1 Validate incoming event summary I7 Apply and monitor ICT security measures K2 Update EHR I8 Monitor and report service delivery performance indicators K3 Maintain audit trail and NDS L. Establish and operate HealthConnect infrastructure M. Maintain national health infostructure L1 Maintain National Data Store L2 Maintain HealthConnect Metadata Repository M2 Develop and maintain national health metadata repository L3 Maintain HealthConnect Consumer Index M3 Implement health information standards L4 Maintain HealthConnect Provider Directory M4 Provide standard terminologies and data sets L5 Manage HealthConnect ICT infrastructure L6 Promulgate metadata and standards for HealthConnect M5 Provide national Health Provider Directory service L7 Run HealthConnect operations L8 Organise clinical systems to inter-operate with HealthConnect M1 Provide National Health Identifier Service Descriptions of each of the above process groups, processes and, where relevant, associated sub-processes are contained in the attachment to this business architecture entitled Specification of HealthConnect Business Requirements. 153 HealthConnect Business Architecture v1.9 11. Technology Components This section provides an overview of the systems and subsystems which interoperate to provide HealthConnect functionality. While the overall technology framework and relationships between the individual parts of the HealthConnect solution should remain relatively constant, more specific requirements will evolve through further detailed design and from experience gained through stage 1. 11.1 Systems Overview National Health Metadata Repository National Health Terminologies etc National HealthConnect Applications ─────────────────────────── NDS Maintenance & Reporting HealthConnect Metadata Maintenance HealthConnect Administrative Applications Secondary User HealthConnect National Data Store (& Audit Trail Index) HRS ─────────────────── HRS Access Control EHR Input Validation & Update EHR Information Retrieval Maintain Consumer Access List Maintain Audit trails Provide NDS Information Messaging Interface HealthConnect Metadata Repository National Health Identifier Service (NHI) National Health Provider Directory HealthConnect Registration Applications ───────────────── Consumer Registration Provider Registration HealthConnect Registration Operatons HealthConnect Consumer Index EHR Repository HealthConnect Provider Directory eHealth Message Bank Application HealthConnect Message Handling & Transport Clinical Information System Web Browser HealthConnect Provider/Consumer Access Portals eHealth Transmission Service (ETS) Consumer Health Information System HCCAS Operations Web Browser PeHAS Operations Provider Consumer Figure 11.1 HealthConnect Systems Overview The core function of HealthConnect is the processing of EHR event summaries and query transactions, which is to be carried out by a federation of HealthConnect Records Systems (HRS) that maintain the primary HealthConnect EHR repository. 154 HealthConnect Business Architecture v1.9 The operating environment of HealthConnect is illustrated in Figure 11.1. To exchange information with HealthConnect users, each HRS interacts with HealthConnect-enabled user applications via a common HealthConnect message handling and transport system. HRS services are the centrepiece of HealthConnect, controlling access to the consumer’s EHR information and managing the input, validation, storage, retrieval and delivery of this information in accordance with HealthConnect processing rules. The HRS also maintains consumer details, an access control list and an audit trail of all access to each EHR. Each HRS is to regularly forward copies of EHR information and logs of audit trail accesses, to the HealthConnect National Data Store for archival storage and approved secondary uses. These core components of HealthConnect are all to be securely interconnected by an eHealth Transmission Service, which is also required to support other applications, such as storage and delivery of electronic prescriptions and referrals. A provider may use a clinical information system to interact with HealthConnect (provided that the clinical information system is HealthConnect-enabled) or, alternatively, may use a web browser to interact with HealthConnect via a provider access portal running a provider front-end application. Consumers will typically use a web browser to access HealthConnect via a consumer access portal running a consumer front-end application. Alternatively, it is expected that consumers may eventually be able to acquire HealthConnect-enabled consumer health information systems that will allow them to interact with HealthConnect via the message handling and transport system. All communications between an HRS and user applications are conveyed as messages via the message handling and transport system that manages communications between HealthConnect and external participants using standard HealthConnect message protocols. It is expected that the message handling and transport system will also be federated across several providers, such as those supplying HRS services, HealthConnect consumer access services, provider eHealth access services and/or value-added health information services. The message handling and transport system and HRS services will rely on the HealthConnect consumer index and HealthConnect provider directory for information needed to identify HealthConnect users and to route messages to and from the appropriate HRS and other application components in the federated HealthConnect environment. The HealthConnect consumer registration application sets up consumer index entries from information provided when the consumer registers with HealthConnect (with the possibility of including identification provided through the proposed national health identifier). Selected parts of the consumer’s personal information may subsequently be maintained by the consumer via online interaction with HealthConnect itself or a HealthConnect consumer registration agency. The HealthConnect consumer index allows HealthConnect applications to use the consumer’s unique HealthConnect identifier to find and access the HRS on which the consumer’s EHR is held. 155 HealthConnect Business Architecture v1.9 A copy of parts of the consumer’s information, necessary for ensuring accurate identification of the consumer eg name, is held on the consumer index for use in managing HealthConnect but should not be made available to external applications using the index. Up-to-date consumer demographic information will be available as part of each EHR and becomes available to those users authorised to access the consumer’s EHR, thereby enabling them to check the identity of a consumer before retrieving further EHR information or updating the EHR. The HealthConnect provider registration application maintains the HealthConnect provider directory based on information set up when a provider registers with HealthConnect (with the possibility of including identification and other information provided through the proposed national health provider directory). Selected parts of the provider’s information may subsequently be maintained by the provider via online interaction with HealthConnect itself or the HealthConnect provider registration agency. Parts of the HealthConnect provider directory are generally accessible to all providers and contain electronic contact details that permit HealthConnect messages to be addressed and delivered to the provider (via a proposed eHealth message bank application). The registration applications are to log all transactions in an audit trail, which is to be archived indefinitely. The HealthConnect registration applications, consumer index and provider directory are proposed as national HealthConnect infrastructure available to: · each HRS; · each consumer registration agency; · those organisations responsible for registering providers; and · the HealthConnect registration centre. Nevertheless, until these national HealthConnect registration components are fully operational, trials and lead-state implementations may proceed with local registration initiatives, with a view to their early integration into the national HealthConnect infrastructure. A HealthConnect Operations Centre should have responsibility for the ongoing management of registration functions in order to ensure the registration process functions effectively on behalf of the HealthConnect governing body and to perform more sensitive functions, such as maintaining consumer identification parameters, periodic reviews, de-registration and enabling of suspended registrations and setting up short-term access to an EHR based on telephone identification. The structure and content of HealthConnect EHR information is defined by HealthConnect metadata, which will be used by the HRS services, national data store, message handling and transport system and clinical information system interfaces to format and exchange EHR information. All versions of HealthConnect metadata that are actually promulgated and used for the formation and storage of HealthConnect EHR information must be retained indefinitely to allow future interpretation of the EHR information. 156 HealthConnect Business Architecture v1.9 The national data store, which is discussed in more depth in sections 8 and 9, is a national repository of all the EHR information held across all the HRS services retained in a perpetual archive and available to support reporting and other approved secondary uses, including research to improve health care and health care delivery. A consolidated access log is also to be maintained as part of the national data store data collections. If the proposed national health identifier and national provider directory are established and when the national health metadata repository, Australian Catalogue of Medicines (ACoM) and clinical terminologies and code sets become available, it is proposed that HealthConnect and its component applications will access these resources to assist with the identification of consumers and providers and to enhance the semantic interoperability of HealthConnect and supporting applications. Security of consumer information and of HealthConnect facilities and services is an important part of the HealthConnect operational infrastructure and is the subject of further analysis in this section, as are the requirements for appropriate interface and messaging technologies. Note Descriptions of the operation and functions of each of the above components are further developed in a separate attachment to this business architecture entitled Specification of HealthConnect Business Requirements. 157 HealthConnect Business Architecture v1.9 Part E – Managing and Implementing HealthConnect 159 HealthConnect Business Architecture v1.9 The previous sections of the Business Architecture have concentrated on defining the principles of HealthConnect, explaining how it would work for the different types of participants and defining the components of HealthConnect. Part E addresses governance, legal and implementation issues associated with realising HealthConnect. These important topics have been the subject of major research initiatives in their own right and detailed reports have been produced in parallel with the development of the Business Architecture. These reports have already been circulated for review under separate cover. The purpose of this section is not to duplicate the findings contained in these related reports, rather to link them back to the Business Architecture. The focus will be on indicating how the recommendations support the realisation of HealthConnect, highlighting key issues necessary for progress to be achieved. 12. Managing HealthConnect This section addresses issues relating to the key aspects of managing HealthConnect namely governance structure, privacy issues and legal issues. 12.1 HealthConnect Governance Structure 12.1.1 The Governance Approach Details of the proposed governance structure for HealthConnect are being finalised in parallel with the documentation of this business architecture. Given that the model for delivering HealthConnect may change over time, the governance arrangements need to have the capacity to change, while at the same time, ensuring that the HealthConnect functions and operations remain accountable to Australian, state and territory governments and the public. It is proposed that the ongoing management of the HealthConnect program at the national level be vested in a dedicated organisational entity on behalf of all the participating governments and other stakeholders. This organisational entity is commonly referred to as the HealthConnect governing body. The functions which this governing body would be expected to cover include: overseeing the implementation and operation of HealthConnect, providing clinical governance, maintaining approval mechanisms to assess requests for secondary uses of HealthConnect data, overseeing registration process for both consumers and providers, determining the rules and standards applicable to HealthConnect activities, establishing contractual and licensing arrangements with various HealthConnect participants and suppliers, and monitoring of compliance throughout the network. In the short term, the governance arrangements of the project implementation activities will be based on the current HealthConnect Board, Steering Committee and Advisory Group arrangements. 161 HealthConnect Business Architecture v1.9 HealthConnect is also being progressed regionally through staged HealthConnect state/territory implementations and the ongoing HealthConnect trials. Each of these initiatives currently has its own governance structure, which encompasses many of the same functions at a local/regional level as are proposed to be carried out by the HealthConnect governing body a national level. For the short- to medium-term some of the HealthConnect management functions will be performed at a regional level. 12.1.2 Ongoing Management Governance Structure The key elements of the ongoing management structure are presented below. More detailed descriptions of the key roles are presented in Part D – HealthConnect Components. The HealthConnect Governing Body The centralised HealthConnect governing body will be established to manage HealthConnect. The Clayton Utz Legal Issues Report has explored a number of structuring alternatives including establishing the governing body as: a departmental function without establishing an executive agency, a company, an executive agency, a statutory authority, or an unincorporated joint venture. These alternatives are currently being reviewed. As stated in Part D in the HealthConnect Context and Roles Section, the HealthConnect governance role may be encapsulated by three high-level functions. · · · Administration of HealthConnect programs, including: - Establish HealthConnect operational policies and standards - Establish arrangements for coordinated national delivery of HealthConnect - Procure HealthConnect systems and infrastructure - License HealthConnect consumer support and eHealth access service providers - Evaluate HealthConnect outcomes. Management of HealthConnect participation including: - Promote community awareness of HealthConnect - Engage with stakeholder bodies - Contract with health providers for use of HealthConnect - Agree HealthConnect supply terms for consumers - Manage approval and monitoring of secondary uses - Administer access to HealthConnect - Monitor access and audit/report usage - Handle consumer and provider complaints. Establishment and operation of HealthConnect infrastructure including: - Promulgate metadata and standards for HealthConnect 162 HealthConnect Business Architecture v1.9 - Maintain National Data Store - Maintain HealthConnect Metadata Repository - Maintain HealthConnect Consumer Index - Maintain HealthConnect Provider Directory - Manage HealthConnect ICT infrastructure - Run HealthConnect operations - Organise clinical systems to inter-operate with HealthConnect. Operational Structure and Support While the HealthConnect governing body will have overall responsibility for HealthConnect operations, many of the routine HealthConnect operational activities will be performed by other organisations contracted to perform them on behalf of HealthConnect. These might include: · Registering and managing consumer and provider participation – A number of HealthConnect Registration Agencies may be contracted to perform front line registration functions. There will also be a requirement for a HealthConnect Registration Centre operating at a national level to set policy and oversee the registration process; · Maintaining the HealthConnect EHR repository; including the individual Health Record Systems and the National Data Store – Approved EHR Managers will be contracted to run the HRS; and · Governing the interaction with HealthConnect - HealthConnect Consumer Access Services will be contracted to support customer interaction with HealthConnect; and Provider eHealth Access Services will be contracted to support providers interacting with HealthConnect. 12.1.3 Project Implementation Governance Structure The key elements of the current governance structure which is overseeing the design and implementation of HealthConnect are presented below. The HealthConnect Board The HealthConnect Board reports to the Australian Health Ministers’ Advisory Council (AHMAC) through the National Health Information Group (NHIG). The Board has the responsibility to: · Oversee the formulation of policy related to the design, development, implementation and evaluation of HealthConnect; · Provide advice to AHMAC on the alignment of Australian, State and Territory Government electronic health records projects within a national architecture; · Monitor the operation and progress of HealthConnect and recommend policy and operational changes. 163 HealthConnect Business Architecture v1.9 Expert Advisory Groups A number of expert advisory groups will be appointed to advise the Board and Steering Committee and, in the future, the HealthConnect governing body on issues that arise in the implementation of HealthConnect and to provide a link with the locally-based implementation activities. The expert advisory groups will maintain this important stakeholder participation. In the first instance these will be: · Clinical Advisory Group - Clinical input into the HealthConnect implementation will be critical to its success. This group will provide expert advice on clinical matters and the effective collection, storage and retrieval of clinical information. Members will also advise on structural, organisational and workforce changes necessary for the implementation of HealthConnect. · Architecture Advisory Group - The Architectural Advisory Group (AAG) will advise on technical aspects of data and systems architecture. This will complement the work of the Clinical Advisory Group (CAG), which will be addressing business process issues associated with the design and implementation of HealthConnect. · Evaluation Advisory Group - The Evaluation Advisory Group (EAG) will provide advice to the HealthConnect Board on processes for evaluating and monitoring HealthConnect implementation. As implementation progresses it is anticipated that other advisory groups may be required. This might include a privacy and access control advisory group to provide input on issues such as establishing and monitoring privacy protocols, defining consent options and rules; approval of research requests. This Group could fulfil the requirements for the independent and transparent monitoring of the role of HealthConnect in authorising and managing access to information for secondary uses. Ensuring overall operation of HealthConnect, monitoring usage and handling complaints will be part of the core HealthConnect governing body role. Regional Implementation Governance While the HealthConnect governing body will have the overall responsibility for the implementation and operation of HealthConnect from a national perspective, the Stage 1 state/territory and trial implementations of HealthConnect will have local governance structures. Key characteristics of these structures will include establishment of: · Local steering committees to make decisions on the scope and priorities of the local implementation. The committees will also be responsible for reporting to the HealthConnect governing body/steering committee to ensure compliance and consistency of implementations; · Local advisory groups such as a clinical group to make decisions relevant to the local implementation, within the framework established by the HealthConnect governing body and its advisory groups; · Support for collaborative partnerships between local stakeholders, public and private organisations; 164 HealthConnect Business Architecture v1.9 · “Champions” who will represent the interests of their clinical area and to assist in the local promotion of HealthConnect; and · Any local Registration Agencies, Approved EHR Managers, HealthConnect Consumer Access Services Operators or Provider eHealth Access Services Operators, as required. Until the HealthConnect governing body and its operational support arrangements are fully active, similar operational functions will be needed locally to support Stage 1 HealthConnect implementations. Longer-term integration of these functions into the national program will need to be considered by the HealthConnect governing body and the relevant jurisdictions. 12.1.4 National eHealth Transition Authority For HealthConnect to be successful it must take into consideration the wider e-health agendas and the bodies responsible for their management. The Australian Health Information Council (AHIC) and the National Health Information Group (NHIG), to which the HealthConnect Board reports, are jointly developing a national IM&ICT strategy due to be completed at the end of 2004. Ministers have endorsed the establishment of the National eHealth Transition Authority (NEHTA) to drive the national priorities over the next 12 months. The longer term strategy will then be determined, potentially including the establishment of an independent legal entity. NEHTA has established a work program focussing on the national priority areas of clinical data standards, identification standards, consumer and provider directories, supply chain procurement standards, consent models, secure messaging and information transfer, and technical integration standards. These initiatives will support the future development and implementation of HealthConnect. The HealthConnect Board has endorsed the establishment of a process to achieve alignment between HealthConnect needs and the NEHTA work program. 12.2 HealthConnect Privacy Issues 12.2.1 Need for Strict Privacy Control The success of HealthConnect will depend on consumers, providers and provider organisations having confidence and trust that health information is kept confidential and secure. To this end, a robust privacy framework, together with strong security measures, is required. Personal health information is particularly sensitive information. Inappropriate handling of such information can lead to serious consequences to the individual such as being socially ostracised, being personally embarrassed or having difficulty gaining employment. While consumers generally have a high level of trust in the way in which their health care providers maintain confidentiality, the capacity of electronic health record systems to quickly assemble, store and transfer information beyond organisational boundaries naturally raises privacy concerns. 165 HealthConnect Business Architecture v1.9 These concerns are evident in the research undertaken to date on consumer and provider attitudes to electronic health record initiatives. While consumers and providers can readily see the benefits of electronic health records, privacy and security issues are consistently of most concern. For HealthConnect to be successful, the privacy concerns of consumers need to be adequately addressed. The results of stakeholder consultations in relation to HealthConnect likewise support these findings. Key concerns raised include the potential for: · the use of information by third parties that act against the interests of the individual concerned (eg employers and insurers); · personal sensitivities or embarrassment if health information is accessed inappropriately; · potential harm to an individual if information is accessed by someone who poses a threat to that person (eg domestic violence); and · information being used for other purposes that are not for the health benefit of the person involved (eg unacceptable commercial use of data). Therefore, before HealthConnect can proceed on a national scale, both providers and consumers would need to have a strong sense of trust that their health information would be adequately protected and that only those who ‘need-to-know’ can access their records. While security and confidentiality are essential prerequisites, the ability for consumers to have access to information held about them and to be able to maintain control over how their information is used and to whom it is disclosed are also fundamental aspects of health information privacy within HealthConnect. 12.2.2 Existing Privacy Frameworks The privacy framework under which health records are currently treated consists of several sets of legislation and rules. The Australian Government public sector is regulated by the Information Privacy Principles18 which are provided by the Privacy Act 1988. The private health sector is covered by the National Privacy Principles19 within the Privacy Act 1988. To aid the private health sector to meet their obligations under this Act the Federal Privacy Commissioner has developed the Guidelines on Privacy in the Private Health Sector. Victoria, New South Wales and the Australian Capital Territory currently have health specific privacy legislation. Western Australia is developing health specific legislation. South Australia, Tasmania and Queensland have administrative arrangements in place which govern the privacy rules of health information. This creates different privacy requirements within the current health system – divided both by the sector (public versus private) and by the State or Territory in which that health service is provided. 18 19 For the Commonwealth public sector only For the private sector only 166 HealthConnect Business Architecture v1.9 To overcome this lack of consistency, the National Health Privacy Code (NHPC) is being developed by the Australian Health Ministers’ Advisory Council (AHMAC) National Health Privacy Working Group. Additional policy rules and/or legislation to deal with specific privacy issues relating to HealthConnect may need to be developed. 12.2.3 HealthConnect Privacy Framework In the absence of a national privacy framework, HealthConnect specific privacy arrangements have been developed based upon the National Privacy Principles and the proposed National Health Privacy Code. Providers participating in HealthConnect will be obligated to abide by existing privacy legislation and by specific HealthConnect privacy protocols – including when they access and use information from consumer’s HealthConnect records, and when they add information to these records. Multi layered Approach Privacy arrangements for HealthConnect will take a multi-layered approach incorporating legislation and policy rules; technical and security measures; and organisational practices. Key elements of this multi-layered approach could include: · The National Health Privacy Code, currently under development by the AHMAC National Health Privacy Working Group; · Specific rules underpinning the establishment and operations of HealthConnect that set out primary uses of data; authority and processes by which secondary uses of data are approved; consent processes; offences, penalties and sanctions for breaches; and complaints mechanisms; · Development of a national security framework for HealthConnect which covers the functions of identification/authentication, access control mechanisms, message protection, monitoring and detection mechanisms; and audit/logging processes; and · Establishment and maintenance of organisational practices, including staff training, which ensure appropriate privacy and security standards are maintained by organisations participating in HealthConnect. Safeguards The HealthConnect framework aims to establish a range of safeguards relating to HealthConnect governance and operations and will include specific reference to: · complaints mechanisms and rights of redress; · the circumstances under which health information can be collected by HealthConnect and subsequently used and disclosed; · how individuals who misuse such information would be held liable for such actions; · HealthConnect information only being used and disclosed for agreed purposes; 167 HealthConnect Business Architecture v1.9 · how consumers can have access to their own health information held on HealthConnect and control who has access to their information and to whom it can be disclosed; and · the controls over who has access to what information and by which authorisation. Checks and Balances The HealthConnect framework will also include a range of checks and balances to be in place including: · Consumers participating in HealthConnect having a clear understanding of how their information may be used and disclosed - informed consent; · Clear lines of decision making for determining the secondary uses of HealthConnect data, including ethics approval and independent scrutiny by an expert external to the HealthConnect governance framework. 12.3 HealthConnect Legal Issues The firm of Clayton Utz has researched and prepared a report20 to provide guidance to the HealthConnect Program Office and key stakeholders on the way forward with potential legal issues identified in the research and development phase of the HealthConnect project. Legal issues raised to date include issues in relation to information privacy, security, access control, data quality (ensuring the integrity and currency of data, and the correct degree of reliance on the data), intellectual property, stakeholder liability and indemnity, and stakeholder rights and responsibilities. The Clayton Utz report has addressed these issues under the following headings: Custodianship and Controls, Information Technology and e-Commerce, Privacy and Consent, Intellectual Property, and Liability and Indemnity. This report is currently being reviewed and finalised and will be circulated under separate cover. At this stage it is understood that issues raised in the report will not necessarily require changes to the HealthConnect solution outlined in the Business Architecture; rather that they need to be managed through specific policy and process planning activities. 20 Clayton Utz HealthConnect Report, 20 August 2004 168 HealthConnect Business Architecture v1.9 13. Implementing HealthConnect 13.1 HealthConnect Implementation Approach Fujitsu has conducted research into implementation approaches required to achieve a successful national implementation of HealthConnect. The Implementation Approach21, together with the HealthConnect Benefits Realisation Framework22, and the HealthConnect Implementation Plan constitutes the HealthConnect implementation planning work. The implementation strategy recognises the need to embrace a change program across the national population base as well as to coordinate the more technical aspects of HealthConnect needed to support the changed work practices, information storage and information provision services. This section discusses how the implementation approach supports the achievement of key HealthConnect principles. 13.1.1 Implementation Drivers The HealthConnect implementation approach is benefits driven and is based on a Benefits Realisation Framework; the key features of which include: · Take up and clinical processes - high take-up rates by both providers and consumers will maximise the realisation of benefits from the implementation of HealthConnect. HealthConnect should focus on increasing the efficiency of the processes that underpin episodes of clinical care; · Information - increasing the usefulness of information to clinicians will ensure providers use the EHR; similarly focus should be on information flows between providers and among health care facilities to increase patient safety by decreasing the impact of adverse events including adverse drug events; · Governance and evaluation - implementing full cycle governance to ensure the ongoing management of the HealthConnect program. This should include an overarching economic evaluation construct to ensure the requisite data is captured to enable benefits to be identified, measured and attributable to HealthConnect in terms of health gains, cost offsets and broader social objectives; and · Population groups - initially focusing the HealthConnect registration, enrolment and communication processes on the areas where there is a high incidence of health care expenditure. In addition to the key benefits drivers, the implementation will focus on achieving high levels of provider and consumer take-up and developing core HealthConnect capabilities, particularly in relation to HealthConnect governance, systems/ infrastructure, organisation and operations. These are discussed below. 21 22 Implementation Approach, Draft for Final Review, Draft 0.18, 2 August 2004, Fujitsu HealthConnect Benefits Realisation Framework V1.0 October 2004 169 HealthConnect Business Architecture v1.9 13.1.2 Provider and Consumer Take-up Consumer Take Up HealthConnect Principles state that consumer participation in HealthConnect will be voluntary and available to all Australian citizens and residents of Australia. The implementation approach proposes that HealthConnect needs to have a focus and priority on specific target consumers that will realise the highest value clinical and social benefits. The targeting of consumers therefore needs to consider factors such as: · Degree of “sickness/wellness” – bringing the more chronically ill consumers onto HealthConnect will address directly the quality of clinical care benefits; · Type of disease and its “growth pattern” – the major types of diseases that could best utilise HealthConnect capabilities, e.g. chronic diseases; · Geographic basis – the population areas would provide opportunity for HealthConnect critical mass. The geographic catchment area must include a cohesive collection of all the key providers and other selected providers; and · Demographic basis – the age groups that could best utilise HealthConnect capabilities in the short and long term, e.g. the very young, the elderly. While this implies a focus on specific consumer groups, once HealthConnect is operational in their geographic area, any consumer may register with HealthConnect. Provider Take-up HealthConnect Principles state that participation in HealthConnect will be made available to all providers involved in the chain of health care delivery. The implementation approach highlights that a critical mass of provider enrolment needs to be achieved. The strategy for provider take-up includes targeting providers taking into consideration the consumer target group and the provider professional focus, and developing and implementing appropriate marketing approaches. For take-up to be effective: · Virtually all of the HealthConnect functionality (provider capability/ infrastructure, HealthConnect data and views) needs to be in place such that provider benefits might be achieved; · A key group of providers must participate in HealthConnect for clinical outcomes to be achieved. Initially this will include general practitioners, community pharmacists, hospital clinicians, pathologists and radiologists; and · A high take-up of consumers with ongoing health care needs and the majority of providers need to be involved to achieve provider efficiency outcomes. Thus a targeted approach that takes account of the realities of consumer and provider capabilities and also key health priority areas, driven by anticipated benefits, is necessary. In this sense, it is not so much the rate of take-up for providers that is important, but more so the mix of take-up. The goal is to be able to support the continuum of care for consumers who participate in HealthConnect. 170 HealthConnect Business Architecture v1.9 When one or two key providers caring for a consumer are not participating in HealthConnect, it is likely that essential data will be absent from their EHR. Hence the consumer’s record will be much less useful to participating providers and consumers. A key goal for provider take-up in HealthConnect is to avoid broken links in the care chain. 13.1.3 HealthConnect Capabilities Compliance For an implementation to be considered a HealthConnect implementation, it must be compliant with the HealthConnect Business Architecture. In particular it must comply with the HealthConnect Principles in Section 3 and the Specification of HealthConnect Business Requirements23 provided as a separate attachment to the Business Architecture. The implementation approach’s HealthConnect Capabilities foundation element is focused on the ability of relevant HealthConnect stakeholders to design, plan, develop and execute each of the Governance, System, Organisational and Operational aspects of HealthConnect. The HealthConnect Capabilities framework defines four specific Compliance Levels, each of them reflecting an increasing depth/breadth of coverage and the sophistication of the capabilities that would be required to deliver progressively higher degrees of HealthConnect benefits. These levels are: 1. Trial, 2. Standalone, 3. Limited National Solution (utilising common National Layer services); and 4. Full National Solution. The implementation approach recognises the reality that HealthConnect implementers are at different stages of HealthConnect compliance and that future implementers are likely implement HealthConnect to accommodate local requirements. To address this, the implementation approach supports the concept of Progressive Compliance Pathways, whereby the implementers can join HealthConnect at different level of compliance and progress through the remaining levels to reach full compliance. This concept is illustrated on the following diagram which has been extracted from the Fujitsu Report. 23 Specification of the HealthConnect Business Requirements - Attachment to the Business Architecture v1.9 (October 2004) 171 HealthConnect Business Architecture v1.9 Figure 13.1 HealthConnect Progressive Compliance Pathways Some HealthConnect implementers may travel down a path whereby they step through all levels of compliance. This would be particularly likely in the case of the stage 1 implementations. In the most likely scenario, the majority of adopters will join the HealthConnect at the compliance Level 3 and then proceed to Level 4 at some later stage. However, depending on the timing of the implementation, it would be feasible for late adopters to directly implement Level 4. 13.2 Current Implementation Activities 13.2.1 HealthConnect Version 1 The first full implementation of HealthConnect is to be termed HealthConnect version 1 and will be based on the requirements detailed in the HealthConnect Business Architecture version 2 which will be developed after version 1.9 consultation. The HealthConnect Principles contained in the Business Architecture define the current design position and is of necessity limited in scope in some areas while further research and analysis is undertaken. Areas requiring further research include access to consumer records based on provider type, introduction of more restricted ‘secure’ areas for sensitive information, and consumer contribution to their EHR. 13.2.2 Stage 1 HealthConnect Implementations The longer term implementation of HealthConnect will be based on the Business Architecture version 2 and the procurement of HealthConnect version 1. Given that the HealthConnect version 1 detailed requirements have not yet been finalised and that there are a number of issues yet to be resolved, the procurement and the subsequent development and implementation will take a number of years. 172 HealthConnect Business Architecture v1.9 HealthConnect is therefore undertaking a staged approach to implementations. The stage 1 implementations will not be extensions of the trials, though they will make use of components and lessons from the trials. These implementations will: · build on the work conducted in the trails, ensuring that key issues are resolved; · be compliant with Version 1.9 of the Business Architecture; · have a scope aligned with the needs and capabilities of the specific regions; · be established as a cooperative project between the Australian government, states and territory with shared development activities; · optionally include HealthConnect related services such as value added services (eg referrals) and eHealth message bank services, according to local priorities; and · importantly, include a migration path to HealthConnect version 1. 13.2.3 Current HealthConnect Trials The HealthConnect trials have been a significant achievement for the HealthConnect project and have been the principal means for testing the HealthConnect concept. While some of the trials are approaching the wrap up phase, others are being extended. Two longer-term HealthConnect trials have been established in Queensland in the second half of 2003. The North Queensland HealthConnect trial, which went live in December 2003, focuses on the peri-operative assessment and preparation of consumers travelling to undergo elective surgery at Townsville Hospital. This trial has now been extended for a further 12 months. The Brisbane Southside HealthConnect trial, commenced in late 2004, focuses on testing new openEHR software technology for managing health records and shared-care plans for consumers with diabetes. The New South Wales Health-e-Link initiative currently under development is also considered a HealthConnect trial. The project will test HealthConnect infrastructure in two pilot sites. The Child Health Information Network (CHIN) will operation in Greater Western Sydney and includes the Children’s Hospital at Westmead. The Chronic Disease Management System project will operation in the Hunter Valley and includes the John Hunter Hospital in Newcastle. These two pilots are expected to go live in mid2005. The Health-e-Link implementations are NSW Health pilots and as such are long term implementations. 173 HealthConnect Business Architecture v1.9 Glossary of Terms 175 HealthConnect Business Architecture v1.9 HealthConnect Business Architecture – Glossary of Terms Access control A means of ensuring that an information system such as HealthConnect can be accessed only by authorised persons and organisations in authorised ways. Access control list A list of provider organisations authorised by a consumer, or by a surrogate of a consumer, to access that consumer’s HealthConnect EHR. Access log Record of access to EHR records (including emergency override access) by healthcare providers, consumers, HealthConnect registration agencies and HealthConnect system administration functions. Access portal A computer system that provides users with a means of accessing an information system across the Internet using a web browser. Consumer access portals and provider access portals will be one means by which consumers and providers respectively may access HealthConnect functions. ACOM Australian Catalogue of Medicines A directory of all medications available in Australia organised according to a common classification scheme and linked to a terminology for medicines and medical devices. ADL Archetype Definition Language A formal language for expressing archetypes that can be used to structure and validate the content of an EHR. AEM Approved EHR Manager A public or private entity authorised by the HealthConnect governing body to provide a HealthConnect Records System (HRS) service. Agent Within HealthConnect, a person nominated by a consumer to access HealthConnect on behalf of the consumer. Also referred to as a “consumer agent” an agent is one form of consumer surrogate and would an appropriate form of arrangement to cover the authorised involvement of a consumer’s family members, friends, or carers. Aggregated data Data about more than one consumer that are grouped together where the identity of the consumers cannot reasonably be ascertained. 176 HealthConnect Business Architecture v1.9 Archetype A formal specification of the allowable structure and content of information held in an EHR system in which the specification is derived by constraining a reference information model of the EHR. The current notion of archetypes in health informatics arose out of the work of the openEHR Foundation. Archetypes are usually used to define clinical information but may be applied in other domains. Archetypes may define simple concepts such as “blood pressure” or “address” or more complex concepts such as “family history” or “microbiology result”. Attestation The process of recording responsibility for a particular unit of information, such as a provider confirming the content of an event summary prior to its transmission to HealthConnect. Audit trail A record of access and changes to information held in a computer system or database. Authentication The process by which a degree of confidence is established about the truth of an identity. In terms of computer security, the identification or verification of the eligibility of a consumer or healthcare provider to access a HealthConnect record. B2B Business to Business. Call centre A group of people processing telephone calls or other electronic communications in accordance with defined protocols and supported by computer systems. A health call centre is a call centre staffed by health professionals that may offer health advice, health assessment (triage) and health screening services. Casemix The Hospital Information, Performance Information Program (HIPIP), formerly known as Casemix, aims to improve health service delivery (in terms of cost, equity and quality) through classification and data development, as well as research, analysis and information dissemination. CCoW Clinical Context Object Workgroup (in HL7) Using a technique called “context management”, standards developed by CCOW allow information in multiple healthcare applications to be unified under the control of the user so that all of the healthcare applications are referring to the same patient, encounter or user at any point in time. CEN Comité Européen de Normalisation (European Standards Organisation) 177 HealthConnect CEN 13606 Business Architecture v1.9 The family of European Standards relating to electronic healthcare record communication, which include: (a) The European Pre-Standard (ENV), CEN ENV13606 issued in four parts between 1999 and 2000; and (b) The full European Standard (EN), CEN EN13606 Electronic Healthcare Record Interchange, now being finalised for issue in five parts: Part 1: Reference model. Part 2: Archetype interchange specification. Part 3: Reference archetypes and term lists Part 4: Security. Part 5: Exchange models. CEN EN13606-1 The European Standard, EN13606 Electronic healthcare record communication, Part 1: Reference model, which describes a reference model for EHR information as it would appear in an EHR extract (in draft form proceeding to ballot at time of writing). CIP Clinical Information Project Project group responsible for developing and recommending definitions of information content for use in HealthConnect Electronic Health Records and the national priorities for HealthConnect event summaries and views. CIS Clinical Information System A computer system designed to support healthcare providers in the delivery of healthcare. Examples include GP desktop systems, pathology laboratory systems and point of care clinical systems Clinical data repository A data store that holds and manages clinical data consolidated from a variety of sources (e.g. hospitals, clinics, etc.) Clinical decision support Systems including computer applications that assist healthcare providers to make decisions about patient care. CDA Clinical Document Architecture (in HL7) A set of HL7 standards that specify the structure of “clinical documents”. Clinical documents are attributed to authenticated authors and differ from HL7 messages in that they are designed to be persistent. CDA is a popular architecture for EHR systems. Coding The process of assigning alphanumeric or numeric symbols to convey information in accordance with an agreed classification system. 178 HealthConnect Business Architecture v1.9 Confidentiality Legal duty of individuals and organisations that receive information in confidence to respect that confidence, not to be confused with privacy. Consumer A general term used for a person who accesses or uses health services. Within HealthConnect, a ‘consumer’ or ‘participating consumer’ means a person that registers with HealthConnect as a consumer in accordance with the HealthConnect rules. Consumer access portal see access portal Consumer agent See agent. Consumer consent Agreement by an informed consumer to participate in HealthConnect or otherwise to authorise the collection or use of their personal information. Consumer health tools Services to consumers that are made available by organisations working with HealthConnect but not a service provided directly by HealthConnect eg access to knowledge bases, care management advice. Consumer index Within HealthConnect, a database holding every HealthConnect consumer identifier, links to the HRS on which a consumer’s EHR is held, consumer demographics and other information that can be used to re-establish the HealthConnect consumer identifier, and information on providers and surrogates that may access the consumer’s EHR. The HealthConnect consumer registration service is responsible for maintaining the consumer index (through the HealthConnect consumer registration system) and for making information in the consumer index available to other HealthConnect services and components including consumer registration agencies, HRS services and message handling and translation services. Consumer registration agency An organisation authorised by the HealthConnect governing body to register HealthConnect consumers in accordance with the HealthConnect rules. Consumer surrogate A person (including a body corporate or partnership) that is uniquely identified to HealthConnect for the purpose of accessing EHR information on behalf of a consumer in accordance with HealthConnect rules. Identified subclasses of consumer surrogate include consumer agents, parents (for a child), persons with powers of attorney over a consumer’s health care, guardians of the incapacitated and any others recognised by the general law as having the right to act on behalf of the consumer. De-identified data Data about a person or persons is termed ‘de-identified’ when the identity of the individual person or persons to which the data refers is not apparent, and cannot reasonably be ascertained from the data. 179 HealthConnect Business Architecture v1.9 Deregister The process by which a consumer or provider discontinues their participation in HealthConnect. When a consumer deregisters, the consumer’s record is retained but made unavailable for further access by provider organisations and the consumer; information in the record remains available for secondary use. D-MIM or DMIM Domain Message Information Model (in HL7) An information model that represents all the concepts needed to support the communications requirements of a particular domain (such as pharmacy, laboratory medicine or patient administration). eHealth Health care components delivered, enabled or supported through the use of information and communications technology. eHealth access service A facility to give healthcare providers effective means of accessing HealthConnect services and any front line support needed to help them in using HealthConnect. eHealth message bank service A facility for conveying eHealth messages between healthcare providers relating to any consumer (not only consumers registered with HealthConnect). EHR Electronic Health Record A longitudinal collection of personal health information about a consumer, stored electronically. HealthConnect is Australia’s implementation of a national EHR. EHR Extract The unit of communication of all or part of the EHR which is itself attestable and which consists of one or more EHR compositions. EHR List A collection of similar EHR items describing a key aspect of a consumer’s health, formed to serve a specific purpose. An EHR List carries with it some notion of persistence, completeness, currency, maintenance, ordering. Examples include problem list and current medications. EHR Notification A type of message or ‘flag’ sent to communicate important occurrences – usually specified in terms of a condition or set of conditions that when satisfied, triggers a pre-defined response. Examples might include hospital admission, emergency department attendance and hospital discharge. EHR Report See report. EHR Request An input transaction component sent to the EHR repository whenever users want to access data, and includes information such as the identity of the requestor, type of request (e.g., EHR view or request to enter/update data), the purpose of the request, and the EHR query itself. 180 HealthConnect Business Architecture v1.9 EHR System Method for recording, retrieving, and manipulating information in electronic health records. EHR Transaction An input or output from an EHR representing a single unit of activity on the EHR repository as a result of a provider’s interaction with the EHR. EHR View A pre-defined set of data items selected from the EHR and returned in response to an EHR request. Encryption Transformation of data to an unintelligible form in such a way that the original data either cannot be obtained (one-way encryption) or cannot be obtained without using the inverse decryption process (two-way encryption). Enrolment The process by which consumers, individual health providers and health provider organisations become participants of HealthConnect. Also see the preferred term: registration. Emergency override The ability of personnel of a healthcare provider organisation to access a consumer’s HealthConnect EHR in an emergency situation where: (a) the consumer is unable to consent; (b) there is no one else available to give consent; and (c) the provider organisation is not already on the consumer’s access control list. Event summary Within HealthConnect, information about one or more healthcare events, that is relevant to the ongoing care of a consumer and may be a subset of the information about the consumer held by the provider. The collection of health event summaries relating to a consumer forms the basis of the consumer’s EHR within HealthConnect. Proposed event summaries include some that contain information currently found in a specialist referral, hospital discharge summary or laboratory test report. Extensible Sufficiently flexible to allow future changes that were not previously anticipated at the outset. FEAF Federal Enterprise Architecture Framework The US Government’s FEAF was selected by the HealthConnect Program Office to guide the development of the HealthConnect architecture. Federation paradigm The assumption that HealthConnect is to be implemented as a unity of potentially different HealthConnect Records Systems operating to common interface standards and supported by common services at a national level. Front end See user interface. 181 HealthConnect Business Architecture v1.9 Governance The process of public accountability for the way in which an organisation conducts its business and may involve stakeholder representation and structures supporting responsibility, accountability and reporting. H2H Health-to-Health Health record A repository of information regarding the health of a consumer. The health record may be paper-based or held electronically. See EHR. Healthcare provider See provider. HealthConnect governing body An entity on behalf of all the participating governments and other stakeholders with the overall management of the HealthConnect program at the national level. HeSA Health eSignature Authority An independent subsidiary of the Health Insurance Commission that acts as a registration authority for the provision of digital keys and certificates required for public key infrastructure used within the Australian health care sector. HL7 Health Level 7 Inc. A global standards development organisation that specialises in standards for information interchange between systems in the health care sector. HRS HealthConnect Records System A computer system for storage and management of consumers’ EHR information and for controlling access to that information. The HealthConnect EHR repository is the sum total of the EHR information held by the HRS services. HRS service The operational function that manages and provides access to EHR information in an HRS. Identified data Data are termed ‘identified’ when an individual’s identity is readily apparent, or can reasonably be ascertained, from elements of the record. Identifier A universal number or code that uniquely identifies a person or other discrete entity. IM&ICT Information Management and Information and Communications Technology 182 HealthConnect Business Architecture v1.9 Individual provider Within HealthConnect, a registered health professional that is registered with HealthConnect as an individual provider under the HealthConnect rules. Individual providers include medical practitioners, registered nurses, pharmacists and allied health professionals involved in the delivery of health services to individual consumers. Initial health profile Summaries of a consumer’s previous health care (eg past medical history, family history and key pathology results) that form the initial entries in a consumer’s HealthConnect EHR. Interoperability Equivalent to ‘functional interoperability’;- The ability of information systems to reliably exchange information without error. Also see semantic interoperability. ISO/IEC 11179 A specification that describes the standardising and registering of data elements to make data understandable and sharable. Metadata Data about data. Metadata describes how and when and by whom a particular set of data was collected, and how the data is formatted. METeOR METadata Online Registry A knowledgebase of metadata items maintained by the Australian Institute of Health and Welfare. National data store A data storage and archiving service that aggregates EHR information from across all HealthConnect HRS services. National health identifier A universal number or code that uniquely identifies each person at a national level. NEHTA National E-Health Transition Authority Entity created to drive the national information management and information and communications technology priorities to June 2005, at which stage a longer term authority may be established. National health provider directory A national repository of healthcare providers supporting several health care initiatives, including HealthConnect. See also provider directory. NHDD National Health Data Dictionary Data definitions recommended for use in Australian health data collections, as well as the National Minimum Data Sets agreed for mandatory collection and reporting at a national level. Non-repudiation The capacity to obtain proof that cannot be forged and confirms the integrity and origin of a data item. 183 HealthConnect Business Architecture v1.9 openEHR openEHR is an international not-for-profit foundation working towards interoperable, life-long electronic health records, proven in practice. OWL Web Ontology Language A semantic web standard that provides a framework for the management, integration and sharing and reuse of data on the web. PIN Personal Identification Number. Provider Within HealthConnect, a term encompassing individual providers and provider organisations. Provider directory Within HealthConnect, a database holding details of every provider participating in HealthConnect, their HealthConnect identifier, and contact information that enables the provider to be contacted by various means including delivery or collection of eHealth messages. Provider organisation Within HealthConnect, an organisation that is registered with HealthConnect as a provider organisation under the HealthConnect rules. A provider organisation may be any business entity (including a sole trader in the case of an independent practitioner) that delivers health services directly to individual consumers. A provider organisation or other legal entity that provides health services may include other provider organisations. For example, a corporation that delivers health services may be registered as a provider organisation and may comprise several regional hospital groups, each registered with HealthConnect as a provider organisation, and each of these may include hospitals and, below that, particular care teams, all registered with HealthConnect as provider organisations. Within HealthConnect, control of access to information within the consumer’s EHR is by provider organisation. Provider registration agency An organisation authorised by the HealthConnect governing body to register HealthConnect providers in accordance with the HealthConnect rules. Registration The process by which consumers, individual health providers and health provider organisations become a participants in HealthConnect. Similar to enrolment. Report Data from one or more EHRs designed to serve the needs of secondary users (such as clinical research or epidemiology reporting). Secondary Use Any authorised use of a HealthConnect EHR other than for the purpose of supporting the direct delivery of healthcare eg clinical research, epidemiology, population health and health planning. 184 HealthConnect Business Architecture v1.9 Semantic interoperability The ability for information shared between disparate information systems to have the same context and meaning within each information system in which the information is used. Shared EHR Those parts of a consumer’s health record that are made available to (and therefore shared) as part of the consumer’s EHR. Standard A document, established by consensus and approved by a recognised body, that provides for common and repeated use, rules, guidelines or characteristics for activities or their results, aimed at the achievement of the optimum degree of interoperability between information systems. Trigger An act that sets in motion some course of events. User interface The aspect of an information system that a person sees, and the way in which the person interacts with the information system. Value-added services Additional services, created due to a specific business need, that are packaged with the core services. VPN Virtual Private Network The concept of using the internet or other 'public' carriers as transit for private network traffic, usually in encrypted form. XML eXtensible Markup Language A language for organising and annotating data for interchange between disparate information systems. In moving from version 1.9 to version 2.0 of this Business Architecture, there will be further amendments to this glossary, including changes arising from further checks against relevant ISO and other standard vocabularies. 185