Detailed Lecture Outline
advertisement

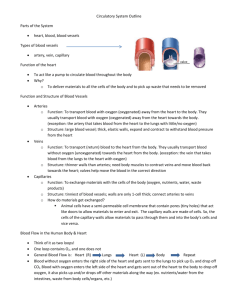
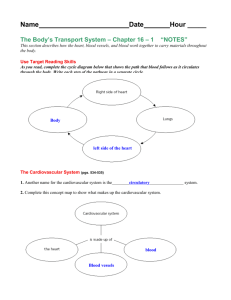
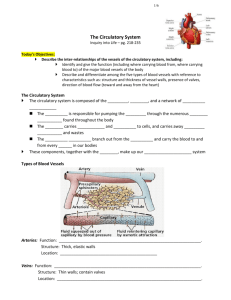
DETAILED LECTURE OUTLINE Fundamentals of Anatomy and Physiology, 7th edition, ©2006 by Frederic H. Martini Prepared by Professor Albia Dugger, Miami-Dade College, Miami, Florida Please note: References to textbook headings, figures and tables appear in italics. “100 Keys” are designated by Key Important vocabulary terms are underlined. Chapter 21: Blood Vessels and Circulation I. The Anatomy of Blood Vessels, p. 709 Objectives: 1. Distinguish between the types of blood vessels on the basis of their structure and function. 2. Describe how and where fluid and dissolved materials enter and leave the cardiovascular system. There are 5 general classes of blood vessels: 1. Arteries carry blood away from the heart. 2. Arterioles are the smallest branches of arteries. 3. Capillaries are the smallest blood vessels, where diffusion between blood and interstitial fluid takes place. 4. Venules collect blood from the capillaries. 5. Veins return blood to the heart. The largest blood vessels attach to the heart. The pulmonary trunk carries blood from the right ventricle to the pulmonary circulation. The aorta carries blood from the left ventricle to the systemic circulation. The smallest blood vessels, about the diameter of a single red blood cell, are the capillaries. All chemical and gaseous exchange takes place by diffusion across capillary walls. Pressure in the blood vessels varies with distance from the heart. Arteries, veins and capillaries have different functions and different structures. The Structure of Vessel Walls, p. 709 Figure 21-1 The walls of arteries and veins have 3 layers which provide strength and control diameter: 1. The tunica intima is the innermost layer, including the endothelial lining and a layer of connective tissue. In arteries, the outer margin of the tunica intima has a layer of elastic fibers called the internal elastic membrane. 2. The tunica media is the middle layer, containing concentric sheets of smooth muscle in loose connective tissue which binds the tunica media to the inner and outer layers. The tunica media is separated from the outer layer by the external elastic membrane. 3. The tunica externa is the outer layer, made up of connective tissue that anchors the vessel to adjacent tissues. In arteries, the tunica externa contains collagen and elastic fibers. In veins, it contains elastic fibers and smooth muscle cells. Arteries and veins are too thick for diffusion of materials. The walls of large vessels contain small arteries and veins (vasa vasorum) that supply the cells of the tunica media and tunica externa. Differences between Arteries and Veins, p. 709 Arteries and veins usually run side by side. Several characteristics distinguish arteries from veins: 1. Walls of arteries are thicker than walls of veins, to withstand higher blood pressure. 2. In section, a collapsed artery has a small, round lumen; a vein has a larger, flat lumen. 3. The lining of a vein can contract; the lining of an artery can not. The lining of a contracted artery folds. 4. Arteries are more elastic than veins. 5. Veins contain valves that prevent backflow of blood. Arteries, p. 710 The elasticity of arteries allows them to absorb the pressure waves that come with each heartbeat. Contractility of arterial walls allows arteries to change diameter under control of the sympathetic division of the autonomic nervous system. Vasoconstriction is the contraction of arterial smooth muscle by the ANS. Vasodilatation is the relaxation of arterial smooth muscle, enlarging the lumen. Vasoconstriction and vasodilation affect: 1. the afterload on the heart 2. peripheral blood pressure 3. capillary blood flow Figure 21-2 As blood moves from the heart to the capillaries, arteries gradually change characteristics: from elastic arteries to muscular arteries to arterioles. Elastic arteries (conducting arteries) are large vessels that transport large volumes of blood away from the heart. The tunica media of elastic arteries has a lot of elastic fibers and few muscle cells. The elasticity of these major vessels (e.g. pulmonary trunk and aorta) evens out the force of the pulse and promotes steady blood flow. Muscular arteries are medium-sized distribution arteries. Most arteries are muscular arteries. The tunica media has more muscle cells than in elastic arteries. Arterioles are small, with very little tunica externa. The tunica media may be incomplete, or have only 1 or 2 layers of muscle cells. The diameters of small muscular arteries and arterioles change in response to sympathetic or endocrine stimulation. More force is required to push blood through a constricted artery than through a dilated one. Since the force opposing blood flow is called resistance (R), arterioles are also called resistance vessels. If the elastic fibers in the wall of an artery fail, a bulge or weak spot called an aneurysm appears -- like a bubble in the wall of a tire. A ruptured aneurysm can cause sudden death. Capillaries, p. 712 The actual exchange function of the cardiovascular system takes place in microscopic capillary networks that permeate all active tissues. Because capillary walls are so thin, materials easily diffuse between the blood and interstitial fluid. Capillaries consist of an endothelial tube inside a thin basal lamina -- no tunica media, no tunica externa. Capillary diameter, 8 micrometers, is about the same as a red blood cell. Figure 21-4 There are 2 major types of capillaries: 1. continuous capillaries 2. fenestrated capillaries Continuous capillaries, which have a complete endothelial lining, are found in all tissues except epithelia and cartilage. Continuous capillaries permit diffusion of water, small solutes, and lipid soluble materials, but block blood cells and plasma proteins. Specialized continuous capillaries in the CNS and thymus have very restricted permeability (e.g. the blood-brain barrier). Fenestrated capillaries, which have pores in the endothelial lining, permit rapid exchange of water and larger solutes between plasma and interstitial fluid. Fenestrated capillaries are found in the choroid plexus of the brain, endocrine organs, kidneys, and absorptive areas of the intestinal tract. Sinusoids are areas in the liver, spleen, bone marrow and endocrine organs which have gaps between adjacent endothelial cells that permit free exchange of water and large plasma proteins between blood and interstitial fluid. Phagocytic cells monitor blood at sinusoids. Figure 21-5 Capillaries function as part of an interconnected network (called a capillary bed or capillary plexus) between one arteriole and one venule. Direct capillary passageways from arteriole to venule are called thoroughfare channels, which are controlled by smooth muscle segments called metarterioles. Multiple arteries that contribute to a single capillary bed are called collaterals. The fusion of 2 collateral arteries is called an arterial anastomosis. Collateral arteries allow circulation to continue even if one artery is blocked. Arteriovenous anastomoses are direct connections between arterioles and venules, bypassing the capillary bed. The entrance to each capillary is guarded by a capillary sphincter which opens and closes, causing capillary blood to flow in pulses. This cycling of contraction and relaxation of capillary sphincters (called vasomotion) causes blood to flow through capillary beds by constantly changing routes. Blood flow through capillary beds is coordinated so that about 25% of capillaries are being used at the same time. Veins, p. 716 Veins collect blood from the capillaries in tissues and organs and return it to the heart. In general, veins are larger in diameter than arteries, but vein walls are thinner than those of arteries because blood pressure is lower. Veins are categorized by size, smallest at the capillaries and largest at the heart. Venules are very small veins that collect blood from the capillaries. Mediumsized veins have a thin tunica media with few smooth muscle cells, and a tunica externa with longitudinal bundles of elastic fibers. Large veins have all 3 tunica layers, with a thick tunica externa and a thin tunica media. Figure 21-6 The blood pressure in venules and medium-sized veins is so low that it cannot overcome the force of gravity. In the limbs, these vessels have folds of tunica intima called valves that keep the blood from flowing backward. Any force that compresses the vein, such as flexing the surrounding muscles, pushes venous blood through the valves toward the heart. If the valves don’t work properly, blood pools and the veins become distended, causing varicose veins or distortion of local tissues such as hemorrhoids. The Distribution of Blood, p. 717 Figure 21-7 Blood volume is not evenly distributed between arteries, veins and capillaries. The heart, arteries and capillaries hold 30-35 percent of the blood, while 60-65 percent is in the venous system. Within the venous system, about 1/3 of the blood (21% of total blood volume) is in the large venous networks of the liver, bone marrow and skin. The capacitance of a blood vessel is the relationship between the volume of blood it contains and the blood pressure (its ability to stretch). Because veins stretch easily (about 8 times as much as an artery) they are also called capacitance vessels. Veins can accommodate large changes in blood volume. If hemorrhaging occurs, vasomotor centers of the medulla oblongata stimulate sympathetic nerves, which has 2 major effects: 1. Systemic veins constrict (venoconstriction) which stabilizes the amount of blood in the arteries and veins by reducing the amount of blood in the venous system. 2. Veins in the liver, skin and lungs constrict, redistributing their venous reserve (21% of blood volume) into the general circulation. II. Cardiovascular Physiology, p. 718 Objectives: 1. Explain the mechanisms that regulate blood flow through arteries, capillaries and veins. 2. Describe the factors that influence blood pressure and how blood pressure is regulated. 3. Discuss the mechanisms and various pressures involved in the movement of fluids between capillaries and interstitial spaces. Figure 21-8 The purpose of cardiovascular regulation is to maintain adequate blood flow through capillaries in peripheral tissues and organs. Capillary blood flow is normally equal to cardiac output. Capillary blood flow is determined by pressure (P) and resistance (R) in the cardiovascular system. The heart generates pressure to overcome resistance in the system. The absolute pressure is less important than the pressure gradient, which is the difference between the pressure at the beginning of the circulation (the heart) and the pressure at the end of the circulation (peripheral capillary beds). Force (F) is proportional to the difference in pressure (∆ P) divided by resistance (R). The pressure gradient in the venous system is relatively low, but resistance in the venous system is also low. Pressure, p. 719 There are 3 important values used when considering pressure: 1. Blood pressure (BP) is arterial pressure in millimeters of mercury (mm Hg). 2. Capillary hydrostatic pressure (CHP) is the pressure within the capillary beds. 3. Venous pressure is the pressure in the venous system. ∆ P across the systemic circuit (circulatory pressure) is about 100 mm Hg. Circulatory pressure must overcome total peripheral resistance (the resistance of the entire cardiovascular system). Resistance, p. 719 Vascular resistance is the resistance of blood vessels due to friction between blood and the vessel walls. Vascular resistance depends on vessel length and vessel diameter. Once an individual stops growing, vessel length is fairly constant. Vessel diameter is varied by vasodilation and vasoconstriction. A small change in diameter may greatly increase or decrease resistance. Resistance (R) is proportional to the inverse of vessel radius (r) to the 4th power. Viscosity is the resistance caused by interactions among molecules and suspended materials in a liquid, such as blood. Whole blood has a viscosity about 4 times that of water. Turbulence is a swirling that disturbs the smooth flow of a liquid. Turbulence occurs in the chambers of the heart and great vessels, but is not normally found in small vessels. Atherosclerotic plaques cause abnormal turbulence in blood vessels that can sometimes be detected using a stethoscope. Table 21-1 summarizes terms and formulaic relationships pertaining to blood circulation. An Overview of Cardiac Pressures, p. 720 Figure 21-9a Following the systemic circuit, beginning at the aorta, arterial diameters decrease to a minimum at the capillaries, venous diameters then increase to the end of the circuit at the vena cava. Figure 21-9b Following the systemic circuit again, total cross-sectional area of blood vessels is lowest near the heart, greatest at the capillary beds. Figure 21-9c Average blood pressure is highest at the aorta, and decreases continually throughout the systemic circulation. Figure 21-9d Blood flow velocity is highest at the aorta, lowest at the capillaries, and low to moderate in the venous system as cross sectional area decreases. Figure 21-10 In detail, arterial blood pressure in the systemic circuit is not constant. With each heartbeat, pressure rises to a peak during ventricular systole (systolic pressure) and a minimum during diastole (diastolic pressure). The difference between the systolic pressure and the diastolic pressure is the pulse pressure. Mean arterial pressure (MAP) is calculated as diastolic pressure plus 1/3 of the pulse pressure. Blood pressure is usually recorded as systolic/diastolic (e.g.120/80). Abnormally high blood pressure is called hypertension (blood pressure > 140/90). Abnormally low blood pressure is called hypotension. During systole, arterial walls stretch. During diastole, they return to their original size (elastic rebound), keeping the blood moving in the arteries during diastole. MAP and pulse pressure decrease in small arteries and arterioles, with distance from the heart. - Blood pressure decreases as it overcomes friction to produce blood flow. - Pulse pressure decreases as a result of elastic rebound. Venous pressure determines venous return (the amount of blood arriving at the right atrium per minute). Effective pressure in the venous system is about 16 mm Hg (18 mm at the venules, 2 mm at the vena cavae), but venous resistance is low. Venous return is assisted by muscular compression of peripheral veins, and the respiratory pump. The compression of skeletal muscles near a vein pushes blood toward the heart because of the one-way valves in the venous system. If leg muscles are immobilized while standing -- as at attention -- venous return can fall, resulting in fainting due to reduced blood supply to the brain. The respiratory pump refers to the action of the thoracic cavity while inhaling and exhaling. Inhaling decreases thoracic pressure, pulling blood into the inferior vena cava and right atrium from the abdominal cavity and lower body. Exhaling raises thoracic pressure, pushing venous blood into the right atrium. Capillary Pressures and Capillary Exchange, p. 723 Capillary exchange is vital to homeostasis. The most important processes that move materials across the capillary walls are diffusion, filtration, and reabsorption. Diffusion is the movement of ions or molecules from an area of high concentration to an area of lower concentration, along the concentration gradient. Different substances diffuse across capillary walls by different routes: 1. Water, ions, and small molecules such as glucose diffuse between adjacent endothelial cells, or through fenestrated capillaries. 2. Some ions (Na+, K+, Ca++, Cl-) diffuse through channels in cell membranes. 3. Large, water-soluble compounds must pass through fenestrated capillaries. 4. Lipids and lipid soluble materials (including O2 and CO2) diffuse through endothelial cell membranes. 5. Plasma proteins cross the endothelial lining only in sinusoids. Figure 21-11 Filtration is the removal of large solutes through a porous membrane, driven by hydrostatic pressure. In capillary filtration, water and small solutes are forced through a capillary wall, leaving larger solutes in the bloodstream. Reabsorption occurs as the result of osmosis (the diffusion of water across a selectively permeable membrane separating 2 solutions with different solute concentrations). Osmotic pressure (OP) equals the amount of pressure required to prevent water from moving across the membrane. Blood has blood colloid osmotic pressure (BCOP) because suspended blood proteins are too large to cross capillary walls. Hydrostatic pressure forces water out of a solution; osmotic pressure forces water into a solution. These factors control the filtration and reabsorption that occurs across the length of a capillary. Figure 21-12 Net hydrostatic pressure pushes water and solutes out of the capillaries and into the interstitial fluid. Net hydrostatic pressure is the difference between capillary hydrostatic pressure (CHP) and hydrostatic pressure of the interstitial fluid (IHP). Under normal conditions, average IHP is zero, and net hydrostatic pressure equals CHP. Net colloid osmotic pressure pulls water and solutes into a capillary from the interstitial fluid. Net colloid osmotic pressure is the difference between blood colloid osmotic pressure (BCOP) and the interstitial fluid colloid osmotic pressure (ICOP). Under normal conditions, ICOP is negligible and net colloid osmotic pressure equals BCOP. Net filtration pressure (NFP) is the difference between net hydrostatic pressure and net osmotic pressure: NFP = (CHP-IHP) - (BCOP-ICOP) At the arterial end of a capillary, NFP = +10 mm Hg, meaning fluid tends to move out of the capillary, into the interstitial fluid. At the venous end of the capillary, NFP = -7 mm Hg, meaning fluid tends to move into the capillary, out of the interstitial fluid. The transition point between filtration and reabsorption is closer to the venous end of the capillary than to the arterial end, meaning capillaries do more filtration than reabsorption. The remainder of the fluid is collected by the lymphatic vessels for return to the venous system. The continuous movement of water out of capillaries and back into the bloodstream via the lymphatic system has 4 important functions: 1. It ensures that plasma and interstitial fluid are in constant communication. 2. It accelerates the distribution of nutrients, hormones and dissolves gases through the tissues. 3. It transports insoluble lipids and tissue proteins that cannot cross capillary walls. 4. It flushes bacterial toxins and other chemicals to immune-system tissues. Conditions that affect hydrostatic or osmotic pressure in blood or tissues affect capillary dynamics: - Hemorrhaging reduces CHP and NFP, increasing reabsorption of interstitial fluid (recall of fluids). - Key Dehydration increases BCOP, accelerating reabsorption. If CHP or BCOP rises, fluid moves out of the blood and builds up in peripheral tissues (edema). Blood flow is the goal, and total peripheral blood flow is equal to cardiac output. Blood pressure is needed to overcome friction and elastic forces and sustain blood flow. If blood pressure is too low, vessels collapse, blood flow stops, and tissues die; if blood pressure is too high, vessel walls stiffen, and capillary beds may rupture. III. Cardiovascular Regulation, p. 725 Objectives: 1. Describe how central and local control mechanisms interact to regulate blood flow and pressure in tissues. 2. Explain how the activities of the cardiac, vasomotor and respiratory centers are coordinated to control blood flow through the tissues. Blood flow through the tissues (tissue perfusion) carries oxygen and nutrients to tissues and organs, and carbon dioxide and wastes away. Tissue perfusion is affected by: 1. cardiac output 2. peripheral resistance 3. blood pressure When a group of cells becomes active, the blood flow in that area must increase. The purpose of cardiovascular regulation is to make sure blood flow changes occur: 1. at an appropriate time 2. in the right area 3. without drastically altering blood pressure and blood flow to vital organs Figure 21-13 Three types of regulatory mechanisms control cardiac output and blood pressure: 1. Autoregulation causes immediate, localized homeostatic adjustments. 2. Neural mechanisms respond quickly to changes at specific sites. 3. Endocrine mechanisms direct long-term changes. Autoregulation of Blood Flow within Tissues, p. 726 Under normal conditions, local blood flow is adjusted by peripheral resistance while cardiac output stays the same. Vasodilators dilate precapillary sphincters. Local vasodilators accelerate blood flow at the tissue level. Local vasodilators include: 1. Low O2 or high CO2 levels. 2. Low pH (acids) 3. Nitric oxide (NO) 4. High potassium or hydrogen ion concentrations. 5. Chemicals released by inflammation (histamine) 6. Elevated local temperature. Local vasoconstrictors, such as prostaglandins and thromboxanes released by damaged tissues, constrict precapillary sphincters. Local vasodilators and vasoconstrictors affect a single capillary bed. Neural Mechanisms, p. 727 The cardiac centers and vasomotor centers of the medulla oblongata (the cardiovascular centers) adjust cardiac output and peripheral resistance. Within the cardiac center, the cardioacceleratory center increases cardiac output and the cardioinhibitory center reduces cardiac output. Within the vasomotor center, vasoconstriction is controlled by adrenergic nerves that release NE, stimulating smooth muscle in arteriole walls to contract. Vasodilation is controlled by cholinergic nerves that release NO, which relaxes the smooth muscle. Sympathetic vasoconstrictor nerves are always active, producing vasomotor tone. Cardiovascular centers detect changes in tissue demand by monitoring arterial blood. Baroreceptor reflexes respond to changes in blood pressure. Chemoreceptor reflexes respond to changes in chemical composition (pH, dissolved gases). When a receptor is stimulated, it triggers a response that counters the stimulus. Figure 21-14 Baroreceptors are stretch receptors found in the carotid sinuses, which maintain blood flow to the brain; the aortic sinuses, which monitors the start of the systemic circuit; and the wall of the right atrium, which monitors blood pressure at the end of the systemic circuit. When blood pressure rises, baroreceptor reflexes alter activity in the CV centers to: 1. decrease cardiac output 2. cause peripheral vasodilation When blood pressure falls, barorecptors: 1. increase cardiac output 2. cause peripheral vasoconstriction Figure 21-15 Chemoreceptor reflexes monitor CO2, O2 and pH. Chemoreceptors in the carotid bodies and aortic bodies monitor blood. Chemoreceptors below the medulla oblongata monitor cerebrospinal fluid, and control respiratory function and blood flow to the brain. Changes in O2 and CO2 concentrations are achieved by coordinating cardiovascular and respiratory activities. The CNS can also affect the cardiovascular centers. Thought processes and emotional states can elevate blood pressure by cardiac stimulation and vasoconstriction. Hormones and Cardiovascular Regulation, p. 730 Figure 21-16 The endocrine system (hormones) has both short-term and long-term effects on cardiovascular regulation. E and NE are hormones produced by the adrenal medullae. Other important hormones include: 1. antidiuretic hormone (ADH) 2. angiotensin II 3. erythropoietin (EPO) 4. natriuretic peptides (ANP, BNP) Antidiuretic hormone elevates blood pressure and reduces water loss at the kidneys. ADH is released by the posterior lobe of the pituitary in response to: 1. low blood volume 2. high plasma osmotic concentration 3. circulating angiotensin II Angiotensin II is released in response to a fall in renal blood pressure. It has 4 important functions: 1. stimulates aldosterone production 2. stimulates ADH production 3. stimulates thirst 4. stimulates cardiac output and peripheral vasoconstriction Erythropoietin is released at the kidneys in response to low blood pressure or low O2 content. EPO stimulates red blood cell production. Key Atrial natriuretic peptide (ANP) is produced in the right atrium in response to excessive diastolic stretching. Brain natriuretic peptide (BNP) is produced by ventricular muscle cells. ANP and BNP lower blood volume and blood pressure, reducing stress on the heart. Cardiac output cannot increase indefinitely, and blood flow to active versus inactive tissues must be differentially controlled. This is accomplished by a combination of autoregulation, neural regulation, and hormone release. IV. Patterns of Cardiovascular Response, p. 732 Objectives: 1. Explain how the cardiovascular system responds to the demands of exercise and hemorrhaging. 2. Identify the principle blood vessels and the functional characteristics of the special circulation to the brain, heart and lungs. Blood, heart and cardiovascular system work together as an integrated complex that constantly responds to physical and physiological changes (e.g. exercise and blood loss) to maintain homeostasis. Exercise and the Cardiovascular System, p. 732 Table 21-2 summarizes the changes in blood distribution during exercise. As light exercise begins, three changes take place: 1. Extensive vasodilation occurs, increasing circulation. 2. Venous return increases with muscle contractions. 3. Cardiac output rises due to the rise in venous return (Frank-Starling principle) and atrial stretching. Regulation by venous feedback causes a gradual increase in cardiac output to about double resting level. With heavy exercise, the sympathetic nervous system is activated, increasing cardiac output to maximum levels (about 4 times resting level). During exercise at maximal levels, blood flow to “nonessential” organs such as the digestive system is severely restricted, redirecting flow to the skeletal muscles, lungs and heart. Only blood supply to the brain is unaffected. Table 21-3 summarizes the effects of training on cardiovascular performance. Regular moderate exercise has several benefits, such as lowering total blood cholesterol levels. Intense exercise, however, can cause severe physiological stress. Cardiovascular Response to Hemorrhaging, p. 733 Figure 21-17 When significant blood loss (hemorrhaging) occurs, the entire cardiovascular system makes adjustments to maintain blood pressure and restore blood volume. The first response to hemorrhaging is to prevent a drop in blood pressure: 1. Carotid and aortic reflexes increase cardiac output (by increasing heart rate) and cause peripheral vasoconstriction. 2. Stimulation of the sympathetic nervous system triggers the hypothalamus to further constrict arterioles, and venoconstriction improves venous return. 3. Hormonal effects: The adrenal medullae secrete E and NE, increasing cardiac output and peripheral vasoconstriction. ADH and angiotensin II enhance vasoconstriction. These short-term responses can compensate for a loss of up to 20% of blood volume. Failure to restore blood pressure results in shock. The long-term response is to restore blood volume, which can take several days: 1. Recall of fluids from interstitial spaces. 2. Aldosterone and ADH promote fluid retention and reabsorption. 3. Thirst increases. 4. Erythropoietin stimulates red blood cell production. Special Circulation, p. 735 Special circulation is circulation through organs which have separate mechanisms to control blood flow, particularly the brain, heart and lungs. Maintaining blood flow to the brain is top priority. The brain has a very high oxygen demand, receiving about 12% of cardiac output. When peripheral vessel constrict, cerebral vessels dilate, keeping blood flow as a normal as possible. A blockage or rupture in a cerebral artery causes stroke or cerebrovascular accident. The coronary arteries supply blood to the heart muscle. When oxygen demand increases with activity, lactic acid production and low O2 levels dilate coronary vessels and increase coronary blood flow. Epinephrine dilates coronary vessels, increases heart rate and strengthens contractions. A blockage of coronary blood flow can cause angina, tissue damage, heart failure or death. Blood flow through the lungs is regulated mainly by oxygen levels within individual alveoli. Where O2 content is high, vessels dilate; where it is low, vessels constrict. This mechanism is the exact opposite of other tissues, because the only purpose of alveolar circulation is to pick up oxygen. Blood pressure in pulmonary capillaries is low to encourage reabsorption. If capillary pressure rises, pulmonary edema occurs. V. The Distribution of Blood Vessels: An Overview, p. 736 Objective: 1. Describe three general functional patterns seen in the pulmonary and systemic circuits of the cardiovascular system. Figure 21-18 There are 3 general functional patterns in blood vessels of the pulmonary and systemic circuits: 1. Peripheral distribution of arteries and veins are the same to the right and to the left, except near the heart. 2. The same vessel may have different names in different locations. 3. Tissues and organs are usually supplied by more than one set of arteries and veins, and may be interconnected by anastomoses, in case of blockage. VI. The Pulmonary Circuit, p. 737 Objective: 1. Identify the major arteries and veins of the pulmonary circuit and the areas they serve. Figure 21-19 The pulmonary circuit is short: - Deoxygenated blood arriving at the heart from the systemic circuit passes through the right atrium and ventricle and enters the pulmonary trunk. - At the lungs, carbon dioxide is removed and oxygen added. - Oxygenated blood then returns to the heart for distribution to the systemic circuit. Pulmonary arteries carry deoxygenated blood, and pulmonary veins carry oxygenated blood. The pulmonary trunk branches from left and right pulmonary arteries into pulmonary arterioles and capillary networks that surround alveoli. Venules then join to become 4 pulmonary veins that empty into the left atrium. VII. The Systemic Circuit, p. 738 Objective: 1. Identify the major arteries and veins of the systemic circuit and the areas they serve. Systemic Arteries, p. 738 Figure 21-20 The systemic circuit (containing 84% of blood volume) supplies the entire body except for the pulmonary circuit. Figure 20-21 Blood moves from the left ventricle into the ascending aorta, where coronary arteries branch out from the aortic sinus. The ascending aorta curves to form the aortic arch, and then becomes the descending aorta. Three arteries that deliver blood to the head and neck originate along the aortic arch: 1. the brachiocephalic trunk 2. the left common carotid artery 3. the left subclavian artery The brachiocephalic trunk branches to form the right subclavian artery and the right common carotid artery. The subclavian arteries have 3 major branches within the thoracic cavity: 1. the internal thoracic artery 2. the vertebral artery 3. the thyrocervical trunk Leaving the thoracic cavity, the subclavian becomes the axillary artery in the arm, and the brachial artery distally. At the coronoid fossa of the humerus, the brachial artery divides into the radial artery and the ulnar artery. At the wrist the radial and ulnar arteries fuse to form the superficial and deep palmar arches, which supply the digital arteries. Figure 21-22 The common carotid arteries carry blood to the head and neck. Each common carotid divides into an external and an internal carotid artery. The external carotid supplies the structures of the neck, lower jaw and face. Figure 21-23 The internal carotid artery enters the skull and divides into 3 branches: 1. the opthalmic artery 2. the anterior cerebral artery 3. the middle cerebral artery The brain also receives blood from the left and right vertebral arteries, which arise from the subclavian arteries. The vertebral arteries enter the cranium through the foramen magnum and fuse to become the basilar artery. The basilar artery branches to form the posterior cerebral arteries, which become the posterior communicating arteries. The internal carotid arteries and the basilar artery are interconnected by an anastomosis called the cerebral arterial circle. An interruption of the vascular supply to a portion of the brain is a cerebrovascular accident (CVA) or stroke. Figure 21-24a The descending aorta is divided by the diaphragm into the thoracic aorta and the abdominal aorta. Figure 21-24b The branches of the thoracic aorta are anatomically grouped into visceral and parietal. Visceral branches supply the organs of the chest: 1. The bronchial arteries 2. The pericardial arteries 3. The esophageal arteries 4. The mediastinal arteries Parietal branches supply the chest wall: 1. The intercostal arteries 2. The superior phrenic arteries The abdominal aorta splits at the terminal segment of the aorta into the left and right common ileac arteries. The major branches (of the abdominal aorta) to visceral organs are unpaired. The branches to the body wall, kidneys, urinary bladder and structures outside the abdominopelvic cavity are paired. Figure 21-25 The abdominal aorta gives rise to 3 unpaired arteries: 1. The celiac trunk, which divides into 3 branches: a. the left gastric artery b. the splenic artery c. the common hepatic artery 2. The superior mesenteric artery 3. The left mesenteric artery The abdominal aorta gives rise to 5 paired arteries: 1. The inferior phrenic arteries 2. The suprarenal arteries 3. The renal arteries 4. The gonadal arteries 5. The lumbar arteries The terminal segment of the abdominal aorta divides to form the right and left common ileac arteries and the middle sacral artery. Each common ileac divides to form an internal ileac artery and an external ileac artery. Figure 21-26 Each external ileac artery passes through the abdominal wall and becomes the femoral artery. The deep femoral artery is the first major branch. Posterior to the knee, the femoral artery becomes the popliteal artery, which then branches to form the posterior and anterior tibial arteries. The posterior tibial artery gives rise to the fibular artery. As they reach the ankle, the anterior tibial artery becomes the dorsalis pedis artery; and the posterior tibial artery divides to form the medial and lateral plantar arteries. The dorsal arch and plantar arch supply the distal part of the foot and toes. Systemic Veins, p. 746 Figure 21-27 Complementary arteries and veins generally run side by side, but the branching pattern of peripheral veins is more variable than that of arteries. One major difference between artery and vein distribution is that, in the neck and limbs, there is one set of arteries, which are deep; but 2 sets of veins, one deep and one superficial. This helps the venous system control body temperature. All the body’s systemic veins drain into either the superior vena cava (SVC) or the inferior vena cava (IVC). Figure 21-28 The superior vena cava (SVC) receives blood from the head, neck, chest, shoulders and upper limbs. The superficial cerebral veins and small veins of the brain stem empty into a network of dural sinuses: 1. The superior and inferior sagittal sinuses 2. The petrosal sinuses 3. The occipital sinus 4. The left and right transverse sinuses 5. The straight sinus The great cerebral vein delivers blood to the straight sinus. Other cerebral veins drain into the cavernous sinus, which delivers blood to the petrosal sinus. The left and right transverse sinuses converge to form the sigmoid sinus, which leaves the skull as the internal jugular vein. Vertebral veins empty into the brachiocephalic veins of the chest. The superficial veins of the head converge to form the temporal, facial and maxillary veins. The temporal and maxillary veins drain into the external jugular vein. The facial vein drains into the internal jugular vein. Figure 21-29 The digital veins empty into the superficial and deep palmar veins, which interconnect to form the palmar venous arches. The superficial arch empties into the cephalic vein, the median antebrachial vein and the median cubital vein. The deep palmar veins drain into the radial and ulnar veins, which fuse above the elbow to form the brachial vein. The brachial vein merges with the basilic vein to become the axillary vein. The cephalic vein joins the axillary vein to form the subclavian vein. The subclavian vein merges with the external and internal jugular veins to form the brachiocephalic vein, which enters the thoracic cavity. In the thoracic cavity, the brachiocephalic vein receives blood from the vertebral vein and, farther down, the internal thoracic vein. The left and right brachiocephalic veins merge to form the superior vena cava. The azygous vein also contributes to the superior vena cava. The azygous vein and hemiazygous vein receive blood from the intercostal veins, esophageal veins, and veins from other mediastinal structures. Figure 21-30a diagrams the venous tributaries of the superior vena cava. Figure 21-30b The inferior vena cava (IVC) collects blood from organs inferior to the diaphragm. Figure 21-31 The capillaries of the sole of the foot drain into a network of plantar veins which supply the plantar venous arch. The plantar network drains into the deep veins of the leg: 1. the anterior tibial vein 2. the posterior tibial vein 3. the fibular vein These 3 veins join to become the popliteal vein. The dorsal venous arch collects blood from the superior surface of the foot and digital veins, and drains into 2 superficial veins: 1. the great saphenous vein, which drains into the femoral vein 2. the small saphenous vein, which drains into the popliteal vein At the femur the popliteal vein becomes the femoral vein. Before entering the abdominal wall, the femoral vein receives blood from: 1. the great saphenous vein 2. the deep femoral vein 3. the femoral circumflex vein Inside the pelvic cavity, the femoral vein becomes the external iliac vein. The external iliac veins are joined by the internal iliac veins to form the right and left common iliac veins. The 2 common iliac veins merge to form the inferior vena cava. Figure 21-29 The abdominal portion of the inferior vena cava collects blood from 6 major veins: 1. lumbar veins 2. gonadal veins 3. hepatic veins 4. renal veins 5. suprarenal veins 6. phrenic veins Figure 21-30b shows the tributaries of the inferior vena cava. Figure 21-32 The hepatic portal system (a portal system connects 2 capillary beds) delivers nutrient-laden blood from the capillaries of the digestive organs to the liver sinusoids for processing. The hepatic portal vein receives blood from: 1. the inferior mesenteric vein (part of large intestine) 2. the splenic vein (spleen, stomach and pancreas) 3. the superior mesenteric vein (stomach, small intestine, part of large intestine) 4. the left and right gastric veins (stomach) 5. the cystic vein (gallbladder) After processing in the liver sinusoids, blood is collected in the hepatic veins and emptied into the inferior vena cava. VIII. Fetal Circulation, p. 753 Objectives: 1. Identify the differences between fetal and adult circulation patterns. 2. Describe the changes in the patterns of blood flow that occur at birth. Fetal and adult cardiovascular systems are significantly different. Embryonic lungs and digestive tract are nonfunctional, since nutrition and respiratory functions are provided by the placenta. Placental Blood Supply, 753 Figure 21-33a Blood flows to the placenta through a pair of umbilical arteries, which arise from the internal iliac arteries and enter the umbilical cord. Blood returns from the placenta in a single umbilical vein, which drains into the ductus venosus. The ductus venosus empties into the inferior vena cava. Circulation in the Heart and Great Vessels, p. 753 Figure 21-33b Before birth, fetal lungs are collapsed and oxygen is provided by the placental circulation. At birth, the newborn must breathe air to get oxygen, expanding the lungs and initiating pulmonary circulation. Before birth, fetal pulmonary circulation is bypassed by 2 short-cuts: 1. The foramen ovale: an interatrial opening in the heart which is covered by a valve-like flap that directs blood from the right atrium to the left atrium. 2. The ductus arteriosus: a short vessel connecting the pulmonary and aortic trunks. Cardiovascular Changes at Birth, p. 754 At birth, the lungs and pulmonary vessels expand, reducing resistance and allowing blood to flow to the pulmonary circuit. The rise in O2 levels causes the ductus arteriosus to constrict, and rising pressure in the left atrium closes the valvular flap over the foramen ovale. Figure 21-34 If proper circulatory changes do not occur at birth, heart defects called congenital cardiovascular problems develop. IX. Aging and the Cardiovascular System, p. 756 Objective: 1. Discuss the effects of aging on the cardiovascular system. Cardiovascular capabilities decline with age. Age related changes occur in blood, heart and blood vessels. Age-related changes in blood: 1. decreased hematocrit 2. blood clots (thrombus) 3. blood pooling in legs due to venous valve deterioration Age-related changes in the heart: 1. reduced maximum cardiac output 2. changes in nodal and conducting cells 3. reduced elasticity of fibrous skeleton 4. progressive atherosclerosis 5. replacement of damaged cardiac muscle cells by scar tissue Age-related changes in blood vessels: 1. arteries become less elastic (sudden pressure change can cause aneurysm) 2. calcium deposits on vessel walls (stroke or infarction) 3. thrombi can form at atherosclerotic plaques X. Integration with Other Systems, p. 756 The cardiovascular system is closely linked to all other systems. Figure 21-35 The relationship between the cardiovascular system and other systems. Clinical Patterns, p. 756 Cardiovascular disorders affect every cell in the body. They may be structural, functional, or result from disease or trauma. The major categories of clinical disorders affecting the cardiovascular system are covered in the Applications Manual. SUMMARY In Chapter 21 we learned about: - the 3 main types of blood vessels - arteries, veins and capillaries - the structure of vessel walls - the differences between arteries and veins - the structure of elastic arteries, muscular arteries and arterioles - atherosclerosis, arteriosclerosis and plaques - the structure of capillary walls - continuous or fenestrated - the structures of capillary beds - precapillary sphincters, vasomotion and arteriovenous anastomoses - the functions of the venous system and valves - the distribution of blood and venous reserves - circulatory blood pressure, capillary hydrostatic pressure and venous pressure - the resistance of blood vessels - viscosity, turbulence and vasoconstriction - cardiovascular pressure and the respiratory pump - capillary pressure and capillary exchange - osmotic pressure, net filtration pressure - the physiological controls of the cardiovascular system - autoregulation, neural controls, hormonal controls - cardiovascular responses to exercise and blood loss - special circulation to brain, heart and lungs - the distribution of arteries in the pulmonary and systemic circuits - the distribution of veins in the pulmonary and systemic circuits - fetal circulation and changes at birth - the effects of aging on the cardiovascular system