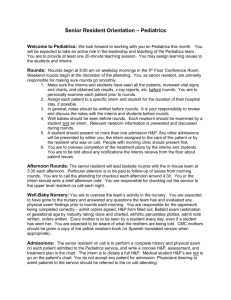
DAILY EXPECTATIONS PRE
advertisement

INTERN SUCCESS ON THE WARDS INTERNAL MEDICINE – MCV/VA TEAM __ MONTH 2006 Attending: XXXX #pager Resident: XXXX #XXXX Interns: XXXX XXXX Med Studs: XXXX PharmD: XXXX Free days: Interns - 4 days off per month Resident-4days off this month home phone number Interns can accept up to 5 patients per call Interns cap overall at 12 patients Each ward team caps at 24 patients Duties expected of interns: Pre-rounding, checking labs, getting work done, writing notes, supervising med studs DAILY EXPECTATIONS PRE-ROUNDING Check your labs – REPLETE YOUR ELECTROLYTES RIGHT AWAY WHEN YOU SEE THE LABS: Hypokalemia: goal around 4.0 Give 10meq KCl for 0.1 mmol deficiency (be more cautious if elevated creatinine) Priority PO (4 tabs or 40meq at a time) – works fastest and best If NPO/unable to eat/ or ultra low, then KCL IV 10meq/hr x 4 hrs Hypomagnesemia: goal > 1.7 PO repletion with Magnesium Gluconate is ineffective Give Magnesium Sulfate 2g IV and then q4hrs prn if very low <1.5 Hypophosphatemia: goal > 2.4 PO Neutrophos packets 1-2 effective If very low, give Potassium Phosphate 15-20mmol IV Sodium Phosphate 15-30mmol IV (if K+ high) FOLLOW TRENDS IN LABS AND ADDRESS THEM WITH ME OR IN ROUNDS Hypernatremia: may be sign of dehydration Elevating BUN/CREAT: may be geting dry Dropping HCO2: getting acidotic – if severe may need ABG Anion Gap: Consider causes of AG acidosis When Seeing the Patient while Pre-rounding • Look through the chart for any overnight happenings or consult recommendations • Get the most recent Vital signs, Tmax, Ins and Outs if applicable, and any variable or impressive vital signs • Every patient needs a heart and lung examination daily, and otherwise a problem focused examination • Address any instabilities/Emergencies immediately and do not leave unstable patients just to finish prerounding • Make any consults or arrangements before rounds if possible if you know they need to be done * Notify me of any major happenings or emergencies – NO SURPRISES DURING ROUNDS! Month 2006: Team X Wards: Intern Guide to Success Resident Name and Pager ROUNDING • • • • Present all patients in SOAP format During your P-Plan section, make a PROBLEM LIST and address each problem with an appropriate plan Your last Problem in every problem list is DISPOSITION – Think ahead to where the patient will be going for discharge and address with social work early on if disposition (Nursing Home/home health) will be an issue - we do NOT want a nursing home team!!! (too much pre-rounding and rounding) If a medical student is following a patient with you, let them present during rounds and try your hardest not to interrupt (Give them some glory!!!) and add your comments at the end (unless there are questions they cannot answer or something is just blatantly wrong) AFTER ROUNDS: GET YOUR WORK DONE in this priority/order: 1. 2. 3. 4. 5. 6. 7. 8. ORDERS: Find a computer and get all your orders into the computer as discussed in rounds DISCHARGES: Get your discharges done right away – get people out as early as possible Call your consults ASAP – early consults get done earlier and we do not waste a day. Before anything else, tell the consultant the reason for consultation so they can focus on listening to the information that may apply to them while you’re giving some history Put in your AM labs Write your notes for the day – as a medical student this was your priority. As a intern and resident this is your last priority. Get your work done and THEN write your notes. You can start writing your note before rounds and during rounds as well when someone else is presenting a patient that is not yours!!! You may temporarily leave rounds to get some orders into the computer as long as you are available to present your patients Make your Checkout sheet and touch base with me before you check out to the appropriate on-call intern or night float Go home, exercise, read, sleep, be merry!!! CLINICAL PEARLS/THINGS TO KNOW AND DO ON THE SPOT: Chest Pain • If you get called for a patient with chest pain, while on the phone get a full set of vital signs and make sure that the patient is hemodynamically stable – if hypotensive this is an emergency and a code should be called or the unit should be notified ASAP if not quite Code Blue material • If vital signs are stable ask the nurse to get an EKG and put on 2L oxygen (at least) while you are en route to see the patient • See the patient and obtain a chest pain history • EXAMINE THE PATIENT with a good heart and lung exam and assess for signs of failure • Make the patient chest pain free sublingual NTG 0.4mg q5min up to 3x morphine 2-4mg IV push metoprolol 5mg IV push (q5min x 3) slow rate to 60’s • Once chest pain free can slap on Nitropaste 1-2” inches • Give an Aspirin 325mg po STAT - NOT ENTERIC COATED as you want immediate effect!!!!! • If the history and physical is impressive for unstable angina or acute coronary syndrome, namely: new chest pain, worse than baseline, or requiring extra NTG exam shows failure new EKG changes from baseline If any of these are positive, then call the CCU resident for evaluation to transfer to the CCU to r/o MI If you know they are going to the unit, do a rectal for heme check Since will be started on heparin • If you are uncertain or if you are certain, you may draw one set of cardiac enzymes on the floor (controversial) Month 2006: Team X Wards: Intern Guide to Success Resident Name and Pager Shortness of Breath: You will get called for this often • Get a set of vital signs including a pulseOx • Give O2 nasal cannula keeping sats appropriate (at least 94%) and jump up to face mask or non-rebreather prn • Obtain a good history on the patient considering past medical conditions (Asthma, COPD, CHF, bedbound) with questions such as wheezing, orthopnea, failure symptoms, acute onset, progressive onset • Perform a directed heart and lung exam – evaluate for crackles, wheezing, breath sounds throughout, tacchypnea • If impressive order a stat portable Chest x-ray • Treat the patient depending on your suspected cause: CHF: If you hear crackles Æ Lasix 40mg IV stat, get an EKG if suspicious for ischemia COPD: If you hear wheezing Æ Albuterol nebs stat and as often as it takes Atrovent nebs q 2-4 hrs Steroids (solumedrol 125mg IV) or (prednisone 60mg PO) If you hear wheezing, may still be CHF (cardiac asthma) so may also diurese PE: If no crackles, no wheezes, clear CXR, acute onset, tacchypneic, tacchycardic, hypoxic With risk factors for embolus, then get an ABG, EKG, rectal exam, heparinize and consider Spiral CT or V/Q Scan PTX: If you hear no breath sounds on one side, has emphysema and bullae, consider pneumothorax And get stat CXR and need for potential needle decompression or chest tube Unresponsiveness: • If you get called for a patient who is unresponsive, get vital signs – If no pulse or BP Æ Call CODE BLUE • If Vital signs are unstable then correct the vital signs and the cause • If Vital Signs are stable and saturations are good with spontaneous breathing then consider different etiologies • Check these things in this order on the spot Vital signs, Accucheck for Blood sugar, EKG, ABG, Electrolytes • Things you can do on the spot and follow up D50 – one amp Å Hypoglycemia Narcan (Naloxone) – one amp Å Drug Overdose (morphine, opiates) Flumazenil – 0.2mg IV push Å Drug Overdose (benzodiazepines) Thiamine 100mg Å It’s Magic – Wernickes Head CT (no contrast) Å Stroke (looking for bleed) EEG - benzos Å Seizure or Status epilepticus ADMISSION HISTORY AND PHYSICALS: • Details, details, details in terms of history of physical; know ER vital signs and what was given there • Definitely know allergies, meds, tobacco, etoh, primary care physician, and code status • Get a phone number of who they live with and where they are going to go before you get stuck with no contact DISCHARGES: • Right when a patient is admitted, think about disposition (know where they are going, who they live with and get appropriate phone numbers, and who their PCP is to set up follow) • Notify Social Work ASAP about possible Nursing Home Placement, Home Health, Home Physical Therapy (must in seen and evaluated by PT in the hospital first!!!), and ride needs (ambulance or transportation) • When you anticipate discharge within one day, touch base with family and make a PCP follow up appointment • Get your discharge meds and orders in as early as possible • Every chart needs a discharge summary (including deaths) – this does not have to be long, but needs to include problem list, discharge medications, and follow up appointment • When a patient is discharged, make sure to keep the chart in the team room so it can be dictated • DICTATIONS: as interns you are not obligated to dictate until October. If you feel comfortable dictating, go right ahead. I recommend that you dictate at least ¼ of the discharges just to practice for when you have to do them all. Let me know which ones you will be dictating so that I don’t repeat the work PAGE ME OR CALL ME AT HOME WITH ANY PROBLEMS OR QUESTIONS RESIDENT PAGER #_____ OR HOME PHONE _____ Month 2006: Team X Wards: Intern Guide to Success Resident Name and Pager