are combinations of antifungals beneficial or deleterious?
advertisement

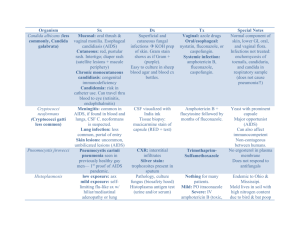
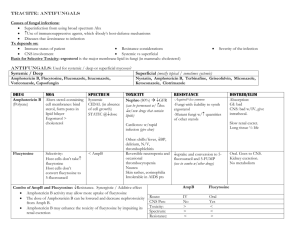
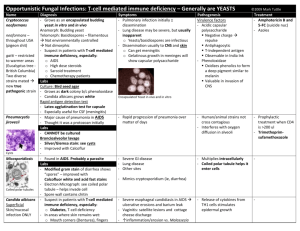
PROCEEDINGS ARE COMBINATIONS OF ANTIFUNGALS BENEFICIAL OR DELETERIOUS?* — Manuel Cuenca-Estrella, MD, PhD ABSTRACT Concomitant combination therapy has been used in recent years to treat invasive fungal infections, but limited data from in vitro, animal, and clinical studies have been reported. We review in this article amphotericin B plus flucytosine, amphotericin B plus azoles, azoles plus flucytosine, amphotericin B or azoles plus terbinafine, and amphotericin B or azoles plus caspofungin, as well as some of the available data on these combinations. Clinical trial data in which combination therapy was compared with monotherapy are available for 3 of the combinations. Overall, combination therapy was similar and sometimes more effective compared with monotherapy. However, with the exception of cryptococcal meningitis, none of the combinations was clearly superior to monotherapy. Clinical trial findings and clinical experience suggest that combination therapy may be an alternative to monotherapy for invasive infections due to multiresistant fungi, as well as an alternative for patients who fail to respond to monotherapy. (Advanced Studies in Medicine. 2003;3(1A):S14-S17) *Based on a presentation given by Dr Cuenca-Estrella at the 12th European Congress of Clinical Microbiology and Infectious Diseases. Address correspondence to: Manuel Cuenca-Estrella, MD, Unidad de Micologia, Instituto de Salud Carlos III, Centro Nacional de Microbiologia, Ctra. Majadahonda a Pozuelo, km.2, 28220 Majadahonda, Madrid, Spain. S14 ombination therapy for invasive fungal infections is typically considered as a therapeutic option to improve results of treatment with a single agent, as well as in cases of treatment failure with monotherapy. However, clinical trial data regarding the safety and efficacy of combination therapy remain limited, underscoring the need for further study. Several combinations of various antifungal agents have been used in recent years (Table 1); these combinations, as well as some of the in vitro, animal, and clinical data, are discussed in greater detail below. C AMPHOTERICIN B PLUS FLUCYTOSINE Concomitant combination therapy with amphotericin B and flucytosine is now considered the standard treatment of cryptococcal meningitis. However, a review of the evidence reveals that, except in Cryptococcus infections,1 the combination is not clearly superior to monotherapy with amphotericin B. In reviewing in vitro studies, results obtained by the checkerboard method show that this combination exhibits indifferent, additive, or synergistic effects against Candida and Aspergillus species. Antagonism has not been reported. In contrast to the checkerboard method, which provides only inhibitory data, other procedures, such as the time-kill curve technique, measure microbiocidal activity and offer a dynamic picture of antimicrobial action. Data from studies using the killing curve technique have indicated that the combination of amphotericin B and flucytosine has additive or synergistic effects against Candida albicans isolates. Animal models have provided limited data showing the com- Vol. 3 (1A) ■ January 2003 PROCEEDINGS bination is similar to or better than amphotericin B monotherapy against Candida and molds. Results from 5 clinical trials evaluating the combination have shown it is generally similar to and sometimes better than monotherapy with either agent alone efficacy and is similar to monotherapy with amphotericin B in terms of safety (Table 2).2-6 Successful outcomes with this combination are documented in case reports. Aerosolized amphotericin B plus itraconazole was more effective than monotherapy in a patient with acquired immune deficiency syndrome (AIDS) who developed tracheobronchial aspergillosis. In another case, amphotericin B plus itraconazole was effective in a patient AMPHOTERICIN B PLUS AZOLES As with the previous combination, checkerboard studies of amphotericin B plus an azole have yielded a variety of results, such as indifference, additive effects, synergy, and outstandingly, antagonism. Studies using time-kill methods have found antagonism between amphotericin B and fluconazole toward Candida and Cryptococcus species and between amphotericin B and itraconazole for Aspergillus isolates. Results from studies using animal models, however, show that amphotericin B plus either fluconazole or itraconazole is similar to or more effective than amphotericin B monotherapy against Candida and Cryptococcus species, and that amphotericin B plus itraconazole is similar to amphotericin B monotherapy, but better than itraconazole therapy against Aspergillus species. Yet, there are some animal data that show antagonism with this combination. Table 1. Drug Combinations Used to Treat Invasive Fungal Infections Amphotericin B + flucytosine Amphotericin B + azoles Azoles + flucytosine Amphotericin B or azoles + terbinafine Amphotericin B or azoles + caspofungin Other combinations, including amphotericin B + rifampin, amphotericin B + quinolones, azoles + quinolones, fluconazole + cyclosporine Table 2. Summary Findings From 5 Reports of Combined Amphotericin B and Flucytosine Therapy Smego et al2 Goldman et al3 Verweij et al4 Abele-Horn et al5 Silling et al6 Infection Neonates (n = 17) Candida meningitis Neutropenic (n = 62) Candida krusei Monotherapy Amphotericin B Intensive care unit (n = 72) Systemic candidiasis Fluconazole (400 mg) Neutropenic (n = 98) Febrile neutropenia Fluconazole Response rate with combined vs monotherapy Combined better Amphotericin B (0.5 mg) Amphotericin B (1 mg) Combined better than low-dose monotherapy Neutropenic (n = 28) Invasive fungal infections Amphotericin B (0.5 mg) Similar Similar Similar Adverse events with combined vs monotherapy Similar Similar Higher with combined Higher with combined Patients Advanced Studies in Medicine ■ Similar S15 PROCEEDINGS with hepatic abscesses caused by Aspergillus terreus and an invasive sinonasal infection due to Scopulariopsis. Amphotericin B plus fluconazole has also been successful in treating a patient with prosthetic valve endocarditis caused by Candida, and a burn patient with an invasive infection due to Trichosporon. A retrospective study by Caillot et al included 30 neutropenic patients with invasive pulmonary aspergillosis who were treated with amphotericin B plus itraconazole or itraconazole alone; 8 of the 30 patients failed to respond to combination therapy.7 Of the 22 patients who were cured or showed improvement with the combination or itraconazole monotherapy, 15 were also treated surgically (lung resection). This makes it difficult to determine the extent to which each of the treatment methods—monotherapy, monotherapy plus surgery, combination drug therapy, and combination drug therapy plus surgery—contributed to cure or improvement. The most important clinical trial of the amphotericin B plus an azole combination was conducted by Rex et al.8 Patients with candidemia (n=236; 60% caused by C albicans) were randomized either to amphotericin B plus fluconazole or fluconazole plus placebo. The overall response rates were 68% in the patients receiving 2 antifungal agents and 56% in those receiving 1 agent plus placebo. However, the patients receiving monotherapy had significantly higher Acute Physiology and Chronic Health Evaluation scores (ie, they were more seriously ill), which could have affected the results of the trial. Despite the promising results in studies reported thus far, more clinical studies of combinations of amphotericin B and azoles are needed. AZOLES PLUS FLUCYTOSINE In vitro studies of azoles plus flucytosine have found additive and synergistic effects against Cryptococcus neoformans and indifference against Candida and Aspergillus species. No antagonism in vitro has been reported. Animal studies have found the combination to be better than or as effective as monotherapy, with some studies finding synergistic effects between azoles and flucytosine, mainly in animal infections due to Cryptococcus. Clinical evidence includes a case report of a patient with lymphoma who developed pulmonary aspergillosis and was treated successfully with itraconazole and flucytosine, and another in which a patient with renal failure who S16 developed disseminated candidiasis was successfully treated with fluconazole plus flucytosine. A double-blind randomized study compared the efficacy of fluconazole plus placebo, itraconazole plus flucytosine, and placebo plus placebo in 85 patients with AIDS who had esophageal candidiasis.9 The 53 men and 32 women were diagnosed endoscopically and clinically at the first episode of esophageal candidiasis and then randomized in double-blind fashion into the 3 treatment groups. After 2 weeks of treatment, patients previously randomized to placebo plus placebo were then randomized in double-blind fashion to either fluconazole plus placebo or itraconazole plus flucytosine. Endoscopic and clinical examinations were performed at weeks 2 and 4 and at the end of follow-up (3 months). Endoscopic and clinical cure rates at week 2 and the end of follow-up are shown in Table 3. The results show that both monotherapy and combination therapy are effective in the short-term treatment of esophageal candidiasis in patients with AIDS. The results also suggest that combination therapy may be an alternative in patients with fluconazole-resistant Candida esophagitis.9 AMPHOTERICIN B OR AZOLES PLUS TERBINAFINE Some in vitro studies have reported indifference for Aspergillus and Zygomycetes species with the combination of amphotericin B and terbinafine, and there have Table 3. Results of Monotherapy vs Combination Therapy at 2 Weeks and 3 Months in Patients With AIDS and Esophageal Candidiasis Fluconazole + Placebo (%) Itraconazole + Flucytosine (%) 2 Weeks Endoscopic cure Clinical cure 68.0 75.8 72.4 72.4 3 Months Endoscopic cure Clinical cure 89.8 94.8 94.8 97.3 Results Data from Barbaro et al.9 Vol. 3 (1A) ■ January 2003 PROCEEDINGS been some reports of antagonism with this combination in Aspergillus species. On the other hand, the combination of an azole agent and terbinafine has shown synergistic effects against yeasts and molds. Animal studies evaluating voriconazole plus terbinafine have found that its effects against Candida, Zygomycetes, and Scedosporium species are synergistic10; however, there are no clinical trial data at this time. AMPHOTERICIN B OR AZOLES PLUS CASPOFUNGIN Studies of the in vitro activity of amphotericin B plus caspofungin have found indifference and additive or synergistic effects against various isolates of Candida, Aspergillus, and Cryptococcus, with the type of effect varying according to the isolate. There are 3 case reports with successful outcome, including 1 report focusing on the combination of amphotericin B and caspofungin to treat aspergillosis, and 2 reports on the combination of itraconazole and caspofungin in A fumigatus and A terreus infections.11 Clinical trial data are needed to evaluate these combinations more fully. OTHER COMBINATIONS Several other combinations of antifungal agents have been studied in vitro. Amphotericin B plus rifampin has shown additive and synergistic effects against Candida and Aspergillus species, whereas combinations of amphotericin B plus a quinolone and fluconazole plus a quinolone have shown additive and synergistic effects against Candida and Mucoraceae species. Another combination, fluconazole plus cyclosporine, has shown additive and synergistic effects in vitro against C albicans. CONCLUSIONS Of the various antifungal combinations described here, there are clinical trial data for only 3 of them: amphotericin B plus flucytosine, amphotericin B plus azoles, and azoles plus flucytosine. Except for the efficacy of amphotericin B plus flucytosine against Cryptococcus infection, none of the 3 combinations was clearly superior to monotherapy. Concomitant combination therapy could be an alternative to monotherapy for invasive infections due to multiresistant fungi, such as Scedosporium, Fusarium, Scopulariopsis, and Rhodotorula, and may also be an alternative for patients who fail to respond Advanced Studies in Medicine ■ to other treatments. Data from well-designed stratified clinical trials are needed. These trials should analyze results not only regarding patients, but also regarding risk factors, infection, and species. REFERENCES 1. van der Horst CM, Saag MS, Cloud GA, et al. Treatment of cryptococcal meningitis associated with the acquired immune deficiency syndrome. National Institute of Allergy and Infectious Diseases Mycoses Study Group and AIDS Clinical Trials Group. N Engl J Med. 1997;337:15-21. 2. Smego RA Jr, Devoe PW, Sampson HA, Perfect JR, Wilfert CM, Buckley RH. Candida meningitis in two children with severe combined immunodeficiency. J Pediatr. 1984; 104:902-904. 3. Goldman M, Pottage JC Jr, Weaver DC. Candida krusei fungemia. Report of 4 cases and review of the literature. Medicine (Baltimore). 1993;72:143-150. 4. Verweij PE, Donnelly JP, Kullberg BJ, Meis JF, De Pauw BE. Amphotericin B versus amphotericin B plus 5-flucytosine: poor results in the treatment of proven systemic mycoses in neutropenic patients. Infection. 1994;22:81-85. 5. Abele-Horn M, Kopp A, Sternberg U, et al. A randomized study comparing fluconazole with amphotericin B/5-flucytosine for the treatment of systemic Candida infections in intensive care patients. Infection. 1996;24:426-432. 6. Silling G, Fegeler W, Roos N, Essink M, Buchner T. Early empiric antifungal therapy of infections in neutropenic patients comparing fluconazole with amphotericin B/flucytosine. Mycoses. 1999;42(suppl 2):101-104. 7. Caillot D, Casasnovas O, Bernard A, et al. Improved management of invasive pulmonary aspergillosis in neutropenic patients using early thoracic computed tomographic scan and surgery. J Clin Oncol. 1997;15:129-147. 8. Rex JH, Pappas PG, Karchmer AW, et al. A randomized and blinded multicenter trial of high-dose fluconazole plus placebo vs amphotericin B plus fluconazole as treatment of candidemia in nonneutropenic patients. Presented at: 41st Interscience Conference on Antimicrobial Agents and Chemotherapy; December 16-19, 2001; Chicago, Ill. Abstract J-681a. 9. Barbaro G, Barbarini G, DiLorenzo G. Fluconazole vs itraconazole-flucytosine association in the treatment of esophageal candidiasis in AIDS patients. A double-blind, multicenter, placebo-controlled study. The Candida Esophagitis Multicenter Italian Study (CEMIS) Group. Chest. 1999;110:1507-1514. 10. Meletiadis J, Mouton JW, Meis JF, Verweij PE. Combination chemotherapy for the treatment of invasive infections by Scedosporium prolificans. Clin Microbiol Infect. 2000; 6:336-337. 11. Rubin MA, Carroll KC, Cahill BC. Caspofungin in combination with itraconazole for the treatment of invasive aspergillosis in humans. Clin Infect Dis. 2002;34:1160-1161. S17