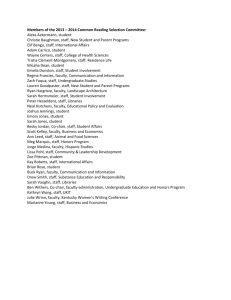
Sarah Murphy`s tattoo experience after facing breast cancer and
advertisement

Sarah Murphy's tattoo experience after facing breast cancer and early menopause Her treatment for breast cancer induced an early menopause at the age of 36. But Sarah refuses to dwell on it, says Catherine Shanahan – Irish Examiner – Feel Good, 23/10/15 THE tattoo is large, bold and defiant, a rebellious response to the cancer that stopped her in her tracks. “My whole life I wanted a tattoo, I have always loved body art. Initially I was going for something discreet, pretty, behind the ear. A small pink ribbon. But then I thought ‘no, this is what I want’.” Sarah Murphy, 40, from Carrigtohill, Co Cork, extends her right arm to properly display the ribbon synonymous with raising breast cancer awareness. Her own discovery that she had a tumour has a familiar ring. She was towelling off postshower when she thought “hang on there, I’m actually feeling a lump”. “From that moment I knew in my heart that it was cancer. Call it women’s intuition, but I just knew. It was a fairly large, hard and slightly painful lump on the top part of my left breast,”Sarah says. That was December 2011. After a Christmas night out, Sarah confided in her sister who had experience of benign cysts. “The cysts had been moveable, but this was not. She advised me to go to my GP.” Anxious not to spoil the family Christmas — Sarah has two sisters and two brothers — she did nothing about the lump until the New Year. On January 4, she went to her GP who made an immediate appointment for her to attend David Gough, consultant surgical oncologist at the Bon Secours Hospital in Cork. She went with her mum to the Bons on January 9 where she says the “running on the hampster wheel began”. She was sent for a mammogram, then an ultrasound, followed by a needle biopsy. Further biopsies were taken from under her arm. She had to wait a week for the results. “That was one tough week to put down. I wanted to prepare mum and dad for the possibility that it was cancer, but I didn’t know how. “So the week more or less went like this: They would say ‘It’ll be great to get the results and put it all behind us’ and I would say ‘Yeah, it will, but let’s not discount entirely the possibility of bad news’. We were all worried, but in true Irish fashion, none of us really had the words.” It was business as usual for Sarah during that week. A music teacher with the Cork Educational and Training Board School of Music, she teaches violin to youngsters in Carrigaline and Glanmire. On January 16, Sarah received the bad news. Her main concern was for her mum. “I could see that the actual words came as a huge shock. I was heartbroken for her. There I was, her 36-year-old daughter, just diagnosed with breast cancer.” She was scheduled to have a lumpectomy (removal of the breast tumor and some of the tissue around it) and sentinel lymph node biopsy on January 19, a procedure in which the sentinel node is removed and examined to determine if further cancer cells are present. Once the surgery results were back, a treatment plan would be formulated. “Mr Gough said I’d have one really horrible year of treatment but then I would return to my life. So the prognosis was really quite good to my ears,” she says. Sarah and her mum went home to break the news to her dad. “That was the hardest. I, of course, had a completely inappropriate reaction. You know that nervous laughter you get sometimes when trying to impart difficult news? So there he was sitting on the couch where he reads his newspaper every day with a bright, hopeful look on his face. And I had to crush him by telling him that yeah, I had cancer”. The cancer diagnosis wrought some immediate changes. Sarah packed up and moved back home. She also told her friends. “Some handled it well and others didn’t,” she says. She returned to the Bons with her mum on January 19. There were a lot of tests. She was injected with a blue dye that “turned me a pale shade of blue which my family thought was hilarious so they bought me a Smurfett”. Family support was invaluable, she says, from the black humour of younger brother Mark which she says sustained her throughout, to the surprise trip home from California by older brother Neil, to sister Ruth who came home from Boston for her first day of chemo and her sister Rachel who was there to offer support closer to home. Her parents were outstanding: her mother went out of her way to make meals tempting “and really researched the area of diet while on chemo”, while “Dad became the juicing king”. Surgery went well. A week after later she was told there were “clear margins” (no cancer) in the area around the tumour but a little evidence of activity in the lymph nodes, necessitating chemotherapy and radiotherapy. “At that stage I was just so glad that I didn’t have to have any more surgery that everything else sounded fine to me. Of course it was a little trickier in reality.” In fact, it was substantially trickier. Her oncologist, Brian Bird, acutely aware of the need to preserve full-arm mobility to allow Sarah carry on teaching violin, “really researched” her case, she says, because chemo can cause peripheral neuropathy leading to numbness and pins and needles, and he was anxious to avoid that. He did a terrific job, Sarah says. She continues to teach violin. There were many challenges on her treatment journey: the sickness brought on by the drugs, the crushing fatigue, the hair loss. She took the hair loss in her stride and found the process of choosing a wig “quite fascinating”. She decided to have her head shaved as soon as her hair started to fall out “to take some of the control back”. She had 18 sessions of radiotherapy at Cork University Hospital (CUH) which she describes as “a walk in the park” compared to chemo. She also started taking tamoxifen. It amplified the cruellest of the chemo side-effects, a chemically induced menopause. “So there were all the usual things like mood swings and bloody hot flushes”, Sarah says, but also the devastating end to dreams of ever having a family. “Of course I would have loved to have had a family but I’m here. I tend not to dwell on it too much, it is out of my control now.” Sarah has just over two years to go before receiving the final all-clear (it takes five years). Her biggest regret is not going for counselling. She coped well while treatment was ongoing but struggled when that “safety net” was taken away. “People say to you ‘you’re back to normal now’, but you’re not. It’s almost like you’re going through a grieving process, for what you were before the cancer got you. You’re supposed to feel you’ve been given a second chance but I didn’t feel it. The spectre of re-occurrence looms over you and it can be quite overwhelming.” She felt guilt that her parents, in their 70s, had to witness their daughter “lying on the couch, bald, sweating, pasty-faced”. There were some lingering physical side effects such as slight cognitive dysfunction, a little joint pain and slight nerve damage. Nonetheless, in January this year, Sarah says she “turned a corner” psychologically. “I actually feel happy now and I’m a much better person. I see and appreciate every small thing.” Unique treatment plan for patient Consultant oncologist Dr Brian Bird on treating breast cancer: “One of the really good things about my profession is assessing the unique characteristics of the patient and their disease and choosing the best possible treatment for them as an individual. I chose to give Sarah chemotherapy that is less nerve damaging than alternatives because playing music is so important to her. Sarah had HER2+ breast cancer. “These breast cancers make too much of the HER2 protein. The protein sits on the surface of cancer cells and receives signals that tell the cancer to grow and spread. About one out of every four breast cancers is HER2+. These breast cancers tend to be more aggressive and harder to treat than HER2-negative breast cancers. “However targeted treatments are very effective. They include Trastuzumab (herceptin). Herceptin works by attaching to the HER2 protein and blocking it from receiving growth signals. “So we knew Sarah needed adjuvant herceptin (trastuzumab) as well as chemo. When I was a registrar I helped to recruit Irish patients to the trials which proved herceptin stops cancer recurring in HER2+ breast cancer.” Dr Bird acknowledges that there are support issues for patients once treatment is completed. “It’s a common complaint. Across the western world, governments pay for treatment but equally it would probably be cost-effective to look at offering a greater degree of support, such as funding cognitive behavioural therapy. Exercising for 30 minutes five times a week substantially reduces the risk of breast cancer re-occurring. “Here at the Bons, if people aren’t back to themselves six months post- chemo, we offer them the a cancer fatigue manual Understanding and Managing Persistent Cancer-Related Fatigue, a very positive guide devised by St James Hospital in Dublin. We have also run survivor courses. A very small number of people may need antidepressants.” * For support contact the Irish Cancer Society (ICS) Daffodil Centre, freephone 1800200700. * To contact Cork Arc Cancer Support House log onto www.corkcancersupport.ie * October is Breast Cancer Awareness Month. To donate to the Irish Cancer Society, log onto www.cancer.ie/donate