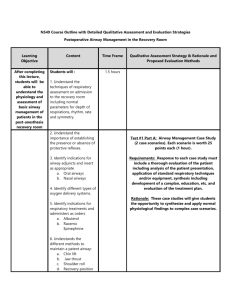
PRACTICE PARAMETER
advertisement

Redmond Emergency Medical Services Practice Parameters 08/01/2010 1 Redmond Regional EMS Practice Parameters The purpose of this document is to provide: Medical protocols regarding permissible and appropriate medical procedures and treatments to be performed by State of Georgia certified EMT-I’s and/or Paramedics (medics) in the performance of their occupational duties with Redmond Regional Medical Center. Communication protocols regarding which medical situations require direct voice communication between medics and a physician (or a nurse who is in direct contact with the physician) prior to those medics rendering specified emergency medical care. These guidelines have been adapted from the Georgia State Office of Emergency Medical Services Pre-Hospital Protocols with changes in the practice parameters based on current standards of care utilized by Redmond Regional Medical Center. Since each medical emergency must be dealt with on an individual basis and appropriate care determined accordingly, professional judgment is mandatory in determining treatment modalities within the practice parameters. The Emergency Medical Services Medical Director is responsible for reviewing and approving the practice parameters annually (or when standards of care and/or technology require a change in the practice). Medical Director Review and Approval: I have reviewed the practice parameters contained within this manual and approve their usage by EMS personnel. Date MD Printed Name MD Signature 2 Table of Contents Opening Statement 7 Using These Protocols 8 Communications Failure 9 Physician On-Scene 10 Criteria for Helicopter Transport 11 IV Therapy 12 IV Therapy – EJ Venous Cannulation 14 IV Therapy – Intraosseous Infusion 15 Medication Administration 16 Thoracic Decompression 17 Medically Assisted Intubation 19 Poisoning and Overdose Information 21 Glasgow Coma Scale 26 APGAR Scale 28 AVPU Scale 29 Average Pediatric Vital Signs 30 Common Causes of Abdominal Pain 31 Cincinnati Stroke Exam 32 Common Medical Abbreviations 33 Medication Profiles 36 Nitroglycerin Drip Chart 76 Heparin Drip Chart 77 Uniform Rules of the Road 78 Reasonable Distance Guidelines 80 3 Destination Selection for Pre-Hospital Patients 81 Pre-Hospital Withholding and Withdrawing Resuscitation 83 Hazardous Materials Exposure 86 Personal Property of Patient 87 EMTALA 89 Adult General Patient Care 90 Acute Respiratory Distress 92 Congestive Heart Failure/Pulmonary Edema 93 Acute Coronary Syndromes/STEMI 94 Altered Mental Status 96 Suspected Stroke/CVA 97 Seizures 98 Allergic Reactions/Anaphylaxis 99 Non-Traumatic Hypotension 100 Shock 101 Hypertensive Crisis 102 Hemodynamically Compromising Bradycardia 103 Stable Tachycardia 104 Unstable Tachycardia 105 Ventricular Fibrillation/Pulseless Ventricular Tachycardia 106 Asystole/Pulseless Electrical Activity 107 Environmental Cold Emergencies 108 Environmental Heat Emergencies 109 Sickle Cell Anemia 110 OB/GYN 111 4 Pregnancy Induced Hypertension 111 Vaginal Bleeding 111 Trauma in Pregnancy 111 Emergency Childbirth 112 Newborn Care 113 Post-Partum Care 113 Childbirth Complications 114 Suspected Sexual Assault 115 Suspected Abuse/Neglect 116 Psychological/Behavioral Emergencies 117 Pediatric and Adult Trauma 118 Spinal Cord Injury 120 Selective Spinal Immobilization 123 Pediatric General Patient Care 124 Pediatric Acute Respiratory Distress 125 Pediatric Altered Mental Status 126 Pediatric Seizures 127 Pediatric Shock and Hypotension 128 Pediatric Allergic Reactions 129 Pediatric Bradycardia 130 Pediatric Tachycardia 131 Pediatric Ventricular Fibrillation/Pulseless Ventricular Tachycardia 132 Pediatric Asystole/Pulseless Electrical Activity 133 Pediatric and Adult Endotracheal Intubation 134 Pain Management for Adults and Pediatric 136 5 Refusal of Services 138 Induced Hypothermia (Post-Arrest) 139 Induced Hypothermia Inclusion Criteria 140 Induced Hypothermia Exclusion Criteria 141 6 OPENING STATEMENT The following standardized treatment protocols are intended to result in improved patient care within the Redmond Regional Emergency Medical Service System. They are meant to aide in expediting patient care, and give the EMT-I and the EMT-P, guidelines with which to follow, prior to contact with Medical Control. They reflect a philosophy of patient care by which all patients should be treated. Redmond EMS and Dr. Johnson, Medical Director, developed these protocols with the goal of safe and efficient Pre-Hospital care. Patients, however, do not always fit into a “cookbook treatment” approach. Therefore, PROTOCOLS ARE NOT A SUBSTITUTE FOR GOOD CLINICAL JUDGEMENT, especially when a situation occurs which does not fit into these guidelines. As an Advanced Life Support Provider, your field treatment must be carefully balanced with the knowledge of when your capabilities fall short of what the patient needs. When treating a patient you must ask yourself, what does the patient need as opposed to what you can provide? Advanced Life Support can benefit the patient greatly by being able to quickly deliver a procedure or medication the patient needs at the scene. However, it can be detrimental to delay transportation when the patient’s needs are beyond what you can provide. 7 Using These Protocols STANDING ORDERS The following protocols have been designed for the pre-hospital professionals within Redmond Emergency Medical Service, both EMT-I's and EMT-P's may utilize some of the modalities within these standing orders; these are reflected on the following Protocols. If at any time you are unclear as to what is allowed on these protocols, ESTABLISH MEDICAL CONTROL, and the Emergency Physician will direct you. ONCE MEDICAL CONTROL HAS BEEN ESTABLISHED, WHETHER BY PHONE OR RADIO, THE EMERGENCY PHYSICIAN'S ORDERS SUPERCEDE THESE STANDING ORDERS AND PROTOCOLS, AND YOU MUST FOLLOW THE DIRECTION OF MEDICAL CONTROL AND NOT RETURN TO THESE PROTOCOLS. When following protocols, the provider should take into consideration self-administered medications within the previous hour. PATIENTS WHO REMAIN UNSTABLE AFTER STANDING ORDERS HAVE BEEN CARRIED OUT REQUIRE CONSULTATION WITH AN ON-LINE PHYSICIAN. Unstable vital signs in an adult are defined as: *Pulse of 55 or less and 120 or more *Diastolic BP of 120 or more *Systolic BP of 85 or less and 200 or more, *Respiratory rate of 10 or less and 30 or more. Specific examples of other "unstable patients" include, but are not limited to, the following: *Patients with chest pain who continue to complain of chest pain after the standing order of NITROGLYCERIN and analgesia have been administered. *Patients with shortness of breath who continue to have shortness of breath after the standing orders of LASIX or ALBUTEROL or ATROVENT have been administered. *Cardiac Arrest patients with return of pulse (even transiently). * Patients with multi-system or penetrating trauma. While the above are examples of “defined” unstable patients, you must remember to always treat the patient and not the equipment. If you always work in the best interest of the patient, you will always be on solid ground if you have to defend your actions and/or treatment decisions. PHYSICIAN OPTIONS While every attempt has been made to list the most logical Physician's Orders, medicine changes rapidly! A Medical Control Physician may ask you to do something different, because of a new development. Any time an order is given which you do not understand or seems to be contrary to established protocol, ask the physician to CONFIRM the order or to EXPLAIN it if you feel uncomfortable carrying the order out. 8 COMMUNICATIONS FAILURE If at any point a breakdown in Medical Control Communications occurs, attempt to establish it again by radio and/or telephone. If this is unsuccessful, begin transportation as soon as possible, follow the appropriate patient care protocols and attempt to contact medical control again enroute. If there is still a break in communications with Medical Control continue to follow protocol and perform any procedures necessary which are in the best interest of the patient and within your scope of practice. A breakdown in Medical Control Communications is defined as the inability to contact Medical Control due to poor radio conditions and/or poor cell phone service. If you do make contact with the receiving facility and request to speak to a Medical Control Physician and the Physician does not come to the phone or radio within an acceptable amount of time considering current circumstances for consultation, you may also consider this a breakdown in Medical Control Communications. 9 Physician on Scene The control of the scene of any emergency should be the responsibility of the individual in attendance who is the most appropriately trained in providing pre-hospital stabilization and transport. As an agent of the Medical Director of Redmond Regional Medical Center EMS, the paramedic represents that individual. Occasions will arise when a physician on the scene will desire to direct pre-hospital care. A standardized scheme for dealing with these contingencies will optimize the care given to the patient. 1. The physician desiring to assume care of the patient must: • Provide documentation of his status as a physician (MD or DO) • Be licensed to practice medicine in the State of Georgia • Document his or her assumption of care on the run report. 2. Contact with Medical Control at the receiving facility must be established as soon as possible. The physician assuming responsibility at the scene should be placed in contact with the Medical Control Physician and acknowledgement of his or her acceptance or responsibility confirmed. 3. Orders provided by the physician assuming responsibility for the patient should be followed as long as they do not, in the judgment of the paramedic, endanger patient well being. The paramedic may request the physician to attend the patient's well being. 4. If the physician's care is judged by the paramedic to be potentially harmful to the patient, the paramedic should: • Politely voice his or her objections. • IMMEDIATELY place the physician on the scene in contact with Medical Control for resolution of the problem. • When conflicts arise between the physician on the scene and Medical Control, EMS personnel should follow the directives of the Medical Control Physician. Offer no assistance in carrying out the order in question, but provide no resistance to the physician performing this care. If the physician on scene continues to carry out the order in question, offer no assistance and enlist aid from law enforcement. 5. All interactions with physicians on the scene must be completely documented in the run report. 10 Criteria for Helicopter Transport 1. Determine potential need for aero medical transport of the patient. 2. Criteria that suggest the need for aero medical transport may include, but are not limited to: • Need for ALS services where none are available or will be significantly delayed. • Mass casualty incidents. • Prolonged extrication. • Insufficient numbers of EMS personnel, equipment, or vehicles to manage a multiple casualty incident or a single patient encounter. • Traffic conditions or geographical terrain, which prohibits adequate ground access to the victim. • Situations in which the time differential between air and ground transport may substantially impact the outcome of the patient. 3. The paramedic in charge of the scene is responsible for determining if aero medical transport is warranted. He/she should notify the Communications Center of the need for aero medical transport as soon as possible in order to minimize response and transport times. The paramedic in charge should also request for assistance from other agencies as needed to help secure the incident site and landing zone. The Communications Center will advise the priority channel on which ground to air communications will occur. 4. If initial indications are that air transport may be required, the air transport should be allowed progress towards the scene in order to decrease response times. 5. Guidelines for Landing Zone Preparation are as follows: • Area should be at least 100 ft. X 100 ft. (day or night), on fairly solid ground, level, free of overhead obstructions, ground obstructions, people and any material which might fly loose. If there are obstructions, inform helicopter crew via radio. THE HELICOPTER PILOT MAKES THE FINAL DETERMINATION FOR A SAFE LANDING ZONE, (LZ) • Mark the four comers of the LZ with lights, flares or high visibility material. The best way to mark the landing position in the LZ at night is to use two vehicles with low headlights ON, shining across the LZ with the intersection of the beams at the landing point. Turn headlights OFF after landing. • Do not shine lights directly at the aircraft. • Keep spectators at least 200 feet from the touchdown area and emergency personnel at least 100 feet away. Do not allow anyone to approach the helicopter after landing. • The individual in charge of the LZ should be clearly identified day or night with either an orange vest or traffic control flashlight and must be wearing eye protection. He/she should have radio contact with the helicopter and is responsible for directional information • Once the patient is packaged and ready to load, the helicopter crew may select 2 or 3 personnel to assist loading. When approaching or departing the helicopter, be aware of the tail rotor. Remain low at all times and follow the crew's directions for safety. 11 Intravenous Therapy IV THERAPY PROCEDURES TO BE USED BY ALL EMT-I’s AND EMT-P’s INDICATIONS 1. Types of intravenous infusions used: • Volume Replacement Infusions: The general use is to replace body electrolytes or to replace fluid volume. NORMAL SALINE may be used with a macro drip (10gtt) administration set and large bore IV catheters. • Medication Line: The general use is to establish venous access in case the patient arrests or a medication is needed. NORMAL SALINE may be used with a micro drip (60gtt) administration set and in IV catheter of sufficient size to keep the vein open and give IV push medications (large bore catheters are helpful during arrests when large volumes of medications must be pushed). 2. Blood samples must be drawn on every patient prior to administration of any medications or fluids, except those in cardiac arrest or exigent circumstances. • Draw blood after the venipuncture. • Fill one of each color blood tube: purple, red, green and blue top, in that order. • After drawing hold all four tubes and gently roll them (do not shake), in order to mix preservatives. • Remove the tourniquet and start the infusion or flush the male adapter with at least 3cc flush. • Label each tube with the patients name, date and time the sample was drawn, and your initials. CONTRAINDICATIONS/PRECAUTIONS 1. Central venous cannulation is not approved in these protocols. 2. In adults, the veins of the upper extremities, external jugular veins, and intraosseous infusion are the preferred sites to be used in these protocols. For pediatric patients, IV sites include the upper and lower (below the knees) extremities, scalp, and intraosseous infusion. Only in extreme circumstances should the EMT-P deviate from these standing protocol sites, which must be documented on the PCR. 3. Patients with IV access in place may not be left unattended. If you have initiated IV access and transport your patient and the receiving facility request you send your patient through triage, you must first turn that patient over to a receiving nurse, obtain receiving signature, and then if the nurse wants the patient to go to triage, they may send them there. Infusion rates must be watched carefully to prevent over hydration or extravasations or infiltrations. 4. Prep the venipuncture site with both Povidone-iodine and isopropyl alcohol, if possible. GENERAL PROCEDURES 1. Generally, distal veins should be attempted prior to attempting access to more proximal veins. 2. Avoid placing IV's in injured extremities, if possible. 12 3. Always wear gloves when starting IV's. 4. In all cardiac patient's the right arm must be avoided, particularly, the right antecubital. Frequently these patients undergo cardiac catheterizations or thrombolysis and many Cardiologists prefer this site now, as opposed to the groin area. ("NOTE THE RIGHT ANTECUBITAL MAY BE USED ONLY AS A LAST RESORT IN THESE PATIENTS") 5. The number of IV attempts, persons attempting, site/location, catheter size, solution, time, started and infusion rate MUST be reported on the PCR. 6. While there is no maximum number of times an IV may be attempted, the amount of discomfort caused the patient must be weighed against the NEEDS of the patient. After two attempts on a patient who does not need medication "right now", consider transport. If it is a hypovolemic patient trapped in a car, it may make more sense to make more attempts. GOOD JUDGEMENT on the part of the EMT-P will supplant any thoughts of maximum attempt numbers. 7. The designated Redmond EMS training officer will be responsible for maintaining records and trends in regards to each EMT-I and EMT-P's average success rate. The training officer and the QA/QI committee will confer when it is apparent that any particular provider is presenting with a poor success rate. If a problem is found to exist, the Training Officer will meet with that particular provider along with the District Commander, and a course of action will be decided upon, as to steps to re-train the provider. 13 Intravenous Therapy External Jugular Venous Cannulation INDICATIONS The more central external jugular (EJ) vein may be cannulated in situations where peripheral sites lack perfusion. The external jugular vein runs from the angle of the jaw to under the first third of the clavicle from the sternoclavicular joint, bilaterally. Redmond EMS paramedics may use external jugular cannulation on standing protocol. CONTRAINDICATIONS / PRECAUTIONS 1. The EJ vein is more a central (although not truly central) vein than the arm veins usually used. Extra care must be taken during cannulation to prevent infection or air embolus injection, as these will cause severe complications down the road. 2. Because of the location of the EJ in relation to the pleural space, care must be taken not to cannulate the lung and produce a pneumothorax. If this happens, do not remove the catheter, refer to the Thoracic Decompression Procedure and contact Medical Control as soon as possible. PROCEDURE 1. Place the patient in a supine, head down position to fill the vein. Turn the patients head to the side opposite the side you wish to cannulate. 2. Locate the vein and cleanse the overlying skin with Povidone iodine and isopropyl alcohol. 3. Hold the vein in place by applying pressure on the vein distal to the point of entry at the angle of the jaw 4. Align the cannula in the direction of the vein with the point toward the ipsilateral nipple. 5. Tourniquet the vein lightly with one finger above the clavicle. 6. Position the catheter, bevel up, against the skin. Make the venipuncture midway between the jaw and the clavicle on the side of the EJ. 7. Note blood return, advance the catheter and withdraw the needle. Draw blood tubes and attach the infusion tubing. This should be done with a tamponade above the clavicle to avoid an air embolism. 8. Cover and dress the site in an appropriate manner and secure it and the IV tubing as necessary. 14 Intravenous Therapy Intraosseous Infusion INDICATIONS Obtaining rapid vascular access in children may be difficult. Intraosseous infusion of fluids and medications has long been regarded as a safe and effective procedure. This procedure may be performed by protocols, in extreme cases where vascular access is difficult. CONTRAINDICATIONS / PRECAUTIONS 1. The patient must be under three years of age in order to insure that the bone marrow has sufficient vasculature to handle fluid and medications. 2. Peripheral IV sites should be considered prior to intraosseous infusion because of the inherent risk of bone marrow infection. PROCEDURE 1. Select the proper IO needle. 2. Prepare the puncture with Povidone-iodine and isopropyl alcohol. IO puncture is performed on the flat, anteriomedial surface of the tibial bone of either leg, 1-3 centimeters below the tibial tuberosity. 3. Direct the needle perpendicular to the flat surface or with a slight angle toward the foot. 4. Advance the needle using firm pressure and a rotary motion. A sudden give of resistance indicates the entry into the bone marrow cavity. 5. Successful cannulation is verified by: • Give of resistance after passing through the bony cortex. • The needle standing up without support. • In most cases, the ability to aspirate bone marrow into a syringe attached to the needle. • Free flow of the infusion without infiltration. 6. Attach an infusion set and infuse as per appropriate protocol. You may need to utilize a pressure infuser if fluid does not free flow into the bone marrow cavity. 7. Secure the needle and IV tubing to the patient's leg. Monitor the puncture site frequently for signs of infiltration. 8. Any fluid and/or medication which can be administered via IV can be administered via IO without complications. 15 Medication Administration MEDICATION PROCEDURES TO BE USED BY PARAMEDICS ADMINISTRATION PROCEDURES 1. Medication may be given only: * Under one of the standing protocols listed. * On the order of any medical control MD or receiving MD either verbally or written. * By a Redmond EMS Paramedic or a Paramedic intern under the direct supervision of his/her Redmond EMS preceptor. 2. The Paramedic team leader is responsible for patient presentation, confirming orders and medication box control. 3. Medical Control will order medications in metric weight only. IF AT ANY TIME AN ORDER IS UNCLEAR, ASK THE PHYSICIAN TO REPEAT THE ORDER OR EXPLAIN IT TO YOU! 4. Three radio transmissions are necessary to confirm an order: * The physician will order the medication and dose. * The Paramedic must repeat the order back. * The Physician will acknowledge the order by giving confirmation. 5. Once the order is confirmed: * Write the order down. *Read the medication container to be sure it is the right one and check the expiration date. * Administer the medication as ordered and document the time. * Evaluate the patients' response to the medication. * WHEN ANY MEDICATIONS ARE ADMINISTERED, THEY MUST BE DOCUMENTED ON A PCR. 16 Thoracic Decompression Protocol Cook Emergency Pneumothorax Decompression Device Definitions: • Simple Pneumothorax: Air in the potential space between the visceral and parietal pleura. • Tension Pneumothorax: A true surgical emergency, air that has leaked into the space between the visceral and the parietal pleura, either from trauma or at times spontaneous, and is unable to continue to escape. It continues to enlarge, with the effect of the shift of the media stinum, creating decreased venous return, and continued respiratory compromise. Eventually left untreated may lead to the patient’s death. • Tension Hemothorax: A true surgical emergency, blood has leaked into the space between the visceral and the parietal pleura, either from trauma or at times spontaneous, and is unable to continue to escape. It continues to enlarge, with the effect of the shift of the media stinum, creating decreased venous return, and continued respiratory compromise. Eventually left untreated may lead to the patient’s death. Indications: 1. Treatment of tension pneumothorax is simple, but the complications of the procedure can be lethal. Diagnosis must be accurate and is not always easy. Field treatment is indicated when the life of the patient is in danger and treatment cannot be delayed until arrival at the hospital. 2. Field relief of tension pneumothorax is indicated ONLY when the patient has progressive severe respiratory distress with cyanosis, decreased breath sounds on the affected side, and hypotension. In addition the patient may have distended neck veins and tracheal shift away from the affected side. If the patient is intubated, there should be increasing difficulty ventilating. Hypotension can be detected by noting loss of radial pulse. Usually there will be loss of consciousness as well. Complications: 1. Hemorrhage from vessel laceration 2. Creation of a pneumothorax if one was not already present 3. Laceration of the lung 4. Infection The Cook Pneumothorax set consists of: • Straight Radiopaque Catheter • Stainless Steel Large Bore Needle • One-way stopcock valve • Connecting Tube • Heimlich Valve • 12cc Syringe • Large Alcohol Prep Pad • Povidone-lodine Swabstick • Blue Rubber Occlusive Seal If tension pneumothorax is diagnosed, and the paramedic believes the life of the patient is in immediate danger (as demonstrated by no peripheral pulses, cyanosis, and no response to verbal stimuli), then the procedure may be followed. 17 Maintain airway and administer oxygen by non-rebreather facemask at 15 L/min. Setting up and using the device: Pre-assemble the set prior to the procedure, connecting the one-way stopcock to the connecting tube and connecting it to the Heimlich Valve. Make sure you tear off enough tape, to fully secure all invasive equipment prior to beginning the procedure. The optimal insertion site of the pneumothorax catheter is in the 2nd anterior intercostal space, either to the right or left of sternum at "the level of the Angle of Louis, in the mid-clavicular line, along the superior of the 3rd rib. An alternative placement site is 4th intercostal Space, at the Anterior or mid-axillary Line, superior of the 5th rib. Prior to insertion, the site should be prepped with the antiseptic Povidone-iodine swabstick. When inserting the Cook Pneumothorax Catheter, locate your landmarks on the affected side. Insert the needle tip with the catheter as its sheath into the pleural cavity, advancing the needle and catheter. Ensure the hub of the catheter is kept open, allowing you to hear the escape of air, signaling you have entered the Pleural Cavity. Remove the inner needle checking for free flow of air, and confirm placement of the catheter tip again. When certain that the catheter is well within the Pleural Cavity, apply the blue rubber occlusive seal around the catheter, and secure it well with tape. Attach the one-way stopcock valve to the hub of the catheter with the valve open. If the catheter placement is correct, and the lung is still under tension, as air is released you will hear the Heimlich Valve make a squealing sound. Secure the entire device to the patient's thoracic area to prevent accidental dislodgement of the needle. Be sure to continuously reassess the patient's vital signs and breath sounds. If the patient's condition worsens or if complications set in, follow appropriate protocol or contact Medical Control. Warning Notes: 1. Tension pneumothorax is rare; but when present, it must be treated promptly. 2. Non-tension pneumothorax is relatively common, is not immediately life threatening and should not be treated in the field. 3. Positive pressure ventilation may lead to the development of a pneumothorax and to rapid progression to tension pneumothorax. 18 Medically Assisted Intubation Protocol The following protocol outlines procedures to be utilized when faced with a patient with a compromised airway, whether the emergency is trauma or medical related. Additionally, this protocol may only be utilized by a Redmond EMS Paramedic that has been checked off and certified competent in advanced airway management. A. Non Compromised Airway: 1. Administer oxygen as needed 2. Assist ventilation as needed B. Compromised Airway: 1. Chin lift or jaw thrust - oral/nasopharyngeal airway. 2. Assist chin lift with BVM @ 100% Oxygen. 3. Consider blind nasal intubation only if there is no evidence of maxillofacial trauma. 4. Consider the need for early intubation. C. Non-Breathing: 1. Chin lift or jaw thrust-oral/nasopharyngeal airway. 2. Hyperventilate patient 1-2 minutes prior to intubation. 3. Oral endotracheal intubation with visualization of the vocal cords. 4. Listen to breath sounds 5. Check pulse ox for significant changes. 6. Units that are equipped with Capnocheck 11 monitors shall utilize the continuous End-Tidal CO2 monitoring for all intubated patients. Patients should maintain Continuous End-Tidal CO2 levels of 35-45mmHg. 7. Units that are not equipped with Capnocheck II monitors shall utilize the Encor CO2 detector for End tidal CO2 monitoring. The Encor CO2 detector should reflect 2-5% yellow. 8. Apply tube holder and maintain cervical stabilization using: a. Back board b. Head bed device c. Spider straps 9. Confirmation of tube placement shall be done after initial intubation, after moving the patient into transport unit and upon arrival at ED. 10. Tube placement should be confirmed whenever the patient is moved. All tube confirmations shall be documented. 11. If ET intubation is unsuccessful utilize the combitube D. (MAI) Medication Assisted Intubation If unable to intubate a conscious medical or trauma patient that meets the following criteria, you may administer MAI. 1. Patient cannot maintain their airway. 2. Patient cannot protect their airway. 3. Patient cannot be appropriately ventilated with BVM or other means. 4. Patient cannot be appropriately oxygenated with BVM or other means. 5. You must intubate patient for treatment of specific condition. Adult: administer ETOMIDATE @ 20 mg IVP. A second dose of ETOMIDATE @ 20 mg IVP may be administered if the first dose is ineffective. If patient has a head injury, also administer LIDOCAINE @ 1 mg/kg IVP. Consider 5 mg VERSED for pre-sedation prior to intubation. 19 Pediatric (<5 y/o): administer ATROPINE @ 0.02 mg/kg IVP. Administer ETOMIDATE @ 0.3 mg/kg IVP. A second dose of ETOMIDATE @ 0.3 mg/kg IVP may be administered if the first dose is ineffective. If patient has a head injury, also administer LIDOCAINE @ 1 mg/kg. Consider VERSED @ 0.05 to 0.1 mg/kg for pre-sedation prior to intubation, not to exceed 5 mg. Pediatric patients over 12 years of age should be dosed as an adult. E. If unable to ventilate with BVM or combitube due to massive facial trauma or obstruction: 1. Attempt digital intubation 2. Attempt needle cricothyroidotomy X 1 3. Transport F. Consider the administration of 5 to 10 mg VERSED IVP for further sedation as needed. NOTE: Nasopharyngeal airways should never be inserted when there is any maxillofacial trauma. 20 Poisoning and Overdose Information Tricyclic Antidepressant Poisoning COMMON NAMES 1. AMITRIPTYLINE (ELAVIL, AMITRIL, ENDEP) 2. CLOMIPRAMINE (ANAFRANIL) 3. IMIPRAMINE (TOFRANIL, ANTIPRES) 4. TRIMIPRAMINE (SURMONTIL) 5. DOXEPIN (SINEQUAN, ADAPIN) 6. NORTRIPTYLINE (PAMELOR, AVENTYL) 7. DESIPRAMINE (NORPRAMINE) 8. PROTRIPTYLINE (VIVACTIL) GENERAL INFORMATION The most common lethal OD Ingestion of 15-20 mg/kg potentially fatal. Death usually occurs prehospital TCA TOXICITY 1. Anticholinergic effects 2. Cardiac toxicity - QUINIDINE-like effect 3. Peripheral alpha receptor blockade - can cause vasodilation (hypotension) ADVERSE EFFECTS 1. Anticholinergic Effects: a. Dry mouth b. Tachycardia c. Blurred vision d. Delirium e. Hyperthermia 2. Neurological Toxicity a. Confusion, agitation b. Seizures c. Hallucinations d. Coma e. Myoclonus 3. Cardiac Toxicity a. Hypotension b. ECG Changes, Dysrhythmias 4. ECG Changes a. Sinus tachycardia b. Ventricular tachycardia c. Prolongation of PR, QRS or QT intervals d. Ventricular fibrillation e. Torsades de Pointes f. Bundle branch blocks g. Junctional dysrhythmias h. AV blocks i. Asystole j. SVT 21 MARKERS OF SERIOUS TOXICITY 1. Clinical signs - most useful 2. QRS Prolongation - correlates well 3. Most patients will manifest some sign of toxicity within 2 hours of ingestion TREATMENT (FIELD MANAGEMENT) 1. Airway / IV / ECG monitor 2. Supportive care 3. Seizure treatment 4. BICARBONATE if there are signs of: a. QRS widening over 0.10 seconds b. Ventricular dysrhythmias c. Hypotension unresponsive to fluid boluses 5. If VF occurs, SODIUM BICARBONATE should be administered early in the code (after defibrillation and first round of EPINEPHRINE) 6. Hyperventilation if patient intubated Other Poisoning & Overdoses ANTIPSYCHOTIC DRUGS: PHENOTHIAZINE derivatives which may cause extrapyramidal reactions including: facial muscle twitch, full body spasm, neck muscle contraction, head deviation, occulogyrations, etc. COMPAZINE (PROCHLORPERAZINE); HALDOL (HALOPERIDOL); LOXITANE (LOXAPINE); MELLARIL (THIORIDAZINE); PROLIXIN (FLUPHENAZINE); SPARINE (PROMAZINE); STELAZINE (TRIFLUOPERAZINE); TARACTAN (CHLORPROTHIXENE); THORAZINE (CHLORPROMAZINE); TRILAFON (PERPHENAZINE); VESPRIN (TRIFLUPROMAZINE); TRICYCLIC ANTIDEPRESSANTS: May cause sudden onset of seizures and arrhythmias in overdose AVENTYL (NORTRIPTYLINE); ELAVIL, TRIAVIL, LIMBITROL (AMITRIPTYLINE); LUDIOMIL (MAPROTILINE); NORPRAMIN (DESIPRAMINE); SINEQUAN, ADAPAN (DOXEPIN); TOFRANIL (IMIPRAMINE); VIVACTIL (PROTRIPTYLINE); ASENDIN (AMOXAPINE) NARCOTIC ANALGESICS: Some of these analgesics are not true opiates yet work and react similarly. NALOXONE (NARCAN) is an effective antidote for all of these. CODEINE; COUGH SUPPRESSANT (DEXTROMETHORPHAN); DARVOCET, DARVON (PROPOXYPHENE); DEMEROL (MEPERIDINE); DILAUDID (HYDROMORPHIRIE); DOLOPHINE (METHADONE); FIORINAL (BUTALBITAL); LOMOTIL (DIPHENOXYLATE); MORPHINE; NUBAIN (NALBUPHINE); PERCODAN, PERCOCET, TYLOX (OCYCODONE); STADOL (BUTORPHANOL); SUBLIMAZE (FENTANYL); TALWIN (PENTAZOCINE); TYLENOL/CODEINE (ACETAMINOPHEN); VICODIN (HYDROCODONE); WYGESIC (PROPOXPHENE); PAREGORIC (LAUDANUM) 22 ACIDS: Caustics rust remover, metal polish. S/S: Pain, GI tract bums, lip bums, and vomiting. Treatment: Transport patient in sitting position, if possible. Caution: Do not induce vomiting. ACETAMINOPHEN: ANALGESIC TYLENOL, APAP S/S: May be no immediate s/s, but ACETAMINOPHEN is toxic to the liver, anorexia, RUQ pain, pale color, diaphoretic. Treatment: ABC's, 02, IV and fluids for hypotension, EKG, ACTIVATED CHARCOAL 50 gm orally. ALKALIS & CAUSTICS: Drano, drain & oven cleaners, bleach. S/S: Epigastric pains, GI tract chemical burns, lip burns, vomiting. Treatment: Prevent aspiration. Transport patient in sitting position, if possible. Caution: Do not induce vomiting. AMPHETAMINES & STIMULANTS: Stimulant methamphetamines, speed, crank. S/S: Anxiety, tachycardia, diaphoresis, seizures, lethal cardiac arrhythmias, HA, palpitations, CV A, HTN crisis, hyperthermia, dilated pupils, dry mouth. Treatment: ABCs, 02, EKG, IV fluids for hypotension. ACTIVATED CHARCOAL 50 gm orally. Keep patient cool. DIAZEPAM as adjunct. ANTIDEPRESSANTS: Mood elevators ELAVIL, TRIAVIL, SINEQUAN, AMITRIPTYLINE. S/S: Hypotension, PVC's, cardiac arrhythmias, QRS complex widening, seizures, coma, and death. Treatment: ABC, 02, IV, EKG, IV fluids, SODIUM BICARBONATE, intubate and hyperventilate. Caution: Onset of coma and seizures can be sudden. ASPIRIN: ANALGESIC BAYER, ASA, SALICYLATES S/S: GI bleeding, LUQ pain, pale color, diaphoresis, shock, ringing in the ears, hyperpnea. Treatment: ABC, 02, IV, EKG, fluids for hypotension, ACTIVATED CHARCOAL 50gm orally. BARBITURATES: Sedatives. Hypnotic Phenobarbital, barbs, downers. S/S: Weakness, drowsiness, respiratory depression, apnea, coma, hypotension, bradycardia, hypothermia, pulmonary edema, death. Treatment: ABCs, 02, ventilate, IV fluids for hypotension. Caution: protect the patient's airway. CARBON MONOXIDE: odorless toxic gas from any source of incomplete combustion IE: car exhaust, fire suppression, and stoves. S/S: HA, dizziness, DOE, fatigue, tachycardia, visual disturbances, hallucinations, cherry red skin color, decreased respirations, cyanosis, ALOC, coma, blindness, hearing loss, convulsions, others in household with same symptoms. Treatment: Remove patient from toxic environment, ABCs, 02, transport. Hyperbaric treatment in severe cases. Caution: Protect yourself from exposure. COCAINE: Stimulant/anesthetic coke, snow, flake, crack. S/S: HA, decreased respirations, decreased temp, agitation, tachycardia, cardiac arrhythmias, chest pain, AMI, HTN, seizure, vomiting, hyperthermia, paralysis, coma, dilated pupils, death. 23 Acute pulmonary edema can occur with IV use. Treatment: ABCs, 02, IV, DIAZEPAM for seizures, ET Intubation, LIDOCAINE for PVC's, cool patient, if hyperthermic. Note: A "speedball" is cocaine & heroin. HALLUCINOGENS: Alter perception LSD, psilocybin mushrooms. S/S: Anxiety, hallucinations, panic, disorientation, paranoia. Treatment: ABC's, Supportive reassurance. Caution: Watch for violent or unexpected behavior. HYDROCARBONS: Fuels, gasoline, oil, and petroleum products. S/S: Breath odor, SOB, seizures, acute pulmonary edema, coma, bronchospasm. Treatment: ABCs, 02, gastric lavage. Caution: Do not induce vomiting. MUSHROOMS: Amanita Deadly mushroom Death Angel S/S: Seizures, death. Treatment: ABCs, 02, IV, DIAZEPAM for seizures. Caution: Protect the patient's airway. OPIATES: NARCOTIC ANALGESIC, DILAUDID, HEROIN, MORPHINE, CODEINE S/S: Decreased respirations, apnea, decreased BP, coma, bradycardia, pinpoint pupils, vomiting, and diaphoresis. Treatment: ABC, 02, ventilate, intubate, IV fluids for hypotension, NALOXONE 2 mg IV, IM, ET, or IO. Caution: Consider other concurrent overdoses. PCP - PHENCYCLIDINE: Tranquilizer Peace Pill, angel dust, horse tranquilizer S/S: Nystagmus (constant involuntary movement of the eyeball), disorientation, HTN, hallucinations, catatonia, sedation, paralysis, stupor, mania, tachycardia, dilated pupils, status epilepticus. Treatment: ABC, 02, vitals, IV, EKG. Caution: Protect yourself against violent patient. Be aware of possible trauma due to anesthetic effect of PCP. TRANQUILIZERS (MAJOR): Antipsychotic HALDOL, NAVANE, THORAZINE, COMPAZINE S/S: EPS, dystonias, painful muscle spasms, respiratory depression, hypotension, Torsades de Pointes. Treatment: 50 mg DIPHENHYDRAMINE for EPS. ABCs, 02, vitals, EKG. Consider ACTIVATED CHARCOAL 50gm orally. IV fluids for hypotension. Consider intubation for the unconscious patient. Caution: Protect the patient's airway. TRANQUILIZERS (MINOR): ANXIOLYTICS (anti anxiety) VALIUM, XANAX, LIBRIUM, DIAZEPAM, MIDAZOLAM S/S: Sedation, weakness, dizziness, tachycardia, hypotension, hypothermia. Treatment: ABCs, monitor vitals, IV. Caution: Coma means some other substance or cause is also involved. OD is almost always in combination with other drugs. Protect the patient's airway. 24 ECSTASY: (methylenedioxymethamphetamine): XTG, wonder drug, and X S/S: Feelings of detachment, loss of drives such as hunger, sleep, and sexual, muscle tension, sweating or chills, tremors, blurred vision, rapid eye movements, hypertension, increased heart rate, dehydration, nausea, fainting, and death. Treatment: ABC's, calm patient GHB: Gamma-Butryolactone G, Georgia Home Boy, Liquid Ecstasy S/S: Drowsiness, dizziness, ataxia (uncoordination), and clonic movements have been observed during GHB induced sleep, orthostatic hypotension, high doses induce sedation, and loss of consciousness, and can induce cardiac and respiratory depression, loss of reflexes. Patient may need continued stimuli to remember to breath. Treatment: ABC, monitor airway, 02, assist ventilations as needed, IV, EKG, pulse oximetry 25 Glasgow Coma Scale ADULT Eye Opening: Spontaneous – 4 To Voice – 3 To Pain – 2 None – 1 Verbal Response: Oriented – 5 Confused – 4 Inappropriate – 3 Incomprehensible – 2 None – 1 Motor Response: Obeys Commands – 6 Localizes – 5 Withdraws – 4 Flexion – 3 Extension – 2 None – 1 PEDIATRIC (AGE 4 TO ADULT) Eye Opening: Spontaneous – 4 Verbal Command – 3 To Pain – 2 None – 1 Verbal Response: Oriented and Converses – 5 Disoriented and Converses – 4 Inappropriate – 3 Incomprehensible – 2 None – 1 Motor Response: Obeys Commands – 6 Localizes – 5 Withdrawal – 4 Flexion Withdrawal – 3 Flexion Abnormal – 2 None – 1 26 PEDIATRIC (BIRTH TO AGE 4) Eye Opening: Spontaneous – 4 Reaction to Speech – 3 Reaction to Pain – 2 None – 1 Verbal Response: Smiles, Oriented to Sound, Interacts Appropriately – 5 Crying but Consolable, Interacts Inappropriately – 4 Crying and Inconsistently Inconsolable, Interacts Restlessly – 3 Crying and Inconsolable, Interacts Restlessly – 2 None – 1 Motor Response: Spontaneous – 6 Localized Pain – 5 Withdraws in Response to Pain – 4 Abnormal Flexion – 3 Abnormal Extension – 2 None – 1 27 APGAR Scale A – Appearance 0 Points – Blue/Pale 1 Point – Body Pink, Extremities Blue 2 Points – Fully Pink P – Pulse 0 Points – Absent 1 Point - <100 2 Points - >100 G – Grimace 0 Points – No Response 1 Point – Grimace 2 Points – Cough, Sneeze A – Activity 0 Points – Limp 1 Point – Some Flex 2 Points – Active Motion R – Respiration 0 Points – Absent 1 Point – Slow 2 Points – Strong Cry *APGAR Score should be calculated at 1 minute and 5 minutes. 28 AVPU Scale ADULT A – Alert V – Responds to Verbal Stimuli P – Responds to Painful Stimuli U – Unresponsive CHILD A – Alert/Aware of Surroundings V – Opens Eyes P – Withdraws from Pain U – No Response INFANT A – Curious/Recognizes Parents V – Irritable/Cries P – Cries in Response to Pain U - Unresponsive 29 Average Pediatric Vital Signs NEONATE: Respiratory Rate – 60 Blood Pressure – 80/46 Pulse Rate – 110 to 150 Weight – 6.6 pounds 3 MONTHS: Respiratory Rate – 40 Blood Pressure – 89/60 Pulse Rate – 110 to 140 Weight – 11 pounds 6 MONTHS: Respiratory Rate – 30 Blood Pressure – 89/60 Pulse Rate – 110 to 140 Weight – 16.5 pounds 1 YEAR: Respiratory Rate – 25 Blood Pressure – 89/60 Pulse Rate – 110 to 140 Weight – 22 pounds 2 YEARS: Respiratory Rate – 20 Blood Pressure – 96/84 Pulse Rate – 90 to 100 Weight – 27.5 pounds 3 YEARS: Respiratory Rate – 20 Blood Pressure – 100/70 Pulse Rate – 80 to 120 Weight – 33 pounds 4 YEARS: Respiratory Rate – 20 Blood Pressure – 100/70 Pulse Rate – 80 to 100 Weight – 39.6 pounds 6 YEARS: Respiratory Rate – 20 Blood Pressure – 100/56 Pulse Rate – 80 to 100 Weight – 55 pounds 30 Common Causes of Abdominal Pain Epigastric: AMI, gastroenteritis, ulcer, diagram esophageal disease, heartburn. RUQ: Liver, gall bladder, kidney large intestine. Gall stones, hepatitis, liver disease, pancreatitis, appendicitis, perforated duodenal ulcer, AMI, pneumonia. LUQ: Spleen, liver, kidney, pancreas, large intestine. Gastritis, pancreatitis, AMI, pneumonia. LLQ: Small intestine, ovary uterus, large intestine. Ruptured ectopic pregnancy, diverticulitis, ovarian cyst, PID, kidney stones, enteritis, abdominal abscess. RLQ: Appendix, Bladder, large intestine, ovary, uterus. Appendicitis, rupture ectopic pregnancy, enteritis, abdominal abscess, PID, diverticulitis, ovarian cyst, kidney stones, strangulated hernia. Midline: bladder infection, aortic aneurysm, uterine disease, intestinal disease, early appendicitis. Diffuse Pain: pancreatitis, peritonitis, appendicitis, gastroenteritis, dissecting/rupturing aortic aneurysm, diabetes, ischemic bowel, sickle cell crisis 31 Cincinnati Stroke Exam FACIAL DROOP- Have the patient show teeth or smile. a. Normal- both sides of the face move equally. b. Abnormal- one side of the face does not move as well as the other side. ARM DRIFT- Have the patient close his or her eyes and hold both arms straight out for 10 seconds. a. Normal- both arms move the same or both arms do not move at all (other signs such as pronator grip may be beneficial). b. Abnormal- one arm does not move or one arm drifts down compared with the other. ABNORMAL SPEECH - Have the patient say "you can't teach an old dog new tricks". a. Normal- patient uses correct words with no slurring. b. Abnormal- patient slurs words, uses the wrong words, or is unable to speak. *Finger to nose and or heel to shin testing typically abnormal **Decreased level of consciousness with headache and stiff neck are typical; this syndrome without associated focal neurologic deficits is most consistent with subarachnoid hemorrhage. With intracerebral, focal deficits may occur. Left Hemisphere Deficits: Arm Droop – right arm drift (weakness) Facial Droop – right sided facial droop Speech – aphasia, wrong or inappropriate speech Right Hemisphere Deficits: Arm Droop – left arm drift (weakness) Facial Droop – left sided facial droop Speech – says statements correctly Brainstem: Arm Droop – may have bilateral drift (weakness) Facial Droop – may have bilateral facial droop Speech – dysarthria slurring Cerebellum: Arm Droop – no drift Facial Droop – no facial droop Speech – says statements correctly Hemorrhage: Arm Droop – no drift Facial Droop – no facial droop Speech – says statements correctly but slowly (often sleepy) 32 Common Medical Abbreviations ABC: airway, breathing, circulation ABD: abdominal ADD: attention deficit disorder ALS: advanced life support AMA: against medical advice AMI: acute myocardial infarction Amp: ampule/one dose A/P: anterior/posterior APAP: acetaminophen ASA: aspirin AT: atrial tachycardia AV: atrioventricular BICARB: Sodium Bicarbonate BID: twice a day BIL: bilateral BLS: basic life support BP: blood pressure CA: cancer CAD: coronary artery disease CC or c/c: chief complaint cc: cubic centimeter CCU: coronary care unit CHB: complete heart block CHF: congestive heart failure CLR: clear cm: centimeter CNS: central nervous system c/o: complains of CO: carbon monoxide CO2: carbon dioxide COPD: chronic obstructive pulmonary disease CP: chest pain CPR: cardio-pulmonary resuscitation CSF: cerebral spinal fluid CSM: circulation/sensory/motor CVA: cerebral vascular accident cx: chest D/C: discontinue DL: deciliter (1/10 of a liter, 100 ml) DOA: dead on arrival D5W: 5% dextrose in water Dx: diagnosis ED: emergency department EKG/ECG: electrocardiogram Epi: epinephrine EPS: extra pyramidal symptoms ET: endotracheal ETOH: alcohol 33 fib: fibrillation fl: fluid FROM: full range of motion fx: fracture GI: gastrointestinal gm: gram gr: grain gt(t): drop(s) h, hr: hour HA: headache HADD: hyperactive attention deficit disorder HTN: hypertension hx: history ICP: intracranial pressure ICU: intensive care unit IM: intramuscular IN: intranasal IO: intraosseous IV: intravenous IVP: intravenous push Kg: kilogram KVO: keep vein open L: liter LPM: liter per minute LOC: level of consciousness/loss of consciousness (depending on context) LR: lactated ringers LS: lung sounds MD: medical doctor mEq: milliequivalents mg: milligram MI: myocardial infarction min: minute ml: milliliter mm: millimeter MOE: moves all extremities MS: morphine sulfate NaCL: sodium chloride NaHCO3: sodium bicarbonate NAD: no apparent distress NG, N/G: naso gastric NPO: nothing by mouth NS: normal saline NSR: normal sinus rhythm NTG: nitroglycerine N/V: nausea/vomiting N/V/D: nausea/vomiting/diarrhea O2: oxygen OB: obstetrics OD: overdose OR: operating room PAC: premature atrial contraction 34 PAT: paroxysmal atrial tachycardia PCN: penicillin PCR: patient care report PE: physical exam or pulmonary edema pedi: pediatric PERL: pupils, equal, reactive to light PJC: premature junctional contraction po: by mouth prn: when necessary PTA: prior to arrival PVC: premature ventricular contraction QID: four times a day R/O: rule out RN: registered nurse Rx: prescription medication SC: subcutaneous sec: second SL: sublingual SIVP: slow intravenous push SNT: soft, non-tender SOB: shortness of breath STAT: immediately s/s: signs/symptoms SVT: supraventricular tachycardia Sx: symptoms Sz: seizure TB: tuberculosis TCA: tricyclic antidepressant TIA: transient ischemic attack TID: three times a day TKO: to keep open U/A: upon arrival UTI: urinary tract infection VF: ventricular fibrillation VT: ventricular tachycardia WNL: within normal limits W/O: wide open X: times y/o: years old 35 Medication Profiles Below is a list of the medications that Redmond Regional Emergency Medical Services currently utilize. This list may be updated as medications are added or deleted from our inventory. After the list of medications, you will find a profile for each medication. ACETAMINOPHEN ADENOCARD (ADENOCARD®) ALBUTEROL SULFATE (VENTOLIN®, PROVENTIL®) AMIODARONE (CORDARONE®) ASPIRIN ATROPINE SULFATE CALCIUM CHLORIDE CLONIDINE HYDROCHLORIDE (CATAPRES®) DEXTROSE (D50, D25, D10) DIAZEPAM (VALIUM®) DILTIAZEM (CARDIZEM®) DIPHENHYDRAMINE (BENADRYL®) DOPAMINE (INOTROPIN®) EPINEPHRINE, EPI-PEN, EPI-PEN JR. (ADRENALINE®) ETOMIDATE (AMIDATE®) FLUMAZENIL (ROMAZICON®) FUROSEMIDE (LASIX®) GLUCAGON HALOPERIDOL (HALDOL®) HEPARIN SODIUM IBUPROFEN IPRATROPIUM BROMIDE (ATROVENT®) KETOROLAC (TORADOL®) LIDOCAINE (XYLOCAINE®) MAGNESIUM SULFATE MEPERIDINE (DEMEROL®) METHYLPREDNISOLONE (SOLU-MEDROL®) METOPROLOL (LOPRESSOR®) MIDAZOLAM HYDROCHLORIDE (VERSED®) MORPHINE SULFATE NALOXONE (NARCAN®) NITROGLYCERIN ODANSETRON HYDROCHLORIDE (ZOFRAN®) PHENYLEPHRINE (NEO-SYNEPHRINE®) SPRAY PROMETHAZINE (PHENERGAN®) SODIUM BICARBAONATE TETRACAINE OPTHALMIC DROPS THIAMINE (BETAXIN®) VASOPRESSIN 36 ACETAMINOPHEN Description/Mechanism: Acetaminophen is a synthetic, non-opiate, centrally acting analgesic and antipyretic agent. Indications: Treats minor pain and reduces fever. Contraindications: Do not use in patients that have a hypersensitivity to acetaminophen. Adverse Reactions: Allergic reaction; bloody stools or black, tarry stools; dark colored urine; light-headedness; fainting; sweating; weakness; nausea and/or vomiting; loss of appetite; severe stomach pain; unusual bleeding or bruising; vomiting blood or coffee-ground emesis; yellowing of the skin or eyes. 37 ADENOSINE (ADENOCARD®) Description/Mechanism: Adenosine is primarily formed from the breakdown product of adenosine triphosphate (ATP). Both compounds are found in every cell of the human body, and have a wide range of metabolic roles. Its actions in the AV node are thought to act through stimulation of specific adenosine receptors. Adenosine slows those tachycardias associated with the AV node (i.e. AV Node Re-entry Tachycardias) by decreasing conductivity through the node. Specifically, activation of A1 receptors in the AV node activates an inward potassium channel and inactivation of inward slow calcium channels that result in membrane hyperpolarization. This decreases the speed of AV node conduction and increases the AV node refractory period. Although there are adenosine receptors in most every cell, includes those of the sinus pacemakers, there is no clinical effect of the drug on tachycardias originating outside the AV node such as sinus tachycardia, atrial fibrillation or atrial flutter. Onset: Within 30 seconds Duration: Approximately 10 seconds Indications: Conversion of PSVT (including those associated with WPW) to sinus rhythm Contraindications: Hypersensitivity to adenosine; second or third degree block or sick sinus syndrome Adverse Reactions: Light-headedness; hypotension; paresthesia; shortness of breath; headache; transient periods of sinus bradycardia or ventricular ectopy; palpitations; chest pain; nausea 38 ALBUTEROL SULFATE (VENTOLIN®, PROVENTIL®) Description/Mechanism: Primarily beta 2 -selective sympathomimetic. Relaxes smooth muscle of the bronchial tree and peripheral vasculature. Activates cAMP via a non-beta receptor mechanism. For this reason, it is sometimes used in betablocker overdoses. It also activates the Na-K pump by the same mechanism which is useful in treating hyperkalemia. Onset: 5 to 15 minutes after inhalation Duration: 3 to 4 hours after inhalation Indications: Relief of bronchospasm; beta-blocker overdose; hyperkalemia Contraindications: tachycardia Hypersensitivity to albuterol; cardiac dysrhythmias associated with Adverse Reactions: Adverse reactions are usually dose related; restlessness; dizziness; apprehension; palpitations; increase in blood pressure; dysrhythmias 39 AMIODARONE (CORDARONE®) Description/Mechanism: Prolongs duration of action potential and effective refractory period, also provides noncompetitive a- and b- adrenergic inhibition. Decreases AV conduction velocity and sinus node function. Onset: Within minutes after IV administration Duration: Days (not firmly established) Indications: VF, unstable VT and SVT refractory to other therapy. Trials underway or recently completed indicated amiodarone is an effective first line medication for VT/VF in cardiac arrest. Contraindications: None in cardiac arrest with VF or VT. High degree AV blocks, sinus node dysfunction and marked bradycardia. Adverse Reactions: Hypotension; bradycardia 40 ASPIRIN Description/Mechanism: Powerfully inhibits platelet aggregation by inhibiting thrombonxane A2 production. Major actions appear to be associated primarily with inhibiting the formation of prostaglandins involved in the production of inflammation, pain and fever. Lowers body temperature by indirectly causing centrally mediated peripheral vasodilation and sweating. Onset: Approximately 15 minutes Duration: 2 to 4 hours Indications: Acute myocardial infarction/injury; relieve pain of low to moderate intensity; inflammatory conditions; reduce fever; prevent recurrence of MI or TIA Contraindications: Hypersensitivity to salicylates; history of GI ulcerations; history of hemophilia or other bleeding disorders; pregnancy or children under 2 years of age Adverse Reactions: Dizziness, confusion; tinnitus; hearing loss; nausea; heartburn; stomach pains 41 ATROPINE SULFATE Description/Mechanism: Atropine sulfate is a potent parasympatholytic. It inhibits actions of acetylcholine at postganglionic parasympathetic neuroeffector sites, primarily at muscarinic receptors. Small doses inhibit salivary and bronchial secretions, moderate doses dilate pupils and increase heart rate. Large doses decrease GI motility, inhibit gastric acid secretion. Blocked vagal effects result in positive chronotropy and positive dromotropy (limited or no inotropic effect). In emergency care, it is primarily used to increase the heart rate in life-threatening bradycardias. You can think of the effects of atropine as being 'anti-SLUDGE'. Onset: Rapid Duration: 2 to 6 hours Indications: Hemodynamically significant bradycardia; asystole; PEA (ventricular rate <60); organophosphate poisoning; pre-treatment for pediatric patients receiving RSI Contraindications: Hypersensitivity to Atropine Sulfate; tachycardia; unstable cardiovascular status in acute hemorrhage with myocardial ischemia Adverse Reactions: tachycardia; palpitations; dysrhythmias; headache; dizziness; nausea/vomiting; flushed and dry skin; dry mouth/nose; photophobia; blurred vision; urinary retention; possible paradoxical bradycardia when pushed slowly or at doses less than 0.5 mg. 42 CALCIUM CHLORIDE Description/Mechanism: Calcium is an essential component for functional integrity of the nervous and muscular systems, for normal cardiac contractility and the coagulation of blood. Calcium chloride contains 27.2% elemental calcium. Calcium chloride is a hypertonic solution and should only be administered intravenously slowly. Onset: 5 to 15 minutes Duration: Dose dependent but effects may last up to 4 hours after IV administration Indications: Hyperkalemia; hypocalcemia (eg. after multiple blood transfusions, dialysis); calcium channel blocker toxicity; hypermagnesemia; prevention of hypotensive effects of calcium channel blocking agents (eg. Verapamil/Diltiazem via IV) Contraindications: VF during cardiac resuscitation; hypercalcemia; digitalis toxicity Adverse Reactions: Decreases in heart rate (may cause asystole); decrease in blood pressure; metallic taste; severe local necrosis following IM administration or IV infiltration 43 CLONIDINE HYDROCHLORIDE (CATAPRES®) Description/Mechanism: Stimulates central alpha-adrenergic receptors to inhibit sympathetic cardioaccelerator and vasoconstrictor centers. Onset: 30 to 60 minutes Duration: 8 hours to several days Indications: Management of hypertension Contraindications: Hypersensitivity to clonidine; patients on anticoagulant therapy; patients with a bleeding diathesis Adverse Reactions: Dry mouth; drowsiness; constipation; sedation; fatigue; headache; lethargy; insomnia; dizziness, impotence; change in taste, nervousness; rash 44 DEXTROSE (D50, D25, D10) Description/Mechanism: The term "dextrose" is used to describe the six carbon sugar dglucose, the principal form of carbohydrate utilized by the body for energy production. D50 is used in emergency care to treat hypoglycemia, and in the management of coma of unknown origin. Onset: Less than 1 minute Duration: Depends on degree of hypoglycemia Indication: Hypoglycemia; refractory cardiac arrest (controversial) Contraindications: Intracranial bleeding; increased intracranial pressure; known or suspected CVA in absence of hypoglycemia Adverse Reactions: Warmth; pain; burning from medication infusion; thrombophlebitis 45 DIAZEPAM (VALIUM®) Description/Mechanism: Diazepam is a frequently prescribed medication to treat anxiety and stress. In emergency care, it is used to treat alcohol withdrawal and grand mal seizure activity. Diazepam potentiates the effects of inhibitory neurotransmitters (GABA), hyperpolarizing the membrane potential and raising the seizure threshold in the motor cortex. It may also be used in conscious patients during cardioversion and TCP to induce amnesia and sedation. Though the drug is still widely used as an anticonvulsant because of its fast action, it is actually a relatively weak anticonvulsant because of its short duration. Rapid IV administration may be followed by respiratory depression and excessive sedation. Onset: IV - rapid; IM - 15 to 30 minutes; ET – rapid Duration: 15 minutes to 1 hour Indications: Acute anxiety states; acute alcohol withdrawal; sedation; seizure activity; premedication prior to cardioversion or TCP Contraindications: Substance abuse; coma; shock; hypersensitivity to the drug Adverse Reactions: Hypotension; reflex psychomotor impairment; confusion; nausea 46 tachycardia; respiratory depression; ataxia; DILTIAZEM (CARDIZEM®) Description/Mechanism: Diltiazem is a calcium channel blocking agent that slows conduction, increases refractoriness in the AV node, and causes coronary vasodilation. The drug is used to control ventricular response rates in patients with atrial fibrillation, atrial flutter, multifocal atrial tachycardia and PSVT. Onset: 2 to 5 minutes Duration: 1 to 3 hours Indications: Atrial fibrillation; atrial flutter; PSVT; multifocal atrial tachycardia Contraindications: Sick sinus syndrome; second or third degree AV block; WPW or other preexcitation syndrome; VT or other wide complex tachycardia of unknown origin; severe hypotension; sensitivity to diltiazem; concomitant use of IV beta blockers Adverse Reactions: Atrial flutter; first and second degree AV block; bradycardia; chest pain; congestive heart failure; syncope; ventricular dysrhythmias; sweating; nausea/vomiting; dizziness; dry mouth; dyspnea; headache 47 DIPHENHYDRAMINE (BENADRYL®) Description/Mechanism: An antihistamine with significant anticholinergic effects and a high incidence of drowsiness. Competes for H1 receptors on effector cells thus blocking effects of histamine release. Effects in Parkinsonism and drug-induced extrapyramidal symptoms are apparently related to its ability to suppress central cholinergic activity and to prolong action of dopamine by inhibiting its reuptake and storage. Diphenhydramine does not affect H2 receptors and therefore has no effect on gastric acid secretion. Onset: Maximal effect in 1 to 3 hours Duration: 6 to 12 hours Indications: Allergic reactions; anaphylaxis; acute extrapyramidal reactions Contraindications: Acute asthma; CNS depression; patients taking MAO inhibitors; hypersensitivity to the drug Adverse Reactions: Dose related drowsiness; sedation; disturbed coordination; hypotension; palpitations; tachycardia; bradycardia; thickening of bronchial secretions; dry mouth or throat 48 DOPAMINE (INOTROPIN®) Description/Mechanism: The essential amino acid tyrosine is converted to L-DOPA and then to dopamine. It is then converted to norepinephrine and then to epinephrine. It acts primarily on alpha 1, beta 1 adrenergic receptors in dose-dependent fashion. At low doses ("renal doses"), dopamine has a dopaminergic effect that causes renal, mesenteric, and cerebral vascular dilation. At moderate doses ("cardiac doses"), dopamine has beta 1 adrenergic effect, causing enhanced myocardial contractility, increased cardiac output, and a rise in blood pressure. At high doses ("vasopressor doses"), dopamine has an alpha 1 adrenergic effect, producing peripheral arterial and venous constriction. Dopamine is commonly used in the treatment of hypotension associated with cardiogenic shock. Onset: 2 to 4 minutes Duration: 10 to 15 minutes after cessation of infusion Indications: Hemodynamically significant hypotension in the absence of hypovolemia Contraindications: VT/VF; hypovolemia; patients with pheochromocytoma Adverse Reactions: dose related tachydysrhythmias; hypertension; increased myocardial oxygen demand 49 EPINEPHRINE, EPI-PEN, EPI-PEN JR. (ADRENALINE®) Description/Mechanism: Epinephrine stimulates alpha, beta 1 and beta 2 adrenergic receptors in dose-related fashion. Rapid injection produces a rapid increase in blood pressure, ventricular contractility, and heart rate. In addition, epinephrine causes vasoconstriction in the arterioles of the skin and mucosa. It antagonizes the effects of histamine by decreasing its release and decreasing membrane permeability. Onset: IM – 5 to 10 minutes; IV or ET – 1 to 2 minutes Duration: 5 to 10 minutes Indications: Bronchoconstriction; anaphylaxis; all forms of cardiac arrest; profound symptomatic bradycardia Contraindications: insufficiency Hypersensitivity to the drug; hypovolemic shock; hypertension; coronary Adverse Reactions: Headache; nausea; restlessness; weakness; dysrhythmias; hypertension; precipitation of angina pectoris 50 ETOMIDATE (AMIDATE®) Description/Mechanism: A hypnotic drug without analgesic properties. Onset: Usually within 1 minute Duration: Dose dependent but usually 3 to 5 minutes with normal dose Indications: Induction of general anesthesia Contraindications: Hypersensitivity to the drug Adverse Reactions: Hyperventilation; hypoventilation; apnea of short periods (usually 5 to 90 seconds with spontaneous recovery); laryngospasm; hiccup and snoring indicative of upper airway obstruction; hypertension; hypotension; cardiac dysrhythmias 51 FLUMAZENIL (ROMAZICON®) Description/Mechanism: Flumazenil antagonizes the actions of benzodiazepines on the central nervous system. It has been shown to antagonize sedation, impairment of recall, and psychomotor impairment produced by benzodiazepines. Flumazenil does not antagonize CNS effects of ethanol, barbiturates or opioids. Onset: 1 to 2 minutes Duration: Generally less than that of the benzodiazepine Indication: Reversal of benzodiazepine sedation Contraindications: Overdose of unknown substances; underlying dependence benzodiazepines; cyclic antidepressant overdose; hypersensitivity to drug or benzodiazepines of Adverse Reactions: Nausea/Vomiting; dizziness; agitation; injection-site pain; cutaneous vasodilation; abnormal vision; seizures 52 FUROSEMIDE (LASIX®) Description/Mechanism: Furosemide is a potent diuretic that inhibits the reabsorption of sodium and chloride in the proximal tubule and loop of Henle. Onset: Diuretic effects within 15 to 20 minutes and vasodilatory effects within 5 minutes when given IV Duration: 4 to 6 hours Indications: Cardiogenic pulmonary edema; congestive heart failure Contraindications: Anuria; hypersensitivity to the drug; hypovolemia/dehydration; known hypersensitivity to sulfonamides; states of severe electrolyte depletion Adverse Reactions: Hypotension; dry mouth; hypochloremia; hypokalemia; hyponatremia; hyperglycemia; tinnitus if given too rapidly 53 GLUCAGON Description/Mechanism: Glucagon is a protein secreted by the alpha cells of the pancreas. When released, it results in blood glucose elevation by increasing the breakdown of glycogen to glucose and inhibiting glycogen synthesis. The drug is only effective in treating hypoglycemia when the patient has adequate stored glycogen. In addition, glucagon exerts positive inotropic action on the heart and decreases renal vascular resistance. It is, therefore, also used in managing patients with beta-blocker cardiotoxicity. Onset: Within 1 minute Duration: 9 to 17 minutes Indications: Hypoglycemia with altered level of consciousness; beta blocker overdose Contraindications: Hypersensitivity to the drug Adverse Reactions: Tachycardia; hypertension; nausea/vomiting 54 HALOPERIDOL (HALDOL®) Description/Mechanism: Potent, long-acting butyrophenone derivative with pharmacologic actions similar to those of phenothiazines but with higher incidence of extrapyramidal effects and less hypotensive and relatively low sedative activity. Exerts strong antiemetic effect and impairs central thermoregulation. Produces weak central anticholinergic effects and transient orthostatic hypotension. Onset: IV – 10 to 20 minutes; IM – 30 to 60 minutes Duration: 12 to 24 hours Indications: Acute psychotic episode Contraindications: CNS depression; coma; pregnancy; hypersensitivity to the drug Adverse Reactions: Orthostatic hypotension; nausea/vomiting; allergic reactions; blurred vision; dose related pseudoparkinsonism; dose related akathisia; dose related dystonias 55 HEPARIN SODIUM Description/Mechanism: Exerts a direct effect on blood coagulation by binding with and enhancing the actions of antithrombin III (heparin cofactor). Antithrombin III binds with and inactivates excess thrombin in order to limit the spread of regionalized clotting activity. By decreasing the amount of available thrombin, fibrinogen is prevented from converting to fibrin and new clots are not made. The antithrombin III-heparin complex is ~1000 X as effective as antithrombin III alone. Heparin does not lyse already existing thrombi (and is therefore NOT a thrombolytic) but may prevent their extension and propagation. Onset: Less than 1 minute via IV Duration: 4 to 8 hours Indication: Acute myocardial infarctions; unstable angina Contraindications: Hypersensitivity to the drug; active bleeding; recent intracranial, intraspinal, or eye surgery; severe hypertension; bleeding tendencies Adverse Reactions: Allergic reaction; hemorrhage; thrombocytopenia 56 IBUPROFEN Description/Mechanism: Ibuprofen tablets contain Ibuprofen which possesses analgesic and antipyretic activities. Its mode of action, like that of other NSAIDs, is not completely understood, but may be related to prostaglandin synthetase inhibition Onset: 15 to 30 minutes Duration: 4 to 6 hours Indications: Used for mild to moderate pain relief; patients with fever Contraindications: Hypersensitivity to the drug Adverse Reactions: Nausea/vomiting; epigastric pain; diarrhea; abdominal distress; heartburn; dizziness; headache; nervousness; rash; tinnitus; decreased appetite 57 IPRATROPIUM BROMIDE (ATROVENT®) Description/Mechanism: Atrovent is an anticholinergic. It works by relaxing and opening bronchial tubes (air passages in the lungs), making it easier to breath. Onset: Up to 1 hour Duration: 4 to 6 hours Indications: Treating and preventing bronchospasm (wheezing or difficulty breathing) associated with chronic obstructive pulmonary disease, including chronic bronchitis and emphysema. It can be used alone or with certain other medications. Contraindications: Hypersensitivity to Atrovent; hypersensitivity to soy lethicin or related products (eg. Soybeans, peanuts); hypersensitivity to Atropine or similar medications Adverse Reactions: Dizziness; dry nose or nose irritations; dry mouth; flu-like symptoms; headache; nausea; nervousness; pain; runny nose; sinus congestion; sore throat; upper respiratory tract infection; blurred vision; nosebleeds; eye pain; trouble urinating; visual halos or colored rings 58 KETOROLAC (TORADOL®) Description/Mechanism: Ketorolac is an anti-inflammatory drug that also exhibits peripherally acting, non-narcotic analgesic activity by inhibiting prostaglandin synthesis. Onset: Within 10 minutes Duration: 2 to 6 hours Indication: Short term management of moderate to severe pain Contraindications: Hypersensitivity to the drug; patients with history of asthma; patients with allergies to aspirin or other NSAIDS; bleeding disorders; renal failure; hypotension Adverse Reactions: Anaphylaxis; edema; sedation; hypertension; hypotension; bleeding disorders; rash, nausea; headache 59 LIDOCAINE (XYLOCAINE®) Description/Mechanism: Suppresses automaticity in His-Purkinje system and by elevating electrical stimulation (fibrillation) threshold of ventricles during diastole. This occurs by blocking fast sodium channels and depressing pathogenic phase 4 diastolic depolarization. Onset: 30 to 90 seconds Duration: 2 to 4 hours Indications: VF/VT; wide complex tachycardia of unknown origin; significant ventricular ectopy in the setting of myocardial ischemia/infarction; pre-medication prior to RSI in patients with closed head injury Contraindications: Hypersensitivity to other amide type anesthetics (NOT ester anesthetics like NOVACAINE®); Stokes - Adams syndrome; second or third degree AV block without an artificial pacemaker Adverse Reactions: Lightheadedness; confusion; CNS depression; muscle twitching; seizures; blurred vision; hypotension; bradycardia; cardiovascular collapse 60 MAGNESIUM SULFATE Description/Mechanism: Magnesium sulfate reduces striated muscle contractions and blocks peripheral neuromuscular transmission by reducing acetylcholine release at the myoneural junction. In emergency care, magnesium sulfate is used in the management of seizures associated with toxemia of pregnancy. Other uses of magnesium sulfate include uterine relaxation (to inhibit contractions of premature labor), as a bronchodilator after beta agonist and anticholinergic agents have been used, replacement therapy for magnesium deficiency, as a cathartic to reduce the absorption of poisons from the GI tract, and in the initial therapy for convulsions. Magnesium sulfate is frequently used as an initial treatment in the management of Torsades de pointes, and dyrhythmias secondary to TCA overdose or digitalis toxicity. The drug is also considered as a class IIa agent (probably helpful) for refractory VF/VT after administration of other antidysrhythmics. Some success has also been found in patients suffering with respiratory distress from asthma or COPD. Onset: Less than 1 minute Duration: 3 to 4 hours Indications: Seizures of eclampsia; Torsades de Pointes; refractory VF; suspected hypomagnesemic state; respiratory distress secondary to asthma or COPD Contraindications: Heart Blocks Adverse Reactions: Diaphoresis; facial flushing; hypotension; depressed reflexes; bradycardia; respiratory depression 61 MEPERIDINE (DEMEROL®) Description/Mechanism: Meperidine is a synthetic opioid agonist that works on opioid receptors to produce analgesia, euphoria, and respiratory and physical depression. It has a tendency for physical dependence and abuse, and is classified as a Schedule II drug. Onset: Less than a minute via IV Duration: 2 to 4 hours Indications: Moderate to severe pain; OB analgesia Contraindications: Hypersensitivity to narcotics; patients taking MAO inhibitors; during labor or delivery of a premature infant; undiagnosed abdominal pain or head injury Adverse Reactions: respiratory depression; nausea and vomiting; euphoria; delirium; agitation/hallucination; seizures; headache; visual disturbances; coma; facial flushing; circulatory collapse; dysrhythmias; allergic reaction 62 METHYLPREDNISOLONE (SOLU-MEDROL®) Description/Mechanism: Methylprednisolone is a synthetic steroid that suppresses acute and chronic inflammation. In addition, it potentiates vascular smooth muscle relaxation by beta adrenergic agonists, and may alter airway hyperactivity. A newer usage is for reduction of posttraumatic spinal cord edema Onset: 1 to 2 hours Duration: 8 to 24 hours Indications: Anaphylaxis; acute spinal cord injury; bronchodilator-unresponsive asthma Contraindications: Use with caution in patients with GI bleeding and diabetes mellitus Adverse Reactions: alkalosis Headache; hypertension; sodium and water retention; hypokalemia; 63 METOPROLOL (LOPRESSOR®) Description/Mechanism: Clinical pharmacology studies have confirmed the beta-blocking activity of metoprolol in man, as shown by (1) reduction in heart rate and cardiac output at rest and upon exercise, (2) reduction of systolic blood pressure upon exercise, (3) inhibition of isoproterenolinduced tachycardia, and (4) reduction of reflex orthostatic tachycardia. Onset: Within 1 hour Duration: Dose dependent but from 3 to 12 hours Indications: Hypertension; angina pectoris; myocardial infarction Contraindications: Hypersensitivity to the drug; bradycardia; sick sinus syndrome; second and third degree heart blocks; cardiogenic shock; severe peripheral arterial circulatory disorders Adverse Reactions: Tiredness; dizziness; mental confusion; short-term memory loss; headaches; insomnia; diarrhea; nausea/vomiting; heartburn; abdominal pain; rash; hypotension; bradycardia; CHF; peripheral edema; palpitations 64 MIDAZOLAM HYDROCHLORIDE (VERSED®) Description/Mechanism: Like all benzodiazepines, enhances the inhibitory effects of GABA receptors on chloride channels in central nervous system, hyperpolarizing membrane. Induces sleep, decreases anxiety, and impairs memory retention. Onset: 1 to 3 minutes (dose dependent) Duration: 2 to 6 hours (dose dependent) Indications: Pre-medication for tracheal intubation or cardioversion; anxiety; status epilepticus (off-label) Contraindications: Hypersensitivity to the drug; depressed vital signs; concomitant use of barbiturates, alcohol, narcotics, other CNS depressants Adverse Reactions: Hiccough; cough; oversedation; pain at the injection site; headache; nausea/vomiting; blurred vision; hypotension; respiratory depression or arrest (especially when given rapidly) 65 MORPHINE SULFATE Description/Mechanism: Morphine sulfate is a natural opium alkaloid that increases peripheral venous capacitance and decreases venous return ("chemical phlebotomy"). It promotes analgesia, euphoria, and respiratory and physical depression. Secondary pharmacologic effects of morphine include depressed responsiveness of alpha adrenergic receptors (producing peripheral vasodilation) and baroreceptor inhibition. In addition, because morphine decreases both preload and afterload, it may decrease myocardial oxygen demand. The properties of this medication make it extremely useful in emergency care. Onset: Less than 1 minute Duration: 2 to 7 hours Indication: Chest pain associated with myocardial infarction/ischemia; congestive heart failure (with or without pain); moderate to severe acute and chronic pain Contraindications: Hypersensitivity to the drug; hypovolemia; hypotension; head injury or undiagnosed abdominal pain; patients who have taken MAO inhibitors within past 14 days Adverse Reactions: Hypotension; tachycardia or bradycardia; palpitations; syncope; facial flushing; respiratory depression; euphoria; bronchospasm; allergic reaction 66 NALOXONE (NARCAN®) Description/Mechanism: Naloxone is a competitive narcotic antagonist that is used in the management and reversal of overdoses caused by narcotics and synthetic narcotic agents. Compared with other narcotic antagonists which do not completely inhibit the analgesic properties of opiates, naloxone antagonizes all actions of morphine. Onset: Within 2 minutes Duration: 30 to 60 minutes Indications: Complete or partial reversal of CNS and respiratory depression induced by opioids; coma of unknown origin; decreased level of consciousness Contraindications: Hypersensitivity to the drug; use with caution in narcotic-dependent patients who may experience withdrawal syndrome (including neonates of narcotic-dependent mothers) Adverse Reactions: Tachycardia; hypertension; dysrhythmias; nausea/vomiting; diaphoresis 67 NITROGLYCERIN Description/Mechanism: It was originally believed that nitrates and nitrites dilated coronary blood vessels, thereby increasing blood flow to the heart. It is now believed that atherosclerosis limits coronary dilation and that the benefits of nitrates and nitrites are due to dilation of arterioles and veins in the periphery. The resultant reduction in preload, and to a lesser extent in afterload, decreases the workload of the heart and lowers myocardial oxygen demand. Nitroglycerin is very lipid soluble and is thought to enter the body from the GI tract through the lymphatics, rather than the portal blood. Onset: 1 to 3 minutes Duration: 20 to 30 minutes Indications: Ischemic chest pain; hypertension; congestive heart failure Contraindications: Hypersensitivity to the drug; use of erectile dysfunction medications within past 24 hours; hypotension; head injury; cerebral hemorrhage Adverse Reactions: Transient headache; postural syncope; reflex tachycardia; hypotension; nausea/vomiting; diaphoresis 68 ODANSETRON HYDROCHLORIDE (ZOFRAN®) Description/Mechanism: Ondansetron is a selective 5-HT3 receptor antagonist. While ondansetron’s mechanism of action has not been fully characterized, it is not a dopamine-receptor antagonist. Serotonin receptors of the 5-HT3 type are present both peripherally on vagal nerve terminals and centrally in the chemoreceptor trigger zone of the area postrema. It is not certain whether ondansetron's antiemetic action in chemotherapy-induced nausea and vomiting is mediated centrally, peripherally, or in both sites. However, cytotoxic chemotherapy appears to be associated with release of serotonin from the enterochromaffin cells of the small intestine. In humans, urinary 5-HIAA (5-hydroxyindoleacetic acid) excretion increases after cisplatin administration in parallel with the onset of vomiting. The released serotonin may stimulate the vagal afferents through the 5-HT3 receptors and initiate the vomiting reflex. Onset: Up to 15 minutes Duration: Up to 4 hours Indications: Prevention of nausea and vomiting. Contraindications: Hypersensitivity to the drug Adverse Reactions: Constipation; angina; hypotension; tachycardia 69 PHENYLEPHRINE (NEO-SYNEPHRINE®) SPRAY Description/Mechanism: A decongestant that shrinks blood vessels in the nasal passages. Onset: 3 to 5 minutes Duration: Up to 4 hours Indications: Temporary relief of congestion or stuffiness in the nose caused by common hayfever or other allergies, colds, or sinus trouble. It may also be used in ear infections to relieve congestion. Contraindications: Hypersensitivity to the drug Adverse Reactions: Fast, irregular, or pounding heartbeat; headache or dizziness; increased sweating; nervousness; paleness; trembling; trouble sleeping; increase in runny or stuffy nose 70 PROMETHAZINE (PHENERGAN®) Description/Mechanism: Long acting derivative of phenothiazine with marked antihistaminic activity and prominent sedative, amnesic, antiemetic, and anti-motion sickness actions. Unlike other phenothiazine derivatives, it is relatively free of extrapyramidal side effects; however, in high doses it carries same potential for toxicity. In common with other antihistamines, exerts antiserotonin, anticholinergic, and local anesthetic action. Anti-emetic action thought to be due to the depression of the CTZ in medulla. Onset: Less than 1 minute Duration: 4 to 6 hours Indications: Nausea and vomiting due to stimulation of CTZ (not from GI bleed, CHI, etc); to potentiate the effects of analgesics; motion sickness; pre-and postoperative, obstetric (during labor) sedation Contraindications: Hypersensitivity to the drug; coma; CNS depressed patients; when signs of Reye’s syndrome are present Adverse Reactions: Hypotension; sedation; dizziness; may impair physical and mental ability; allergic reactions; dysrhythmias; nausea/vomiting; hyperexcitability; EPS 71 SODIUM BICARBONATE Description/Mechanism: Sodium bicarbonate reacts with hydrogen ions to form water and carbon dioxide and thereby can act to buffer metabolic acidosis. By increasing the plasma concentration of bicarbonate, blood pH rises. Onset: 2 to 10 minutes Duration: 30 to 60 minutes Indications: Known pre-existing bicarbonate responsive acidosis; intubated patient with continued long arrest interval; upon return of spontaneous circulation after long arrest interval; tricyclic antidepressant overdose; alkalinization for treatment of specific intoxications Contraindications: Patients with chloride loss from vomiting and GI suction; metabolic and respiratory alkalosis; hypocalcemia; hypokalemia Adverse Reactions: Metabolic alkalosis; hypoxia; electrolyte imbalance; seizures; tissue sloughing at injection site; rise in intracellular PCO2 and increased tissue acidosis 72 TETRACAINE OPTHALMIC DROPS Description/Mechanism: Tetracaine Drops are an anesthetic. It works by blocking nerve impulses, which results in loss of feeling. Onset: Less than 1 minute Duration: 10 to 15 minutes Indications: To numb the eye during certain procedures Contraindications: Hypersensitivity to the drug Adverse Reactions: Temporary burning, stinging, or redness 73 THIAMINE (BETAXIN®) Description/Mechanism: Thiamine combines with adenosine triphosphate (ATP) to form thiamine pyrophosphate (TPP) coenzyme, a necessary component for carbohydrate metabolism. Most vitamins required by the body are obtained through diet, however, certain states such as alcoholism and malnourishment may affect the intake, absorption, and utilization of thiamine. The brain is extremely sensitive to thiamine deficiency. Onset: Less than 1 minute Duration: Depends on degree of deficiency Indications: Prior to the administration of D50 in hypoglycemia when alcohol abuse and/or malnourishment is suspected; delirium tremens Contraindications: None significant Adverse Reactions: Hypotension (from rapid injection or large dose); anxiety; diaphoresis; nausea/vomiting; allergic reaction (usually from IV injection, very rare) 74 VASOPRESSIN Description/Mechanism: Vasopressin is a peptide hormone that controls the re-absorption of molecules in the tubules of the kidneys by affecting the tissue's permeability. It also increases peripheral vascular resistance, which in turn increases arterial blood pressure. Onset: IV – Less than 1 minute Duration: Approximately 3 hours Indication: Asystole; diabetes insipidus; esophageal varices Contraindications: Hypersensitivity to the drug Adverse Reactions: Angina; abdominal cramps; nausea/vomiting; gas; gangrene; ischemic colitis; tissue necrosis (with extravasation); allergic reaction 75 Nitroglycerin Drip Chart Drug Amount: 50 mg pre-mixed Final Volume: 250 ml Final Concentration: 200 mcg/ml Usual Dose: 1 – 20 mcg/min Maximum Dose: 200 mcg/min Instructions: Find the desired dosage in mcg/min on the chart and locate the rate in ml/hr below it. Dose mcg/min Rate ml/hr 1 2 3 4 5 6 0.3 0.6 0.9 1.2 1.5 1.8 7 8 9 10 15 20 2.1 2.4 2.7 3 4.5 6 Dose mcg/min Rate ml/hr 30 40 50 60 70 80 9 12 15 18 21 24 Dose mcg/min Rate ml/hr 90 100 110 120 130 140 27 30 33 36 39 42 Dose mcg/min Rate ml/hr 150 160 170 180 190 200 45 48 51 54 57 60 Dose mcg/min Rate ml/hr 76 Heparin Drip Instructions and Chart Drug Amount: 25,000 units Final Volume: 500 ml Final Concentration: 50 units/ml Procedure: Administer Heparin Bolus 5000 units via IV Administer Heparin Drip IV-weight adjusted @ 60 units/kg, not to exceed 4000 units. Use the following formula to determine drip rate: Initial Drip Rate: 12 units/kg multiplied by weight in kg then divide by 50 units/ml to equal dosage in ml/hr. Max dose is 20 ml/hr. Chart Instructions: Find weight on chart and locate drip rate below it. Weight in kg 40 45 50 55 60 Drip Rate ml/hr 9.6 10.8 12 13.2 14.4 Weight in kg 65 70 75 80 85 15.6 16.8 18 19.2 20 Drip Rate ml/hr *For all weights over 85 kg, the drip rate is 20 ml/hr. 77 THE LAW UNIFORM RULES OF THE ROAD OCGA 40-6-6. Authorized emergency vehicles. (a) The driver of an authorized emergency vehicle, when responding to an emergency call, or when in the pursuit of an actual or suspected violator of the law, or when responding to but not upon returning from a fire alarm, may exercise the privileges set forth in this Code section. (b) The driver of an authorized emergency vehicle may: (1) Park or stand, irrespective of the provisions of this chapter; (2) Proceed past a red or stop signal or stop sign, but only after slowing down as may be necessary for safe operation; (3) Exceed the maximum speed limits so long as he does not endanger life or property; (4) Disregard regulations governing direction of movement or turning in specified directions. (c) The exceptions granted by this Code section to an authorized emergency vehicle shall apply only when such vehicle is making use of an audible signal and use of a flashing or revolving red light visible under normal atmospheric condition s from a distance of 500 feet to the front of such vehicle, except that a vehicle belonging to a federal, state, or local law enforcement agency and operated as such shall be making use of a flashing or revolving blue light with the same visibility to the front of the vehicle. (d) The foregoing provisions shall not relieve the driver of an authorized emergency vehicle from the duty to drive with due regard for the safety of all persons. No emergency response is so urgent that we cannot respond in a safe manner so as to protect the lives of the public and ourselves. To do otherwise could compound an already urgent situation and result in additional emergency patients. The safety of individuals proceeding to the scene as well as the public through which they are traveling is of high priority. LIGHTS & SIREN DEFINITIONS "Hot" Response - This type of response includes use of the ambulances warning lights and siren. "Cold" Response - This type of response, while it may be deemed to be an emergency response, does not dictate the use of lights and siren by the ambulance service personnel. During a "cold" response the ambulance will be operated in compliance with the "Rules of the Road" and all traffic laws will be obeyed. Emergency or Emergent - any circumstance calling for immediate action in which medical attention is indicated. Rules and Regulations for Ambulance Services 290-5-30.02 (bb). Note: An emergency or emergent call can be considered a "hot" or "cold" response. Non-Emergency - means any circumstances in which a delayed action is appropriate and in which transport to a medical facility is indicated. Note: A non-emergency is always considered a "cold" response. GUIDING PRINCIPLES The driver of the ambulance should be advised by the attending medic, as outlined by ambulance protocol, whether it is necessary to respond under "hot" conditions. If a question arises concerning the transport of any patient, medical control should be contacted. The driver should be advised by the attending medic if the patient's condition changes during transport, and the method of operating as an authorized emergency vehicle can be altered as 78 appropriate. When operating a vehicle as "an authorized emergency vehicle", both the warning lights and audible signal must be in use. Operating a vehicle with only one of these warning devices in use does not satisfy the requirements of OCGA 40 -6-6. There are certain medical conditions that may require the rapid transport of the patient, but without the use of an audible warning device due to the patient's condition (i.e. acute MI, pre -eclampsia, etc.). In circumstances where lights only are used for transport, the driver should be advised that the vehicle cannot proceed as "an authorized emergency vehicle" under the conditions set forth in OCGA 40-6-6. The operator of the ambulance using lights only without the use of an audible warning device must proceed in complete compliance with the "Rules of the Road". Despite the existence of an emergency situation, there are times when it may be more appropriate to approach a scene or transport the patient t o a medical facility silently or "cold". Similarly, there may be environmental conditions (i.e. traffic, weather, etc.) in which operating as an emergency vehicle or "hot" introduces unreasonable risk and/or disruption and provides minimal opportunity to arrive at the scene early. In any case, remember ambulance charges and third party payment rates do not correspond directly with the use of warning lights and siren. When transporting a patient, either "hot" or "cold", the driver of the ambulance should be especially aware of the physical danger inherent and the operation of an emergency vehicle, and drive in a manner to minimize turbulence to passengers resulting from quick and/or sudden stops, acceleration, and turning movements. Realizing all contingency cannot be considered and a hard and fast rule established, the practice of returning to a station or quarters "hot" for any reason other than an emergency is discouraged. Proper use of backup personnel and vehicles and the use of common sense should all but eliminate returning to station "hot". Any 911 call received should be considered an emergency call and lights and sirens should be used when responding unless otherwise advised by 911 or another agency. *** NOTE*** The paramedic may make the decision not to respond emergency to a 911 call emergency. The Paramedic should always take all precautions into consideration while making this decision. If call is an “unknown problem” call you should consider this an emergency until otherwise advised. 79 Reasonable Distances for Rendition of Pre-Hospital Emergency Care for EMS Reasonable distances have been determined based on the patient’s medical or: (1) Trauma related emergency (2) Resources at the local and surrounding facilities (3) Geographic location of the various facilities (4) Ambulance service resources (5) Obligation to provide emergency services in the assigned ambulance zone (6) Availability of mutual aid With due consideration of normal workloads and/or extraordinary circumstances at the time of the request for service (i.e. medics, ambulances, and resources of intended receiving facility). A distance of 25 miles (or closest appropriate medical facility) shall be within reasonable distance for rendition of pre-hospital emergency care. The patient shall be transported by the ambulance service to the hospital of his/her choice providing that the hospital chosen is within reasonable distance of the patient's location and is capable of meeting the patient's immediate needs. The ambulance service medical director has established reasonable distances for rendition of prehospital emergency care for EMS. (See below) In the event of exigent circumstances on-line medical control may override the established reasonable distances. 1. If the patient's choice of hospital is not within a reasonable distance, medical control will determine the closest hospital capable of meeting the patient's immediate needs. 2. If the patient's choice of hospital is within a reasonable distance but medical control (or the medic, if the medic is unable to communicate with medical control) determines that A) The patient's condition is too critical to risk excessive time necessary to reach the hospital chosen and a nearer hospital is capable of meeting the patient's immediate needs, or B) The hospital chosen is unable to meet the patient's immediate needs, or C) The hospital chosen by the patient has notified the medic that it is unable to receive the patient, THEN medical control and/or the medic should make a reasonable effort to convince the patient that a hospital other than the one chosen is more capable of meeting the patient's immediate needs. If the patient continues to insist on being transported to the hospital he/she has chosen then the patient shall be transported to that hospital. If the patient does not, cannot, or will not express a choice of hospitals, the ambulance service shall transport the patient to the nearest hospital believed capable of meeting the patient's immediate medical needs without regard to other factors, (e.g., patient's ability to pay, hospital charges, county or city limits, etc.). Reference: DHR Public Health Rule 290-5-30-.05(8)(k) Destination of Pre-hospital Patients. 80 DESTINATION SELECTION FOR PREHOSPITAL PATIENTS Use the following criteria to help determine if air transportation is needed: GENERAL Land transport time greater than 30 minutes for critically ill/injured patients whose condition is likely to worsen in transport and air transport will significantly reduce that time. TRAUMA Physiologic Status Glasgow Coma Scale <14 Systolic blood pressure <90 Respiratory rate <10 or >29 Revised Trauma Score <11 Anatomy of Injury All penetrating injuries to head, neck, torso, and extremities proximal to elbow and knee Flail chest Combination trauma with burns Two or more proximal long-bone fractures Pelvic fractures Open and depressed skull fracture Paralysis of extremities, new onset Amputation or near amputation, excluding digits Major burns >10% of body surface of face, hands, feet or perineum, or burns with significant respiratory involvement or major electrical or chemical burns Mechanism of Injury Ejection from automobile Death in same passenger compartment Extrication time >20 minutes Falls >20 feet Rollover High-speed auto crash: Initial speed >40 mph Major auto deformity >20 inches Intrusion into passenger compartment >12 inches Auto-pedestrian/auto-bicycle injury with significant (>5 mph) impact Pedestrian thrown or run over Motorcycle crash >20 mph or with separation of rider from bike Other Factors Age <5 or >55 years Cardiac disease, respiratory disease Insulin-dependent diabetes, cirrhosis, or morbid obesity Pregnancy Immunosuppressed patients Patient with bleeding disorder or patient on anticoagulants 81 **NOTE** EACH PATIENT AND SITUATION IS DIFFERENT AND VARIATIONS FROM THESE GUIDELINES MAY BE NECESSARY. CRITERIA FOR TRANSPORT BY HELICOPTER SHOULD NOT REPLACE DECISIONS BASED ON SOUND MEDICAL JUDGEMENT. TRANSPORT TO LOCAL FACILITY FOR STABILIZATION AND TRANSFER TO TERTIARY CARE IN CRITICAL SITUATIONS WHERE AIR TRANSPORT IS NOT FEASIBLE. 82 Pre-Hospital Withholding and Withdrawing Resuscitation General Comments 1. Emergency medical services provide rapid evaluation and treatment of potentially life threatening illnesses and injuries in the out of hospital environment. The first obligation is to the patient(s) in distress. The receipt of a 911 call establishes an implied contract to perform a patient assessment and give appropriate treatment. 2. Patient assessment should always occur promptly and without delay. NEVER withhold or put off patient assessment to take time to read a document. Vital moments in a patient's life may be spent in such an effort. In the absence of a valid DNR, requests by family members to withhold assessment and lifesaving treatment should be set aside initially except in the setting of a patient who is obviously dead. 3. EMS personnel are not trained in making legal opinions and should not attempt to decide if DNR orders or living wills are valid or not while on the scene of a patient in distress. Instead, verbal communication from (1) the patient, (2) the immediate family (authorized person), or (3) medical personnel specifically assigned to and familiar with the patient should be used to make decision. 4. CPR can be stopped in the field in the proper setting (OCGA 31-39-4). Patients experiencing asystole in the field almost always die. Even if they respond initially, almost no studies show survival of any of these patients to hospital discharge. must be warm (95°) before they are pronounced dead. The exception is in the obviously dead patient. terminally ill cancer patients will still have terminal cancer when resuscitated. have many more years of quality life when resuscitated. 5. Patients that have died or for whom it is later determined did NOT want intubation (or the individuals who legally may substitute their judgment for them did NOT want intubation) can be extubated in the emergency department. Endotracheal extubation should not be performed in the field. 6. Since each DNR situation must be dealt with on an individual basis and appropriate care and decision -making determined accordingly, professional judgment is mandatory in determining treatment modalities within the parameters of this protocol. 7. Emergency medical providers must always remember the primary goal of this profession: Render aid and comfort to the suffering. The application of this protocol in no way diminishes this responsibility. All patients whether they are dying, are near death, or have some other clinical problem deserve the provider's utmost compassion and concern. Withholding of Resuscitation 1. It is proper that resuscitation should not be attempted on certain patients. Any victim meeting one or more of the criteria of "obvious death" should have resuscitative attempts withheld. You must be familiar with the signs of obvious death. A patient, who is in rigor mortis, has dependent lividity (pooling of blood due to gravity), has decomposition, or has experienced decapitation or obviously fatal trauma should have resuscitation withheld. If there is EVER any doubt, attempt resuscitation. 2. "Down time", while not a nebulous concept is fraught with too many variables to permit a specific period of time being used in this protocol to determine whether or not to withhold resuscitation. The medic must exercise professional judgment in determining if "down time", say, 15 -minutes in a particular set of circumstances, would clearly indicate withholding resuscitation. If there is any doubt the medic will initiate a resuscitative attempt and proceed to URGENT 83 HISTORY. 3. Living Will - In recognition of the dignity and privacy which patients have a right to expect, the Georgia General Assembly allows a competent adult person to make a written directive, known as a living will, instructing his physician and others to withhold or withdraw life-sustaining procedures in the event of a terminal condition, a persistent coma, or persistent vegetative state. SEE OCGA 31 -32. Each medic should be familiar with this statute which includes a sample living will and goes into the execution and revocation of a living will, including the immunity of participants from liability. : If you elect to ignore a living will and resuscitate the patient, you are protected from liability. REMEMBER: If you elect to follow a living will's instructions, you are protected from liability. 4. DNR Order - This is an order in writing by the attending physician using the term "do not resuscitate", "DNR", "order not to resuscitate", "no code", or substantially similar language in the patient's chart. This constitutes a legally sufficient order and authorizes a physician, health care professional, emergency medical technician, cardiac technician, or paramedic to withhold or withdraw cardiopulmonary resuscitation whether or not the patient is receiving treatment from or is a resident of a health care facility. SEE OCGA 31 -39. Each medic should be familiar with this statute. Urgent History 1. Obtain the urgent history only after the appropriate medical measures have been initiated. The resuscitation measures should not be interrupted while the urgent history is obtained. 2. Determine the most legitimate person present from whom the history should be taken, for example the spouse, next of kin, and so on. This is the "authorized person". Know what durable power of attorney for health care means. 3. Determine the following: a. Is there a terminal illness involved? b. Is there an advance treatment directive such as a living will or DNR order? c. Did the patient express to an authorized person any desires regarding resuscitative measures, e.g. proxy directive through durable power of attorney for health care? If so, what? 4. REMEMBER: Just because a living will exists does NOT mean that the patient wants NO resuscitative effort. Even a terminal cancer patient would likely want to have an airway suctioned, oxygen given, and proper aid and comfort administered. Endotracheal Intubation 1. The field patient who is experiencing an arrest state should be evaluated where possible to determine if the patient may or may not have wanted to be intubated. This should not delay the medic's efforts to do so if, in the judgment of the medic, that intubation is the proper course to follow. 2. The unresponsive field patient in asystole, PEA, or in ventricular fibrillation or unstable tachycardia refractory to initial care needs to be intubated. If the patient's family or authorized medical agent states that they and/or the patient did not wish to have endotracheal intubation even for a short period, this wish should be followed. When in doubt, intubate. The tube can always be removed in the emergency department. Medical Control Generally speaking medical control should always be contacted prior to withholding or withdrawing resuscitative efforts. DEATH SCENE The Cardiac Arrest Protocol is to be initiated on all patients except under the following situations: 1. The patient is displaying obvious and accepted signs of irreversible death such a rigor mortis, dependent lividity, decapitation, decomposition, or incineration. 84 2. Blunt trauma victims who have no respirations, no pulse, show asystole confirmed in 2 leads on the cardiac monitor and have obvious signs of trauma. 3. A Georgia Licensed Physician, Medical Examiner, Coroner or other person legally authorized in Georgia to pronounce death. 4. The physician (patient’s physician, medical director, or Emergency Room physician) states to at least two (2) EMS personnel, (Paramedics and/or EMTs), that resuscitation is not to be attempted on this patient and the physician agrees to accept responsibility for pronouncing the patient dead. 5. The patient’s family has a “Do Not Resuscitate” Order present on the scene that has been signed by a Licensed Physician. The Paramedic’s/EMTs responsibility is to the patient. 1. Neither the family nor Law Enforcement Officers have the right to refuse resuscitation attempts for the patient. 2. The Paramedic/EMT is responsible for the medical judgment as to whether a patient is obviously dead or dismembered. 3. Document absence of vital signs and attach the EKG strip to the EMS record. In possible crime cases, do not remove or cut clothing, remove penetrating objects, or cut through penetrating holes in clothing unless absolutely necessary for patient evaluation/care. If the Paramedic/EMT has any doubt as to how to handle a situation, notify medical control and give an assessment of the situation. WITHDRAWING RESUSCITATION Cardiac Arrest APPROPRIATE PROTOCOL Continue CPR if it is in progress upon arrival, or clear airway and start rescue breathing and chest compressions OBTAIN URGENT HISTORY Identify authorized person giving information id DNR orders present? Notify proper authorities Protect the dignity of the patient Provide support for the family Watch for emergent medical problems in family members Protect the crime scene (if appropriate) Stay until proper authorities arrive IF Asystole, V-Fib, Pulseless V-Tach, or PEA is present go to appropriate protocol THEN Contact Medical Control AND consider termination unless hypothermia and/or short (<15 min) down time Resuscitate as ordered Terminate resuscitation as ordered 85 HAZARDOUS MATERIAL EXPOSURE Arrive at Scene Signs of hazardous materials present Proceed to appropriate protocol Haz Mat Team on scene Keep patients isolated to avoid contaminating EMS crew & equipment Report to scene commander Contact Medical Control and notify receiving facility (or facilities) Implement Haz Mat Response Move patients to safe area out of the hazardous environment and emergency personnel should wear appropriate PPE Is medical treatment necessary? Decontaminate by thorough cleansing Medical attention or surveillance required Report to supervisor for instructions Transport to appropriate facility Do patients require transport by EMS? If yes, package patients appropriately and transport 86 Personal Property of Patient A medic’s first responsibility is to treat the patient. Handling a patient’s valuables or personal property is secondary to proper pre-hospital emergency care. However, special attention needs to be paid to how a patient’s personal property is handled by the medic (when handling it cannot be avoided) to minimize potential problems for the medic and the EMS later on. In “load-and-go” situations, do not waste time handling patient’s valuables. In Georgia case law, Bricks v. Metro Ambulance Service, Inc., et.al. 70517,177 Ga. App. 62 (1985) the court ruled that an ambulance service is a common carrier under Georgia law and therefore it owes duty to passengers not only to protect their lives and persons from insult and injury but to also protect their personal effects from loss. The common carrier (ambulance service) is liable for willful and wanton acts of its own servants in its employment, so proper handling of a patient’s valuables is very important. Proper procedure under this protocol is determined by location of the patient (at home, accident scene, etc.) whether family members or friends of the patient are present, whether law enforcement personnel are present and several other factors. Every situation cannot be described here, but the following is to serve as a guideline. Patient’s personal property could include but not be limited to: glasses, dentures, wallets, money, watches, jewelry, expensive clothing, medications, and keys. PATIENT AT HOME OR A RESIDENCE Advise and encourage the patient to leave all unnecessary personal items and valuables at home or with a family member or friend. A patient’s medication in most cases would need to go to the hospital either with the patient or be carried by a family member. If it is necessary for the medic to handle these medications they should be treated like any other patient valuables. Do not remove a watch, jewelry, or wallet from a patient unless it is necessary to treat the patient, e.g., start an I.V. If it is necessary to do so tell the patient you are removing the item. Then try to give it to the patient if conscious and alert or to a family member if present and document this on the ambulance trip report. If possible have another medic or law enforcement officer witness what you did with the patient’s personal property. If the patient insists on taking personal items with him, the patient must be alert enough to keep possession of the items. If you are uncomfortable about the security of the premises you are leaving, notify law enforcement. PATIENT AT ACCIDENT SCENE OR NOT AT HOME If the patient is conscious encourage the patient to give personal property and valuables to a responsible person of his choice. If you have to remove any item from the patient (e.g., watch, jewelry, etc.) to treat the patient, return the items to the patient, and if possible, have someone witness this and document it on the trip report. If law enforcement presents you with a patient’s personal items, request that they (law enforcement) present the items to the patient (if conscious and alert) or to the patient’s family, or present them to the hospital staff. If personal items or valuables are handled by first responders or bystanders before they were presented to you, document this on the trip report. 87 If personal items or valuables are destroyed in order to gain access to the patient, this should be documented and the items kept. If patient is disoriented or unconscious give the patient’s personal items to a family member or law enforcement officer if possible. Document any incident involving valuables on the trip report and obtain signature from the person receiving valuables. If family or law enforcement are unavailable, transport valuables with patient. TAKING CHARGE OF PATIENT’S PERSONAL ITEMS When the medic finds himself in possession of a patient’s personal items and valuables, he/she should carefully document what he/she did with the items. Place the items in a container provided for that purpose – zip lock bags for small items and plastic garbage bags for larger items. Make a list of the items placed in each bag and place the list on the bag or in the bag. Medications should be listed separately. Currency should be listed by amount. Have your partner or law enforcement officer verify (sign) the list of items included in the bag. When you arrive at the hospital, turn the bag(s) over to the appropriate hospital staff (depending on hospital protocol) and have them sign for the items. Retain a copy of this signed list to be attached to the EMS copy of the trip report. 88 Practice Parameter Emergency Medical Treatment and Active Labor Act The purpose of this practice parameter is to provide guidance as to EMS’ role in meeting the guidelines concerning the Emergency Medical Treatment and Active Labor Act regulations. a. When patient contact is made, the patient is considered to be “in the emergency department” and the obligation to provide an appropriate medical screening exists. b. The Paramedic should perform an assessment of the patient to include general appearance, vital signs, and symptoms related to the chief complaint. c. Care rendered will be performed based on the Practice Parameters established for EMS. d. The Emergency Department physician at RRMC is responsible for performing the medical screening exam except when the following conditions apply: I. The patient is in active labor (RRMC does not provide obstetrical services); II. The patient or family requests that the patient be transported to another facilities’ emergency department; III. The following trauma related injuries are apparent: Multi-system trauma with cardiovascular compromise Combination trauma with burns Open and depressed skull fractures OR IV. The following mechanism of injury occurs: Ejection from automobile Death in same passenger compartment Extrication time >20 minutes Falls>20 feet Rollover Intrusion into passenger compartment > 12 inches Major auto deformity > 20 inches Auto-pedestrian/auto-bicycle injury with significant (>5 mph) impact Pedestrian thrown or run over e. In the event the patient or family does not have a preference for facility or is unable to voice a preference, the patient will be transported to Redmond Regional for the MSE to be completed. **In certain situations, the requirement to complete Initial Medical Care, as written, may be altered or waived in favor of rapidly transporting the patient for definitive care. Document the patient's condition or behaviors which interfered with the performance of any needed assessments and / or interventions. If no response to Practice Parameters, contact Medical Control for consult. 89 ADULT GENERAL PATIENT CARE INDICATIONS: Any adult patient requiring pre-hospital medical evaluation by a pre-hospital health care provider with Redmond Regional Medical Center EMS. The Adult General Patient Care protocol will be followed in conjunction with all other applicable protocols. Perform scene survey. Observe universal precautions. *Follow Infection Control Directive Consider the need for additional resources. Determine responsiveness using AVPU. Evaluate Airway, Breathing, Circulation, and Disability, Exposing the patient as necessary. Secure a patent airway appropriately. Manage cervical spine appropriately. Treat life-threatening conditions as necessary per specific treatment protocols. Assess body systems as appropriate. Monitor patient via the use of pulse oximetry and/or capnography, as appropriate. Administer OXYGEN as appropriate. (Maintain a SaO2 of at least 92%) Obtain medical history (HPI, PMH, allergies, and medications). Evaluate blood pressure, pulses, respiratory rate, pulse oximetry and tactile temperature. Reassess with a frequency indicated by patient condition (ideally q 5 to 10 minutes) and prior to each ALS intervention. Monitor cardiac rhythm and/or 12 lead ECG as appropriate. Assess blood glucose level as necessary per PMH or S/S. Assign treatment priority and make transport decision. Establish intravenous access with normal saline infused as appropriate or with a saline flush as appropriate. Limit 2 attempts unless situation dictates further attempts. Inability to establish IV does not preclude other interventions for definitive therapy. Obtain appropriate blood tubes. Consider intraosseous access, if IV access cannot readily be obtained for patients in extremis that are in need of medication or fluid resuscitation. *Administer 20 – 40 mg LIDOCAINE IO over 1 minute in the conscious patient if not contraindicated *Administer 10 ml NSS rapid IO push *All IV medications can be administered IO Consider the administration of ZOFRAN 4mg undiluted over 2-5 minutes or the administration ® of 12.5 mg to 25 mg PROMETHAZINE (PHENERGAN ) IV or IM for nausea and vomiting (must be diluted with 9 ml Bacteriostatic solution). ZOFRAN IS PREFERRED. If tactile temperature indicates possible fever in an adult, perform *Obtain temperature - oral or axillary *Passive cooling of patient with removal/loosening of clothing and change of environmental conditions. Note: Do not cool to point of shivering. 90 following: *For temperatures of 101.5° f (38.5° C) or greater and no ACETAMINOPHEN in last 4 hours, consider administering ACETAMINOPHEN 650 mg PO in absence of nausea and vomiting and any allergies to medication. *If ACETAMINOPHEN has been administered within the last 4 hours and temperature is still 101.5° F, then consider administering IBUPROFEN 600mg PO if no allergies, contraindications and without nausea and vomiting. For animal bites or stings: o Irrigate and cleanse wound with normal saline. o Assess degree of bite or sting by measuring bite/sting marks. Outline edematous, erythemic and ecchymotic areas with pen and mark the time. Try to confirm size, type and length of any snakes. (Do not bring LIVE snakes to the ER) o Apply constricting band IF your ETA to receiving facility is <20 minutes or if the bite or sting shows signs of increasing reaction. Apply constricting band proximal to wound and ensure constricting band does not impede arterial blood flow. o Remove stingers as necessary and take care to avoid compression of the area. o Immobilize affected part and keep it below the level of the heart. Remove any distal jewelry on the affected part. o Monitor ABC’s, apply cardiac monitor, obtain IV access, apply O2 as needed. o Frequently reassess patient for airway patency. o Do not apply ice or cold pack to any bite or sting. In certain situations, the requirement to complete Initial Medical Care, as written, may be altered or waived in favor of rapidly transporting the patient for definitive care. Document the patient's condition or behaviors which interfered with the performance of any needed assessments and / or interventions. If no response to Practice Parameters, contact Medical Control for consult. 91 ACUTE RESPIRATORY DISTRESS INDICATIONS: Acute exacerbation of asthma, emphysema, and reactive airway disease; cough, shortness of breath, air hunger, wheezing, diminished breath sounds, retractions, and tachypnea. Contact medical control prior to medication administration if the patient's heart rate is greater than 150 beats per minute (BPM). Consider capnography. Consider CPAP for an alert patient who is able to maintain a patent airway but is, or continues to be, in moderate to severe respiratory distress. If the patient who is short of breath has a history of asthma, emphysema, or is actively wheezing, administer up to 5 mg of ALBUTEROL via nebulized aerosol. Consider the administration of 0.5 mg nebulized IPRATROPIUM BROMIDE (ATROVENT ) with ALBUTEROL. If wheezing continues after first nebulized aerosol treatment is completed, you may repeat ALBUTEROL or ALBUTEROL with ATROVENT treatment up to 3 times IF the patient’s heart rate remains less than 150 BPM. Consider the administration of 0.3 to 0.5 mg SC EPINEPHRINE 1:1000 for asthma only. Consider the administration of 125 mg METHYLPREDNISOLONE (SOLU-MEDROL ) IV for moderate to severe respiratory distress secondary to asthma or COPD. Contact medical control for consideration of administration of 1-2 g MAGNESIUM SULFATE IV diluted in 250 ml Normal Saline over 10 minutes for continuing severe respiratory distress secondary to asthma or COPD. If suspected severe Carbon Monoxide Poisoning, contact Medical Control for possible transport to closest Hyperbaric Chamber. ® ® 92 Congestive Heart Failure/Pulmonary Edema Indications: Shortness of breath, air hunger, tachypnea, tachycardia, elevated blood pressure, rales, neck vein distention, and diaphoresis. If patient presents with CHF symptoms BUT is febrile, consider treating with the Acute Respiratory Distress protocol secondary to possible Pneumonia. Allow patient to maintain position of comfort (usually sitting). Consider use of capnography. Consider CPAP for an alert patient who is able to maintain a patent airway but is, or continues to be, in moderate to severe respiratory distress. Administer 0.4 mg NITROGLYCERIN (NTG) SL. Repeat 0.4 mg NTG every 3-5 minutes. If systolic blood pressure (SBP) is less than 90 mmHg, discontinue NTG administration until SBP recovers to greater than 90 mmHg. IV must be established prior to NTG administration for patients not currently prescribed and taking NTG. If the patient is on FUROSEMIDE (LASIX ), administer FUROSEMIDE IV in a dose equivalent to the patient's total daily dose. Give FUROSEMIDE doses up to 100 mg. Withhold if systolic blood pressure is less than 90 mmHg. ® 1. If the daily dose is unknown, administer 40 mg FUROSEMIDE IV. 2. Contact Medical Control to administer doses in excess of 100 mg IV. If wheezing present and heart rate is <150, consider ALBUTEROL 2.5 mg via nebulizer Consider MORPHINE via IV (2-10mg) If heart rate <60 AND systolic BP <90 mm Hg, consider ATROPINE 0.5 mg IV. If heart rate >60 AND systolic BP <90 mm Hg, consider fluid challenge. If no response, administer DOPAMINE 5-20 mcg/kg/min. Perform and interpret 12 lead ECG. Contact Medical Control for consideration of NITROGLYCERIN Drip at 3mcg/minute via IV pump IF systolic BP is above 110 mmHg. Assessment and management of airway and breathing precedes the performance of a 12 lead ECG. Withhold nitrates and contact medical control if the patient relates taking SILDENAFIL ® ® ® (VIAGRA ) or VARDENAFIL (LEVITRA ) within the last 24 hours or TADALAFIL (CIALIS ) within the last 48 hours. 93 Acute Coronary Syndrome (ACS) and/or ST Elevation MI (STEMI) Suspect ACS and or STEMI for the following presentations: classic anginal chest pain, atypical chest pain, or anginal equivalents such as dyspnea, palpitations, syncope or pre-syncope, general malaise, or DKA. All of these patients should have a 12 lead EKG performed and interpreted. Indications for ACS: Classic anginal chest pain OR patients whose 12 lead is suspicious for ischemia. Indications for STEMI: Suspicion of ACS and a pre-hospital12 lead diagnosis of STEMI. Administer OXYGEN via nasal cannula @ 4 lpm. Obtain Pulse Ox, IV access, and labs Cardiac Monitor, obtain and transmit 12 lead EKG to ER. Follow chest pain flow sheet. Administer BABY ASPIRIN 324 mg, chewed, if no allergies to ASA exist. If systolic BP is above 110 mm Hg: 1. Administer NITROGLYCERIN 0.4 mg SL spray. Repeat at 5 minute intervals for 3 doses. Do not give NTG if patient is on an erectile dysfunction drug. Document BP before and after NTG administration. 2. Consider MORPHINE SULFATE 1 to 4 mg IVP, then 1 to 2 mg IV every 5 minutes PRN for continued chest pain until stable (unless allergy to MORPHINE SULFATE exists). 3. If patient allergic to MORPHINE SULFATE, administer DEMEROL 12.5 to 25 mg IV for chest pain, then 12.5 mg every 5 minutes until stable (unless allergy to DEMEROL exists). If patient vomiting or severe nausea, administer ZOFRAN 4 mg undiluted over 2 to 5 minutes or PROMETHAZINE 12.5 mg slow IVP diluted with 9cc NORMAL SALINE. ZOFRAN is preferred. If systolic BP below 90 mmHg, elevate lower extremities and administer 200 to 300 ml NORMAL SALINE bolus. If systolic BP above 90 mmHg, place patient in semi-fowlers position for transport or in position of comfort. If heart rate less than 75 bpm and systolic BP above 100 mmHg, administer LOPRESSOR 5 mg slow IVP; may repeat times 2 every 5 minutes PRN. Repeat 12 lead ECG throughout transport as necessary. Contact Medical Control for consideration of NITROGLYCERIN Drip at 3 mcg/minute via IV pump. Titrate and increase NTG Drip at 2 mcg/minute increments every 3 to 5 minutes until relief of discomfort. Monitor and document BP q 5 minutes. IF STEMI is present, perform above treatments AND: 1. Notify Medical Control immediately 2. Contact Medical Control for consideration of administration of HEPARIN Bolus (units) 5000 IV. 3. Contact Medical Control for consideration of administration of HEPARIN Drip IV-weight adjusted: 60 units/kg not to exceed 4000 units. 94 If NTG or HEPARIN IV drip medications are initiated, obtain 2nd IV with NORMAL SALINE at KVO rate prior to administration. Both IV’s should be in the left upper extremity. Avoid putting IV in right arm if possible. Early notification to receiving hospital is paramount in the treatment of ACS. The 12 lead ECG may be deferred initially in order to stabilize the hemodynamically unstable patient. Contact medical control for consideration of the administration of VERSED in the presence of suspected cocaine usage within the past 72 hours. ® Withhold nitrates and contact medical control if the patient relates taking SILDENAFIL (VIAGRA ) ® ® or VARDENAFIL (LEVITRA ) within the last 24 hours or TADALAFIL (CIALIS ) within the last 48 hours. Observe the following precautions for administration of LOPRESSOR: Early aggressive beta blockade may be hazardous in hemodynamically unstable patients; Do not give to patient with STEMI if there are signs of heart failure, low cardiac output, or increased risk for cardiogenic shock; Relative contraindications include PR interval >0.24 second, second or third degree heart block, active asthma, reactive airway disease, severe bradycardia, or systolic BP <100 mm Hg; Concurrent IV administration with calcium channel clocking agents like VERAPAMIL or DILTIAZEM can cause severe hypotension; and Monitor cardiac and pulmonary status during administration. 95 Altered Mental Status Indications: Incomprehensible speech, inappropriate verbal responses, inability to follow verbal commands, decreased responsiveness, or unresponsiveness. Consider C-spine precautions if necessary Obtain blood sugar reading via glucometer If blood sugar less than 60 mg/dl, administer 25 g DEXTROSE 50% via IVP. Monitor for IV patency and protect against tissue necrosis secondary to infiltration. For pediatric administration dilute DEXTROSE 50% to DEXTROSE 25% or DEXTROSE 10% and refer to Broselow tape. If hypotensive, place patient in Trendelenburg position and administer fluid bolus. If ethanol or malnourishment suspected, administer THIAMINE 100 mg IVP. Consider the administration of NARCAN to provide for patent, self maintained airway and adequate respirations: 1. If patient’s weight is <50 kg, administer NARCAN 2 mg IVP q 3 minutes PRN but not to exceed 6 mg until airway and respiratory status improve. If unable to establish IV line, utilize MAD device. 2. If patient’s weight is >50 kg, administer NARCAN 2 mg IVP q 3 minutes but not to exceed 10 mg until airway and respiratory status improve. If unable to establish IV line, utilize MAD device. 3. Refer to Broselow tape for pediatric administration of NARCAN. If benzodiazepine overdose suspected, contact Medical Control for consideration of administration of FLUMAZENIL 0.2 mg increments rapid IVP q 5 minutes if transient response observed, not to exceed 1 mg. If tricyclic antidepressant overdose suspected, contact Medical Control for consideration of administration of SODIUM BICARBONATE. If beta blocker overdose suspected, contact Medical Control for consideration of administration of GLUCAGON. If calcium channel blocker overdose suspected, contact Medical Control for consideration of administration of CALCIUM CHLORIDE. 96 Suspected Stroke / CVA Indications: Altered mental status, seizure, headache, parasthesia, hemiparesis in the absence of trauma, weakness, ataxia, visual disturbances, dysarthria, nausea, vomiting, general malaise, positive pronator drift, facial droop, abnormal papillary function, or other symptoms of suspected cerebral ischemia or hemorrhage. Administer OXYGEN via nasal cannula at a quantity sufficient to maintain the oxygen saturation level equal or greater than 95%. Maintain head and neck in neutral alignment without flexing the neck. Elevate head of stretcher 15 to 30 degrees if systolic BP is above 90 mmHg. Obtain IV access Obtain blood sugar level via glucometer. If reading is below 60 mg/dl, administer 25 g DEXTROSE 50% via IVP and THIAMINE 100 mg IVP. Patient is to remain NPO. Administer 1 mg GLUCAGON if IV access cannot be established and blood sugar reading is below 60 mg/dl. Obtain and interpret 12 lead EKG If seizures are present and lasting >2 minutes, consider the administration of VERSED 2.5 to 10 mg IVP or DIAZEPAM 2 to 20 mg slow IVP titrated to control seizure activity. If no IV access obtained, consider same doses VERSED or VALIUM IM up to total of 2 ml per large muscle injection site and 1 ml per small muscle injection site. VERSED is preferred. Monitor and record neurological status and any changes. Protect paralyzed limbs from injury. If patient is vomiting or has severe nausea, administer ZOFRAN 4 mg IV with 9cc flush or PROMETHAZINE 12.5 mg slow IVP (diluted with 9cc of NORMAL SALINE). ZOFRAN is preferred. Transport to nearest appropriate CT-capable hospital without delay. Notify Emergency Room of Stroke Alert if verified onset is less than 3 hours. Maintain on scene time of less than 20 minutes. 97 Seizures Indications: EMS witnessed active seizure activity. Administer OXYGEN at rate sufficient enough to maintain SpO2 at/or above 95%. Protect airway and protect patient from injury. Do not place anything inside patient’s mouth. Observe type, location, and duration of seizure activity. Obtain IV access if possible. Obtain blood glucose reading. If blood sugar level below 60 mg/dl, administer 25 g of DEXTROSE IV. If unable to obtain IV access, administer 1 mg GLUCAGON IM. Administer up to 5 mg VERSED slow IVP, if patient has witnessed generalized seizure activity. If unable to obtain IV access, VERSED may be administered IM or IN. This may be repeated times 1 as needed. May consider administering up to 5 mg VALIUM slow IVP for seizure activity if patient does not have a history of epilepsy or does not respond appropriately to VERSED. This may be repeated times 1 as needed. (VERSED is preferred) Administer 1 g MAGNESIUM SULFATE diluted in 250 ml Normal Saline via IV infused over 10 minutes for seizures secondary to eclampsia. Contact Medical Control for consideration of additional VERSED if the patient continues to have seizure activity after the second dose. Be prepared to maintain control of airway after administering VERSED should severe respiratory depression or respiratory arrest occur. 98 Allergic Reactions/Anaphylaxis Moderate Allergic Reaction Indications: Allergic manifestations without airway compromise or shock. Hives (urticaria) and/or history of systemic reaction in the past. Maintain airway and administer OXYGEN at level to maintain SpO2 levels above 95%. Establish IV access Consider the administration of 25 to 50 mg DIPHENHYDRAMINE (BENADRYL) IV, IM, or PO If wheezing and heart rate <150, consider the administration of 2.5 mg ALBUTEROL via nebulizer Apply cardiac monitor, obtain labs if possible. Severe Allergic Reaction Indications: Allergic manifestations with urticaria and/or history of an allergic exposure with: 1. Airway obstruction (partial or complete) OR 2. Systolic blood pressure less than 80 mmHg with clinical evidence of shock Maintain airway and administer OXYGEN at level to maintain SpO2 levels above 95% Establish IV access using NORMAL SALINE and administer a fluid bolus of 500 ml. Administer 0.25 mg EPINEPHRINE (1:10,000) IV over a one minute interval. If unable to establish IV access, administer 0.3 to 0.5 mg EPINEPHRINE (1:1,000) IM or SC. Reassess patient, if acute respiratory obstruction persists or systolic BP is less than 80 mmHg with clinical evidence of shock present, repeat 0.25 mg EPINEPHRINE (1:10,000) IV over a one minute period, or repeat 0.3 to 0.5 mg EPINEPHRINE (1:1,000) IM or SC, if no IV access established. May repeat IV fluid bolus of 500 ml if systolic BP remains below 80 mmHg with continued evidence of clinical shock. Consider administration of 50 mg DIPHENHYDRAMINE (BENADRYL) IV or IM. Consider administration of 125 mg METHYLPREDNISOLONE (SOLU-MEDROL) IV. Consider administration of 2.5 to 5.0 mg ALBUTEROL via nebulizer if wheezing is present and heart rate is below 150. 99 Non-Traumatic Hypotension Indications: Systolic blood pressure less than 80 mmHg and heart rate greater than 60 beats per minute. Infuse up to 500 ml bolus of NORMAL SALINE via IV if clinical signs of CHF are not present Reassess vital signs and lung sounds Infuse an additional 500 ml bolus of NORMAL SALINE via IV if clinical signs of CHF are note present. Reassess vital signs and lung sounds Contact Medical Control for consideration of a 5 to 20 mcg/kg/min DOPAMINE infusion for continued hypotension not due to hypovolemia. 100 Shock Indications: Systolic blood pressure less than 80 mmHg and heart rate greater than 60 beats per minutes with signs of decreased tissue perfusion secondary to HYPOVOLEMIA. Administer OXYGEN necessary to maintain SpO2 at/or above 95% Place patient in Trendelenburg position. Control external hemorrhage if necessary. Apply cardiac monitor Establish IV access via 2 large bore IV lines. Administer fluid boluses of LACTATED RINGERS in increments of 20 ml/kg, to titrate systolic BP >80 mmHg. Monitor for signs of fluid overload. If known hemorrhagic shock, infuse fluid rapidly until systolic BP >80 mmHg. Monitor patient for signs of fluid overload. Administration of DOPAMINE for patients with hypovolemia is contraindicated. 101 Hypertensive Crisis Indications: Systolic BP >230 mmHg and/or Diastolic BP >120 mmHg. Consider medical etiology for hypertensive crisis and refer to appropriate protocol: Congestive Heart Failure/Pulmonary Edema, Acute Coronary Syndrome/STEMI, and/or Suspected Stroke/CVA. Administer OXYGEN at levels sufficient to maintain SpO2 levels at or above 95%. Apply cardiac monitor and establish IV access Draw labs, if possible Administer 0.1 to 0.2 mg CATAPRES (CLONIDINE) PO Continue to monitor and document BP q 5 min If patient exhibits signs of severe nausea or vomiting, administer ZOFRAN 4 mg undiluted over 2 to 5 minutes or PROMETHAZINE 12.5 mg slow IVP diluted with 9cc NORMAL SALINE. ZOFRAN is preferred. Contact Medical Control for consideration of NITROGLYCERIN 0.4 mg SL, repeat q 5 min or until NITROGLYCERIN Drip is established at 3 mcg/minute via IV pump. DO NOT GIVE NITRO IF PATIENT IS ON VIAGRA, CIALIS, or LEVITRA. Discontinue NITROGLYCERIN therapy when systolic BP <200 mmHg and/or diastolic BP <110 mmHg. Contact Medical Control for consideration of administration of 5 mg VALIUM slow IVP over 1 to 2 minutes (excluded for patients that exhibit any CVA like signs and/or symptoms.) 102 Hemodynamically Compromising Bradycardia Indications: Pulse less than 60 bpm AND systolic blood pressure less than 80 mmHg OR absence of radial pulses bilaterally, with clinical evidence of shock. Patients with altered mentation and clinical evidence of shock are hemodynamically compromised, even if the systolic blood pressure is greater than 80 mmHg. Administer 0.5 mg ATROPINE IV. Repeat 0.5 mg ATROPINE IV every 3-5 minutes until a maximum of 3 mg of ATROPINE is administered or the pulse rate is 60 bpm or greater. ATROPINE in 2 mg doses may be given via ET every 3-5 minutes to a total of 6 mg. Consider initiating transcutaneous cardiac pacing (TCP) if patient does not respond to ATROPINE. Set rate at 80 per minute. Rapidly increase the output (MA) until capture occurs, or the maximum MA is reached. o If electrical or mechanical capture is achieved, do not give ATROPINE, unless capture is lost, and bradycardia recurs. o If the patient is experiencing discomfort due to pacing and the systolic blood pressure is greater than or equal to 100 mmHg, administer up to 5 mg ® MIDAZOLAM (VERSED ) IV for sedation.. Administer an intravenous bolus of up to 500 ml NSS if clinical signs of CHF are not present. Contact medical control for consideration of a 5-20 mcg/kg/min DOPAMINE infusion for continued hypotension not due to hypovolemia. Contact medical control for consideration of GLUCAGON IV if a beta-blocker overdose is suspected. Contact medical control for orders to administer CALCIUM CHLORIDE and possibly SODIUM BICARBONATE, if the patient has a history of chronic renal failure and either hemodialysis or peritoneal dialysis. 103 Stable Tachycardia Indications: A wide complex tachycardia (QRS ≥ 0.12 seconds) presumed to be ventricular tachycardia (VT), with a rate exceeding 100 bpm, or a narrow complex tachycardia (QRS < 0.12 seconds) other than sinus tachycardia, with a rate exceeding 150 bpm. There should be no evidence of trauma. ** For purposes of these Protocols, STABLE is defined as a patient with a systolic blood pressure greater than 80 mmHg. Consider Valsalva maneuver. (Carotid massage may not be performed.) If the rhythm is a wide complex tachycardia at a rate exceeding 100 bpm, administer 150 ® mg AMIODARONE (CORDARONE ) IV infused over 10 minutes. If the rhythm is a narrow complex tachycardia, other than sinus tachycardia, atrial fibrillation or atrial flutter, at a rate exceeding 150 bpm, administer 6 mg ADENOSINE ® (ADENOCARD ) IV rapidly. o If there is no response to the initial 6 mg dose, administer 12 mg ADENOSINE. o If there is no response to the second dose, administer 12 mg ADENOSINE. If the rhythm is a narrow complex atrial fibrillation, atrial flutter, or SVT refractory to ADENOSINE, at a rate exceeding 150 bpm, and the patient is without signs or symptoms of ® congestive heart failure, administer 20 mg DILTIAZEM (CARDIZEM ) IV over 2 minutes. After administering DILTIAZEM (CARDIZEM®) bolus, hang a maintenance drip with remaining DILTIAZEM (CARDIZEM®) at rate of 5 mg/hr. May repeat DILTIAZEM (CARDIZEM®) bolus if desired effects not achieved after 15 minutes at dose of 25 mg via IV, then continue with the maintenance drip at 5mg/hr. Contact medical control for orders to administer CALCIUM CHLORIDE and possibly SODIUM BICARBONATE, if the patient has a history of chronic renal failure and either hemodialysis or peritoneal dialysis. DILTIAZEM (CARDIZEM) use with caution, contact medical control when patients are on DIGOXIN. ADENOSINE: potentiated by DIPYRIDAMOLE (PERSANTINE), use half (1/2) doses. Use with caution with patients on CARBEMAZEPINE (TEGRETOL), DIGOXIN and VERAPAMIL. 104 Unstable Tachycardia Indications: A wide complex tachycardia (QRS ≥ 0.12 seconds) presumed to be ventricular tachycardia (VT), with a rate exceeding 100 bpm, or a narrow complex tachycardia (QRS < 0.12 seconds) other than sinus tachycardia, with a rate exceeding 150 bpm. There should be no evidence of trauma. **For purposes of these Protocols, UNSTABLE is defined as systolic blood pressure less than 80 mmHg OR radial pulses are absent bilaterally, with clinical evidence of shock. Patients with altered mentation and clinical evidence of shock are UNSTABLE, even if the systolic blood pressure is greater than 80 mmHg. If appropriate, consider ADENOSINE administration for narrow complex tachycardia if IV is established. Consider the administration of up to 20 mg ETOMIDATE (AMIDATE ) IV prior to cardioversion of an alert patient. This is in consideration of the weight for a normal size adult. Otherwise, ETOMIDATE dose is 0.2 mg/kg IV. Perform synchronized cardioversion using 100 joules. Perform synchronized cardioversion using 200 joules. Perform synchronized cardioversion using 300 joules. Perform synchronized cardioversion using 360 joules. Administer intravenous fluid bolus up to 500 ml. Upon successful conversion, perform and interpret 12 lead ECG. For wide complex tachycardia, administer 150 mg AMIODARONE (CORDARONE ) IV infused over 10 minutes: ® ® o If there is no response to cardioversion, o OR upon successful conversion, o AND if needed for a recurrence. Contact medical control for consideration to administer CALCIUM CHLORIDE and possibly SODIUM BICARBONATE, if the patient has a history of chronic renal failure and either hemodialysis or peritoneal dialysis. Biphasic devices may use FDA approved/recommended energy settings. 105 Ventricular Fibrillation/Pulseless Ventricular Tachycardia In the absence of effective CPR on arrival and when response time is greater than four (4) minutes, perform 2 minutes of chest compressions prior to first defibrillation or intubation. Defibrillate using 360 joules every 2 minutes. If an IV/IO can be established: Administer 1 mg EPINEPHRINE (1:10,000) IV. Repeat 1 mg EPINEPHRINE (1:10,000) IV every 3-5 minutes if VF or pulseless VT persists. Consider administration of 2 g MAGNESIUM SULFATE via IV if Torsade de Pointes is identified (withhold for renal dialysis patients). Administer 300 mg AMIODARONE (CORDARONE ) IV, with a repeat dose of 150 mg after 10 minutes. (Do not administer if LIDOCAINE has already been given). ® If an IV/IO cannot be established: Administer 2 mg EPINEPHRINE 1:10,000 ET every 3–5 minutes until IV access is obtained. Administer 3 mg/kg LIDOCAINE via ET once. If an IV is established, continue with 0.75 mg/kg LIDOCAINE IV every 5-10 minutes until a max dose is given of 4.5 mg/kg. With return of antiarrhythmic: spontaneous circulation (ROSC) prior to administration of any ® Administer 150 mg AMIODARONE (CORDARONE ) IV infused over 10 minutes or 3 mg/kg LIDOCAINE ET if no IV access is available. Guidelines • Biphasic devices may use FDA approved/recommended energy settings • Ventilations o ventilate at 8-10 breaths per minute to decrease intrathoracic pressure o patients should be bagged using a one-hand squeeze • Compressions o perform 2 minutes of chest compressions between each defibrillation attempt o CPR should be adjusted to provide for an EtCO 2 reading of greater than 10 mmHg, with greater than 20 mmHg preferred to improve chance of return of spontaneous circulation (ROSC) o ensure proper depth and rate of compressions and minimize hands-off time o frequently switch providers performing chest compressions to maintain peak performance o ensure complete recoil of the chest wall prior to the next compression 106 Asystole/Pulseless Electrical Activity Consider early transcutaneous pacing for heart rates less than 60 bpm. Administer 1 dose of VASOPRESSIN 40 U IV/IO. administering EPINEPHRINE. This should be completed prior to Administer 1 mg EPINEPHRINE (1:10,000) IV. Repeat 1 mg EPINEPHRINE (1:10,000) IV every 3 to 5 minutes if asystole or PEA continues For asystole or PEA at a ventricular rate less than 60 bpm, administer ATROPINE 1 mg IV. ATROPINE 1 mg IV may be repeated every 5 minutes until ventricular rate is greater than 60 bpm or a total of 3 mg of ATROPINE has been given. Administer intravenous bolus of NORMAL SALINE up to 500 ml. Guidelines • Ventilations o ventilate at 8-10 breaths per minute to decrease intrathoracic pressure o patients should be bagged using a one-hand squeeze • Compressions o CPR should be adjusted to provide for an EtCO 2 reading of greater than 10 mmHg, with greater than 20 mmHg preferred to improve chance of return of spontaneous circulation (ROSC) o ensure proper depth and rate of compressions and minimize hands-off time o frequently switch providers performing chest compressions to maintain peak performance o ensure complete recoil of the chest wall prior to the next compression 107 Environmental Cold Emergencies Note: All patients should have their temperature assessed. Frostbite Initiate medical care. Remove wet garments and move patient to a warm environment ASAP. Elevate affected part and cover with loosely applied, dry, sterile dressings. Systemic Hypothermia Mild / Moderate 95 to 90 degree Fahrenheit. Conscious or altered sensorium with shivering. Initiate medical care o OXYGEN via NC @ 4 lpm, EKG, and obtain IV access o Warm IV packs using hot packs Remove wet clothing and protect patient against heat loss and wind chill. Place patient in horizontal position avoiding rough movement and excess activity Completely dry patient and cover with insulating blanket. Severe Systemic Hypothermia Temperature of 90 degrees Fahrenheit or less. Patient may appear uncoordinated with poor muscle control or stiff, simulating rigor mortis. There will be NO shivering. Sensorium: confused, withdrawn, disoriented, comatose. Initiate medical care o OXYGEN 4 lpm via NC. Do not intubate unless patient is apneic. o Warm IV tubing, fluids, and oxygen tubing with hot packs. Refer to Systemic Hypothermia and Contact Medical Control. For Ventricular Fibrillation and Pulseless Ventricular Tachycardia: do not administer any medications unless core body temperature is above 90 degrees Fahrenheit and do not defibrillate more than 3 times until patient is re-warmed. 108 Environmental Heat Emergencies Note: All patients should have their temperature assessed. Heat Cramps Initiate medical care Move patient to a cool environment and transport. Heat Exhaustion Initiate medical care and administer OXYGEN via NC at 4 lpm If Systolic BP <90 mm Hg then administer NORMAL SALINE boluses in 200 to 300 ml increments to titrate systolic BP >90 mm Hg Move patient to cool environment Lay patient in supine position with feet elevated Remove as much clothing as possible to facilitate cooling Sponge with cool water or cover with wet sheet and fan patient’s body Heat Stroke Initial Medical Care - OXYGEN 4 lpm via Nasal Cannula. Pulse ox / cardiac monitor / IV access / labs If systolic BP < 90 mm Hg, Fluid boluses in increments of 200 - 300 ml, to titrate systolic BP > 90 mm Hg. Move patient to cool environment Semi-reclining position with head elevated 15 - 30 degrees if systolic BP > 90 mm Hg. Evaluate and take precautions for increased intracranial pressure Initiate rapid cooling. Remove as much clothing as possible to facilitate cooling; place cold packs on lateral chest wall, groin, axilla, carotid arteries, temples, and/or behind knees; sponge with cool water or cover with wet sheet and fan patient’s body. 109 Sickle Cell Anemia Signs and Symptoms include: severe dyspnea, severe pain secondary to hypoxia or vasoocclusive disease process and pain may include any large muscle mass. Initiate medical care, pulse oximeter, OXYGEN via NC @ 4 lpm Cardiac monitor, IV access, and draw labs Keep patient as calm as possible to minimize oxygen needs Administer a NS fluid bolus of 200 to 300 ml then continue IV infusion KVO If wheezing is present and HR <150 bpm, administer 2.5 mg ALBUTEROL via nebulizer If the patient is exhibiting severe altered mental status, consider endotracheal intubation and ventilate with OXYGEN at 100% via BVM. Consider the administration of pain management to include MORPHINE SULFATE and/or TORADOL. Refer to the Pain Management protocol. 110 OB/GYN Pregnancy Induced Hypertension Initiate Medical Care. Provide OXYGEN via NRM or assist with BVM as indicated. Apply cardiac monitor, obtain IV access, draw labs, obtain blood glucose level, and be prepared for seizures. Handle patient gently. Maintain minimal CNS stimulation. Patient should be positioned on left side or raise the right side of the backboard approximately 30 degrees. If seizure occurs, administer MAGNESIUM SULFATE 1 gm IV diluted in 250 ml Normal Saline over 10 minutes. If seizures last longer than 2 minutes, administer VERSED 5 mg IV or IM for adults and titrate to control seizure activity. If patient does not respond appropriately, consider administering VALIUM 2 to 20 mg slow IVP and titrate to control seizure activity. VERSED is the safer medication for the unborn fetus. Vaginal Bleeding Initiate Medical Care. Administer OXYGEN via nasal cannula at 4 lpm, apply pulse oximeter, apply cardiac monitor. Determine LMP, note if there is a passage of clots or tissue and if present then save them for analysis. Examine perineum and do not perform vaginal examination. Determine if there is any possibility of trauma. If unknown pregnancy status and/or LMP and/or if it is a known pregnancy in the first 6 months then place patient in left lateral position and treat for Shock as indicated. If Third Trimester Bleeding then establish 2 large bore IV lines, place patient in left lateral recumbent position for transport, and mark fundal height and time of measurement with a pen then reassess fundal height every 20 minutes as needed. If hypotensive then treat for Shock as indicated. Trauma in Pregnancy Initiate Medical Care. Apply pulse oximeter and administer OXYGEN via NRM or assist ventilations with BVM as needed. Check for uterine contractions, vaginal bleeding and/or leaking amniotic fluid. Assess for fetal movements. Apply cardiac monitor, obtain IV access, draw labs, and check blood glucose level. 111 Raise right side of backboard approximately 30 degrees. If hypotension is present, treat for Shock as indicated. Emergency Childbirth PHASE 1 – LABOR Obtain history and determine if there is adequate time to transport. If time allows have mother remove all clothing and place a hospital gown on patient. Inspect for bulging perineum, crowning or whether patient is involuntarily pushing with contractions. If contractions are two minutes apart or less, or if any of the above is present, prepare for delivery. Do not attempt to restrain or delay delivery unless there is a prolapsed cord present. Initiate medical care. Apply pulse ox, cardiac monitor, and IV as time allows. Administer OXYGEN as necessary. If mother is hyperventilating, encourage eye contact and coach her to take slow, deep breaths. If mother becomes hypotensive or lightheaded at any time, administer fluid boluses in increments of 200-300 ml, to titrate BP >90 mm Hg and apply OXYGEN via NRM or assist with BVM as needed. Place mother supine on flat surface if possible. If time permits, put on full blood and body secretion barriers. Open OB pack. Place drapes over mother’s abdomen and beneath perineum. Prepare bulb syringe, cord clamps, and tux to receive the infant. PHASE 2 – DELIVERY If amniotic sac is not punctured you must puncture it with a gloved hand and pull away from the face. Allow head to deliver passively. Control rate of delivery by placing palm of one hand gently over occiput. Protect perineum with pressure from other hand. Gently suction infant’s mouth then nose as soon as head delivers if time allows. Once the head is delivered, allow it to passively turn to one side. This is necessary for the shoulders to deliver. Feel around the infant’s neck for the umbilical cord (nuchal cord). If present, attempt to gently lift it over the baby’s head. If unsuccessful, double clamp and cut the cord between the clamps. To facilitate delivery of the upper shoulder, gently guide the head downwards. Support and lift the head and neck slightly to deliver the lower shoulder. The rest of the infant should deliver quickly with one contraction. Firmly grasp the infant as 112 it emerges. Baby will be wet and slippery. Keep newborn level with perineum until the cord stops pulsating and is double clamped. Check blood sugar and rectal temp. If blood sugar is <60 mg/dl, then follow the hypoglycemic protocol. If patient is hypothermic, keep warm and dry. Turn heat on in unit no matter the weather outside the unit. If able, mother may hold infant on chest/abdomen during transport. Remember the mother may be very tired or lethargic from blood loss after delivery. Newborn care Record APGAR score at 1 minute and 5 minutes. Continue to suction mouth first then nose of infant with bulb syringe. For meconium-stained infants: suction only upon delivery of the head prior to delivery of the body; after delivery, intubate the infant and apply suction to the lumen of the ETT while withdrawing from the trachea. After establishing airway, dry, warm and stimulate the infant, clamp and cut cord provided pulsations have ceased. Assess respiratory rate If respirations are adequate or patient crying: place infant in Trendelenburg position; assess color and provide OXYGEN via NRM if central cyanosis is present; if respirations improve then administer “blow-by” OXYGEN; keep warm and check rectal temp. If respirations are shallow, slow or absent: assist ventilations with BVM and OXYGEN at 100%; If respirations improve, provide OXYGEN via NRM; if apneic after OXYGEN and BVM then consider intubation; keep warm and check rectal temp. Assess heart rate. If rate is below 100, deliver high flow OXYGEN. If below 60, begin compressions. If no response, administer EPINEPHRINE 0.01 mg/kg (0.1 ml/kg of 1:10,000 solution) IV/IO. Contact Med Control for further orders. Post-Partum Care Placenta should deliver in 20 to 30 minutes. If delivered, collect in plastic bag. Do not pull on cord to facilitate delivery of the placenta. Gently massage the fundus in order to facilitate delivery of the placenta. Note the time placenta was delivered. Do not discard the placenta. The placenta must be taken with mother and released to the RN in labor and delivery. Do not delay transport if placenta has not delivered. 113 If perineum is torn and bleeding apply direct pressure with sanitary pads and have patient bring her legs together. If significant blood loss or signs of hypoperfusion: administer high flow OXYGEN, apply pulse ox, and cardiac monitor; administer fluid boluses in increments of 200-300 ml, to titrate BP > 90 mm Hg; gently massage abdomen over the uterus until the uterus is firm. If altered sensorium, and signs of hypoperfusion persist after treatment, then follow the Shock protocol. Childbirth Complications Breech Birth Initiate medical care. Apply oxygen via NRM or assist ventilations with BVM as needed. Never attempt to pull the infant from the vagina. As soon as legs are delivered, support the baby’s body wrapped in a towel. After the shoulders are delivered, if face down, gently elevate the legs and trunk to facilitate delivery of the head. Head should deliver within 30 seconds. If not, reach two sterile gloved fingers into vagina to locate baby’s mouth. Push vaginal wall away from baby’s mouth to form an airway. If possible suction the mouth then the nose. Apply gentle pressure to the fundus. If head does not deliver in two minutes, keep your fingers in place to maintain the airway. Prolapsed Cord Initiate medical care. Administer OXYGEN via NRM or assist ventilations with BVM as needed. Elevate mother’s hips. Place sterile gloved hand into vagina between pubic bone and presenting part with cord between two fingers to monitor cord pulsations and exert counter-pressure on presenting part. Cover exposed cord with moist dressing and keep warm. NOTE: All the above described patients in the OB/GYN section should be transported to the nearest facility that provides comprehensive obstetrical care. 114 Suspected Sexual Assault Perform generalized evaluation. Attempt to calm patient as needed, protect patient’s privacy and suspected crime scene. Refer to appropriate medical or trauma protocols as needed. Do not remove clothing unless medically necessary for treatment. If clothing is already removed, place clothing in a paper bag to preserve evidence. Contact law enforcement Transport to closest appropriate facility At the conclusion of the call, wrap and leave stretcher sheets in the patient’s room for evidence. If possible, female EMS personnel should accompany patient during transport and perform the majority of the evaluation. 115 Suspected Abuse / Neglect Initiate medical or trauma care as indicated. Note environment, patient’s interaction with care-givers, discrepancies in the history obtained from patient and care-givers, and any signs of obvious injury. If parents / guardians refuse to let you transport the patient, leave scene, remain in safe location and contact law enforcement for assistance. Transport. It is mandatory that you report your suspicions to the ER Physician upon arrival at the ED. EMS personnel are considered ‘mandatory reporters’ and are legally bound to report all suspicions concerning possible abuse and/or neglect to the ER Physician. It is the Emergency Department Physician’s responsibility to contact DFACS or ensure DFACS is contacted in all suspected abuse and neglect cases. Carefully document history and physical exam findings as well as environmental / circumstantial data on the patient care report. 116 Psychological / Behavioral Emergencies Consider medical etiology of psychological / behavioral disorder and treat accordingly. Establish scene safety and maintain personal safety. Call law enforcement to scene if needed. Do nothing to jeopardize your safety. Determine and document if the patient is a threat to self or others and if the patient is unable to care or provide for self. Protect patient from harm to self or others. Attempt to calm patient verbally as able and encourage patient to leave current environment. Physically restrain as necessary. Document use, type, time applied, and reason for restraints. Document distal circulation, sensory, and motor assessments every 5 minutes. Notify medical control that physical restraints were necessary. If physical restraints are necessary, every attempt should be made to contact law enforcement for assistance. Consider the administration of HALDOL 5mg IV/IM if patient is violent and is a potential harm to self or others. Use caution in IM usage due to delayed onset of medication action. If patient then remains violent and a danger to self or others, you may repeat HALDOL 5mg IV/IM times 1. After administration of HALDOL, continually monitor patient for any complications with respirations and level of consciousness. Initiate medical care after mechanical or chemical restraint. Consult medical control in ALL instances where a refusal of transport of a patient with a psychological / behavioral emergency is being considered due to patient being conscious, alert and oriented times 4. If patient appears to have any degree of confusion or appears to be a potential harm to themselves or others, the patient should be transported against his will. Law enforcement should be involved in this instance. 117 Pediatric and Adult Trauma Indications: This trauma protocol applies to patients with any of the following field triage criteria: Mechanism: Ejection from vehicle Death of passenger in same vehicle Extrication > 20 minutes Falls 2 ½ times patient’s height Obvious Injury: Penetrating injury to the chest, abdomen, head, neck, proximal injuries or groin Major burns, inhalation injury, or trauma with burns More than one proximal long bone fracture Suspected spinal column or cord injury or limb paralysis Pelvic fracture (suspected on clinical grounds) Flail chest, multiple rib fractures, or subcutaneous emphysema Major external bleeding Amputated limb Vital Sign Abnormalities: Adults: Glasgow Coma Scale <13; Systolic BP <90 mmHg; Respiratory rate <10 or >30; Heart rate <50 or >120 bpm Pediatrics: Pediatric Glasgow Coma Scale <13; Refer to abnormal Vital Signs section of Broselow Tape Extenuating Circumstances (Not stand alone criteria for initiation of trauma protocol or helicopter transport): Pregnancy Age <15 or >65 yoa Known significant cardiac or respiratory disease Rollovers High-speed crash Pedestrian >5 mph impact Motorcycle >20 mph or rider thrown Consider helicopter transport if ground transport to appropriate hospital is expected to exceed 20 minutes Consider medication assisted intubation as needed. If unable to intubate, maintain cricoids pressure and resume ventilations via BVM pending placement of an appropriate airway device Consider needle chest decompression for patients with severe respiratory compromise due to tension pneumothorax or for patients in trauma arrest with possible chest involvement. For clinical shock, initiate bilateral IV with fluid resuscitation of 20 ml/kg of NORMAL SALINE or LACTATED RINGERS as indicated. If unable to obtain IV access, IO access is permissible. For suspected unstable pelvic fractures, apply pelvic compression device. Initiate transport to an appropriate trauma facility without delay 118 If head or spinal trauma, consider direct transport to a medical facility with immediate neurosurgical capabilities If isolated burns, consider direct transport to the nearest appropriate specialty burn facility via helicopter or ground without delay for patients with 2 nd or 3rd degree burns greater than or equal to: o 20% BSA in adults o 10% BSA in ages less than 10 and over 50 years of age o 5% BSA in infants o 5% BSA of third degree in any patient o Circumferential burns or burns of the airway, neck, face, head, hands, feet, major joints or perineum o Patients with severe underlying medical conditions o Chemical burns with serious threat to functional or cosmetic impairment o Bandage burn areas using a dry or wet sterile dressing for burns <10% BSA. For burns greater than or equal to 10% BSA, use dry sterile dressing only. Cover the patient and provide for a warm environment to prevent heat loss. *Trauma scene times should be less than 10 minutes unless there are extenuating circumstances. Reasons for scene times greater than 10 minutes should be documented on the patient care report. Appropriate reasons for prolonged trauma scene times include extrication, securing scene safety, presence of multiple patients, necessary stabilizing patient treatment, etc. 119 Spinal Cord Injury THERAPEUTIC GOAL: The patient with a suspected or known spinal cord injury will be recognized and all resources will be utilized to prevent further injury or deficit to the patient. The patient’s entire spine will be adequately immobilized and maintained throughout transport. PATHOPHYSIOLOGY: All trauma patients must be assumed to have a spinal cord injury until proven otherwise. Traffic accidents are the most frequent cause of spinal cord injuries in all age groups, and falls amount for over half of all work-related spinal injuries. Approximately seven percent of spinal injuries are the result of sports and recreational activities. Five percent of patients with a known vertebral fracture have a second fracture along their vertical vertebral axis. The majority of injuries to the bony spine and cord are closed injuries and are usually the result of indirect forces, as opposed to a direct blow. Areas of the spine with great mobility are the most susceptible to injury such as the lower cervical spine, thoracolumbar junction, and lumbar sacral junction. Injury may involve the bony skeleton, the cord itself or both. There may or may not be a neurological deficit. Hyperextension, hyperflexion, vertical loading, or rotational forces may cause blunt spinal injury. Hyperextension injuries often occur as the occupant of a car is thrown forward, striking his chin on the dash or windshield. Similarly, a victim involved in a motor vehicle collision may incur a hyperflexion injury when the top of his head strikes an object, forcefully flexing the head forward. Diving accidents and falls result in direct axial forces being applied to the spine and frequently lead to crush injuries of the vertebrae. Ligamentous injuries (rupture or tearing of ligaments) can cause subluxation of a vertebral body over another, increasing the risk of spinal cord damage. Spinous process fractures are painful but are considered stable fractures. Comminuted fractures of the vertebral body may produce teardrop fractures. Any bony fragments that penetrate the spinal canal have potential to damage the cord. Herniated tissue from disc rupture may result in nerve damage and/or cord compression. Fractures of intervertebral articulations may be associated with subluxation. Damage to the spinal cord at or about the level of the fifth cervical vertebral may result in paralysis of the diaphragm that may compromise the ability to ventilate. Thoracic spine injuries are frequently the result of acute flexion, rotational, and/or axial load forces. Rotational forces are usually associated with thoracolumbar injuries. Edema and contusions are serious complications of a spinal cord injury at any level and may lead to ischemia and necrosis. Neurogenic shock may accompany a low cervical or high thoracic spine injury and is defined as a transient distal areflexia which can last from hours to weeks. Due to loss of sympathetic tone below the level of the injury, hypotension and a paradoxic bradycardia occur, resulting in inadequate perfusion of tissues. Skin below the level of injury is warm and dry due to vasodilation, and urinary output is adequate. The patient may have symptoms of autonomic nerve dysfunction evidenced by acute urinary retention and gastric dilation. The patient in neurogenic shock loses the ability to regulate body temperature and may become hypo or hyperthermic. 120 ASSESSMENT: Conduct a primary survey for assessment of airway, breathing and circulation with simultaneous C-spine control. Immobilize the entire spine if indicated by potential mechanism of injury. If the patient is an interfacility transport trauma patient and the immobilization devices have been removed the patient should be re-immobilized for transport UNLESS ALL OF THE FOLLOWING ARE TRUE: o No neck pain exists. o At least three adequate radiographic views of the C-spine rule out fracture (lateral, AP, and odontoid) or lateral C-spine and complete C-spine CT rules out fracture. o The patient is neurologically intact with a GCS of 15. o There is no potentially distracting injury. o The patient is not under the influence of alcohol or drugs. o The mechanism of injury was not highly suspicious of neck injury (i.e. high speed, head-on MVC). o Medical Control is aware and agrees that re-immobilization is not necessary. If any doubt exists, the patient should be completely immobilized for transfer. Assess vital signs. shock. Hypotension associated with bradycardia may indicate neurogenic Assess for soft tissue injury, swelling, bony crepitus, pain, deformity, and/or muscle spasm. Assess movement, sensation, and strength of extremities. Assess for abdominal breathing, use of accessory muscles, indicating injury at or above the cervical three, four, or five level. Assess patient’s body temperature (poikilothermy is possible). Assess for bladder distention, lack of bowel control, and/or priapism. TREATMENT: Assess and manage airway, breathing, and circulation. Initiate full spinal precautions. Protect patient from hypothermia. Consider anti-emetic medications as needed. Assess blood glucose level. Be prepared to treat patient according to the “Shock” protocol as needed. 121 If the patient has a potential non-penetrating spinal cord injury with motor/sensory deficits and the injury has occurred within the prior eight hours, consider contacting Medical Control for orders to administer METHYLPREDNISOLONE (SOLU-MEDROL®) at rate of 30 mg/kg diluted in 250 ml Normal Saline over 15 minutes. Patient should be transported to nearest medical facility equipped to adequately manage a spinal injury patient. High-dose steroids are not indicated for patients with a spinal injury that is older than eight hours and will have no therapeutic effect on those patients. If you are over 45 minutes away from a facility that can adequately consider transport via aviation. The patient should have METHYLPREDNISOLONE (SOLU-MEDROL®) initiated 45 minutes high-dose steroidal bolus. The maintenance infusion will run at a next 23 hours. handle a spinal injury patient, a maintenance infusion of after the administration of the rate of 5.4 mg/kg/hr over the High dose steroidal treatment for a spinal injury is a twenty-four hour process and requires the adequate and timely recognition of a spinal injury. Proper pre-hospital treatment is an important key to the patient survivability and being able to have an opportunity to resume a normal or near normal lifestyle after a spinal injury. 122 Selective Spinal Immobilization Apply this guideline to all patients in known or suspected blunt trauma Implement spinal immobilization in the following circumstances: Significant multiple system trauma Severe head or face trauma Any penetrating trauma such as GSW or stabbing If altered mental status (including drugs, alcohol, and trauma) AND: no history available; patient found in setting of possible trauma (lying at bottom of stairs, in street, etc.); or near drowning with a history or probability of diving. Loss of consciousness after trauma Spinal pain or tenderness, including any neck pain with a history of trauma Numbness or weakness in any extremity after trauma Patient with significantly painful distracting injury High Risk (should be immobilized): Age >64 years Dangerous mechanism (fall >5 stairs, axial load, high speed MVC with ejection and/or rollover) Motorized recreational vehicles Bicycle collisions Low Risk (may be cleared) Simple low speed rear-end MVC without being pushed into oncoming traffic, without rollover, without being struck by a large vehicle or high speed vehicle Ambulatory at any time after traumatic incident 123 Pediatric General Patient Care Indications: Any patient that is 12 years of age or less requiring pre-hospital medical evaluation by a pre-hospital health care provider. The Pediatric General Patient Care protocol should be followed in conjunction with all other applicable protocols. Perform scene survey Observe universal precautions Consider the need for additional resources Determine responsiveness using AVPU Evaluate airway, breathing, circulation, and disability exposing the patient as necessary Secure a patent airway as needed Manage cervical spine as needed Treat life-threatening conditions as necessary per specific treatment protocols Assess body systems as appropriate Monitor patient via the use of pulse-oximetry as appropriate Administer OXYGEN as necessary to maintain SpO2 at 92% or greater Obtain medical history (HPI, PMH, allergies, and medications) Evaluate blood pressure, pulses, respiratory rate, and tactile temperature. Reassess as needed. Monitor cardiac rhythm and/or 12 lead EKG as appropriate Establish IV access with NORMAL SALINE as needed and appropriate Consider IBUPROFEN or ACETAMINOPHEN via rectal suppository for pediatric temps above 101.5 F or may be given PO at ACETAMINOPHEN 15 mg/kg or IBUPROFEN 10 mg/kg. Alternate medications if already administered <4 hrs prior EMS contact. Use Broselow Tape to estimate drug dosages Consider IO access, if IV access cannot be readily obtained for critically ill and/or injured pediatric patients in extremis that are in urgent need of medication or fluid resuscitation. Contact medical control for consideration of obtaining IO access in all other pediatric patients in extremis that you cannot readily obtain IV accessibility. Consider transport to an appropriate pediatric capable facility 124 Pediatric Acute Respiratory Distress Indications: Acute exacerbation of asthma and reactive airway disease; cough, shortness of breath, air hunger, wheezing, diminished breath sounds, retractions, and tachypnea. Contact medical control prior to medication administration if patient’s heart rate is greater than 180 beats per minute. If patient has history of asthma or is actively wheezing and is less than 2 years of age: administer one dose of ALBUTEROL (2.5 mg) via nebulized aerosol by face mask or blow by. Contact medical control for additional doses. If patient has history of asthma or is actively wheezing and is 2 years of age or older: administer one dose of ALBUTEROL (2.5 mg) via nebulized aerosol. In children 2 years of age or greater, who continue to exhibit respiratory distress, consider the administration of 0.5 mg IPRATROPIUM BROMIDE (ATROVENT) via nebulizer with additional dose of ALBUTEROL 2.5 mg. In children less than 2 years of age, contact medical control for orders and dosage of IPRATROPIUM BROMIDE. Consider the administration of 0.01 mg/kg EPINEPHRINE 1:1,000 IM/SC for patients in severe respiratory distress (maximum dose of IM/SC EPINEPHRINE 1:1,000 is 0.3 mg). For patients suspected of having croup, consider administration of nebulized SALINE for inhalation. For continued distress, contact medical control for consideration of the administration of 2 mg of EPINEPHRINE 1:1,000 via nebulizer. Patient who present with acute respiratory distress of sudden onset accompanied by fever, drooling, hoarseness, stridor, and sitting forward in the tripod position should be suspected of having a partial airway obstruction. Do nothing to upset the child. Perform critical assessments only and have parent administer blow-by OXYGEN. Transport immediately. If patient’s airway becomes obstructed, in the setting of potential epiglottis. Attempt airway management primarily with a BVM. Contact medical control for consideration of administration of 2 mg/kg SOLUMEDROL IV (up to total dose of 125 mg) for children in moderate to severe respiratory distress and a history of asthma in which an IV/IO has been started. Contact medical control for consideration of administration of 25 mg/kg MAGNESIUM SULFATE (up to a max dose of 2 g) diluted in 250 ml NS via IV infused over 10 minutes for continued severe respiratory distress. 125 Pediatric Altered Mental Status Indications: Incomprehensible speech, inappropriate verbal responses, inability to follow verbal commands, decreased responsiveness, or unresponsiveness. If blood sugar less than 60 mg/dl via glucometer, administer 0.5 mg/kg DEXTROSE IV at the following dilutions (max dose 25 g): DEXTROSE 25% (D25) at 2 ml/kg; or DEXTROSE 10% (D10) at 5 ml/kg for neonates. Administer GLUCAGON 1 mg IM if unable to obtain IV access. Consider the administration of up to 0.1 mg/kg NALOXONE (NARCAN) IV, ETT, IN, or IM (max dose is 2 mg) for suspected drug overdose. Contact medical control for consideration of SODIUM BICARBONATE for tricyclic antidepressant overdose, glucagon for beta blocker overdose, and CALCIUM CHLORIDE for calcium channel blocker overdose. 126 Pediatric Seizures (active) If blood sugar less than 60 mg/dl via glucometer, administer 0.5 mg/kg DEXTROSE IV at the following dilutions (max dose 25 g): DEXTROSE 25% (D25) at 2 ml/kg; or DEXTROSE 10% (D10) at 5 ml/kg for neonates. Administer GLUCAGON 1 mg IM if unable to obtain IV access. Administer 0.2 mg/kg MIDAZOLAM (VERSED) up to max dose of 5 mg IV, IN, or IM for seizure activity greater than 5 minutes in duration. 127 Pediatric Shock and Hypotension Indications: Altered mental status, tachycardia, absent peripheral pulses, or cool, clammy, or mottled skin with a capillary refill greater than 2 seconds. Heart rate is greater than 60 bpm. Infuse a 20 ml/kg fluid bolus of NORMAL SALINE via IV. If signs of hypovolemic shock persist, boluses may be repeated at the same volume up to a maximum of 60 ml/kg. 128 Pediatric Allergic Reactions Moderate Allergic Reaction Indications: Allergic manifestations such as urticaria or history with allergic exposure without airway compromise or shock. In patients over the age of two (2) years, consider the administration of 12.5 to 25 mg DIPHENHYDRAMINE (BENADRYL) PO without the necessity of IV access. Severe Allergic Reaction Indications: Generalized allergic manifestations such as urticaria or history of an allergic exposure with airway obstruction (partial or complete) OR clinical evidence of shock including altered mental status, confusion, delayed capillary refill, and cool, clammy, or mottled skin. Administer 0.01 mg/kg (0.1 mL/kg) EPINEPHRINE (1:10,000) IV over a one-minute interval. If unable to establish IV access, administer 0.01 mg/kg EPINEPHRINE 1:1,000 (max 0.3 mg) IM/SC. If respiratory distress and clinical shock are still present and there is no evidence of SVT, ventricular ectopy, or ventricular tachycardia: repeat 0.01 mg/kg EPINEPHRINE 1:10,000 (max 0.25 mg) IV over a one-minute interval. Administer 1 mg/kg DIPHENHYDRAMINE (BENADRYL) IV or IM (max dose is 50 mg). Administer an IV bolus of 20 ml/kg NORMAL SALINE if shock persists. If signs of shock persist, bolus may be repeated at the same volume up to 2 additional times for a max dose of 60 ml/kg. Contact medical control for consideration of administration of 2 mg/kg METHYLPREDNISOLONE (SOLU-MEDROL) up to a max dose of 125 mg IV for children which an IV has been initiated. 129 Pediatric Bradycardia Indications: Pulse less than 60 bpm, systolic blood pressure less than 80 mmHg, patient not in cardiac arrest, and any of the following signs or symptoms: chest pain, dyspnea, altered mental status, dizziness, diaphoresis, slow capillary refill, shock, or pulmonary edema. If severe cardio-respiratory compromise is present as evidenced by poor perfusion, hypotension, or respiratory difficulty continues: Begin CPR if heart rate is less than 60 bpm despite adequate ventilation and oxygenation. Administer 0.01 mg/kg EPINEPHRINE (1:10,000) via IV; or 0.1 mg/kg EPINEPHRINE (1:1,000) via ETT if no IV present. May repeat every 3 to 5 minutes as needed. Administer 0.02 mg/kg ATROPINE via IV; or 0.04 mg/kg via ET is no IV present. Max single dose is 0.5 mg IV or 1 mg via ET. May repeat once in 3 to 5 minutes. Consider cardiac pacing Search for and treat possible contributing factors: hypovolemia, hypoxia, hydrogen ion (acidosis), hypo-hyperkalemia, hypoglycemia, hypothermia, toxins, cardiac tamponade, tension pneumothorax, thrombosis, and trauma. 130 Pediatric Tachycardia Indications: A wide complex tachycardia (QRS ≥ 0.08 seconds) presumed to be ventricular tachycardia (VT), with a rate > 180 bpm in children more than 1 year old or > 220 bpm in children less than 1 year of age OR a narrow complex tachycardia (QRS ≤ 0.08 seconds) other than sinus tachycardia, with a rate >180 bpm in children > 1 year old or > 220 bpm in children less than 1 year old. There should be no evidence of trauma. Stable: patients with signs of adequate tissue perfusion, not in cardiac arrest, and not displaying signs or symptoms of slow capillary refill, altered mental status, shock, or pulmonary edema. Consider vagal maneuvers (valsalva, ice packs applied to face). Carotid massage may not be performed. Administer fluid bolus of 20 ml/kg of NORMAL SALINE if no signs of pulmonary edema. Obtain 12 lead EKG on all patients Contact medical control for consideration of: o If rhythm is a wide complex tachycardia at a rate exceeding 180 in children >1 year old or 220 in children less than 1 year old, administer 5 mg/kg AMIODARONE IV (up to max dose of 150 mg) infused over 10 minutes. o If rhythm is narrow complex tachycardia (SVT) at a rate exceeding 180 bpm in children > 1 year of age or 220 bpm in children less than 1 year of age, administer ADENOSINE (ADENOCARD) 0.1 mg/kg IV to max dose of 6 mg. May repeat at 0.2 mg/kg IV to max dose of 12 mg one time. Unstable: patient with signs of poor tissue perfusion, delayed capillary refill, altered level of consciousness, shock, or pulmonary edema. Synchronized cardioversion: 0.5 to 1 J/kg, if this is not effective may repeat once at 2 J/kg. Consider sedation but do not delay cardioversion. May sedate with 0.2 mg/kg ETOMIDATE (AMIDATE) via IV to max dose of 20 mg. 131 Pediatric Ventricular Fibrillation (VF) and/or Pulseless Ventricular Tachycardia (VT) In the absence of effective CPR on arrival and when response time is greater than four (4) minutes, perform 2 minutes of chest compressions prior to first defibrillation or intubation. Defibrillate at 2 joules/kg Perform 2 minutes of chest compression while attempting IV and/or intubation Defibrillate using 4 joules/kg every 2 minutes If IV/IO can be established: o Administer 0.01 mg/kg EPINEPHRINE (1:10,000) IV. Repeat every 3 to 5 minutes for the duration of the resuscitation. o Administer 5 mg/kg AMIODARONE (CORDARONE) bolus IV. (Do not administer if LIDOCAINE has already been given). o Follow each medication administration with a single shock of 4 joules/kg and 2 minutes of chest compressions. If IV/IO cannot be established: o Administer EPINEPHRINE 0.1 mg/kg (0.1 mL/kg) of 1:1,000 via ET. Repeat every 3 to 5 minutes for duration of resuscitation. o Administer 1 mg/kg LIDOCAINE via ET once (diluted in 10 ml of NORMAL SALINE). If an IV/IO is established, continue with 0.5 mg/kg LIDOCAINE every 5 to 10 minutes until a max dose of 3 mg/kg is given. o Follow each medication administration with a single shock of 4 joules/kg and 2 minutes of chest compressions. With return of spontaneous circulation prior to administration of any antiarrhythmic: o Administer 2.5 mg/kg AMIODARONE (CORDARONE) IV infused over 10 minutes or 1 mg/kg LIDOCAINE via ET if no IV access is available. 132 Pediatric Asystole / Pulseless Electrical Activity (PEA) Ensure adequate oxygenation and ventilation Administer 0.01 mg/kg EPINEPHRINE (1:10,000) via IV/IO or 0.1 mg/kg EPINEPHRINE (1:1,000) via ET. May repeat every 3 to 5 minutes. Administer IV bolus of up to 20 ml/kg NORMAL SALINE. Boluses may be repeated at the same volume up to max dose of 60 ml/kg. 133 Pediatric and Adult Endotracheal Intubation Indications: Respiratory failure, inadequate ventilatory effort with minimal air exchange, severe dyspnea with an increased or decreased respiratory rate, retractions, difficulty speaking, extreme agitation, anxiousness, altered mental status or situations where airway protective reflexes are lost (loss of gag reflex). Central cyanosis may be noted. Consider the administration of up to 0.4 mg/kg ETOMIDATE (AMIDATE) IV/IO as needed prior to intubation. Perform endotracheal intubation and ventilate with 100% OXYGEN. If unable to intubate or ventilate, maintain cricoid pressure and resume ventilations via BVM pending insertion of an approved rescue airway device. Cricothyrotomy (Quick-Trach) is authorized for the difficult airway when unable to ventilate and oxygenate a patient. Verify proper endotracheal placement via the following methods: o Visualization of tube passing through the vocal cords or the substitution of a whistle device (e.g. BAAM) for nasotracheal intubation o Visualization of chest rising and falling with ventilations o Presence of bilateral breath sounds and absence of air sounds over the epigastrium o Clearing of the ET tube with lung inflation and misting of the tube with lung deflation o SaO2 reading o Capnography with waveform reading. Every effort should be made to continuously monitor waveform on intubated patients. A printout of the capnography with the waveform should be obtained upon transfer of patient to receiving facility for documentation purposes. o A printout of the trend report with the patient’s heart rate, pulse oximetry and capnography readings will be presented to the receiving physician and copied for the agency’s medical director, regardless of intubation success. Ventilator management (device dependent): o Tidal volume should be set to 8 ml/kg of body weight o Rate should be set to: 8 to 10 for cardiac arrest To titrate as close to 35-45 mmHg via digital capnography for perfusing patients To titrate as close to 30-35 mmHg via digital capnography for patients with a head injury and signs of impending herniation o FiO2 should be set to: 100% OXYGEN for cardiac arrest patients Titrate to maintain SpO2 of at least 95% for perfusing patients. Consider the administration of up to 5 mg MIDAZOLAM (VERSED) IV/IO as needed following intubation and placement confirmation in adults if the systolic blood pressure is greater than 100 mmHg. For children 12 years of age and under, contact medical control for a sedation order. 134 Oral endotracheal intubation is the preferred route of intubation. If unable to perform oral intubation, nasotracheal intubation should be attempted using an endotracheal tube with a directional control tip along with a whistle device (e.g. BAAM). 135 Pain Management for Adults and Pediatrics Indications: Moderate to severe pain Contraindications: Altered mental status, head injury, multi-system trauma, SaO2 less than 95%, or systolic blood pressure less than 100 mmHg (80 mmHg in the pediatric patient) Contact medical control for pain management for all pediatric patients Angina / Myocardial Infarction o MORPHINE SULFATE 2 to 10 mg IVP as needed for pain o May consider 25 mg IV DEMEROL if patient has allergy to MORPHINE SULFATE. If DEMEROL is administered, consider 4 mg IV ZOFRAN to prevent nausea from euphoria. If ZOFRAN is ineffective, consider administering 12.5 mg PHENERGAN via slow IV diluted in 9 cc of Normal Saline. ZOFRAN is preferred. Acute Abdominal Pain o MORPHINE SULFATE IV 2 to 5 mg, up to max dose of 5 mg. o May consider administration of 30 mg TORADOL via IV as a substitute for MORPHINE SULFATE o Renal Colic (Kidney Stones) may respond better to DEMEROL at 25 to 50 mg IV. If DEMEROL is administered, consider 4 mg IV ZOFRAN to prevent nausea from euphoria. If ZOFRAN is ineffective, consider administering 12.5 mg PHENERGAN via slow IV diluted in 9 cc of Normal Saline. ZOFRAN is preferred. Combative Post Resuscitation o DIAZEPAM 2 to 20 mg slow IVP titrated to effect. Monitor respirations. Environmental Frostbite o DIAZEPAM 2 to 20 mg slow IVP titrated to effect. Monitor respirations. o May consider 0.1 mg/kg MORPHINE SULFATE IV up to 5 mg as a substitute for DIAZEPAM. Sickle Cell Anemia Crisis o Consider MORPHINE SULFATE IV 2 to 5 mg, up to max dose of 5 mg IV o May consider use of 30 mg TORADOL IV as a substitute for MORPHINE SULFATE. Combative Head Injury o Contact medical control for consideration of administration of 2 to 20 mg DIAZEPAM (VALIUM) slow IVP titrated to effect. Monitor respirations. May also consider 5 mg MIDAZOLAM IV or up to 5 mg MORPHINE SULFATE IV. Extremity Injuries o MORPHINE SULFATE 2 to 5 mg IV o May consider 25 to 50 mg DEMEROL IV as a substitute for MORPHINE SULFATE. If DEMEROL is administered, consider 4 mg IV ZOFRAN to prevent nausea from euphoria. If ZOFRAN is ineffective, consider administering 12.5 mg PHENERGAN via slow IV diluted in 9 cc of Normal Saline. ZOFRAN is preferred. May consider 30 mg TORADOL IV/IM as a substitute for MORPHINE SULFATE and Demerol. Burns o MORPHINE SULFATE 2 to 5 mg IV 136 Use caution when administering any medications for pain management. Always monitor patient’s respiratory efforts when administering any pain medications and be prepared to utilize BVM to assist patient’s respiratory efforts if needed. Never give more than one type of pain medication unless medical control has been contacted and orders have been given. This protocol should not prevent you from contacting medical control should you have any concerns over the correct dosage/type of medication to be administered. Use proper judgment when utilizing any portion of this protocol and remember to monitor patient closely after the administration of any medication. 137 Refusal of Service Indications: EMS often responds to scenes where the patient wishes to decline service. It is important that the EMS provider obtains the patient’s informed consent before leaving the scene; otherwise the EMS provider might be exposed to legal liability for abandonment of the patient. Assess the patient fully and document all finding on the PCR. Inform the patient about needed treatment and possible outcomes if patient refuses treatment and transport. If the patient is felt to need treatment, every effort should be made to persuade the patient to consent to needed health care. Consider involving family, medical control, and law enforcement. Document the informed consent process, and, if applicable, the medical control physician on your PCR. Medical control is not needed for patient refusals if patient is alert and oriented to normal mentation and not inhibited by alcohol or drugs. If you suspect the patient is being coerced or is a victim of domestic violence or abuse, etc. then law enforcement should be contacted immediately. You should consider contacting medical control if patient is wishing to refuse treatment and/or transport and any of the following are present: Intoxication by drugs or alcohol Acute mental disease or suicidal or homicidal ideations Significant head injury Respiratory distress Abnormal vital signs (normal vital signs are defined as heart rate between 60 and 100 bpm, systolic blood pressure > 100 mmHg, respiratory rate of 12 to 20 bpm, and SaO2 reading > 95% on room air) Altered mental status Age less than 18, unless parents are on scene and consent to the refusal Patient who suffer from same mechanism of injury that could be classified as something that could cause serious medical problems that would normally require direct transport to a trauma center under a possible trauma alert designation Refusals of service account for many instances of litigation every year and caution should be taken on all refusals and documentation should include every detail so that you are covered in your actions should you have to appear in court. Any time you have doubts or concerns, contact medical control, they are there to help you make this important decision. 138 Induced Hypothermia (POST-ARREST) “Iceman” Complete inclusion and exclusion worksheet Perform a baseline patient assessment Perform a neurological exam Intubate as needed Obtain 12 lead EKG Draw blood for labs Decrease temperature to lowest setting in back of ambulance Induce hypothermia procedures o Apply ice packs to axial, groin and neck areas o Establish chilled 0.9% NORMAL SALINE IV and administer 1000 ml bolus. Consider the establishment of a second IV line in order to administer the fluid bolus. (This is the preferred method except in fluid overload.) Evaluate and treat for first signs of shivering o Administer VERSED 2.5 mg (may repeat times 1) o Administer 5 mg MORPHINE (may repeat times 1) o Prepare for DOPAMINE administration if systolic BP ≤ 90 Properly document the inducement of hypothermia on PCR Transport to closest appropriate facility, preferably a facility that participates in the “Iceman” program (i.e. Redmond Regional Medical Center) Advise Medical Control that you have initiated the Induced Hypothermia protocol Monitor and document vital signs every 15 minutes 139 Induced Hypothermia INCLUSION Criteria Age 18 or older Women must be over 50 or not be pregnant Cardiac arrest, asystole, with return of normal rhythm (initial rhythm outside of hospital of ventricular fibrillation, pulseless ventricular tachycardia or PEA can be considered if returned to normal rhythm and other criteria is met) Persistent coma as evidenced by no eye opening to pain after resuscitation (no waiting period required) Blood pressure can be maintained at a minimum of 90 mmHg systolic either spontaneously or with fluid and pressors (not aortic balloon pump) Known time of cardiac arrest within 6 hours (excludes “found down” of unknown duration. All witnessed cardiac arrest: consider all patients who survived the cardiac arrest as candidates if return of circulation was quick and/or effective circulation was maintained during resuscitation Resuscitation started within 5 to 15 minutes of arrest Restoration of systemic circulation within 60 minutes of initiation of ACLS (if onset outside of the hospital) and systolic BP ≥ 90 mmHg Enrollment and initiation of hypothermia within 90 minutes of initiation of ACLS Informed consent obtained from family NOTE: If post-arrest intervention is needed, that takes precedence over therapeutic hypothermia. 140 Induced Hypothermia EXCLUSION Criteria Evidence of another reason to be comatose (e.g., drug overdose, status epilepticus) Pregnancy A known terminal illness preceding the arrest Known, pre-existing coagulopathy or bleeding disorder Pre-existing DO NOT INTUBATE code status and patient not intubated as part of the resuscitation efforts Arrest < 5 minutes or > 15 minutes prior to resuscitation being initiated CPR failed to achieve spontaneous circulation within 1 hour (as evidenced by palatable pulse for > 5 minutes) Unfavorable cerebral performance prior to arrest Arrest > 15 minutes prior to initiation of ACLS, hypotension, prolonged hypoxia (O2 sat < 85 for > 15 minutes) Failure to achieve favorable cardiac status EKG evidence of ischemia, due to increased risk for malignant ventricular dysrhythmia Failure to obtain informed consent Significant cardiac dysrhythmia or cardiac instability Evidence of sepsis Cardiogenic shock (systolic BP < 90 mmHg) Coagulopathy or thrombocytopenia QT interval > 40 milliseconds 141