Outpatient Services and Medicare Three Day Window
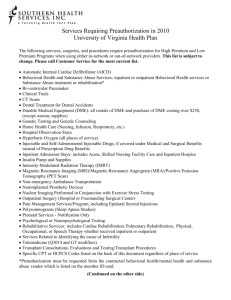
advertisement

DEPARTMENT: Health Information Management Services PAGE: 1 of 5 EFFECTIVE DATE: May 31, 2004 POLICY DESCRIPTION: Outpatient Services and Medicare Three Day Window REPLACES POLICY DATED: 4/3/98; 8/1/00; 6/1/02 REFERENCE NUMBER: HIM.GEN.001 SCOPE: All personnel responsible for performing, supervising or monitoring coding of services that meet Medicare’s Three Day Window criteria, including, but not limited to, the following departments: Admitting/Registration Resource Management Ethics & Compliance Officers Patient Accounting/Business Office Health Information Management Services Facility Health Information Management Ancillary Departments Administration Nursing Case Management/Quality Service Centers Finance PURPOSE: To ensure that medical records for outpatient services and for inpatient services falling within the Centers for Medicare and Medicaid Services (CMS) regulations for the Three Day Window are processed and coded according to standards as outlined in this policy. Specific guidelines on billing procedures are documented in the BILLING-Outpatient Services and Medicare Three Day Window Policy, GOS.BILL.001. POLICY: When Medicare claims are combined for billing purposes under CMS regulations for Three Day Window, the outpatient medical records must not be combined with inpatient admission medical records. Coded data will be combined for purposes of claim submission only. For situations in which there is an immediate transfer from outpatient status to inpatient status with no break in service, outpatient medical records must be combined with inpatient admission medical records and the entire medical record must be coded as an inpatient admission. PROCEDURE: In addition to the steps listed in the BILLING-Outpatient Services and Medicare Three Day Window Policy, GOS.BILL.001, the following must be performed to ensure that Medicare medical records are processed in accordance with accepted standards: 1. If outpatient services are rendered and the patient is immediately transferred to inpatient status, the registration personnel must use a single account number for use with the inpatient and outpatient claim as this is considered to be one encounter. a. The entire encounter, including any outpatient procedures, must be coded according to the Coding Documentation for Inpatient Services Policy, HIM.COD.001. b. The entire encounter must be abstracted under the single account number. c. All documentation for the visit must be filed in one medical record admission. d. Patient type should reflect inpatient status. 5/2004 DEPARTMENT: Health Information Management Services PAGE: 2 of 5 EFFECTIVE DATE: May 31, 2004 POLICY DESCRIPTION: Outpatient Services and Medicare Three Day Window REPLACES POLICY DATED: 4/3/98; 8/1/00; 6/1/02 REFERENCE NUMBER: HIM.GEN.001 e. Guidelines should be developed at the hospital to ensure consistency in determining which single account number to use. 2. If outpatient services are rendered and the patient goes home, the registration personnel must use one account number for the encounter. a. This encounter must be coded according to the Coding Documentation for Outpatient Services Policy, HIM.COD.002. b. The encounter must be abstracted under the outpatient account number. c. The outpatient record must be filed per the facility’s outpatient record filing policy and procedure. 3. If a Part A acute Medicare inpatient admission occurs within three days of an outpatient service provided at the same hospital, a new account number must be assigned for the inpatient admission. (See the BILLING- Outpatient Services and Medicare Three Day Window Policy, GOS.BILL.001.) a. The outpatient encounter must be: i. coded following the Coding Documentation for Outpatient Services Policy, HIM.COD.002; ii. abstracted under the outpatient account number; and iii. filed per the facility’s outpatient record filing policy and procedure. b. The inpatient admission must be: i. coded following the Coding Documentation for Inpatient Services Policy, HIM.COD.001; ii. abstracted under the inpatient account number; and iii. filed per the facility’s inpatient record filing policy and procedure. c. For billing purposes, Health Information Management (HIM) Department personnel must review the inpatient and outpatient records in order to accomplish the following: i. for any diagnostic outpatient service, provide Business Office, or Service Center staff with the sequence of the combined outpatient and inpatient ICD-9-CM diagnosis and procedure code(s) following the Coding Documentation for Inpatient Services Policy, HIM.COD.001. Recalculate the DRG based on any coding changes and provide this information to Business Office staff. See Attachment 1 for a list of revenue codes defined as diagnostic; OR ii. for non-diagnostic or therapeutic outpatient services, determine if the services are related. If the services are not related, notify the Business Office or appropriate Service Center that the claims should not be combined. Related services are defined as those in which there is an exact match (for all digits) between the ICD-9-CM diagnosis code assigned for the outpatient visit and principal ICD-9-CM diagnosis code assigned for the inpatient stay; iii. for related non-diagnostic or therapeutic outpatient services, the claims must be combined. 5/2004 DEPARTMENT: Health Information Management Services PAGE: 3 of 5 EFFECTIVE DATE: May 31, 2004 POLICY DESCRIPTION: Outpatient Services and Medicare Three Day Window REPLACES POLICY DATED: 4/3/98; 8/1/00; 6/1/02 REFERENCE NUMBER: HIM.GEN.001 Related services are defined as those in which there is an exact match (for all digits) between the ICD-9-CM diagnosis code assigned for the outpatient visit and principal ICD-9-CM diagnosis code assigned for the inpatient stay; Sequence the diagnoses and any procedure codes according to the Coding Documentation for Inpatient Services Policy, HIM.COD.001; recalculate the DRG; and forward this information to Business Office or Service Center staff for use in submitting the claim. d. For accounts determined to meet the requirements for the Medicare three-day window, Business Office or Service Center personnel must combine the inpatient and outpatient charges for all related services and submit one claim for all related services as defined by the BILLING-Outpatient Services and Medicare Three Day Window Policy, GOS.BILL.001. 4. If an inpatient admission subsequently occurs within three days of an outpatient service performed in another hospital or entity that is wholly owned or operated by the admitting hospital, the inpatient admission medical record is processed independently of the outpatient record from the facility providing the outpatient services. (See the BILLING-Outpatient Services and Medicare Three Day Window Policy, GOS.BILL.001.) a. The inpatient admission must be: i. coded at the admitting hospital following the Coding Documentation for Inpatient Services Policy, HIM.COD.001; ii. abstracted at the admitting hospital under the inpatient account number; and iii. filed at the admitting hospital per the facility’s inpatient record filing policy and procedure. b. The outpatient encounter from the facility providing the outpatient services must be: i. coded at the facility providing the outpatient service following the Coding Documentation for Outpatient Services Policy, HIM.COD.002; ii. abstracted at the facility providing the outpatient service; and iii. filed at the facility providing the outpatient service. c. HIM Department, Business Office, Service Center and/or Admitting/Registration personnel from the admitting hospital must contact the HIM Department and Patient Accounts Department personnel of the facility that provided the outpatient service in order to: i. determine if claims must be combined; and ii. compile charges and ICD-9-CM coded diagnoses and procedures for the outpatient account meeting the criteria for the Three Day Window. d. HIM Department personnel must combine the inpatient and outpatient codes according to the Coding Documentation for Inpatient Services Policy, HIM.COD.001. e. Business Office or Service Center personnel must combine charges for submission of the inpatient claim. 5/2004 DEPARTMENT: Health Information Management Services PAGE: 4 of 5 EFFECTIVE DATE: May 31, 2004 POLICY DESCRIPTION: Outpatient Services and Medicare Three Day Window REPLACES POLICY DATED: 4/3/98; 8/1/00; 6/1/02 REFERENCE NUMBER: HIM.GEN.001 5. If an inpatient admission occurs within three days of an outpatient service performed in a physician’s office that is wholly owned or operated by the admitting hospital (see the BILLINGOutpatient Services and Medicare Three Day Window Policy, GOS.BILL.001), the inpatient admission medical record is processed independently of the physician office visit. a. The inpatient admission must be: i. coded at the admitting hospital following the Coding Documentation for Inpatient Services Policy, HIM.COD.001; ii. abstracted at the admitting hospital under the inpatient account number; and iii. filed at the admitting hospital per the facility’s inpatient record filing policy and procedure. b. The outpatient encounter from the physician office providing the outpatient services must be coded at the physician office providing the outpatient service following physician office coding and documentation guidelines. HIM Department, Business Office and/or Admitting/Registration personnel from the admitting hospital must contact physician office personnel of the physician office that provided the outpatient service in order to: i. determine if services must be combined on a single claim (technical component only); and ii. compile charges and ICD-9-CM coded diagnoses and procedures for the services meeting the criteria for the Three Day Window. c. HIM Department personnel must combine the inpatient and outpatient codes according to the Coding Documentation for Inpatient Services Policy, HIM.COD.001. d. Business Office personnel must combine charges for submission of the inpatient claim that meets Medicare Three Day Window criteria. 6. On a daily basis, the HIM Department personnel must discuss the “Three Day Window Report” with Admitting/Registration and Business Office personnel to determine if any patients have received outpatient services within the applicable “window.” Communication between HIM Department, Admitting/Registration, and Business Office personnel must be established. a. Admitting/Registration or Business Office personnel must communicate all occurrences of outpatient services provided within the “window” of an inpatient admission that meet the criteria as defined in the BILLING-Outpatient Services and Medicare Three Day Window Policy, GOS.BILL.001. b. HIM Department personnel must review all accounts in the Three Day Window in order to provide the accurate sequencing of codes and DRG recalculation following the above procedures. 7. Review of remittance advice rejections relation to this policy and the BILLING - Outpatient Services and Medicare Three Day Window Policy, GOS.BILL.001 must be performed by the HIM Department, Business Office or Service Center at least semi-annually (or more frequently as 5/2004 DEPARTMENT: Health Information Management Services PAGE: 5 of 5 EFFECTIVE DATE: May 31, 2004 POLICY DESCRIPTION: Outpatient Services and Medicare Three Day Window REPLACES POLICY DATED: 4/3/98; 8/1/00; 6/1/02 REFERENCE NUMBER: HIM.GEN.001 directed by company initiatives or facility leadership) and the results reported to the Facility Monitoring Oversight Group. Reasons for rejection and resolution strategies must be documented in accordance with the Coding Documentation for Inpatient Services Policy, HIM.COD.001. 8. The HIM Department, Admitting/Registration, and Business Office or Service Center must develop a communication tool to ensure compliance with this Policy. DEFINITIONS: Window: Three (3) calendar days prior to an inpatient admission for acute care Prospective Payment System (PPS) (DRG reimbursed) facilities/units and one day prior to an inpatient admission for hospitals or units exempt from acute care PPS. Diagnostic Services: An examination or procedure to which the patient is subjected, or which is performed on materials derived from a hospital outpatient, to obtain information to aid in the assessment of a medical condition or the identification of a disease. Among these examinations and tests are diagnostic laboratory services such as hematology and chemistry, diagnostic X-rays, isotope studies, EKGs, pulmonary function studies, thyroid function tests, psychosocial tests and other tests given to determine the nature and severity of an ailment or injury. See GOS.BILL.001 for additional information. Non-Diagnostic Services: Services and supplies furnished as an integral, although incidental, part of a physician's professional service in the course of diagnosis or treatment of an illness or injury. Related Services: Services are related when there is an exact match (for all digits) between the ICD9-CM principal diagnosis code assigned for both the outpatient services and the inpatient stay. REFERENCES: Federal Register, February 11, 1998, Vol. 63, No. 28, pp.6864-6869 St. Anthony’s Medicare Billing Compliance Guide (pp 6-10 through 6-14) & (pp 8-75 through 8-79)* American Hospital Association –Legal Update #6 and #7* Coding Documentation for Inpatient Services Policy, HIM.COD.001 Coding Documentation for Outpatient Services Policy, HIM.COD.002 Outpatient Services and Medicare Three Day Window Policy, GOS.BILL.001 *Non-Authoritative Resources 5/2004 ATTACHMENT 1 Revenue and/or HCPCS Codes Meeting Criteria for Diagnostic Services 254 Drugs incident to other diagnostic services 255 Drugs incident to radiology 30X Laboratory 31X Laboratory pathological 32X Radiology diagnostic 341 Nuclear medicine, diagnostic 35X CT scan 40X Other imaging services 46X Pulmonary function 48X Cardiology with CPT codes (includes but are not limited to): 93015, 93307, 93308, 93320, 93501, 93503, 93505, 93510, 93526, 93541, 93542, 93543, 93544, 93545, 93561, or 93562 53X Osteopathic services 61X MRI 62X Medical/surgical supplies, incident to radiology or other diagnostic services 73X EKG/ECG 74X EEG 92X Other diagnostic services Note: Any services, items and/or supplies that are integral to the performance of a diagnostic procedure also need to be combined with the inpatient admission. For example, pharmacy items and injections provided in conjunction with a diagnostic radiology procedure subject to the three day window, must also be combined with the inpatient account. Attachment to HIM.GEN.001