Sex organs and hormonal control
advertisement

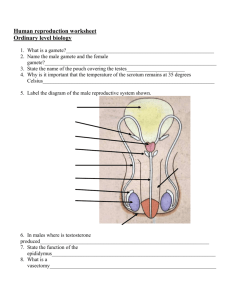
HIGHER HUMAN BIOLOGY UNIT 2 THE CONTINUATION OF LIFE Reproduction Development Sex organs and hormonal control This section looks at the male and female reproductive organs and the related hormones. Major body changes in males and females at puberty At puberty a number of profound changes take place, which bring about sexual maturity and the ability for males and female to ________________________. Puberty starts off with the release of hormones from the pituitary gland. The release of these hormones first occurs several years before sexual maturity is reached. It causes the start of the growth spurts, which results in the attainment of full adult height. During this growth spurt, four important physical changes occur: 1. Changes in body height 2. Changes in body weight/shape 3. Development of primary sexual characteristics (procession of the male of female genitals which are present from birth 4. Development of secondary __________ characteristics Secondary Sexual Characteristics Male 1. The penis and testes grow and develop 2. Pubic hair appears about one year after the penis and testes have started to increase in size. Armpit, facial and body hair appear after the pubic hair has completed its growth. 3. The hair becomes coarser and the pores enlarge. The sweat producing glands become more active, which may cause odour. Perspiration increases. 4. The muscles increase markedly in size and strength, giving shape to the arms, legs and shoulders. 5. The voice begins to change due to enlargement of the voice box (larynx). At first it becomes husky and later drops in tone. Voice squeaks are common when maturing is rapid. Female 1. The oviducts, uterus and vagina grow and develop. 2. The mammary glands (breasts) grow and develop. 3. Menstruation begins. 4. Adult body hair develops e.g. in armpits and pubic region. 5. The hips become wider and rounder due to enlargement of the pelvic girdle (hip girdle) and to the development of adipose tissue (under skin) fat. 6. The hair becomes coarser and the pores enlarge. The oil producing glands become more active. Infection of these glands can cause acne. Perspiration increases. The Male Reproductive System The diagram below shows us the different parts of the male reproductive system. You must be able to identify/label these parts and know their specific function. Use your text book or other class resources to match up the structures with their functions Structures- Testis, interstitial cells, penis, prostate gland, Sperm duct, epididymis, seminal vesicle, urethra and seminiferous tubules Structure Function Site of sperm and testosterone production Outer area of the testis Tubes in the testis where sperm are produced from sperm mother cells during meiosis. Located between the seminiferous tubules in the testis. Produce testosterone, which passes directly in to the blood. Tube through which spermatozoa is ejaculated and urine is excreted. Consists of erectile tissue and blood vessels. The urethra is extended into the penis. Secretes a viscous liquid rich in fructose and prostagladins. Fructose provides sperm with the energy required to swim. Prostagladins are hormone-like compounds, which stimulate contractions of the female’s reproductive tract. Secretes a thin lubricating liquid containing enzymes whose actions maintain the fluid medium at the optimum viscosity for sperm mobility. Tube through which spermatozoa leave the testis and enter the urethra. Spermatozoa Sperm are motile (they can move). During sexual intercourse inside the female’s body, the sperm move from the _____________________________ __________________________________ in the _____________________________________ to the _____________________________________ and then to the ______________________________________________to leave the males body. The sperm swim through the female uterus and along the oviducts where they may meet an egg/ovum and fertilisation will take place. The female reproductive system The diagram shows us the different parts of the female reproductive system. You must be able to identify/label these parts and know their function. Match up the structures and the functions using classroom resources. Structures- ovary, oviduct, vagina, endometrium, cervix and uterus Structure Function Site of ovum/egg production through meiotic division. Embryo develops here Neck of the uterus Site of fertilisation. Tube through which sperm swim to the egg and through which the egg is propelled down towards the uterus. Lining of the uterus Birth canal. Area of the female’s body where the male’s penis enters The ovaries In the female reproductive system diagram, you can see inside the ovaries. This is showing us the formation of the ovum by meiotic division. This process does not occur around the ovary as the diagram indicates but it is a step-by-step process in the one place in the ovaries. The developing ovum is contained in an immature ______________________________ _________________________. The Graafian follicle develops and the ovum is released during ________________________________. The Graafian follicle then develops into the _________________________ _________________________, which forms and then begins to degenerate. Structure Graafian follicle Function Encloses the developing ovum and secretes ______________________ Corpus luteum Develops after ovulation and secretes ______________________ Hormonal Control Hormones are the chemical messengers produced by the ductless glands of the ______________________system. Released in small amounts into the ______________, they circulate all around the body until they reach their own target organ(s). Only there do they have an effect. Thus, glands control the workings of the other parts of the body. Hormone molecules do not last long. The _________________destroys them as they pass through it in the blood. So if the gland is controlling a long-term process like growth, it must continually make fresh hormone. On the other hand, if the hormone’s effect is needed for only a short-time e.g. to help control digestion, then the liver makes sure it does not overdo it. Pituitary Hormones The pituitary gland is a small gland about the size of a pea. It is located underneath the hypothalamus. Despite its small size it is known as the ______________________________ gland of the body because its hormones actually stimulate other endocrine hormones. If anything goes wrong with the pituitary other parts of the body may be affected. Among the pituitary hormones which stimulate other glands, are Thyroid-stimulating hormone (TSH), Folliclestimulating hormone (FSH) and Luteinising hormone (LH). We need to learn about these other pituitary hormones at the end of this unit. The reproductive organs are also controlled by pituitary hormones. Hormonal control of the reproductive organs Hormones are chemical messengers produced by a persons ________________________________ system glands. Hormones are secreted directly into the blood stream to be carried to a _____________________________ tissue to bring about a __________________________. The ______________________________ in the brain is part of the endocrine system and releases hormones that are gonadotrophic, this means that their target organs are the _____________________________________ organs. The gonadotrophic hormones are released when a person reaches ____________________________________. Male hormonal control Male time line Males born Puberty Death Fertile due to their ability to produce sperm The two gonadotrophic hormones in males are: _________________(follicle stimulating hormone) _________________(interstitial cell stimulating hormone) Hormone Function FSH ICSH Importance of Testosterone Testosterone is the male sex hormone that causes the appearance of the secondary male sexual characteristics. Production starts at puberty and is stimulated by ICSH from the pituitary. Testosterone is released from the ____________________________ _______________________________ in the testis. Testosterone also stimulates___________________________________________production. Testosterone activates the prostrate gland and seminal vesicles into producing their secretions that will join with the sperm to produce semen. Self regulation of testosterone The level of testosterone produced is controlled by a ____________________________ ______________________ ______________________________. (self regulating mechanism) When the levels of testosterone reaches a certain level in the blood (too high). Testosterone inhibits the production of the gonadotrophic hormones FSH and ICSH by the ____________________ ______________________ gland. ICSH stimulates the testosterone production so its reduction reduces testosterone production. When the levels of testosterone drop to a certain point because there is not enough ICSH to produce it (too low), then there is a re-start to the pituitary gland producing ICSH and FSH and an ________________________ in testosterone production. It is a continual cycle. Hormonal control of the ovaries Female time line Female born puberty menopause death Female fertile due to the production of ova/eggs Reproduction depends on a regular pattern of events in females called the ___________________________ ___________________________. This cycle usually lasts about 28 days and begins with the breaking away of the uterus lining along with some blood through the vagina. This is called_______________________________. Men can continue producing sperm throughout life but women lose their ability to have children between about 40 and 50. Menopause is the technical name for this loss of ____________________, but it is commonly known as the “change of life”. At this time ovulation and menstruation stop and the reproductive organs decrease in size. In females the 28 day cycle is dependant on pituitary and ovarian hormones. Pituitary Hormones The two gonadotrophic hormones released from the pituitary gland that are involved in the females reproduction system are: ________________(follicle stimulating hormone) ________________(luteinising hormone) The two ovarian hormones released from the tissues inside the ovaries are: __________________________________ __________________________________ FSH (follicle stimulating hormone) Stimulates the development of each immature Graafian follicle inside the ovary. Stimulates the ovarian tissue into secreting ___________________________. LH (luteinising hormone) Triggers ________________________ Release stimulated by the ovarian hormone _____________________________. Stimulates the development of the Graafian follicle into the _______________________ ________________________. The development of the corpus luteum brings about the release of the ovarian hormone ________________________________ 9 Ovarian Hormones Oestrogen Oestrogen stimulates the _________________________ of the inner layer of the uterus called the _____________________________________. Oestrogen stimulates the repair of the endometrium Oestrogen also stimulate the secretion of the Pituitary hormone ________________________. LH trigger ovulation and the development of the Graafian follicle into the ____________________ ______________________, which in turn stimulates the production of the other ovarian hormone __________________________ Oestrogen also causes the appearance of the female secondary sexual characteristics at puberty. These include growth of _________________ and breasts. 10 Progestertone Stimulates the_________________________ of the uterus lining, the endometrium into a spongy layer rich in blood vessels. This is in anticipation that an egg will be fertilised and become __________________________________ in the wall of the uterus Progesterone also inhibits the secretion of _____________and _____________________ by the anterior pituitary to stop the development of another ovum 1. Fill in the table to summarise the male and female hormones Male Hormone Secreted from Target area Effect FSH ICSH Testosterone 11 Females Hormone Secreted from Target area Effect FSH LH Oestrogen Progesterone The female menstrual cycle Starting at puberty the female reproductive system undergoes a regular sequence of events, repeated monthly, called the menstrual cycle. One menstrual cycle lasts about ________ days, although it can be longer or shorter than this depending on each individual female. During one menstrual cycle the endometrium degenerates and menstruation occurs, an ovum is released from an ovary and the lining of the uterus endometrium is repaired and thickened. The endometrium develops to a stage at which it can receive and support/nourish the ovum should this be fertilised and begin to grow into an embryo. These events are controlled by hormones from the ovaries and from the anterior pituitary gland. Events during one menstrual cycle There are two main phases in the menstrual cycle; Follicular Phase Luteal Phase 12 Follicular phase At the beginning of this phase the endometrium breaks down and menstruation occurs. During the first half of the menstrual cycle, __________________ from the pituitary gland stimulates the development and maturation of the Graafian follicle and the production of the ovarian hormone _______________________ by the ovarian tissues. The increase in oestrogen causes ___________________ to the endometrium and eventually the high concentration of oestrogen causes a surge of ____________________ to be released from the pituitary to cause ovulation on Day 14. The ovum will now move along the oviduct. Luteal phase During the second half of the cycle (following ____________________________________), LH stimulates the Graafian follicle to become the __________________________ _____________________________. The gland like structure secretes ___________________________. The rise in progesterone stimulates the _____________________________ of the endometrium, so that it is ready to accept an implanted egg. The high level of oestrogen and progesterone inhibit the release of ______________ and ________________., this results in no new follicle developing.. This is a further example of a negative ____________________ _________________________. The lack of LH leads to the degeneration of the corpus luteum, which in turn leads to a drop in the _________________________________levels and the endometrium can no longer be maintained. Menstruation begins and the cycle starts again if a fertilised egg has not been implanted. 13 menstruation new cycle LH Concentration of FSH and LH in blood FSH progesterone oestrogens Concentration of oestrogens and progesterone in blood 1 2 3 4 5 6 7 8 9 10 11 12 13 141516 17 18 19 20 21 22 23 oocyte 25 26 27 28 Time (days) OVARY primary follicle UTERUS (thickness of endometrium) developing follicles OESTROGENS ovulation corpus luteum PROGESTERONE & SOME OESTROGENS 5 1 14 28 menses follicular phase luteal or secretory phase 14 Use the diagram to fill in the table to summarise the main events in the menstrual cycle. Days Events Hormone controlling event Drop in 1-5 ___________________________ 1-5 Graffian follicle is starting to mature 1-5 Level of oestrogen begins to rise 6-13 Graafian follicle matures 6-13 Level of oestrogen rises ______________________ 6-13 The endometrium is __________________________ 11-13 Level of LH_______________________________ 14 Peak of ________________ 14-22 Levels of ______________________ increase 14-22 Graffian follicle develops into the _________________ ________________________ 14-22 _______________________________ is thickening 22-28 The ___________________ ___________________ degenerates 28 Menstruation begins 15 Fertilisation About 3.5 ml of semen, containing up to 350 million sperm, are ejaculated into the female reproductive system during copulation (sexual intercourse), but only one sperm is needed to fertilise an ovum. A large number of sperms are necessary because many sperm _____________________________ to complete the long journey to the oviduct where fertilisation usually occurs. Sperms swim through the __________________ into the uterus and up to the oviducts. Sperms are helped by being sucked into the uterus by muscular contractions of its walls caused by the stimulation of sexual intercourse. If a ripe ovum is present at the time of sexual intercourse then fertilisation occurs, usually in the upper third of an ____________________. The ovum is surrounded by a membrane, which sperm must penetrate. The first sperm to reach the ovum releases a chemical, which softens the membrane at the point of contact, allowing the sperm to enter and move into the ovum’s cytoplasm. Immediately after penetration by a sperm the membrane undergoes rapid changes, which make it impenetrable and cause it to lift away from the surface of the ovum. It is now called a fertilisation membrane and forms a barrier to the entry of other sperm. Only the _______________of a sperm enters the ovum. It moves through the cytoplasm towards the nucleus of the ovum and the two fuse together. This fusion brings together the inherited characteristics of the mother and the father. The ______________ chromosomes from the sperm and the ______________ from the ovum in the zygote. A fertilised ovum is called a Zygote. 16 A sperm cell fertilising an egg. Picture courtesy of wwwPDImages.com Continuous and cyclical fertility Males have relatively constant levels of FSH, ICSH and testosterone and are therefore, fertile (able to produce sperm) all the time. (_____________________________ __________________________). Females have changing levels of FSH, LH, oestrogen and progesterone which result in _____________________________________ ________________________________________. They produce an egg only once per month and therefore, have only one fertile period. Infertility Infertility is the inability to conceive. There are a number of causes for infertility in couples. 1. Failure to Ovulate This is often hormonal in origin due to disorders of the endocrine system or due to emotional stress. 2. Blockage of Oviducts (fallopian tubes) This can be due to infections, cysts (abnormal growths or swellings), fibroids (non cancerous tumours of the uterus), cancer etc. or to spasms (involuntary muscular contractions) in the oviducts due to stress. 3. Failure for the fertilised ovum to Implant in the wall of the uterus The fertilised egg fails to embed in the uterine wall due to hormonal imbalance, infections etc. 4. Low Sperm Count in the Male This can be due to hormonal problems, stress, poor health etc. 20,000,000 ml semen (infertile) 17 Cause of Underlying factor Treatment infertility failure to ovulate 1. Hormonal imbalance (failure of FSH & LH secretion) Fertility drugs to stimulate FSH and LH secretion. Use LH taken from the placenta of fertile women. 2. Prolonged use of the pill Use FSH taken from blood and urine of menopausal 3. Emotional stress women. 4. Poor health caused by smoking, excessive alcohol, obesity or drugs blockage of the 1. Tissue growths (cyst or tumour) Laser treatment to clear blockage oviduct 2. Infections IN VITO treatment (IVF) 3. Spasms in the tube caused by stress Use of drugs to stop contractions 1. Hormonal imbalance Fertility drugs to restore a normal cycle implantation failure of the egg caused by the ovaries failing to secrete hormones. low sperm count 1. Problems secreting FSH & ICSH Hormone treatment, use of controlled volumes of testosterone 2. Emotional stress Artificial insemination 3. Poor health less stress and men watching their diet and stopping smoking. Infertility can also be caused by smoking, drug abuse, obesity and venereal diseases (sexually transmitted infections). Treatment for Infertility 1. Fertility Drugs These are given to correct hormone imbalance. Some contain FSH and LH. Some stimulate the secretions of FSH and LH. Others are substances which prevent muscular spasms in the oviducts which would hinder conception. 2. In Vitro Fertilisation This literally means fertilisation in glass i.e. “test tube baby techniques”. Fertility drugs are used to stimulate the woman’s ability to produce several mature eggs at once. These are then removed by surgical techniques through her abdomen. The eggs are then fertilised with sperm in a special fluid medium and allowed to divide. The “bestlooking” embryos are then inserted into the woman’s uterus through her vagina and she has to hope that at least one will implant in the uterus lining and develop as normal. 18 Using the diagram opposite, describe the stages involved in the treatment of infertility using IVF. 3. Artificial Insemination Insemination is the release of semen into the female reproductive tract, this usually occurs naturally during intercourse. Artificial insemination is the release of semen into the female reproductive tract by some means other than intercourse. Artificial insemination can be used as a treatment for infertility, if a man has a ___________________or if they are sterile. 19 4. A surrogate mother A surrogate mother can be used to treat infertility, by placing an embryo inside another woman for her to carry. Contraception Contraception:- Methods to prevent a female from conceiving/becoming pregnant by natural or artificial means. Natural Methods of Contraception A woman’s fertile period can be calculated (either to try and ensure or to try and avoid conception) by a combination of timing the stages of the menstrual cycle and by monitoring subtle changes in body temperature and cervical mucus. Sympto-thermal method/Rhythm method The sympto-thermal method combines observation of cervical mucus with charting the basal body temperature, and, if acceptable to the individual woman, the cyclical changes of the cervix. Use is also made of a formula, related to the shortest menstrual cycle, to double-check the beginning of the fertile period. Other symptoms such as breast tenderness; mid-cycle pain and mood swings are recorded. Cervical mucus – The cells lining the cervix secrete mucus, which lubricates the vagina. Three or four days before ovulation, under the influence of oestrogen mucus appears in the vagina. At first it is thick, sticky and opaque, the pre-ovulatory phase. The mucus then becomes wetter, slippery and crystal clear like albumen. Through this mucus, sperm can ascend the reproductive tract. This is the fertile phase. After ovulation, progesterone changes the mucus so that it becomes antagonistic to sperm, and forms a plug blocking the cervical canal. This is the late or postovulatory infertile phase, which lasts until the beginning of the next period. The mucus can be used to calculate the female ______________________ ___________________________. The basal body temperature - To use temperature in the rhythm method, a woman must record her temperature before getting up, drinking tea or any other activity. A cycle in which ovulation has occurred is characterised by a __________ temperature chart. The temperature remains at the lower level until ovulation, when there is a rise of about 0.5 C. This is due to the thermogenic action of progesterone. The postovulatory infertile phase begins after the third recording at the higher level. 20 The cervix uteri – the cervix is the most sensitive organ in the body to the effect of oestrogen. Not only does it produce the mucus, but also undergoes changes, which can be detected by gentle palpation with the fingertip. Women who have used a diaphragm will have learnt to locate the cervix. During the infertile phase it appears to be long and firm and the os is tightly________________. During the fertile phase it shortens, softens and the os ___________________slightly to admit the fingertip. This observation is not essential, but gives valuable information and is particularly useful for women who use this method of family planning after childbirth or during the pre-menopause. This rhythm method enables each woman to recognise day by day whether she is in an infertile state when sexual intercourse will not lead to conception or whether she is in the fertile phase of the cycle when conception is possible. Females have a normal period of fertility that last for ____ to ____ days. (Caution should be taken because sperm can survive in the female body for around ________ days and this can extend the fertile period) (NB All methods of natural contraception require careful training before they can be relied upon. Advice from professional family planning organisations of doctors should always be sought) Jill’s case – calculating a fertile period Jill has a regular 28 day cycle. In February, for example: Her period began on Sunday February 1st It continued until the 5th Her cervix was closed from the 5th to the 9th She noticed sticky mucus on the 9th to 11th and that the cervix was open until the 15th There was slippery, stretchy mucus from the 12th to 14th This was replaced by sticky mucus from the 15th to 18th and dry days until the next period began on March 1st. Jill took her temperature at 7.00am every day Date (feb) 1 Date (feb) 22 2 3 23 4 24 5 25 6 7 26 8 27 9 28 10 11 1 2 12 13 14 15 16 17 18 19 20 21 21 Use this information to complete a “Sympto-Thermal chart” to identify Jill’s fertile period. In the row above the dates on the chart put in the letter C or O to indicate whether the cervix is open or closed. In the boxes below the dates put in the letters:P indicate Period D for Dry Days SM for Sticky Mucus FM for Fertile mucus. Divide the chart into 3 regions shade each section of the table a different colour: Pre-ovulatory infertile days (blue), Fertile days (red) and Post-ovulatory days (yellow). NB. The egg will normally live for 24–28 hours after ovulation. The sperms can live up to 5 days after intercourse. Work out the key days for Jill using the 28 day regular cycle. This will help us work out on which days of the month she is fertile: She’s most likely to ovulate on day _________. The egg is likely to live until day ___________ of ____________. The earliest likely time for intercourse to result in pregnancy is on day ________ or ____________. The latest likely time for intercourse to result in pregnancy is on day 15 or __________. If Jill had intercourse on the following days is it likely that she would have become pregnant? (circle the correct answer) 1. 22.00 Sat 7th not possible just possible likely 2. 06.00 Mon 16th not possible just possible likely 3. 22.00 Fri 20th not possible just possible likely In March Jill had intercourse on the 19th (which had been an infertile day in February) and she became pregnant. Suggest a reason why she was still fertile at that time. (NB The infertile periods mentioned apply to Jill only. Each individual must perform her own calculations, after expert guidance 22 Hormonal Methods of Contraception All these methods involve the use of natural or, more usually synthetic/artificial female sex hormones, (_________________ and _________________). Differing combinations of these can have several effects resulting in the prevention of conception. (a) inhibiting follicle maturation and ovulation (b) thickening the cervical mucus forming a barrier to sperms (c) making the endometrium less suitable for implantation Combined Pill (oestrogen and progesterone (a synthetic progesterone) Taken by mouth – daily. 21 days active pill: 7 days no pill or a ‘dummy’ pill leads to Menstruation. Effects – a), b), c). Mini Pill (progesterone only) Taken by mouth – daily Effects - a) (in some women), b), c). Post Coital (Morning After) Pill (recommended as emergency contraception only!) A unique combination of oestrogen and progesterone taken within 72 hours of intercourse for a duration of 2 days. Effects - a) (if it has not already occurred) plus shortening of menstrual cycle leading to early menstruation. Implants (normally progesterone) A small capsule of progesterone, placed under the skin releases the hormone slowly for up to 5 years. Effects – a) (in some women), b), c) Injectables (synthetic forms of female hormones) 2-3 monthly injections into muscle (eg buttock, thigh, arm etc.) of long lasting forms of the hormones. Slow release from the muscle ensures protection for up to 12 weeks at a time. Effects – a), b), c) Tick the appropriate boxes in the table to explain the effects of each method of artificial contraception Type of Inhibiting Thickening cervical Making the contraception follicle mucus forming a endometrium less maturation barrier to sperm suitable for implantation Combined pill Mini pill Morning after pill Implants Injectables 23 Vasectomy This diagram shows a simplified vasectomy, explain how this prevents conception Embryo Development Cleavage The fertilised egg ( zygote ) is propelled towards the uterus mainly by wave-like contractions ( _____________ ) of the oviduct. However, it is also helped along by the beating movements of the _________ lining the tube. During this journey, which takes about 7________days, the zygote divides several times by a process known as CLEAVAGE. 24 Implantation To begin with, the cells resulting from cleavage of the zygote all appear ______________________ to each other. However, quite soon it becomes apparent that some of the new cells are smaller than others. At this stage it is possible to distinguish which cells will form the embryo proper and which will give rise to the embryonic membranes and the _________________. By the time the embryo reaches the uterus it is a hollow ball of cells filled with fluid. It embeds in the lining of the uterus and the outermost layer of cells develops small finger-like projections (__________________), which project into the tissue of the uterus wall. Food and water are absorbed across these villi. As development proceeds, the embryo becomes surrounded by protective membranes. The innermost membrane, the amnion, encloses a fluid-filled cavity in which the embryo is protected by the cushioning effect of the fluid. Meanwhile two other membranes unite to form the placenta. This develops in association with the uterus wall and is connected to the embryo by the _________________________ __________________________. Differentiation The cells in the embryonic area continue to divide by mitosis forming a multi-layered mass of cells, which undergoes _______________________. The unspecialised cells are altered and develop into cells, which have specific functions as part of the permanent tissues. This occurs because during differentiation all the cells start with the same genes and the individual genes are either switched on or off, this means that different types of specialised cells are formed. For example; heart, lung, brain, liver cells etc. 25 Pregnancy and the placenta The period of development between fertilisation and birth is called gestation. Human pregnancy lasts about _____ months or ________ weeks. During this time hormones like progesterone in the mother’s blood prevents the monthly occurrence of menstruation and ovulation. Implantation of a developing __________________ is the signal, which ensures that these hormones flow. If implantation takes place, cells surrounding the embryo produce the hormone HCG which prevents the breakdown of the corpus luteum so that it continues to produce __________________________ . Modern pregnancy tests detect HCG in the urine. (Later in the pregnancy the _______________________________ takes over the role of a temporary endocrine gland and secretes progesterone and oestrogen). A developing embryo must have ________ and food. At first it obtains these directly from its mother’s _________ flowing through vessels in the lining of the uterus. Within 4-5 weeks of implantation, however, food and oxygen are absorbed within the newly developed _______________________. The embryo’s ________________ pumps blood through blood vessels in the umbilical cord into the placental villi. The villi hang inside spaces in the uterus wall filled with the mother’s _________. Transfer of materials across the placenta Mother to foetal blood capillaries Oxygen by _________________________ Glucose by _________________________ diffusion Maternal antibodies by pinocytosis (Foetus gains passive immunity to many diseases until its own immune system develops) Fats Amino acids Mineral salts 26 Foetal to mother’s blood capillaries Carbon dioxide by _____________________ Urea (waste) by _______________________ EXCHANGES BETWEEN MATERNAL AND FOETAL CIRCULATIONS IN THE PLACENTA Draw an arrow into the table to show the direction of transfer and fill in the method of transfer. Substance Direction of Transfer oxygen Foetus Mother carbon dioxide Foetus Mother glucose Foetus Mother antibodies Foetus Mother Method of Transfer Harmful substances The close proximity of the foetal and maternal circulation allows harmful substances to enter the foetal blood circulation. Alcohol Drinking excessive volumes of alcohol during pregnancy can firstly cause ___________________________, but those women who continue during pregnancy let the alcohol enter the foetal bloodstream. The alcohol causes some of the foetal blood vessels to collapse temporarily and the growing tissues (especially the brain) do not receive an adequate ______________________ supply. Alcohol also interferes with the absorption of vitamin B6 and zinc, which is essential for the foetal development. In extreme cases the foetus suffers from ALCOHOL SYNDROME, this includes: Mental disabilities Facial abnormalities Heart defects Development of abnormal joints and limbs Nicotine Nicotine is present in tobacco and smoking during pregnancy has been shown to cause stunted growth of the foetus because carbon monoxide reduces the volume of _______________ the blood can carry. Nicotine in the bloodstream prevents adequate glucose reaching the foetal tissue including the brain cells. Babies born to smokers are on average _____________________ and do not develop intellectually at the same rate as babies born to non-smokers. Heroin Heroin is very addictive and regular use during pregnancy leads to the baby being born an addict, because the heroin travels into the foetal blood and the baby has to go through a gradual __________________ programme. Heroin addicts usually do not take care of themselves (eating badly to fund their habit) and this is reflected in the baby. Babies born to heroin addicts are usually weak and undersized. 27 Thalidomide A drug given to pregnant mothers in the 1950s to help them cope with nausea (morning sickness). This leads to deformed babies. For example, their hands can be joined to their shoulders and feet joined to their hips. Rubella Females are vaccinated against rubella to prevent it; rubella if caught during pregnancy can cause defects to the eyes, ears and heart of the newborn. HIV HIV can pass from mother and affect the foetus. 30% of pregnancies of an infected mother lead to an infected baby. Most HIV babies develop full-blown aids and die very young. Drugs can be used during pregnancy can help prevent the foetus catching HIV, or women can choose to terminate the pregnancy. Mammary glands during pregnancy Oestrogen and progesterone also stimulate ________________________ of the milk-secreting tissues of the mammary glands causing the breast to increase in ___________________ and become prepared for post-natal lactation (milk production). Lactation does not occur during pregnancy due to the lack of the hormone prolactin. Prolactin is secreted by the anterior _____________ gland and it becomes active following the birth of the baby because the levels of oestrogen drop after the expulsion of the placenta with the afterbirth 28 TWINS There are two types of twins: Monozygotic twins (identical) Dizygotic twins (non-identical) Monozygotic Twins Monozygotic twins both originate from the same _____________________ fertilised by a _____________________ ______________________. During cell division, the developing embryo divides to form two separate embryonic areas within the one fluid filled ball. As development occurs the twins have separate amniotic sacs, but share a __________________________. They are ____________________ _______________________ since they derived from the same zygote. Dizygotic Twins Dizygotic twins are formed when _______________ ova are released from the ovary at the same time and fertilised by ____________ different sperm. Each embryo undergoes independent development and posses their own amniotic sac, umbilical cord and ___________________________. They are ___________________ _________________ to one another as normal siblings of the same parents. 29 Effect of the foetus on the maternal immune system The mother’s immune system recognises foetal antigens as foreign or “non-self” i.e. as harmful if it met them. (Antigens are the protein identification markers on the surface of all cells) Normally the placenta acts as a barrier between mother and foetus so preventing recognition of the foetus by the mother. Mixing of foetal blood with the mother’s blood (e.g. during _______________________ or ____________) causes the mother’s immune system to produce antibodies against the foetus. In a subsequent pregnancy these antibodies may cross the placenta and harm the foetus. A good example of this is the “__________________ factor” RHESUS FACTOR In addition to the ABO system of antigens, most people have a further antigen on the surface of the red blood cells. This called ____________________________, people who posses it are said to be rhesus positive (Rh+). People who lack antigen D are rhesus negative (Rh-). 85% of the population of the UK are Rh+. Problems arise when a mother is Rh- and the father is Rh+ This means that the baby could have different Rh factor to the mothers Complete the following punnet squares in the space provided below Determined by dominant allele D Rh+ and recessive d Rh- Woman dd X All offspring Man Woman DD dd Man X Dd All offspring How Rhesus factor effects the mother and foetus If a Rh- mother has a developing Rh+ foetus, the mother’s immune system will regard the antigen D on the foetal blood cells as ________________ or non-self. Normally because the foetal and maternal blood never come in contac,t the first pregnancy is ok. If the blood mixes during birth or miscarriage the foetal blood will comes in contact with the mother’s blood. The mother becomes ____________________. (Mother has produced anti – D antibodies). 30 During the second pregnancy the mother’s immune system will attack and try to destroy the foetal red blood cells because the anti D antibodies will pass through the __________________________ and will join with the foetal red blood cell and the blood ____________________________________. This results in the haemolytic disease of the new born HDNB. HDNB can be treated when blood transfusions are given to the newborn. HDNB can be prevented by giving the mother anti D immunoglobulins soon after the birth of the first Rh+ baby to destroy D antigens on the foetal red blood cells before the mother immune system has the time to respond to them. 31 BIRTH The gestation period of humans is ______________ weeks; the foetus is described as full-term after 38 weeks. Around 38 weeks gentle contractions of the uterus occur and gradually the foetus moves so that its head is close to the cervix ready for birth. Labour now begins involuntary rhythmic contractions of the uterine wall start at the top and move in waves downwards. Early in labour the amniotic sac ________________ (waters breaking) and the cervix ____________. The contractions increase in power and frequency until the baby is expelled from the uterus and delivered through the vagina. Hormonal control of birth Progesterone is produced by the placenta and inhibits muscular of the uterus wall during the pregnancy. Oestrogen levels rise close to the end of the pregnancy and sensitises the uterus wall to the hormone _____________________________________. Oxytocin stimulates contraction of the uterus at birth. Oxytocin is secreted from the __________________________ gland Induced Labour Birth can be induced by gradually injecting oxytocin (or a synthetic hormone which will mimic it’s effects) into the mother’s bloodstream. Breast – Feeding ( Lactation) After the birth of the baby the lacteal glands are ready to produce milk, having been prepared during pregnancy by hormonal influences. The small glands within the breast develop at puberty because of the female hormones. However, they only produce milk under the influence of the hormone _____________________________, which is secreted by the pituitary gland. They physical act of suckling causes further release of prolactin and continuation of milk production. For the first few days after birth the secretion is called _____________________________________ not milk. This is a watery yellowish fluid similar to milk but containing less fat. It has important ingredients for the baby and is said to act as a “laxative” to help clear out the infant’s digestive tract. There are antibodies to diseases in both colostrums and breast milk. This gives the breast-fed child and advantage against disease because it suckles a “short term antibody package” which the bottle-fed child cannot obtain. Breast milk contains all that is needed for the young baby in terms of nutrients and vitamins but there is no iron present. Iron is needed to make haemoglobin so it has to be obtained from the stores that the baby has accumulated while it was in the uterus. After a time it will need iron in its diet. Toxic substances (e.g. organochlorine pesticides, mercury, lead compounds, alcohol, nicotine, heroin) can be excreted in the milk and pass to a breast-fed baby. 32 Typical Composition of Colostrum, Human Breast Milk & Cows’ Milk (mean figures from several sources) per 100ml) Component Colostrum Breast milk Cows milk Total protein g 2.7 1.2 3.3 Antibodies mg 720 315 0 Fat g 2.9 3.8 3.6 Lactose g 5.3 6.9 4.8 Calcium mg 31 33 128 Vit C 4.4 4.3 1.6 Vit A 89 53 34 Powdered cows milk lacks _______________which give the baby protection until its own immune system develops. The pattern of growth after birth Humans have two major stages of rapid growth: Between birth and 5 years Puberty During these growth stages the body changes its body proportions. 33 The body proportions vary through development from foetus to adult. The head of a foetus takes up over _____% of body height compared to an 21 year old adult with head of _____% of the body height. Complete the table below: AGE % OF BODY HEIGHT THAT IS MAE UP OF HEAD 2 month old foetus 5 month old foetus Newborn baby 2 year old 6 year old 12 year old 25 year old The lower limb proportions also change and the limbs make up a larger % The limbs of a foetus takes up ____% of body height compared to a 21 year old adult with the limbs taking uo _____% of the body height. Describe how the growth rate of the brain and head differs from the growth rate of the reproductive organs. ____________________________________________________________________________ ____________________________________________________________________________ ____________________________________________________________________________ 34 Role of the human growth hormone. The human growth hormone (_____________________) is secreted from the pituitary gland, under the control of the hypothalamus. The human growth hormone promotes growth by accelerating the transport of amino acids into the cells of soft tissues and bones and also stimulates the breakdown of fats for energy release. This allow the synthesis of tissue proteins to occur, in particular it promotes the growth of long bones during the adolescence years. This diagram shows the effect of under-production of the human growth hormone during adolescence, or overproduction in adolescence and adulthood. 35 Treatment of dwarfism. Genetic engineers have been able to transfer the gene that carries the code for the production of the human growth hormone ________________ into a bacterium from a human cell, The bacterium then reproduces and produces the human growth hormone. The hormone is then extracted and used to treat children who show the early signs of dwarfism. The major stages of the human growth curve Male Female Average Height Average Weight Average Height Average Weight (cm) (kg) (cm) (kg) 0 51 3.4 50 3.2 0.5 67 7.8 66 7.2 1 76 10.2 75 9.5 2 88 11.5 86 11.0 3 91 13.0 89 12.5 4 95 15.0 93 14.0 5 100 17.0 98 16.0 6 105 18.5 103 17.0 7 110 20.0 108 19.0 8 115 21.5 113 21.5 9 120 23.0 117 23.0 10 125 25.0 124 25.0 11 133 28.0 130 28.0 12 140 31.5 139 32.0 13 145 36.0 145 39.0 14 154 41.0 157 47.0 15 167 53.5 161 53.0 16 175 60.0 164 57.0 17 177 63.0 165 58.0 18 178 65.0 165 58.5 Age (yrs) Draw a line graph of age against height (use red for the girls and blue for the boys). Do the same for weight against age. What can you conclude about age and growth rate? ___________________________________________________________________________________________ ___________________________________________________________________________________________ ___________________________________________________________________________________________ ___________________________________________________________________________________________ ___________________________________________________________________________________________ The peak times of growth are called the infant growth spurt and the adolescent growth spurt. Label these on your graphs. Stick your graphs into the blank pages that follow, 36 37 38 Other pituitary hormones Hormones are the chemical messengers produced by the ductless glands of the endocrine system. Released in small amounts into the blood, they circulate all around the body until they reach their own target organ (s). Only there they have an effect. Thus, glands control the workings of the other parts of the body. Thyroxin Thyroxin is produced in the thyroid gland and is stimulated by TSH. Thyroxin controls the rate at which the tissues use energy ( the _________________________ rate) and so, affects the performance of the whole body. It is especially important during growth and development. A child whose thyroid does not produce enough thyroxin will be stunted in growth and severely mentally retarded. This condition is called cretinism. In adults if insufficient thyroxin is made then the person becomes fat and slow to think and speak (Myxodema). If too much is produced then the person becomes thin, nervous and over-active. Not all pituitary hormones stimulate other endocrine glands. Some have direct control over body processes e.g. Anti-diuretic hormone _____________________________________(adjusts the amount of water in the blood) and the Growth Hormone. If too little of the growth hormone is produced during the childhood years then the person suffers from _______________ or ________________if too much is produced. Insulin Insulin is made in the pancreas by patches of cells called Islets of Langerhans. Insulin lowers the level of ____________ in the blood when it gets too high. If the pancreas cannot make enough insulin then the person suffers from a condition called _______________. Adrenaline Adrenalin is made by the adrenal glands, which lie above the kidneys. It is often called the fight or flight hormone as it prepares the body for action. In a stressed situation adrenalin is produced quickly and affects a number of organs:The liver converts glycogen to glucose to raise the blood sugar level. The heart beat and breathing rate ___________ . Blood is diverted from the gut to the muscles to give the muscles the extra energy they need. 39