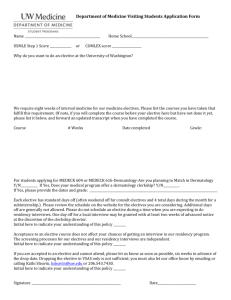
guidelines for electives - Baylor College of Medicine
advertisement

Pediatric Residency Elective Listing 2010-2011 (Updated: 06/16/2010) 1 TABLE OF CONTENTS GUIDELINES FOR ELECTIVES ........................................................................... 3 ADOLESCENT MEDICINE ................................................................................... 5 ALLERGY IMMUNOLOGY ................................................................................... 5 AMBULATORY PEDIATRICS............................................................................... 6 ANESTHESIOLOGY ............................................................................................. 7 CARDIOLOGY ...................................................................................................... 9 DERMATOLOGY ................................................................................................ 12 DEVELOPMENTAL PEDIATRICS ...................................................................... 13 ENDOCRINOLOGY AND METABOLISM ........................................................... 13 GASTROENTEROLOGY, HEPATOLOGY, AND NUTRITION ........................... 14 GASTROENTEROLOGY AND NUTRITION – BOLIVIA ..................................... 15 GENETICS ......................................................................................................... 16 HEMATOLOGY-ONCOLOGY............................................................................. 18 HOSPITALIST .................................................................................................... 19 HOSPITALIST – AWAY (GUATEMALA)............................................................. 21 INFECTIOUS DISEASE...................................................................................... 22 HIV/RETROVIROLOGY AND GLOBAL HEALTH ............................................... 22 NAVAJO ELECTIVE ........................................................................................... 24 NEPHROLOGY ELECTIVE ................................................................................ 26 NEUROLOGY ELECTIVE................................................................................... 27 ORTHOPEDIC ELECTIVE.................................................................................. 30 OTOLARYNGOLOGY ELECTIVE ...................................................................... 31 PATHOLOGY ELECTIVE ................................................................................... 32 PICU Elective ...................................................................................................... 32 PEDIATRIC SLEEP MEDICINE .......................................................................... 33 PHYSICAL MEDICINE AND REHABILITATION ................................................. 34 PRIVATE PEDIATRICIAN OFFICE .................................................................... 35 PSYCHIATRY ..................................................................................................... 35 PULMONARY AMBULATORY ELECTIVE ......................................................... 36 RADIOLOGY ...................................................................................................... 37 RESEARCH ........................................................................................................ 38 RHEUMATOLOGY ............................................................................................. 38 SIMULATION MEDICINE ELECTIVE ................................................................. 39 SPORTS MEDICINE ELECTIVE ........................................................................ 39 PEDIATRIC SURGERY ...................................................................................... 40 SURGICAL SUBSPECIALTIES .......................................................................... 41 UROLOGY .......................................................................................................... 43 GUIDELINES FOR ELECTIVES A resident's total elective program, as well as each individual elective, must be in keeping with the requirements of the American Board of Pediatrics and the Residency Review Committee of the ACGME. In order to meet RRC guidelines regarding total amount of ambulatory time, residents may be limited regarding the number of predominantly inpatient electives that they can do. This issue primarily affects third year residents. Please consult with one of the chief residents if you have questions about your specific situation. In order to meet RRC guidelines regarding subspecialty time, categorical pediatric residents must do seven subspecialty months, four from list A and three from either list A or B. Residents in the combined internal medicine-pediatrics program must do at least four subspecialty months, which must come from list A. These lists are dictated by the RRC and are not negotiable. *Rising PL-2 residents received credit for 1 List A subspecialty by completing TCH 9. Rising PL-3 residents received credit for 3 subspecialities by completing TCH 9, TCH 15, and Blue Bird/Neuro Consult rotations. The remaining subspecialty months are completed by doing electives or additional subspecialty months from the lists below: **BIPAI elective counts as Infectious Disease from List A. Selective (List A) Subspecialties Allergy/Immunology Cardiology* Endocrinology Genetics Gastroenterology Hematology/Oncology* Infectious Diseases** Nephrology Neurology* Pulmonary Rheumatology Other (List B) Subspecialties Pediatric Anesthesiology Child Psychiatry Pediatric Dermatology Pediatric Ophthalmology Pediatric Orthopedics and Sports Medicine Pediatric Otolaryngology Pediatric Radiology Pediatric Surgery Pediatric Surgical Subspecialties Pediatric Physical Medicine and Rehabilitation Away Electives - Coordinating away electives, particularly the Navajo, BIPAI, and Guatemala electives, requires a great deal of effort on the part of the physicians and staff at those institutions. If you sign up for one of these electives, you are expected to go. Switching out of the elective should only be done under extreme circumstances. Pulling out residents that we committed to go reflects poorly on Baylor and may jeopardize the future availability of these electives. During the PL II year, only one elective month may be taken away from the Baylor system. No more than a total of two months (PL-II and PL-III years combined) may be taken outside of the Baylor Affiliated Hospitals. Exceptions will be permitted only for extenuating reasons, and must be approved by Dr. Ward or the Curriculum Committee. Dr. Ward must approve all outside electives (electives in the private practice offices in 3 Houston of pediatricians on the voluntary faculty of TCH and with clinical appointments to the Baylor faculty do not count as outside electives). Any elective that includes 10 or more calendar days away shall be counted as an away elective. Away electives are not permitted during the months of December and June as well as the month of the intern retreat - usually October. Back-up call is required during all electives except those outside Houston. The back-up call schedule will be published in conjunction with the monthly call schedule. SPECIAL ELECTIVES AND AWAY ELECTIVES - Electives may be arranged in areas other than those listed on the following pages. Prior arrangements must be made and approval must be obtained by both the appropriate attending and Dr. Ward. Such electives must be educationally appropriate for a career in pediatrics and must meet all RRC and ABP requirements for credit. Electives may be taken outside the Baylor program. Prior approval must be obtained from Dr. Ward. Please keep in mind that your institutional certificate from Baylor does not legally permit you to practice medicine outside of Texas. Therefore, you must either have a valid state medical license for the state in which the elective is to be done or obtain an appropriate institutional certificate when doing an elective outside of Texas. Failure to do so could place you in great professional jeopardy, since you would be practicing Medicine-pediatrics without a license. Your malpractice insurance through Baylor will cover you while on an official elective, even if outside Texas. The Department of Pediatrics does not send residents on away electives. We permit residents to use time for valid educational activities outside of the Baylor Affiliated Hospitals. Therefore, the resident is responsible for all arrangements for away electives and also is responsible for his or her safety during travel to, from the elective, and at the elective itself. The Department bears no responsibility for any risk incurred as part of this elective. Specifically for residents who choose to go to under-served or under-developed areas, the resident is responsible for assessing any personal risks involved, including, but not limited to infectious diseases. In the case of travel outside the United States, it is the resident’s responsibility to ascertain whether or not special immunizations, chemoprophylaxis for malaria, or other health measures are required and to obtain these. The Pediatric Department has informal contacts with several U.S. Public Health Service Indian Hospitals on the Navajo Reservation in Arizona, the Hospital Gustavo CastanedaPalacios (pediatric community clinic), Zacapa, Guatemala, and Hospital Pedro de Bethancourt in Antigua, Guatemala. All of these are unique educational opportunities. Although individual arrangements will need to be made by the residents taking these electives, we can facilitate the process. For more information about these electives, see description below. If you are interested in doing BIPAI please see HIV/Retrovirology elective information. Vacations, meetings, and holidays will need to be scheduled during away electives as during any other elective. Please keep this in mind as you submit your requests. Residents planning to do special electives should obtain and complete a Special Elective Request Form from Dr. Ward's office. This is to be done after the year's schedule has been published and the month of assignment for the special elective determined. 4 ADOLESCENT MEDICINE Director:Albert C. Hergenroeder, M.D. Contact:Albert C. Hergenroeder, M.D. (832-822-3660) Where to report first day: CCC, Suite 1710 Goals: The resident will understand how to pursue further scholarly activity in a content area specific to adolescent medicine. Objective: By the end of the rotation, the resident will be able to perform/produce one or more of the following activities/products: (1) an in-depth literature review of an adolescent medicine topic with subsequent presentation of the material to the adolescent medicine section faculty; (2) with the guidance of a faculty member, perform a thorough literature review and write an UpToDate chapter in the Adolescent Medicine Section of UpToDate that will be subject to peer review and publication; (3) provide research assistance for an existing research project in the section and be involved in the development of a research manuscript (if the resident were interested in continuing the work initiated during the elective) or a summary paper of 5 pages or more describing the research project and the research "lessons learned" Description: As there is a required PL-II Adolescent Medicine rotation, the goals of this special elective can be suited to the career goals of the resident, to include clinical and research work and can be discussed with Dr. Hergenroeder or any of the Adolescent Medicine faculty. Restrictions on who is eligible for elective: None Restrictions on time of year elective offered: None ALLERGY IMMUNOLOGY Director: William T. Shearer, M.D., Ph.D. Contact: Program Coordinator, Teri McCumber, please contact prior to the start date of the elective (mccumber@bcm.edu; 832-824-1319) Where to report first day: Feigin Center, Suite 330 Goals & Objectives: (1) To enhance the pediatric evaluation of allergic/immune deficient disorders by refinement/expansion of interview and physical examination skills. (2) To provide insight into diagnosis and medical management of allergic/immunodeficient disorders in children. (3) To stimulate interest in Allergy/Immunology and participation in better understanding of the immunopathogenesis of disorders such as asthma, primary immune deficiency, and pediatric HIV infection. 5 (4) To provide an opportunity for interested residents to participate in special projects including clinical research and introduction to immunology laboratory research. Activities: (1) Attend outpatient clinic when working with outpatient team and complete patient sign-out to clinic fellow. (2) Attend inpatient rounds when working with inpatient team. (3) Observe administration of diagnostic tests and maintain patient and procedure log. (4) Attend all AI conferences and Immunodeficiency Rounds. (5) Give a presentation on an allergy/immunology topic during one of the teaching conference sessions. (6) Discuss educational and scholarly activity experiences with one or more of the following: AI Faculty Member, Associate Program Director, Program Director. Description: The elective is offered at Texas Children's Hospital. Residents will participate in the outpatient evaluation of children with hypersensitivity diseases and primary and acquired immune deficiencies. Inpatient activities will be limited to participation in rounds and consultations will occupy not more than 25% of the resident's time. Allergy/Immunology Outpatient Clinics are held Monday through Friday at Texas Children's Hospital. Patients are also seen at Ben Taub General Hospital on Wednesday mornings at the outpatient allergy clinic. These clinics provide residents an opportunity to evaluate a spectrum of diseases including: allergic rhinitis, asthma, urticaria (acute and chronic), drug hypersensitivity, eczema, primary immune deficiencies, pediatric HIV infection, and other secondary immune deficiencies. Teaching conferences include a weekly section conference and CPC, section immunodeficiency rounds, section Hypersensitivity Course conference, section Fellow-Based Clinics conference, and Pediatric Grand Rounds. During the elective, residents are requested to present a topic of their choice in allergy/immunology at one of the teaching conference timeslots. Additional learning opportunities include participation in Allergy/Immunology Board Review sessions, laboratory observations in our Allergy/Immunology Clinical Laboratory (ie. flow cytometry) among other Allergy/Immunology educational experiences. Restrictions on who is eligible for elective: None Restrictions on time of year elective offered: None AMBULATORY PEDIATRICS Director: D’Juanna White-Satcher, M.D Contact: Ida Hernandez, 832-822-3441 Where to report first day: Clinical Care Center 15th floor Suite 1540.00- 9 AM Goals: To better prepare the resident for independent practice in primary care pediatrics. 6 Objectives: To expand the residents exposure to a variety of clinical subspecialties, support services and community resources in order to better prepare themselves for pediatric practice. Description: The elective is fairly flexible in that it can be organized and planned according to the individual's needs and objectives. The resident will devise a schedule for the entire month of activities chosen from a list of 15 different activities. The experiences include some subspecialty clinics such as ophthalmology, urology, sports medicine, and otolaryngology. In addition, the resident can observe how children with specific needs such as the developmentally or mentally retarded child or handicapped child are evaluated and managed in the community. This is accomplished by visiting such agencies as the Avondale House ( community program for children with Autism or PDD) or MHMRA-Infant-Parent Training Program. There is also a session with a billing specialist. If the resident wishes to do something not listed, this activity may be done but must be discussed with Dr. White-Satcher prior to finalizing the schedule. At the completion of the elective the resident will complete a project based on their learning experiences. This elective is an excellent choice for the resident interested in general pediatrics or private practice. The elective is limited to two house officers per month. Restrictions on who is eligible for elective: None Restrictions on time of year elective offered: None ANESTHESIOLOGY Director: Nancy Glass, M.D. and Carlos Rodriquez, M.D. Contact: Nancy Glass, M.D. Email: nlglass@texaschildrenshospital.org Carlos Rodriguez, M.D. email: clrodrig@texaschildrens.org Where to report first day: Main OR Control desk at 7AM, dressed in scrub attire, and request assignment from the Anesthesia GOAT (Anesthesiologist running the schedule) Please see Pediatrics website via the TCH Intranet (under DocumentsElectives) for Patient Log, Procedure Checklist, and further information regarding the elective. Bring the Patient Log and Checklist with you on the first day of the rotation. Goals: (1) Acquire a basic understanding of Pediatric Anesthesiology, including the special considerations imposed by pediatric anatomy and physiology. (2) Understand the rationale for when an artificial airway is necessary, and develop competence in the placement of common airway devices. (3) Develop an understanding of acute postoperative pain management Objectives: Patient care Assist the anesthesiologist with all aspects of anesthetic care, including the preoperative assessment, and in the recovery room. This will include procedures such as IV placement, bag mask ventilation, and endotracheal intubation. Develop an appropriate post operative pain management plan with the Anesthesiology attending 7 Medical Knowledge Discuss pertinent topics with assigned attendings relating to pediatric anesthesia and common co-existing pediatric diseases Attending morning teaching conferences, held Mondays, Tuesdays, Thursdays and Fridays at 6:15am. Attendance at Wednesday conferences is not required. Practice Based Learning and Improvement Attend departmental Quality Improvement meetings Actively seek and accept feedback from attendings regarding all aspects of performance Maintain a case log Professionalism At all times, conduct him/herself in a manner befitting the medical profession. This includes, but is not limited to, appropriate attire, personal grooming, demonstrating courtesy and empathy with patients and family, and collegial behavior towards other medical and nursing staff Interpersonal and Communication skills Communicate with attending staff regarding any questions regarding the anesthesia plan. Be able to perform a basic pre-anesthesia assessment Systems Based Practice Develop an appreciation of how systems are put in place to improve patient outcomes and avoid medical error. Such an example would be the surgical timeout. Description: The pediatric anesthesiology elective for pediatric residents is designed to improve resident's skills at airway management, including effective mask ventilation, placement of laryngeal mask airways and endotracheal tubes. These skills will be practiced on a daily basis and will be accompanied by considerable attention to early recognition of the difficult airway and strategies for avoiding common pitfalls. Additionally, residents will have the opportunity to practice IVs and to learn about the perioperative care of pediatric surgical patients. Pain management options are discussed for each patient. The pediatric resident will NOT be expected to perform as the primary anesthetist, and will not be expected to "learn anesthesiology" in one month! The pediatric resident will never be left alone in the OR with a patient. This elective is designed to be a lowstress, high-yield experience. This elective is designed to provide one-on-one teaching and feedback with faculty anesthesiologists at Texas Children's Hospital for PGY 2 and 3 residents. The responsibilities will be approximately 6:15AM - 4 PM, and the residents are expected to attend the daily didactic conferences held from 6:15 – 7:00 AM (except Wednesdays). Residents are encouraged to participate actively, and are welcome to stay later if they are interested in the care of a particular patient. There are no call or weekend requirements from the Anesthesiology department, but residents are expected to be available for back-up call and Continuity Clinic as scheduled by the Department of Pediatrics. In the event of unexpected overnight call, the resident is to inform the Anesthesiology department via email the evening before 8 (clrodrig@texaschildrens.org). The resident will be assigned to an operating room each day of the week including days with Continuity Clinic, and will be expected in the OR either in the afternoon after, or morning before a Clinic obligation. On the first day of their rotation, residents should present to the Main OR Control desk, in West Tower 3rd floor, at 7AM, dressed in scrub attire, and request their assignment from the Anesthesia GOAT. The next day’s assignments may be checked on the Master OR schedule after approximately 3pm at the Main OR desk. Residents are expected to maintain a patient encounter list documenting each procedure and/or anesthesia they perform. This list should include patient identifier (name or MR#), age, diagnosis, procedure performed, and any complications that occurred. In addition, residents should complete a checklist of desired discussions, procedures and types of patient encounters. A copy of both the case logs and checklist of discussions and procedures must be turned in at the end of the rotation. We recommend this elective for residents planning careers in Emergency Medicine and Pediatric Critical Care Medicine, as well as those residents who will be practicing Primary Care in remote or non-urban areas, without ready access to subspecialists. The number of safe, controlled intubations that we can offer during a one-month elective should considerably increase the skills and confidence level of the graduating resident. Restrictions on who is eligible for elective: One resident per month Restrictions on time of year elective offered: None CARDIOLOGY Director: Regina L. Lantin, MD Contact: Cathy Umeh 832-826-5639 or Veronica Perez 832-826-5637 * Please let us know of your intention to participate in our elective, preferably at least 6 weeks before the designated start date. Where to report the first day: TCH West Tower – 19th Floor Objectives: (1) To be familiar with the different aspects of the evaluation and treatment of the child with cardiac disease (2) To be proficient in cardiac history taking and performing the cardiac physical exam (3) (4) (5) (6) (7) To be competent in distinguishing innocent vs pathologic heart murmurs. To know the anatomy and physiology of common congenital heart defects (CHD) To enumerate the basic cardiac operations performed in the child with CHD. To be able to interpret a pediatric ECG To know the unique aspects of anticipatory guidance for the child with CHD. Description: 9 This elective is primarily based in the cardiology outpatient clinic. The clinic meets Monday – Friday except on official Holidays. The clinic begins at 8:30 AM and concludes at 5:00 PM. During the 4 week elective, the medical student, pediatric resident, or visiting fellow will interact one-on-one with all of the Staff Cardiology Attendings in the General Cardiology Clinic. The participants will also participate in the Heart Transplant Clinic, Cardiomyopathy/Heart Failure Clinic, Cardio-Genetics Clinic and Electrophysiology Clinic. The participants will pre-evaluate the patients (history, physical exam, assessment, and plan) and then present to the Cardiology Attending in the Clinic. CONFERENCES / LECTURES: Participants will also be given the option to attend the conferences and didactic lecture series at the TCH Heart Center. These are held at the Taussig Auditorium @ 7:15 AM or 12 noon on various days of the week. A schedule of these conferences and lectures will be made available to the participants. ELECTIVE OPTIONS: During the latter part of the elective, the participant may request to spend time reading ECGs with the Cardiology Electrophysiology Service (EPS). The EPS reads all ECGs performed in the hospital. The participant will read the ECG with the EPS Attending and the Cardiology Fellow and have rapid feedback about his/her interpretation. The participant may also elect to spend a day as an observer in the ECHO or CATH lab. Please let the director know ahead of time if you wish to add these options to your elective. EVALUATION: A pre- and post-test evaluation is part of the curriculum and will enable us to give an objective assessment of the attainment of the learning objectives as outlined. The participant is instructed to keep a daily log of his/her activities: ie – the lectures or conferences attended, the Cardiology attending the participant worked with, and the number of patients, with their respective diagnoses that he/she has participated in the care of. This information, along with a pre and post test clinical evaluation, will be collected at the end of the elective and be part of the basis for evaluation. At the end of the elective, the participant will have been introduced to every facet of outpatient care of the child with heart disease while at the same time obtaining a solid foundation in the basic evaluation of the child and young adult with heart disease. Restrictions on who is eligible for elective: None Restrictions on time of year elective offered: None General restriction: Due to the potential for having too many participants and the risk of diluting the learning experience, the director may have to limit the choice of months on a case by case basis. CHILD MALTREATMENT Director: Michelle Lyn Contact: Dr. Michelle Lyn, M.D., MaLyn@texaschildrens.org 10 Where to report first day: Please email Dr. Michele Lyn one week prior to rotation to set up first meeting time. Goals: 1) Understand the various categories of Child Maltreatment 2) Learn essential skills in the evaluation and management of suspected abuse. Objectives 1. Review normal and abnormal genital findings in the context of the Sexual Assault Examination 2. Review range of physical and radiographic findings in context of the Physical Assault Examination 3. Review definition and findings in cases of medical care neglect 4. Review the mediocolegal aspects of Child Abuse reporting (eg. documentation, testimony) 5. Participate in Child Abuse Team weekly meeting 6. Observe Forensic interview 7. Participate in the evaluation of child abuse cases 8. Review Domestic Violence impact on Child Abuse 9. Participate in pre and posttest knowledge of child abuse Pediatric Residents Elective in Child Abuse Program Residents will be evaluated on the six core competencies during this elective. A biannual report of the evaluation process and it’s outcome will be forwarded to the Residency Director and the Chairman. Competency in patient care will be assessed through their participation in patient evaluations. This will be accomplished with both direct observations of their interview and physical examination as well as through their presentations. Competency in medical knowledge will be achieved by their review of the major categories of child abuse, pre and posttest analysis, and participation in the Child Abuse Team weekly meetings Competency in practice-based learning will be assed through the case analysis in specific areas of child abuse Interpersonal skills will be assessed through direct observation with families and staff. Competency in Professionalism will be assessed by direct observation with patient, families, staff and participation in the weekly meeting. Competency in System based practice will be achieved by their teamwork within the Child Protection Program Schedule for residents for a one day rotation: Schedule for 1-day rotation 8am: Meet with attending to review goals and objectives, review SAE video take pretest and posttest, Review significance of history and physical findings of abuse 9am:Meet with attending and CPT nurse case manager to review in house cases, possible consults. If no consults review physical assault and medical care neglect cases and management 11 12noon: lunch 1pm-5pm: Tour the Children’s Assessment Center Observe evaluation of SAE, Review genital anatomy, and discuss the significance and evaluation of an acute sexual assault. Observe a forensic interview Alternative schedule: If court case on abuse is ongoing may observe a trial. If no court case, may review video on a particular trial. Restrictions on who is eligible for elective: None Restrictions on time of year elective offered: None DERMATOLOGY Director: Denise Metry M.D., Teresa Wright M.D. Contact: Laura Heras, Administrative Assistant, Dermatology Service; CC620.16, office# 832-822-3718 Where to report first day: Ms. Laura Heras (see above) at 8 am, and then Dermatology Clinic (8th floor, CCC). Goals: (1) To expose pediatric residents to a wide range of dermatologic disease. (2) To improve diagnostic skill in trainees who will become general pediatricians. Objectives: (1) To acquaint residents to a differential diagnosis for commonly encountered pediatric skin disorders. (2) To review diagnostic and therapeutic procedures useful in evaluating dermatologic disease including eczema, acne, and other common pediatric conditions. (3) To improve resident understanding of presentation, pathophysiology, and treatment of common and rare dermatological disorders in more depth than is available through core clerkships. Description: During the rotation on Dermatology, a resident can expect exposure to a wide range of cutaneous disease. Pediatric dermatology clinics currently operate at Texas Children's Hospital. Pediatric in-house consultations are seen in variable numbers. Each resident is encouraged to initiate the evaluation of patients seen in the clinics, as well as develop a treatment plan with the help of our staff. Background reading is expected during the rotation. Restrictions on who is eligible for elective: This elective is restricted to 2 residents. Restrictions on time of year elective offered: None; residents who rotate during the month of August are encouraged to attend Camp Dermadillo the 2nd week of August. 12 DEVELOPMENTAL PEDIATRICS Director: Lane Strathearn MD PhD Contact: Ms. Rosie Knight (Ph: 832 822 3425; email: rosiek@bcm.edu) Where to report first day: 8:30 a.m. in suite 1530 of the TCH CCC (The Meyer Center for Developmental Pediatrics/Developmental Pediatrics academic office) Goals/Objectives: Refer to the Pediatrics website via the TCH Intranet (under DocumentsElectives) for Goals and Objectives. Once assigned to this elective, the resident must complete the questionnaire found at the Pediatrics website via TCH Intranet (under DocumentsElectives). Return ASAP to Dr. Strathearn. Description: No call/no weekends on schedule. Typical day begins at 8 a.m. and ends at 5 p.m. and includes a lunch-time conference on Tuesdays and Wednesdays. The rotation is one month long and is designed around the specific goals/objectives mentioned in the questionnaire completed by the resident wanting to do the elective with these goals/objectives aimed at expanding the residents general developmental behavioral pediatrics experience to a more specific focus in this elective. For example, a resident doing the elective may want to concentrate on patients with a particular disorder such as Down Syndrome Autism, or ADHD; or to focus on children with particular conditions such as multiple handicaps, sleep problems, toileting problems, behavior problems, prematurity, mental retardation or learning disabilities, instead of the general experience seen during the required developmental pediatrics rotation. Alternately, a resident may want to choose several specific problems mentioned above instead of focusing on one particular condition. An opportunity to participate in clinical research is also available, including functional MRI and automated eye tracking studies involving children with autism or parents. Restrictions on who is eligible for elective: The clinical elective participant needs to have successfully completed the required for Pediatric Residents Developmental Behavioral Pediatrics rotation either at Baylor College of Medicine or equivalent rotation at another institution. No restrictions apply for the research elective. Restrictions on time of year elective offered: None ENDOCRINOLOGY AND METABOLISM Director: Morey Haymond, M.D. Contact: Sandra Vale. 832-822-3776 or vale@bcm.edu Where to report first day: CCC1020.05, 8:30am, ask for Sandra. Goals: Will obtain broad clinical experience including managing patients with growth disorders, 13 abnormalities of pubertal development, Type 1 and Type 2 diabetes, thyroid disorders, adrenal insufficiency, ambiguous genitalia, pituitary disorders and disorders of bone metabolism. Obtain an overview of the impact of endocrine disease on growth and development in children. Develop competency in pediatric endocrinology. Objectives: (1) Participate in consults and follow-up appointments under the supervision of the pediatric endocrine attending faculty. (2) Observe the pediatric endocrine staff during teaching for diabetes care and endocrine testing to provide depth of understanding of these disorders. (3) Attend Case presentation/Journal review meetings on a weekly basis to further increase knowledge of endocrine subjects and research methods. (4) Present a PowerPoint case presentation of one of the interesting patients seen during the rotation at the weekly case conference. Description: The resident will work with the faculty attending physicians and endocrine fellows for the month of the elective. Residents will participate in approximately 6 half day clinic sessions per week. They may observe our diabetes education sessions, including newly diagnosed Type 1 diabetes, Type 2 diabetes and insulin pump education. The resident will attend the section’s conferences held on Thursday afternoons, which on a rotating basis may include journal club, research club and case presentations. The resident will be responsible for one 20 minute case presentation at the end of their rotation. The hours will be from 8 to 5. Restrictions on who is eligible for elective: None Restrictions on time of year elective offered: None GASTROENTEROLOGY, HEPATOLOGY, AND NUTRITION Director: Mark Gilger, M.D. Contact: Contact Dr. Gilger as needed. CCC, 11th Fl, MC CC 1100.36; 832-822-3131 Where to report first day: Report to the GI offices, CCC Suite 10.10 at 8 a.m. They should see Dr. Gilger or his designee. Goals: (1) To offer a broadened exposure to Gastroenterology/Hepatology/Nutrition for residents with a special interest in the field or for those with plans to pursue a career in this specialty. (2) To provide the resident with inpatient, outpatient, and procedural experience as well as GI-focused academic opportunities. Objectives: (1) To learn the evaluation and management of gastrointestinal diseases such as acute and chronic diarrhea, inflammatory bowel disease, peptic ulcer disease, and acute and chronic liver disease. (2) To gain experience in the diagnosis and treatment of nutritional disorders with 14 emphasis on the use of total parenteral nutrition, chemically defined "tube" diets, and infant formulas (3) To observe and participate in upper and lower gastrointestinal endoscopy, liver biopsies, gastrointestinal manometry and esophageal pH monitoring. (4) To present and participate in the daily teaching conferences. Description: “Did you know that there are more neurons in the intestine that in the brain?” This elective gives the resident an active and exciting entry into the science and practice of pediatric gastroenterology, hepatology, and nutrition. During this one-month elective residents will have the opportunity to participate in the daily activities of clinical gastroenterology, including inpatient and outpatient evaluations, and daily teaching conferences. The resident will be able to participate in the full array of gastroenterologic procedures, including upper and lower endoscopy, ERCP, liver biopsy and gastrointestinal manometry. Residents are asked to take daytime call with the "fellow" during the week, but weekend call is optional. Teaching conferences include Monday Pathology Conference or "GI" Research Conference, Tuesday Clinical "Show and Tell" Conference, Wednesday "Liver" Case Conference, Friday "Fellows" rounds and the monthly Journal Club. Restrictions on who is eligible for elective: Two residents per block. Restrictions on time of year elective offered: None GASTROENTEROLOGY AND NUTRITION – BOLIVIA This elective if available one month out of the year in May-August (we will be notified by Dr Ferry when he knows which month) Director: George Ferry, M.D. Contact: George Ferry, M.D. 832-822-3602, cell 713-208-9071 Where to Report First Day: GI Clinic, 11th floor of the Clinical Care Center Goals/Objectives: (1) To learn about the diagnosis and treatment of common GI/Liver/Nutrition problems while attending the Texas Children's Hospital GI outpatient clinic. (2) The objectives for the 10 days in Bolivia include: learning appropriate clinical assessment and physical findings in a variety of nutritional disturbances common to third world countries, learning about the natural history and treatment of a variety of parasitic infections (both those seen in the US and in underdeveloped countries, such as Chagas disease), learning about public health issues related to safe water supply, and management of maternal and neonatal health issues through home visits. Description: During the Bolivia part of this elective, residents will be seeing patients in an outpatient clinic from 8-12 and 2-5:00 each day. Dr. Ferry will be supervising the patient care and will review the findings and appropriate treatment for each patient. There will be no night 15 call. During the TCH part of the rotation, the residents will be working in the outpatient clinic from 8-12 and 1-5 each day and they will be supervised by the GI faculty. All of the Pediatric GI faculty will be involved during the rest of the month in the GI/Nutrition Clinic at Texas Children’s Hospital. There will be no night call. Any restrictions as to who can take elective: None Any restrictions as to when elective is available: This varies from year to year. Financial Obligations: Airfare covered and probably room and board if necessary (about $40/day or a bit less if sharing a room). GENETICS Director: Reid Sutton,MD Contact: Reid Sutton, MD, CC-15670, Tel 2-4296, pager 6099, vsutton@bcm.edu Where to report first day: E-mail/call/page Dr. Sutton about 2 weeks prior to the elective in order to individualize schedule. Offices on the 15th floor of the CCC, suite 1560. Goals: (1) Gather essential and accurate information about the patient to determine whether a medical condition has a genetic etiology. (2) Identify conditions requiring urgent referral and recognize and respond to urgent and/or severe conditions related to medical genetics and inborn errors of metabolism (including abnormal expanded newborn screening results). (3) Recognize presenting symptoms, diagnose, describe the pathophysiology and manage common presentations of the following genetic conditions. (4) Differentiate disorders in patients associated with genetic predisposition or genetic disease from acquired disorders or normal variation. (5) Undifferentiated signs and symptoms. Evaluate, treat and/or refer patients with the presenting signs and symptoms that suggest a genetic disease process (6)Participate in provision of genetic counseling to a patient or the patient’s family, including: Diagnosis, prognosis, recurrence risk and strategy for management and anticipatory guidance. Objectives: (1) Obtain and document a medical history that includes a detailed prenatal history, history of present illness, family history (four-generation pedigree) (2) Perform and document a thorough physical exam that includes measurements to determine normal vs. abnormal anthropometrics (3) Perform and document a thorough physical examination on an individual suspected of having a specific genetic disorder, identifying major and minor congenital anomalies that may be indicative of a genetic disorder (4) Develop a management plan for commonly encountered genetic disorders, identifying principles of long-term management, including use of disorder-specific practice guidelines from textbooks, professional societies (5) Identify resources in the community for diagnosis, genetic counseling, therapy and psychosocial support of children with genetic disorders and congenital anomalies 16 Further goals, objectives, and detailed elective and schedule information are available online through the Pediatrics website via TCH Intranet (under DocumentsElectives). Description: The Genetic Elective for Pediatric Residents is a 90% outpatient clinical experience. It is designed to expose residents to both common genetic diagnoses, seen in the pediatric genetic clinics as well as exposure to subspecialty clinics that are typically focused on treatment of more rare disorders. There is also experience in the adult outpatient clinic at the Baylor Clinic; this clinic frequently deals with issues of transition of care, which are critical to the current practice of pediatrics. The resident should e-mail the elective director, Dr. Reid Sutton vsutton@bcm.edu at least 2-3 weeks prior to starting the elective to provide Dr. Sutton with any vacation days or scheduling conflicts. In addition, if pediatric residents have a particular interest, the rotation or patients selected for the pediatric resident may be tailored to focus the clinical experience on a particular area of interest. Dr. Sutton will schedule a meeting with the resident on or before the first day of the rotation to briefly review the rotation. The reason for this pre-contact is to provide the best learning experience possible. New patients in our clinics are typically scheduled 3-4 weeks in advance and we will schedule the patient specifically for a pediatric resident/attending visit. These visits are allotted more time than a new patient visit seen only by an attending to ensure that the pediatric resident receives the best-possible clinic experience with time to discuss cases with attendings and to be able to have each patient encounter serve as an intensive learning experience. Residents will typically see 2-4 new patients per clinic. The resident should review the patient’s medical records prior to the clinic visit. If this is not done in the days prior to the clinic appointment, the resident should arrive in the clinic area 15-20 minutes prior to the scheduled appointment to review the electronic and paper medical records, prior to the patient evaluation. New patients are scheduled for 90 minute visits, in most clinics. It is expected that the resident will spend 30 - 45 minutes obtaining the history and physical examination, independently. Upon completion of the H&P, the resident should notify the family that he/she will discuss their case with the attending and return in 20-30 minutes. The resident should then take 1015 minutes to synthesize the information that has been obtained and utilize online resources and textbooks available in the clinic area to formulate a differential diagnosis and develop a plan for diagnostic evaluation and/or treatment. The resident should then locate the attending physician for the patient and present a precise, yet thorough summation of the H&P, including thoughts about possible diagnosis and a strategy for diagnostic evaluations and/or treatments. The resident and the attending will then return to the patient’s room together to discuss the recommendations with the patient/family. The resident is responsible for documentation of the encounter in the medical record. The resident may use papers found with the clinic chart to make notes, but is not required to hand-write a clinic note. The resident will dictate or type a clinic note in the electronic medical record. This may be done at the completion of the patient encounter; however, if other patients are ready to be seen, the patient should not be made to wait while the resident documents the visit. The resident should edit the documentation once it is complete (if dictated, it should either arrive on the desktop or should be on the attending’s desktop) and route to the attending (without signing) for him/her to edit and sign. 17 TCH Clinics 8:00 9:00 10:00 11:00 Cancer/NF Monday Tuesday TCH Pediatric Genetics Didactic Lecture Clinic Biochemical Genetics Case Review 12:00 1:00 Clinical Genetics Seminar 2:00 Inpatient 3:00 Consults 4:00 BTGH Pediatric Clinic (1st & 3rd) Baylor Clinic Wedensday TCH CV TCH Genetics Pediatric Clinic Cancer Genetics Clinic Inpatient Consults (2nd, 4th & 5th) Ben Taub Clinics Thursday TCH Pediatric Genetics Clinic TCH Metabolic Clinic Post-Clinic Conference Conferences Friday Baylor Clinic Adult Genetics Clinic Genetics Grand Rounds TCH TCH Ben NF Skeletal Taub Clinic Dysplasia Adult (1st) Clinic Genetics (2nd) Clinic (3rd) Restrictions on who is eligible for elective: None Restrictions on time of year elective offered: None HEMATOLOGY-ONCOLOGY Director: Philip Steuber, MD Contact: Dr. Steuber’s assistant Anita Arriaga at 832-822-4207 and arrange a time to meet with Dr. Steuber on the first day of the rotation Where to report first day: See Contact Goals and Objectives: (1) Evaluation and therapy of hematological problems encountered in the pediatric patient (2) Increase awareness of the spectrum and natural history of childhood malignancies (3) Experience dealing with families and patients with stressful chronic and possibly fatal disorders (4) Increase knowledge of clinical experimental research design and how to follow therapeutic protocols Description: Residents choosing this elective will spend the majority of their time on the outpatient service or the consultation service or some combination thereof. Rotations are set to meet the residents’ goals in taking the elective. Residents will have exposure to all types of hematological diagnoses, as well as to the management of patients being followed on a variety of therapeutic protocols for both hematologic and oncologic disorders. 18 If he/she wishes, the resident can see new consultations and learn basic evaluation and management skills. The latter includes examination and interpretation of marrow specimens, as well as peripheral blood smears. Attendance and participation in weekly chart rounds and educational conferences is expected. No night call. Residents may be requested to present a review of a topic at the end of the elective. Specific laboratory research projects can be prearranged with staff but generally require greater than one-month commitment. Restrictions on who is eligible for elective: None Restrictions on time of year elective offered: None HOSPITALIST Director: Dr. Singhal and Dr. Nag Contact: Felecia Smith (832-824-5399) Where to report first day: 2nd floor Abercrombie (take red elevators to Abercrombie second floor) – Peds Emergency Medicine offices, ask for Felicia, 8am Goals and Objectives: 1) Patient Care - Admit, manage and discharge patients admitted to the hospitalist group (as assigned by the attending). - Systematically evaluate and generate a problem definition, differential diagnosis and management plan for each patient, including reasonable and effective use of laboratory and radio logic services, as well as consultants. - Develop comprehensive, pertinent and expeditious discharge plan for each patient, ensuring continuation of care as outpatient. - Be the leader of a multidisciplinary care team for your patients (if pertinent), involving consultants, nurses, rehabilitation team, social workers, and other ancillary services. - Function as consultant for other pediatric specialties in the inpatient environment. - Serve as advocate for the patient and ensure high quality, general pediatric care. 2) Medical knowledge - Understand and become knowledgeable on the most common inpatient pediatric problems, including but not limited to: asthma, bronchiolitis, croup, pneumonia, gastroenteritis and dehydration, urinary tract infection, fever without a source in infants under 3 months, seizures, ALTE, cellulitis and other soft tissue infections, adenitis and retropharyngeal infections, and child abuse. Use practice-based guidelines in diagnostic and management procedures to systematically approach these conditions. - Attend and participate in FIS patient run-through meetings 3) Practice-based learning and improvement - Using information technology to locate and utilize available evidence to maximize diagnostic and therapeutic effectiveness. - Use the "educational prescription" as a guide to formulate clinical questions pertinent to your patient and investigate available evidence. - Be aware of potential quality improvement issues regarding hospital-based therapy pertinent to our specific clinical practice and patient population. Consider ideas/methods 19 to improve these areas. 4) Interpersonal and communication skills - Develop effective communication skills by discussing plan of care with the patient and family in a timely fashion, demonstrating compassion and empathy. Promote respectful interdisciplinary interactions among colleagues, ancillary and non-medical services. - Understand the importance of maintaining clear, opportune and reciprocal hospital interfaces (communication with outpatient settings). 5) Professionalism - Take ownership of patients and perform clinical care with respect, compassion and integrity. - Know your limitations. - Serve as educator and advocate for patients and their families, exercising cultural sensitivity and social awareness. 6) Systems-based practice - Gain experience in the management and coordination of care of chronically ill children with complex medical needs. - Be aware of and properly utilize available community, state and/or federal resources and other material (systems-based practice) useful for patient care, counseling and education. - Learn the basics of coding and billing for inpatient practice, using the International Statistical Classification of Diseases and Related Health Problems (ICD-9 coding). - Understand healthcare economics and hospital organization by participating in administrative meetings and/or committees, which impact hospital care. Description: The main focus of this elective is to further train pediatric residents in the realm of hospital medicine and its unique responsibilities. A study conducted among practicing hospitalists suggests that these graduates felt less prepared in areas such as medical consultation, communication skills, systems issues and continuum of care competency. There is also little if any training in administrative responsibilities and quality improvement processes during standard residency training. Therefore, this elective will emphasize the development of three main areas in which a future pediatric hospitalist should be skillful: clinical, academic and administrative. The rotating resident will gain expertise in these skills through autonomous management of patients and close interaction with their families, primary care physicians, and hospital staff. One resident is allowed per month and will be determined on a first-come, first-serve basis. The resident will also manage and attend these patients during the day Monday through Friday, when possible expediting discharges of patients before the weekend, as to improve continuity of care and not burden the team covering for the weekend. The patient assignment and load will be determined at the discretion of the FIS attendings. Most of the resident/attending contact and teaching will be one-to-one. Ongoing verbal evaluations will take place throughout the rotation. At the end, a written evaluation with valuable feedback will be provided by FIS attendings. All ACGME required general core competencies (patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism and systemsbased practice) would be stressed and evaluated during this rotation. Completion of preand post-rotation surveys is encouraged for continuous evaluation and improvement of 20 the elective. Schedule: Monday - Rounds 8:30-9:30; Noon conference 1200-1300 Tuesday - Rounds 8:30-9:30; 1000-1100 Feigin Rounds; 1200-1300 Noon conference/Section Meetings Wednesday - Rounds 8:30-9:30; Noon conference 1200-1300 Thursday - Rounds 8:30-9:30; Noon conference 1200-1300 Friday - Grand Rounds 8:30-9:30; Rounds 9:30-10 am - Noon conference 1200-1300 Restrictions on who is eligible for elective: One resident per month Restrictions on time of year elective offered: None HOSPITALIST – AWAY (GUATEMALA) Director: Ricardo Quinonez, M.D. quinonez@bcm.tmc.edu Contact: Monica Flokuet, 832-824-5447 Where to report first day: Resident should contact Dr. Quinonez at least one month in advance. Goals and Objectives: (1) Participate in the evaluation and management of patients with conditions that commonly present to Hospital Pedro de Bethancourt in Antigua. (2) Expand on previously acquired medical knowledge to include tropical diseases, common pediatric conditions encountered in third world countries and an appreciation of the barriers encountered by pediatricians who work in underdeveloped countries. (3) Demonstrate and expand on interpersonal and communication skills in Spanish. (4) Apply and encourage evidence based guidelines, where applicable, to some of the same conditions routinely seen in Guatemala that are seen in the US. (5) Demonstrate the professionalism and ethic principles which guide medical practice in the US and how these can be applied in the Guatemalan Health Care System. (6) Realize and understand the limits encountered in the Guatemalan health care system. Description: The Guatemala Inpatient Elective takes place in Hospital Nacional Pedro de Bethancourt in Antigua, Guatemala. This hospital is a general hospital that serves the colonial city of Antigua and its surrounding villages. The elective resident/student will work in the pediatric department along with their medical students, residents and attending physicians. They will get to experience the work of an inpatient department and emergency center of a third world country with its limited resources and financial limitations. They will be exposed to patients with a variety of illness with infectious illnesses being the most common. Tropical diseases such as malaria, dengue, and yellow fever are endemic to the region and this will enhance your overall clinical experience. Antigua is the largest colonial city in the Americas. It is Guatemala’s #1 tourist attraction and there are a large variety of services for international travelers. All interested participants are encouraged to visit their physician or Baylor’s International Health department for recommended immunizations and preventive medications. 21 Restrictions on who is eligible for elective: Spanish strongly encouraged. Limit 2-3 residents per month, please contact Dr. Quinonez at least 1 month in advance of elective. Restrictions on time of year elective offered: None Financial Responsibilities: Resident is responsible for all costs including flight, housing, meals. Arrangements are the responsibility of the resident, as well. INFECTIOUS DISEASE Director: Deb Palazzi, MD Contact: Residents should contact the ID fellow at 832-824-7243 #6224 one to three days prior to the start of the rotation for instructions on where and when to meet. Where to report first day: (Mondays only; otherwise page ID fellow) 8am, Infectious Diseases Office Taber Conference Room, Suite 1150, 11th Floor, Feigin Center Goals and Objectives: (1) To refine skills in diagnosis and management, both for common and for unusual infections. (2) To enhance competence in selection of antimicrobials, including developing expertise in route of administration, drug metabolism, adverse effects, desirable serum levels, and duration for optimal outcome. (3) To learn the pathogenesis of infections so that the expected course and complications of a process can be anticipated. Description: The elective is offered at TCH exclusively. PL-II and PL-III residents will perform inpatient consultations, including a detailed summary of pertinent microbiologic, virologic and serologic studies, review textbook and literature material relevant to evaluated patients, and present this material to the attending faculty for detailed discussion. Patients then will be followed daily until the diagnosis(es) is established, management is advised, and improvement is documented. Inpatient rounds with an ID fellow and faculty member occupy approximately 8 hours per weekday. A full library of ID journal articles and textbooks are available to residents taking the elective. Also, weekly conferences that include journal club and citywide ID case presentations (pediatrics and medicine), and a monthly ID fellow, resident and medical student clinical conference and monthly research conference are parts of the elective. Finally, there are opportunities for residents to learn special laboratory procedures. Residents will take night call from home approximately every third night and one weekend per month. Restrictions on who is eligible for elective: None Restrictions on time of year elective offered: None HIV/RETROVIROLOGY AND GLOBAL HEALTH Director: Heidi Schwarzwald, M.D. Contact: International: Meg Ferris, PhD mferris@bcm.edu, 832-822-1366 22 Domestic: Heidi Schwarzwald, MD MPH, 832-822-6730, pgr 5320, heidis@bcm.edu Where to report first day: Domestic: CCC 1210; 8:15 am on the first day. International: Appropriate BIPAI clinic (more info sent once country determination is made) Goals and Objectives: (1) To become familiar with the routine outpatient diagnosis and management of HIVexposed and HIV- infected infants and children. (2) To understand the indications and rationale for current antiretroviral and prophylactic medications in the HIV-infected child. (3) To gain appreciation for the multidisciplinary team approach to pediatric HIV infection, and the essential role of patient, family, and health care professional education in disease management. (4) To become familiar with the medical, behavioral, and developmental issues unique to children adopted internationally. (5) To understand cultural differences in the approach to and practice of medical treatment in a resource restricted setting. Description: DOMESTIC ELECTIVE: This is a predominantly outpatient elective. The resident will work as one member of a multidisciplinary team in the outpatient management of HIV-exposed and HIV-infected infants and children. The resident will become familiar with specialized diagnostic testing for HIV in infancy, clinical manifestations of HIV, specialized assays of immunologic function and virus load, and current approaches to antiretroviral therapy and prevention of complicating infections. She/he will have an opportunity to participate in the management of HIV-infected children enrolled in a variety of HIV treatment trials and other clinical research studies. Children with complications of HIV will be evaluated and treated in both the outpatient and inpatient settings. Residents will attend an adolescent HIV clinic at Thomas Street, an HIV dental clinic associated with Bering-Omega, and one afternoon in a clinic for HIV + pregnant women to deepen their understanding of how transmission of HIV to the newborn is prevented. In addition, residents will have an opportunity to participate in the care and treatment of children adopted internationally. They will assist with the review of medical records provided prior to the completion of an adoption, see children who have recently immigrated to the United States as well as the management of some of the long-term issues faced by families and children adopted internationally. In the initial post-adoption care, many of the issues faced by internationally adopted children are infectious: parasites, tuberculosis exposure, etc. The longer term issues often center around behavioral and developmental issues. INTERNATIONAL ELECTIVE: The international elective will take place in one of the following sites: Botswana, Lesotho, Malawi, or Swaziland. Due to heavy demand for training of both international and American health professionals, the international HIV elective will be available on a restricted basis. The resident will work as one member of a multidisciplinary team in the 23 outpatient management of HIV-exposed and HIV-infected infants and children. The resident will become familiar with specialized diagnostic testing for HIV in infancy, clinical manifestations of HIV, specialized assays of immunologic function and virus load, and current approaches to antiretroviral therapy and prevention of complicating infections. Depending on the country assigned and the country director’s discretion, some inpatient responsibilities may be included. The resident will further become familiar with providing medical care in a resource limited setting. They will become familiar with treatment of pediatric illnesses not often seen in the United States, such as tuberculosis and malaria. They will become familiar with the causes and consequences of pediatric malnutrition and the appropriate WHO treatment guidelines. Resident’s will participate in both inpatient and outpatient care, as determined by their country directors. BIPAI generously provides funds to pay for the round-trip flight to Africa, however, this is only available to the resident once. For example, if a resident would like to participate in the elective as a second year and again as a third year, they would be responsible for paying for the flight the second time. Funding can change from year-to-year, so please inquire if you have questions regarding the above. Night/Weekend Call: None Restrictions on who is eligible for elective: Domestic – None International – Must have completed internship year and prefer that pediatric ICU rotation completed Restrictions on time of year elective offered: None Financial obligations: Residents are financially responsible for their own ground transport, meals, and incidentals. Shared housing is available in-country. For the Malawi placement, some small extra expenses apply (The charges for stay at the Malawi guest house are $12/week/person. Each resident of the apartment will be required to provide a maintenance $100 deposit, refundable upon departure, except in instances the resident is deemed to have damaged apartment furnishing(s) or appliance(s). The Medical Council of Malawi requires that all foreign medical students/residents visiting Malawi on any medical mission or as part of their training in the form of research or clinical observation pay a student index fee. This fee is $100, payable in US Dollars.) NAVAJO ELECTIVE Director: Martin Lorin, M.D. Contact: Dr. Lorin several months prior to the start of the elective Where to report first day: See contacts Goals and Objectives: (1) Enhance the resident's understanding of the interaction of culture and health (2) Enhance the resident's understanding of the effects of poverty on health and illness (3) Enhance the resident's skills in primary care (4) Enhance the resident's ability to care for patients without ready access to 24 subspecialty consultation Description: The Navajo Reservation is the largest Indian Reservation in the United States, larger than the state of West Virginia. Located in the Four-Corners region of the Southwest, the area is extraordinarily scenic, but the area is also beset by poverty and health care problems. The reservation shares some of the characteristics of a third world country, including a high unemployment rate, numerous unpaved and often impassible roads, and a lack of health care resources. Pediatric Residents generally will be assigned to the Shiprock Hospital of the Navajo Indian Reservation at Four Corners, NM located in the Northeast corner of the reservation. Housing is provided by Shiprock Hospital and may require residents to share lodging in the event that multiple residents are participating in the same month. Several full time pediatricians provide supervision. Night and weekend duty is not required. The resident will have a unique opportunity to learn about a Native American culture and its interaction with health and health care. Restrictions on who is eligible for elective: None Restrictions on time of year elective offered: Anytime but more ice/snow in December/January and less patients in July/August Financial obligations (for away electives): The Azzam Foundation provides a $500 scholarship to offset costs of travel. Contact Dr. Marty Lorin with questions regarding the scholarship. NEONATOLOGY ELECTIVE Director: Tiffany McKee-Garrett, M.D Contact: Dr. McKee-Garrett - by e-mail tiffanym@bcm.edu - 2-3 days prior to start date to determine meeting location Where to report first day: See Contact Goals and Objectives: (1) To learn and practice circumcision skills. To review risks, benefits, and contraindications to performing circumcisions. (2) To round as an integral part of the neonatology hospitalist team at St. Luke’s and Methodist Hospitals. (3) To supervise interns and students in normal newborn care at St. Luke’s and Methodist . To refine teaching skills in well newborn care. (4) To attend deliveries and complete newborn resuscitation at Methodist. Description: This elective is offered only to PL-III residents. Residents will round in the normal newborn nurseries at Methodist and St. Luke’s Hospitals. Residents will have the opportunity to learn and practice procedures, including circumcisions, at both institutions. 25 Residents will be expected to provide teaching to students at St Luke’s and Methodist, as well as interns rotating through the normal newborn nursery at St. Luke's regarding normal newborn exam and care. Residents will attend deliveries and complete resuscitations at Methodist. This rotation is a great rotation for a graduating resident needing to "brush-up" on newborn exams and circumcisions. Building a new practice starts with new patients -often newborns! There will be no call during this rotation. The resident will be expected to attend TCH Neonatology noon conferences and the Department of Pediatrics Grand Rounds. This rotation will be limited to one resident per month. Restrictions on who is eligible for elective: PL-III Restrictions on time of year elective offered: None NEPHROLOGY ELECTIVE Director: Eileen Brewer, M.D. Contact: Karen Shelton, kpshelto@texaschildrens.org; phone 832-824-3800 Where to report first day: Renal Office, Suite 260 Feigin Center Goals and Objectives: (1) Development of skills in the diagnosis and evaluation of congenital and acquired renal diseases (2) Evaluation and management of hypertension in childhood (3) Management of fluid and electrolyte disorders. (4) Acquisition of knowledge about the normal physiology of the kidney, especially with regard to regulation of body water, electrolytes, and acid-base metabolism (5) Introduction to the principles of management of children with chronic kidney disease (CKD stages 1-5); end stage renal disease, including both chronic dialysis and renal transplantation; and acute renal failure/injury and the therapeutic role of acute dialysis and continuous renal replacement therapy. Description: Residents will have the opportunity to participate in the evaluation and management of children with renal diseases, hypertension and electrolyte problems in both the inpatient and outpatient setting. Residents will see patients admitted to the inpatient Renal Service as well as interesting consultations. Inpatient rounds are conducted daily with a renal faculty member and the renal fellows for bedside teaching. Residents will also have the opportunity to see children with a faculty teacher in the Renal Clinic at least one half day weekly. The resident is encouraged but not required to review and present one topic at a renal conference during the month. The resident will also attend bimonthly Renal Biopsy Conference, monthly Uroradiology Conference, and weekly Renal Fellows Conference for didactic and interactive teaching. The clinical experience can be adapted to emphasize areas of interest specific to the needs of the rotating resident (examples: 1. more electrolyte problems and outpatient evaluation of hematuria and proteinuria for those interested in general pediatrics, 2. more intensive care consults for those with 26 subspecialty interests, or 3. a broad spectrum of problems specific to nephrology care for those interested in pediatric nephrology specialty). No call is expected. Restrictions on who is eligible for elective: None Restrictions on time of year elective offered: None NEUROLOGY ELECTIVE Director: Gary Clark, M.D. Contact: Robert S. Zeller, M.D. 832-822-1750, rszeller@texaschildrens.org Where to report first day: Discuss with Dr. Zeller Goals: (1) Acquisition of a broader base of knowledge and experience with chronic neurological problems of children commonly encountered in pediatric practice. Objectives: (1) Be able to perform a thorough neurological examination, take a neurological history (2) Feel comfortable treating common neurological problems including seizures and headaches Description: Blue Bird Clinic, 9th Floor, CCC. Diagnostic evaluation and continuing clinical management of neurological disorders commonly encountered in pediatric practice (seizures, C.P., headache, retardation, etc.). Residents work up new and return patients and present/discuss each child with attending neurologist. Psychologist and social workers are available for consultation. New patients 8:00 a.m. - 12 noon. Follow-up clinic 1:00 p.m. - 5:00 p.m. Restrictions on who is eligible for elective: None Restrictions on time of year elective offered: None OPHTHALMOLOGY ELECTIVE DIRECTOR: David K. Coats, MD CONTACT: Louise Thomas, please contact her prior to your start date 832.822.3234 WHERE TO REPORT THE FIRST DAY: CCC 640.00 - by 7:30 a.m. on the first day of your rotation so that you can receive this orientation and be available to start clinic at 8 a.m. GOALS: Your rotation in Ophthalmology is very short. Therefore, specific goals from the start need to be enumerated clearly so you can take advantage of your period of time with the Service. During the rotation we would like you to achieve the following goals: 1. Learn the 8-point ophthalmologic examination components. This does not mean that you need to know how to specifically perform all components that an 27 ophthalmologist does, but you should know what components comprise the examination and be able to perform them at a basic level. 2. The following examination skills should be mastered during your rotation. a. Motility examination, including Hirschberg Light Reflex Test, Alternate Cover Test, Ductions and Versions (Extraocular movements) b. Visual acuity testing, including fixation preference c. Pupils/ Brückner's simultaneous red reflex test d. External exam, including eyelid eversion e. Anterior examination with penlight f. Confrontation visual fields g. Pressure - intraocular by tactile tonometry h. Retinal/optic nerve examination, with a direct ophthalmoscope to evaluate the optic nerve and macula 3. Clinic responsibilities: 4. Surgery responsibilities: OBJECTIVES: We want you to have fun while on the service. We also want you to learn. Therefore, expectations on the rotation are high, and the work may be intense at times. There will be daily skill and knowledge assignments as well as a daily reading assignment. You will be graded based upon your performance during the rotation. The following may be used to help formulate your final grade on the rotation: Ability to master clinical skills, ability to master and apply new knowledge, ability to generate a differential diagnosis, examination skills, interaction with the faculty, participation in educational process, participation in patient care process, attendance, and other factors. DESCRIPTION: The following schedule is provided to facilitate your learning experience in the department of pediatric ophthalmology at Texas Children's Hospital. Morning activities began at 8 a.m., while afternoon activities began at 1 p.m. If the assigned attending physician is not available for a given session, you should spend that session with one of the fellows. At the beginning of the session, please remind the attending physician or fellow what skill or knowledge activity you are to master during the session. Please have the attending physician or fellow sign off on your activity sheet at the end of the session. If you are on an elective, rather than a selective, your rotation will last longer than two weeks. At the end of the training sessions outlined below you should begin seeing patients in the clinic on your own. You will be following the attending/fellow rotation day by day as outlined for the first two weeks. Ask the attending or fellow of that session about their protocol for medical student patient examination. You may also wish to spend additional time in the operating room during the final two weeks. Please arrange this with individual faculty members. In addition to the activities listed, there is a conference that Begins at 7:30 a.m. on Wednesday and Friday mornings in room 600.18. You are encouraged to attend these conferences if you are available, though we recognize that you may have lectures or a scheduled during this time if you are on the selective. We also recognize that you may not be available certain afternoons during the week due to continuity clinic activities. Please make up the skill or knowledge activity you miss by reviewing the activity with one of the fellows. 28 Week 1 Monday Dr. Paysse AM S: Vision Testing Dr. Yen K: Signs of serious red eye 2PM Dr. Steinkuller for Skills Overview PM Reading Assign. K: Tuesday Wednesday Dr. Steinkuller Dr. Yen Pupil Testing and Motility Exam Fellow, Resident or Dr. Steinkuller K: Pediatric Eye Examination Lecture **** S: Red reflex test Thursday Dr. Paysse (In OR 7th fl) S: IOP testing and S: Eyelid eversion techniques Dr. Paysse K: Differential diagnosis and primary care responsibility when abnormal red reflex detected Friday Dr. Steinkuller K: Dr. Fellow K: (If student is available) Using a direct ophthalmoscope Dr. Fellow S: Anterior segment exam and use of the slit lamp TBD *Develop report topic with a faculty member by the end of week 1 if you are interested in honors consideration. S = Skill training K = Knowledge acquisition **** Directions to get to the "Pediatric Eye Examination Lecture (this should be reviewed with either the fellow, resident or Dr. Steinkuller) Go to "Microsoft Powerpoint", File, Open, G: drive, Conference Rooms, CCC, Ophthalmology, ;MVPea_CPR 29 Week 2 Monday Dr. Paysse AM S: Visual field testing Dr. Yen PM Reading Assign. Tuesday Dr. Steinkuller K: Abnormal head posture Dr. Fellow Wednesday Dr. Coats (In OR 7th floor) S: IOP testing and Eyelid eversion techniques Thursday Friday Dr. Edmond Dr. Steinkuller K: Management K: AAP vision/eye of screening conjunctivitis recommendations for pediatricians Dr. Paysse Dr. Fellow K: Nasolacrimal K: Primary care K: Infant vision K: (If student duct management development available) obstruction of eye trauma Dr. Fellow K: "Written/oral examination" TBD S = Skill training K = Knowledge acquisition RESTRICTIONS ON WHO IS ELIGIBLE FOR THE ELECTIVE: None, but we request only one person at a time per rotation. Medical Students receives priority on rotation RESTRICTION ON TIME OF YEAR ELECTIVE OFFERED: None ORTHOPEDIC ELECTIVE Director: William Phillips, M.D. Contact: William Phillips, M.D. - WAPhilli@texaschildrens.org Where to report first day: 8th floor CCC, Orthopedic Surgery Clinic Goals and Objectives: (1) Improve their ability to evaluate a child with a musculo-skeletal problem, including history taking, examination and ordering appropriate imaging and laboratory studies. (2) Learn how to apply splints and casts. Description: The Pediatric Orthopaedic Surgery and Scoliosis Section at Texas Children's Hospital provides care for patients, aged newborn to skeletal maturity, with acute and chronic orthopaedic problems. Diagnostic and treatment management programs are provided for patients with musculoskeletal problems associated with trauma (including sports injuries), infection, metabolic disorders, connective tissue disorders, hematological disorders, inflammation, neuromuscular, bone tumors, congenital abnormalities, spinal injuries and many other general orthopedic problems. Children with normal variations such as intoeing, flat feet and truncal asymmetry are also seen. 30 The Pediatric Orthopaedic Surgery and Scoliosis Service also includes sub-specialty care for scoliosis, orthopedic oncology, leg length inequality, musculo-skeletal infections, skeletal dysplasias and neuromuscular diseases. Residents are welcome to observe orthopedic surgical procedures in the operating room and fracture reductions in the emergency room, but this is strictly optional. Emergency room call and night/weekend call are not required. Restrictions on who is eligible for elective: None Restrictions on time of year elective offered: None OTOLARYNGOLOGY ELECTIVE Director: Ellen M. Friedman, M.D. Contact: Rotations should be coordinated with Andrea Croft at 832-822-3268. Where to report first day: Otolaryngology clinic, 5th floor of CCC Goals and Objectives: (1) Master Pneumatic Otoscopy (2) Master the pediatric head and neck exam, as well as pneumatic otoscopy. (3) Learn to evaluate the role of and timing for medical versus surgical intervention in case management. (4) Interpret related diagnostic tests, including CT scans, MRI's and audiograms. (5) Become familiar with pediatric audiologic and speech, language and learning testing techniques. Description: A significant percentage of pediatric visits both in the office and emergency center are related to ear, nose, and throat problems. This one-month elective in pediatric otolaryngology has been developed to help the pediatric resident prepare for a role as a pediatric primary care giver. The emphasis of this elective will be the non-surgical, ambulatory management of patients. Pediatric residents (PL II & PL III) are invited to join this fulltime elective with eight-clinic sessions/week. Elective residents will also see inhouse consultations. If a resident wishes to follow a patient to the operating room or to go to the operating room to familiarize themselves with common otolaryngologic surgical procedures, this can be arranged easily. This is a very practical elective for pediatricians who will specialize in general pediatrics, since there is such a high incidence of otolaryngologic diseases in general practice. The specific spectrums of diseases seen on the elective generally are patients with airway distress or obstruction. The pediatric resident may expect to see patients with otitis media with effusion, acute otitis media, external otitis, cholesteatoma, hearing loss, pharyngitis, nasal obstruction, sinusitis, speech delay, head and neck masses, congenital malformation of the airway and head and neck, etc. There will be no required night or weekend call. This elective is limited to one house officer per month. 31 Restrictions on who is eligible for elective: None Restrictions on time of year elective offered: None PATHOLOGY ELECTIVE Director: Edwina Popek, D.O. Contact: Dr. Popek at least one week prior to the start of your elective to discuss personal goals and where to report on the first day. (832-824-2250) ejpopek@texaschildrens.org Where to report first day: See Contact Goals and Objectives: As mentioned above. Also, candidates must discuss their goals and plans with Dr. Popek prior to beginning the elective. Regardless of the choice of activity, each resident is expected to present a set of goals for the elective for the attending's approval and is then evaluated on the attainment of those objectives. This allows us to prepare for the resident. Especially if a specific area of study is wanted, we want to insure that there are appropriate and adequate pathology faculty to fulfill those goals. Description: Any area of Laboratory Medicine may be pursued during a 1 month elective. The resident will participate in the processing of gross specimens to develop an understanding of what is entailed in going from a tissue sample to having a pathology slides to examine and how a diagnosis is rendered. Residents are expected to participate in at least one autopsy during their 4 week rotation. In the past, pediatric residents have participated in autopsies, concentrated in microbiology or hematology, blood banking, neuropathology, gastrointestinal, renal, cardiac or pulmonary pathology, dermatopathology, etc., according to their expressed interests. Persons planning to practice in rural areas have benefited from practical experience in hematology, urinalysis, and microbiology. Attendance at the conferences within the department and preparation of pertinent presentations at these conferences are expected. Residents interested in Medical Informatics/management can undertake projects relevant to laboratory data usage and interpretation under the supervision of Gregory Buffone.There is no call or weekends associated with this elective. The day begins at 8am and usually is complete by 6pm. Accommodations can be made for residents who have clinical duties. Restrictions on who is eligible for elective: None. Two residents can be accommodated each month. Restrictions on time of year elective offered: None PICU Elective Director: Laura Loftis, MD, Associate Professor Contact: Pat Salazar 832-826-6208 Where to report first day: Transport office in the PICU by 6:20 am. 32 Goals and Objectives: (1) Learn assessment of the critically ill child (2) Learn the pathophysiology and management of common diagnoses seen in the ICU such as respiratory failure, shock and head injury (3) Learn the application of advanced modalities of support such as mechanical ventilation, high-frequency ventilation, renal replacement therapies (4) Gain experience with invasive procedures such as intubations and placement of central venous lines, arterial lines and chest tubes Description: One-month experience on the Pediatric Intensive Care Team participating in the care of critically ill children along with a fellow, attending and Nurse Practitioner or Physician Assistant. The elective will give the resident dedicated time with the fellow and attending for bedside teaching at an advanced level. The resident will follow his/her own patients, arriving at 6:20 a.m., rounding with the team twice a day, and departing after evening check-out rounds. Participation in twice weekly Section conferences will be encouraged. The resident may also accompany the fellow in resuscitation efforts as part of the In-patient Code Team (including RRTs), assessing patients on the floor for potential transfer, and evaluating and triaging transport calls. Shifts will be 6:30 a.m. - 6:30 p.m. Monday through Friday. Restrictions on who is eligible for elective: One resident per month Restrictions on time of year elective offered: September through May (There may be additional months that will be restricted due to number of people on a team. Schedules will have to be coordinated with ED/hospitalist fellows and anesthesia resident who also do the PICU rotation.) Call Dr. Loftis or Dr. Tcharmtchi regarding availability. PEDIATRIC SLEEP MEDICINE Director: Daniel Glaze, MD Professor of Pediatrics and Neurology Contact: Daniel Glaze, 832-826-2156 Where to report on the first day: 21st Floor West Tower Neurophysiology Office 8:00 am Goals and Objectives: (1) The learner will become familiar with common pediatric sleep problems such as sleep apnea, insomnia, parasomnias, Restless Legs Syndrome and Periodic Limb Movement Disorder, circadian disorders such delayed sleep phase disorder, and hypersomnia such as childhood narcolepsy, and the management of these sleep problems. (2) The learner will develop skills to effectively screen and identify pediatric sleep problems in the setting of a pediatric practice, to make appropriate referrals to the Sleep Center, and to understand when to refer for a sleep study and the information a sleep study provides. (3) The learner will gain a basic fund of knowledge concerning the developmental aspects of sleep in children and adolescents in order to promote healthy sleep habits and appropriately address concerns of parents concerning the sleep of their children. (4) The learner will understand the impact of sleep problems on cognitive and behavioral functioning of children, as well as, on the health of their families. 33 Description: This is a one month elective. Learners will participate in the TCH Children's Sleep Center including the evaluation and management of childhood sleep problems in the Sleep Clinic. The learner will have the opportunity to join the sleep medicine physicians as they interpret sleep studies and spend time with the day and nighttime sleep technologist as they perform and score sleep studies. Learners will attend sleep clinics and gain experience in evaluating and managing common sleep problems of children and teenager. They will attend weekly and monthly sleep conferences and activities of the Sleep Medicine Fellowship Program including didactic lectures, multidisciplinary case presentations, and journal club. The learner will have opportunities to participate in the weekly Sleep Center meetings concerning the operation of the Sleep Center. Ongoing clinical research will be reviewed with the learner. Reading materials covering the field of pediatric sleep medicine will be given to the learner and reviewed weekly. Recent informative journal articles will also be reviewed with the learner. The medical director of the TCH Children's Sleep Center is Daniel G. Glaze, M.D., Diplomate, American Board of Sleep Medicine, Associate Professor Pediatrics and Neurology, Baylor College of Medicine. Restrictions on who is eligible for elective: None Restrictions on time of year elective offered: Limited availability as elective is shared with Neurology residents PHYSICAL MEDICINE AND REHABILITATION Director: Aloysia Schwabe, M.D./Suzanne Woodbury, M.D. Contact: Becky See, 832-826-6106 Where to report on the first day: West Tower, 21st floor, Rm 329 Goals and Objectives: (1) Gain knowledge in a comprehensive approach towards maximizing the cognitive, physical, and overall functional status of a child with a disability. (2) Gain a basic understanding of the indications for bracing, special equipment, therapy services, and indications for a PM&R referral. Description: This full-time one month elective will give the pediatric resident an opportunity to see outpatients and consults with common and uncommon neurologic, developmental, orthopedic, oncologic, traumatic, or other disorders which lead to a functional deficit. Clinics presently include general PM&R, spasticity, and spina bifida. We also participate in the multidisciplinary MDA clinic and a peripheral nerve clinic. Procedures scheduled separately from clinic include EMG/NCS (electrodiagnostic studies), spasticity procedures including botox injections and intrathecal baclofen trials. In addition to clinics, the resident will participate in the consult service at TCH. The resident will also be introduced to the indications for electrodiagnostic studies and observe these studies. Restrictions on who is eligible for elective: Restriction of 2 residents per month 34 Restrictions on time of year elective offered: None PRIVATE PEDIATRICIAN OFFICE Director: Dr. Mark Ward, M.D. Contact: Pediatric Chief residents (chiefresidents@texaschildrens.org) Where to report on the first day: Will vary based on placement Goals: (1) To provide greater exposure to outpatient pediatric practice Objectives: (1) To improve diagnostic and therapeutic skills in common outpatient pediatric concerns. (2) To better understand the business and management practices of a private practice pediatric office. (3) To prepare the resident who is interested in a career in primary practice pediatrics. Description: One month spent in the community in a private pediatric practice. Electives in private practitioners' offices must be well supervised, not a locum tenens, and the resident must not be paid for such activities; the resident must be involved in patient care in a meaningful way and not simply an observer; the elective must be approved by a sponsoring pediatric department and such approval must be based on the CV of the preceptor and planned goals and learning objectives for the elective. It is imperative that a Board eligible or Board certified pediatrician be present to supervise the resident. Covering a solo practitioner's practice while he or she is on vacation cannot provide this type of supervision and is unacceptable. This must be done in the state of Texas, unless the resident has a valid medical license in the state in which it is to be done or can obtain a temporary license or an institutional permit. Restrictions on who is eligible for elective: None Restrictions on time of year elective offered: None PSYCHIATRY Director: Dana Kober Contact: Dana Kober, 832-822-3752 Where to report on the first day: Psychiatry and Psychology Service, CCC 1740.01 Goals: (1) Further knowledge of development: (2) Increase knowledge regarding the manifestations diagnosis and treatment of psychiatric disorders, such as ADHD, depression etc., and to be exposed to children with various neuropsychiatric syndromes. Objectives: 35 (1) To learn how to perform a comprehensive initial psychiatric evaluation of a pediatric patient which will include a detailed history, mental status exam, acquisition of corroborative data, laboratory work-up, medical consultations etc. (2) To learn follow-up management of both simple and complex pediatric psychiatry patients in an outpatient setting (3) To have exposure to multi-disciplinary treatment planning individualized for each patient, including psychopharmacology, school intervention, family, and group therapy etc. (4) To learn how to formulate a case and devise a treatment plan along a biopsychosocial format. Description: The resident will participate in in-patient and outpatient psychiatric consultations, the Pediatric Psychopharmacology Clinic and a multidisciplinary ADHD Clinic. The resident will work with child psychiatry and general psychiatry residents, child psychologists and the child and adolescent psychiatry staff. Teaching will be done by individual supervision by staff members, team participation, and didactic seminars. (1) Residents will observe and then have ‘hands on’ participation in the initial evaluation of a child or adolescent at the outpatient clinic at TCH. This would include interview with the present parent/guardian, and the child, as well as an opportunity to utilize play with the patient as an interviewing and diagnostic technique. (2) Residents will evaluate outpatients at the CAP, aftercare, feedback and follow-up clinics at TCH. (3) Residents will participate in educational activities: student presentations on Tuesday afternoon, department grand rounds on Wednesday. (4) Each resident is expected to present a brief (15-20 minutes) case report on a challenging patient with a diagnostic and management plan. Restrictions on who is eligible for elective: None Restrictions on time of year elective is offered: All months EXCEPT July, December and January. PULMONARY AMBULATORY ELECTIVE Director: Barbara West, M.D. Contact: Barbara West, M.D. (beeper 6236, ext 23302) Where to report on the first day: 8:30am to Clinical Care Center, Pulmonary Academic Offices, D1040.00. Ask to have Dr. Barbara West paged (beeper 6236) Please email Dr. West the week prior to your elective to confirm your start date. blwest@texaschildrenshospital.org Goals and Objectives: (1) Demonstrate the ability to: diagnose asthma in different pediatric age groups order diagnostic testing appropriately (such as CXR, sweat test, pulmonary function tests) explain the diagnosis to patient and family 36 - present treatment options to patient and family construct a treatment plan with input from the family educate the family about medications, triggers, environmental control, management of exacerbations. construct a written Asthma Action Plan for the family (2) Demonstrate the ability to use pulmonary function tests appropriately in the process of diagnose and ongoing management of pulmonary disorders such as asthma, cystic fibrosis, chronic cough, vocal cord dysfunction. (3) Demonstrate the ability to: appropriately prescribe a variety of inhaled drug delivery devices (such as spacers) teach families proper maintenance and use of these devices (4) Demonstrate the ability to appropriately manage premature infants with bronchopulmonary dysplasis after discharge from the nursery, especially in regard to: determining when supplemental oxygen can safely be discontinued determining when apnea monitor can be discontinued counseling families about SIDS risk factors and how to reduce risk (5) Demonstrate the ability to:recognize the signs and symptoms of vocal cord dysfunction and habit cough (6) Demonstrate a working knowledge of how to diagnose and treat these entities. Description: Usual work hours: M-F, 8:30-5:00 Location Texas Children’s Hospital. This elective is intended for those planning a career in ambulatory pediatrics, as well as anyone pursuing subspecialty training in which experience in pulmonary medicine will be useful. The elective emphasizes outpatient management of respiratory problems including asthma, cystic fibrosis, recurrent pneumonia, chronic cough (including habit cough), bronchopulmonary dysplasia, stridor, and vocal cord dysfunction. The importance of a collaborative selfmanagement approach to chronic illness will be emphasized. Residents will have opportunities to learn about the role of pulmonary function testing in pediatric patients. Residents will also receive instruction in haled drug delivery devices, such as spacers and dry-powder inhalers. Residents may also observe bronchoscopy, if desired. No call is involved with this elective Restrictions on who is eligible for elective: None Restrictions on time of year elective is offered: None RADIOLOGY Director: Amy Mehollin-Ray, M.D. Contact: Precillia P. Williams, Diagnostic Imaging, West Tower First Floor B120.21, 832/824-5325 Where to report on the first day: Arrive at 7am for ER readout in the main Reading Room, West Tower, and then check in with Precillia at 8am. Goals and Objectives: (1) An introduction to the principles of diagnostic imaging (2) A demonstration of the importance of clinicoradiologic correlation in proper 37 interpretation of imaging studies (3) Sufficient exposure to advanced imaging techniques to enable the resident to explain to patients and parents the test their child is to undergo (4) An understanding of the components of various diagnostic imaging examinations to facilitate the ordering of the correct examination for a given clinical indication Description: To accomplish these goals, the resident will review plain films with the attending radiologist each day, observe the performance and interpretation of advanced imaging procedures, and attend all clinicoradiologic and radiologic teaching conferences that occur during the elective period. The resident will also be expected to read a text on fundamentals in pediatric imaging*, present a case at one of the weekly radiology review conferences, complete a series of approximately 25 computer-based online pediatric imaging learning modules and pass a short multiple choice examination based on the reading material. Lane Donnelly's Fundamentals of Pediatric Radiology is available to borrow with a deposit. Restrictions on who is eligible for elective: 3 residents per month Restrictions on time of year elective is offered: None RESEARCH A resident may elect to do one or more months of research. Projects must have an attending as sponsor and supervisor and must be approved by Dr. Ward. The American Board of Pediatrics is concerned about any time during the residency spent in non-clinical assignments. To protect Board eligibility, it is imperative that all research electives be discussed with Dr. Ward. RHEUMATOLOGY Director: Maria Perez, M.D. Contact: Luis Paxtor, Dr. Perez’ secretary (832-824-3831) lpaxtor@bcm.tmc.edu Where to Report on the First Day: Feigin suite 940 at 8:15 am Goals and Objectives: (1) To allow Pediatric Rheumatology Fellows to enhance their medical knowledge of the pathophysiology, clinical features, diagnosis and management of pediatric rheumatologic diseases through supervised patient care in an outpatient setting. (2) To enable Pediatric Rheumatology Fellows to become competent in the longitudinal care of patients with pediatric rheumatic diseases and to recognize how to diagnose and manage disease flares, infection and other comorbid illnesses and the side effects of medications. (3) To enable Pediatric Rheumatology Fellows to diagnose and prevent those diseaserelated and treatment-related complications that lead to long term morbidity such as avascular necrosis, osteoporosis, and cardiovascular disease. 38 (4) To enable Pediatric Rheumatology Fellows to enhance their interpersonal and communication skills in dealing with the complex cultural, social, emotional and economic burden of a pediatric rheumatologic disesae. (5) To instruct Pediatric Rheumatology Fellows on the important systems-based practice issues including the internal and external systems that contribute to the betterment or detriment of the health care of pediatric rheumatology patients and the practice of evidence-based cost effective care. (6) To develop practice-based learning skills in the Pediatric Rheumatology Fellows to help deal with the complicated diagnostic and therapeutic challenges pediatric rheumatology patients present. (7) To involve pediatric rheumatology patients in ongoing research studies in pediatric rheumatology, including laboratory studies of aberrant immune function, clinical outcome studies including therapeutic infusion studies with new biological agents, research ethics, and the consent process. Description: The resident who selects this elective will spend his/her time managing both inpatients and outpatients with rheumatologic diseases. The majority of time will be spent in clinics at various settings. The resident will see patients at Texas Children's Hospital and Ben Taub General Hospital. Team-based care is emphasized. Goals for residents selecting this elective include the following: competence in the musculoskeletal examination; recognition of life or limb threatening diseases which affect the joints; awareness of significance and limitations of rheumatologic serologic markers; and indepth knowledge concerning the more common rheumatic diseases. Restrictions on who is eligible for elective: None Restrictions on time of year elective is offered: None SIMULATION MEDICINE ELECTIVE New for 2010-2011, Dr.Arnold will be offering an elective in simulation medicine. More information will be added to the elective guide soon. For questions, contact Dr. Jen Arnold at jlarnold@texaschildrens.org or by phone at 832-824-4990. SPORTS MEDICINE ELECTIVE Director: Joseph Chorley, M.D. Contact: Penny Johnson 832-822-3660 Where to report on the first day: 9AM in the office on the 17th floor of the CCC unless otherwise direct by email. Goals: This elective's primary educational and clinical goals are to facilitate expertise in the evaluation, examination, and treatment of musculoskeletal injuries Objectives: (1) completely examine the acutely and chronically injured ankle and knee (2) Know the basic principles of acute management of musculoskeletal injuries (3) Perform the preparticipation sports evaluation 39 (4) Research and present 20 minute presentation on musculoskeletal topic of their choice. Description: Residents will see patients in the TCH Sports Medicine Clinic with Drs. Hergenroeder and Chorley, as well as in outlying Baylor Teen Health Clinic sites and training room at the high school and collegiate level. Patients include children, adolescents, and adults with non-operative musculoskeletal complaints. There are some weekend and evening training room and sideline game coverage seasonally. Other topics include Sports Nutrition (Roberta Anding), Exercise Physiology, Physical Therapy Principles (Gabriel Brooks), Sports Psychology, and Musculoskeletal Radiology. Restrictions on who is eligible for elective: None Restrictions on time of year elective is offered: None PEDIATRIC SURGERY Director: Mary L. Brandt, M.D. Contact: Melissa Vaesa (mjvaesa@texaschildrens.org or 2-3143) Where to report on the first day: To be decided by email the week before. Please email Dr. Brandt in advance to set up your schedule (brandt@bcm.edu) or contact her administrative assistant, Melissa Vaesa (mjvaesa@texaschildrens.org or 832-822-3143) Goals and Objectives: (1) To learn diagnosis and appropriate referral of routine surgical problems in children such as inguinal hernias, soft tissue masses, and the thryoglossal duct cysts in the outpatient setting; (2) To learn and practice basic surgical skills needed for general pediatrics such as infant circumcision and repair of lacerations; (3) Depending on the learner’s needs, the elective may also include the inpatient care of complex pediatric surgical patients, and focus on more specific surgical skills. Description: The elective will focus on office based problems and procedures as well as the outpatient evaluation and management of surgical problems (e.g. differentiating inguinal and scrotal pathology, evaluating abdominal pain and appreciating the surgical significance of soft tissue and skin lesions). When appropriate, the resident may choose to participate in outpatient surgery, to correlate physical examination in the office setting with operative findings. However, the focus of this elective is ambulatory, and therefore no inpatient care, night or weekend call will be required. We encourage any resident who may be interested in the elective to contact us. For different aspects of a career in pediatrics, some areas of pediatric surgery will be more interesting than others and the elective can be tailored to the individual resident’s needs. For example, a resident anticipating a career in cardiology may choose to participate in placement of central lines and Portacaths or a resident interested in emergency medicine could choose to see ER consults. 40 Restrictions on who is eligible for elective: None Restrictions on time of year elective is offered: None SURGICAL SUBSPECIALTIES Elective Coordinator: Mary L. Brandt, M.D. Contact: Please email Dr. Brandt in advance to set up your schedule (brandt@bcm.edu) or contact her administrative assistant, Melissa Vaesa (mjvaesa@texaschildrens.org or 2-3143) Directors: David Coats, M.D., Ellen Friedman, M.D., Edmond Gonzales, M.D., William Philips, M.D., David Wesson, M.D. Where to report on the first day: To be determined in advance by email Goals: To learn how to diagnosis, treat, and appropriately refer routine outpatient surgical problems in children. Objectives: Learning Objectives will include, but are not limited to, the following: Pediatric Surgery (1) Accurate diagnosis of umbilical hernias, inguinal hernias and hydroceles (2) Diagnosis and treatment of routine neck masses Urology (1) Evaluation and treatment of enuresis (2) Current therapy for VU reflux Otorhinolaryngology (1) Therapy of recurrent otitis media, including indications for placement of PE tubes (2) Indications for tonsillectomy Ophthalmology (1) Evaluation and treatment of strabismus (2) Evaluation and treatment of amblyopia Orthopedic Surgery (1) Evaluation and diagnostic workup of the limping child (2) Evaluation of scoliosis in the outpatient setting Description: This elective will provide the resident with experience in the pediatric surgical subspecialty clinics. It is specifically designed for those residents planning a career in general pediatrics. A schedule will be given to each resident at the beginning of the rotation with assignments to each of the surgical clinics. The resident will be assigned to a specific attending each day who will be responsible for making sure the educational goals for the clinic are achieved. At the beginning of the rotation, the resident will receive reading material to cover the core concepts for each surgical subspecialty. No night or weekend call. 41 Restrictions on who is eligible for elective: None Restrictions on time of year elective is offered: None TOUCHPOINTS Director: Teresa Duryea, M.D. Contact: Teresa Duryea, M.D. teresad@bcm.edu or 832-822-3441 Where to report first day: Please contact Dr. Duryea 1 week prior to the rotation to arrange teresad@bcm.edu or 832-822-3441. Goals: The resident will gain more knowledge in the area of preventive health care through emphasizing behavior, anticipatory guidance, injury prevention and normal development. Objective: 1. To increase the learner’s level of comfort in areas chosen by the participant from a predetermined list of common behavioral and developmental themes. 2. To list strategies of anticipatory guidance specific for these families based on observation of children within their own communities and homes 3. To practice counseling techniques for common behavioral issues 4. To describe and outline issues relevant to patients and their families around common behavioral and developmental issues. 5. Reflect on patient care issues from a “parental” lens and discuss methods to improve one’s own care to families Instructional Methods: Readings Observation Reflection and discussion Experiential learning activities Evaluation: 1. Observation of counseling skills 2. Knowledge assessment 3. Written reflection relating to impact of newfound knowledge and skills on future patient care Description: The elective is tailored to the individual learner’s needs. A self-assessment is completed by each participant prior to starting the rotation and the learning activities are then selected to match the participant’s needs. Restrictions on who is eligible for elective: None Restrictions on time of year elective offered: None 42 UROLOGY Director: Edmond Gonzales, M.D. Contact: Edmond Gonzales, M.D. gonzales@bcm.tmc.edu 832-822-3172 Where to report on the first day: Contact the Urology fellow through TCH page operator prior to start date to discuss reporting time and location for first day. Goals: (1) Develop an understanding of the diagnosis and management of common pediatric urological problems. (2) Understand common pediatric urology surgical procedures such as hydrocele repair, hypospadias repair, hernia repair and orchiopexy. Objectives: (1) Residents are expected to integrate fully into the program; seeing office patients with their preceptor, working up hospitalized patients, and participating in operative care. Description: Pediatric Urology offers an opportunity to study the management of developmental and infectious problems of the genitourinary system in children. A third (PGY3) and fifth (PGY5) year urology resident and a pediatric urology fellow are currently assigned to pediatric urology and the pediatric resident will participate in their rounds and participate actively in the Outpatient Clinic and the Spina Bifida Clinic. Restrictions on who is eligible for elective: None Restrictions on time of year elective is offered: None 43