Cutaneous manifestations of autoimmune diseases A
advertisement
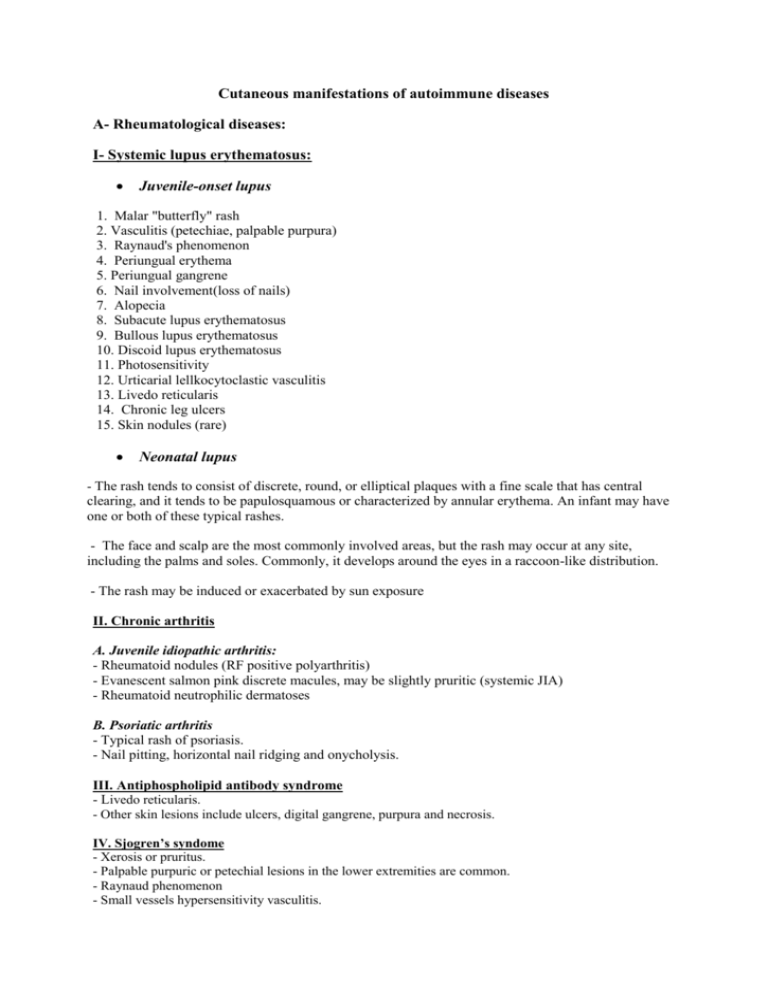
Cutaneous manifestations of autoimmune diseases A- Rheumatological diseases: I- Systemic lupus erythematosus: Juvenile-onset lupus 1. Malar "butterfly" rash 2. Vasculitis (petechiae, palpable purpura) 3. Raynaud's phenomenon 4. Periungual erythema 5. Periungual gangrene 6. Nail involvement(loss of nails) 7. Alopecia 8. Subacute lupus erythematosus 9. Bullous lupus erythematosus 10. Discoid lupus erythematosus 11. Photosensitivity 12. Urticarial lellkocytoclastic vasculitis 13. Livedo reticularis 14. Chronic leg ulcers 15. Skin nodules (rare) Neonatal lupus - The rash tends to consist of discrete, round, or elliptical plaques with a fine scale that has central clearing, and it tends to be papulosquamous or characterized by annular erythema. An infant may have one or both of these typical rashes. - The face and scalp are the most commonly involved areas, but the rash may occur at any site, including the palms and soles. Commonly, it develops around the eyes in a raccoon-like distribution. - The rash may be induced or exacerbated by sun exposure II. Chronic arthritis A. Juvenile idiopathic arthritis: - Rheumatoid nodules (RF positive polyarthritis) - Evanescent salmon pink discrete macules, may be slightly pruritic (systemic JIA) - Rheumatoid neutrophilic dermatoses B. Psoriatic arthritis - Typical rash of psoriasis. - Nail pitting, horizontal nail ridging and onycholysis. III. Antiphospholipid antibody syndrome - Livedo reticularis. - Other skin lesions include ulcers, digital gangrene, purpura and necrosis. IV. Sjogren’s syndome - Xerosis or pruritus. - Palpable purpuric or petechial lesions in the lower extremities are common. - Raynaud phenomenon - Small vessels hypersensitivity vasculitis. V. Dermatomyositis - Heliotrope discoloration of the upper eyelids. - Gottron’s papules. - Periungual erythema - Photosensitivity. - Vasculitic ulcers. - Hyperkeratosis. - Skin atrophy. - Calcinosis. VI. Scleroderma Diffuse Cutaneous systemic scleroderma - Edema - Sclerosis: acrosclerosis , Proximal scleroderma, and face is expressionless - Atrophy: shiny appearance of the skin accompanied by areas of hypo- or hyper-pigmentation (salt and pepper appearance). - Digital pitting scars - Telangiectases - Calcinosis. - Raynaud’s phenomenon Limited cutaneous scleroderma (CREST syndrome) - Calcinosis limited to the digits and telangiectases Morphea Plaque morphea: Generalized morphea Bullous morphea Linear morphea Linear morphea (linear scleroderma) En coup de sabre scleroderma Progressive hemifacial atrophy VII. Overlap syndrome A combination of Cutaneous features of lupus, dermatomyositis and scleroderma. VIII. Vasculitis disorder - General features: Palpable purpura, vasculitic urticaria, livedo reticularis, skin nodules and ulcers - Specific features: * In Henoch- schonlein purpura, the rash is most prominent on dependent or pressure-bearing surfaces, especially the lower extremities and buttocks, but it may occur in other areas. The cutaneous lesions range from small petechiae to large ecchymoses to rare hemorrhagic bullae; they tend to occur in crops and progress in color from red to purple to brown. Eruption may occasionally develop in large ecchymotic areas. The rash is often preceded by maculopapular or urticarial lesions. Subcutaneous edema over the dorsa of the hands and feet and around the eyes, forehead, scalp, and scrotum may occur early in the disease In Hypocomplementemic urticarial vasculitis, there are recurrent episodes of urticaria that are associated with pruritus and a burning sensation. In Kawasaki disease, although the rash usually begins on the trunk, there is often a perineal confluence during the first days of the illness, followed by desquamation in the diaper area by day 6 in most cases. Macular, morbilliform or targetoid lesions of the trunk and extremities are most characteristic. The rash is seldom pruritic, and vesicular or bullous lesions are rare. Acute hemorrhagic edema (AHE) Large cockade (rosette or knot of ribbons), annular, targetoid vasculitic rash. In Behcet disease, oral and genital ulcers. Other lesions include erythema nodosum, subcutaneous thrombophlebitis. Pathergy and dermatographism are seen in Behçet patients. In Wegener’s granulomatosis include palpable purpura, pyoderma gangrenosum-like ulcers on the extremities or the head and neck (so-called malignant pyoderma), papules over the extensor joints, oral ulcers. In sarcoidosis, the lesions may be maculopapular, vesicular, papular, or nodular (including erythema nodosum). Nodular subcutaneous sarcoid lesions. IX. Rheumatic fever - Erythema marginatum - Subcutaneous nodules - Erythema nodosum B- Endocrinal autoimmune disorders I. Graves’ Disease/ Hashimoto thyroiditis - Pretibial myxedema or thyroid dermopathy is raised waxy lesions in the pretibial area are usually the first sign of thyroid dermopathy with orange peel (peau d’orange) appearance. Lesions are usually symmetrical and asymptomatic, manifesting as diffuse non pitting edema, the plaque form, nodular form, and the most severe form which is associated with elephantiasis. -Vitiligo II. Diabetes mellitus typeI - Diabetic dermopathy or shin spots - Necrobiosis lipoidica (well-defined waxy plaques with central atrophy and telangiectasia on the shin). - Bullosis diabeticorum - Scleredema adultorum (commonly on the neck, upper back or the dorsa of the hands and fingers). - Granuloma annulare - There may be greater incidence of vitiligo, eczema and psoriasis in patients with type I diabetes. III. Polyendocrinopathies Autoimmune polyendocrine syndrome type 1 (APS-1) or autoimmune polyendocrinopathy candidiasis ectodermal dysplasia (APECED) - Chronic mucocutaneous candidiasis. - Alopecia areata, alopecia totalis, vitiligo, enamel hypoplasia and naildystrophy. APS-2 - Alopecia and vitiligo also occur in APS-2 but less frequently than in APS-1. IV. Autoimmune Addison’s Disease - Loss of axillary and pubic hair, dry skin and generalized hyperpigmentation . - Alopecia and vitiligo have been reported. C. Gastrointestinal Disorders I. Inflammatory Bowel Disease - Erythema nodosum (painful red nodules on pretibial area). - Pyoderma gangrenosum (papules or pustules leading to deep painful ulcerations with central necrosis). - Gastrointestinal-cutaneous fistulas (only in Crohn’s disease). II. Autoimmune hepatitis - Scleroderma-like lesions, erythema annulare centrifugum, morphea and hypertrichosis III. Primary Biliary Cirrhosis - Pruritus, xanthomatous lesions, melanosis and fungal infections IV. Celiac disease - Dermatitis herpetiformis - Alopecia - Dental enamel hypoplasia - Psoriasis D. Graft versus host disease (GVHD) I. Acute GVHD - Pruritic maculopapular lesions, skin dyspigmentation. In severe GVHD, generalized erythroderma, bullae formation or desquamation can develop, which may even progress to epidermal necrolysis. II. Chronic GVHD - Poikiloderma (pigment, atrophy, telang), sclerotic lesions, morphea like lesions. - Alopecia and nail loss are also common. Shin lesions resulting from treatment: - Bacterial, viral, fungal infections and warts. - Skin atrophy, telangiectasia: steroid therapy Skin manifestations of complications: e.g. ESRD - Uremic frost - The pigmentary alteration resulting from retained urochromes and hemosiderin deposition. - Large bullae: bullous disease of dialysis. - Nails show distal brown-red and proximal white coloring of half-and-half nails.