UPIQ Overview 9-14
advertisement

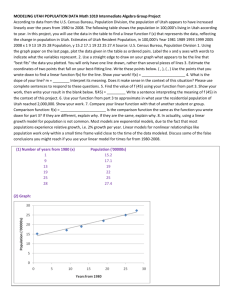
Translating medical knowledge into daily practice www.upiq.org Background: Continually improving the care we deliver is an obligation for all clinicians. Delivery of sub-optimal health care has been documented in every setting studied, including pediatric primary care. Mangione-Smith, et al. reported in 2007 that children in the U.S. receive less than half of the recommended preventive, acute and chronic care.1 This is not because clinicians don’t try to provide the best care possible – providing high quality, evidence-based, primary care is difficult, requiring that physicians incorporate ever-expanding scientific knowledge, evolving screening tools, and current treatment guidelines into their daily practices. They must provide care for children with routine needs, as well as for children with specialized and complicated needs, like those with cerebral palsy, depression, Down syndrome, celiac disease, Tourette syndrome, and many more. They must also guide patients and parents through a complex healthcare system, coordinate the care provided by specialists, and advocate for their patients with insurers and schools, all while adapting to a rapidly changing healthcare environment and responding to myriad demands from payers, government, and credentialing organizations. All this with limited resources and little training in quality improvement. The Utah Pediatric Partnership to Improve Healthcare Quality (UPIQ), established in 2003, is a collaborative effort of organizations and individuals with a common interest in promoting evidencebased best practices and assisting physicians in implementing quality improvement at the practice level. UPIQ provides education, guidance, tools, measurement, and ongoing support to help bridge the gap between knowing best practices and consistently implementing them in practice. Led by the University of Utah Department of Pediatrics, the Utah Chapter of the American Academy of Pediatrics, and the Utah Department of Health, UPIQ is a public-private partnership supported by grants, foundations, state programs, and generous in-kind contributions from its member organizations. Mission: To engage, lead and support practices in transforming the delivery of children's healthcare. Goals: 1. To foster innovation and the use of evidence in clinical practice and delivery systems to provide accessible, coordinated, and family-centered healthcare for Utah's children. 2. To champion, facilitate, and support practice change that improves the quality of care. Approaches: UPIQ is a pioneer in applying quality improvement (QI) principles and collaborative learning to primary care practice at the state level. Our Learning Collaboratives bring together practice teams (physician, nurse or MA, office manager, and, often, a family partner) for “learning sessions” where relevant scientific evidence is presented, QI techniques are taught, and teams are assisted in developing goals and strategies for improvement. Practices receive ongoing support and technical assistance from UPIQ staff (and each other) through conference calls, site visits, and repeated practice assessments over 9-12 months. Topics have included: preventive services delivery, asthma, ADHD, screening for developmental, social-emotional problems maternal depression, and toxic stress, obesity prevention, motivational interviewing, mental health, and providing comprehensive care for children with special health care needs (Medical Home). For their participation in our Learning Collaboratives, UPIQ offers pediatricians and, for some projects, family physicians credit toward part 4 of their specialty board’s Maintenance of Certification programs. Looking Forward: As of June 2014, UPIQ’s Learning Collaboratives have involved over 260 clinicians from over 90 practices statewide, including close to 50% of the state’s pediatricians and a growing number of family physicians and mid-level providers. To make a substantial difference in the health of Utah’s children, UPIQ aims to reach more practices, to help clinicians implement sustained QI processes and systems, and to support and to integrate our efforts with health system reform. We will also continue to identify collaborators, needs, and opportunities to help medical practices and to build a broad base of support for ongoing improvements in children’s healthcare. 1 Mangione-Smith R, DeCristofaro AH, Setodji CM, Keesey J, Klein DJ, Adams JL, et al. The quality of ambulatory care delivered to children in the United States. NEJM. 2007 Oct 11;357(15):1515-23. Updated June 2014 1 Partners: UPIQ’s Steering Committee includes the following representatives & organizations: • Department of Pediatrics, University of Utah (UPIQ’s administrative home) - Chuck Norlin, MD and Paul Young, MD • Utah Chapter, American Academy of Pediatrics - Mary Tipton, MD, Chapter Representative • Utah Department of Health (UDOH) > Division of Medicaid and Health Finance - Gail Rapp, Director, Bureau of Managed Health Care - Charlene Frail-McGeever, MBA, Project Director, Children’s Healthcare Improvement Collaboration > Division of Family Health and Preparedness - Nan Streeter, MS, RN, Deputy Director - Harper Randall, MD, Medical Director > Utah State School Nurse Consultant - Catherine Sparks, MSN, RN, NCSN Intermountain Healthcare’s Primary Care Clinical Programs - Wayne Cannon, MD, Medical Director • HealthInsight, (the quality improvement organization for Utah and Nevada) and Utah Chapter, American Academy of Family Physicians (UAFP) - Sarah Woolsey, MD, Medical Director • Pediatric Education Services (PES) of Primary Children’s Hospital (PCH) - Jonell Murray, Administrative Manager • University of Utah Health Plans - Julie Day, MD, Medical Director for Quality • Molina Healthcare of Utah - Brandon Hendrickson, Vice President for Provider Network Management & Operations • SelectHealth - Dot Verbrugge, MD, Medical Director • Family Voices of Utah - Gina Pola-Money, Director • Voices for Utah Children - Lincoln Nehring, JD, Senior Health Policy Analyst • Parent Representative and Advocate - Lisa Wade Current staff: • Director – Chuck Norlin, MD • Co-Director – Paul Young, MD • Senior Program Manager – Amy Wuthrich, MS • Quality Improvement Specialists – Homa Rehmani, MSW; Stephanie O’Brien, MS, CMHC; Gabrielle Baraghoshi, RN, MPH • Administrative Assistant – Yvonne Stayer Previous and current funding (since inception in 2003) – in addition to the generous in-kind and institutional support of the Partner organizations: • Primary Children’s Medical Center Foundation • American Academy of Pediatrics (AAP) Community Access to Child Health (CATCH) grant • Commonwealth Fund Assuring Better Child Development (ABCD2) grant / Utah Medicaid • AAP Partnerships for Quality grants • Church of Jesus Christ of Latter-Day Saints Foundation • Asthma Program, Utah Department of Health (UDOH) • Health Resources and Services Administration/Maternal & Child Health Bureau, through UDOH • Centers for Disease Control & Prevention / Utah County Early Head Start and Medicaid • Immunization Program, Utah Department of Health • Sanofi Pasteur (immunization manufacturer) • Utah Medical Association Foundation • Marriner S. Eccles Foundation • Abbott Laboratories • CHIPRA Quality Demonstration grant / Utah and Idaho Medicaid/CHIP programs Updated June 2014 2 UPIQ Learning Collaboratives and other Projects #1: Preventive Services Learning Session: 10/23/03; # of practice teams: 14 Funding: Primary Children’s Medical Center Foundation Focused on a range of preventive services. Published as: Young PC, Glade GB, Stoddard GJ, Norlin C. Evaluation of a learning collaborative to improve the delivery of preventive services by pediatric practices. Pediatrics. 2006 May;117(5):1469-76. #2: Developmental Screening Learning Session: 5/11/04; # of practice teams: 13 Funding: American Academy of Pediatrics (AAP) CATCH grant Focused on periodic assessment of developmental progress in infants and young children, use of validated tools in practice, and appropriate referral for those identified with delays or at risk. #3: Social and Emotional Screening of Infants Learning Session: 10/15/04; # of practice teams: 11 Funding: ABCDII grant through Utah Medicaid Focused on screening practices for identifying social and emotional problems in infants less than one year of age, and referring these young children for mental health assistance if problems are identified. #4: Social and Emotional Screening of Toddlers Learning Session: 5/25/05; # of practice teams: 10 Funding: ABCDII grant through Utah Medicaid Focused on screening practices for identifying social and emotional problems in toddlers, and referring these children for mental health assistance if problems are identified. #5: Attention-Deficit/Hyperactivity Disorder Learning Session: 6/22/05; # of practice teams: 18 Funding: AAP Partnerships for Quality grant Focused on improving care for patients with ADHD, including adherence to the American Academy of Pediatrics guidelines for the diagnosis and management of ADHD. #6: Medical Home/Integrated Services 1 Learning Session: 4/7/06; # of practice teams: 12 Funding: federal Maternal Child Health Bureau MCHB) Integrated Services grant through the UDOH Bureau of CSHCN Focused on introduction of the Medical Home concept, improving care of children with special health care needs (CSHCN), and collaborating with community services #7: Asthma Learning Session: 4/26/06; # of practice teams: 12 Funding: Utah Department of Health (UDOH) contract Focused on improving the care of children with asthma, including adherence to national guidelines and collaboration with subspecialists #8: Medical Home/Integrated Services 2 Learning Session: 6/23/06; # of practice teams: 12 Funding: MCHB Integrated Services grant through the Bureau of CSHCN Focused on newborn screening, hearing screening, vision screening in the Medical Home and collaborating with community services. #9: Maternal Depression Learning Session: 9/15/06; # of practice teams: 6 Funding: ABCDII grant through Medicaid Focused on screening for maternal depression at pediatric well child visits, telemedicine used to involve providers in St. George (southern Utah) Updated June 2014 3 #10: Early Childhood Oral Health Screening Learning Session: 11/2&3/06; # of practice teams: 13 Funding: Federal grant through Utah Valley Early Head Start Training pediatricians and family physicians to screening young children for oral health problems and application of fluoride varnish. #11: Medical Home/Integrated Services 3 Learning Session: 12/1/06; # of practice teams: 11 Funding: MCHB Integrated Services grant through the Bureau of CSHCN Focused on developmental, social emotional, and depression screening in the Medical Home and collaborating with community services. #12: Medical Home/Integrated Services 4 Learning Session: 6/13/07; # of practice teams: 11 Funding: MCHB Integrated Services grant through the Bureau of CSHCN Focusing on transition to adult care systems for CSHCN #13: Medical Home/Integrated Services 5 Learning Session: 10/10/07; # of practice teams: 11 Funding: MCHB Integrated Services grant through the Bureau of CSHCN Focused on transition to adult care systems for CSHCN #14: Improving Immunization in Primary Care Practice Project started: Winter, 2008; # of practices: 10 Funding: Phase 1 with CDC funds through the Utah Immunization Program Phase 2 with also a donation from sanofi-pasteur Using academic detailing and peer mentoring, IRB-waived study in 2 geographic areas #15: Prescribing for Asthma in Children Project started: Spring, 2008; # of practice teams: 7 Funding: Centers for Medicare and Medicaid Services through Utah Medicaid, 2 year project Focusing on prescribing asthma medications in primary care #16: Preventing, Identifying, and Treating Childhood Obesity Learning Sessions: May and June 2008; # of practice teams: 18; second set in spring, 2009 Funding: participant fees, UDOH, Church of Jesus Christ of Latter-day Saints Foundation Focusing on primary care interventions related to childhood overweight and obesity. #17: Preventing, Identifying, and Treating Childhood Obesity Learning Sessions: May and June 2009; # of practice teams: 13 Funding: American Academy of Pediatrics Utah Chapter, Church of Jesus Christ of Latter-day Saints Foundation, Marriner S. Eccles Foundation, Utah Medical Association Foundation, fees #18: Early Identification and Diagnosis of Autism in the Medical Home and supporting Dental Homes for children with Autism and Developmental Disabilities Project began: Winter, 2009; 15 practice teams in first year, 3-year project Funding: Health Resources and Services Administration, through the Utah Department of Health #19: Improving Short- and Long-term Outcomes of Newborn Screening Project began: October, 2009; 4-year project (with extension), 2 practices plus 4 group presentations Funding: Health Resources and Services Administration, through the Utah Department of Health #20: Preventing, Identifying, and Treating Childhood Obesity Learning Sessions: September and October 2010; # of practice teams: 7 Children’s Health Insurance Program Reauthorization Act (CHIPRA) Quality Demonstrations grant Updated June 2014 4 #21: Early Identification and Diagnosis of Autism in the Medical Home and supporting Dental Homes for children with Autism and Developmental Disabilities Project began: Winter, 2010; 17 practice teams; phase 2 of a 3-year project Funding: Health Resources and Services Administration, through the Utah Department of Health #22: Motivational Interviewing to Effect Behavioral Change in Pediatric Practice Learning Session: October, 2010; # of practice teams: 4, along with 4 physicians, 6 dieticians, and 1 nurse practitioner Funding: CHIPRA Quality Demonstration grant #23: Improving Immunization Rates in Primary Care Practice Project started: November, 2010; # of practice teams: 5 Funding: CDC funds through the Utah Immunization Program Using academic detailing and peer mentoring Medical Home Demonstration Project started: March, 2011; 3 ½ year project; # of practice teams: 9 primary care and 3 subspecialty. Funding: CHIPRA Quality Demonstration grant. Four sub-projects: #24: Improving Collaboration Among Pediatric Generalists and Specialists, June 2011 – Feb. 2012 #28: Implementing Care and Self-Care Plans for Children with Chronic Conditions, June 2012 – Feb. 2013 #31: Improving Healthcare Transitions, April – Dec. 2013 #34: Sustaining Medical Home Improvements, March – Nov. 2014 #25: Early Identification and Diagnosis of Autism in the Medical Home and supporting Dental Homes for children with Autism and Developmental Disabilities Project began: Winter, 2010; 10 rural practice teams; phase 3 of a 3-year project Funding: Health Resources and Services Administration, through the Utah Department of Health #26: Mental Health Problems in Children Learning Sessions: November 2011 and March 2012; # of practice teams: 7 Funding: CHIPRA Quality Demonstration grant #27: Improving Immunization Rates in Primary Care Practice Project started: March 2012; ongoing open enrollment; # of practices to date: 12 Funding: CDC funds through the Utah Immunization Program Using academic detailing and practice coaching #29: Mental Health Problems in Children (Phase 2) Learning Sessions: November 2012 and March 2013; # of practice teams: 9 Funding: CHIPRA Quality Demonstration grant #30: Immunization Protection in Child Care (IPiCC) Collaborating on a research grant studying QI in daycare settings to enhance immunization Funding: CDC #32: Improving Asthma Care for Children Learning Sessions: May and October 2013; # of practice teams: 12 Funding: CHIPRA Quality Demonstration grant, in collaboration with the Utah Department of Health Asthma Program and Utah School Nurses #33: Toxic Stress, Child Abuse, and Foster Care in Primary Care Learning Sessions: April and fall 2014; # of practice teams: 9 Funding: CHIPRA grant, collaborating with Division of Child and Family Services and others Updated June 2014 5 #35: Improving Asthma Care for Children Open enrollment, academic detailing project; recruitment began June 2014 Funding: CHIPRA grant Comments from Participants in UPIQ Learning Collaboratives I participated in 2 UPIQ learning collaboratives, one on developmental screening tools and the other on ADHD. They were both extremely informative and practical allowing me to implement new tools and approaches into my practice. We now use the ASQ screening questionnaire routinely in our well visits and have a more thorough and consistent way of tracking development. I am sure that I have made more referrals to up-to-3 programs than I did in the past. Parents also seem more clued into what their children should be capable of doing at various ages. Nina Jorgenson, MD Logan, UT I have been involved with the ADHD and Medical Home learning collaboratives. They were valuable to me & my patients. Our chronic patients have especially been pleased with the changes we've made because of the Medical Home Project. Marty Nygaard, MD St. George, UT Participating in the UPIQ developmental collaborative helped me edit the CHC’s (Community Health Centers) well-child forms to make them more practical … In the two years since I made those changes, I have seen a sharp reduction in calls from family practitioners asking me what to do with their 2 year old patient who only says single words. It was also useful for me to review the validated developmental tests, even though we can’t afford to use them. I am now turning again to that knowledge as I push CHC to institute some form of routine testing for autism at the 18 month visit. UPIQ participation was very useful for me. Carole Stipelman, MD Salt Lake City, UT The learning session in December was my first … I was very impressed with the presentations on Mental Health, Attention deficit, Autism and behavior issues. The young man who was the keynote speaker was excellent. I was impressed with all the presenters and the fact that they all provided the names of agencies, phone numbers and contact people. I think learning sessions are the key to providing opportunities and educating caregivers of people who have special needs Nancy Johnson, Parent Partner Orem, UT The recent learning session was very informative … the break out group [was] struggling with the issue of keeping the medical home alive after the grant is up, which totally surprised me as I feel as though it is not a huge deal to sustain this way of care. I really feel if you want to keep this idea alive and in action you need to educate the public to this way of care so they in turn can demand it for themselves and their loved ones who benefit the most from it. Liz Wall, Parent Partner Summit County, UT I found the asthma UPIQ very useful despite my resistance to the request to include my medical assistant and center manager. I ultimately included both employees and I believe they had a better understanding for the asthma education process. However, the only person who adopted or needed the kick in the butt to change her ways was me and I have given out "tons" more asthma education with asthma control tests and asthma action plans since the UPIQ meeting. Mindy Boehm, MD Ogden, UT Updated June 2014 6 [UPIQ’s] learning style is by far the best way to educate and empower physicians to really learn and change their practices. UPIQ is much more important to me than Grand Rounds, Common Problems and most articles/textbooks I read because the collaborative style gives me time to process my own ideas. It encourages (requires) me to synthesize hypotheses, test them and rethink the whole process again and again. Active learning! They didn't teach me that in medical school... Seriously, I would not have thought possible what I am doing now with the CATCH grant and reforming how my community thinks about medical homes for the uninsured without the direction UPIQ has given me. Kathy Ostler, MD Summit County, UT I have found UPIQ to be an important organization for the overall goal of all pediatricians – the improvement of the quality of healthcare given to children. I participated in the Learning Collaborative to improve screening for developmental disorders in the first two years of life. I am positive that my participation did in fact improve my screening ability which, of course, translates to better care for my patients. I must also say how impressed I have been with the UPIQ organization in general. One very important point in specific has been the willingness to work with each participant to make minor changes that meet the needs of a particular provider and that provider’s staff. That effort to individualize when possible absolutely makes each Learning Collaborative more likely to bring about a positive change in the practice of pediatrics in Utah. Joseph Jopling, MD Salt Lake City, UT Just let me take a minute to say thanks for all your efforts. Your work really has made a difference in our practice and in the lives of our patients. The difference can't be easily quantified but I am certain that it is substantial. I use the UPIQ project information every day. Thanks so much for all your hours of teaching and the ongoing contribution you make to our careers. We appreciate you very much. John Bennett, MD Spanish Fork, UT Although I was rather distant on participating following the in-house conferences, using the information at my clinic is a different story. I am very upbeat and encouraged by how easy it is to address childhood obesity with parents. Based on the project and things we have utilized here in my clinic, our whole clinic has decided to do a quality improvement project dealing with Childhood Obesity. Tricia Ferrin, DO Roy, UT Updated June 2014 7