21920 Describe support for a mental health consumer
advertisement

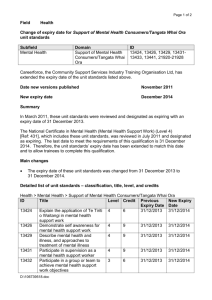
NZQA Expiring unit standard 21920 version 4 Page 1 of 6 Title Describe support for a mental health consumer/tangata whai ora using alcohol or other drugs Level 4 Credits 6 Purpose People credited with this unit standard are able to describe: aspects of the use of alcohol and other drugs; how to respond to a situation associated with the problematic use of alcohol and/or other drugs; and how to support a mental health consumer/tangata whai ora to minimise harm from their use of alcohol and/or other drugs. Classification Mental Health > Support of Mental Health Consumers/Tangata Whai Ora Available grade Achieved Explanatory notes Version 3 of this unit standard was republished in March 2012 to update the last date for assessment for superseded versions to 31 December 2014. 1 Glossary Alcohol and other drugs is the chosen term for this unit standard. Alcohol is a drug, but it is specified for two reasons. First, reference to drugs may or may not be interpreted to include alcohol. Secondly, specifying alcohol is an aid to people searching the NZQA web site for unit standards related to the use or management of alcohol. Consumer/tangata whai ora is used as a generic term to denote people who are users of mental health services. They may be referred to by various descriptive terms in the range of mental health settings. Characteristics and needs of the consumer/tangata whai ora may be physical, spiritual, or mental. Characteristics and needs include: age and stage of development; culture; disability; gender; health status; language; sexual orientation; and needs for physical comfort, safety, and privacy. Harm minimisation involves a range of approaches to reduce harm related to the use of alcohol and/or other drugs. It is a comprehensive approach that uses realistic strategies to take into account three interacting components: the people involved; their social, physical, cultural and economic environments; and the alcohol or other drugs themselves. Strategies will vary for different people in different circumstances, but they share the aim of minimising the impact of the use of alcohol and other drugs on individuals and their community. Abstinence based interventions can have a place within a harm minimisation framework. Community Support Services ITO Limited SSB Code 101814 New Zealand Qualifications Authority 2016 NZQA Expiring unit standard 21920 version 4 Page 2 of 6 Negative impacts may include but are not limited to: economic, health, effect on meeting full potential, forgetfulness regarding medication, abuse or other violence, crime, risky or illegal behaviours necessary to obtain and maintain use of alcohol and other drugs, disruption to family or whānau, compromise of culture, effect on ability to take part in cultural activities, other problems. Negative economic impacts may include homelessness, poverty, unemployment, absenteeism, reduced productivity. Negative health impacts include the impact on mental wellness and may include emotional, physical, and spiritual impacts. Other problems may relate to driving, learning, sexual activity. Other drugs refers to both prescribed and non-prescribed drugs, and includes anticholinergics, cannabis, benzodiazepines, inhalants, hallucinogens, opiates, and nicotine and other stimulants. Safe use is a relative concept that relates to the context and individual circumstances of the consumer/tangata whai ora. Any definition of safe use acknowledges the vulnerability of specific populations to the use of alcohol and other drugs; for example, age, gender, culture, and health status. This unit standard recognises that use of alcohol by a consumer/tangata whai ora is not necessarily unsafe or problematic, and that use of other drugs may be legal or illegal. 2 Assessment notes People awarded credit in this unit standard can outline the service provider's standards for safe practice in dealing with needles and body fluids. The following applies to the performance of all outcomes of this unit standard. All activities must comply with: a service provider guidelines, protocols, staff manuals, strategic plans, kawa, tikanga; b Mental Health Commission. 2001. Recovery competencies for New Zealand mental health workers. Wellington: Mental Health Commission; c relevant cultural, legislative, and regulatory requirements, which include but are not limited to: Code of Health and Disability Services Consumers’ Rights 1996; NZS 8134:2001, Health and Disability Sector Standards; Health and Disability Services (Safety) Act 2001; Health and Safety in Employment Act 1992; Human Rights Act 1993; Official Information Act 1982; Privacy Act 1993. 3 Resources may include but are not limited to a Adams, John B.; McKergow, Timothy W.; Eds. 1993. Drugs in Psychiatry – An Ashburn Hall Manual. 11th ed. Dunedin: Ashburn Hall Education and Research Foundation. b Alcohol Advisory Council of New Zealand. Oct 2004. Hui Whakakotahi 2004 – Proceedings from the 2004 Hui Whakakotahi 2004 in Rotorua. Wellington: Alcohol Advisory Council of New Zealand. c American Psychiatric Association Task Force on DSM-IV. c1994. Diagnostic and statistical manual of mental disorders – DSM-IV. Washington, DC: American Psychiatric Association. d Huriwai, Terry; Sellman, J. Douglas; Sullivan, Patrick; and Potiki, Tuari L. 2000. Optimal Treatment for Maori with Alcohol and Drug-Use-Related Problems: An Investigation of Cultural Factors in Treatment. Substance Use & Misuse. 35(3). 281-300. e Hutt, Marten. 1999. Te iwi Maori me te inu waipiro: He tuhituhinga hitori: Maori & alcohol: A history. Wellington: Health Services Research Centre for Kaunihera Whakatupato Waipiro o Aotearoa/Alcohol Advisory Council of New Zealand. Community Support Services ITO Limited SSB Code 101814 New Zealand Qualifications Authority 2016 NZQA Expiring unit standard 21920 version 4 Page 3 of 6 f MacEwan, Ian; and Ariell, Greg. 2003. Drinking and Your Health: Helping Problem Drinkers. Wellington: Alcohol Advisory Council of New Zealand. g Ministry of Health. 2001. A national strategic framework for alcohol and drugs. Wellington: Ministry of Health. This resource is available from the Ministry of Health website: http://www.moh.govt.nz h Rollnick, S.; Mason, P.; and Butler, C. 1999. Health Behavior Change: A Guide for Practitioners. London: Churchill Livingstone. i Todd, Fraser; Sellman, J. Doug; Robertson, Paul. 1999. The assessment and management of people with co-existing substance use and mental health disorders – A paper commissioned for the Alcohol Advisory Council of New Zealand; the Ministry of Health, New Zealand; and the Mental Health Commission. Wellington: Alcohol Advisory Council of New Zealand. j World Health Organisation. 1992. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organisation. k The Alcohol Drug Association New Zealand has a useful website related to alcohol and other drugs. The internet address is: http://www.adanz.org.nz l The Alcohol Advisory Council (ALAC) has a series of Pacific Reports available on its web site. The reports discuss the place of alcohol in the lives of people from Tokelau, Fiji, Niue, Tonga, Cook Islands and Samoa living in New Zealand. The internet address for ALAC is: http://www.alcohol.org.nz Note: the above references were current at the time of registration of this unit standard. New editions of resources a, c, and j are published from time to time. It is recommended that assessors and candidates use the editions that are current when candidates are preparing for assessment against this unit standard. Outcomes and evidence requirements Outcome 1 Describe aspects of the use of alcohol and other drugs. Evidence requirements 1.1 Alcohol and other drugs are described according to relevant factors. Range 1.2 relevant factors – classification; signs and effects, including positive feelings and negative impacts; continuum of use; classification – alcohol; other drugs (refer to glossary definition for range); signs and effects – behavioural, physical, psychological, social; positive feelings may include but are not limited to – belonging, celebration, feeling good, getting by, relaxing, socialising; negative impacts – refer to glossary definition; continuum of use – abstinence, safe use, hazardous use, problem use, dependence. Factors that may contribute to the use of alcohol and other drugs are described. Community Support Services ITO Limited SSB Code 101814 New Zealand Qualifications Authority 2016 NZQA Expiring unit standard Range 1.3 issues may include but are not limited to – loss of whenua, use of alcohol as a means of colonisation, change and loss of cultural practices, cultural isolation, pattern of consumption. Evidence is required in relation to two issues. Issues related to Pacific Peoples and alcohol and other drugs are described. Range 1.5 factors – biological, cultural, psychological, social, membership of an 'at risk' group; biological may include but is not limited to – family history of problematic use; genetic and physiological differences in reaction to intoxication, tolerance, dependence, and drinking behaviour; cultural includes cultural factors within Māori and Pacific peoples' cultures, and may include but is not limited to – cultural factors within other cultures defined by ethnicity, cultural factors within mental health consumer culture; psychological may include but is not limited to – grief, pleasure, symptom relief, trauma; social may include but is not limited to – hostility, prejudice, shame, socio-economic status, work pressures; 'at risk' groups may include but are not limited to groups defined by – age, gender, disabilities, peer group, sexual orientation. Evidence is required of two each of biological, cultural, psychological, social factors, and one 'at risk' group. Issues related to Māori and alcohol and other drugs are described. Range 1.4 21920 version 4 Page 4 of 6 issues may include but are not limited to – use of alcohol as a means of colonisation, change and loss of cultural practices, cultural isolation, pattern of consumption. Evidence is required in relation to two issues. Processes and services for intervention for people seeking assistance related to the use of alcohol and other drugs are described. Range processes – screening, assessment, cultural assessment, treatment (including brief and longer term treatment), after care; services – cultural, crisis, detoxification, assessment, treatment, peer support, services for people with co-existing disorders. Evidence is required of two service providers in the local community. Outcome 2 Describe how to respond to a situation associated with the problematic use of alcohol and/or other drugs. Evidence requirements 2.1 The description identifies skills that could be used to respond to a situation associated with the problematic use of alcohol and/or other drugs. Community Support Services ITO Limited SSB Code 101814 New Zealand Qualifications Authority 2016 NZQA Expiring unit standard Range 2.2 skills may include but are not limited to – raising and discussing the issue, de-escalation, self-protection strategies, request for Police assistance, referral to mental health support worker's supervisor or the clinical team. The description identifies priorities for responding to a situation associated with the problematic use of alcohol and/or other drugs. Range 2.3 21920 version 4 Page 5 of 6 priorities – safety and wellbeing of the mental health support worker; safety and well being of the consumer/tangata whai ora; safety and well being of family/whānau and others affected by the situation. The description outlines the standards and resources of the service provider for responding to a situation associated with the problematic use of alcohol and/or other drugs. Outcome 3 Describe how to support a mental health consumer/tangata whai ora to minimise harm from their use of alcohol and/or other drugs. Evidence requirements 3.1 The description outlines the change process involved in minimising harm from the use of alcohol and/or other drugs. Range 3.2 evidence is required in relation to a recognised model of change, which may include but is not limited to the Stages of Change model included in the resource referenced at explanatory note 3 f. The description outlines ways of supporting the consumer/tangata whai ora towards decisions and actions that minimise harm from their use of alcohol and/or other drugs. Range ways may include but are not limited to – recognising there is an issue; discussion with supervisor or others; raising the issue with the consumer/tangata whai ora; encouraging the consumer/tangata whai ora to take action; information giving; referral. Evidence is required of two ways. This unit standard is expiring. Assessment against the standard must take place by the last date for assessment set out below. Community Support Services ITO Limited SSB Code 101814 New Zealand Qualifications Authority 2016 NZQA Expiring unit standard 21920 version 4 Page 6 of 6 Status information and last date for assessment for superseded versions Process Version Date Last Date for Assessment Registration 1 26 October 2005 31 December 2016 Review 2 18 March 2011 31 December 2016 Rollover 3 17 November 2011 31 December 2016 Republication 3 13 March 2012 31 December 2016 Rollover 4 22 May 2014 31 December 2016 Consent and Moderation Requirements (CMR) reference 0150 This CMR can be accessed at http://www.nzqa.govt.nz/framework/search/index.do. Please note Providers must be granted consent to assess against standards (accredited) by NZQA, before they can report credits from assessment against unit standards or deliver courses of study leading to that assessment. Industry Training Organisations must be granted consent to assess against standards by NZQA before they can register credits from assessment against unit standards. Providers and Industry Training Organisations, which have been granted consent and which are assessing against unit standards must engage with the moderation system that applies to those standards. Requirements for consent to assess and an outline of the moderation system that applies to this standard are outlined in the Consent and Moderation Requirements (CMR). The CMR also includes useful information about special requirements for organisations wishing to develop education and training programmes, such as minimum qualifications for tutors and assessors, and special resource requirements. Community Support Services ITO Limited SSB Code 101814 New Zealand Qualifications Authority 2016