Neuromuscular Disease
advertisement

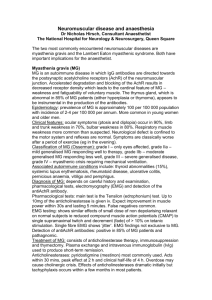
Neuromuscular disease is a term applied to diseases of nerve roots, plexuses, peripheral nerves, the neuromuscular junction, and muscle. Disorders of motor and sensory somatic cell bodies (anterior horn cells, dorsal root ganglia, and cranial nerve nuclei) are generally considered in this category as well. By exclusion, then, diseases of cerebral cortex, basal ganglia, cerebellum, and white matter tracts of the brain, brainstem, and spinal cord are not neuromuscular diseases. Hence, neuromuscular diseases typically present with progressive weakness and/or sensory symptoms without cognitive or higher cortical dysfunction, abnormal involuntary movements, bradykinesia, pathologic reflexes, spasticity, or a sensory level. The evaluation of patients with suspected neuromuscular disease begins by distinguishing patients with weakness only (that is, without sensory symptoms or signs) from those with sensory or sensorimotor symptoms. While neuropathy can spare sensory fibers in certain specific circumstances, weakness without sensory symptoms or signs usually suggests the neuromuscular diseases that are not neuropathies: muscle diseases, diseases of the neuromuscular junction, and motor neuron disorders. Each of these has distinct clinical features. Muscle Diseases Muscle diseases are classified into several categories. Among the most common are: 1. Muscular dystrophies. Dystrophies are heritable disorders in which the defect is generally in a gene coding for a structural protein, leading to destruction of muscle cells and, as a clinical consequence, gradually progressive limb weakness. Many dystrophies have now been shown to be due to mutations in genes coding for a complex of proteins that, among other things, anchor the contractile apparatus within the muscle cell to the cell membrane. Perhaps the best known of these proteins is dystrophin, which is abnormal in Duchenne muscular dystrophy, an Xlinked dystrophy that causes progressive weakness and early death in boys. Other common dystrophies include Becker dystrophy, a dystrophinopathy with a milder phenotype than Duchenne, Facioscapulohumeral dystrophy, an autosomal dominant condition named for the distribution of weakness and due to a mutation on chromosome 4, and limb-girdle dystrophy, which is in fact a genetically heterogeneous syndrome which can result from a variety of described mutations. Because dystrophies are disorders of structural proteins, they lead to striking pathologic alterations of muscle cells and, ultimately, cell death, with fibrosis and atrophy of affected muscles. 2. Inflammatory myopathies. The common inflammatory myopathies are polymyositis, dermatomyositis, and inclusion body myositis. Polymyositis is a T-cell mediated autoimmune myopathy characterized histologically by lymphocytic infiltration of muscle fibers. Polymyositis generally presents in adulthood with progressive, symmetric, proximal-predominant limb and neck flexion weakness. Dysphagia can occur due to involvement of the bulbar musculature. Myocarditis occurs rarely as well and can cause congestive heart failure. Serum CK is nearly always elevated and 1 electromyography of affected muscles demonstrates characteristic myopathic features. The diagnosis is confirmed histologically, and it is best to biopsy a muscle that is clinically affected to a moderate degree. Treatment of polymyositis with oral or intravenous steroids generally results in significant improvement, although treatment must be continued for months and often years. Because long-term immunosuppression is commonly needed and results in significant cumulative steroid side effects, steroid-sparing agents such as azathioprine can be very useful adjuncts in polymyositis. Like polymyositis, dermatomyositis typically presents with progressive, symmetric, proximal-predominant weakness of the limbs and trunk, at times with bulbar and cardiac involvement as well. Nonetheless, dermatomyositis is distinct from polymyositis in several important respects. In polymyositis the primary immune attack is against muscle itself, whereas dermatomyositis is an inflammatory microvasculopathy. Thus, polymyositis is characterized histologically by direct inflammatory infiltration of muscle fibers, while in dermatomyositis, inflammatory infiltrates are most prominent in the perviscular spaces and perimysial connective tissue. Both result in necrosis and regeneration of muscle fibers, but in polymyositis the distribution of necrotic fibers is relatively diffuse, whereas the histologic hallmark of dermatomyositis is “perifascicular atrophy,” in which groups of atrophic fibers are seen, largely on the periphery of muscle fascicles, and presumably due to infarction. Dermatomyositis is a multisystem disease, and is associated with a characteristic erythematous rash which is most commonly seen on the dorsum of the hands, the face, and the eyelids. The relative degree of involvement of skin and muscle varies considerably among patients. Involvement of other organ systems, either individually in the context of a specific connective tissue disease, can occur as well. Dermatomyositis occurs in both children and adults and is associated with an increased incidence of malignancy in adults. Inclusion body myositis (IBM) is a progressive myopathy generally presenting in men in mid to late adult life. IBM has several distinct features. Clinically, it progresses inexorably over many years and can result in severe disability and, ulltimately, severe dysphagia and ventilatory failure. Unlike nearly all other neuromuscular disorders, IBM has a predilection for involvement of the quadriceps muscle. The long finger flexors are also disproportionately affected in this condition. The diagnosis is confirmed by muscle biopsy. In addition to variably severe inflammatory infiltrates, IBM demonstrates a distinct combination of congophilic inclusions and rimmed vacuoles. The inclusions represent deposition of amyloid. While the cause of IBM is unknown, it is suspected that the primary pathology is the amyloid deposition and that the inflammatory infiltrates are secondary. This view is supported by the observation that treatment with immune modulating therapies results in transient improvement at best but does not influence the long-term course of the disease. Other categories of muscle disease include: 3. Toxic myopathies 4. Endocrine myopathies 5. Congenital myopathies 6. Mitochondrial myopathies 2 7. Myotonic dystrophy Disorders of Neuromuscular Transmission The neuromuscular junction is a specialized adaptation of both the nerve terminal and the muscle cell membrane which allows depolarization of a motor axon to result in depolarization of a muscle cell membrane and, ultimately, contraction of that muscle fiber via excitation-contraction coupling. The motor nerve terminal is a specialized structore containing vesicles of the neurotransmitter acetylcholine. The arrival of a wave of depolarization at the nerve terminal allows voltage gated calcium channels in that region to open. The resultant influx of calcium results in turn in the fusion of acetylcholine vesicles with the nerve terminal (the presynaptic membrane) and release of acetylcholine into the synaptic cleft between the nerve terminal and muscle membrane. The muscle membrane (the postsynaptic membrane) is a highly redundant structure studded with acetylcholine receptors. The redundancy of the postsynaptic membrane and the exceedingly high number of acetylcholine receptors assure effective transmission across the synapse. When a sufficient quantity of acetylcholine binds to the postsynaptic receptors, sodium channels in adjacent muscle membrane open, leading to depolarization of the muscle cell and, in turn, contraction. Disorders of neuromuscular transmission can thus be classified as due to either presynaptic or postsynaptic pathology. Myasthenia gravis is the most common disorder of neuromuscular transmission and is due to postsynaptic pathology. Myasthenia is caused by autoantibodies directed against the acetylcholine receptor. While antibodies can disrupt neuromuscular transmission by blocking the receptor site, the primary cause of impaired neuromuscular transmission in myasthenia is antibody-mediated destruction of the postsynaptic membrane, either due to complementmediated destruction of the membrane, internalization and destruction of acetylcholine receptors, or both. The result is a simplified postsynaptic membrane and enlarged synaptic cleft. This reduces the “safety factor” of neuromuscular transmission and, ultimately, leads to failure of neuromuscular transmission. Myasthenia presents with muscle weakness and prominent fatiguability. Because repeated discharges of motor neurons lead to relative depletion of acteylcholine available for release, fatigue is not only a symptom but can be observed clinically after repeated or sustained muscle contraction. Extraocular and bulbar muscles are often prominently affected in addition to limb and trunk musculature. Unlike many myopathies, both proximal and distal muscles are affected, usually in an asymmetric distribution. Symptoms are often more prominent towards day’s end. While most patients have some limb or bulbar weakness (generalized myasthenia), in a significant minority of patients, weakness is restricted to the extraocular muscles (ocular myasthenia). Neurophysiologic testing will often demonstrate subclinical involvement of other muscles in patients with ocular myasthenia. A clinical diagnosis of myasthenia gravis can be confirmed in three ways: 3 1. 2. 3. Neurophysiologic testing. Repetitive nerve stimulation at 2-3 Hz results in a characteristic progressive decrement in the amplitude of the evoked muscle response, as neuromuscular transmission fails in some muscle fibers due to depletion of available acetylcholine. In single fiber electromyography, abnormal variation in the relative latency of muscle fiber contraction can be demonstrated when two fibers innervated by the same motor neuron are compared. This abnormal variation, called “jitter,” is also an indication of impaired neuromuscular transmission. Neurophysiologic studies are highly sensitive when symptomatic muscles are studied, or in any muscles of patients with clinically significant generalized myasthenia. They are not specific for myasthenia gravis, but are strongly supportive of the diagnosis when the clinical presentation is consistent. Antibody testing. Serum antibodies that bind to the acetylcholine receptor are present in at least 80% of patients with generalized myasthenia gravis and 55% of patients with purely ocular myasthenia. These antibodies are rarely seen in individuals with other autoimmune conditions. They are highly specific for myasthenia gravis in patients whose clinical presentation is typical. Response to anticholinesterase medications. By inhibiting metabolism of acetylcholine in the synaptic cleft, edrophonium (Tensilon®) enhances the availability of acetylcholine. A clinical response to an intravenous bolus of Tensilon has long been used as a functional diagnostic test for myasthenia gravis. Unfortunately, the response to Tensilon is often equivocal; furthermore, any condition in which neuromuscular transmission is impaired might improve transiently with Tensilon. While still occasionally used as an adjunctive diagnostic tool, this procedure should not be used as the sole diagnostic test for myasthenia gravis. Effective treatment of myasthenia gravis requires immunosuppressive therapy. The mainstay of treatment is steroid therapy. Prednisone is typically begun at a dose of about 1 mg/kg. Myasthenic weakness often worsens 1 to 2 weeks after starting prednisone, followed by a striking and sustained improvement in most patients. After a sustained response is achieved, prednisone is tapered very gradually, generally over a period of months to years. Unduly rapid tapering commonly leads to relapse, particularly when the prednisone dose drops below 20-30 mg/day. In order to avoid the weakness commonly associated with initiation of high dose prednisone, as well as for the purpose of determining the minimum effective dose, some neurologists begin with relatively low doses and gradually increase until an adequate response is obtained. Steroid-sparing agents such as azathioprine, cyclosporine, and mycophenylate mofetil are often used as adjuncts to allow a more rapid steroid taper and are occasionally used alone. The clinical improvement from these medications is generally not as immediate as that seen with prednisone. Myasthenia gravis sometimes worsens abruptly, leading to life-threatening dysphagia and ventilatory failure. This is referred to as myasthenic crisis, and can occur spontaneously 4 or after a medical illness such as infection. In addition to intensive supportive care and mechanical ventilation if necessary, rapid improvement in myasthenic weakness can often be achieved with plasma exchange (PLEX) or intravenous immunoglobulin (IVIg). Unlike steroid therapy, which generally requires several weeks’ time to take effect, PLEX and IVIg often provide benefit within days, and are thus ideal treatment modalities in the setting of myasthenic crisis. Although the benefit of these treatments is short-lived (generally several weeks), repeated courses of PLEX or IVIg are occasionally used in patients who are refractory to or intolerant of other immunosuppressant therapies. Thymectomy is also commonly used as a treatment in myasthenia gravis. Uncontrolled series suggest that thymectomy enhances the chance for a sustained remission, with the apparent benefit developing months to years after the procedure. Both B- and CD4+ T-cells that recognize the acetylcholine receptor have been found in the thymus in myasthenia gravis. Thymectomy is generally recommended in patients under the age of 60 with generalized myasthenia; it appears to be less effective in older patients and its use in patients with ocular myasthenia is controversial. About 10% of patients with myasthenia have a thymoma, a histologically benign tumor of the thymus gland. Thymectomy is recommended in all patients with thymoma. Finally, oral anticholinesterase agents are used for symptomatic relief. Mestinon® is the most commonly used such drug in North America. While Mestinon is clearly beneficial in alleviating symptoms in most patients, it is important to emphasize that it has no effect on the autoimmune pathogenesis of the disease, and should therefore not be used as the sole treatment modality in patients with clinically significant generalized myasthenia. Lambert-Eaton Myasthenic Syndrome (LEMS) is a rare acquired presynaptic disorder of neuromuscular transmission. LEMS is caused by an antibody to the voltage gated calcium channel (VGCC) and can occur either in isolation or as a paraneoplastic syndrome, most commonly in association with small cell lung carcinoma. When LEMS presents as a paraneoplastic phenomenon, it is believed that the pathogenic antibody forms as part of the immune response to VGCCs on tumor cells. Symptoms of LEMS often develop before the tumor becomes symptomatic, which may reflect the beneficial effect of the immune response in suppressing tumor growth. As indicated above, release of acetylcholine from the nerve terminal is triggered by calcium influx via VGCCs. Thus, blockade of VGCCs leads to impaired acetylcholine release and, in turn, impaired neuromuscular transmission. The clinical presentation in LEMS differs from that seen in myasthenia. In LEMS, patients typically present with mild to moderate bilateral proximal weakness with hypo- or areflexia. In contrast to myasthenia, extraocular muscles are usually spared. LEMS is also associated with autonomic findings such as anhidrosis, dry mouth, and erectile dysfunction. Antibodies to VGCCs are detectable in the serum in most patients with LEMS. The diagnosis can also be confirmed with neurophysiologic studies. As in myasthenia gravis, 2-3 Hz repetitive nerve stimulation often demonstrates a decremental response in LEMS. In LEMS, however, routine motor nerve conduction studies demonstrate a low amplitude response in most if not all muscles. After rapid repetitive stimulation or a sustained 5 voluntary contraction, there is a transient but marked increment in the amplitude of the response. This is not common in myasthenia unless the deficit is very severe. The increment after exercise in LEMS occurs because sustained or repetitive contraction facilitates calcium entry through available VGCCs, thus enhancing the chance of effective acetylcholine release after the subsequent test stimulus. Treatment of LEMS is generally less satisfactory than treatment of myasthenia. Perhaps the most important initial intervention is an aggressive search for malignancy. Treatment of a tumor, when one is found, may result in improvement in neurologic symptoms. As in myasthenia, LEMS can also be treated with both symptomatic therapy as well as immunotherapy. Some patients obtain symptomatic relief with mestinon, although the benefit is usually modest. LEMS is also treated with 3,4 diaminopyridine (3,4-DAP). 3,4-DAP blocks the potassium channel responsible for restoring the resting membrane potential after nerve depolarization. This results in prolonged depolarization of the nerve terminal and, in turn, prolonged opening of the voltage-gated calcium channel. LEMS can be treated with immunotherapy as well. Steroids, azathioprine, PLEX, and IVIg have all been used, with less consistent benefit than in myasthenia. Because the pathogenic antibodies may suppress tumor growth, immunotherapy should probably not be used in patients with paraneoplastic LEMS without treatment of the tumor itself. Acetylcholine release can also be inhibited by bacterial toxins, most notably tetanus and botulinum toxins. Treatment is largely supportive. Antitoxins are available for both. Motor Neuron Disorders Voluntary muscle is innervated by motor neurons in the brainstem nuclei and the anterior horn of the spinal cord. These neurons are in turn innervated by cortical motor neurons of the primary motor cortex. While motor neurons can be damaged in a wide variety of pathologic processes, several disorders selectively target motor neurons. These include amyotrophic lateral sclerosis (ALS), primary lateral sclerosis (PLS), spinal muscular atrophy (SMA), focal motor neuron disease, X-linked spinobulbar muscular atrophy (SBMA, or Kennedy’s Disease), and poliomyelitis. The following is a review of ALS, the most common of the motor neuron diseases. Diagnosis of ALS ALS is characterized by gradual, progressive loss of both cortical (“upper”) as well as bulbar and spinal (“lower”) motor neurons. It is this combination of upper and lower motor neuron disease in the same myotomes that makes ALS unique. Clinically, this is revealed by the presence of hyperreflexia, pathologic reflexes, loss of abdominal reflexes, or spasticity 6 – all signs of upper motor neuron disease – in myotomes with neurogenic atrophy – a sign of lower motor neuron disease – in the absence of sensory, cognitive, cerebellar, or extrapyrimidal symptoms or signs. Fasciculations, which can be seen in a variety of disorders of anterior horn cells, nerve roots, and peripheral nerve, as well as in some normal individuals, are often prominent as well. Electromyography and nerve conduction studies (EMG/NCS) are always needed to confirm lower motor neuron involvement, to determine the extent of lower motor neuron involvement, and to exclude other neuromuscular causes of weakness such as polyneuropathy, disorders of neuromuscular transmission, and myopathy. In some cases, neurogenic atrophy may not be prominent but needle electromyography will demonstrate widespread evidence of loss of lower motor neurons. Conversely, in some cases the clinical presentation may be so striking that EMG/NCS hardly seems necessary; however, the consequences of making a diagnosis of ALS are so profound that a careful search for other causes of weakness is mandatory. For the same reason, neurologists will often perform serologic screening for certain metabolic, toxic, or infectious conditions even though these conditions mimic ALS exceedingly rarely. Such conditions include hyperthyroidism, hypoparathyroidism, lead toxicity, Lyme disease, and HIV infection. A progressive disorder of motor neurons has also rarely been described in the setting of lymphoma and other malignancies, so a general physical examination and appropriate malignancy screening should be performed in any ALS suspect. There is a handful of conditions that are particularly likely to be misdiagnosed as ALS. These include structural lesions of the cervical cord and brainstem, inclusion body myositis, and multifocal motor neuropathy. There are also other motor neuron diseases which must be distinguished from ALS and which will be discussed separately. Any lesion that damages corticospinal tracts as well as nerve roots or cell bodies in the brainstem or anterior horn will result in a combination of upper and lower motor neuron findings. The clue, of course, is that the lower motor neuron findings – reflecting injury to cell bodies at the level of the lesion – will be in myotomes rostral to the upper motor neuron findings, which reflect injury to the descending corticospinal tracts. For this reason, whenever lower motor neuron findings exist exclusively rostral to lower motor neuron findings, imaging (usually MRI) of the relevant level of the central nervous system is mandatory. Cervical spondylosis, meningioma, and syrinx are among the many lesions that might result in such a presentation. Inclusion body myositis (IBM) is a slowly progressive myopathy of older adults which, because of the presence of atrophy, weakness without sensory findings, and largely preserved reflexes, is occasionally mistaken for ALS. The distinction is made on the basis of a distinctive distribution of muscle weakness, absence of pathologic reflexes, myopathic features on EMG, and characteristic findings on muscle biopsy. IBM is discussed further above among the inflammatory myopathies. Multifocal motor neuropathy (MMN) is a pure motor demyelinating neuropathy which is often associated with prominent cramps and fasciculations, clinical features that are also common in ALS. In MMN, unlike ALS, pathologic reflexes are rarely, if ever, present; furthermore, MMN tends to present in the distribution of individual nerves rather than 7 spinal cord segments, and is diagnosed on the basis of distinctive electrodiagnostic features that are usually readily identified. Unlike ALS, MMN responds to immunotherapy, so it is important not to miss the diagnosis. ALS typically begins focally and spreads to adjacent regions. Thus, if the initial symptom is weakness of the left lower limb, it is likely to spread to the left side of the trunk or right lower limb before affecting the upper limbs or bulbar musculature. Bulbaronset ALS, in which the initial symptoms are in the bulbar musculature, is often distinguished from limb-onset ALS. Furthermore, in some individuals symptoms and signs of upper motor neuron dysfunction, such as spasticity and hyperreflexia, predominate, while in others there is more prominent involvement of lower motor neurons, characterized by atrophy and fasciculations. The variation in distribution of weakness and degree of upper motor neuron involvement combine to result in a wide variety of clinical findings, so that any casual visitor to an ALS clinic might be surprised to learn that all patients carry the same diagnosis. For example, patients with bulbar ALS commonly walk unaided into the examining room, with little overt functional disability in the limbs, but with severe dysarthria and dysphagia. Careful examination will reveal variable degrees of upper motor neuron, or “pseudobulbar,” findings, such as a spastic dysphonia, slow and awkward tongue movements, jaw clonus, or a brisk gag reflex despite diminished volitional elevation of the palate. For unclear reasons, a “pseudobulbar affect,” characterized by exaggerated and socially embarrassing laughing or crying, is often seen as well. The most striking evidence of lower motor neuron bulbar involvement in most patents with bulbar ALS is atrophy and fasciculations in the tongue. By contrast, patients with upper motor neuron-predominant lower limb-onset ALS develop a spastic gait followed by progressive quadriparesis, usually with good bulbar function until very late in the disease. These patients often progress slowly and remain independent for a long period of time because of relatively preserved strength and hand function. Others present with prominent lower motor neuron findings in the upper limbs (“brachial amyotrophic diplegia”). And so on. As will be discussed below, the variety of presentations leads to a variety of functional needs that must be addressed by the ALS care team. Etiology Although a great many hypotheses have been put forward, the cause of ALS remains unknown. It may be that several mechanisms can cause death of motor neurons. Current hypotheses include excitotoxicity due to impaired reuptake of glutamate, an excitatory neurotransmitter, neurofilament dysfunction, leading to impaired protein transport within the axon, and accelerated apoptosis of motor neurons. Despite numerous clinical trials, only one drug, riluzole, has been approved for treatment of ALS. Riluzole is a glutamate antagonist which has been shown to retard progression of ALS to a very modest degree. Management 8 The management of ALS is largely supportive. Occupational and physical therapists can be very helpful in devising strategies to maintain function despite disability. Patients with bulbar symptoms require speech therapy as well as periodic swallowing evaluations because of the risk of aspiration. As speech and swallowing difficulties progress, communication devices and gastrostomy become necessary. Pseudobulbar affect can often be managed successfully with tricyclic agents. Spasticity is managed with lioresal or tizanidine. Ventilatory dysfunction poses a special problem in ALS. Mild to moderate ventilatory insufficiency can often be managed successfully with noninvasive positive pressure ventilation such as BiPAP (bilevel positive airway pressure). BiPAP is often remarkably effective even in patients who have severe ventilatory dysfunction and are dependent upon mechanical ventilation. Invasive mechanical ventilation via tracheostomy and a ventilator has two significant advantages over BiPAP, however: first, tracheostomy provides airway protection in patients at risk for aspiration, and second, tracheostomy allows for much more effective pulmonary toilet. Tracheostomy is usually not necessary until the late stages of ALS, when patients are entirely dependent in activities of daily living. Because most patients perceive the quality of life at this point to be poor, few choose invasive mechanical ventilation. End of life care End-stage ALS brings the complications of immobility, such as frozen shoulder, pain, and constipation. Caregiver burnout is a common problem, as patients require around the clock care. Hospice care often plays an important role in end-stage ALS by providing respite care, pain management, and narcotic analgesics to alleviate the anxiety and air hunger due to ventilatory failure. Neuropathy As indicated above, neuropathy (or polyneuropathy; that is, a systemic process affecting multiple nerves) should be suspected in any patient presenting with sensory and motor symptoms affecting more than one limb without signs referable to the central nervous system. To simplify the evaluation of neuropathy, neurologists classify neuropathies according to four features: the time course, the modalities affected (motor, sensory, and autonomic), the distribution (diffuse or multifocal), and the nature of the primary pathology (axonal or demyelinating). Once characterized in this fashion, the differential diagnosis of a neuropathy is generally reduced to a manageable list of possibilities. How does one determine these things in clinical practice? The time course is self evident. The distribution and modalities afffected can also be determined largely from history and examination, and can be buttressed by EMG/NCS. To reliably determine the nature of the primary pathology, one needs electrodiagnostic studies and, at times nerve biopsy as well, 9 although experienced clinicians can often make an educated judgement regarding the pathologic process on the basis of clinical findings. Most neuropathies are chronic, involve both sensory and motor fibers to some degree, and conform to one of the following four patterns: multifocal vasculiti sinfiltrative MMN/LSS CIDP metaboli c toxic diffuse nutritional CMT II axona l CMT I demyelinati ng 1. Symmetric, sensory-predominant, axonal polyneuropathy. This is the pattern seen with most metabolic, toxic, and nutritional causes of polyneuropathy, and is thus the pattern most commonly seen by physicians in primary care. These neuropathies are lengthdependent; that is, the longest nerves are affected first. This seems consistent with the concept that the longest axons, which have the greatest metabolic demand, the greatest exposure to external stresses, and perhaps the greatest vulnerability to conditions which compromise transport mechanisms, axonal membrane, or other structures, might be most vulnerable to systemic toxic, metabolic, or nutritional disorders. These neuropathies are rarely associated with clinically significant weakness. Thus, the clinical presentation is of numbness, often accompanied by paresthesias, burning discomfort, and sensitivity to touch, in the toes and feet. Initial clinical findings are loss of sensation in the distal lower limbs, followed by loss of Achilles' reflexes and weakness of the intrinsic foot muscles. Examples of known etiologies of such a presentation include diabetes, alcohol abuse, and vincristine. The etiology in this syndrome is often unknown, and management generally consists of treating the causative condition, if known, and treatment of pain. These neuropathies usually develop gradually over a period of months to years. 10 2. Very symmetric sensorimotor axonal or demyelinating neuropathy. The presence of significant numbness and weakness in a symmetric, length-dependent fashion, generally manifesting as sensory loss in the feet and ankle dorsiflexion weakness ("foot drop"), should bring to mind an inherited sensorimotor polyneuropathy, or Charcot-Marie Tooth (CMT). Though there are some important exceptions, most inherited sensorimotor neuropathies present in this fashion, and are notable for their exquisite symmetry. Nerve conduction studies in CMT demonstrate either striking slowing of conduction, indicating a primary disorder of myelin (CMT I), or low amplitude responses with normal or near-normal conduction, indicating a primary axonal disorder (CMT II). Regardless of the primary pathology, disability in CMT develops because of progressive loss of axons. Thus, patients with CMT I demonstrate very slow nerve conduction velocity throughout life but only develop disability gradually as axons degenerate. This illustrates two important points: first, conduction slowing alone does not cause weakness or numbness. Clinical dysfunction due to disorders of myelin is due to secondary axon loss or conduction block (block of the wave of depolarization due to focal demyelination, a problem encountered in CIDP (see below) but not CMT). Second, genetic disorders of myelin lead to axon loss, indicating that normal myelin plays a role in maintaining normal axons. Symptoms in CMT often develop in adolescence or early adulthood and progress gradually throughout adult life. 3. Variably asymmetric or multifocal demyelinating neuropathy. When a neuropathy is not quite as exquisitely symmetric as CMT I or CMT II and the EMG/NCS suggests that demyelination is the primary pathologic process, one should consider Chronic Inflammatory Demyelinating Polyradiculoneuropathy, or CIDP. This is a relatively common acquired neuropathy due to immune mediated demyelination. CIDP is usually bilateral but not quite as symmetric as CMT I or II, and is occasionally overtly multifocal. CIDP can be sensory or motor predominant but usually has overt clinical evidence of both. The diagnosis can be supported by CSF examination, which characteristically demonstrates a high protein without a cellular infiltrate (albuminocytologic dissociation; see Guillain-Barre Syndrome), and by evidence of demyelination on nerve biopsy. CIDP is usually treated with corticosteroids, intravenous immunoglubulin, plasma exchange, or cyclophosphamide. CIDP generally presents with progressive symptoms over a period of months and, untreated, can run a continuously progressive or relapsing/remitting course. Although CMT I and II are symmetric, the differential diagnosis of a slightly asymmetric or multifocal demyelinating polyneuropathy does include two other inherited neuropathies, Hereditary Neuropathy with Liability to Pressure Palsies (HNPP) and X-linked CMT (CMTX), which can be identified by genetic testing. 4. Multifocal axonal neuropathy, often referred to as "mononeuropathy multiplex." In this pattern, individual nerves are affected in a patchy fashion; for example, such a patient might present with a left median neuropathy, followed shortly thereafter by a right 11 peroneal neuropathy, then a right sixth cranial nerve palsy. Mononeuropathy multiplex can affect sensory or motor axons but usually involves both. The most common etiologies are vasculitis and infiltrative disorders, such as sarcoidosis and lymphoma, in which there is direct infiltration of cells into affected peripheral nerves. Diagnosis usually rests upon biopsy of a nerve or another affected tissue. Acute polyneuropathies Most neuropathies develop gradually over months to years. There are relatively few conditions which cause an acute polyneuropathy. The most important cause of acute polyneuropathy is Guillain-Barre Syndrome (GBS). This is a rapidly progressive, motorpredominant, diffuse demyelinating polyradiculoneuropathy. Classically, GBS presents as a nearly symmetric, progressive hyporeflexic and ultimately areflexic quadriparesis which nearly always resolves spontaneously but which can lead to sufficient weakness to require mechanical ventilation at its nadir. GBS is usually accompanied by bothersome sensory symptoms but rather modest sensory findings. There is often striking autonomic involvement, leading to a resting tachycardia and dramatic fluctuations in blood pressure. GBS often follows a systemic infection by several weeks, an observation which is consistent with the view that it is of autoimmune etiology and is sometimes triggered by an immune attack upon a foreign antigen which shares an epitope with a component of peripheral nerve. Pathologically it is characterized by macrophage-mediated segmental demyelination of nerve and nerve roots, followed by remyelination in the recovery phase. The clinical diagnosis is confirmed by EMG/NCS confirmation of a demyelinative process and by “albuminocytologic dissociation;" that is, the finding of an elevated CSF protein, reflective of stripping of myelin proteins from nerve roots, without a CSF pleocytosis. Though most patients recover from GBS, the rate of recovery is accelerated by treatment with plasma exchange or intravenous imunoglobulin. Certain variants of GBS, including an axonal form as well as a post-infectious pure dysautonomia and post-infectious ataxia and ophthalmoplegia, have been described as well. Some toxic neuropathies, including neuropathies due to chemotherapeutic agents, can develop acutely as well. Findings isolated to one limb The discussion so far has focused on systemic neuromuscular disorders that usually affect more than one limb as well as the trunk or face. Some neuromuscular disorders present with findings isolated to one limb. In such cases, the differential diagnosis is generally between a radiculopathy, plexopathy, or mononeuropathy (disease of an individual nerve). The examiner is therefore obliged to carefully examine the reflexes, distribution of sensory deficits, and individual muscle groups, all the while thinking carefully about which neuroanatomic structure is common to all of the abnormal findings. 12 Radiculopathy, plexopathy, and mononeuropathy are usually due to extrinsic compression, trauma, or infiltration. Specifically, the most common causes of radiculopathy are extrinsic compression from herniated disk or foraminal osteophytes, infiltration from meningeal processes such as carcinomatous meningitis, lymphomatous meningitis, chronic meningeal infections, Lyme meningoradiculitis, or meningeal sarcoidosis, and root avulsion due to trauma. The most common causes of plexopathy are extrinsic compression from mass lesions, infiltration, trauma, and certain conditions specific to plexuses: neuralgic amyotrophy, a syndrome of severe proximal upper limb pain followed by weakness and atrophy, occurring most commonly in young adult men; lumbosacral radiculoplexopathy, a syndrome of severe proximal lower limb pain followed by weakness and atrophy, occurring most commonly in diabetics; and postradiation injury.The most common cause of mononeuropathies is compressive, either repetitive, minor trauma (median entrapment at the wrist, or carpal tunnel syndrome; ulnar entrapment at the elbow) or single episodes of prolonged compression (radial neuropathy at the spiral groove; peroneal neurpathy at the fibular head). Infiltration of malignant or inflammatory cells can also cause mononeuropathies, particularly of the cranial nerves, as can vasculitis. 13