DOLS Application Process: Plymouth Hospitals NHS Trust
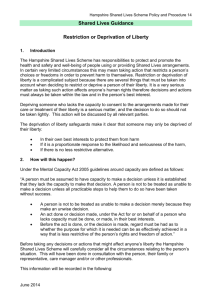
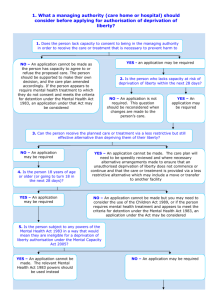
advertisement

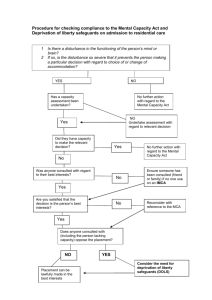
PLYMOUTH HOSPITALS NHS TRUST Process for application for Deprivation of Liberty Safeguards For people who lack mental capacity to consent to treatment which requires them to be in hospital in their best interest, in circumstances amounting to deprivation of their liberty Patient needs detaining or have their liberty deprived, for care/treatment in hospital See Restraining Therapies Policy restraint/deprivation must be proportionate to the risks to patient and least restrictive or invasive option Plan of care to be recorded restraint & staffing issues must be discussed with Matron Assess & record Mental Capacity (see over) Assess & Record patient for risks – ( see Restraining Therapies Risk Assessment) Review proposed treatment - planned procedures or continuation of care implemented urgently Undertake Best Interest Review (see over) Consider if proposed care/treatment constitutes Deprivation of Liberty This does NOT apply if patient : Has Mental Capacity Needs Mental Health Act assessment Is detained under criminal law (police, prison, court order) If patient has no family members or unpaid carer support - refer to IMCA to be involved in Best Interest review Independent Mental Capacity Advocates Tel 01752 305193 Is the patient under constant supervision or control? Do staff exercise complete & effective control over movement of person for significant period? Is the person prevented from maintaining contact with the outside world or social contacts? Are family, friends prevented from taking the patient to another care setting or out of ward? Is the person being prevented from leaving or being released to the care of others? Has a request by carers for a person to be discharged to their care been refused? Does the cumulative effect of all restrictions placed on a person amount to Deprivation of Liberty? Deprivation of liberty depends upon the degree or intensity of restriction - not simply the nature of restriction Refer for application for DOLS Clinical Team to complete authorisation forms – to be signed by Consultant and Nurse In charge Ensure the following are recorded: Mental Capacity Assessment Proposed treatment/care with timescales Best interest review Risk Assessments Involvement of family, carers, IMCA Restraining/deprivation of liberty required Short term restriction or deprivation for urgent treatment in patient’s best interest, is lawful if recorded and regularly reviewed. Advice regarding DOLS, involvement of IMCA or any other enquiry regarding the lawful detention of a patient under the Mental Capacity Act can be obtained through the city-wide DOLS office: Ballard House, West Hoe Road, Plymouth PL1 2AA Tel - 01752 308889 Fax 01752 308715 Roslynn.azzam@plymouth.gov.uk For Cornwall - Tel: 01872 324466 For Devon – Tel: 01392 381676 DOLS application process – Jan 2013 PLYMOUTH HOSPITALS NHS TRUST ASSESSMENT OF CAPACITY CHECKLIST The assessment of the patient’s mental capacity should be undertaken by the clinician making the decision for treatment or care, with involvement of other health professionals who may be able to assist in the assessment of capacity. The assessment of capacity must be recorded in the clinical records: Is the patient 16 years old or more? Have all reasonable steps been taken to facilitate capacity? (list as appropriate) Does the patient have impairment of, or disturbance in functioning of mind or brain? Does this impairment mean the patient cannot make specific decision when required? Is the incapacity permanent and or does decision need to be made before it is anticipated the patient will regain capacity? There are no clinically applicable Advance Directives, Lasting Power of Attorney (Personal Welfare LPA) or Court Appointed Deputy Are you satisfied the decision made regarding capacity has not been reached on the basis of unjustified assumptions (age, appearance, behaviour) Where the answer to all the above is ‘YES’ – the person is deemed to lack mental capacity to make decisions regarding the treatment or care in question Best Interest Checklist for Deprivation of Liberty A decision to undertake care or treatment for a patient using Best Interest principles, ONLY applies when: The patient lacks mental capacity for the decision re treatment/care The person is unlikely to regain capacity in relation to the specific decision: The patient is unable to: 1: Understand the information presented in a manner intended to help them do so 2: Retain that information long enough to make a decision 3: Use or weigh that information as part of the process of making the decision 4: Communicate the decision? In order to make a decision for care or treatment in the person’s Best Interest, the clinical decision maker MUST record in the clinical record: The person’s previous wishes, beliefs and feelings that would be likely to influence their decision if he or she had capacity been accounted for All relevant factors and circumstances that the person would have considered when making this decision. The involvement and consultation of anyone named by the patient as a significant other who an IMCA (Independent Mental Capacity Advocate) When considering Deprivation of Liberty Safeguards, the decision MUST be made and recorded as being in the patient’s Best Interest. Good practice re Best Interest decisions involves: Encouraging and enabling the patient to take part in making the decision Delaying the decision re care/treatment when there is a chance that the person will regain the capacity to make a particular decision, if it is not urgent Considering the person’s past and present wishes, feelings, beliefs and values Including the views of other people who are close to the person who lacks capacity Recording any risks of harm to the person if the deprivation of liberty does not take place; is the level of risk sufficient to justify a step as serious as depriving a person of liberty?) Considering other care options which could avoid deprivation of liberty DOLS application process – Jan 2013